Larynx, hypopharynx & trachea
General
Staging-larynx
Editor-in-Chief: Debra L. Zynger, M.D.
Last author update: 22 August 2019
Last staff update: 6 October 2022
Copyright: 2002-2024, PathologyOutlines.com, Inc.
PubMed Search: Staging larynx
Page views in 2023: 5,797
Page views in 2024 to date: 1,919
Cite this page: Magliocca K. Staging-larynx. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/larynxtnm.html. Accessed April 25th, 2024.
Definition / general
- Staging of definitive resections for carcinoma (squamous cell carcinoma, neuroendocrine carcinoma and minor salivary gland carcinoma) of the supraglottic, glottis and subglottic larynx should use this system
- Pyriform sinus represents part of the hypopharynx which expands bilaterally and forward around the sides of the larynx and lies between the larynx and the thyroid cartilage
- Cancers of the pyriform sinus are included in the protocol on pharynx cancers
- Staging protocols such as those of CAP document procedure, tumor site, transglottic extension, tumor laterality, tumor focality, tumor size, histologic type, histologic grade for squamous cell carcinoma, margin status, lymphovascular invasion, perineural invasion, regional lymph node findings and summarize these pathologic findings using TNM system
Anatomy
- Anatomic boundaries of the larynx (AJCC: Cancer Staging [Accessed 26 September 2018], CAP: Protocol for the Examination of Specimens from Patients with Cancers of the Larynx [Accessed 26 September 2018]):
- Anterior limit of the larynx is composed of the anterior or lingual surface of the suprahyoid epiglottis, the thyrohyoid membrane, the anterior commissure and the anterior wall of the subglottic region, which is composed of the thyroid cartilage, the cricothyroid membrane and the anterior arch of the cricoid cartilage
- Posterior and lateral limits include the laryngeal aspect of the aryepiglottic fold, the arytenoid region, the interarytenoid space and the posterior surface of the subglottic space represented by the mucous membrane covering the surface of the cricoid cartilage
- Superolateral limits are composed of the tip and the lateral borders of the epiglottis
- Inferior limits are made up of the plane passing through the inferior edge of the cricoid cartilage
- Anatomic compartments, sites and subsites for the larynx (AJCC: Cancer Staging [Accessed 26 September 2018], CAP: Protocol for the Examination of Specimens from Patients with Cancers of the Larynx [Accessed 26 September 2018], see figure 1 in Diagrams / tables):
- Supraglottis: extends from the tip of the epiglottis to a horizontal line passing through the apex of the ventricle
- Epilarynx, including marginal zone
- Suprahyoid epiglottis, including tip, lingual (anterior) and laryngeal surfaces
- Aryepiglottic fold, laryngeal aspect
- Arytenoid
- Supraglottis, excluding epilarynx
- Infrahyoid epiglottis
- Ventricular bands (false cords)
- Ventricle
- Glottis: extends from the ventricle to approximately 0.5 - 1.0 cm below the free level of the true vocal cord
- Vocal cords
- Anterior commissure
- Posterior commissure
- Subglottis: extends approximately 1.0 cm below the level of the true vocal cord to the inferior rim of the cricoid cartilage
- Subglottis has no additional subsites
- Additional anatomic compartments (AJCC: Cancer Staging [Accessed 26 September 2018], CAP: Protocol for the Examination of Specimens from Patients with Cancers of the Larynx [Accessed 26 September 2018]):
- Paraglottic space is a potential space deep to the ventricles and saccules filled with adipose tissue and connective tissue (see figure 2 in Diagrams / tables)
- It is bounded by the conus elasticus inferiorly, the thyroid cartilage laterally, the quadrangular membrane medially and the piriform sinus posteriorly
- Pre-epiglottic space, like the paraglottic space, is filled with adipose tissue and connective tissue (see figure 3 in Diagrams / tables)
- It is triangular in shape and is bounded by the thyroid cartilage and thyrohyoid membrane anteriorly, the epiglottis and thyroepiglottic ligament posteriorly and the hyoepiglottic ligament at its base (see figures 1 and 2 Diagrams / tables)
- Paraglottic and preglottic spaces contain lymphatics and blood vessels but no lymph nodes
- Site specific carcinomas (AJCC: Cancer Staging [Accessed 26 September 2018], CAP: Protocol for the Examination of Specimens from Patients with Cancers of the Larynx [Accessed 26 September 2018]):
- Supraglottic squamous cell carcinoma: a squamous cell carcinoma that involves the structures of the supraglottic larynx, including the epiglottis (laryngeal and lingual surfaces), aryepiglottic folds, arytenoids, false vocal cords and ventricles
- Glottic squamous cell carcinoma: a squamous cell carcinoma that involves the structures of the glottis, including the true vocal cords and the anterior and posterior commissures
- Subglottic squamous cell carcinoma: a squamous cell carcinoma that involves the subglottis, which begins 1 cm below the apex of the ventricle to its inferior border represented by the rim of the cricoid cartilage
- Transglottic carcinoma: a carcinoma that crosses the ventricles in a vertical direction arising in either the glottic or supraglottic larynx
ICD coding
- ICD-10:
- C10.1 - anterior (lingual) surface of epiglottis
- C32.0 - glottis
- C32.1 - supraglottis (laryngeal surface)
- C32.2 -subglottis
- C32.8 - overlapping lesion of larynx*
- C32.9 - larynx, NOS*
* Stage by location of tumor bulk or epicenter
Diagrams / tables
Images hosted on other servers:

Anatomic compartments

Paraglottic space

Pre-epiglottic space


Levels of neck
Primary tumor (pT) - supraglottis
- pTX: Primary tumor cannot be assessed
- pTis: Carcinoma in situ
- pT1: Tumor limited to 1 subsite of supraglottis with normal vocal cord mobility
- pT2: Tumor invades mucosa of > 1 adjacent subsite of supraglottis or glottis or region outside the supraglottis (e.g. mucosa of base of tongue, vallecula, medial wall of pyriform sinus) without fixation of the larynx
- pT3: Tumor limited to larynx with vocal cord fixation or invades any of the following: postcricoid area, pre-epiglottic space, paraglottic space or inner cortex of thyroid cartilage
- pT4a: Moderately advanced local disease: invades through the outer cortex thyroid cartilage or invades tissues beyond the larynx (e.g. trachea, soft tissues of neck including deep extrinsic muscle of tongue, strap muscles, thyroid or esophagus)
- pT4b: Very advanced local disease: invades prevertebral space, encases carotid artery or invades mediastinal structure
Primary tumor (pT) - glottis
- pTX: Primary tumor cannot be assessed
- pTis: Carcinoma in situ
- pT1: Tumor limited to the vocal cord(s) (may involve anterior or posterior commissure) with normal mobility
- pT1a: Limited to 1 vocal cord
- pT1b: Involves both vocal cords
- pT2: Tumor extends to supraglottis or subglottis or with impaired vocal cord mobility
- pT3: Tumor limited to the larynx with vocal cord fixation or invasion of paraglottic space or inner cortex of the thyroid cartilage
- pT4a: Moderately advanced local disease: invades through the outer cortex of the thyroid cartilage or invades tissues beyond the larynx (e.g. trachea, cricoid cartilage, soft tissues of neck including deep extrinsic muscle of the tongue, strap muscles, thyroid or esophagus)
- pT4b: Very advanced local disease: invades prevertebral space, encases carotid artery or invades mediastinal structures
Primary tumor (pT) - subglottis
- pTX: Primary tumor cannot be assessed
- pTis: Carcinoma in situ
- pT1: Tumor limited to subglottis
- pT2: Tumor extends to vocal cord(s) with normal or impaired mobility
- pT3: Tumor limited to larynx with vocal cord fixation or invasion of paraglottic space or inner cortex of the thyroid cartilage
- pT4a: Moderately advanced local disease: tumor invades cricoid or thyroid cartilage or invades tissues beyond the larynx (e.g. trachea, soft tissues of neck including deep extrinsic muscles of the tongue, strap muscles, thyroid or esophagus)
- pT4b: Very advanced local disease: tumor invades prevertebral space, encases carotid artery or invades mediastinal structures
Pathological regional lymph nodes (pN)
- pNX: Regional lymph nodes cannot be assessed
- pN0: No regional lymph node metastasis
- pN1: Metastasis in a single ipsilateral lymph node ≤ 3 cm in greatest dimension and extranodal extension (ENE)-
- pN2a: Single ipsilateral lymph node ≤ 3 cm and ENE+ or single ipsilateral lymph node > 3 cm but ≤ 6 cm in greatest dimension and ENE-
- pN2b: Metastases in multiple ipsilateral lymph nodes, none > 6 cm in greatest dimension and ENE-
- pN2c: Metastases in bilateral or contralateral lymph node(s), none > 6 cm in greatest dimension and ENE-
- pN3a: Metastasis in a lymph node that is > 6 cm in greatest dimension and ENE-
- pN3b: Metastasis in either
- Single ipsilateral lymph node, > 3 cm and ENE+ or
- Multiple ipsilateral, contralateral or bilateral lymph nodes, any with ENE+ or
- Single contralateral lymph node of any size and ENE+
Notes:
- Designation of "U" or "L" may be used for any N category to indicate metastasis above the lower border of the cricoid (U) or below the lower border of the cricoid (L)
- Per AJCC 8th edition, for pN, a selective neck dissection ordinarily will include > 10 lymph nodes and a radical or modified radical neck dissection ordinarily will include > 15 lymph nodes
- Negative pathologic examination of a smaller number of nodes still mandates a pN0 designation
- Midline nodes are considered ipsilateral nodes
- Extranodal extension (ENE)
- All macroscopically negative or equivocal lymph nodes should be submitted in toto
- Grossly positive nodes may be partially submitted for microscopic documentation of metastasis
- Reporting of lymph nodes containing metastasis should include whether there is presence or absence of extranodal extension (ENE), which is now part of N staging
- This finding consists of extension of metastatic tumor, present within the confines of the lymph node, through the lymph node capsule into the surrounding connective tissue, with or without associated stromal reaction
- Distance of extension from the native lymph node capsule is now suggested (but not yet required) with the proposed stratification of ENE into ENEma (> 2 mm) and ENEmi (≤ 2 mm)
- However, pitfalls in the measurement (i.e. in larger, matted lymph nodes, in nodes post fine needle aspiration and in nodes with near total replacement of lymph node architecture) and the disposition of soft tissue deposits are still not resolved
- In general, absence of ENE in a large (> 3 cm) lymph node, especially with traversing fibrous bands, should be viewed with skepticism
- Soft tissue deposits for lymph node metastases based on limited studies appear to be the equivalent of a positive lymph node with ENE and should be recorded as such
- Measurement of lymph node metastasis
- Cross sectional diameter of the largest lymph node metastatic deposit (not the lymph node itself) is measured in the gross specimen at the time of macroscopic examination or if necessary, on the histologic slide at the time of microscopic examination
AJCC prognostic stage grouping
| Stage 0:
| Tis
| N0
| M0
|
| Stage I:
| T1
| N0
| M0
|
| Stage II:
| T2
| N0
| M0
|
| Stage III:
| T3
| N0
| M0
|
|
| T1 - 3
| N1
| M0
|
| Stage IVA:
| T4a
| N0 - 1
| M0
|
|
| T1 - 4a
| N2
| M0
|
| Stage IVB:
| Any T
| N3
| M0
|
|
| T4b
| Any N
| M0
|
| Stage IVC:
| Any T
| Any N
| M1
|
Registry data collection variables
- ENE clinical (present versus absent)
- ENE pathological (present versus absent)
- Extent of microscopic ENE (distance of extension from the native lymph node capsule to the farthest point of invasion in extranodal tissue)
- Perineural invasion
- Lymphovascular invasion
- Performance status
- Tobacco use and pack year
- Alcohol use
- Depression diagnosis
Histologic grade
- GX: Cannot be assessed
- G1: Well differentiated
- G2: Moderately differentiated
- G3: Poorly differentiated
Notes:
- For histologic types of carcinomas that are amenable to grading, 3 histologic grades are suggested, as shown below (AJCC: Cancer Staging [Accessed 26 September 2018], CAP: Protocol for the Examination of Specimens from Patients with Cancers of the Larynx [Accessed 26 September 2018])
- For conventional squamous cell carcinoma, histologic grading as a whole does not perform well as a prognosticator
- Nonetheless, it should be recorded when applicable as it is a basic tumor characteristic
- Selecting either the most prevalent grade or the highest grade for this synoptic protocol is acceptable
- Variants of squamous cell carcinoma (i.e. verrucous, basaloid, etc.) have an intrinsic biologic potential and currently do not appear to require grading
- Histologic (microscopic) grading of salivary gland carcinomas has been shown to be an independent predictor of behavior and plays a role in optimizing therapy
- However, most salivary gland carcinoma types have an intrinsic biologic behavior and attempted application of a universal grading scheme is merely a crude surrogate
- Thus, a generic grading scheme is no longer recommended for salivary gland carcinomas
- Carcinoma types for which grading systems exist and are relevant are incorporated into histologic type
- 3 major categories that are amenable to grading include adenoid cystic carcinoma, mucoepidermoid carcinoma and adenocarcinoma, not otherwise specified
- In some carcinomas, histologic grading may be based on growth pattern, such as in adenoid cystic carcinoma, for which a histologic high grade variant has been recognized based on the percentage of solid growth
- Those adenoid cystic carcinomas showing ≥ 30% of solid growth pattern are considered to be histologically high grade carcinomas
- Histologic grading of mucoepidermoid carcinoma includes a combination of growth pattern characteristics (e.g. cystic, solid, neurotropism) and cytomorphologic findings (e.g. anaplasia, mitoses, necrosis)
- Adenocarcinomas, not otherwise specified, do not have a formalized grading scheme and are graded intuitively based on cytomorphologic features
Histopathologic type
- Predominant cancer is squamous cell carcinoma
- Staging guidelines are applicable to all forms of epithelial carcinoma including those arising from minor salivary glands
- Other nonepithelial tumors such as lymphoid tissue, bone, cartilage (i.e. lymphoma and sarcoma) are not included
- Squamous cell carcinoma (conventional, variants)
- Carcinoma of minor salivary gland
- Acinic cell
- Adenoid cystic
- Adenocarcinoma, NOS
- Basal cell adenocarcinoma
- Carcinoma ex pleomorphic adenoma
- Carcinoma type cannot be determined
- Carcinosarcoma
- Clear cell adenocarcinoma
- Cystadenocarcinoma
- Epithelial myoepithelial carcinoma
- Mammary analogue secretory carcinoma
- Mucoepidermoid carcinoma
- Mucinous carcinoma
- Myoepithelial carcinoma
- Oncocytic carcinoma
- Polymorphous adenocarcinoma
- Salivary duct carcinoma
- Non salivary gland adenocarcinoma
- Neuroendocrine carcinoma
- Well differentiated neuroendocrine carcinoma (typical carcinoid tumor)
- Moderately differentiated neuroendocrine carcinoma (atypical carcinoid tumor)
- Poorly differentiated neuroendocrine carcinoma, small cell type
- Poorly differentiated neuroendocrine carcinoma, large cell type
- Combined (or composite) neuroendocrine carcinoma (specify types)
- Carcinoma type cannot be determined
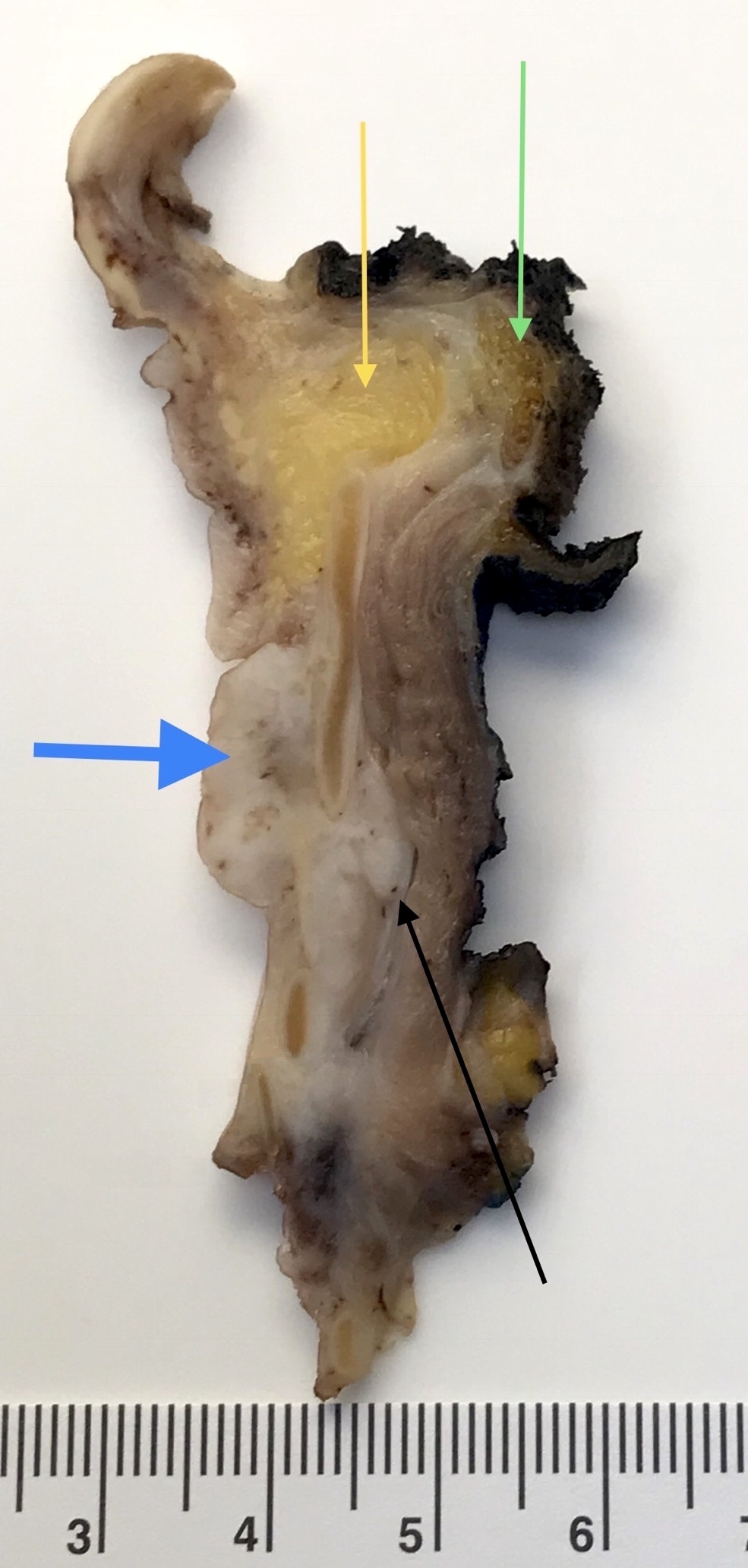
Gross images
Contributed by Kelly R. Magliocca, D.D.S., M.P.H.
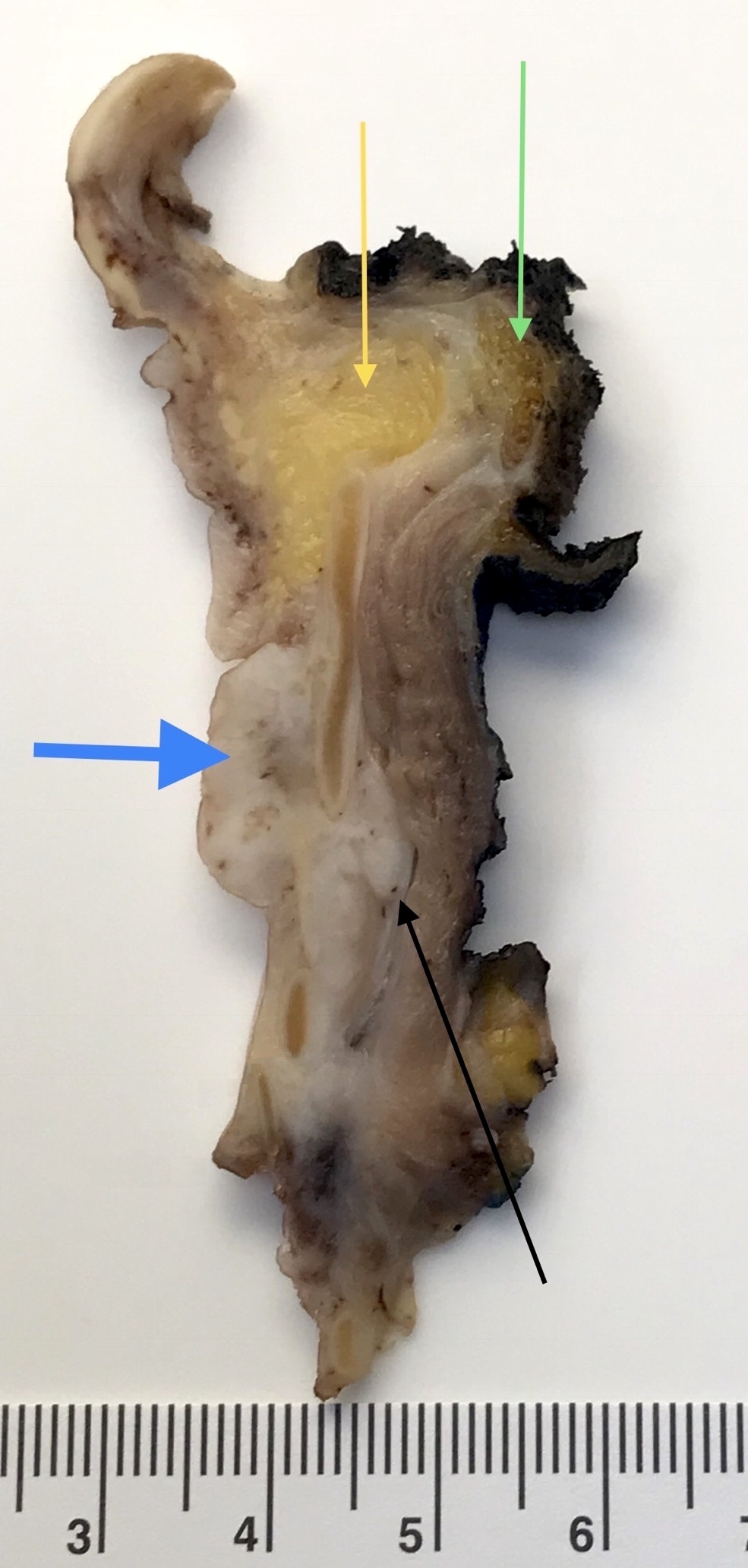
Glottic tumor (pT4)
Board review style question #1
Regarding laryngeal squamous cell carcinoma, which of the pT category criteria in the 8th edition AJCC staging guide is likely to be satisfied by examination of this parasagittal section taken through the right side of a total laryngectomy specimen?
- pT2 due to infiltration of paraglottic space
- pT3 due to extension into pre-epiglottic space
- pT3 due to subglottic extension
- pT4a due to extralaryngeal extension
Board review style answer #1
Back to top