Table of Contents
Definition / general | Clinical features | Case reports | Microscopic (histologic) description | Microscopic (histologic) images | Peripheral smear images | Positive stains | Negative stains | Flow cytometry description | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Differential diagnosisCite this page: Mihova D. AML without maturation (FAB AML M1). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/leukemiaM1.html. Accessed April 23rd, 2024.
Definition / general
- 10 - 20% of AML cases, 44% in one Brazil hospital (Sao Paulo Med J 2006;124:45)
- Usually adults (median age 46 years), present with anemia, thrombocytopenia and neutropenia; may have leukocytosis with markedly increased blasts
- 4% of childhood AML
Clinical features
- Criteria for diagnosis: 90%+ of nonerythroid cells in marrow are myeloblasts; < 10% granulocytic elements; 3%+ of blasts must be positive for myeloperoxidase or Sudan Black B and / or Auer rods by enzyme cytochemistry
- Enzyme cytochemistry: 3%+ of blasts are positive for myeloperoxidase or Sudan Black B (confirm by immunohistochemistry if only 3 - 10% positive for MPO by enzyme cytochemistry); chloroacetate esterase positive
- Poor prognosis
Case reports
- 4 year old child with t(6;9) and basophilia (Ann Biol Clin (Paris) 2003;61:352)
- 44 year old man with large and small blasts (Arch Pathol Lab Med 2004;128:448)
- Presenting with arterial thromboembolism (Leuk Res 2007;31:869)
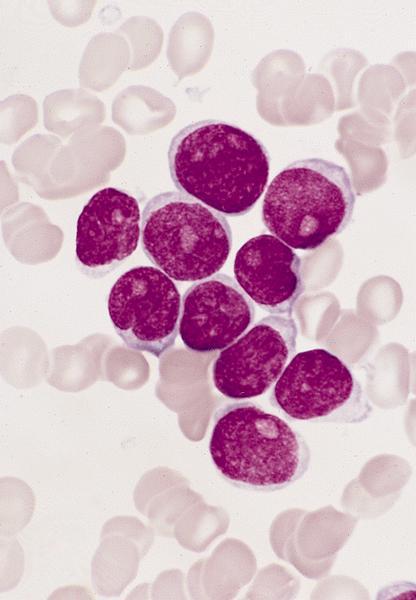
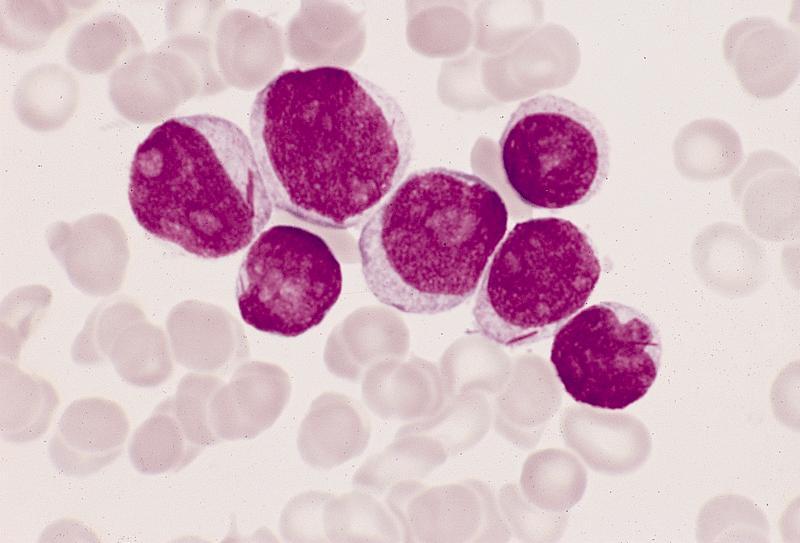
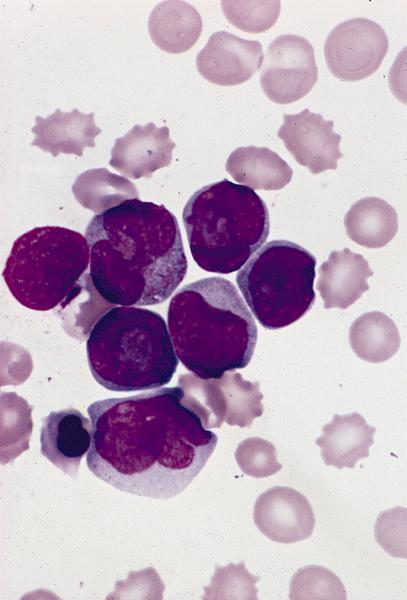
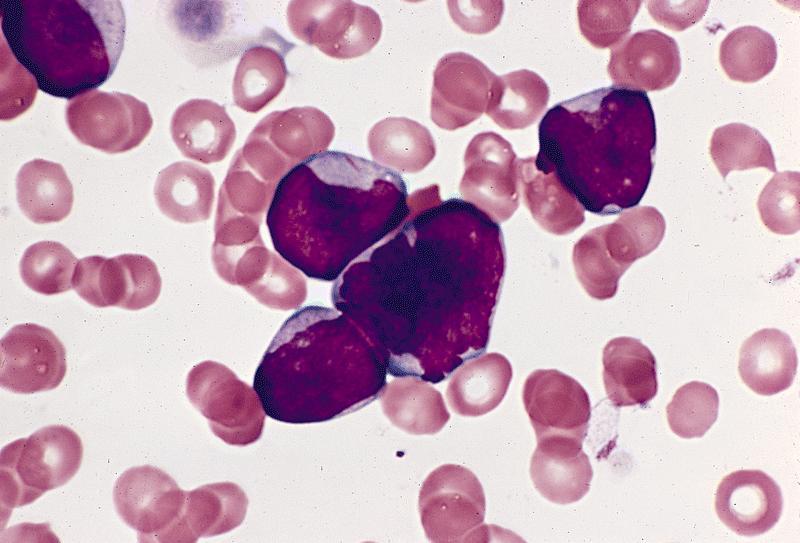
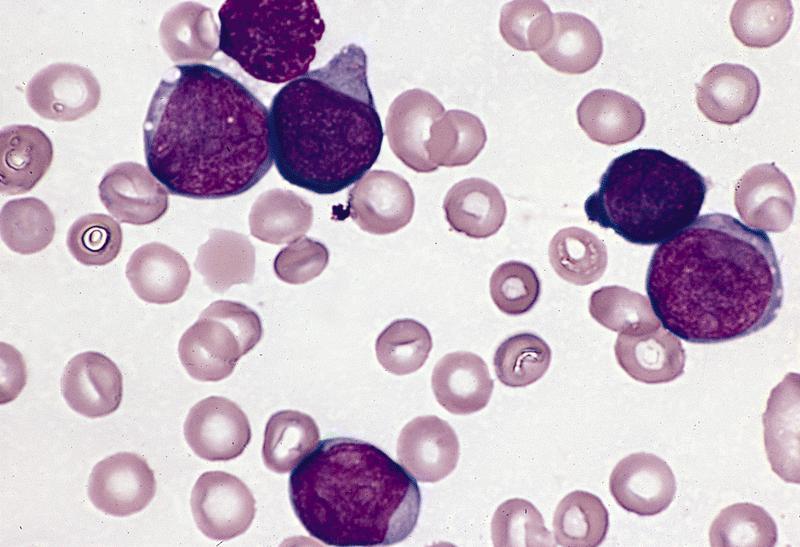
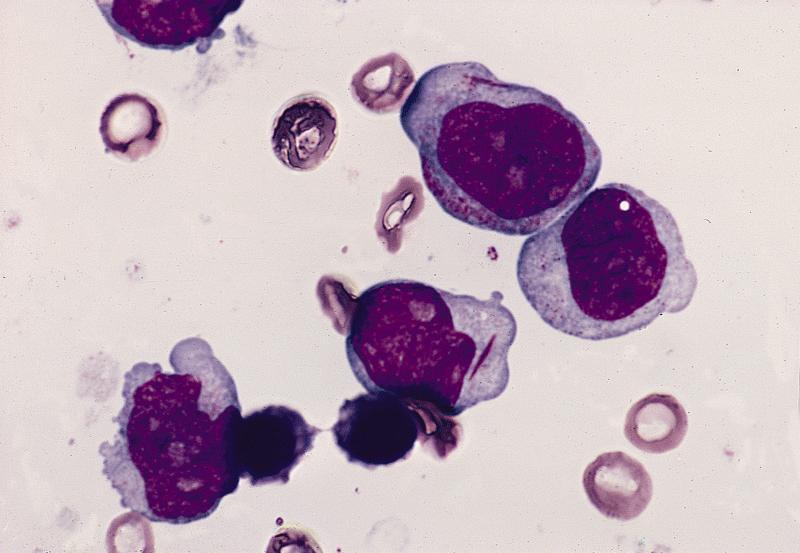
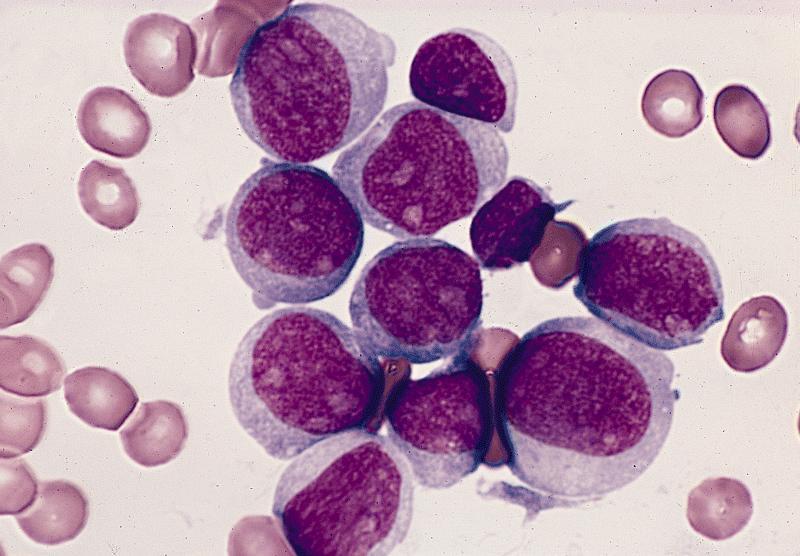
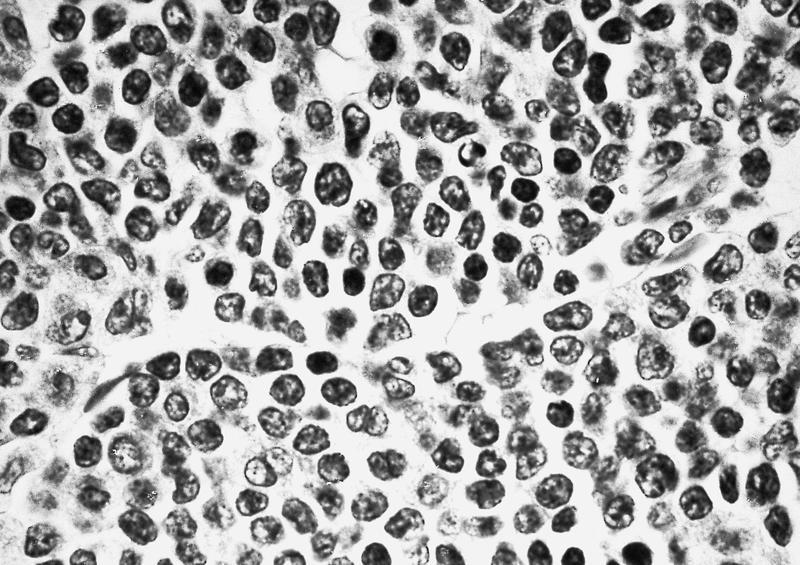
Microscopic (histologic) description
- Typically markedly hypercellular marrow, but normocellular and hypocellular cases occur
- Very immature cells, usually round with few azurophilic cytoplasmic granules or Auer rods
- Nuclei are round or indented; little maturation beyond myeloblast stage
- Cells may may resemble lymphoblasts and not appear myeloid
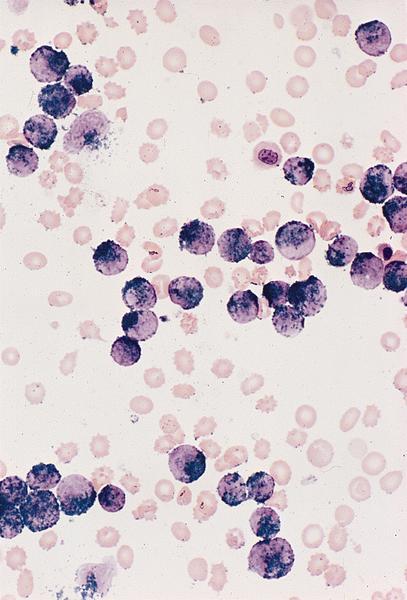
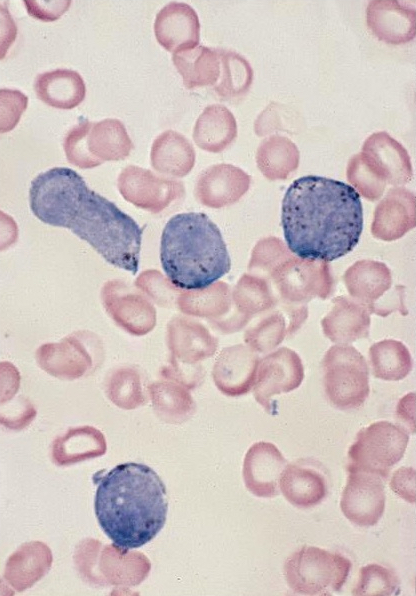
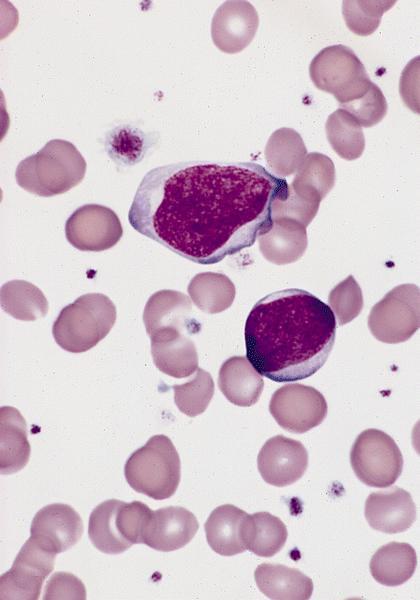
Microscopic (histologic) images
AFIP images
Positive stains
Negative stains
Flow cytometry description
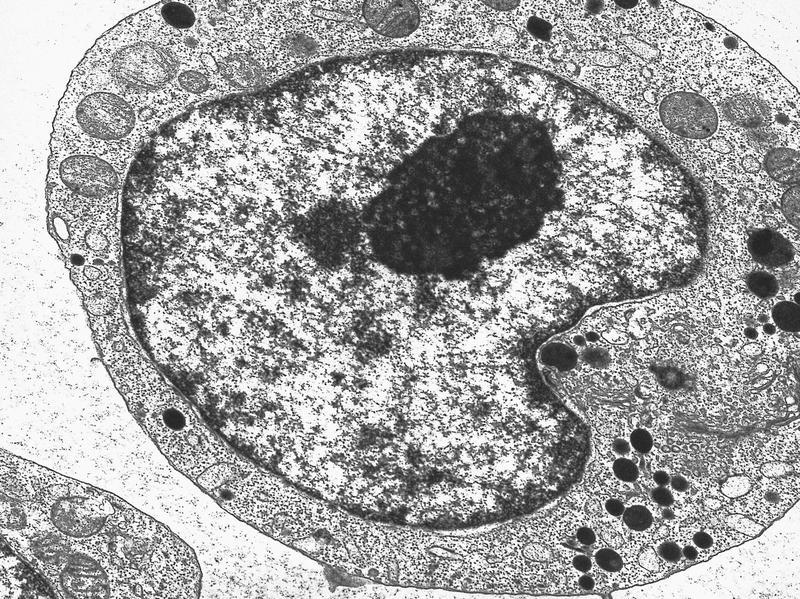
Electron microscopy description
- May have heterogeneous features (Ultrastruct Pathol 1995;19:9)
Molecular / cytogenetics description
- Associated with t(8;21)
- FLT3 ITD in 22% (Ai Zheng 2007;26:58)
- FLT3 mutations associated with HLA-DR negative patients (Leuk Res 2007;31:921)