Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Flow cytometry description | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Khattar P, Bedi P, Yabe M. Acute basophilic leukemia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/leukemiabasophil.html. Accessed April 19th, 2024.
Definition / general
- First described (basophilic leukemia) in 1906 by Joachim (Dtsch Arch Klin Med 1906;87:437)
- Acute myeloid leukemia (AML) with primary differentiation to basophils
- To qualify as a type of AML, not otherwise specificed (NOS), other specifically described groups (i.e. AML with myelodysplasia related changes, therapy related AML or AML with recurrent genetic abnormalities) must be excluded
- Wide age range, 1 day - 82 years (Leuk Lymphoma 1999;32:269)
- Rapid clinical progression
Essential features
- First step in diagnosis is the recognition of the presence of coarse basophilic granules
- Immunophenotyping and electron microscopy features are essential to identify basophilic lineage
- Crucial to differentiate basophilic cells from mast cells
- Diagnosis of acute basophilic leukemia (J Clin Oncol 2011;29:e623):
- Circulating peripheral blood and bone marrow immature basophils / blasts
- Positive with metachromatic staining (toluidine blue), acid phosphatase (diffuse pattern), some cases with periodic acid Schiff (PAS) positivity in large blocks
- Negative for myeloperoxidase (MPO), Sudan black B (SBB) or naphthol ASD chloroacetate esterase (CAE)
- Circulating peripheral blood and bone marrow immature basophils / blasts
Terminology
- Basophilic leukemia (no longer used)
ICD coding
Epidemiology
- Rare disease
- ~ 4 - 5% of all cases of acute nonlymphocytic leukemia and < 2% of all hematopoietic malignancies (Leuk Lymphoma 1999;32:269)
Sites
- Peripheral blood, bone marrow, skin, organomegaly
Diagrams / tables
| Immunophenotypic profile of basophils, plasmacytoid dendritic cells (pDC) and mast cells | ||||
| CD203c | Positive | Positive | Negative | Positive |
| CD123 | Positive | Positive / Negative | Positive | Negative |
| HLA-DR | Negative | Positive / Negative | Positive (high) | Positive (low) |
| CD34 | Negative | Negative | Negative | Negative |
| CD117 | Negative | Negative | Negative | Positive |
| CD38 | Positive | Positive / Negative | Negative | Positive (low) |
| CD33 | Positive | Positive / Negative | Negative | Positive (moderate) |
| CD64 | Negative | Positive / Negative | Negative | Negative |
Clinical features
- Wide age range: 1 day - 82 years (Leuk Lymphoma 1999;32:269)
- Typically presents with bone marrow failure
- Variable circulating blasts
- Cutaneous involvement (due to high histamine levels): pruritus, edema, urticarial rashes, focal hyperpigmentation
- GI symptoms: nausea, vomiting, diarrhea, dyspepsia, abdominal swelling or ulcers
- Organomegaly and lytic lesions
Diagnosis
- Prerequisite for the diagnosis of acute basophilic leukemia (ABL) and chronic basophilic leukemia (CBL) (Leukemia 2017;31:788)
- Presence of hyperbasophilia (HB) (absolute basophil count exceeding 1,000 per microliter of peripheral blood (PB), present for over at least 8 weeks)
- Percentage of basophils must be ≥ 40% of total leukocytes
- Basophils must belong to the malignant clone as evidenced by
- (Immature) morphology of basophils
- Type of underlying neoplasm (myeloid), if present
- Presence of cytogenetic or molecular alterations is helpful for establishing clonality
- It is important to distinguish ABL from CBL:
- ABL: HB criteria + basophils ≥ 40% of nucleated bone marrow or PB cells + myeloblasts +
metachromatic blasts ≥ 20%
- Primary ABL: no preceding / underlying bone marrow neoplasm
- Secondary ABL: known preceding / underlying bone marrow neoplasm
- CBL: HB criteria + basophils ≥ 40% of nucleated bone marrow or PB cells + myeloblasts +
metachromatic blasts < 20%
- Primary CBL: no preceding / underlying bone marrow neoplasm
- Secondary CBL: known preceding / underlying bone marrow neoplasm
- ABL: HB criteria + basophils ≥ 40% of nucleated bone marrow or PB cells + myeloblasts +
metachromatic blasts ≥ 20%
Laboratory
- CT scan for spleen size and lymph node status
- Complete blood count - white blood cell, hemoglobin, platelets, differential leukocyte count (basophil)
- Serum chemistry, including serum tryptase level
- Allergy diagnostics, including total IgE
- Inflammation markers (C reactive protein (CRP), erythrocyte sedimentation rate (ESR))
- Bone marrow histology (biopsy, clot and smears) and immunohistochemistry
- Chromosome analysis and extended FISH panel for myelodysplastic syndromes (MDS) or myeloproliferative neoplasms (MPN)
- Molecular studies / next generation sequencing panel:
- BCR-ABL1 to be excluded by real time PCR or FISH
- JAK2 V617F by real time PCR
- JAK2 exon 12
- MPL mutation
- CALR mutation
- FIP1L1-PDGFRA by real time PCR or FISH
- Reference: Leukemia 2017;31:788
Prognostic factors
- Poor prognosis
- Survival time ranges from 2 to > 36 months in chronic basophilic leukemia (CBL); 2 to 16 months in acute basophilic leukemia (ABL) (Leukemia 2017;31:788)
Case reports
- 44 year old woman with trisomy 19 and t(9;22) and acute basophilic leukemia (Case Rep Pathol 2011;2011:269491)
- 63 year old man presenting with infectious pneumopathy (Am J Hematol 2004;76:134)
- 63 year old woman with history of MDS with isolated del(5q) (Br J Haematol 2019;185:817)
- 63 year old woman with FLT3 ITD+ acute basophilic leukemia with rare complex karyotype presenting with acute respiratory failure (Rev Romana Med Lab 2018;26:87)
- 65 year old man with leukocytosis; acute basophilic leukemia with t(16;21)(p11;q22) generating the FUS‐ERG fusion gene (Clin Case Rep 2017;5:1938)
- 74 year old woman with a history of acute myeloid leukemia (Blood 2014;123:3071)
- 82 year old woman with acute basophilic leukemia associated with loss of gene ETV6 and protean complications (J Clin Oncol 2011;29:e623)
- Acute basophilic leukemia with add(3)(q12) accompanied by histamine excess symptoms (Ann Hematol 2017;96:1197)
- Acute basophilic leukemia with U2AF1 mutation (Blood Cells Mol Dis 2019;76:63)
Treatment
- Stem cell transplant (SCT)
- If SCT is not possible, polychemotherapy, targeted drugs, experimental drugs or palliative cytoreductive treatment
- Histamine related symptoms (if HB is present): prophylactic histamine receptor (HR) antagonists (HR1 and HR2 blocker), proton pump inhibitors and steroids
- Combination of daunorubicin / idarubicin and cytarabine (Oncol Lett 2014;8:2513)
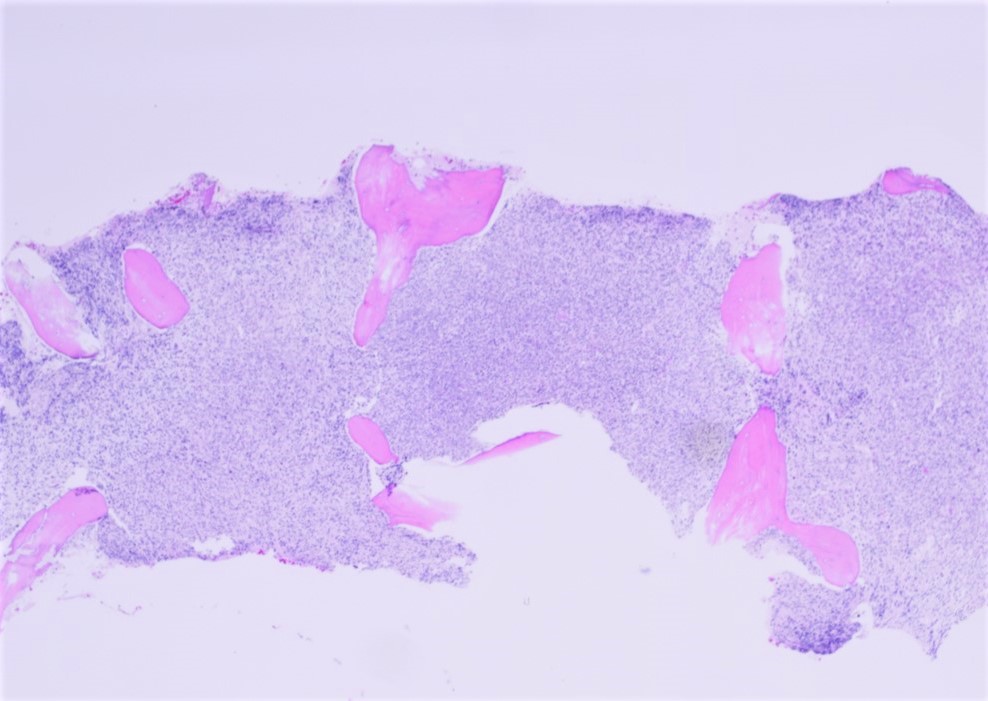
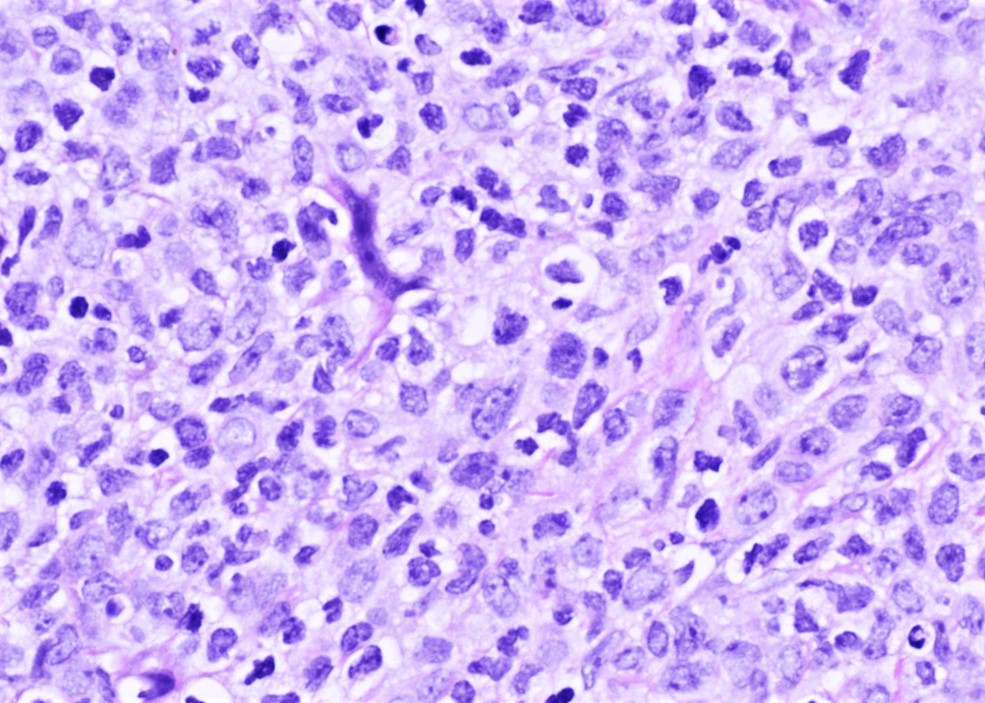
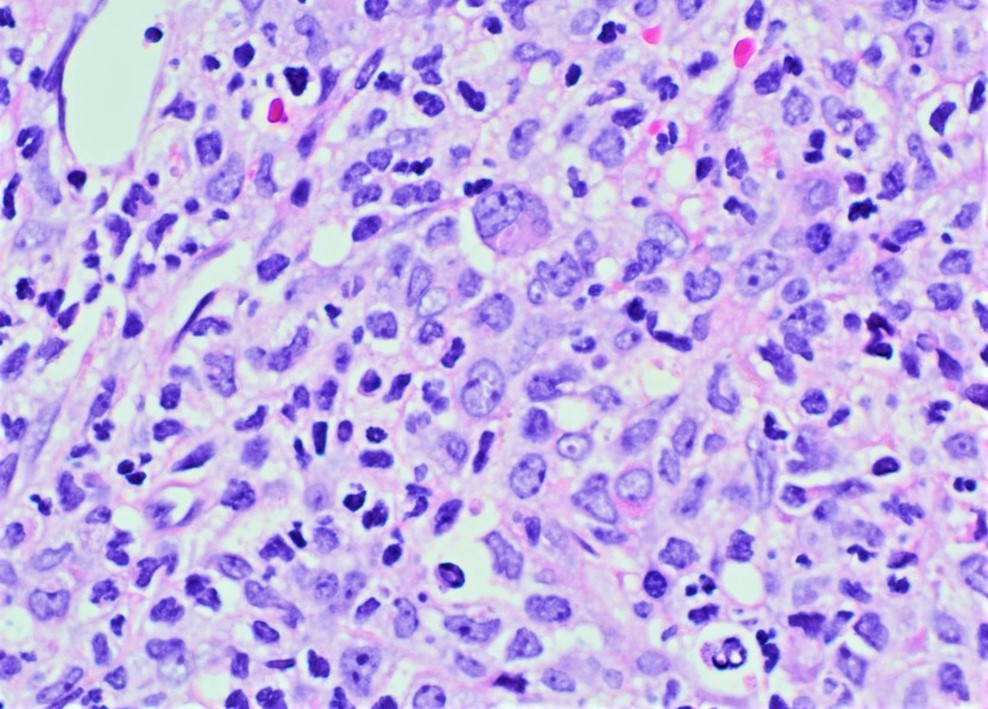
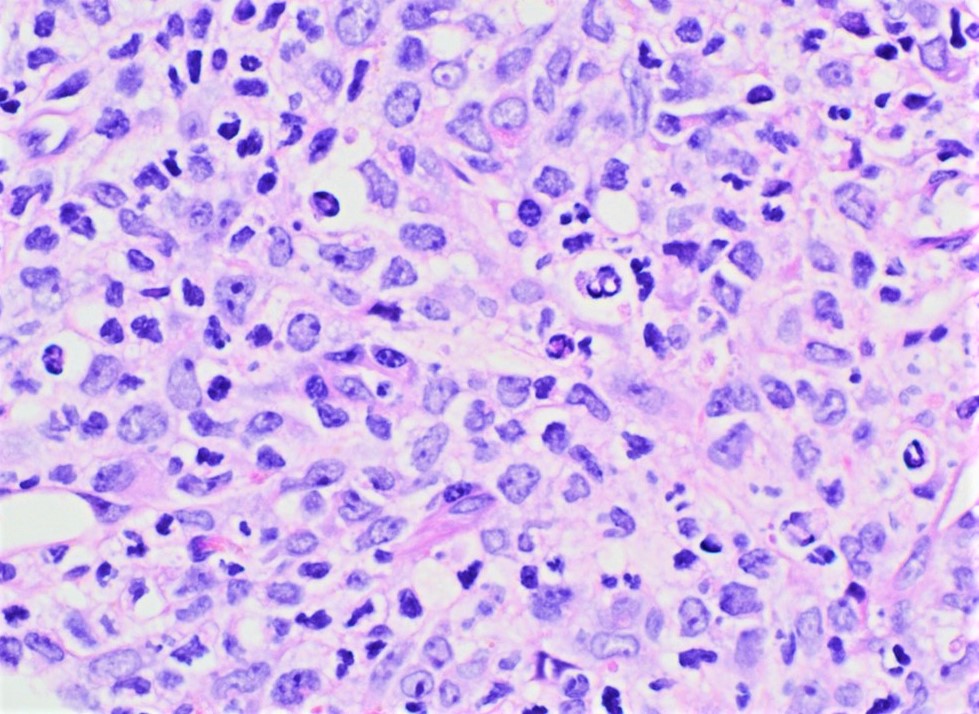
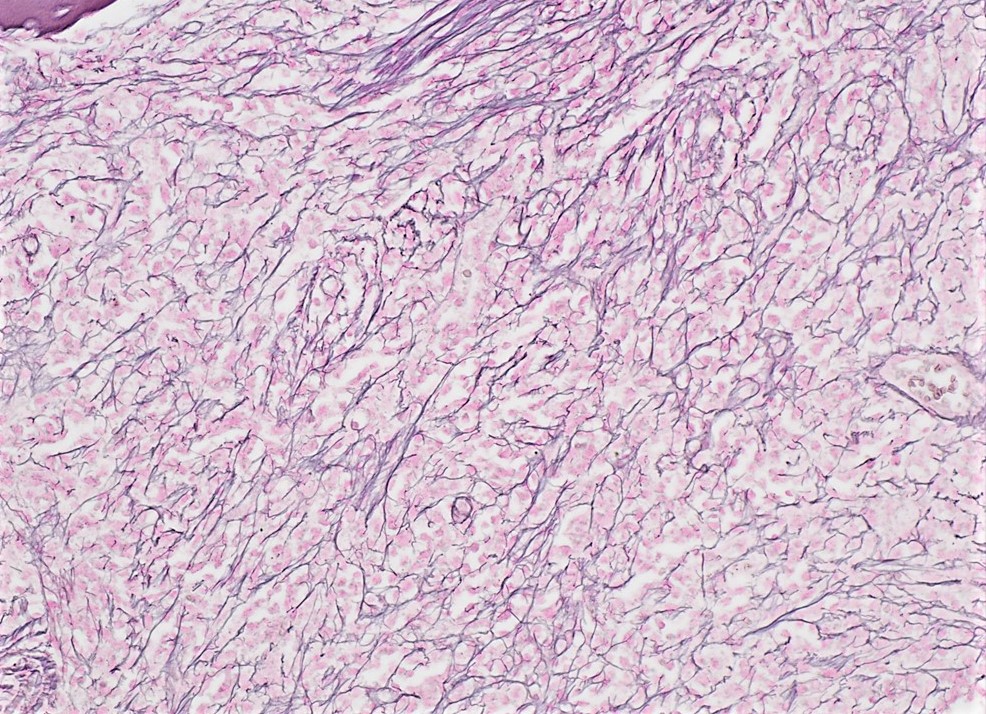
Microscopic (histologic) description
- Bone marrow biopsy / aspirate
- Hypercellular bone marrow with medium sized blasts with high nuclear to cytoplasmic ratio, an oval, round or bilobed nucleus, dispersed chromatin with 1 - 3 prominent nucleoli
- Moderate amounts of basophilic cytoplasm that contains a variable number of coarse basophilic granules
- Cytoplasmic vacuolation may be present
- Mature basophils are usually sparse
- Dysplastic features in the erythroid precursors may be present
Microscopic (histologic) images
Positive stains
- CD13, CD33, CD123, CD203c, CD11b, CD34, CD9, CD25, CD22 (subset), TdT (subset), HLA-DR, Basogranulin (BB1), 2D7a (Leukemia 2017;31:788)
- Cytochemical stains: toluidine blue (metachromatic staining), acid phosphatase (diffuse pattern), periodic acid-Schiff (PAS) (large block-like pattern)
Negative stains
- CD117, tryptase, most monocytic markers and most lymphoid markers
- Cytochemical stains: myeloperoxidase (MPO), Sudan black B (SBB), naphthol AS-D chloroacetate esterase (CAE)
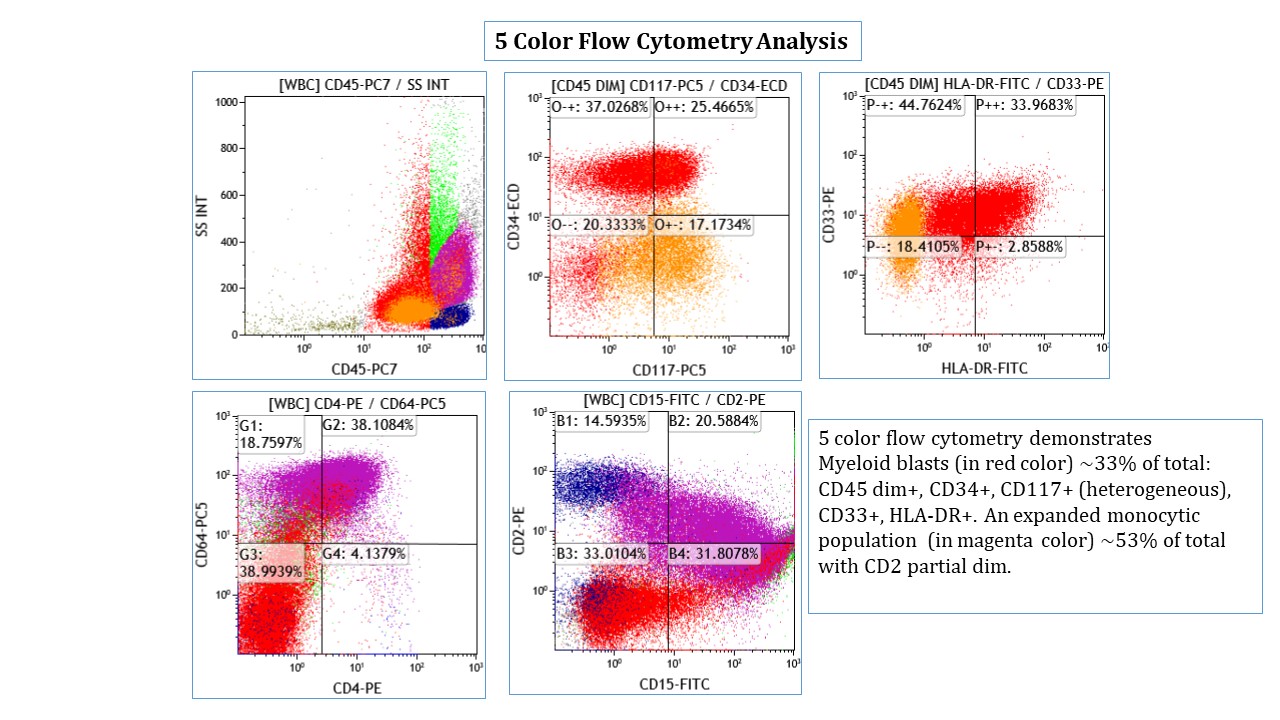
Flow cytometry description
- Immunophenotypic profile of basophils (See Diagrams / tables)
- Positive: CD45, CD9, CD13, CD33 , CD11b, CD25, CD123 (IL3 R alpha chain), Fcε receptor type I (IgE-R), Bsp-1, CD203c (ectoenzyme ENPP3)
- Negative: CD117, CD25, monocytic markers (except CD11b), lymphoid markers (except CD22)
- Reference: Leukemia 2017;31:788
Electron microscopy description
- Granules contain an electron dense particulate substance and are internally bisected, e.g. have a theta character (θ) or contain crystalline material arranged in a pattern of scrolls or lamellae
- Coexistence of basophil and mast cell granules may be identified in the same immature cells
Molecular / cytogenetics description
- No consistent chromosomal abnormality identified; exclude cases with t(9;22) BCR-ABL
- Complex karyotype may be present (Cancer Genet Cytogenet 2008;182:46, Cancer Genet Cytogenet 1991;51:215)
- Recurrent t(X;6)(p11.2;q23.3) resulting in MYB-GATA1 appears to occur in male infants (Blood 2011;117:5719)
- t(3;6)(q21;p21) and abnormalities involving 12p (Bibl Haematol 1978;45:142)
Sample pathology report
- Bone marrow, right posterior iliac crest, core biopsy, clot section, aspirate smears and touch imprint:
- Consistent with acute myeloid leukemia, NOS favor acute basophilic leukemia (see comment)
- Comment: Hypercellular marrow (100%) is essentially replaced by sheets of immature myeloid cells (approximately 70% of total cellularity) with increased basophils. Bone marrow aspirate smears show blasts, 25%; atypical immature basophils, 38%; mature basophils, 7%. The blasts often had basophil-like dark, coarse granules. Special stains demonstrate that the blasts were positive for metachromatic toluidine blue but negative for myeloperoxidase (MPO). Flow cytometric analysis demonstrates immature myeloid cells (comprises 30% of total) expressing CD13, CD33, CD34, CD38 and HLA-DR and heterogeneous population of basophils (approximately 35% of total) express CD11b, CD13, CD33, CD22, CD123 and CD203. No monotypic B cells or immunophenotypically abnormal T cells are detected. Additional cytogenetic and molecular studies are in progress and will be reported separately.
- Peripheral blood: Anemia, thrombocytopenia and leukocytosis. Hemoglobin was 8.9 g/dl, platelet 61/ 109/L and total leukocyte count 15 /109/L. The smear revealed a large population of basophils with a variable degree of maturation ranging from blasts with coarse basophilic granules to mature basophil granulocytes, some of which had signs of degranulation.
- Bone marrow biopsy: Quality adequate. Hypercellular marrow (100%), large population of basophils with a variable degree of maturation ranging from blasts with coarse basophilic granules to mature basophil granulocytes, some of which had signs of degranulation. Bone marrow residual myeloid as well as erythroid lineages were markedly reduced to absent. Rare unremarkable megakaryocytes were seen. There are no granulomas. The bony trabeculae show evidence of remodeling. Stainable iron is present (iron stain). There is a diffuse increase in reticulin fibers with focal collagen fibrosis; (reticulin stain, trichrome stain).
- Bone marrow clot section: Quality adequate. Cellularity - 100% morphologic features are similar to those observed in the core biopsy.
- Bone marrow aspirate: Quality adequate. The smears show blast cells, 25%; atypical immature basophils, 38%; mature basophils, 7%; normal mature neutrophils, 11%; lymphocytes, 7%; monocytes, 2% and erythroid cells, 10%. The blasts often had basophil-like dark, coarse granules and basophils had characteristic confluent vacuoles merged with the cell membrane suggestive of degranulation.
- Special Stains: Blasts were toluidine blue metachromatic but negative for myeloperoxidase.
- Flow Cytometry Analysis: Gating - mononuclear cells by forward and side light scatter.
- Interpretation: Immature myeloid blasts (comprises 30% of total) were positive for CD13, CD33, CD34, CD38 and HLA-DR. In addition, heterogeneous population of basophils (approximately 35% of total) express CD11b, CD22, CD13, CD33, CD123 and CD203. The immature myeloid blasts were negative for TdT, CD10, CD14, CD61, CD64, CD2, sCD3, cCD3, CD4, CD5, CD8, CD16, CD56, CD19, CD20, CD22, CD23, cCD79a, CD103, CD117, FMC7, kappa and lambda.
Differential diagnosis
- Reactive conditions with a massive expansion of polyclonal basophils
- Acute promyelocytic leukemia with basophilic differentiation (Br J Haematol 1982;50:201, Leukemia 1994;8:1441)
- AML with t(6;9)(p23;q34.1) DEK-NUP214:
- Seen in older children; rare in infants
- Often associated with basophilia, multilineage dysplasia and poor prognosis (Br J Haematol 2014;166:254)
- Myeloproliferative and myelodysplastic neoplasm with basophilia (MPN basophils; MDS basophils):
- Accelerated phase of chronic myeloid leukemia (CML)
- Blast phase of myeloproliferative neoplasm
- JAK2 mutated MPN, MDS / MPN overlap diseases (Am J Clin Pathol 2015;144:188)
- AML with t(8;21) RUNX1-RUNX1T1 and basophilia:
- Seen in younger patients
- Blasts are large with abundant basophilic cytoplasm containing numerous azurophilic granules and perinuclear hofs
- Often with large granules (pseudo-Chédiak-Higashi granules)
- Usually associated with high rate of complete remission and longterm disease survival (Rinsho Ketsueki 2017;58:991)
- Lymphoblastic leukemia with prominent coarse granules (rare)
- Mast cell leukemia:
- Expresses CD117, tryptase and CD25 (Diagn Pathol 2018;13:14)
Additional references
Board review style question #1
What is the most specific marker for basophils in peripheral blood?
- CD25
- CD117
- CD123
- CD203c
Board review style answer #1
D. CD203c is a relatively specific marker for basophils in peripheral blood. Other markers such as CD13 or CD33, CD123, CD11b, CD34 are also positive, while CD25, CD117 and tryptase are negative. This immunophenotype helps to differentiate acute basophilic leukemia from mast cell leukemia.
Comment Here
Reference: Acute basophilic leukemia
Comment Here
Reference: Acute basophilic leukemia
Board review style question #2
Board review style answer #2
D. Myeloblast. Recommended markers to delineate between basophils, eosinophils and mast cells are CD34, CD117, tryptase, 2D7 and BB1 (basogranulin). Myeloblasts are often CD34 or CD117 positive; Mast cells express CD117 and tryptase and are negative for CD34. Eosinophils and basophils are negative for both CD34 and CD117 and express BB1 and 2D7.
Comment Here
Reference: Acute basophilic leukemia
Comment Here
Reference: Acute basophilic leukemia