Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Chan AWH. Alcoholic liver disease. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/liveralcoholichep.html. Accessed April 19th, 2024.
Definition / general
- Liver damage caused by excessive alcohol consumption
Essential features
- Liver damage caused by excessive alcohol consumption
- Steatosis, steatohepatitis or perivenular and pericellular fibrosis are typical histological features
Terminology
- Alcoholic liver disease
ICD coding
Epidemiology
- 90 - 95% of heavy drinkers develop steatosis; up to 35% develop advanced alcoholic liver diseases (i.e., alcoholic hepatitis, fibrosis, cirrhosis or hepatocellular carcinoma) (J Hepatol 2012;57:399)
- Proportion of current drinkers among the total population in 2016: 43.0% (world), 59.9% (European region), 54.1% (region of the Americas), 53.8% (Western Pacific region), 33.1% (Southeast Asian region), 32.2% (African region) and 2.9% (Eastern Mediterranean region) (WHO: Global Status Report on Alcohol and Health 2018 [Accessed 6 December 2021])
- Harmful alcohol use is associated with 5.3% of all deaths and 5.1% of disability adjusted life years (DALYs) worldwide in 2016 (WHO: Global Status Report on Alcohol and Health 2018 [Accessed 6 December 2021])
- Cirrhosis accounts for 607,000 and 22.2 million alcohol attributable death and DALYs, respectively (WHO: Global Status Report on Alcohol and Health 2018 [Accessed 6 December 2021])
- Liver cancer accounts for 84,000 alcohol attributable cancer deaths (WHO: Global Status Report on Alcohol and Health 2018 [Accessed 6 December 2021])
Sites
- Liver
Pathophysiology
- Alcohol enhances hepatic lipid biosynthesis
- Excess NADH generation from alcohol dehydrogenase and acetaldehyde dehydrogenase
- Impaired assembly / secretion of lipoproteins
- Increased peripheral fat catabolism
- P450 induction causes other drugs to be transformed to toxic metabolites; free radicals, from microsomal oxidation of alcohol, damage proteins and membranes
- Alcohol directly affects microtubular and mitochondrial function, also induces immunologic attack on hepatic neoantigens
- Acetaldehyde (alcohol metabolite) causes lipid peroxidation and acetaldehyde protein adduct formation
- Collagen deposition by perisinusoidal hepatic stellate (Ito) cells is due to Kupffer cell activation (release of TNFα, IL1 / 6, TGFβ), platelet activating factor, influx of neutrophils into parenchyma
- Alcohol also causes derangements of vascular perfusion
- Alcohol consumption results in translocation of gut bacteria into the portal system along with lipopolysaccharides that interact with toll-like receptors and results in production of inflammatory and immunogenic mediators such as TNFα and interferons (World J Hepatol 2011;3:114)
Etiology
- Excessive regular alcohol consumption (> 20 g/day for females and > 30 g/day for males)
Clinical features
- Nonspecific clinical features for any chronic liver disease
- Odor of alcohol on breath
- Alcohol withdrawal syndrome: fine tremor, psychomotor agitation, transient hallucinations or illusions, tachycardia
- Reference: J Hepatol 2018;69:154
Diagnosis
- Alcoholic liver disease (J Hepatol 2018;69:154):
- Regular alcohol consumption of > 20 g/day for females and > 30 g/day for males
- AND clinical or biological abnormalities suggestive of liver injury
- Alcoholic hepatitis (Hepatology 2020;71:306):
- Recent onset (< 8 weeks) of jaundice
- Heavy alcohol consumption (> 40 g/day for females and > 60 g/day for males for ≥ 6 months or < 60 days of abstinence before the onset of jaundice)
- Serum aspartate transaminase (AST) > 50 IU/L, AST/alanine transaminase (ALT) > 1.5 and both AST & ALT < 400 IU/L
- Serum bilirubin > 50 µmol/L (3 mg/dL)
- In presence of diagnostic uncertainly, liver biopsy is required to confirm histologically alcoholic steatohepatitis and rule out other diagnoses
Laboratory
- Serum AST:ALT > 2
- Elevated serum gamma glutamyltransferase (GGT; sensitivity 42 - 86%; specificity 40 - 84%) (J Hepatol 2018;69:154)
- Elevated mean corpuscular volume (MCV; sensitivity 24 - 75%; specificity 56 - 96%) (J Hepatol 2018;69:154)
- Elevated percentage of carbohydrate deficient transferrin per total transferrin (%CDT; sensitivity 25 - 84%; specificity 70 - 98%) (J Hepatol 2018;69:154)
Prognostic factors
- Increasing the risk of alcohol related liver injury (Hepatology 2020;71:306):
- Drinking pattern: daily drinking, drinking while fasting, binge drinking
- Female
- Genetics: PNPLA3, TM6SF2, MBOAT7, HSD17B13
- Smoking cigarettes
- Increased BMI
- Concurrent liver disease: chronic viral hepatitis, genetic hemochromatosis, nonalcoholic fatty liver disease
- Ameliorating the risk of alcohol related liver injury:
- Coffee consumption
Case reports
- 27 year old man with alcoholic hepatitis presenting with high levels of triglyceride, direct hyperbilirubinemia and elevated ALP without an obvious obstruction cause (Case Rep Gastroenterol 2020;14:448)
- 47 year old woman with alcoholic hepatitis masquerading as tumor infiltration (Clin Case Rep 2019;7:2174)
- 55 year old man with severe alcoholic hepatitis and superimposed Candida esophagitis, who was found to have leukemoid reaction during diagnostic workup (Cureus 2020;12:e9747)
- 67 year old man with acute liver injury and false positive results of enzymatic ethanol assay secondary to lactic acidosis due to intravascular large B cell lymphoma (BMJ Case Rep 2019;12:e229814)
Treatment
- Abstinence is the most important treatment
- Corticosteroid should be considered for patients with severe alcoholic hepatitis without contraindications to the corticosteroid (J Hepatol 2018;69:154, Hepatology 2020;71:306)
- Intravenous N-acetylcysteine may be combined with corticosteroid in patients with severe alcoholic hepatitis (J Hepatol 2018;69:154, Hepatology 2020;71:306)
- Liver transplantation for alcoholic cirrhosis
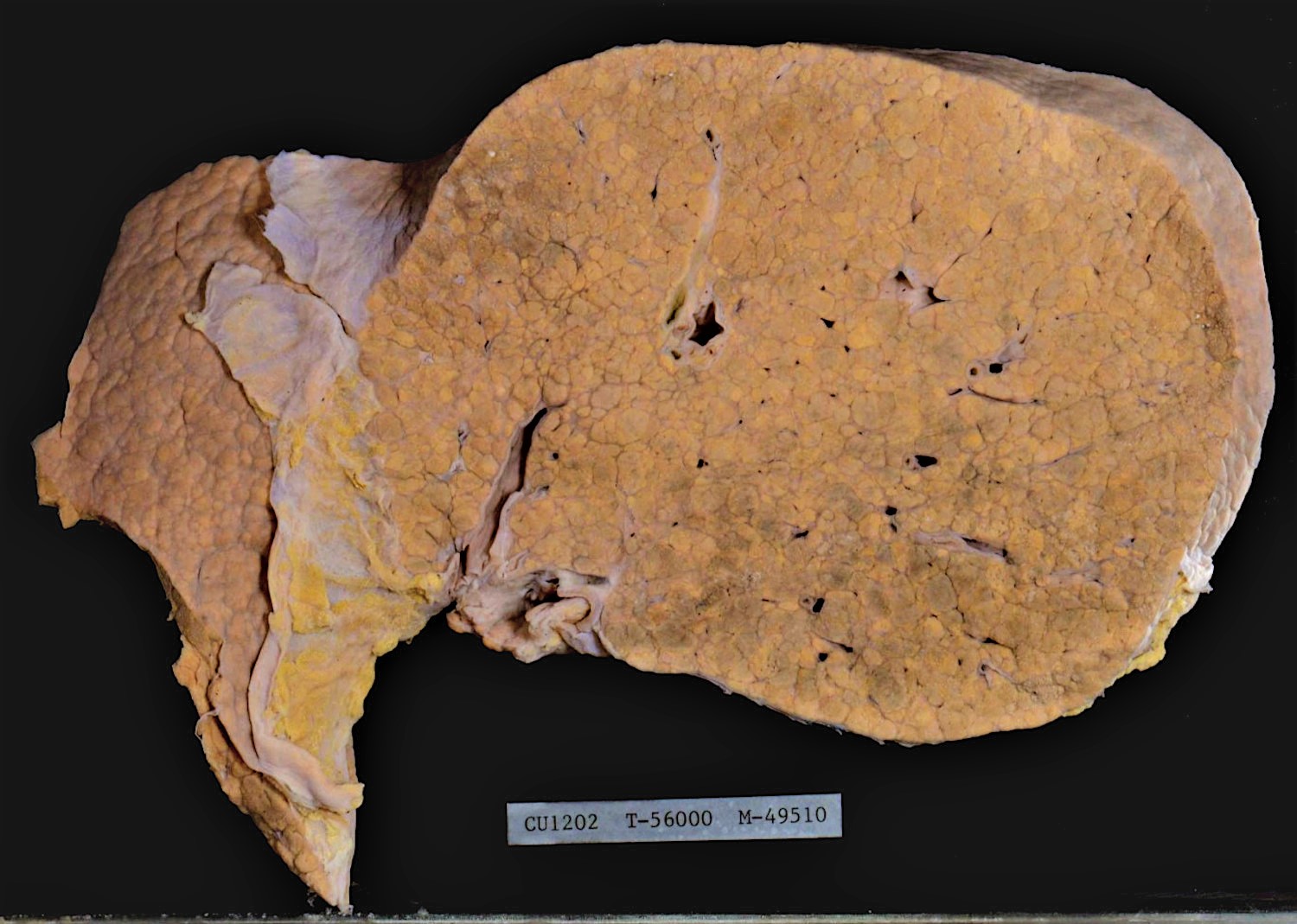
Gross description
- Early stage: enlarged liver with diffuse yellowish greasy appearance
- Later stage:
- Typical micronodular cirrhosis
- Mixed micronodular and macronodular cirrhosis after abstinence
- Yellowish greasy (due to steatosis) or greenish (due to cholestasis)
- Reference: Clin Liver Dis 2016;20:473
Gross images
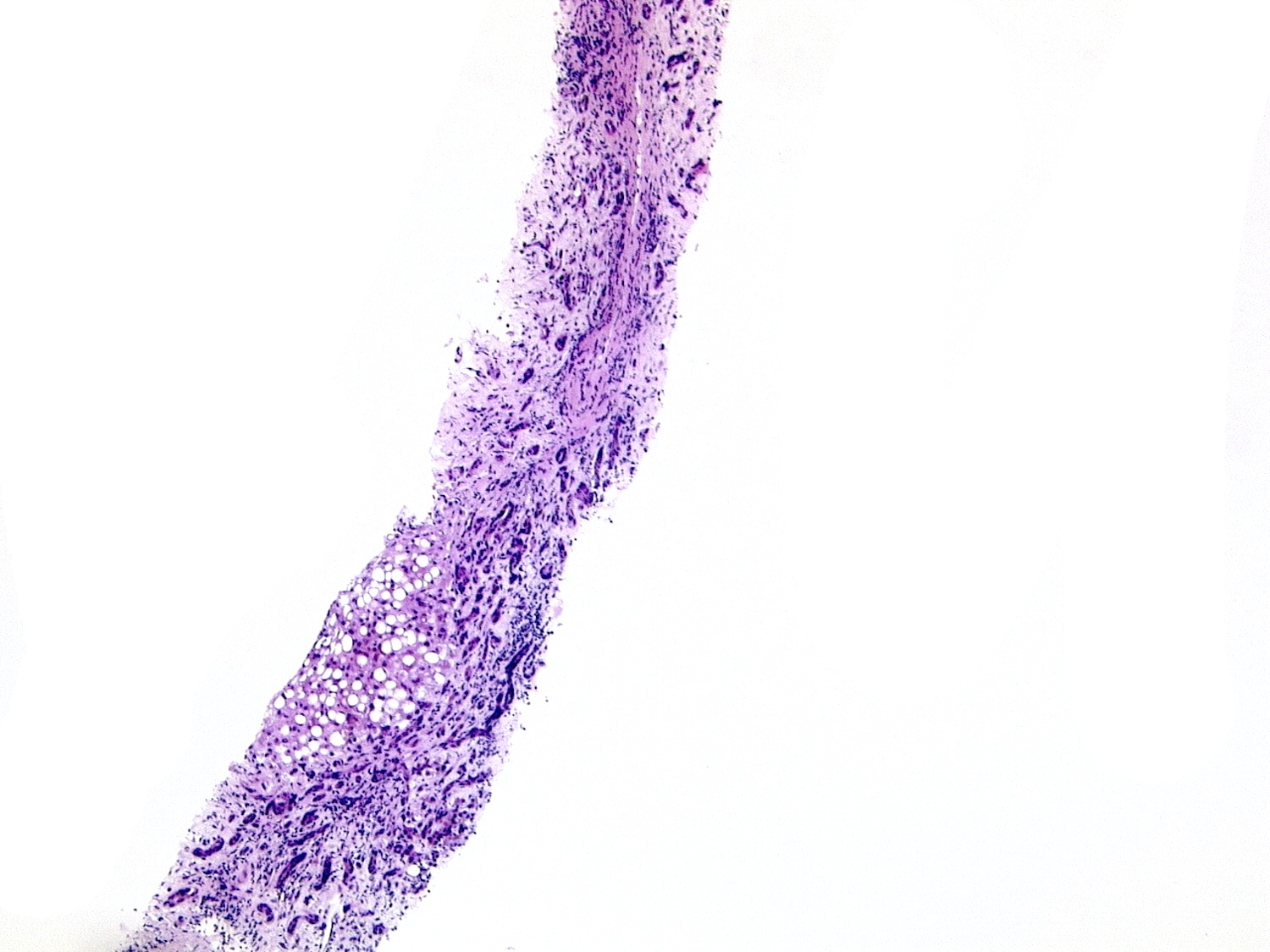
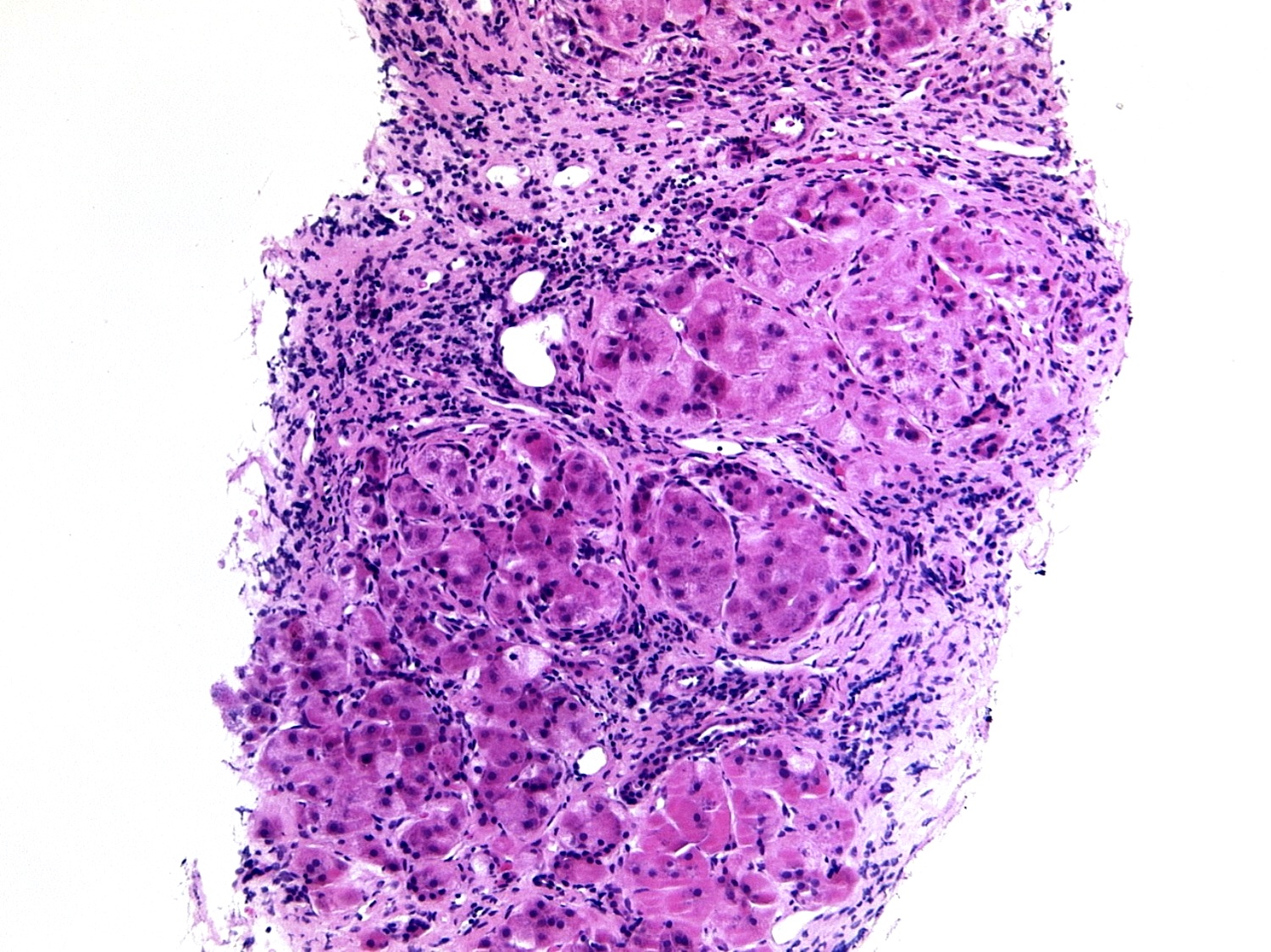
Microscopic (histologic) description
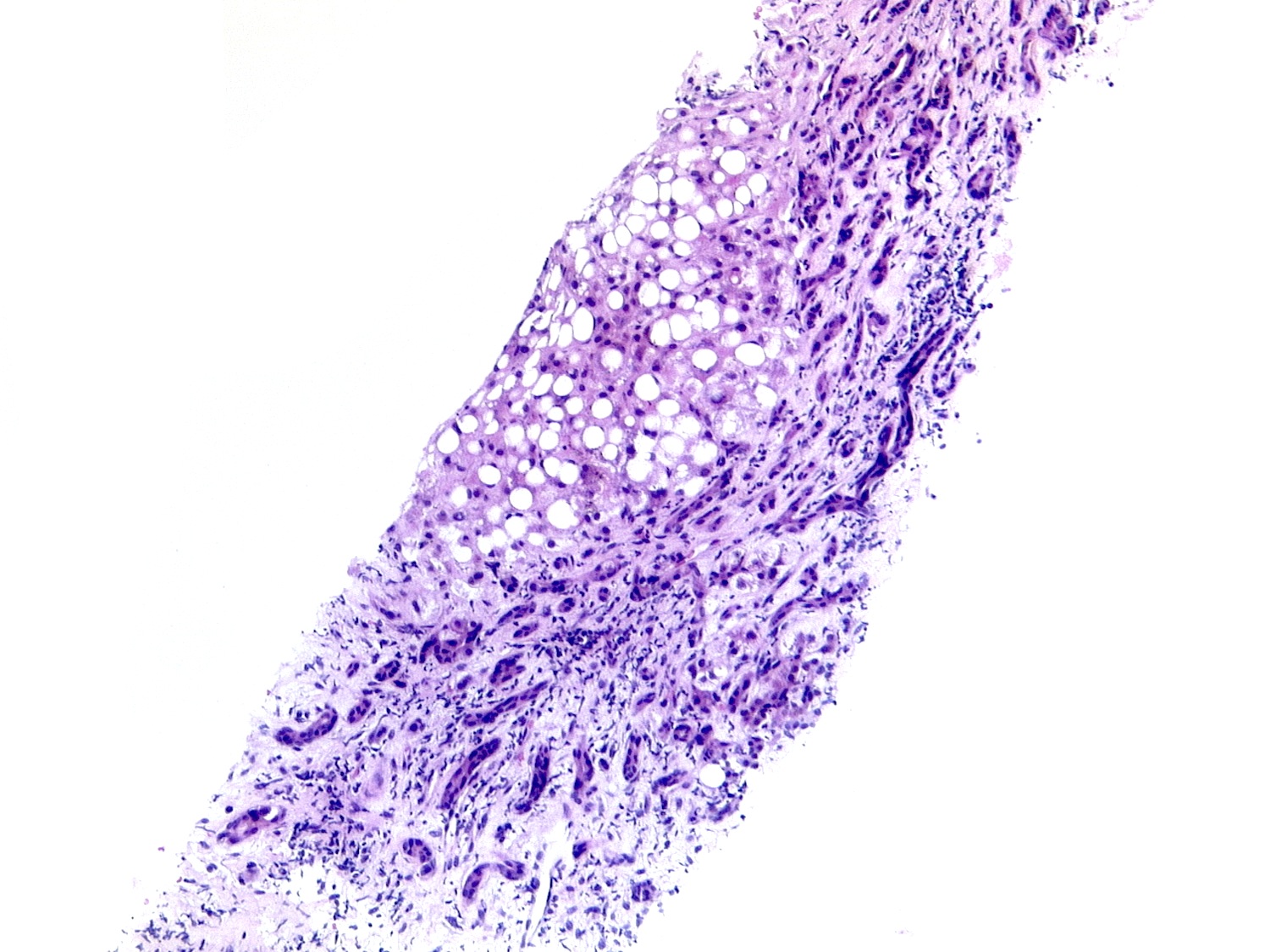
- Steatosis:
- Most common and earliest form of alcoholic liver disease
- Predominantly macrovesicular steatosis: large droplet (classical; a single large fat droplet displacing the nucleus to the periphery) and small / medium droplets
- First appears in perivenular region (zone 3) and spreads to other regions if drinking persists; may disappear within 1 month after alcohol cessation
- Whether it is a benign, nonprogressive lesion is controversial (J Hepatol 2012;57:399)
- Association between degree of steatosis and disease progression is also controversial
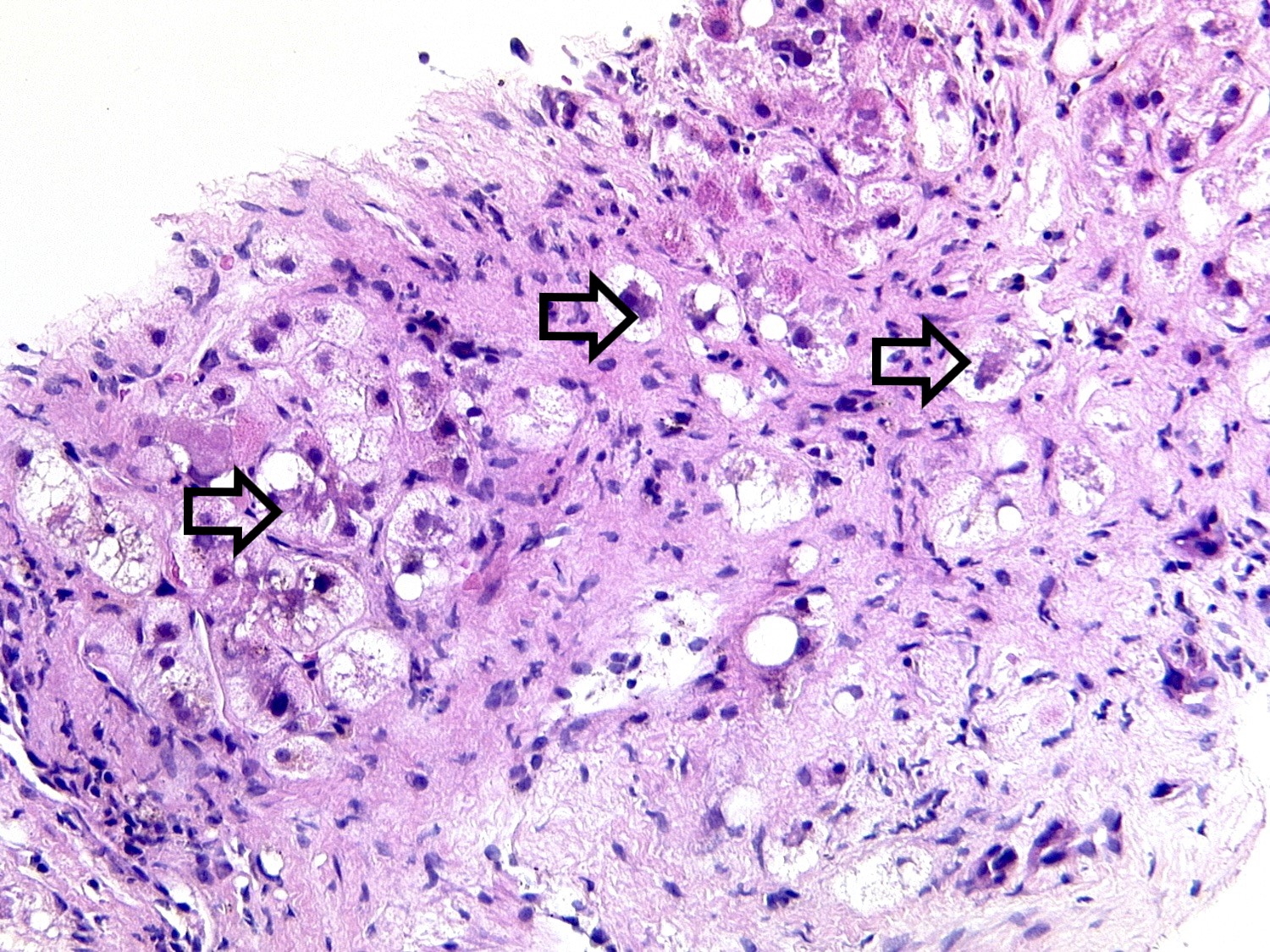
- Alcoholic steatohepatitis:
- Steatosis with inflammation and ballooning degeneration, which is the hallmark of hepatocellular injury in steatohepatitis
- Ballooning degeneration is characterized by cellular swelling, rarefaction of the hepatocytic cytoplasm and clumped strands of intermediate filaments
- Satellitosis is featured by ballooned hepatocyte surrounded by neutrophils
- Mallory-Denk body, also known as Mallory body or Mallory hyaline, is a deeply eosinophilic, ropy intracytoplasmic inclusion that represents aggregates of misfolded intermediate filaments with other different classes of proteins, including p62 and ubiquitin
- Often but not necessarily found in ballooned hepatocytes (Exp Cell Res 2007;313:2033)
- Persists for several months after cessation of drinking
- Associated with increased risk of progression to cirrhosis
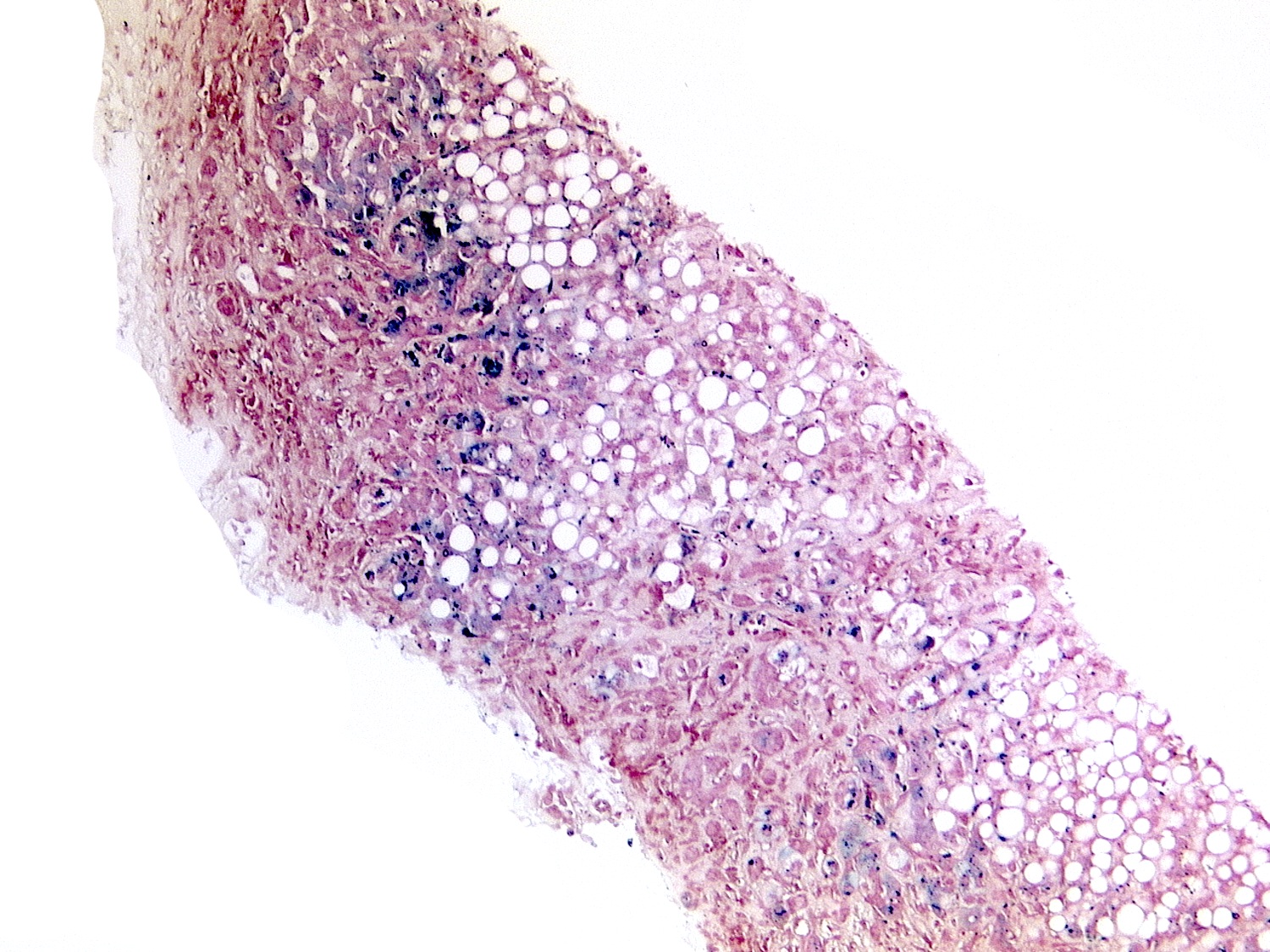
- Fibrosis is not a necessary diagnostic feature; perivenular and pericellular (perisinusoidal) fibrosis is characteristic for fatty liver disease; as disease progresses, portal / periportal fibrosis, bridging fibrosis and cirrhosis will develop
- Alcoholic hepatitis histologic score is proposed to predict 90 day mortality based on 4 parameters: fibrosis, bilirubinostasis, neutrophilic infiltration and giant mitochondria (Gastroenterology 2014;146:1231)
- Alcoholic cirrhosis:
- Classically micronodular cirrhosis
- Steatosis and ballooned hepatocytes may burn out in advanced fibrosis or cirrhosis
- Other pathological lesions:
- Lipogranuloma
- Giant mitochondria: associated with recent heavy alcohol intake and disease progression (J Clin Pathol 1992;45:412)
- Acute foamy degeneration: rare, extensive microvesicular steatosis with no / minimal inflammatory activity; clinically presents with jaundice, abdominal pain and hepatomegaly (Gastroenterology 1983;84:683)
- Sclerosing hyaline necrosis: fibrous obliteration of terminal hepatic venule (phlebosclerosis) due to perivenular fibrosis; severe form of alcoholic hepatitis associated with noncirrhotic portal hypertension
- Iron deposition: usually mild; mainly in hepatocytes (grade 1 - 2) and occasionally in Kupffer cells
Microscopic (histologic) images
Virtual slides
Positive stains
- Stains for collagen (Masson trichrome / Sirius red / reticulin): highlight perivenular and pericellular fibrosis
- Ubiquitin, p62, CK8/18: highlight Mallory-Denk bodies (Exp Cell Res 2007;313:2033)
Sample pathology report
- Liver, right lobe, biopsy:
- Moderate steatosis with perivenular and pericellular fibrosis (see comment)
- Negative for significant lobular necroinflammatory activity
- Negative for bridging fibrosis or cirrhosis
- Negative for malignancy
- Comment: In view of significant alcoholic consumption in absence of metabolic risks, the overall features are consistent with alcoholic steatosis.
- Liver, native, transplantation:
- Cirrhotic liver, clinically alcoholic cirrhosis
- Negative for significant steatosis, ballooning degeneration or Mallory-Denk bodies, consistent with abstinence
- Negative for dysplasia or malignancy
Differential diagnosis
- Chronic viral hepatitis C:
- Steatosis is typically mild at most
- Presence of lymphocyte predominant portal inflammation, portal lymph follicle, bead-like sinusoidal lymphocyte infiltration and mild bile duct injury differentiates hepatitis C from alcoholic liver disease
- Drug induced liver injury (e.g., amiodarone, glucocorticoids, methotrexate, synthetic estrogens, tamoxifen)
- Nonalcoholic fatty liver disease:
- Pathologically almost indistinguishable from alcoholic liver disease
- Alcoholic liver disease has few specific pathological changes and all are rare:
- Acute foamy degeneration
- Sclerosing hyaline sclerosis
- Acute / chronic cholestasis and sinusoidal obstruction syndrome
- Alcoholic liver disease tends to have more Mallory-Denk bodies and giant mitochondria, much less glycogenated nuclei and has satellitosis (ballooned hepatocyte surrounded by neutrophils), although all of these are nonspecific
- Key distinguishing feature is in fact the amount of alcohol consumption obtained from clinical history
- Consumption of 2 standard drinks/day for men and 1 standard drink/day for women is endorsed as the acceptable threshold to define nonalcoholic
- Wilson disease:
- Mild steatosis, glycogenated nuclei and Mallory-Denk bodies
- Deposition of copper associated protein (particularly in hepatocytes out of periportal region) differentiates Wilson disease from alcoholic liver disease
- Other uncommon inherited metabolic diseases
Board review style question #1
Which of the following histological features is useful to differentiate alcoholic liver disease from nonalcoholic fatty liver disease?
- Acute foamy degeneration
- Ballooning degeneration
- Mallory-Denk body
- Satellitosis
- Severe steatosis
Board review style answer #1
A. Acute foamy degeneration. Acute foamy degeneration (diffuse microvesicular steatosis) is a rare presentation of severe acute alcoholic hepatitis presenting with jaundice and hepatomegaly. Rapid recovery occurs on abstinence from alcohol. Diffuse microvesicular steatosis is not a histological feature of nonalcoholic fatty liver disease.
Comment Here
Reference: Alcoholic liver disease
Comment Here
Reference: Alcoholic liver disease
Board review style question #2
Board review style answer #2
E. p62. The highlighted structures are Mallory-Denk bodies, which are misfolded and aggregated intermediate filaments combined with other different classes of proteins, including p62 and ubiquitin. They are immunoreactive to CK8/18, p62 and ubiquitin.
Comment Here
Reference: Alcoholic liver disease
Comment Here
Reference: Alcoholic liver disease