Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1Cite this page: Gonzalez RS. Budd-Chiari syndrome. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/liverbuddchiari.html. Accessed April 19th, 2024.
Definition / general
- Venous outflow obstruction caused by occlusion of hepatic outflow
- Either acute thrombotic occlusion (usually fatal) or subacute / chronic occlusion with hepatomegaly, ascites, abdominal pain
Essential features
- Thrombotic outflow obstruction developing from various causes
- Patients may experience fatal acute occlusion or may develop symptomatic chronic occlusion leading to cirrhosis
- Sinusoidal dilation and portal tract changes are the most common findings on biopsy
Terminology
- Also called hepatic vein thrombosis
- Historically, Budd-Chiari syndrome technically referred to the triad of painful hepatomegaly, ascites and liver dysfunction
- Membranous obstruction of the vena cava / obliterative hepatocavopathy likely represents recanalized thrombosis, more commonly seen in developing countries
ICD coding
- ICD-10: I82.0 - Budd-Chiari syndrome
Epidemiology
- Occurs in roughly 0.001% of the population
Sites
- Occlusion may occur anywhere from hepatic venules to inferior vena cava
Pathophysiology
- In addition to outflow obstruction, patients often have decreased portal perfusion with eventual compensatory increase in arterial inflow (Hepatology 2003;37:510)
Etiology
- Hepatic vein thrombosis can occur for a variety of reasons (contraceptives, steroids, myeloproliferative disorders, paroxysmal nocturnal hemoglobinuria, pregnancy, postpartum state, hepatocellular carcinoma with inferior vena cava occlusion), though 30% of cases are idiopathic
- Venous obliteration can lead to bridging fibrosis and eventually cirrhosis (Hepatology 1998;27:488)
Clinical features
- Symptoms include painful hepatomegaly, jaundice, ascites and possibly liver failure
- Elevation of transaminases and alkaline phosphatase (Mod Pathol 2004;17:874)
Diagnosis
- Typically diagnosed by radiology, though some cases may be missed
Prognostic factors
- High mortality for acute thrombotic occlusion (especially if all 3 hepatic veins are occluded)
- 5 year survival of 50% for chronic form
Treatment
- Anticoagulation; portosystemic venous shunt (causes reverse flow through portal vein); angiography (to dilate obstruction)
Gross description
- Swollen, congested liver with reddish purple, tense capsule
Microscopic (histologic) description
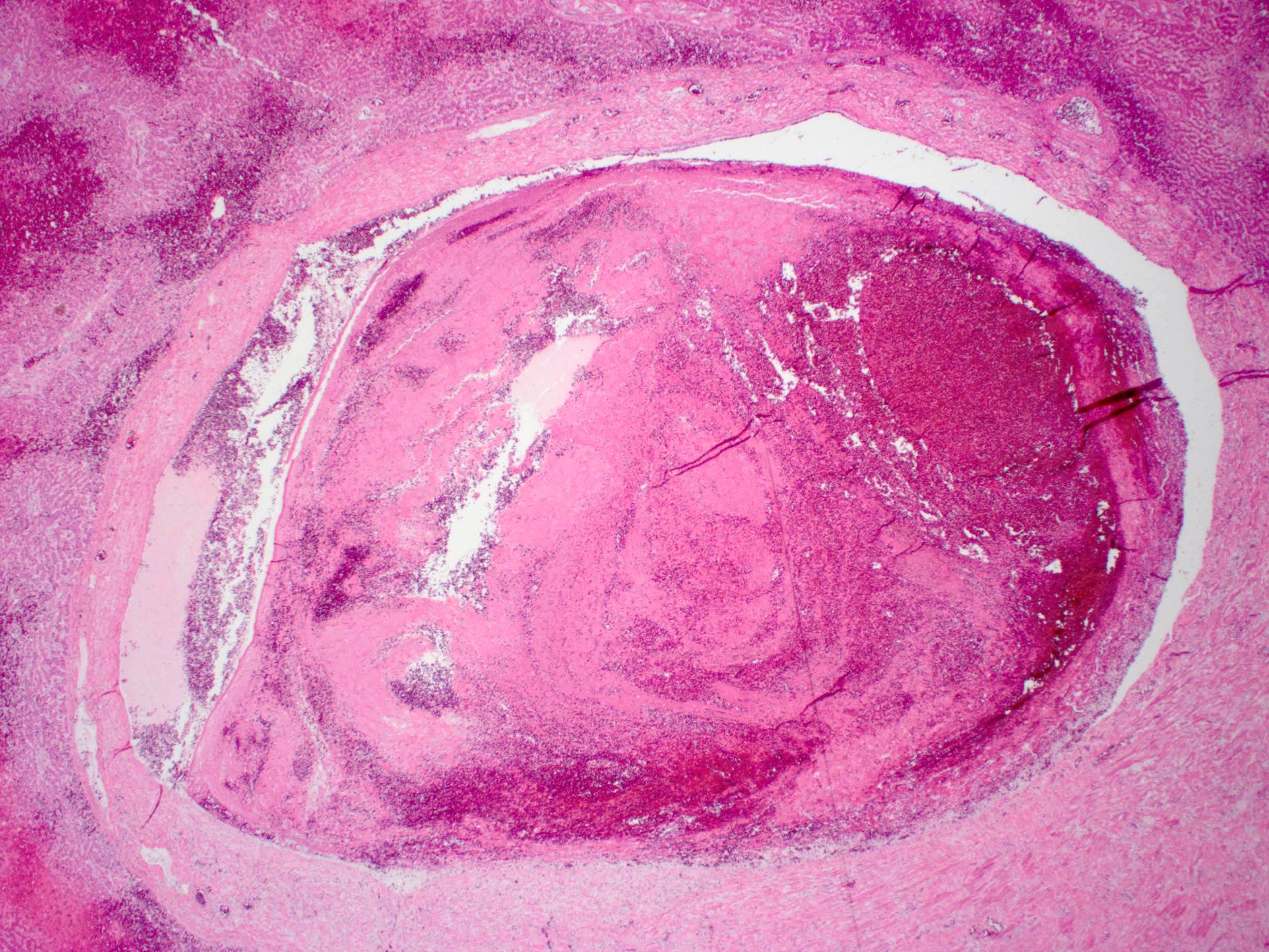
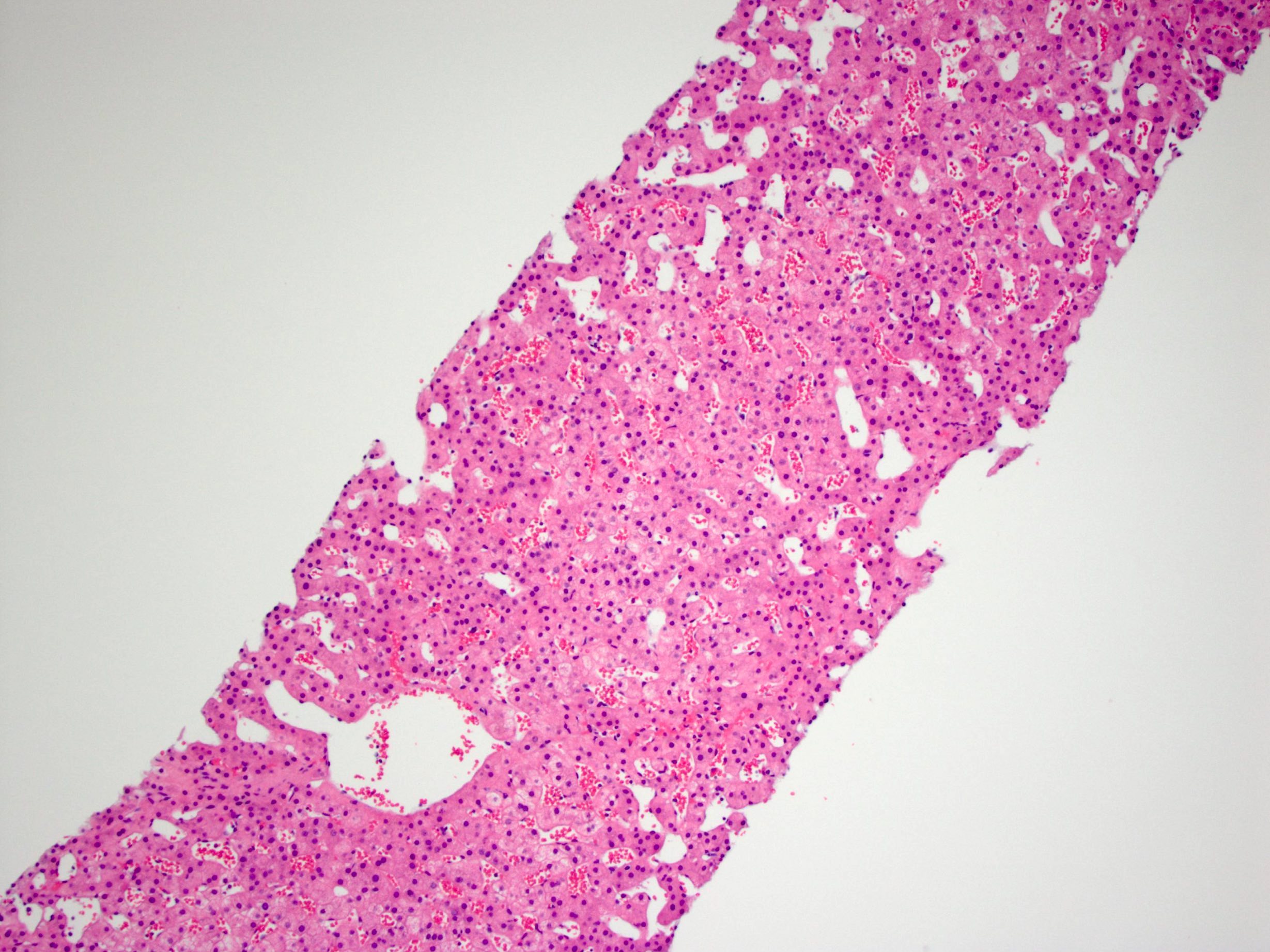
- Severe centrilobular congestion / necrosis, progressing to centrilobular fibrosis
- Sinusoidal dilation, portal tract expansion / fibrosis and ductular reaction in zones 1 and 3 may be seen (Am J Surg Pathol 2014;38:205)
- Large regenerative nodules, focal nodular hyperplasia and hepatocellular adenomas can develop (Histopathology 2004;44:172)
Microscopic (histologic) images
Sample pathology report
- Liver, biopsy:
- Liver parenchyma with prominent zone 3 sinusoidal dilation (see comment)
- Comment: The findings are most consistent with outflow obstruction (e.g., Budd-Chiari syndrome). Trichrome and iron stains are unremarkable.
Differential diagnosis
- Cardiac / congestive hepatopathy:
- More commonly shows pericellular / sinusoidal fibrosis and fibrosis around central vein (Arch Pathol Lab Med 2017;141:98)
Additional references
Board review style question #1
Which of the following histologic findings is commonly seen in Budd-Chiari syndrome?
- Central vein thrombosis
- Lobular inflammation
- Periportal necrosis
- Sinusoidal dilation
Board review style answer #1