Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Evason KJ. Angiomyolipoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/livertumorAML.html. Accessed April 25th, 2024.
Definition / general
- Benign mesenchymal tumor composed of smooth muscle cells, adipocytes and blood vessels
Essential features
- Hepatic perivascular epithelial cell tumor (PEComa) composed of 3 components, present in variable amounts and growth patterns: smooth muscle, fat and blood vessels
- Usually sporadic but ~ 5 - 10% occur in the setting of tuberous sclerosis
- Generally benign, although rare malignant behavior has been reported and is difficult to predict (Histopathology 2012;61:863)
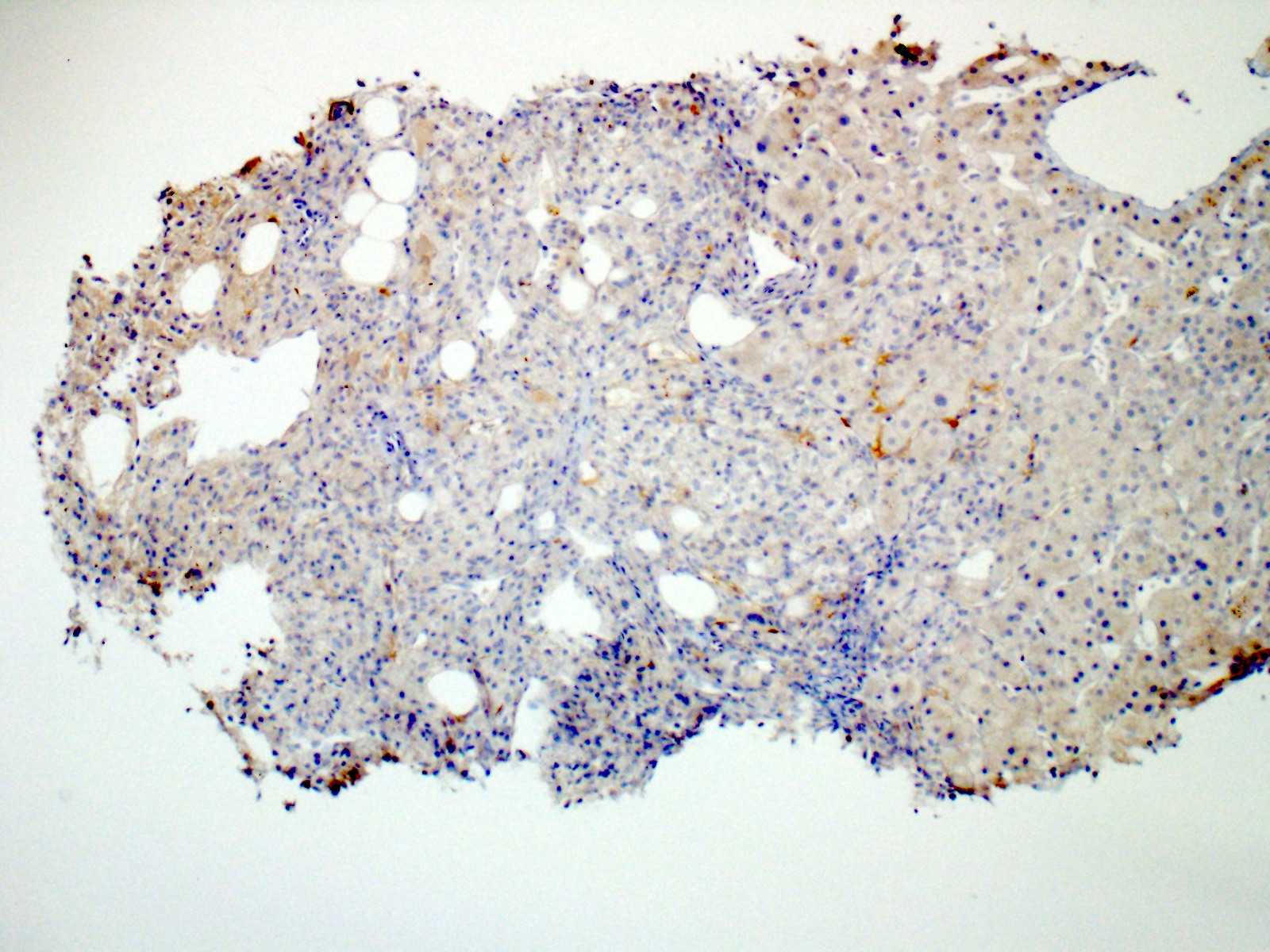
- Smooth muscle component, which usually predominates, shows positive staining with HMB45, SMA and MelanA
Terminology
- Hepatic epithelioid angiomyolipoma (HEAML)
- PEComa
ICD coding
Epidemiology
- F > M; mean age ~ 56 years old (HPB (Oxford) 2020;22:622)
Sites
- Hepatic parenchyma (right lobe > left lobe > caudate lobe) (Histopathology 2012;61:863)
Pathophysiology
- Sporadic: mutations in TSC2 → upregulation of mTOR signaling + activation of Wnt signaling pathway (Histopathology 2018;73:101, Histopathology 2015;66:695)
- Tuberous sclerosis: germline mutations in TSC1 or TSC2
Clinical features
- ~ 5 - 10% occur in tuberous sclerosis patients, where they are more likely to be multiple and associated with renal angiomyolipoma (Am J Surg Pathol 1999;23:34)
Diagnosis
- Biopsy required for diagnosis as radiologic features are overlapping with other entities, especially hepatocellular carcinoma (HCC)
- Ultrasound, CT or MRI alone result in correct diagnosis in < 33% of patients (Clin Radiol 2020;75:88)
- Ultrasound + CT + MRI with or without angiography result in correct diagnosis in 52% of patients (J Surg Oncol 2011;103:807)
Radiology description
- Ultrasound: heterogeneously echogenic lesion with hypoechoic foci
- CT: hypoattenuating lesion showing arterial and persistent enhancement without washout
- MRI: heterogeneously T2 hyperintense lesion with variable T1 intensity; MRI is best modality for detecting fat component
- Reference: Clin Radiol 2020;75:88
Radiology images
Prognostic factors
- Rarely (< 5%) display malignant behavior (recurrence, metastasis) but this is difficult to predict
- High risk features: size > 5 cm, infiltrative growth pattern, high nuclear grade / nuclear pleomorphism and high cellularity, mitoses > 1/50 high power fields, necrosis and vascular invasion (Sarcoma 2012;2012:541626, Am J Surg Pathol 2005;29:1558)
Case reports
- 31 year old man with ruptured hepatic mass (Clin Mol Hepatol 2017;23:179)
- 45 year old woman with hepatic mass, enlarging from 12 to 20 cm over 5 years (J Surg Case Rep 2020;2020:rjaa353)
- 50 year old woman with abdominal pain and liver mass (In Vivo 2017;31:1169)
- 54 year old woman with right upper quadrant pain and liver mass (Case Reports Hepatol 2019;2019:2362618)
- 65 year old woman with hepatic mass noted on annual health check ultrasound (Korean J Gastroenterol 2018;71:49)
Treatment
- Surgical resection
- Conservative management / watchful waiting with imaging at regular intervals can be employed if diagnosis is confirmed by biopsy
- Reference: HPB (Oxford) 2020;22:622
Gross description
- Well circumscribed, unencapsulated or partially encapsulated, gray to tan to yellow, rubbery, soft liver mass with patchy areas of red-brown hemorrhage (Histopathology 2012;61:863)
- Nonneoplastic background liver usually noncirrhotic
Gross images
Frozen section description
- Because the epithelioid component is often the dominant cell type in these lesions, frozen section can often mimic HCC, showing pleomorphic cells with ample eosinophilic cytoplasm and prominent nucleoli (Korean J Gastroenterol 2018;71:49)
- Unlike HCC, usually arises in noncirrhotic liver
Microscopic (histologic) description
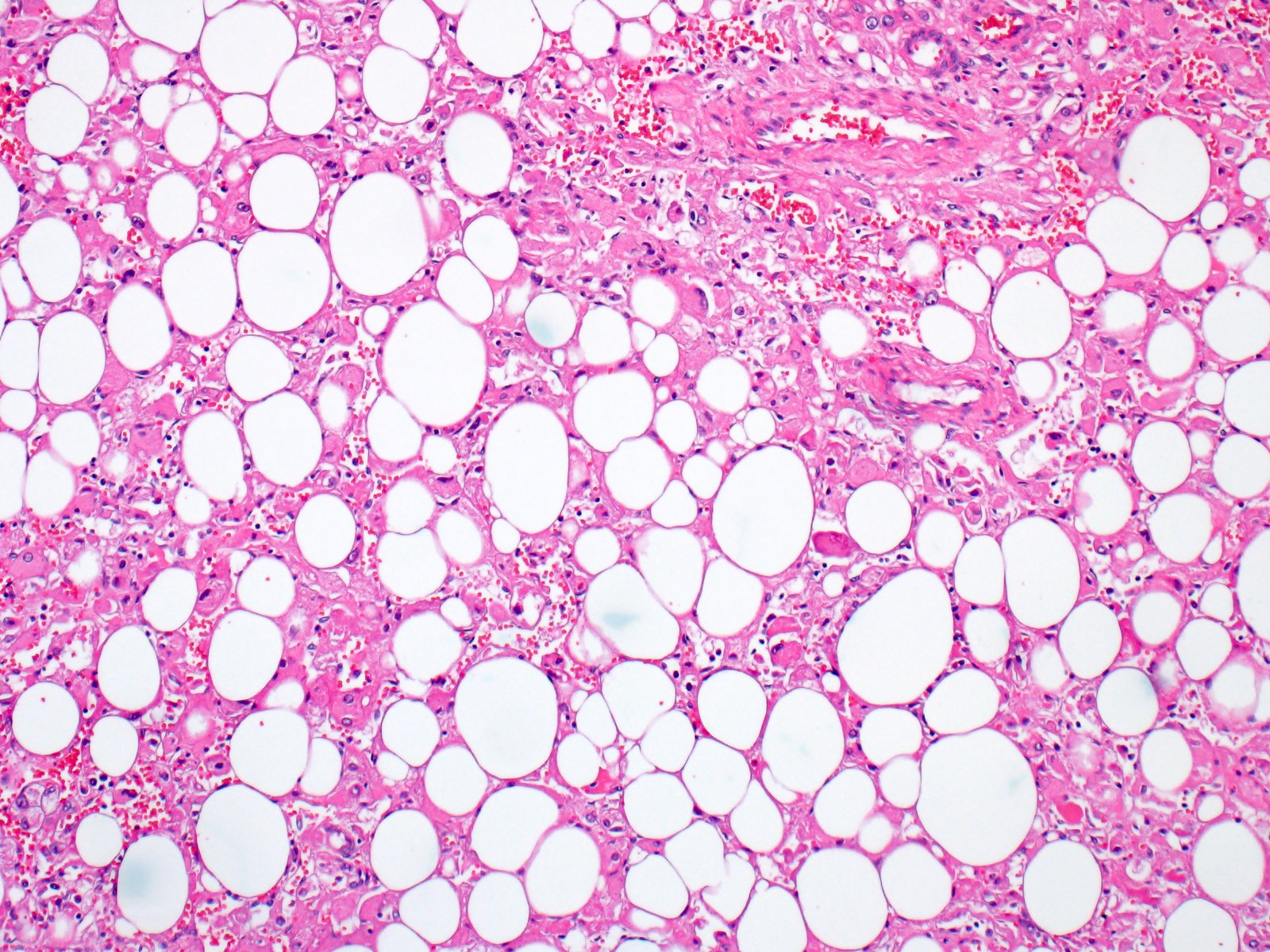
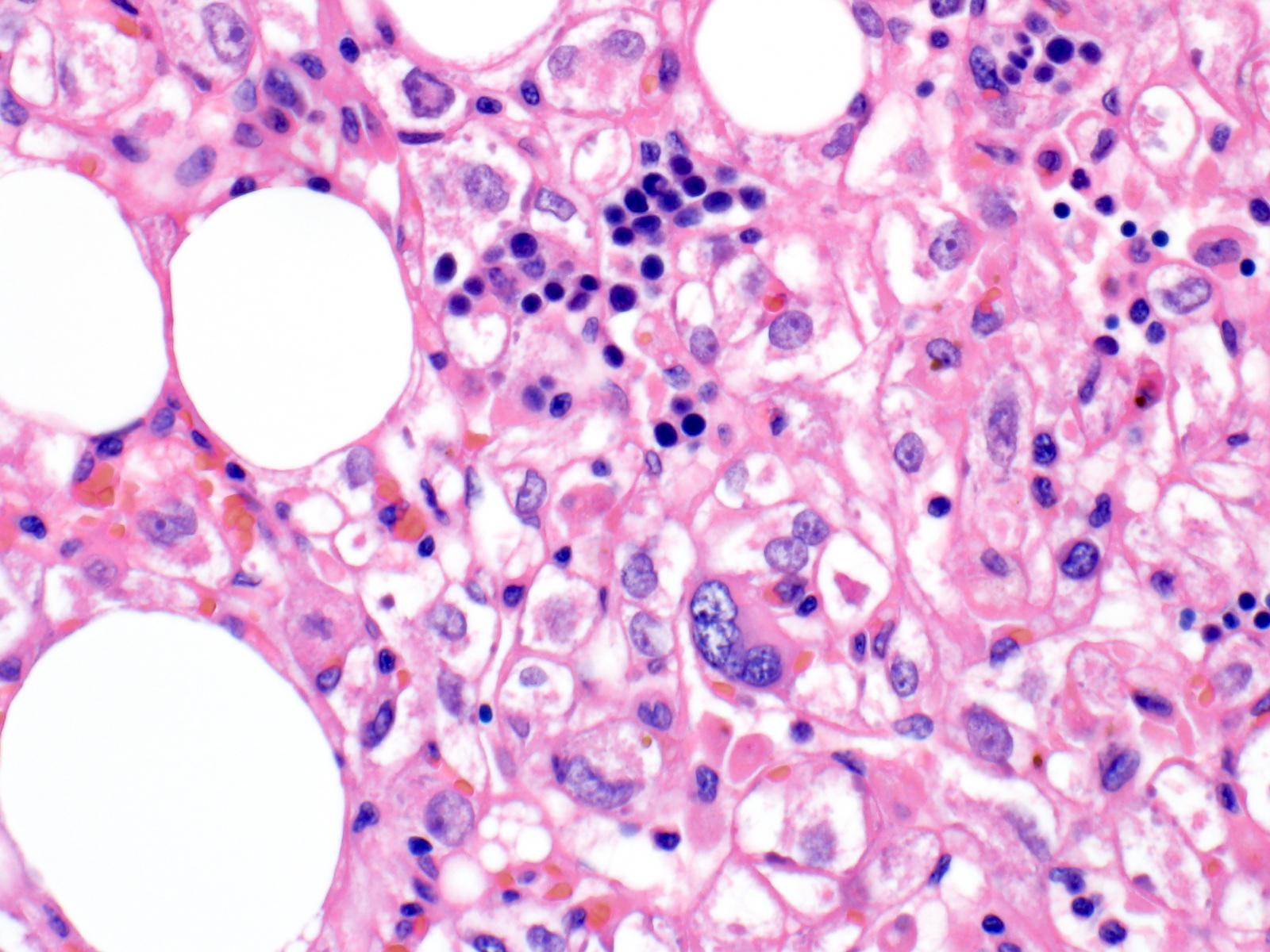
- Composed of 3 components present in variable amounts and growth patterns: smooth muscle (usually predominant), fat and blood vessels
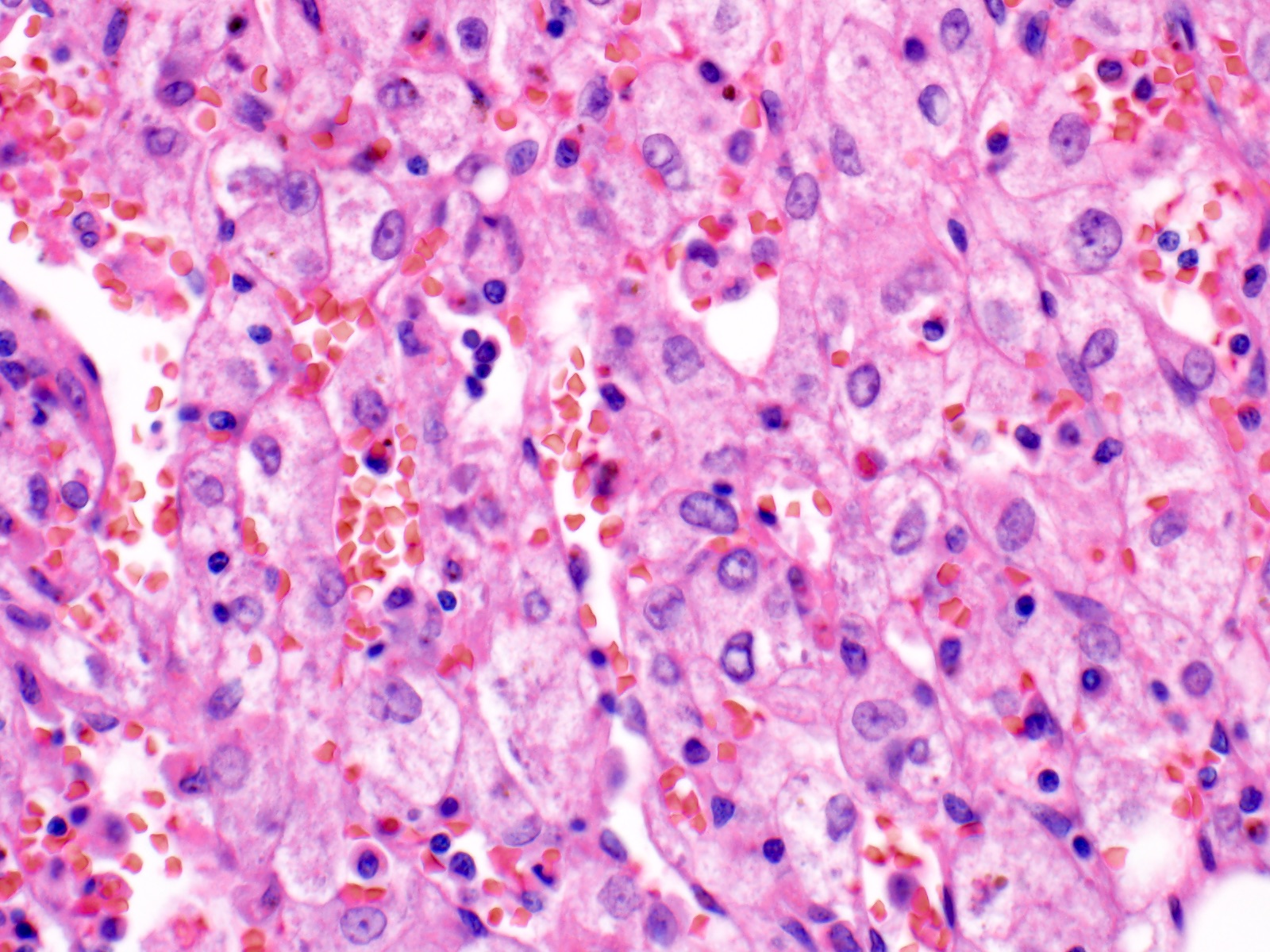
- Smooth muscle component may be spindled, intermediate, epithelioid or pleomorphic (Histopathology 2012;61:863)
- Epithelioid smooth muscle cells typically show ample eosinophilic cytoplasm and round to oval nuclei with prominent small nucleoli
- Nuclear pleomorphism is present at least focally in all tumors and marked cytologic atypia is seen in ~ 25% (Histopathology 2012;61:863)
- Low mitotic rate
- Vascular component includes 4 types of neoplastic blood vessels (cellular, hemangiopericytic, glomeruloid, aneurysmal) as well as nonneoplastic sinusoidal type and collagenous blood vessels; large, dilated vessels may be present at tumor / nontumor interface (Histopathology 2012;61:863)
- May show foci of extramedullary hematopoiesis
- May have an infiltrative border with nonneoplastic liver, which is usually not cirrhotic
- Can be classified based on the relative amounts of the 3 tissue types: mixed (conventional) type (> 20% of each of the 3 tissue types); lipomatous (> 80% fat); angiomatous (> 80% blood vessels); myomatous (> 80% smooth muscle); angiomyomatous, myoangiomatous, myolipomatous, lipomyomatous, lipoangiomatous, angiolipomatous (Histopathology 2012;61:863)
Microscopic (histologic) images
Virtual slides
Cytology description
- Fine needle aspiration has been rarely reported
- Clusters of adipocytes and mesenchymal cells with granular to fibrillary cytoplasm, pleomorphic oval nuclei and occasional prominent nucleoli (Ann Saudi Med 2001;21:324)
- No mitoses or necrosis (Ann Saudi Med 2001;21:324)
Positive stains
- HMB45 (smooth muscle component)
- SMA (smooth muscle component)
- MelanA (smooth muscle component)
- KIT / CD117 (Am J Surg Pathol 2002;26:493)
Negative stains
Molecular / cytogenetics description
- Sporadic: mutations in TSC2 via next generation sequencing (NGS) (Histopathology 2018;73:101)
Sample pathology report
- Liver, partial hepatectomy:
- Angiomyolipoma (see comment)
- Comment: Sections show a tumor composed of epithelioid cells, adipocytes and blood vessels. The epithelioid cells show positive staining for HMB45 and SMA and negative staining for keratin (AE1 / AE3) and hepatocyte markers (arginase and HepPar). The positive HMB45 and SMA stains support melanocytic and smooth muscle differentiation, respectively. The negative keratin stain argues against carcinoma and the negative HepPar and arginase stains argue against hepatocellular adenoma and hepatocellular carcinoma. Overall, the morphologic and immunohistochemical features are those of angiomyolipoma.
Differential diagnosis
- Hepatocellular carcinoma:
- Hepatocellular adenoma:
- Gastrointestinal stromal tumor:
- Metastatic melanoma (J Cutan Pathol 2020;47:824):
- Lacks lipomatous component
- More diffusely S100 positive
- High mitotic rate
- Clinical history of melanoma
- Metastatic carcinoma:
Board review style question #1
The cells in this image of a liver tumor show positive staining for HMB45 and negative staining for arginase. Which of the following is true about this lesion?
- It frequently recurs or metastasizes following resection
- It is a rare variant of hepatocellular carcinoma with good prognosis
- It is associated in about 5 - 10% of cases with tuberous sclerosis
- It is more common in men than in women
Board review style answer #1
C. It is associated in about 5 - 10% of cases with tuberous sclerosis
Comment Here
Reference: Angiomyolipoma
Comment Here
Reference: Angiomyolipoma
Board review style question #2
Board review style answer #2