Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Ijaz K, Yin F. Bile duct adenoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/livertumorbileductadenoma.html. Accessed April 17th, 2024.
Definition / general
- Bile duct adenoma is a benign biliary neoplasm consisting of uniformly distributed small bile ducts in a background of fibrotic stroma
Essential features
- Benign epithelial tumor
- Most commonly a solitary subcapsular nodule (90%)
- Frequently an incidental finding at surgery or autopsy
- Frequently submitted for frozen section to rule out metastatic process
- Can be difficult to distinguish from adenocarcinoma, especially on frozen section
- Uniform distribution of small tubules with no cytological atypia or mitotic figures
- Frequent BRAF V600E mutation supports a neoplastic process
Terminology
- Also known as peribiliary gland hamartoma, cholangioma, cholangioadenoma
ICD coding
- ICD-O: 8160/0 - bile duct adenoma
- ICD-11: 2E92.7 & XH6KR6 - benign neoplasm of liver or intrahepatic bile ducts & bile duct adenoma
Epidemiology
- Usually adults (age > 20), no gender predilection
- Accounts for 1.3% of primary liver tumors and 2.4% in a total of 1,456 resection cases for primary liver tumors and explant for liver cirrhosis (Am J Surg Pathol 1988;12:708, Pathol Int 2014;64:551)
Sites
- Liver, typically subcapsular location
Pathophysiology
- Originally considered to be a reactive ductular proliferation in response to focal injury, a localized biliary healing response equivalent to the function of a peribiliary gland or pyloric gland metaplasia in the foregut or a hamartomatous process (Am J Surg Pathol 1988;12:708, Am J Surg Pathol 2010;34:1312, Am J Surg Pathol 1996;20:858)
- Presence of frequent BRAF V600E mutation supports a neoplastic process (Hepatology 2015;61:403, Histopathology 2015;67:562, Histopathology 2017;70:485)
Etiology
- Unknown; whether focal injury acts as trigger event remains controversial
Clinical features
- Mostly an incidental finding during surgery or autopsy
- Frequently submitted for frozen section to rule out metastatic process
Diagnosis
- Clinical presentation and histopathologic findings
Radiology description
- Hypointense on T1 weighted images, hyperintense on T2 weighted images
- Characteristic arterial phase hyperenhancement that persists into the portal venous and delayed phases on CT and MRI (Diagn Interv Radiol 2018;24:249)
Prognostic factors
- Potential and controversial precursor to intrahepatic cholangiocarcinoma (Histopathology 2021;78:310, Hepatology 2015;61:403, Histopathology 2015;67:562)
Case reports
- 18 month old boy with a large (10 cm) exophytic solid liver tumor (World J Gastrointest Surg 2019;11:414)
- 35 year old woman with resolution of bile duct adenomas after discontinuing oral contraceptive pills (Middle East J Dig Dis 2016;8:327)
- 62, 65 and 76 year old men were identified as having a bile duct adenoma (Endosc Int Open 2018;6:E1312)
- 70 year old man with an incidental finding of intrahepatic bile duct adenoma during laparoscopic distal gastrectomy for gastric cancer (Int Cancer Conf J 2018;8:7)
Gross description
- Usually subcapsular, well circumscribed but nonencapsulated
- Majority are solitary but can be multiple
- Firm, gray-white
- Size ranging from 1 to 20 mm (mean: 5.8 mm) (Am J Surg Pathol 1988;12:708)
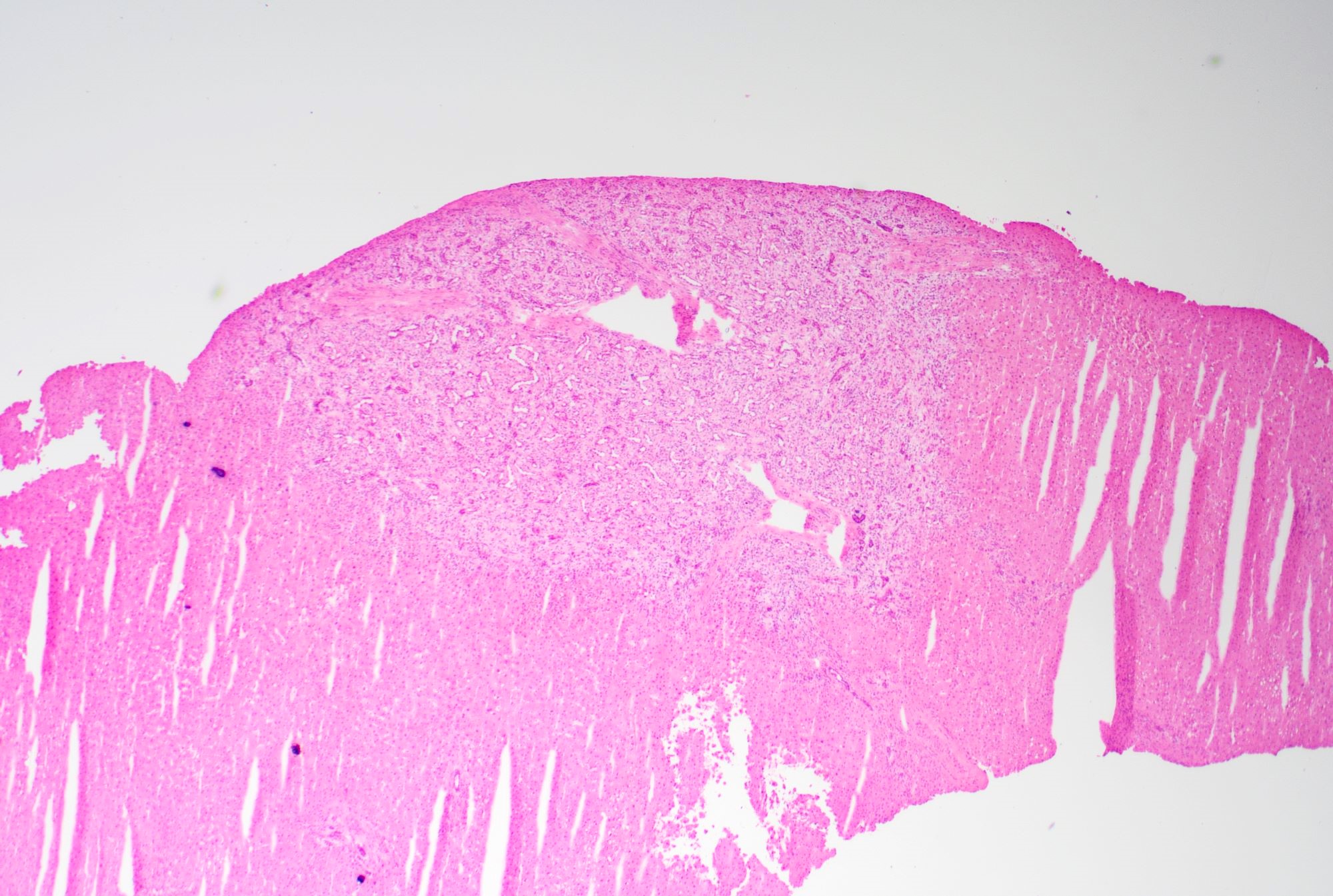
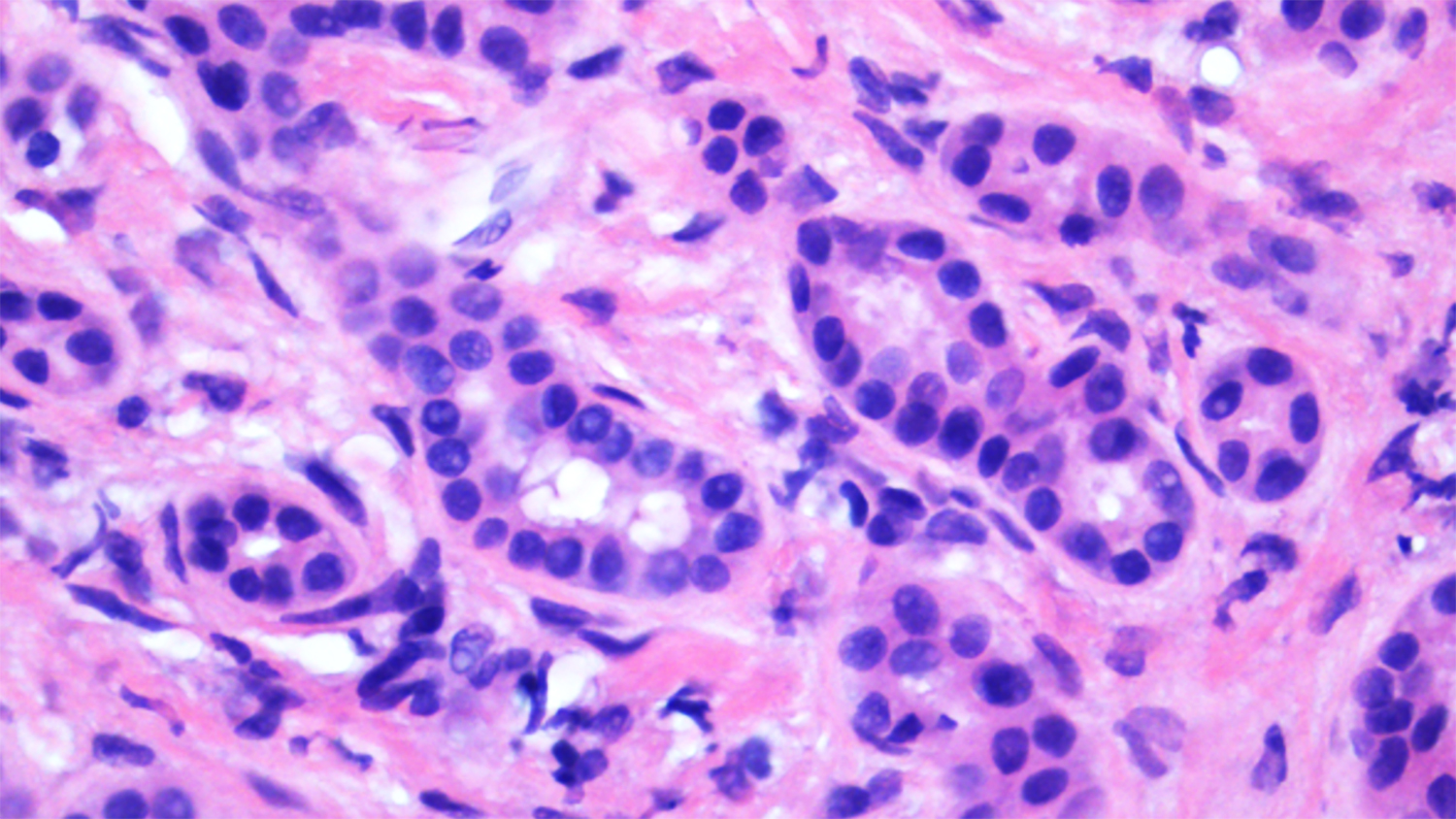
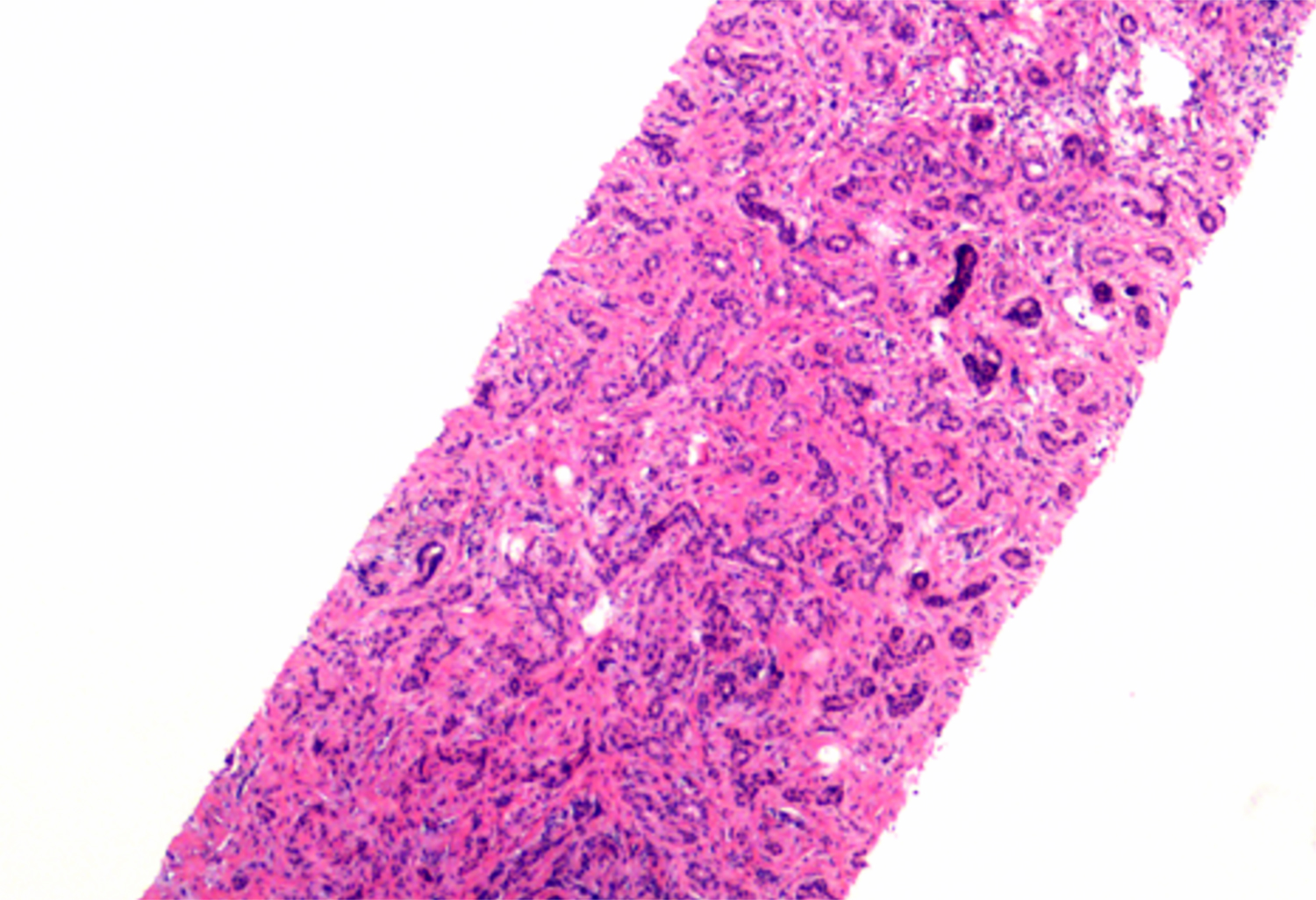
Frozen section description
- Usually solitary subcapsular lesion, well circumscribed and nonencapsulated
- Bland small tubular proliferation in a background of fibrotic stroma
- Lack of marked nuclear atypia, mitotic figures, necrosis or intraluminal bile
- Potential diagnostic pitfalls: cellular stroma, back to back compact architecture, mucin production, unusual variant (oncocytic, clear cell, etc.), cytologic atypia enhanced by frozen section artifact
Frozen section images
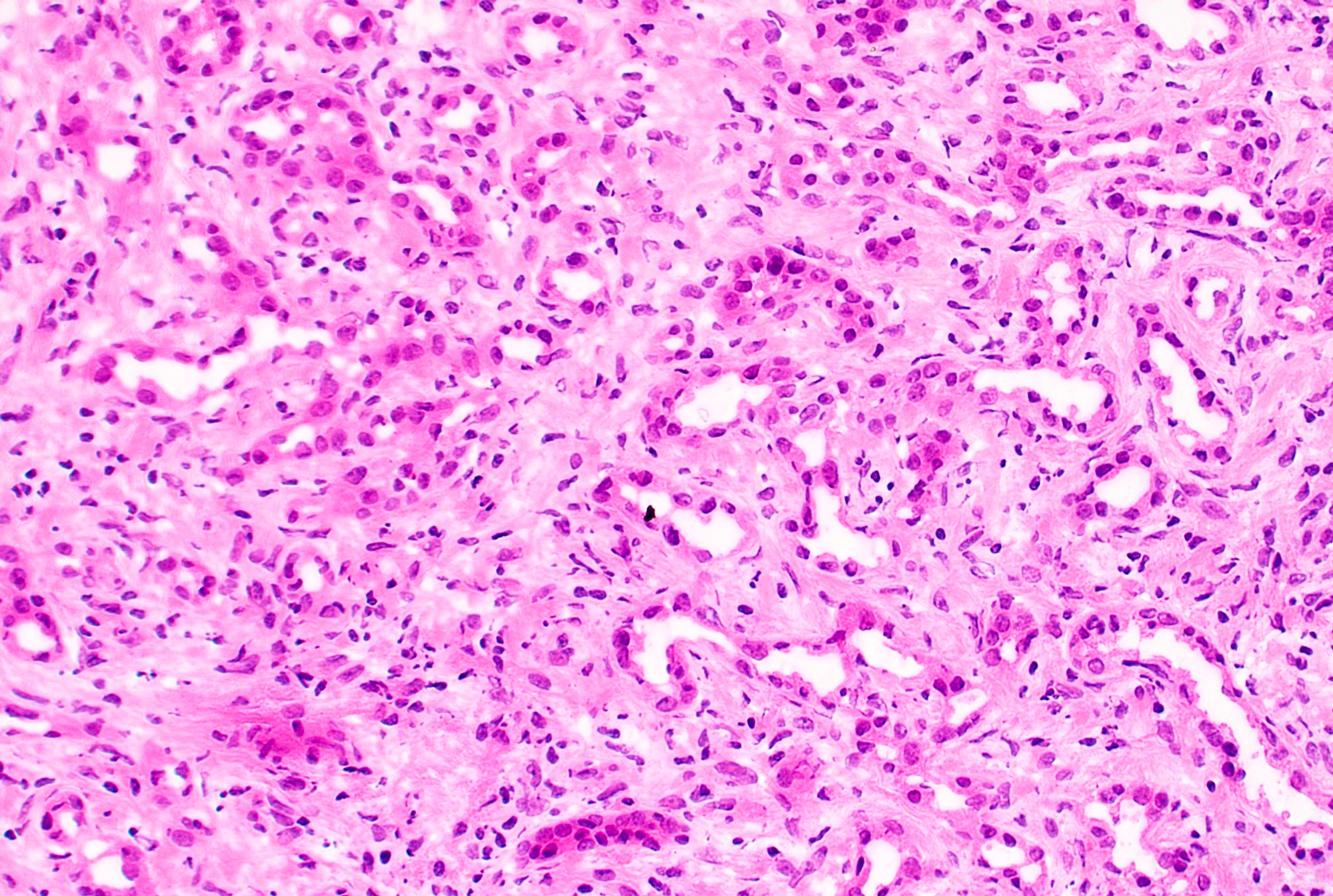
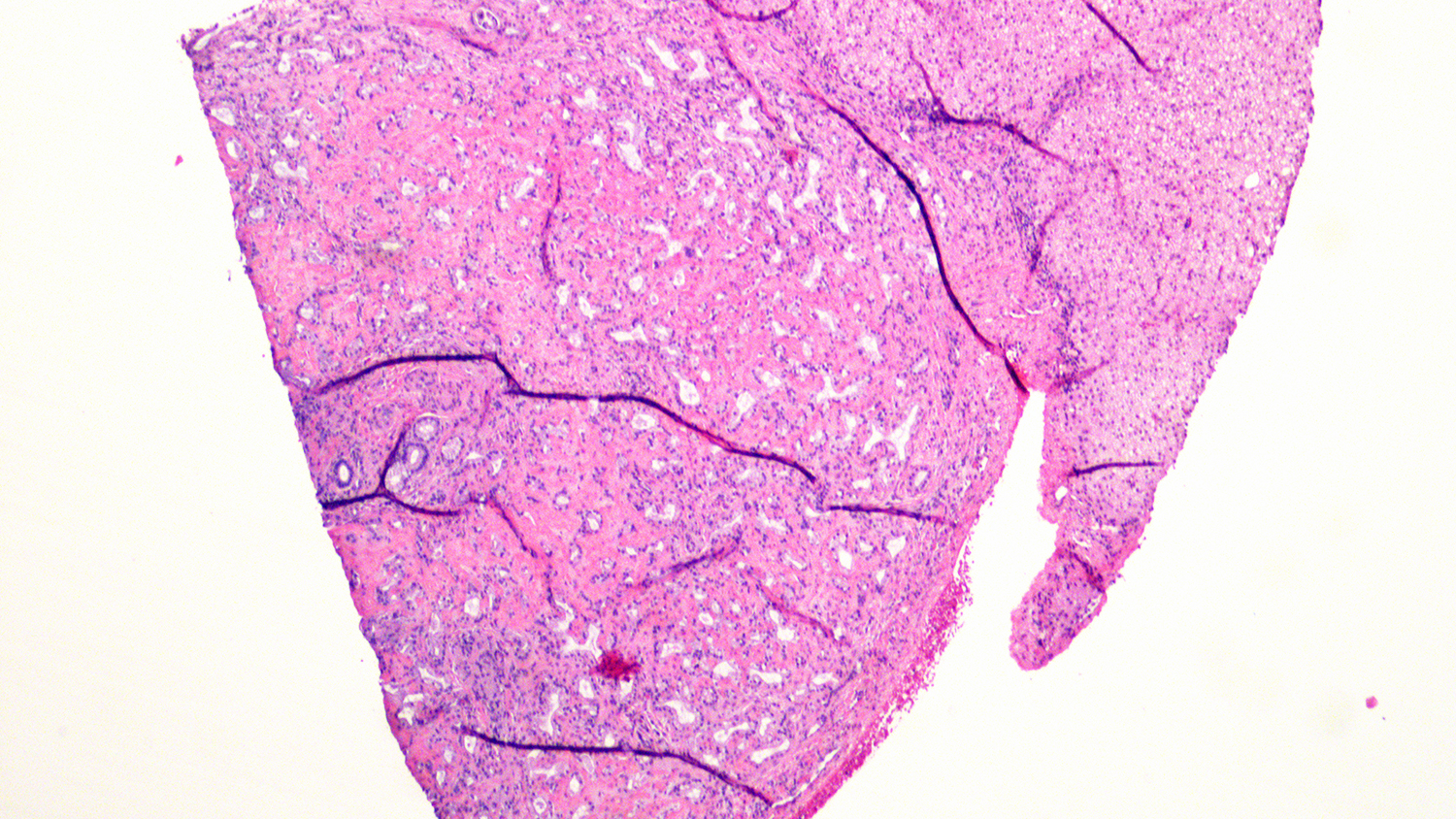
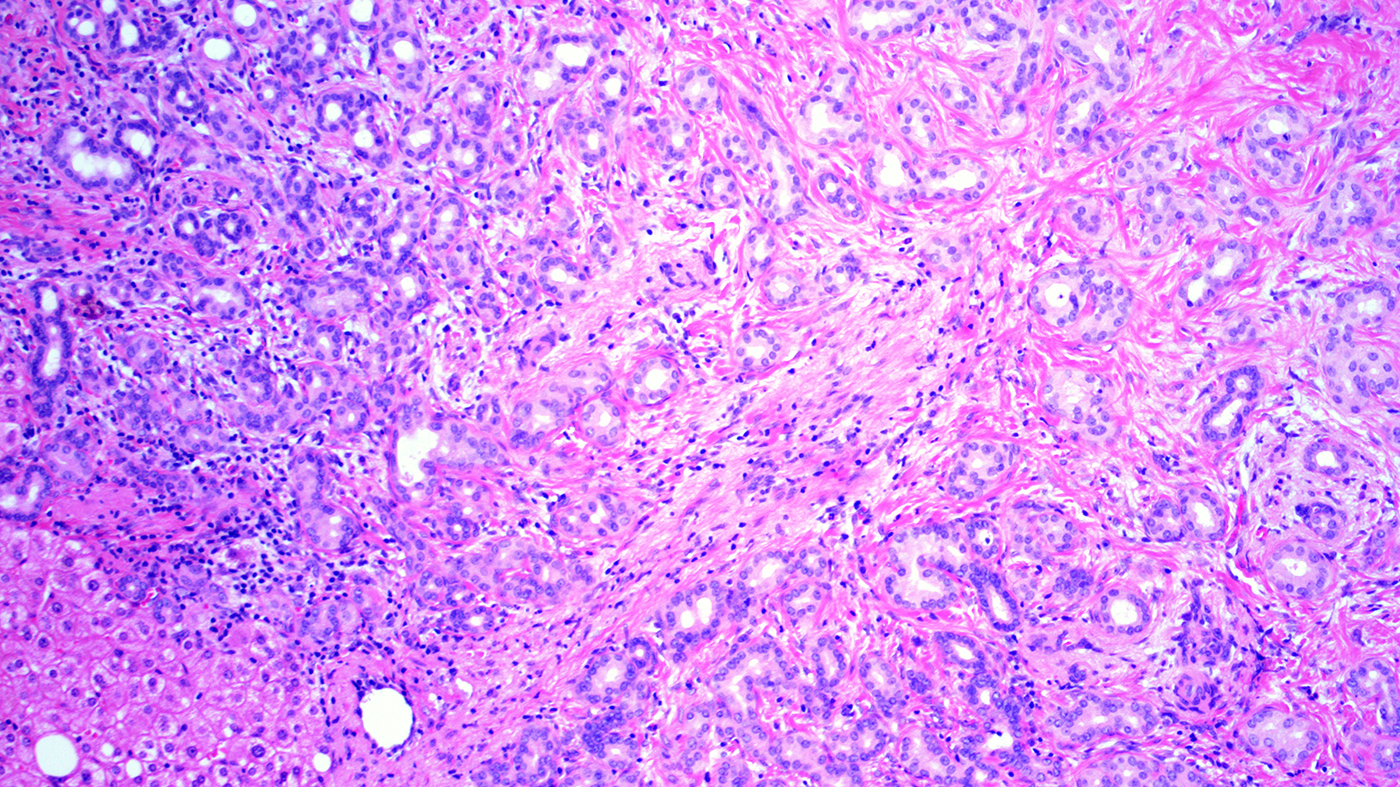
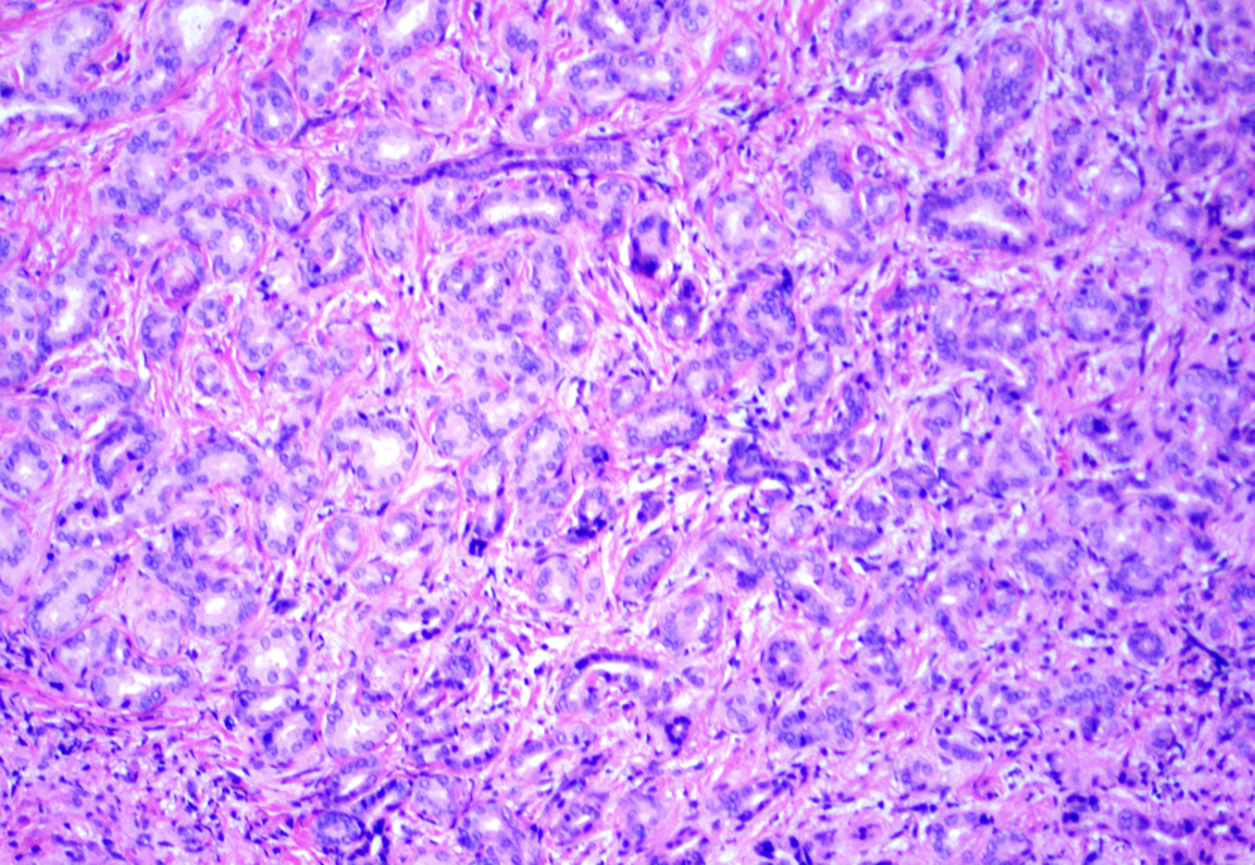
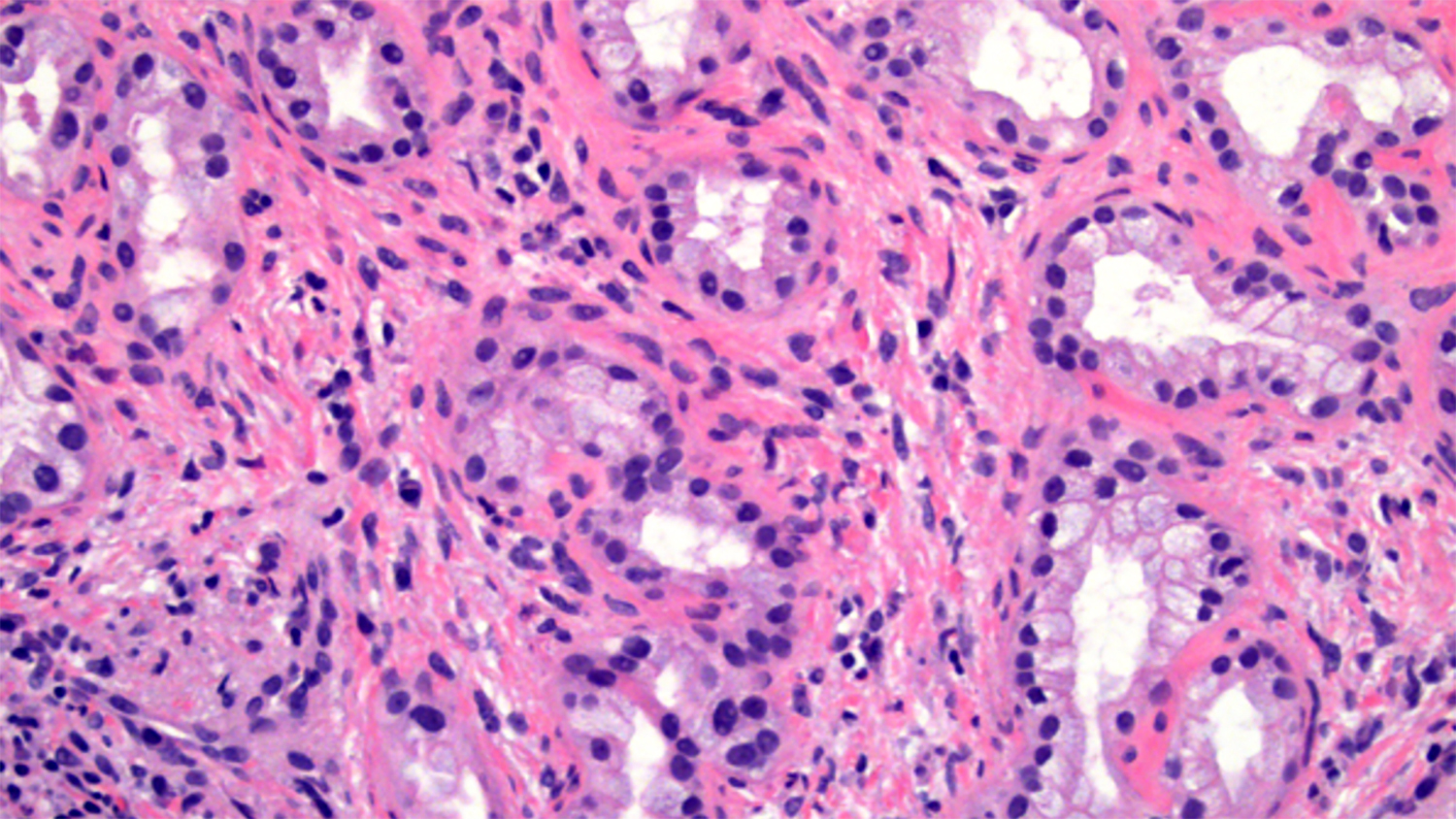
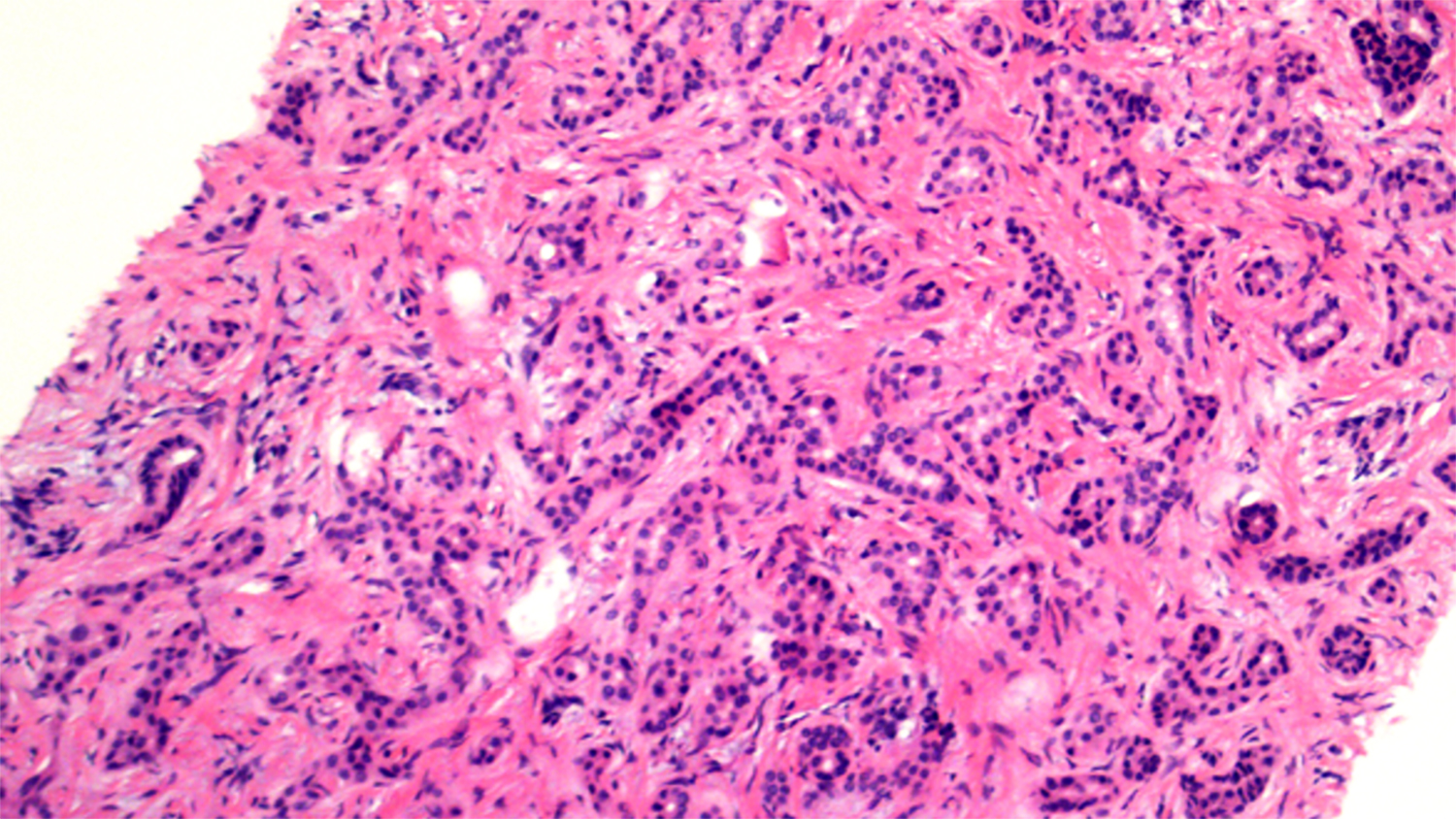
Microscopic (histologic) description
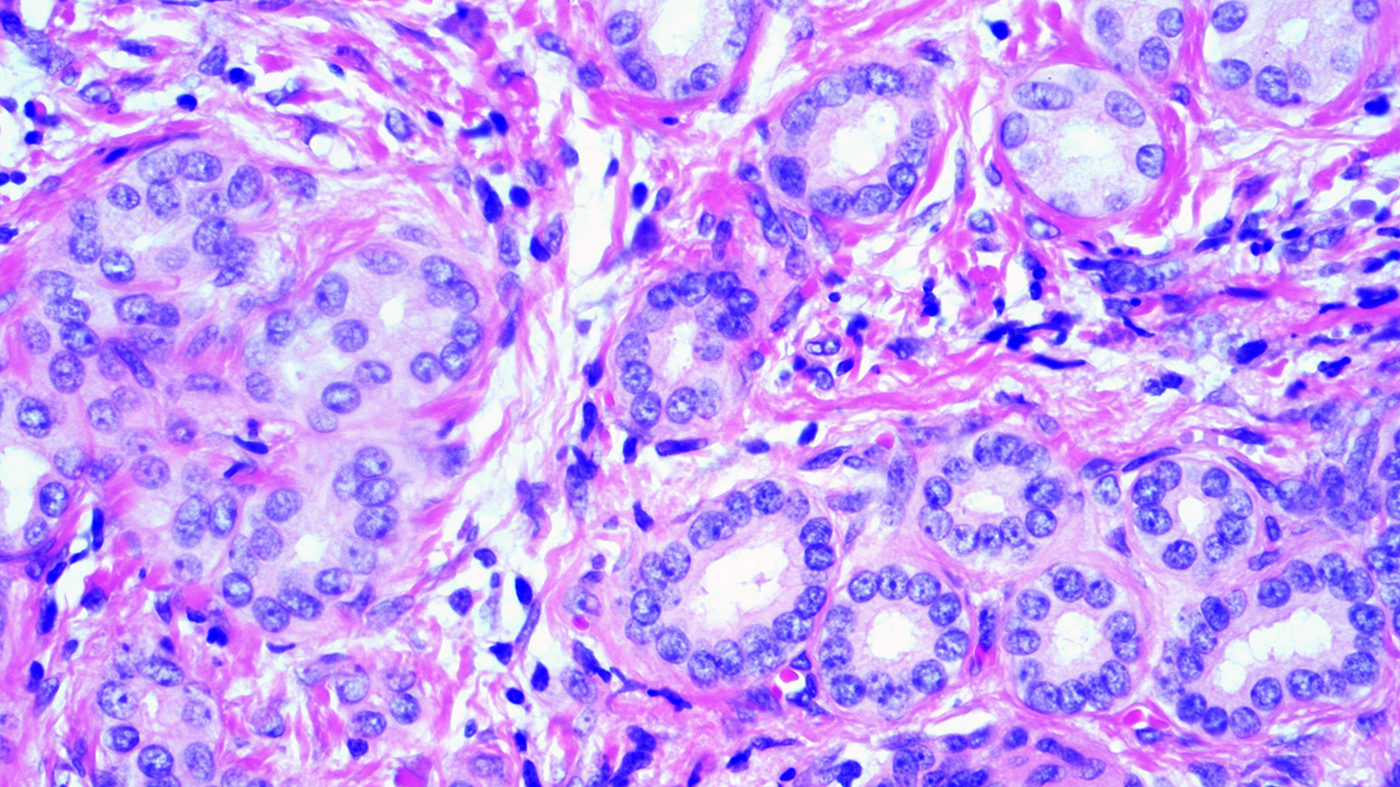
- Relatively uniform distribution of small tubules with little to no lumen
- Lined by single layer of cuboidal cells with no cytological atypia or mitotic figures
- Well circumscribed with fibrotic stroma
- No intraluminal bile; the ducts do not communicate with the biliary tree
- Rarely, variants with clear cell change, oncocytic features, mucin secreting and alpha-1 antitrypsin droplets (Am J Surg Pathol 2001;25:956, Case Rep Pathol 2014;2014:874826, Case Rep Pathol 2014;2014:282010, Dig Surg 2002;19:324, Int J Surg Pathol 2008;16:218)
Microscopic (histologic) images
Cytology description
- Abundant normal appearing biliary epithelium
- Often admixed with benign hepatocytes
- Cell block may be useful
- Reference: Sidawy: Fine Needle Aspiration Cytology, 1st Edition, 2007
Positive stains
- Typical biliary immunoprofile (positive for CK7 and CK19)
- Expression of foregut antigens (positive for MUC5AC and MUC6) (Am J Surg Pathol 2010;34:1312)
- Ki67 proliferation rate is low (should not be more than 10%)
- BRAF V600E immunoreactivity in 53% of cases (Histopathology 2015;67:562)
- p16INK4a immunoreactivity in 81% of cases (Am J Surg Pathol 2014;38:364)
Negative stains
Molecular / cytogenetics description
- Majority of bile duct adenomas are positive for albumin in situ hybridization, a feature that distinguishes it from metastatic pancreatic adenocarcinoma (Histopathology 2016;69:423)
Sample pathology report
- Liver, wedge biopsy:
- Intrahepatic bile duct adenoma (see comment)
- Comment: The biopsy demonstrates the proliferation of small tubules with no cytological atypia embedded in the fibrous stroma, consistent with bile duct adenoma.
Differential diagnosis
- Cholangiocarcioma or metastatic adenocarcinoma:
- Cytological atypia, mitosis, size may be > 2 cm
- Infiltrative growth pattern
- Extensive expression of EZH2, no or low expression of p16INK4a (Am J Surg Pathol 2014;38:364)
- Ki67 > 10%
- Lymphovascular or perineural invasion
- Von Meyenburg complex (biliary microhamartoma):
- Angulated, branching and irregularly dilated ducts
- Intraluminal bile plugs
Board review style question #1
A 55 year old man with pancreatic adenocarcinoma was admitted for Whipple procedure. A small liver nodule was noted during surgery and sent for intraoperative consultation. A representative photomicrograph of the frozen section is shown. Which of the following is the most likely diagnosis?
- Bile duct adenoma
- Metastatic pancreatic adenocarcinoma
- Reactive ductular proliferation
- Von Meyenburg complex
Board review style answer #1
A. Bile duct adenoma. The diagnosis of a bile duct adenoma is favored during intraoperative consultation, largely attributed to the presence of uniform distribution of small tubules in a background of fibrous stroma. There are no worrisome morphological features, such as infiltrative growth pattern, desmoplastic stromal reaction, marked cytological atypia, frequent mitosis and necrosis.
Comment Here
Reference: Bile duct adenoma
Comment Here
Reference: Bile duct adenoma
Board review style question #2
Which gene is most frequently mutated in bile duct adenoma?
- BRAF
- KRAS
- p53
- SMAD4
Board review style answer #2
A. BRAF mutations are present in about 53% of bile duct adenomas.
Comment Here
Reference: Bile duct adenoma
Comment Here
Reference: Bile duct adenoma