Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Albayrak NE, Ward SC. Focal fatty change. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/livertumorfattychange.html. Accessed April 23rd, 2024.
Definition / general
- Steatosis is normally a diffuse process; however, a more localized form called focal fatty change (FFC) was first described in 1980 (Gastroenterology 1980;78:247)
Essential features
- Benign, asymptomatic and incidental finding in 10 - 20% of livers
- Uncommon in infants and young children
- Major clinical importance lies in its differentiation from other lipomatous liver lesions
Terminology
- Focal fatty change, focal steatosis, focal fatty infiltration
ICD coding
- ICD-10: K76.0 - fatty (change of) liver, not elsewhere classified
Epidemiology
- Incidental finding found in approximately 10 - 20% of livers
- Prevalence increases with advancing age:
- 0% for 1 month - 4 years
- 7.3% for 5 - 9 years
- 10.2% for 10 - 14 years
- 25.6% for 15 - 19 years (AJR Am J Roentgenol 2001;177:1035)
Sites
- Typical areas include the gallbladder fossa, subcapsular, left lobe medial segment near the fissure for the ligamentum teres, anterior to the porta hepatis and around the inferior vena cava
Pathophysiology
- May be caused by relative ischemia due to decreased portal venous blood flow or decreased delivery of substances via the portal vein
- Aberrant vascular supply to the liver other than the portal vein or hepatic artery
- Aberrant localized (endogenous or exogenous) insulin effects: injection or intraperitoneal administration of insulin in patients with peritoneal hemodialysis has led to unusual patterns of focal liver steatosis in the subcapsular region (AJR Am J Roentgenol 2003;180:1601)
Clinical features
- Causes no mass effect or symptoms
Diagnosis
- Contrast enhanced ultrasound (CEUS)
- Abdominal CT with or without contrast
- MRI with fat suppression
- Radionuclide liver scan (Clin Nucl Med 1986;11:503)
- Definitive diagnosis with biopsy can be established in clinically challenging cases where it is difficult to distinguish from metastatic disease
Laboratory
- Liver function tests are usually within normal limits
Radiology description
- Hypodense appearance on CT scan makes it difficult to differentiate fatty infiltration from metastatic disease, particularly when multiple lesions are present
- In focal fatty infiltration, the normal hepatic vessels traverse the area of decreased attenuation, a finding not usually present in malignancy
- Persistent isoenhancement on contrast enhanced ultrasound compared with liver parenchyma
- MRI with fat suppression is more sensitive than T1 and T2 weighted imaging for fatty infiltration, with fatty infiltration having decreased signal intensity compared with normal liver
- Decreased signal on opposed phase T1 weighted imaging
- Reference: Medicine (Baltimore) 2019;98:e15431
Case reports
- 30 year old man with a history of chronic hepatitis C (World J Radiol 2014;6:932)
- 49 year old woman with multifocal lesions of the liver, interpreted as angiomyolipomas (Ann Ital Chir 2003;74:217)
- 60 year old woman who had undergone subtotal gastrectomy for gastric cancer (Br J Radiol 1998;71:888)
Treatment
- Directed against underlying disorder
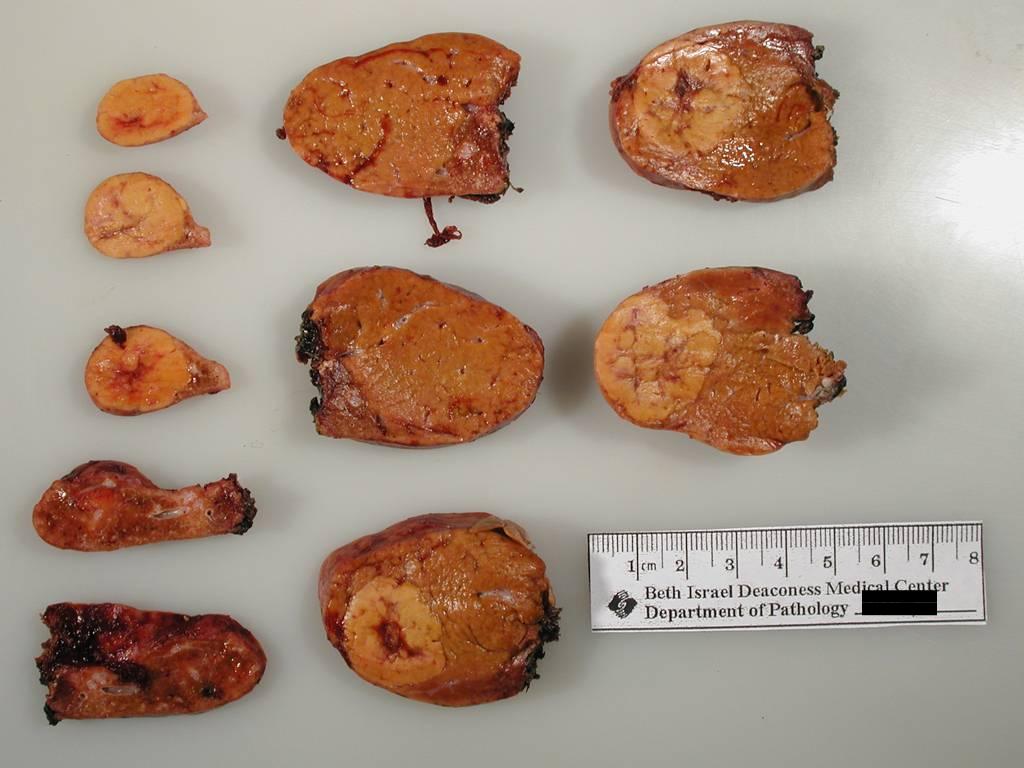
Gross description
- May be solitary or multifocal
- Well demarcated, unencapsulated nodule(s) with a yellow greasy cut surface
- Measures up to 4.0 cm
- Predominantly subcapsular in location
- Reference: Gastroenterology 1980;78:247
Gross images
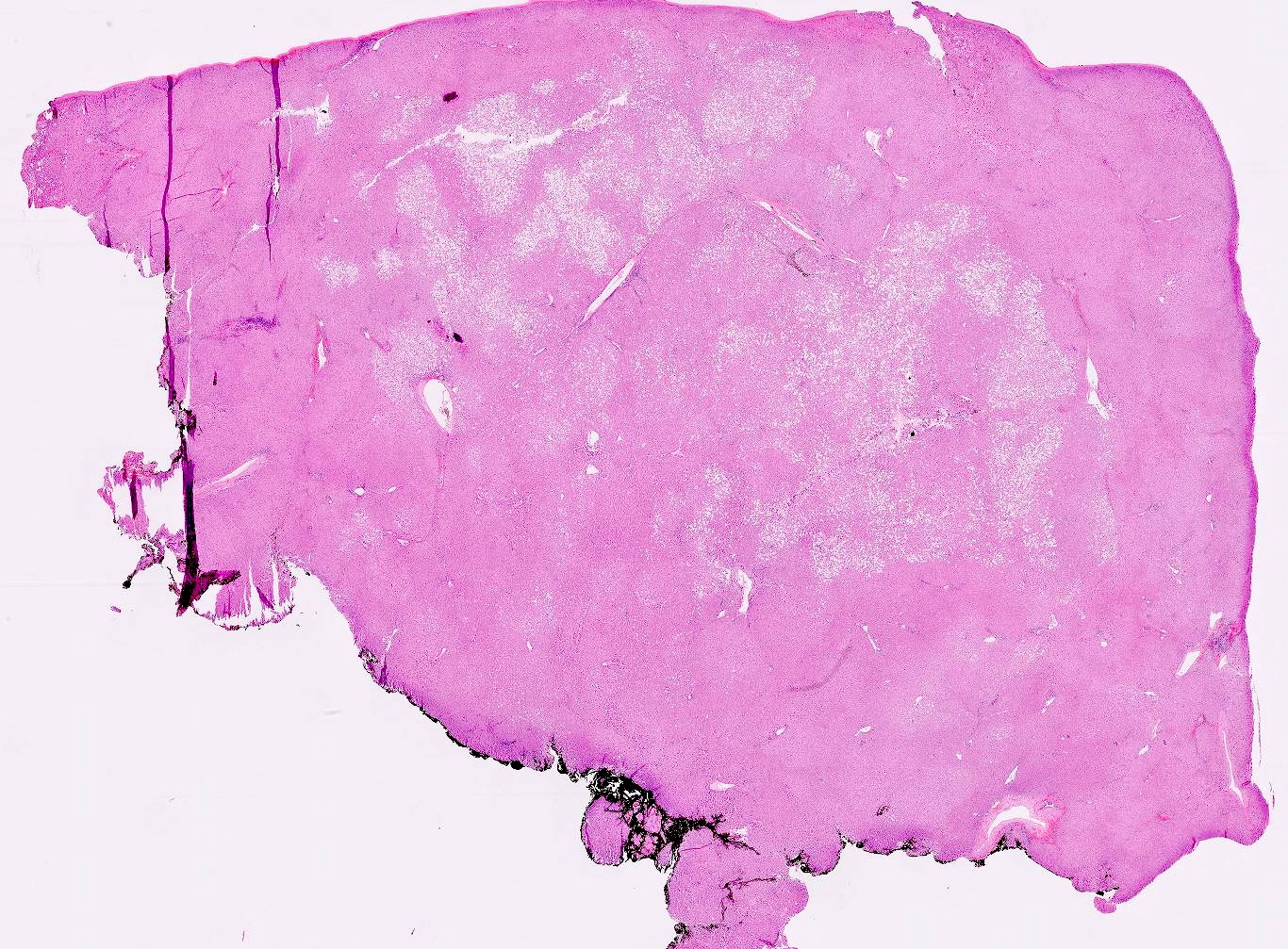
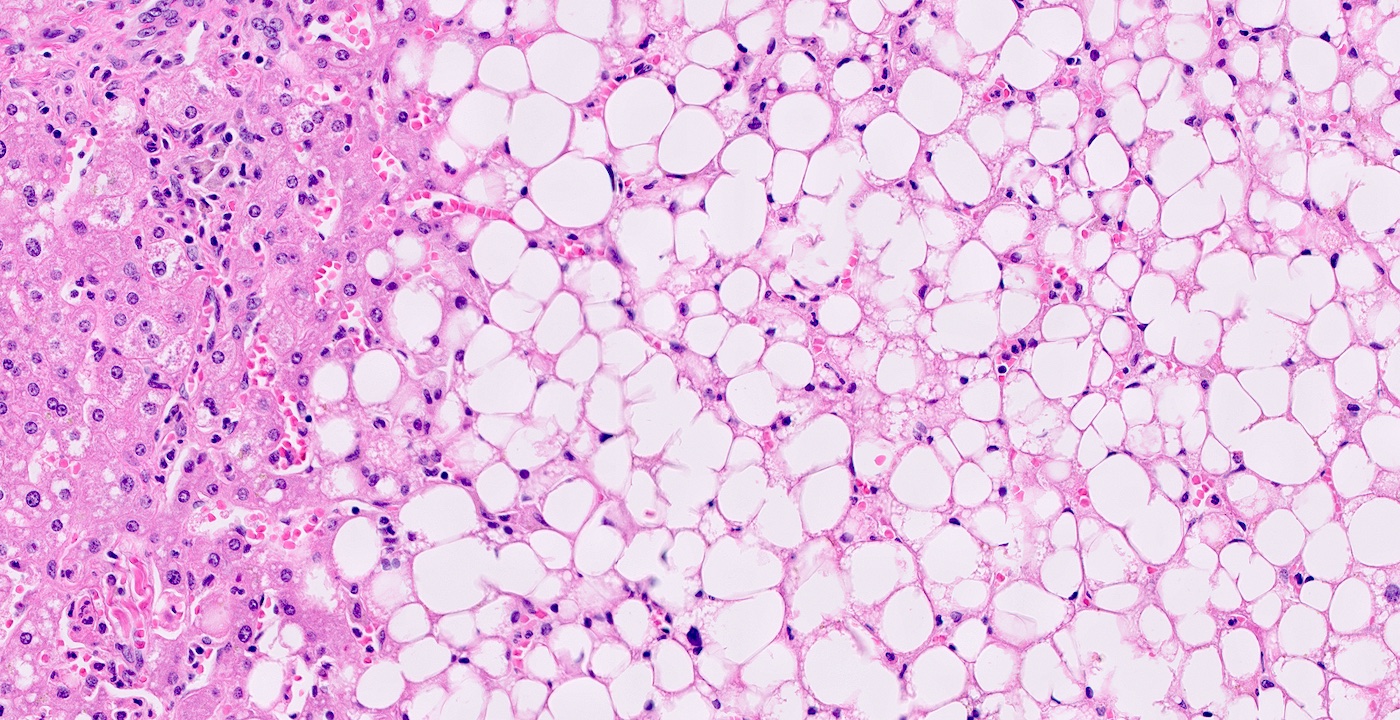
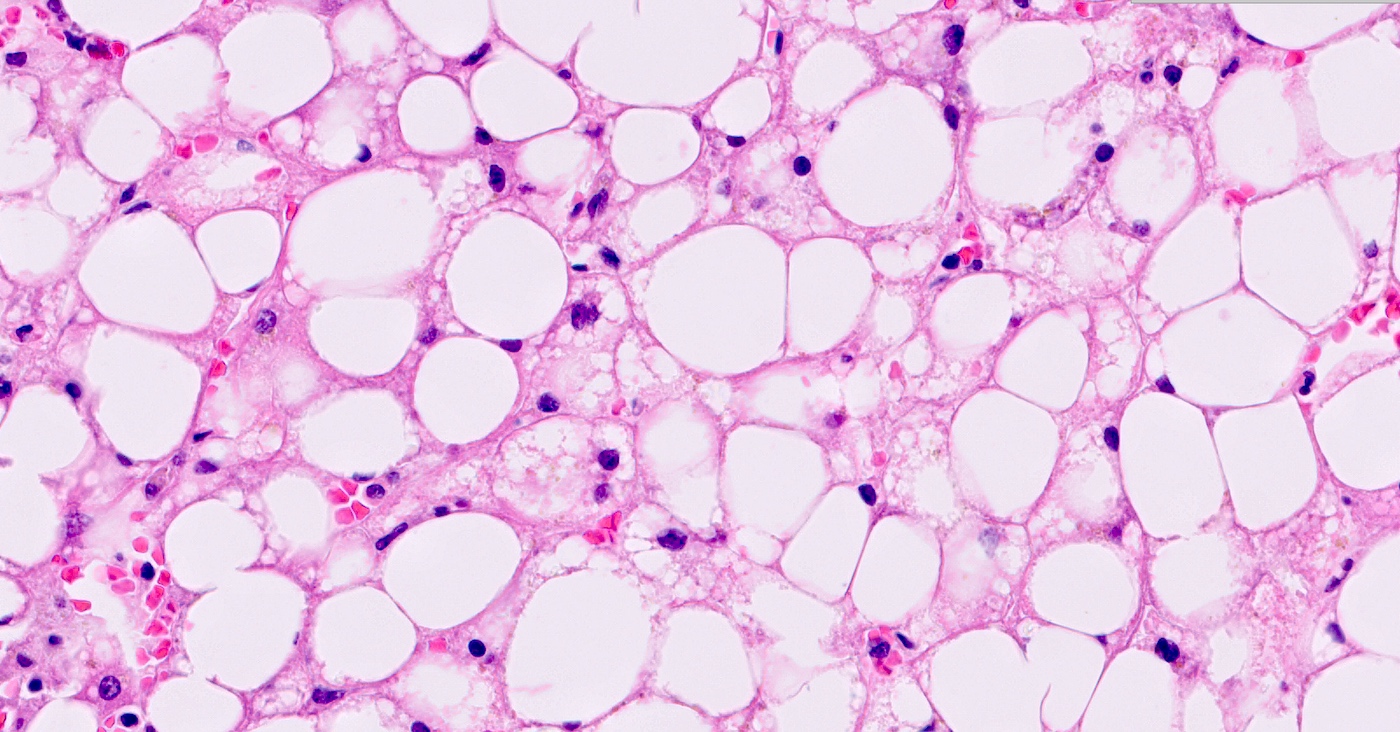
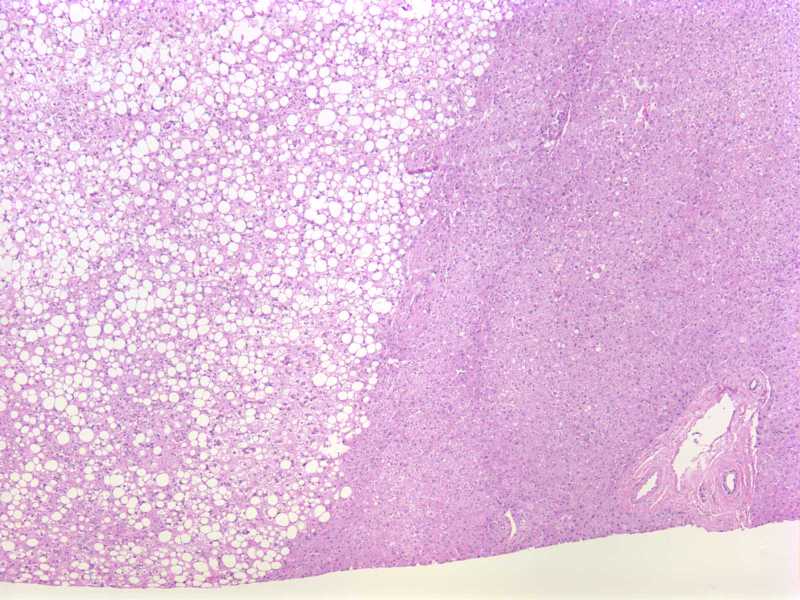
Microscopic (histologic) description
- Well demarcated, unencapsulated areas of severe and typically, macrovesicular steatosis, surrounded by hepatic parenchyma that contains little or no steatosis
- Portal tracts and terminal hepatic veins are present throughout the lesion in a normal architectural pattern
- Adjacent nonsteatotic liver parenchyma may be congested without fibrosis or cirrhosis
- Reference: Gastroenterol Hepatol (N Y) 2007;3:199
Microscopic (histologic) images
Cytology description
- Aspirates are cellular with numerous benign hepatocytes in a background of blood
- Hepatocytes are isolated or organized in sheets
- Characterized by large, intracytoplasmic, clear vacuoles that displace nuclei to the periphery of the cells, sometimes flattening them against the cytoplasmic membrane
- Displaced nuclei by intracytoplasmic, clear vacuoles give these cells a signet ring appearance, resembling signet ring carcinoma
- Special stains:
- PASD stain will give negative results, confirming that intracytoplasmic vacuoles are not constituted of mucus
- Reference: Acta Cytol 2002;46:567
Positive stains
- Oil Red O
- Sudan Black B
- Reference: Cytojournal 2005;2:7
Negative stains
- PASD
- Mucicarmine
- Reference: Cytojournal 2005;2:7
Sample pathology report
- Liver lesion, needle biopsy specimen:
- Focal fatty change (see comment)
- Comment: Within some of the cores are areas of benign liver tissue that show relatively more extensive steatosis, portal tracts that are quite distant from each other and liver cell plates that are slightly thickened (reticulin stain). Based on the given information of a hypodense mass having been biopsied, these findings are consistent with focal fatty change (also known as focal steatosis).
Differential diagnosis
- HNF1α inactivated hepatocellular adenoma:
- Yellow / pale cut surface due to diffuse fatty change
- Markedly steatotic hepatocytes intermingled with clear hepatocytes
- Has other typical features of HCA: unpaired arteries, lack of portal tracts
- Negative LFABP is a surrogate marker for HNF1α inactivation
- Hepatocellular carcinoma, steatohepatitic variant:
- Most occur in background of cirrhosis
- Neoplastic hepatocytes in trabeculae of more than 3 cells thickness
- High nuclear to cytoplasmic ratio, mitoses, unpaired arteries, lack of portal tracts
- Trabecular pattern or pseudoglandular architecture is typically seen
- Angiomyolipoma:
- Focal nodular hyperplasia:
- Nodular but lacks the lipomatous component
- Unencapsulated, well circumscribed lesion with central stellate scar
- Fibrous septa contain thick walled arteries with peripheral ductular reaction but no true bile ducts
- Myelolipoma:
- Variable proportion of hematopoietic precursor cells scattered throughout mature fat
- Lipoma:
Additional references
Board review style question #1
Which of the following liver lesions contains portal tracts and central veins throughout the lesion?
- Focal fatty change
- Focal nodular hyperplasia
- Hepatocellular carcinoma
- HNF1α inactivated hepatocellular adenoma
- Lipoma
Board review style answer #1
Board review style question #2
A 60 year old woman with poorly controlled diabetes mellitus and remote history of gastric cancer was found to have multifocal hypodense lesions in the liver, detected incidentally on an abdominal CT scan. A representative core needle biopsy of the lesion is shown above. What is your diagnosis?
- Focal fatty change
- Focal nodular hyperplasia
- Hepatocellular carcinoma
- Lipoma
- Metastatic gastric adenocarcinoma
Board review style answer #2