Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: McCarthy M, Zhang L. Hemangioma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/livertumorhemangioma.html. Accessed April 26th, 2024.
Definition / general
- Benign vascular tumors further classified based on characteristic morphologic findings
- Predominately asymptomatic with no reported malignant transformation
Essential features
- Hepatic hemangiomas are the most common benign tumor of the liver
- Classification is based on characteristic histologic features; there should be no significant cytologic atypia or mitotic activity
- Vast majority of hemangiomas are asymptomatic and require no intervention; larger lesions (> 5 cm) are more likely to be symptomatic and susceptible to complications such as hemorrhage, rupture and Kasabach-Merritt syndrome
- No cases of malignant transformation have been documented
Terminology
- Cavernous hemangioma
- Most common subtype of hepatic hemangioma
- Capillary hemangioma
- Extremely rare
- Anastomosing hemangioma
- Rare, newly described variant
- More frequently occurs in genitourinary tract
- Sclerosing / sclerosed hemangioma
- Hepatic small vessel neoplasm
- Rare, with mild atypical features
- Benign or low grade entity in adults
- No cases of recurrences or metastasis reported
ICD coding
Epidemiology
- Most common benign hepatic tumor (Visc Med 2020;36:292)
- Prevalence as high as 20% in general population (Visc Med 2020;36:292)
- Occurs at any age but the third to fifth decade is most common
- Female predominance, F:M = 5:1 (Visc Med 2020;36:292)
Sites
- Most often found in right lobe of liver, particularly segment IV, subcapsular location (J Med Life 2015;8 Spec Issue:4)
Etiology
- Precise pathogenesis unknown
- Arises from vascular malformation (Visc Med 2020;36:292)
- Vascular endothelial growth factor (VEGF) may contribute to development of hepatic hemangiomas (Visc Med 2020;36:292)
- Hormone replacement, oral contraceptives and pregnancy may contribute to growth of hepatic hemangiomas; however, the lesions are negative for estrogen and progesterone receptors (Visc Med 2020;36:292, World J Gastroenterol 2020;26:11)
Clinical features
- Vast majority are asymptomatic and incidental findings on imaging studies
- Large tumors (> 5 cm) are more likely to be symptomatic
- Spontaneous hemorrhage is uncommon; 1 literature review shows only 46 cases between 1898 and 2010 (Visc Med 2020;36:292, J Hepatobiliary Pancreat Sci 2011;18:797)
- Kasabach-Merritt syndrome is a rare, potentially life threatening consumptive coagulopathy leading to intravascular coagulation and thrombocytopenia (Visc Med 2020;36:292, StatPearls: Kasabach Merritt Syndrome [Accessed 11 December 2020])
- Occurs in 26% of hemangiomas > 15 cm
- Reversible with resection of hemangioma
Diagnosis
- Predominantly based on imaging studies
- Core needle biopsy contraindicated due to risk of hemorrhage and low diagnostic yield (J Med Life 2015;8 Spec Issue:4)
Laboratory
- Alkaline phosphatase (ALP) and gamma glutamyl transferase (GGT) usually within normal limits (Visc Med 2020;36:292)
- Alpha fetoprotein (AFP), carcinogenic antigen 19-9 (CA 19-9) and carcinogenic antigen (CEA) within normal limits (J Med Life 2015;8 Spec Issue:4)
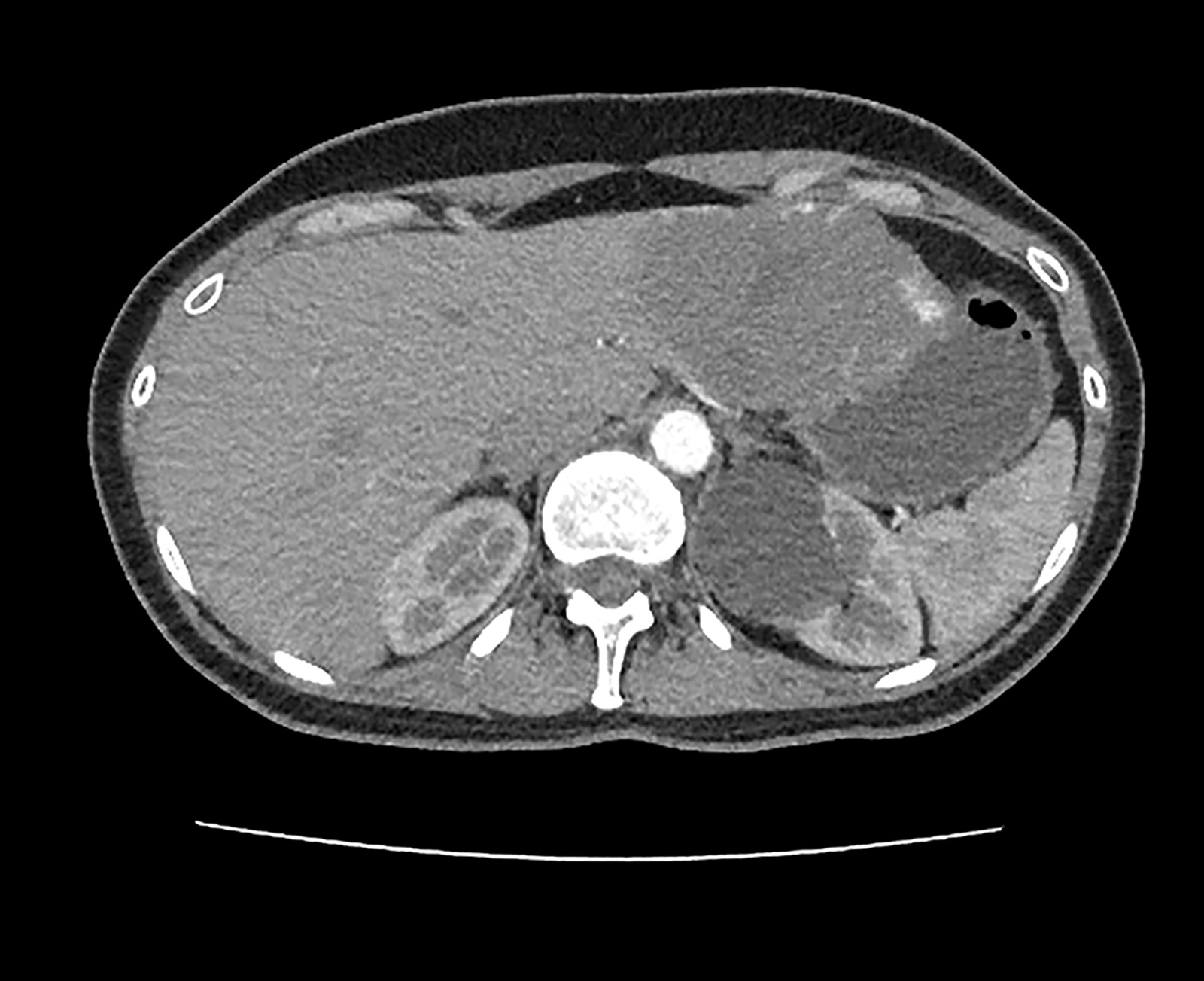
Radiology description
- Multiple modalities available (J Med Life 2015;8 Spec Issue:4)
- Overall stable findings on serial exam are a reliable indicator of benignity
- Contrast enhancing ultrasonographic and technetium-99m scintigraphy are most specific
- Ultrasound (US)
- Conventional: well circumscribed homogenous nodule; hyperechoic in smaller lesions, mixed echogenicity in larger lesions
- Contrast enhancing: more specific; peripheral nodular enhancement in arterial phase, centripetal filling in late phase
- Computer tomography (CT)
- Well circumscribed hypodense lesion
- Contrast demonstrates peripheral nodular enhancement with progressive centripetal filling
- Magnetic resonance imaging (MRI)
- Well circumscribed homogenous lesion
- Hypointense on T1, hyperintense with "cotton wool" appearance on T2
- Technetium-99m scintigraphy
- Perfusion / blood pool mismatch
- Cold lesion in early phase, intensive activity in late phase
Prognostic factors
- Most patients remain asymptomatic and without complication
- No malignant transformation has been reported (Visc Med 2020;36:292)
- < 40% may grow over time and the clinical significance of growth rate is uncertain (World J Gastroenterol 2020;26:11)
Case reports
- 56 year old man with history of gastrointestinal stromal tumor, now with incidental right hepatic lobe mass (J Radiol Case Rep 2019;13:32)
- 57 year old man with lateral hepatic mass (Radiol Case Rep 2018;13:1025)
- 70 year old woman with liver mass and abdominal pain (Rom J Morphol Embryol 2018;59:557)
- 78 year old man with abdominal pain and hypotension (Rev Esp Enferm Dig 2016;108:431)
- 83 year old woman with jaundice, hypofibrinogenemia and thrombocytopenia (Surg Case Rep 2015;1:93)
Treatment
- If small and asymptomatic, surveillance via serial imaging is sufficient (Visc Med 2020;36:292, World J Gastroenterol 2020;26:11)
- If large, symptomatic or malignancy cannot be excluded, surgical management is indicated (Visc Med 2020;36:292, World J Gastroenterol 2020;26:11)
- Surgical management includes: enucleation, segmental resection, lobectomy and rarely transplant
- Nonsurgical management includes angiographic embolization, portal vein embolization, radiofrequency ablation and irradiation (Visc Med 2020;36:292, World J Gastroenterol 2020;26:11)
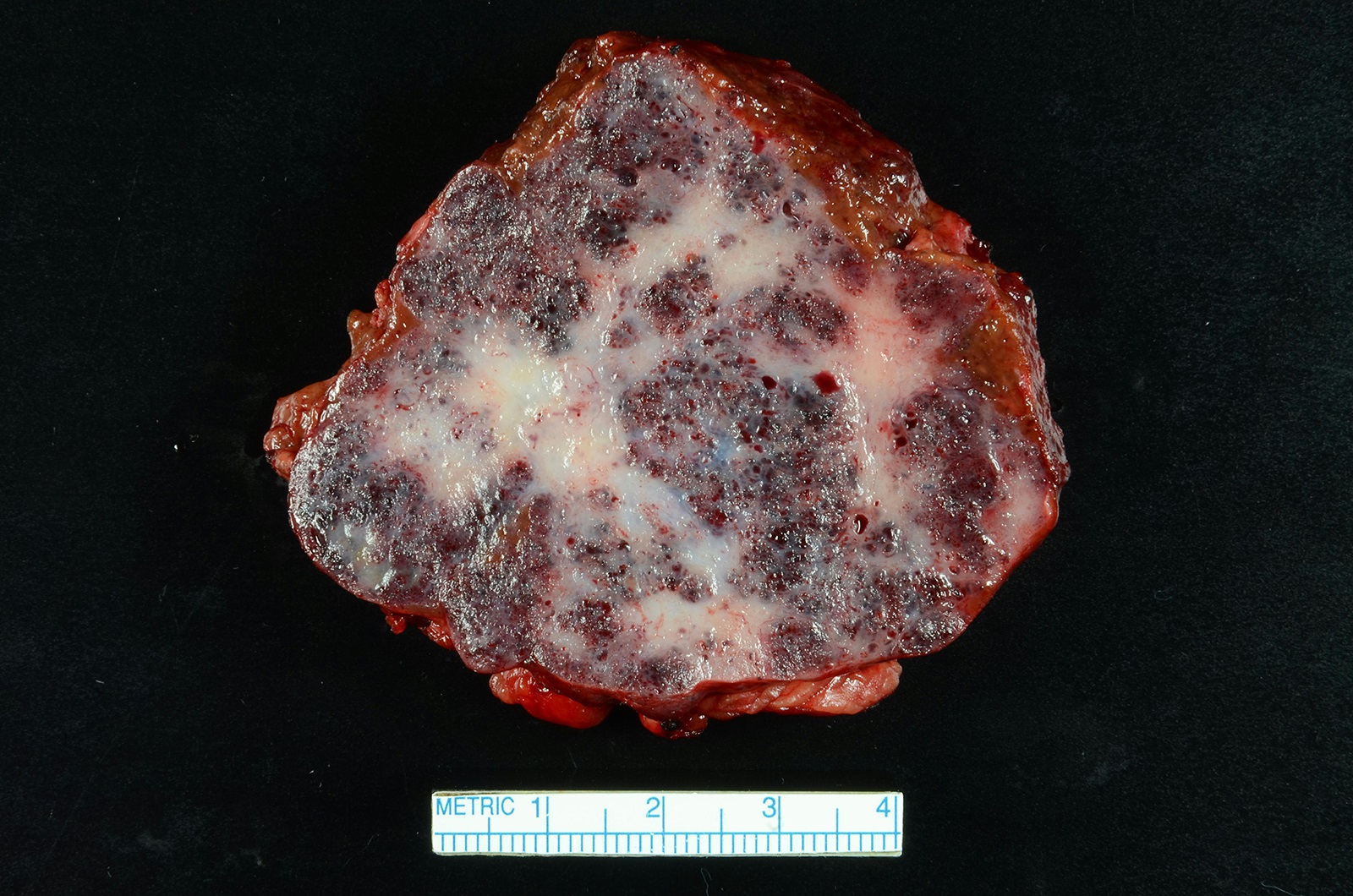
Gross description
- Most often solitary lesions
- Usually < 4 cm but range from a few millimeters to > 30 cm in size
- If > 10 cm, referred to as giant hemangioma
- Well circumscribed with red-brown, spongy / honeycombed cut surface
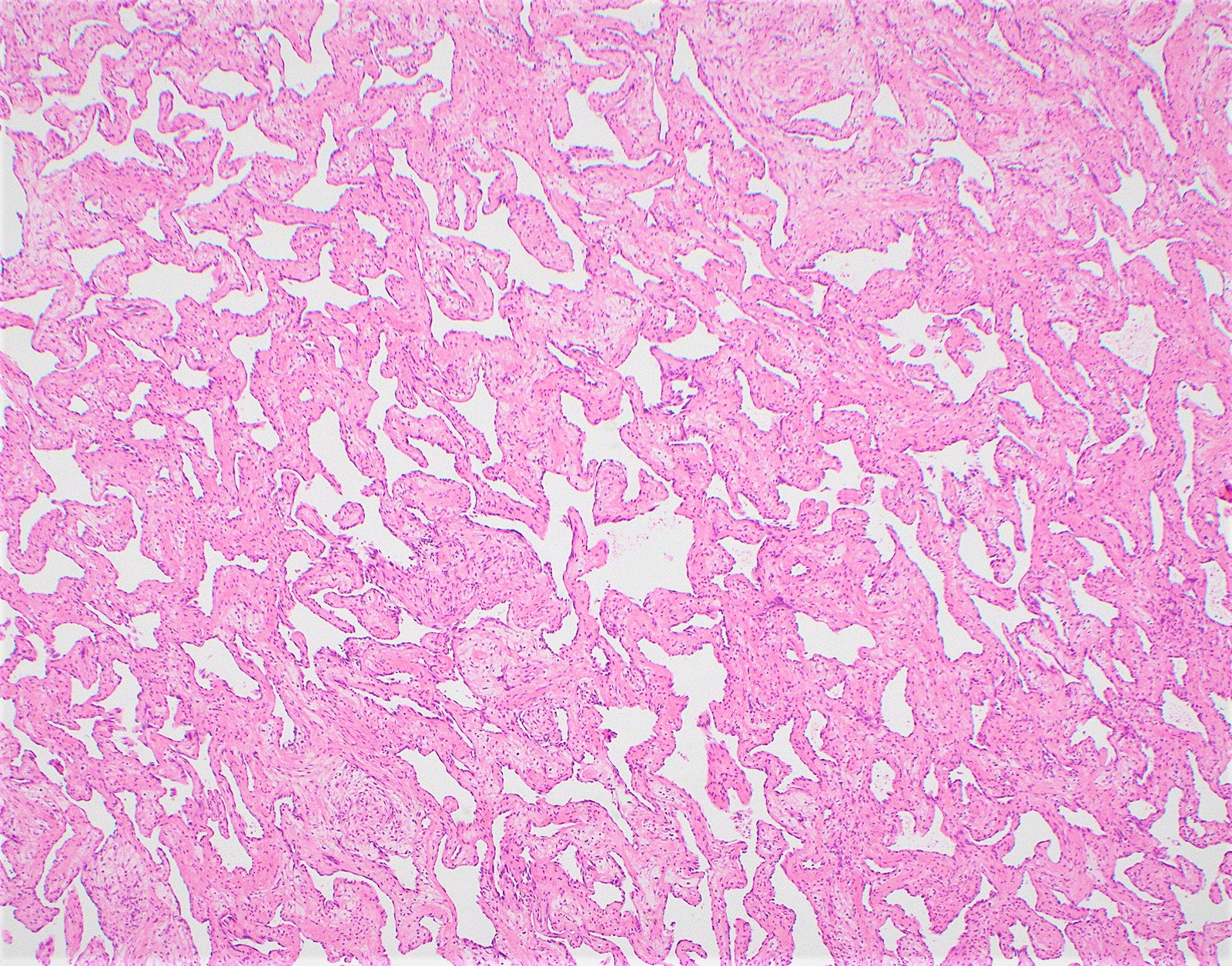
Microscopic (histologic) description
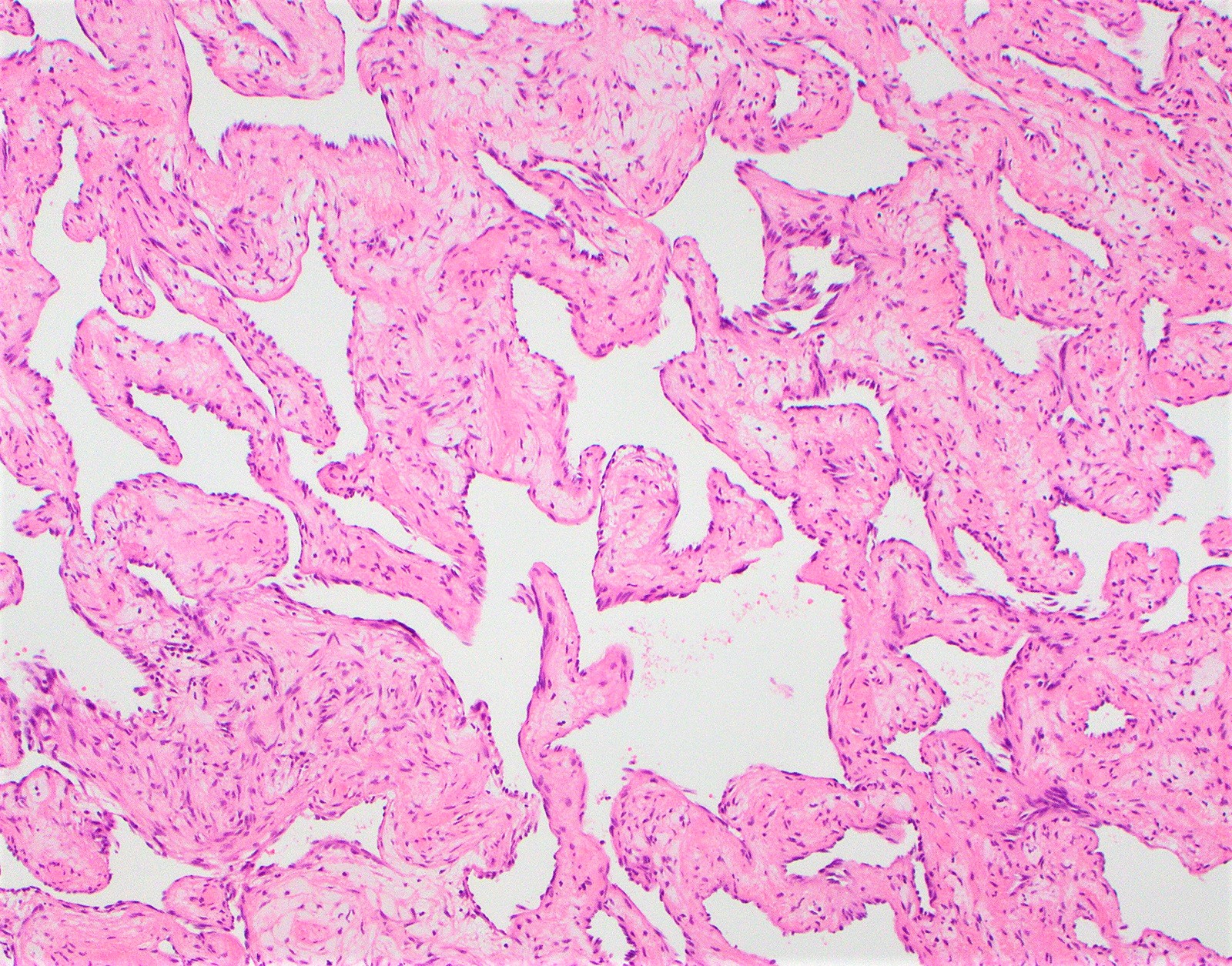
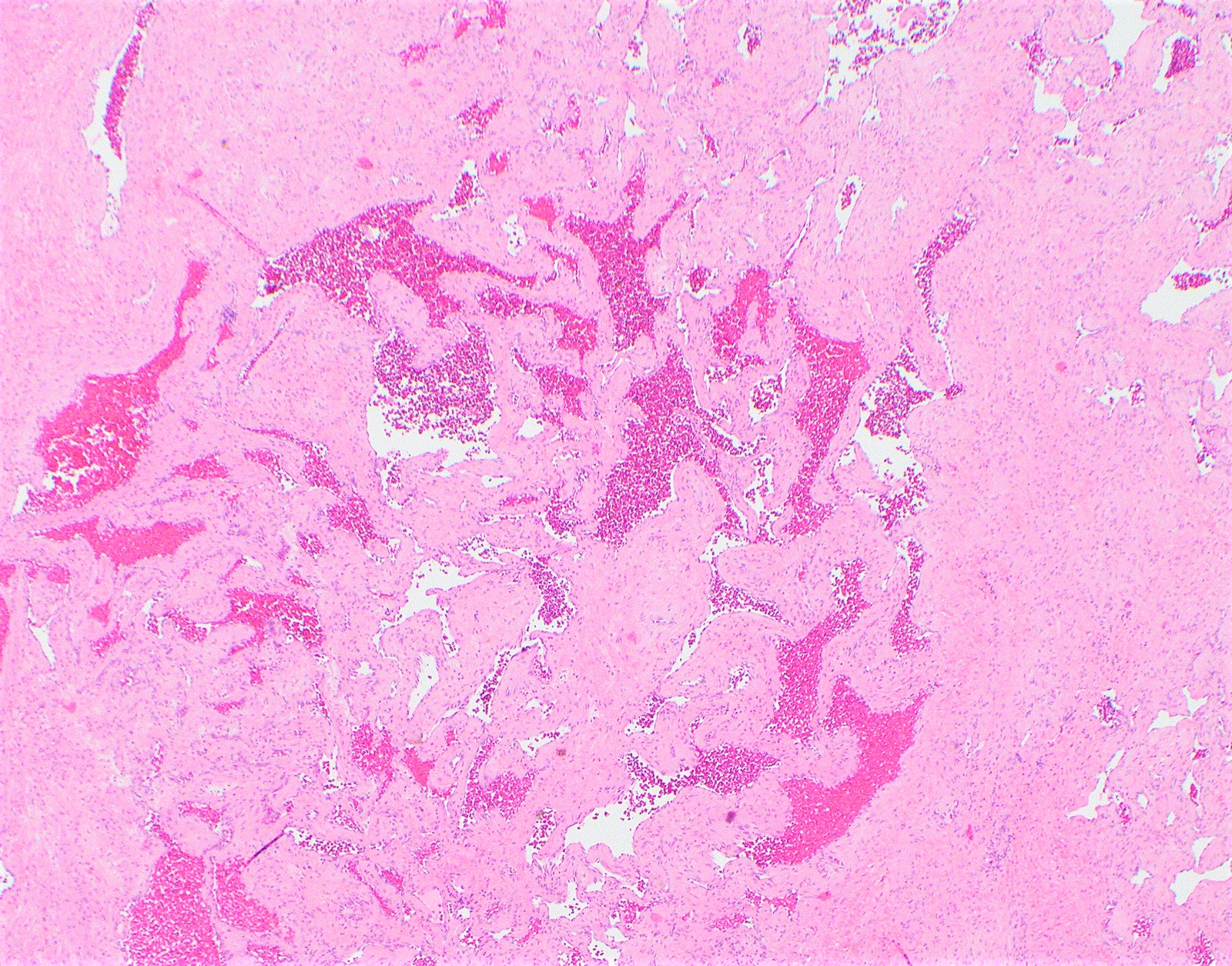
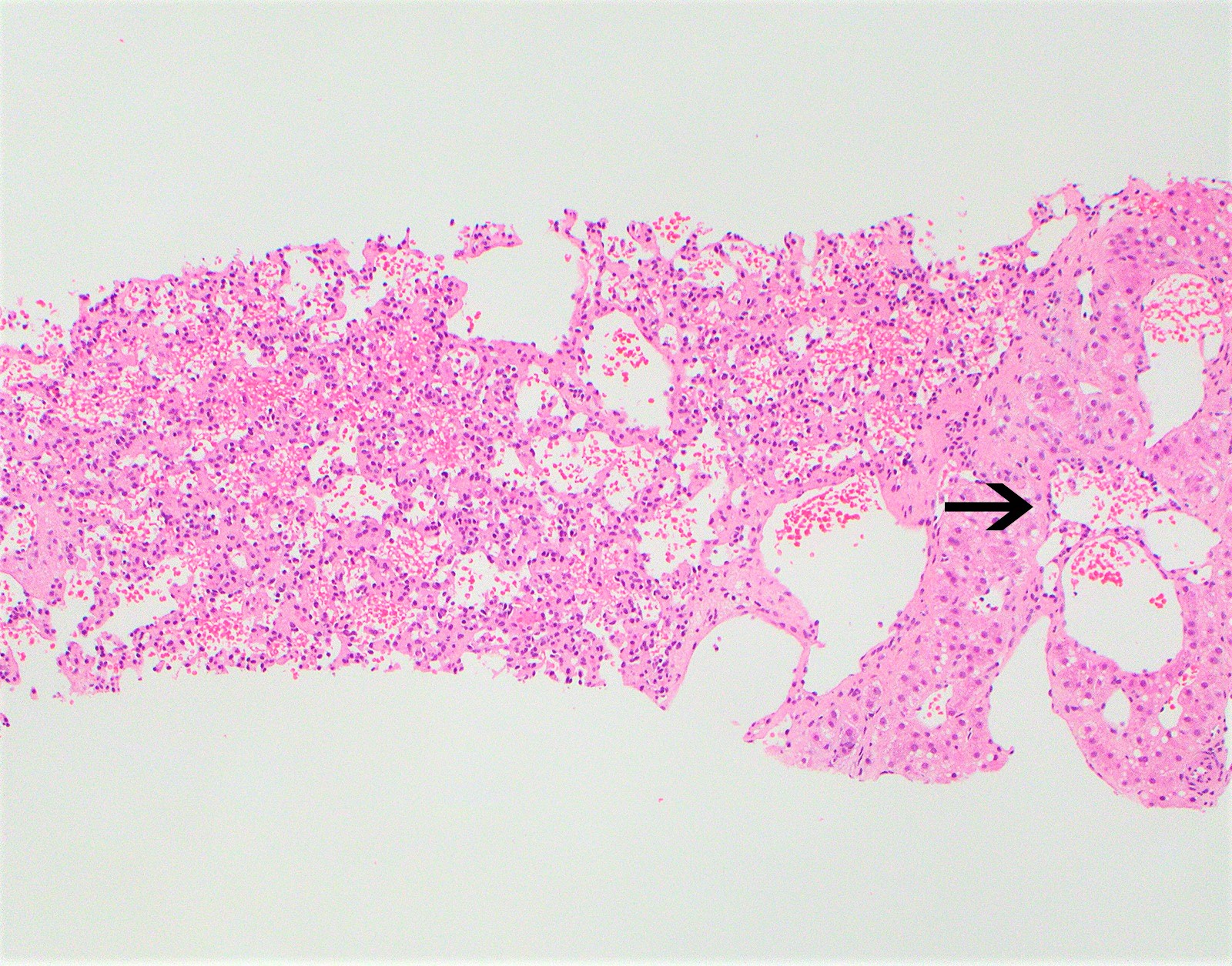
- Cavernous hemangioma
- Circumscribed proliferation of variably sized, dilated and thin walled vessels lined by a single layer of flat endothelial cells
- No cytologic atypia or mitosis
- Vascular spaces separated by fibrous septa containing small vessels
- Focal thrombi, calcification, hyalinization, extramedullary hematopoiesis and stromal edema may be present
- May have irregular interface with surrounding hepatic parenchyma
- Sclerosing / sclerosed hemangioma
- Abundant fibrotic stroma that compresses and replaces lesional vessels
- Only vague outline of residual vessels may be present; elastin or trichrome may aid in highlighting such vessels
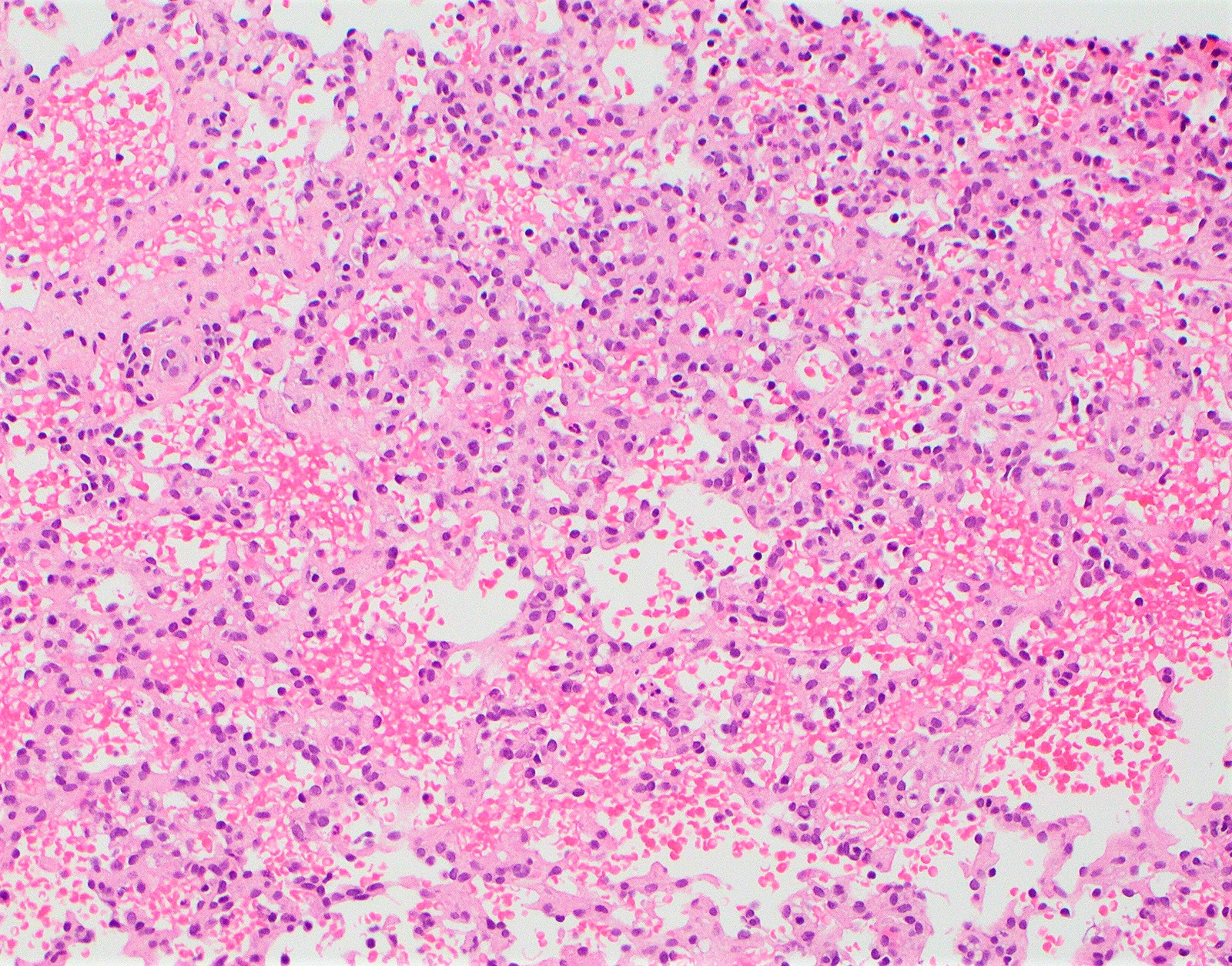
- Capillary hemangioma
- Lobular proliferation of small, thin walled vessels lined by a single layer of bland endothelial cells
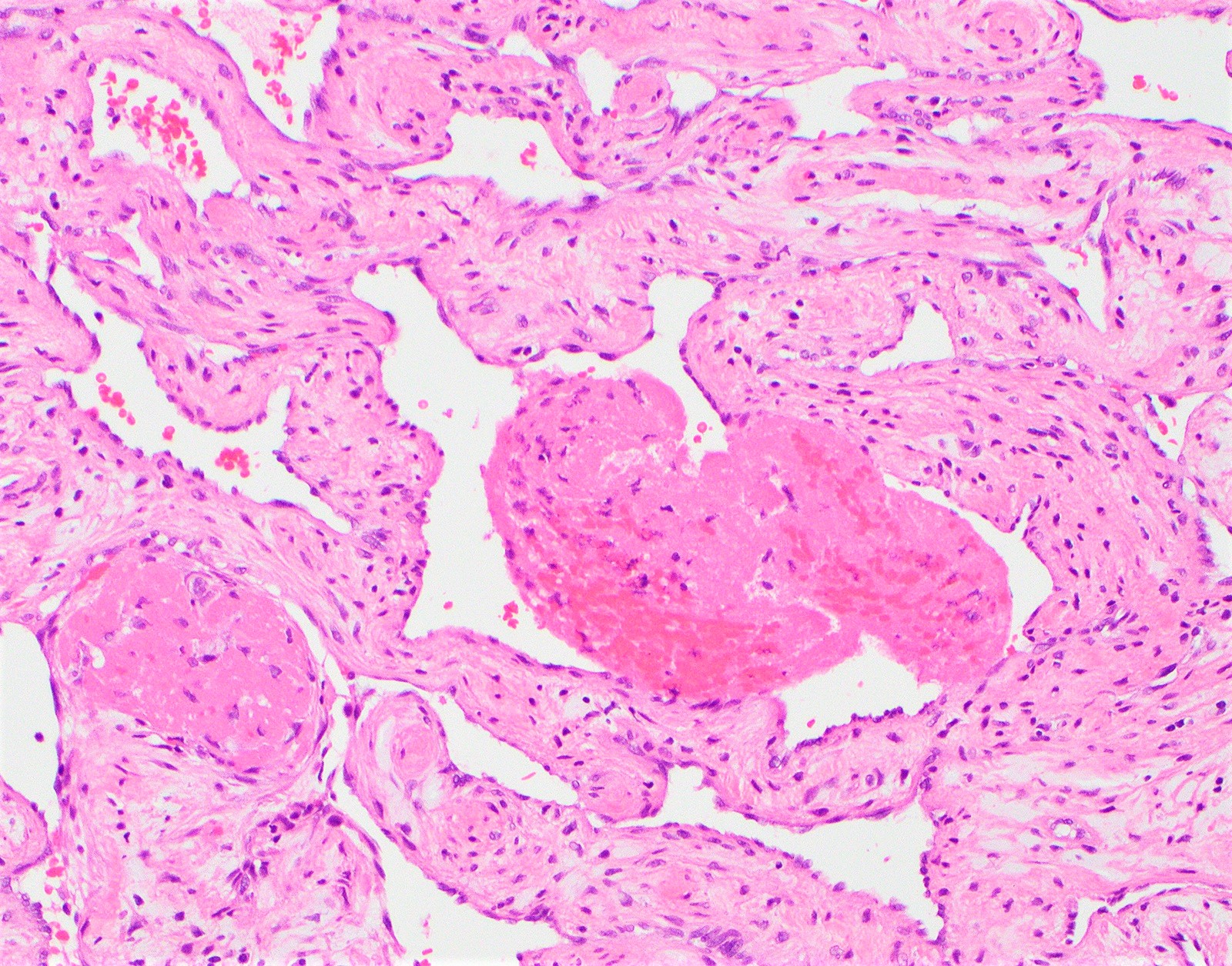
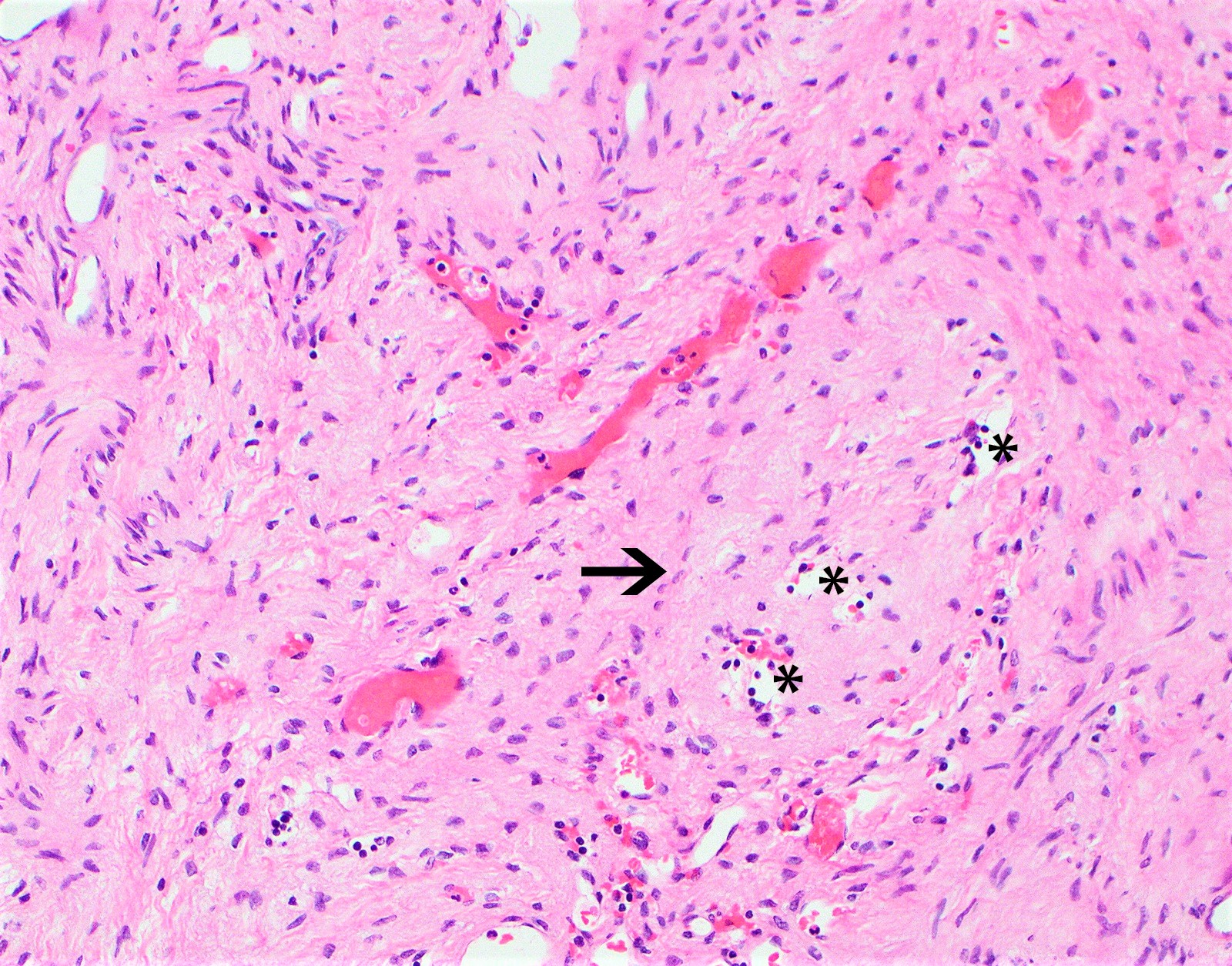
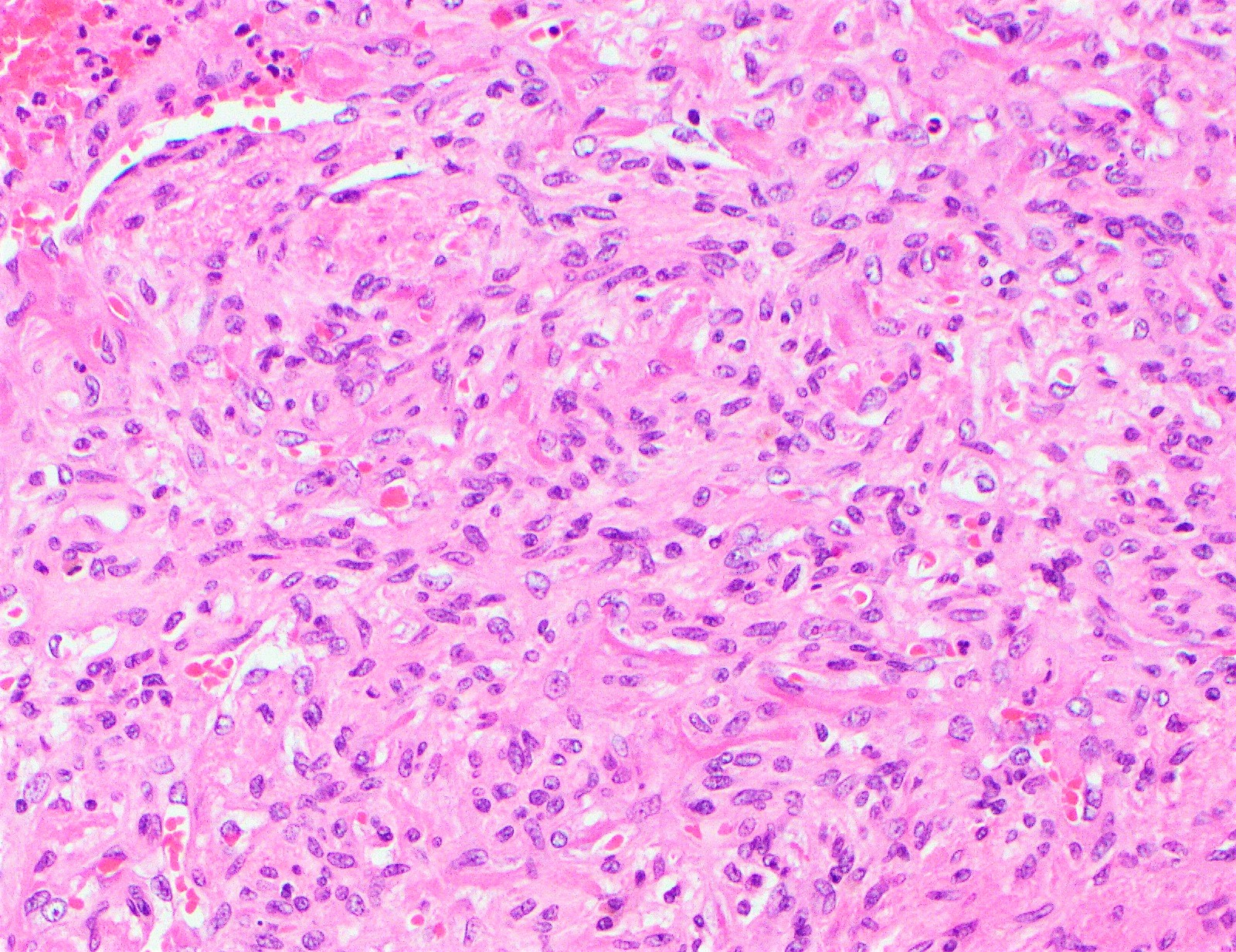
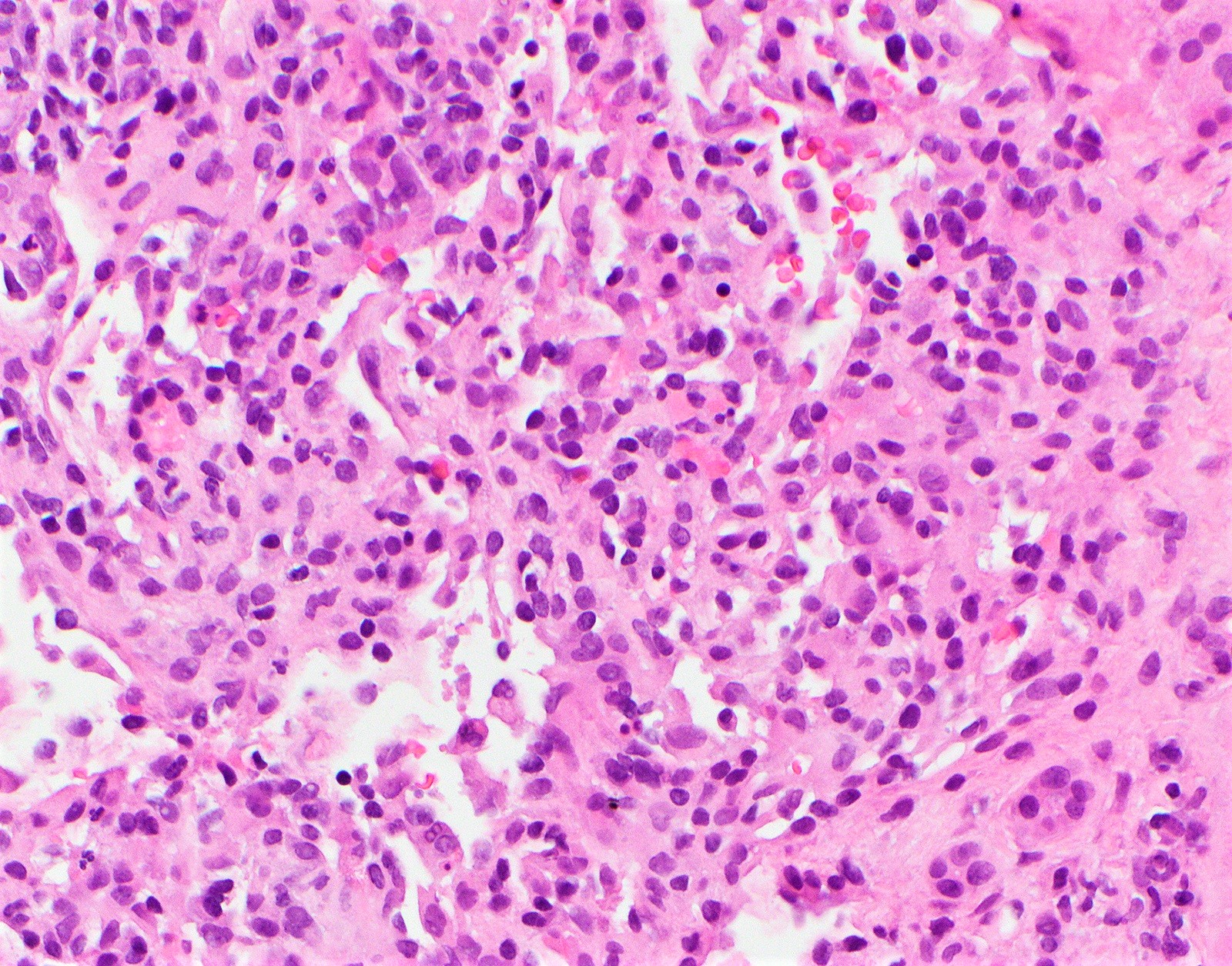
- Anastomosing hemangioma
- Overall well circumscribed; anastomosing, small, capillary-like vessels lined by endothelium with mild cytologic atypia and focal hobnailing
- Thrombi are frequent
- Hyaline globules and extramedullary hematopoiesis may be present
- May resemble angiosarcoma but lacks infiltrative growth, severe cytologic atypia or mitotic activity
- Hepatic small vessel neoplasm
- Similar to anastomosing hemangioma but with infiltrative proliferation of small, thin walled vessels around portal tracts and into adjacent liver parenchyma
- Lined by flattened to plumped or hobnailed endothelial cells
- Extramedullary hematopoiesis may be present
- Lack of multilayering, papillary architecture, significant cytologic atypia, mitotic activity and necrosis
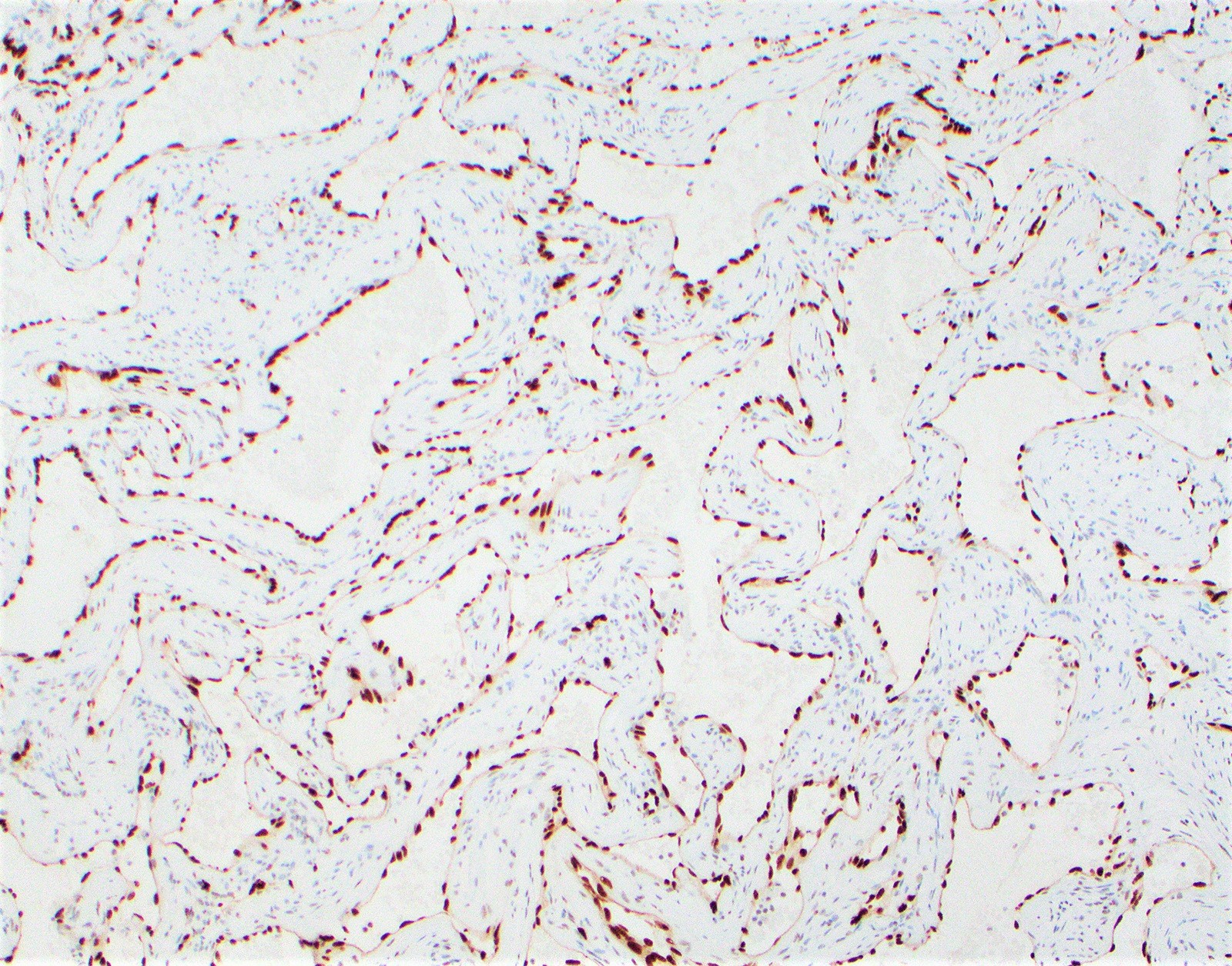
- Ki67 proliferation index most helpful tool in distinguishing from angiosarcoma (Hum Pathol 2016;54:143)
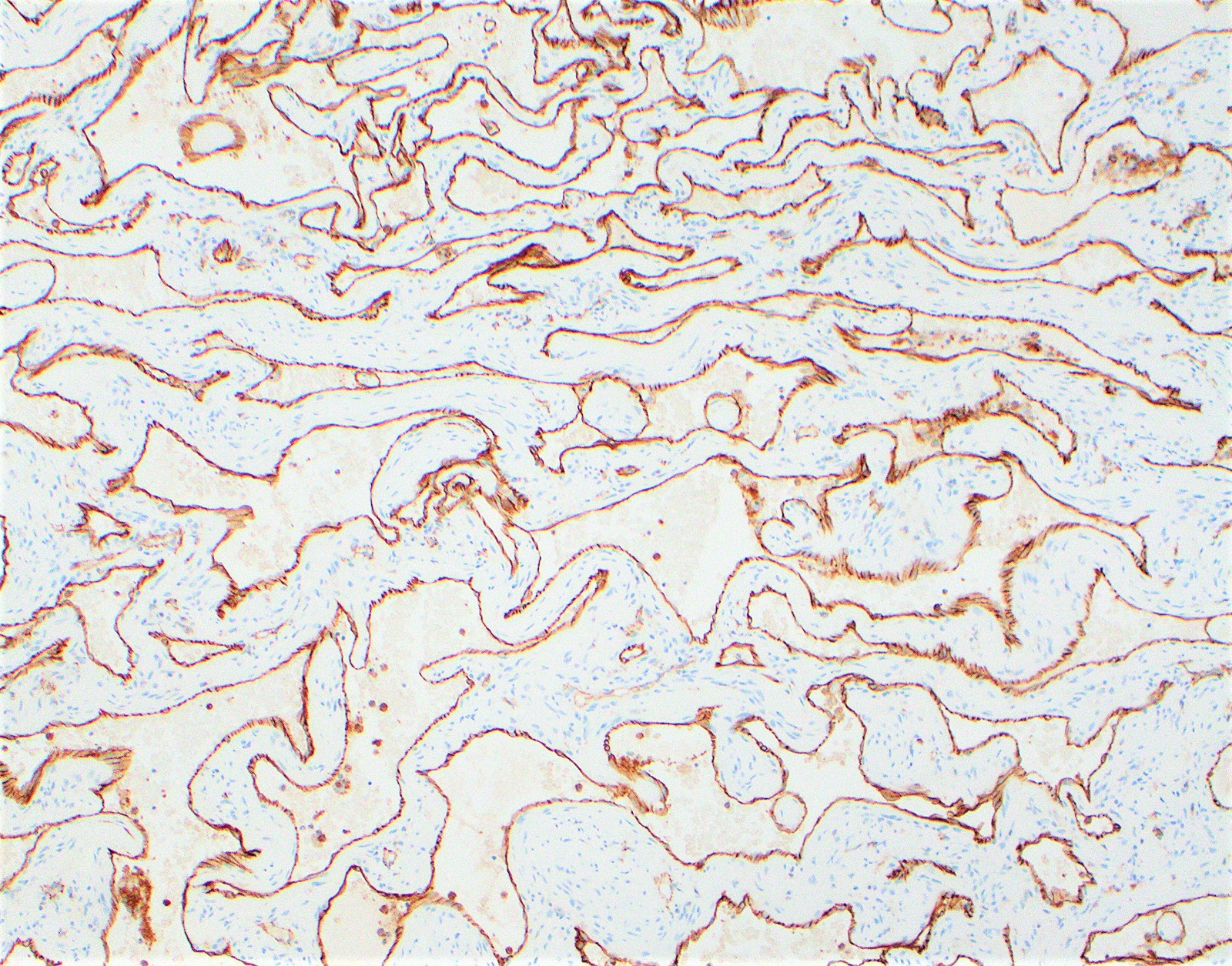
Microscopic (histologic) images
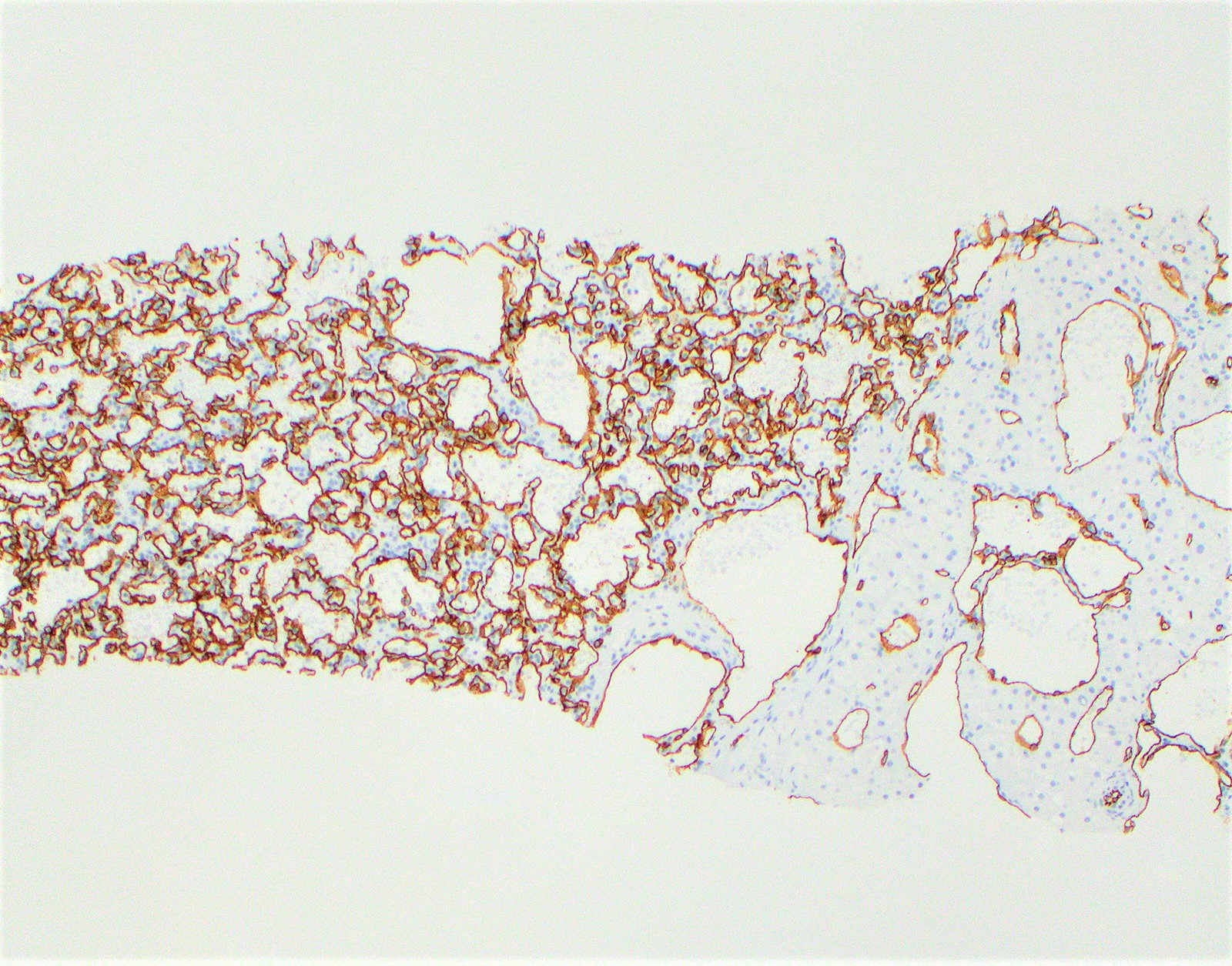
Positive stains
- Endothelial markers: CD31, CD34, ERG, FLI1, Factor VIII are strongly and uniformly positive
- Elastin and trichrome useful in highlighting lesional vessels in sclerosing hemangioma
- Ki67 proliferation index is most helpful tool in distinguishing hepatic small vessel neoplasm from angiosarcoma
- Mean nuclear labeling 3.7% and 42.8% respectively
Negative stains
Molecular / cytogenetics description
- Most hemangiomas have no recurrent genetic abnormalities
- 70 - 90% of anastomosing hemangiomas or hepatic small vessel neoplasms have GNAQ, GNA14 or GNA11 alterations (Am J Surg Pathol 2018;42:1201, Virchows Arch 2020;476:475)
Sample pathology report
- Liver, segment IV, segmentectomy:
- Cavernous hemangioma (3.5 cm in greatest dimension)
Differential diagnosis
- Angiosarcoma:
- Infiltrative with ill defined borders
- Severe cytologic atypia, increased mitotic activity and necrosis
- High Ki67 proliferation index
- No GNAQ, GNA14 or GNA11 alterations
- Juvenile hemangioendothelioma:
- Proliferation of capillary-like vessels with central fibrous scar
- Vessels lined by plump endothelial cells
- Epithelioid hemangioendothelioma:
- Multinodular with ill defined borders
- No vascular channel formation or poorly defined vascular spaces lined by atypical epithelioid cells
- > 90% with recurrent fusion gene WWTR1-CAMTA1 (Genes Chromosomes Cancer 2011;50:644)
- Peliosis hepatis:
- Predominately lakes of blood, no endothelial cell lining
- Hereditary hemorrhagic telangiectasia:
- Dilated vascular channels within portal tracts and surrounding areas
- Aberrant portal vessels present
- Segmental atrophy or nodular elastosis:
- May mimic sclerosing / sclerosed hemangioma
- Variable amount of elastosis and fibrosis with islands of residual hepatocytes, cystic dilated bile ducts and abnormally thick walled vessels (Am J Surg Pathol 2011;35:364)
- No vascular channel formation or residual outlines of vascular channel
Additional references
Board review style question #1
What subtype of hepatic hemangioma is most common?
- Anastomosing
- Capillary
- Cavernous
- Hepatic small cell neoplasm
- Sclerosing / sclerosed
Board review style answer #1
Board review style question #2
A 35 year old woman presents with an incidental 2.5 cm hepatic mass. A representative field from the resection specimen is shown above. The lesional cells are positive for FLI1 and CD34. Which stain would be most useful in distinguishing hepatic small vessel neoplasm from angiosarcoma?
- Cytokeratin
- ER / PR
- Glypican 3
- Ki67
- Podoplanin
Board review style answer #2