Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive staining - disease | Molecular / cytogenetics description | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1Cite this page: Yoshikawa A. Lymphoid interstitial pneumonia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lungnontumorLIP.html. Accessed April 16th, 2024.
Definition / general
- In 1969, Leibow and Carrinton first described lymphoid interstitial pneumonia (LIP) as interstitial lung disease with diffuse and dense lymphocytic infiltration (Simon: Frontiers of Pulmonary Radiology, 1st Edition, 1969)
- In American Thoracic Society / European Respiratory Society classification of the idiopathic interstitial pneumonia, idiopathic LIP is categorized as a rare idiopathic interstitial pneumonia (Am J Respir Crit Care Med 2002;165:277, Am J Respir Crit Care Med 2013;188:733)
Essential features
- Rare type of interstitial lung disease due to different diseases including Sjögren syndrome, rheumatoid arthritis and human immunodeficiency virus (HIV) infection
- On histology, diffuse infiltration of polyclonal lymphocytes with scant interstitial fibrosis is characteristic
Terminology
- Also called lymphocytic interstitial pneumonia
ICD coding
- J84.2: lymphoid interstitial pneumonia
Epidemiology
- Rare
- Typical onset at ages 40 - 70 years old but can occur at any age (Chest 2002;122:2150)
- More common in women
- No association with smoking history
Sites
- Bilateral lower lobes of the lung
Pathophysiology
- Pathogenic mechanisms of LIP are still unclear
- Has aspects of lymphoproliferative disease and lymphoid hyperplasia of polyclonal T or B cells (Chest 2002;122:2150)
- Although it may transform to lymphoma, especially MALT, the risk is lower than initially reported (Eur Respir J 2006;28:364)
Etiology
- Associated with several systemic diseases and conditions (Chest 2002;122:2150,
Respirology 2016;21:600, Eur Respir J 2006;28:364)
- Autoimmune (most common)
- Sjögren syndrome (SjS); 25% of LIP cases have SjS and 1% of SjS cases present with LIP
- Rheumatoid arthritis
- Systemic lupus erythematosus
- Polymyositis / dermatomyositis
- Hashimoto disease
- Hypothyroidism
- Castleman disease
- Myasthenia gravis
- Autoimmune hemolytic anemia
- Pernicious anemia
- Primary biliary cirrhosis
- Infection
- Human immunodeficiency virus (HIV)
- Epstein-Barr virus
- Human T cell lymphotropic virus type 1
- Legionella pneumonia
- Mycoplasma
- Chlamydia
- Tuberculosis
- Immunodeficiency
- Acquired immunodeficiency syndrome (AIDS); especially in children
- Monoclonal or polyclonal gammopathy
- Common variable immunodeficiency
- Idiopathic LIP accounts for 20% of cases (Eur Respir J 2006;28:364)
- Autoimmune (most common)
Clinical features
- Very slowly progressive respiratory symptoms
- Dyspnea on exertion
- Dry cough
- Systemic symptoms such as malaise, fever and weight loss
- Duration of the symptoms prior to diagnosis can exceed a year
- Bibasilar inspiratory crackles on chest auscultation
Diagnosis
- Based on clinical, radiological and pathological findings (multidisciplinary diagnosis)
- No firm diagnostic criteria currently exist
Laboratory
- Dysproteinemia is often present
- Hypergammaglobulinemia is more common than hypogammaglobulinemia
- Restrictive pattern on pulmonary function tests
- Reduced forced vital capacity (FVC)
- Reduced diffusing capacity of the lung for carbon monoxide (DLCO)
Radiology description
- Chest radiography
- Bibasilar opacities with lower lobe predominance
- High resolution computed tomography (Eur J Radiol 2015;84:542,
Respirology 2016;21:600)
- Ground glass opacity with / without consolidation with lower lobe predominance
- Cyst formation and thickening of bronchovascular bundle and interlobular septa are often present
- Cysts often remain even after resolution of symptoms
Radiology images
Prognostic factors
- Prognosis varies from resolution without treatment to progression to end stage (Respirology 2016;21:600)
- Median survival: 11.5 years (Eur Respir J 2006;28:364)
- No characteristic prognostic factor has been found so far
Case reports
- 30 year old woman with LIP related to common variable immunoglobulin deficiency (Intern Med 2008;47:763)
- 35 year old man with HIV related LIP treated with antiretroviral therapy (Int J STD AIDS 2000;11:119)
- 35 year old woman with idiopathic LIP and good response to mycophenolate mofetil (Respir Med Case Rep 2013;9:27)
- 47 year old woman with LIP related to systemic lupus erythematosus and secondary Sjögren syndrome (BMJ Case Rep 2013 Aug 2;2013)
- 52 year old man with HIV related LIP treated with highly active antiretroviral therapy (Sex Transm Infect 2004;80:417)
Treatment
- No treatment data from a controlled study is available so far (Respirology 2016;21:600)
- Corticosteroid therapy is commonly used as a first line treatment and improves the symptoms in most cases
- Immunosuppression (eg, cyclophosphamide, azathioprine, cyclosporine A) may be used as a second line
- Treatment for underlying disease is also essential for secondary LIP
- Antiretroviral therapy can resolve HIV related LIP and its symptoms (Int J STD AIDS 2000;11:119, Sex Transm Infect 2004;80:417)
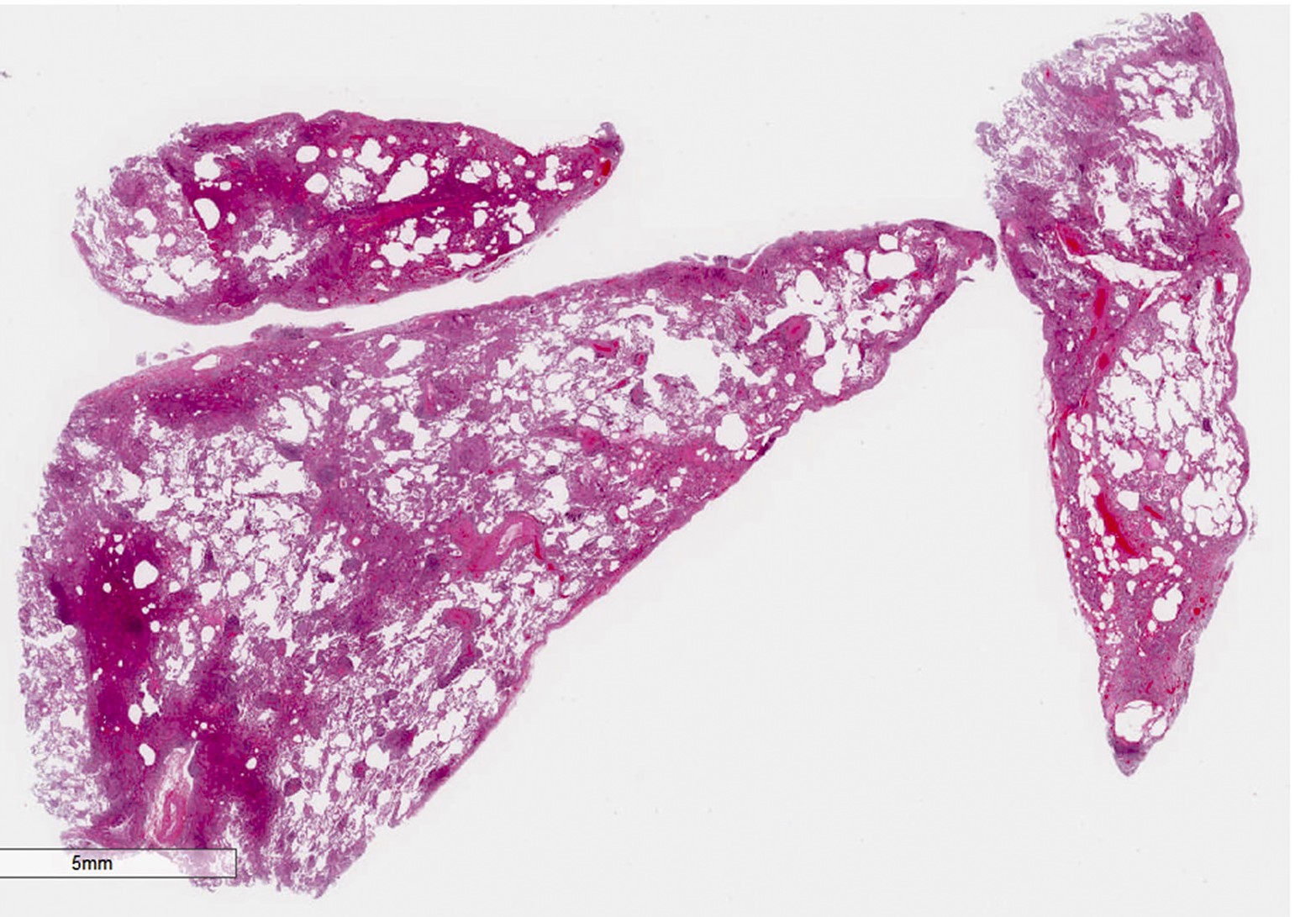
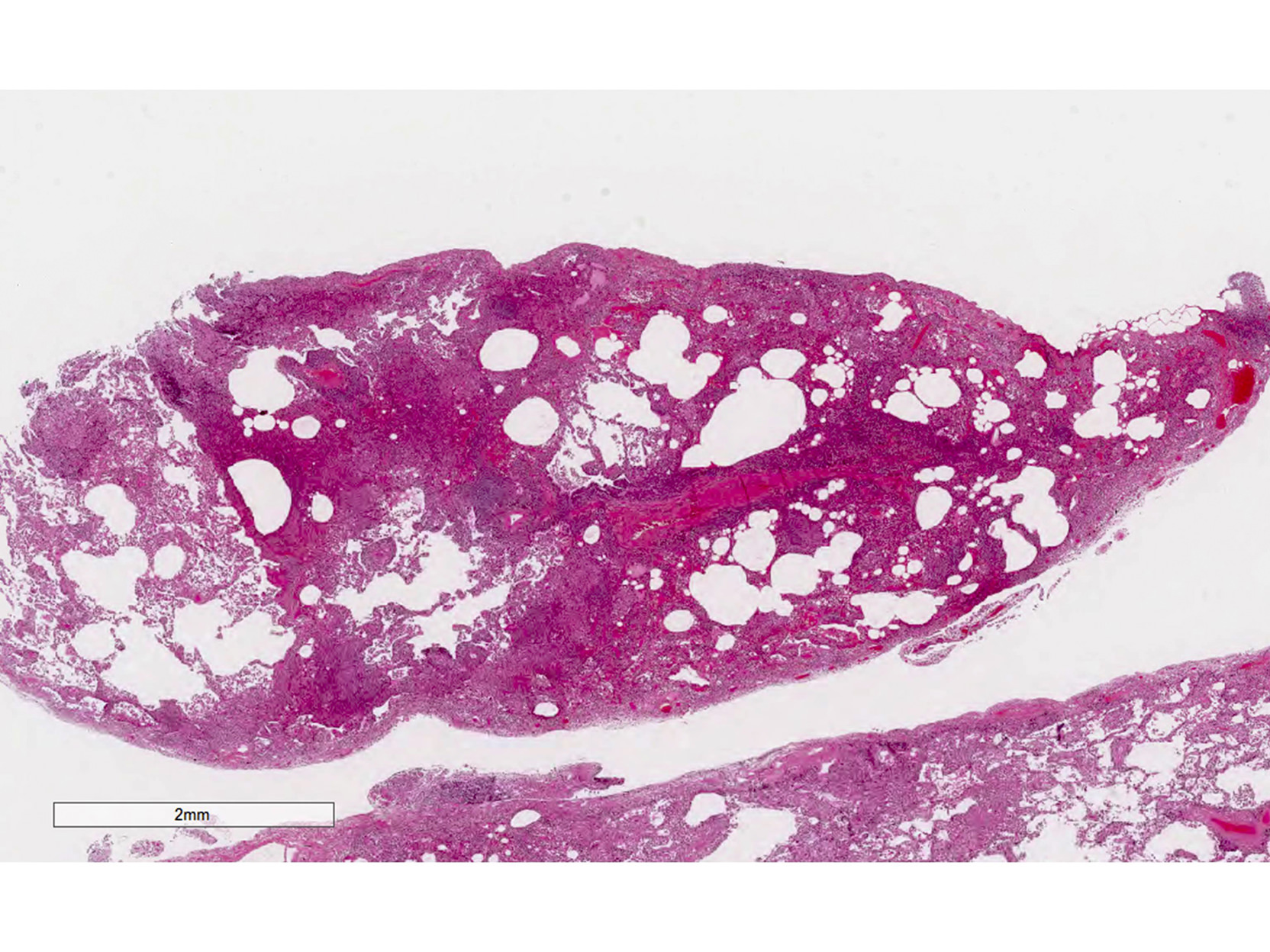
Gross description
- Ill defined lesion
- Mild increase in lung weight
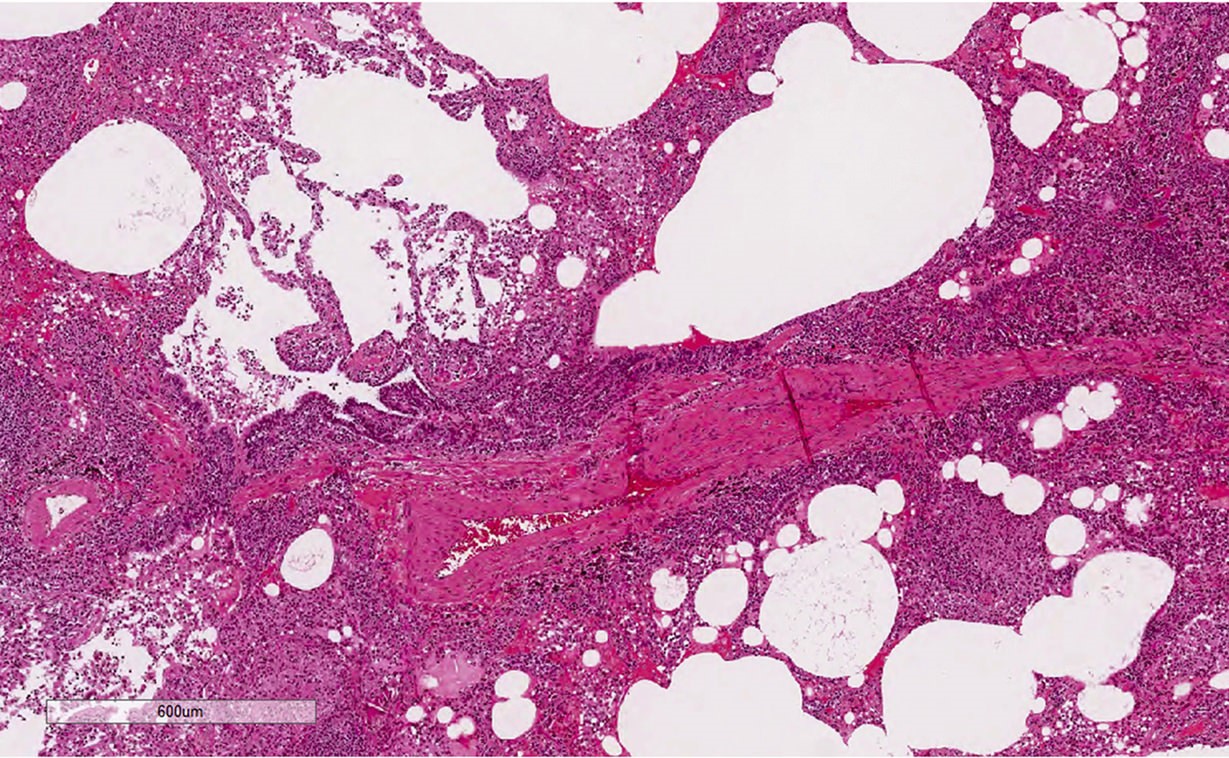
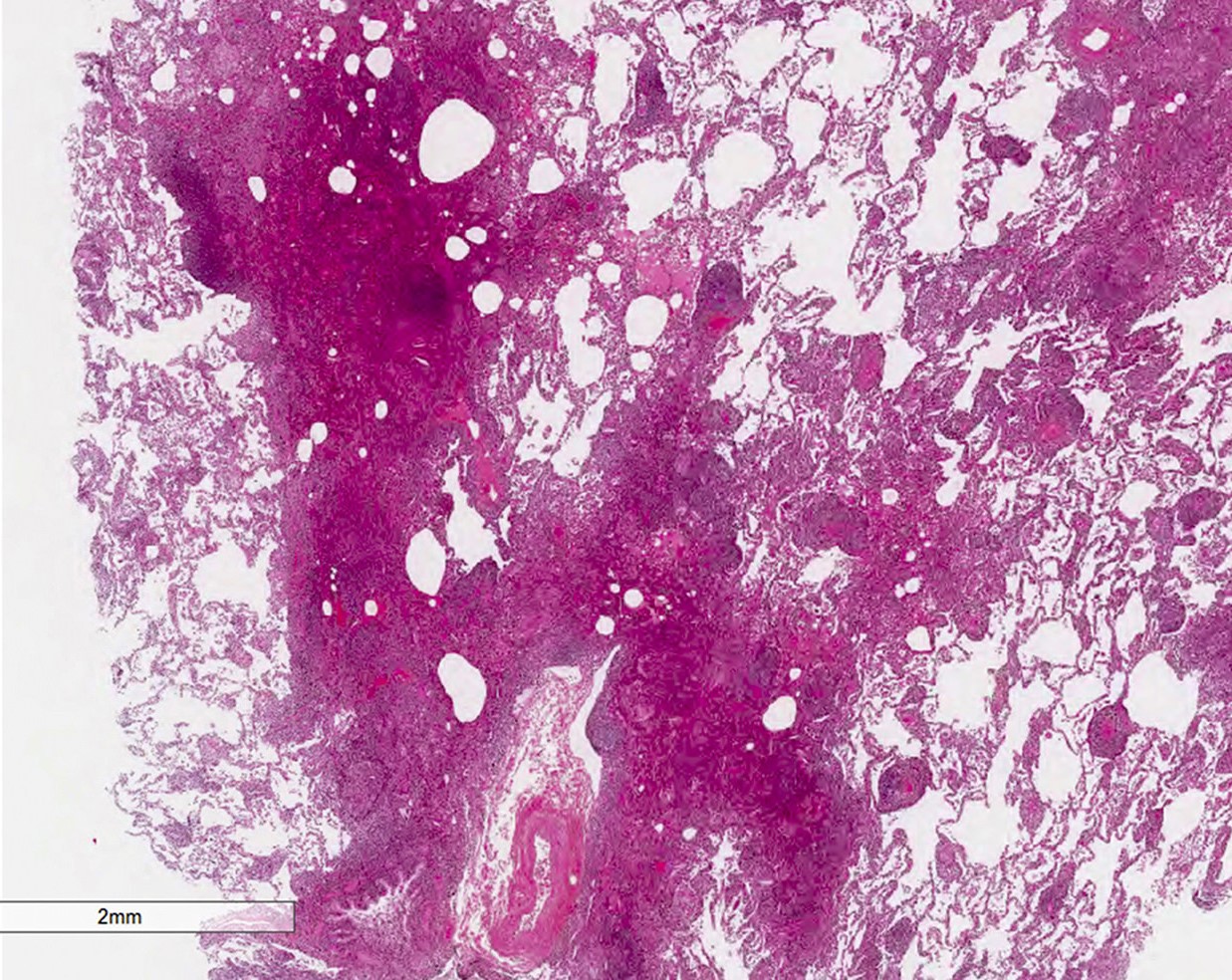
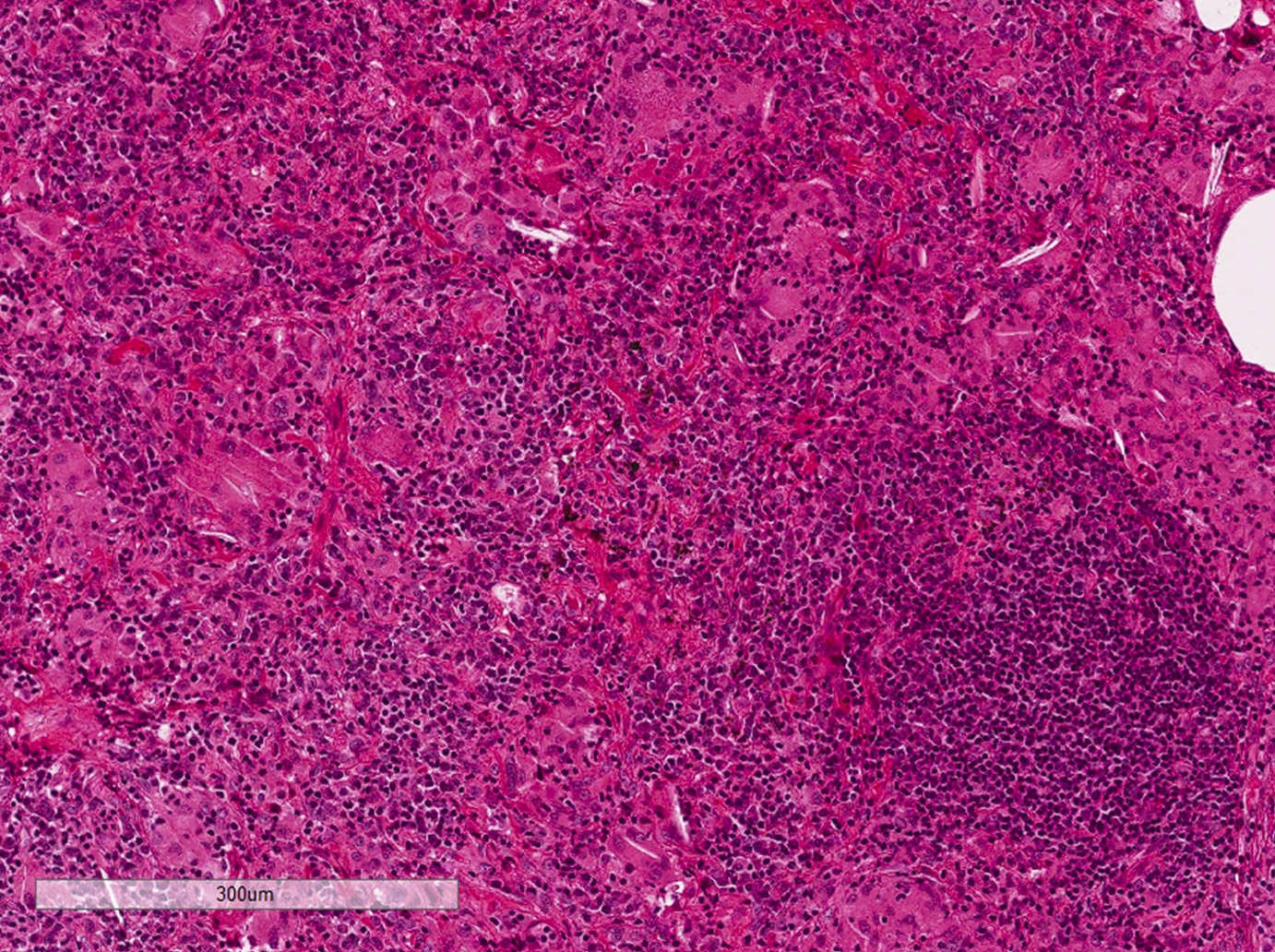
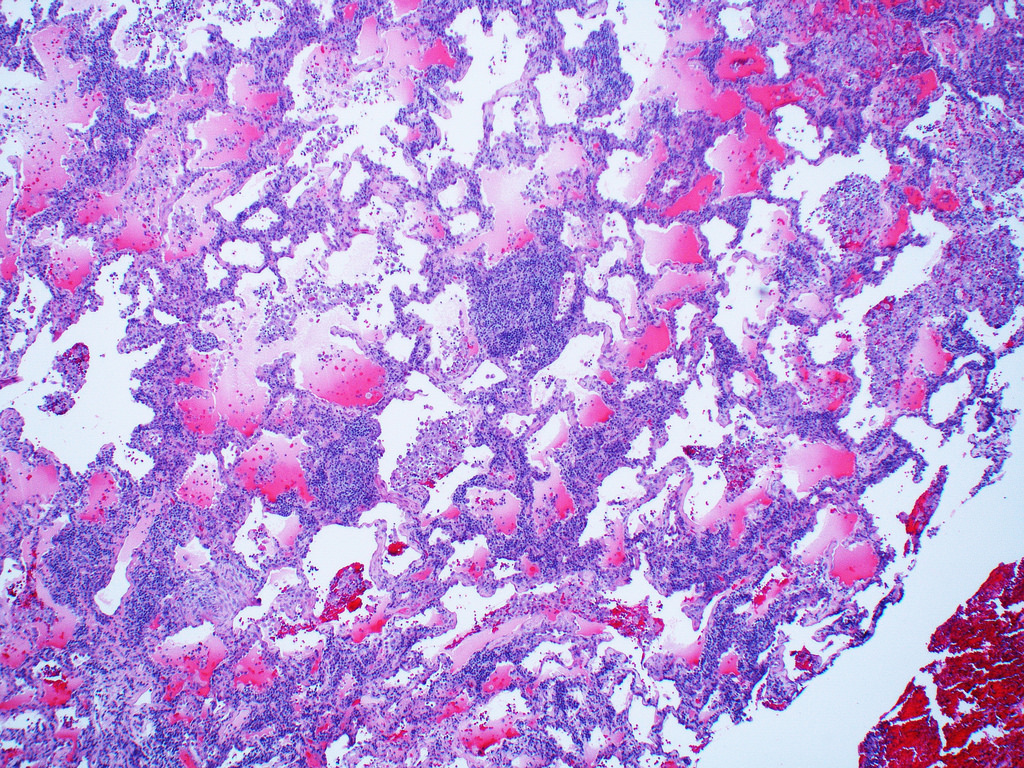
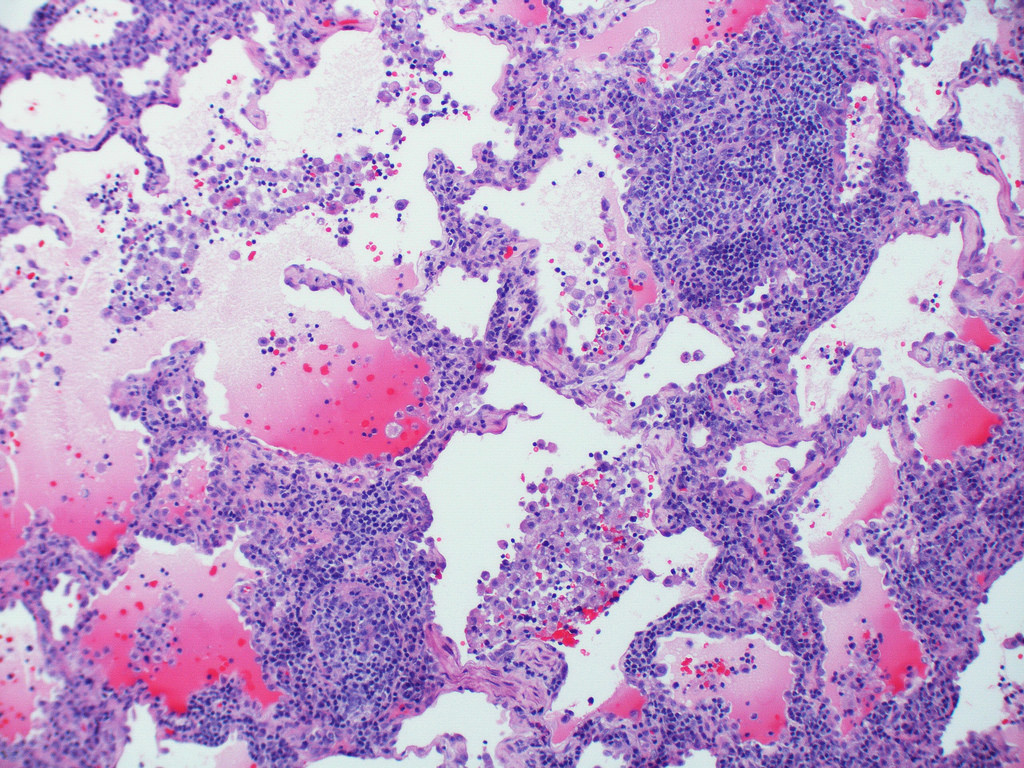
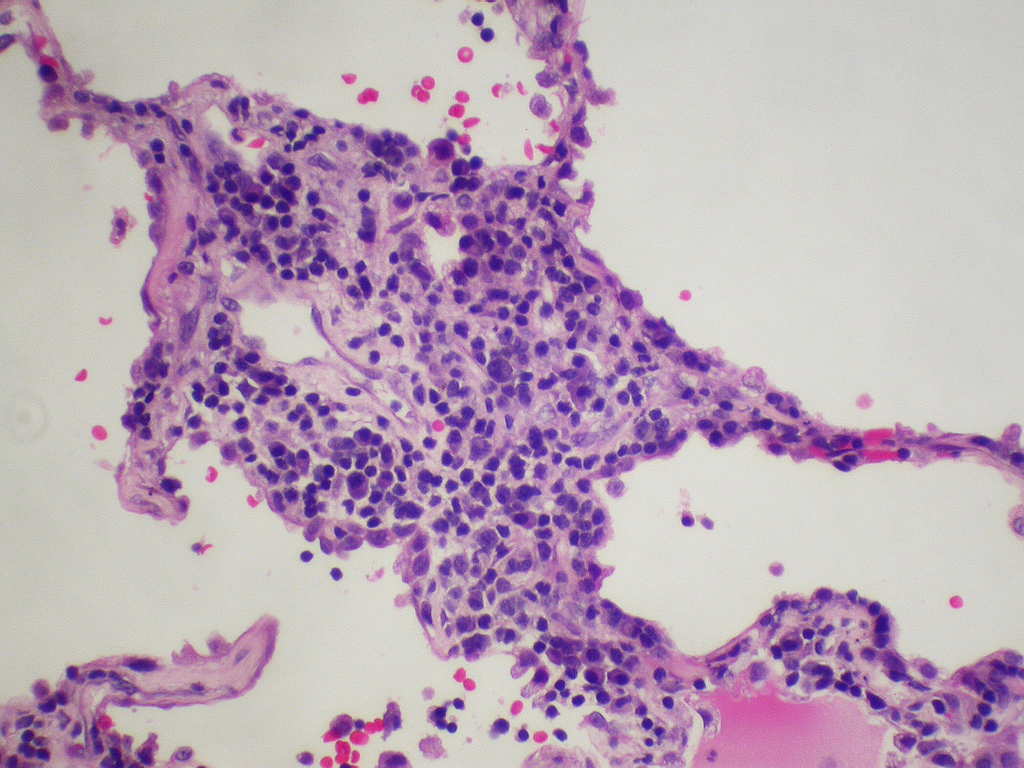
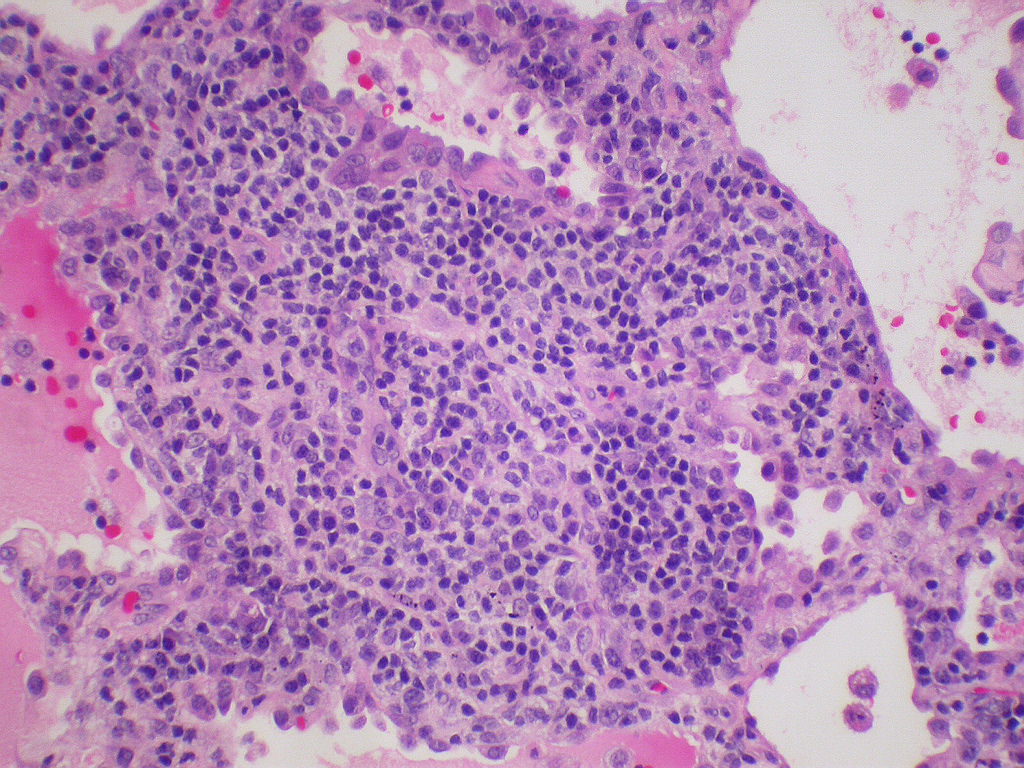
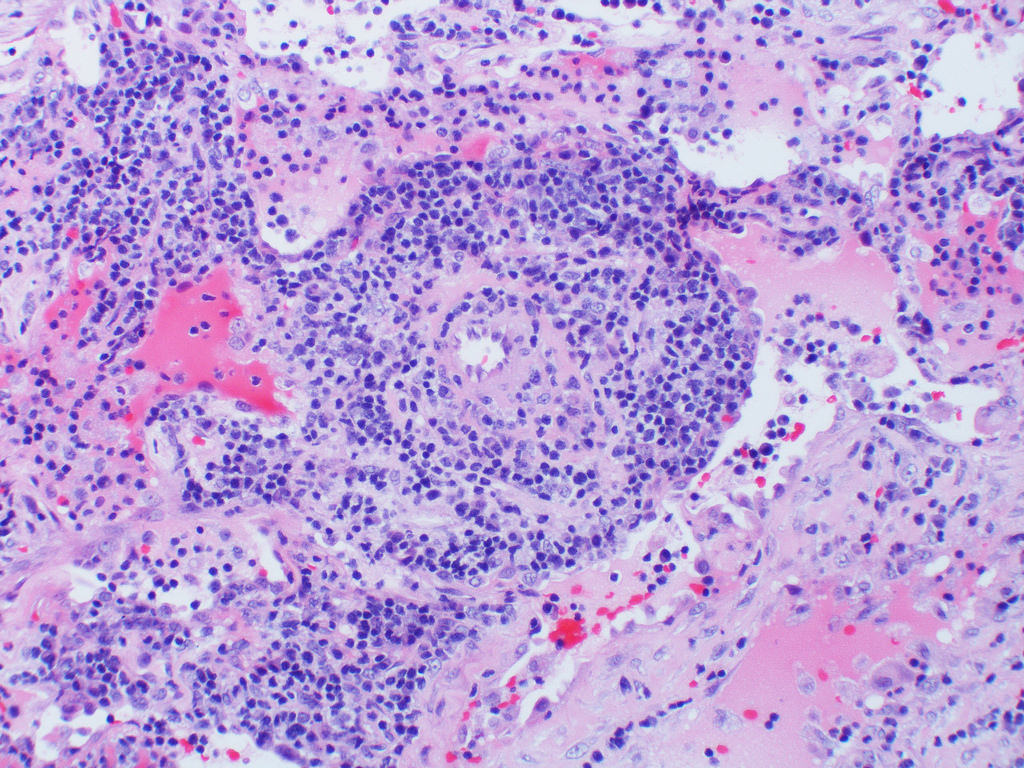
Microscopic (histologic) description
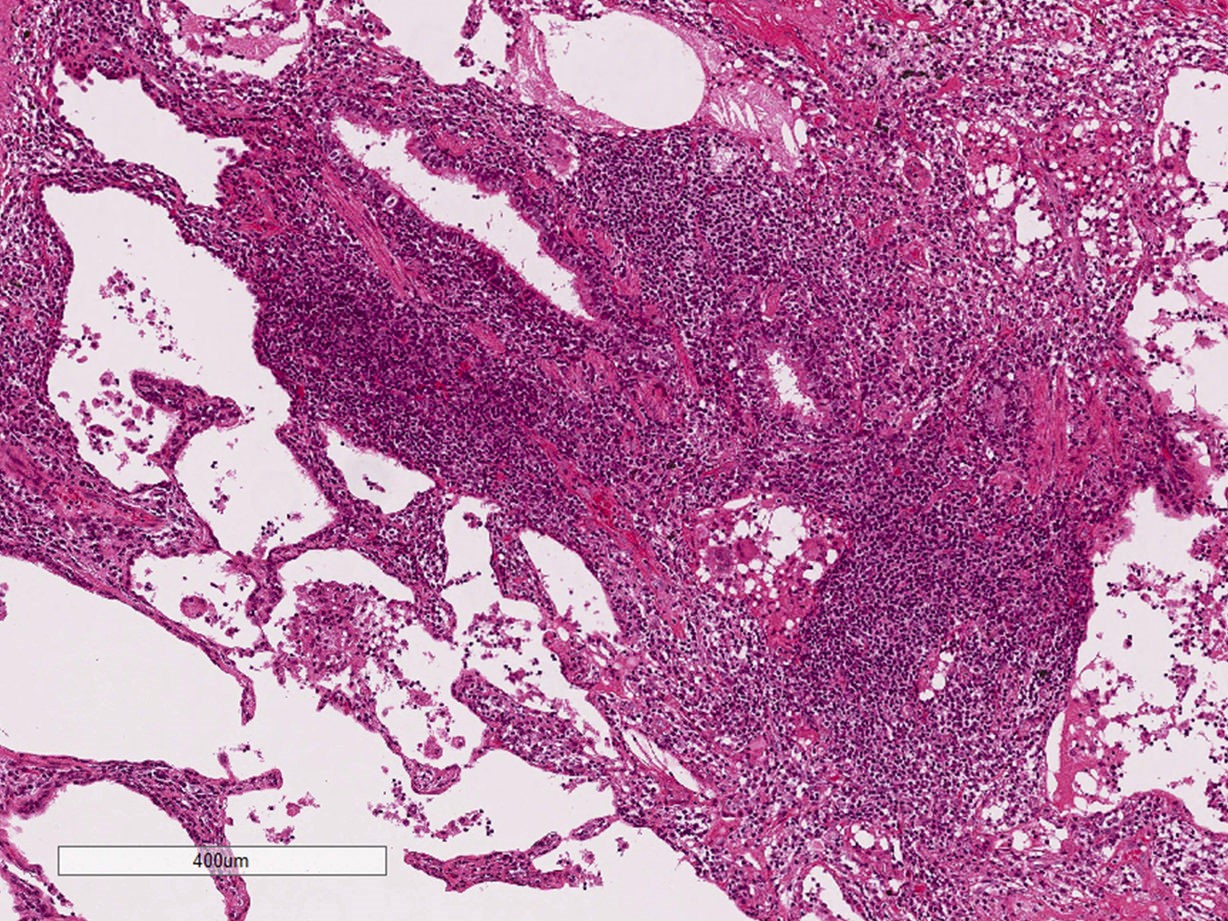
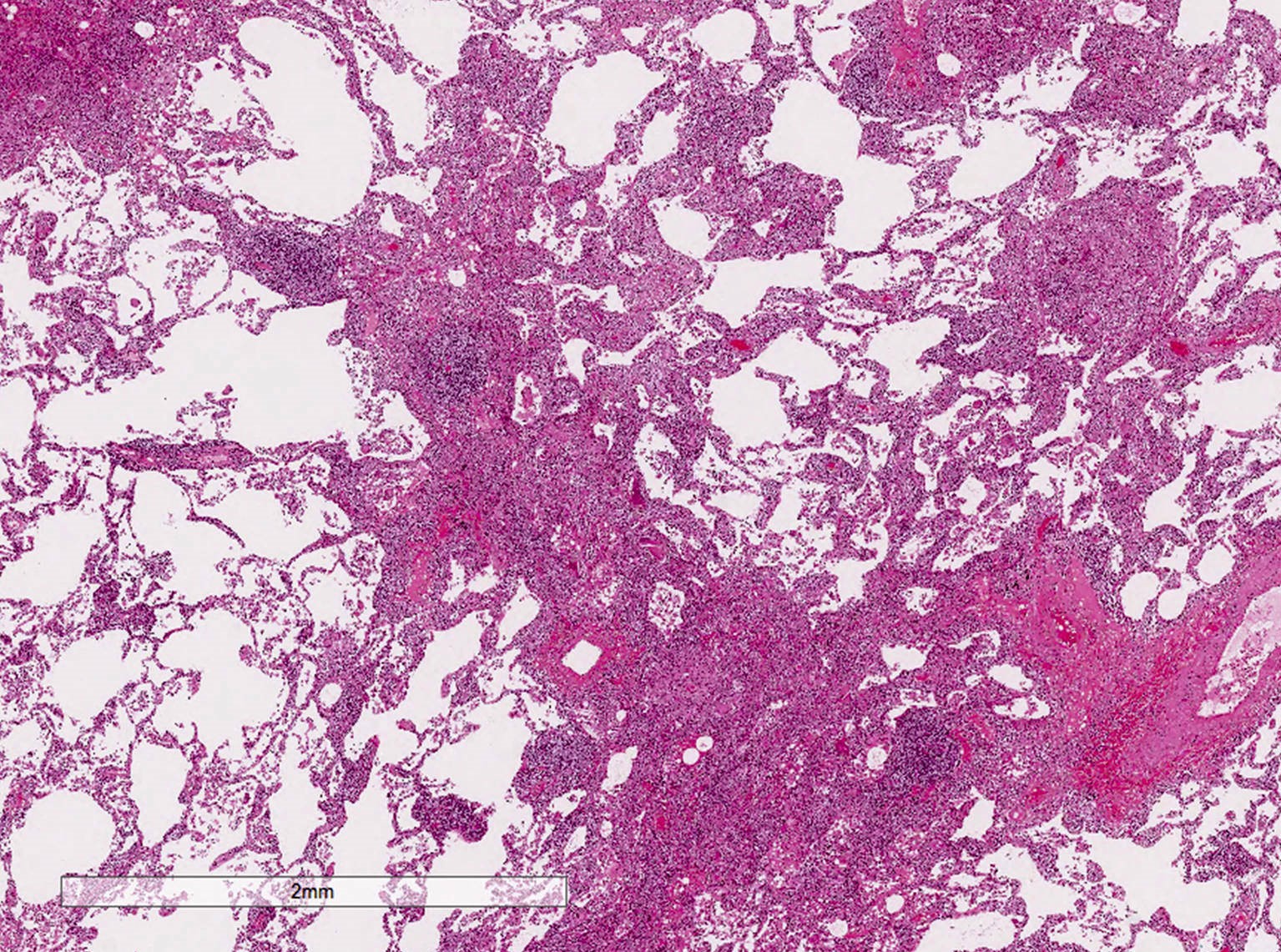
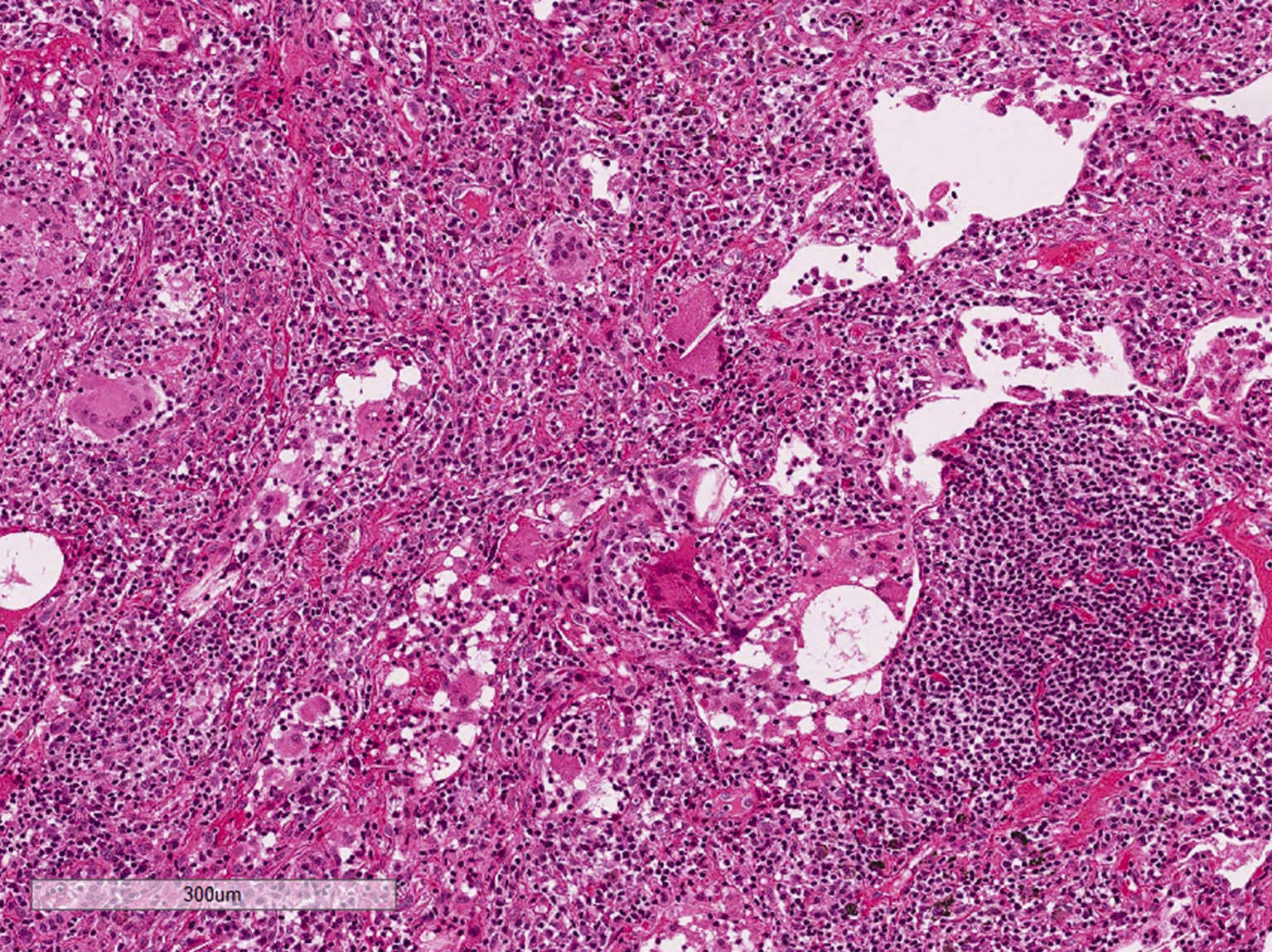
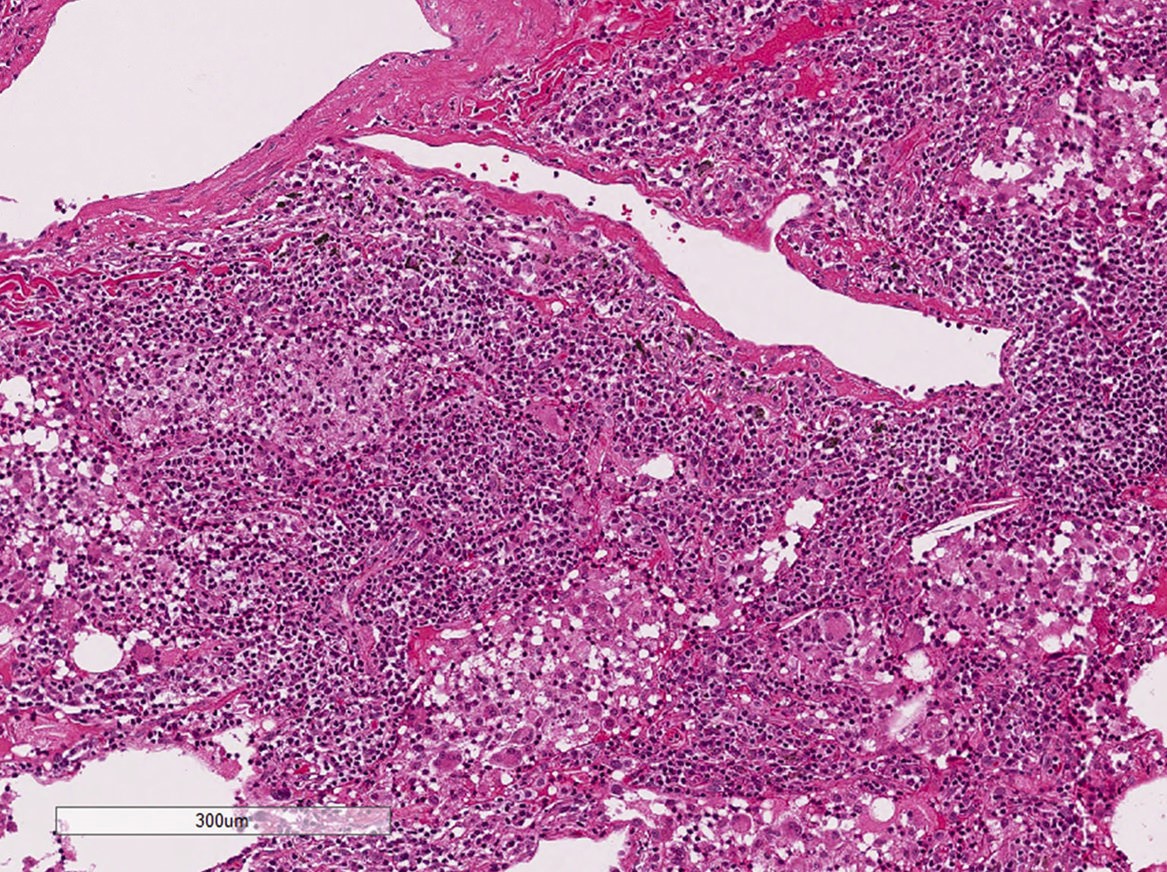
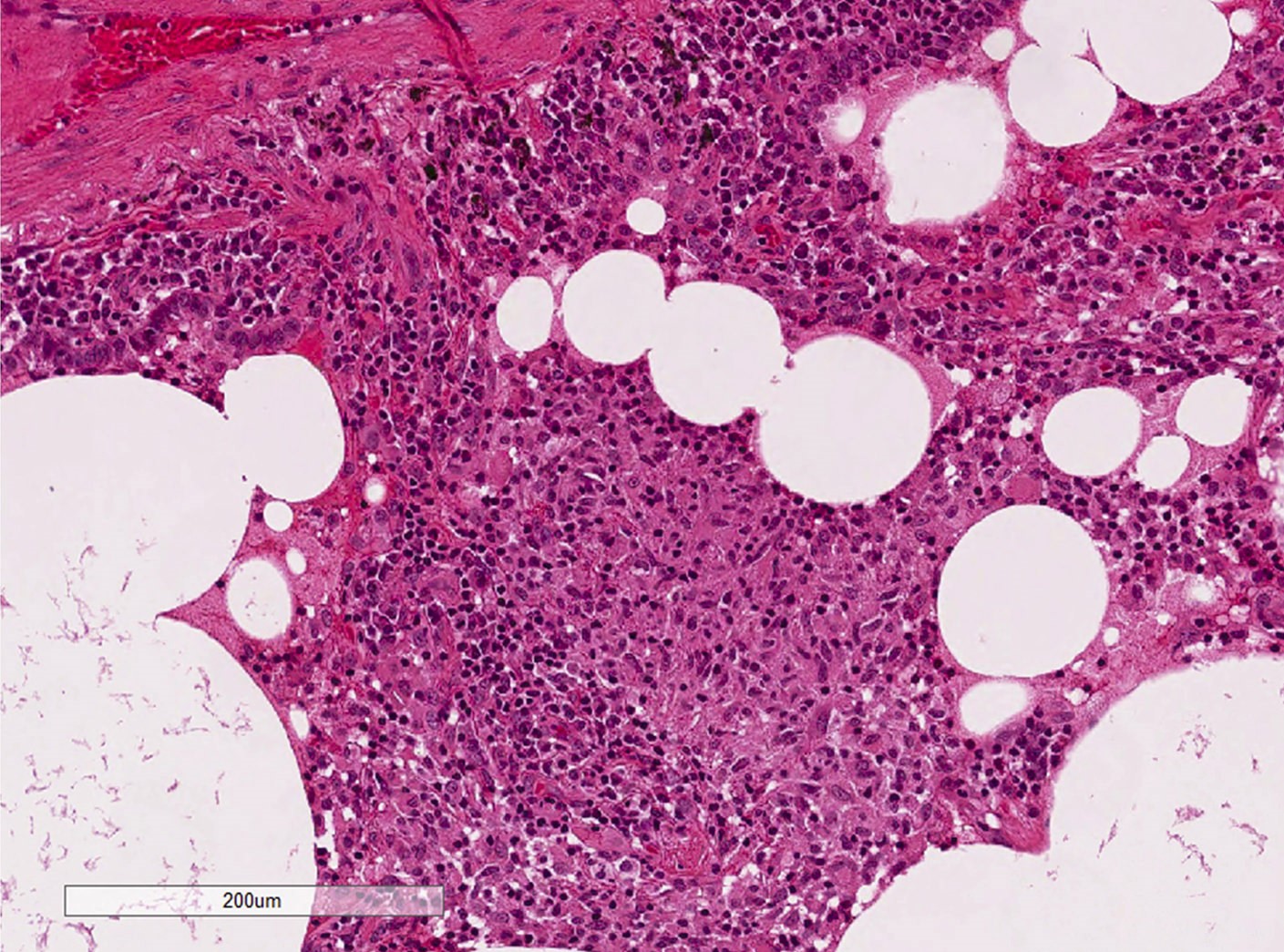
- Diffuse interstitial infiltration of polymorphous lymphocytes and plasma cells
- Lymphoid follicles with germinal centers, histiocytes and macrophages are often present
- Bronchovascular bundles and interlobular septa are usually involved
- Alveolar structure is often inflated and disrupted
- Typically CD8+ or CD4+ T cells or B cells predominate, with an admixture of other lymphocytes
- Immunohistochemistry or molecular testing are necessary to confirm polyclonality
- Additional findings
- Loose ill defined epithelioid granulomas
- Interstitial or intra-alveolar giant cells
- Intra-alveolar macrophages
- Type II pneumocyte hyperplasia
- Cyst formation without marked fibrosis
- Pertinent negative findings
- Loose and dense fibrosis (more common in fibrotic / cellular nonspecific interstitial pneumonia (NSIP))
- Fibroblastic focus (more common in usual interstitial pneumonia or fibrotic NSIP)
- Honeycomb change (more common in usual interstitial pneumonia or fibrotic NSIP)
- Organizing pneumonia (more common in hypersensitivity pneumonitis)
- See: Respirology 2016;21:600, Chest 2002;122:2150, Am J Respir Crit Care Med 2002;165:277
Microscopic (histologic) images
Contributed by Akira Yoshikawa M.D. and Yale Rosen, M.D.
Images hosted on other servers:
Cytology description
- Increase in the number of lymphocytes (especially CD8 positive) of bronchoalveolar lavage, without clonality (Eur Respir J 2006;28:364)
Positive staining - disease
Differential diagnosis
- Follicular bronchitis / bronchiolitis
- Lymphocytic infiltration into bronchial / bronchiolar walls with multiple lymphoid follicles
- No or slight lymphocytic aggregation in intralobular septa
- Hypersensitivity pneumonitis (HP)
- History of an antigen exposure such as animals, birds and chemicals
- Less diffuse but bronchocentric distribution
- Loose ill defined granuloma and giant cells can be seen in both LIP and HP
- Lymphoma, especially mucosa (bronchus) associated lymphoid tissue lymphoma
- Monomorphous infiltration of lymphocytes, distortion of alveolar architecture, Dutcher bodies, pleural infiltration are more common in lymphoma
- Immunohistochemistry is often helpful
- Nonspecific interstitial pneumonia
- Lymphoplasmacytic infiltration is also seen in NSIP but less severe
- Alveolar structure is usually preserved compared with LIP
Additional references
Board review style question #1
Board review style answer #1
C. Honeycomb change. Lymphoid interstitial pneumonia is predominantly a cellular interstitial pneumonia. Fibrotic processes such as dense fibrosis or honeycomb change usually exclude a diagnosis of LIP.
Comment Here
Reference: Lymphoid interstitial pneumonia
Comment Here
Reference: Lymphoid interstitial pneumonia