Table of Contents
Definition / general | Pathophysiology | Clinical features | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Differential diagnosis | Additional referencesCite this page: Weisenberg E. Asthma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lungnontumorasthma.html. Accessed April 25th, 2024.
Definition / general
- Defined by the National Asthma Education and Prevention Program as a "chronic inflammatory disorder of the airways" in which many cells and cellular elements play a role - in particular, mast cells, eosinophils, T lymphocytes, macrophages, neutrophils and epithelial cells
- In susceptible individuals, causes episodes of wheezing, breathlessness, chest tightness and coughing, particularly at night or early morning
- Episodes are usually associated with widespread but variable airflow obstruction that is often reversible, either spontaneously or with treatment
- Inflammation also causes an associated increase in the existing bronchial hyperresponsiveness to a variety of stimuli
- Very common, affects 14 - 15 million Americans
- Causes 3,000 US deaths annually (American Academy of Allergy, Asthma & Immunology)
- Has increased in Western hemisphere over past 40 years
Pathophysiology
- Atopic or Extrinsic: initial sensitization affects T helper 2 cells, which release IL4 / 5, which promote IgE release by B cells, mast cells, and eosinophils
- Re-exposure to allergen leads to mediator release from mucosal mast cells
- Acute / intermediate response is bronchoconstriction, edema, mucus secretion and vasodilation with increased vascular permeability
- Late phase reaction is due to influx of other inflammatory cells stimulated by chemokines released by mast cells, epithelial cells, T lymphocytes and other cytokines; includes release of major basic protein from eosinophils, which causes epithelial damage and airway constriction
- Putative mediators are leukotrienes C4, D4, E4 and acetylcholine; minor mediators are histamine, prostaglandin D2; associated with serum eosinophilia, sputum eosinophils
Clinical features
- Atopic or Extrinsic: Type I hypersensitivity, generally due to allergens; begins in childhood, triggered by environmental allergens (dander, dust, pollen, food), often positive family history; more common in African American children; evidence of allergen sensitization; skin test causes wheel and flare reaction (CMAJ 2009;181:E181)
- Noneosinophilic ("neutrophilic") asthma: a subgroup of atopic asthma not associated with eosinophilia; IL8 recruiting neutrophils are an important mechanism; patients tend to be less responsive to corticosteroids (Thorax 2011;66:942)
- Nonatopic or Intrinsic: nonimmune; due to aspirin ingestion, pneumonia, cold, stress, exercise; follows respiratory infection (rhinovirus, parainfluenza virus); usually not familial; no evidence of allergen sensitization; normal serum IgE, negative skin tests; viral induced inflammation may lower threshold of subepithelial vagal receptors to irritants
- Occupational asthma: due to repeated exposure to fumes, dusts, gases, chemicals, often in minute quantities; varying mechanisms of disease depending upon the stimulus
- Drug induced asthma: associated with several drugs, but most noteworthy is aspirin use; rare, aspirin related cases are associated with recurrent rhinitis, nasal polyps and urticaria; patients are sensitive to small doses of aspirin; may be due to direct effects of aspirin on cyclooxygenase pathway
- Status asthmaticus: unremitting attacks due to exposure to previously sensitized antigen; may be fatal, usually in patients with a long history of asthma
Gross description
- Overdistended lungs, small areas of atelectasis, thick mucus plugs in proximal bronchi containing whorls of shed epithelium
Microscopic (histologic) description
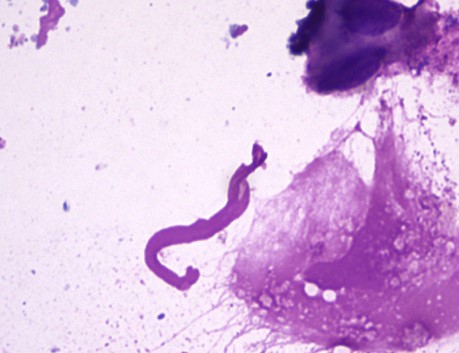
- Curschmann spirals, eosinophils, extracellular Charcot-Leyden crystals (crystalloids composed of galectin-10, an eosinophil lysophopholipase), increased mucosal goblet cells and submucosal glands, thickened basement membrane, bronchial smooth muscle hypertrophy, airway wall edema
Microscopic (histologic) images
Differential diagnosis
- Allergic bronchopulmonary aspergillosis: important complication of asthma and cystic fibrosis
- Bronchocentric granulomatosis without the granulomatous inflammation
Additional references