Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Perry W, Konopka K. Respiratory bronchiolitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lungnontumorrespbronchiolitis.html. Accessed April 24th, 2024.
Definition / general
- Common histologic marker of current or former smoker status
- Usually an incidental pathologic finding but can occasionally be associated with clinically significant interstitial lung disease (respiratory bronchiolitis interstitial lung disease [RB-ILD])
Essential features
- Respiratory bronchiolitis present in virtually all smokers
- Characterized by the accumulation of lightly pigmented (smoker's) macrophages in distal airways and peribronchiolar airspaces with or without mild inflammation and fibrosis in adjacent interstitium
- Diagnosis of respiratory bronchiolitis interstitial lung disease relies on pathologic, clinical and radiographic correlation and is a diagnosis of exclusion
Terminology
- Smoker's bronchiolitis
ICD coding
- ICD-10: J84.115 - respiratory bronchiolitis interstitial lung disease
Epidemiology
- 98% of patients with smoking history have respiratory bronchiolitis (N Engl J Med 1974;291:755, Am J Surg Pathol 2002;26:647)
- Rare cases in nonsmokers related to environmental exposure
- Respiratory bronchiolitis interstitial lung disease accounts for 2% of idiopathic interstitial pneumonias (Am J Respir Crit Care Med 1998;157:199, Chest 2005;127:178)
- M = F
- Mean age: 43 ± 7 years
Sites
- Distal airways of lungs
Pathophysiology
- Unknown at this time
Etiology
- Smoking
Clinical features
- Nearly all patients with respiratory bronchiolitis asymptomatic
- Respiratory bronchiolitis interstitial lung disease patients often symptomatic (Chest 2005;127:178, Chest 2007;131:664)
- 90% dyspnea; 50% cough
- Pulmonary function tests: obstructive or restrictive > normal > mixed patterns
Diagnosis
- Diagnosis of respiratory bronchiolitis interstitial lung disease requires correlating clinical, radiologic and pathologic findings:
- Clinical: patient symptoms, pulmonary function testing
- Radiologic: chest Xray, high resolution computed tomography (HRCT)
- Pathologic: histologic examination of lung wedge biopsy
- Diagnosis of respiratory bronchiolitis interstitial lung disease only applicable after other forms of diffuse lung disease have been ruled out
Radiology description
- Respiratory bronchiolitis without interstitial lung disease: radiologic abnormalities rarely detectable; when present, may consist of poorly defined centrilobular nodules or multifocal ground glass opacities, often more pronounced in the upper lung fields (Radiology 1993;186:107, AJR Am J Roentgenol 1999;173:1617, AJR Am J Roentgenol 1993;161:44)
- Respiratory bronchiolitis interstitial lung disease: radiologic abnormalities often detectable; may include centrilobular nodules, ground glass opacities or thickening of bronchial walls (J Comput Assist Tomogr 2002;26:13, AJR Am J Roentgenol 1999;173:1617, J Comput Assist Tomogr 1993;17:46)
Prognostic factors
- Symptomatic patients usually have stable disease course (Chest 2005;127:178, Chest 2007;131:664)
Case reports
- 11 year old boy with respiratory bronchiolitis interstitial lung disease due to heavy second hand smoke exposure (Pediatrics 2015;136:e1026)
- 33 year old man with respiratory bronchiolitis interstitial lung disease thought to be related to electronic nicotine delivery system (Respirol Case Rep 2017;5:e00230)
- 2 cases of respiratory bronchiolitis interstitial lung disease in men under 50 initially diagnosed with idiopathic pulmonary fibrosis (Chest 2000;117:282)
Treatment
- Smoking cessation
Gross description
- No gross abnormality
Microscopic (histologic) description
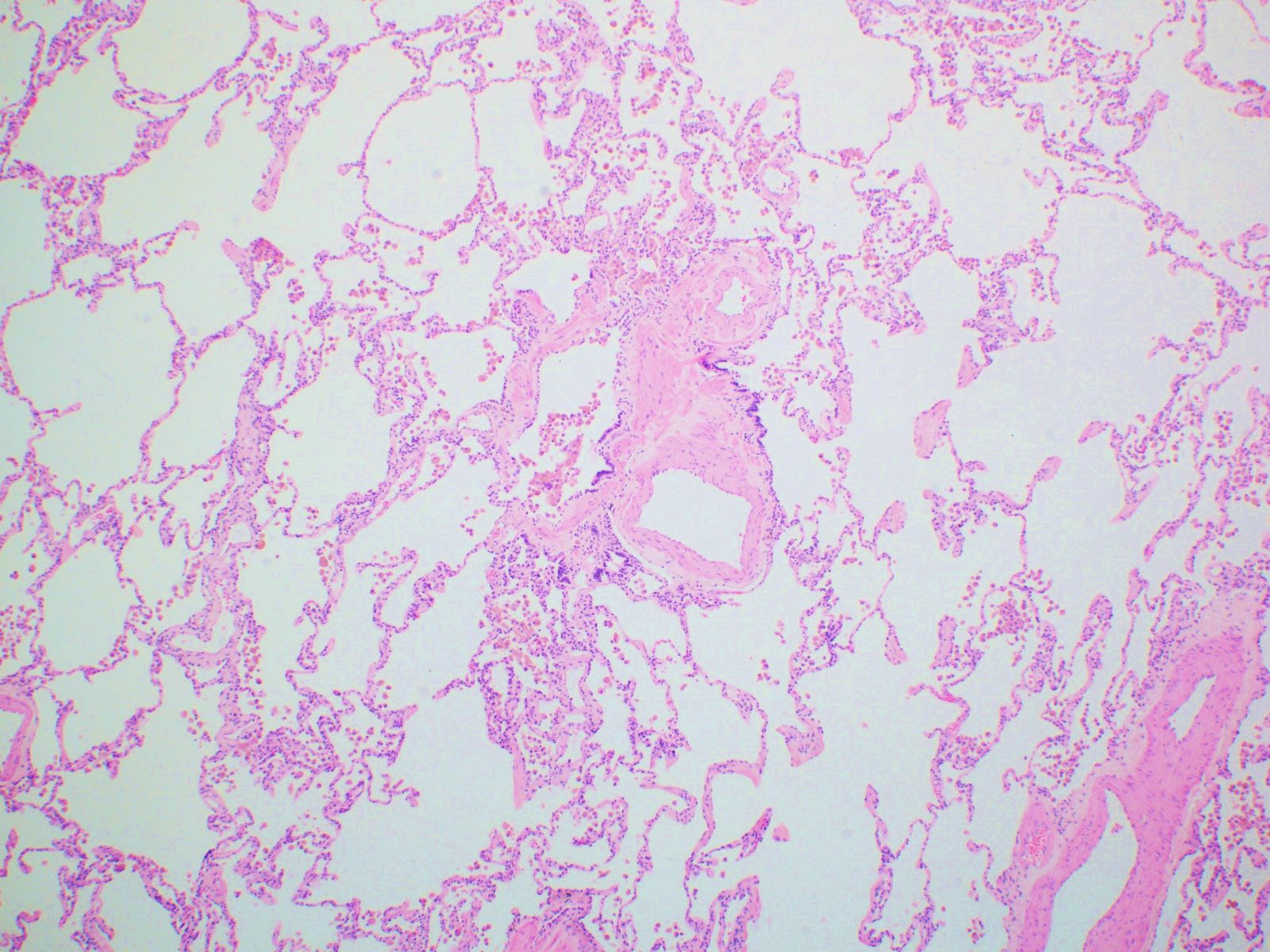
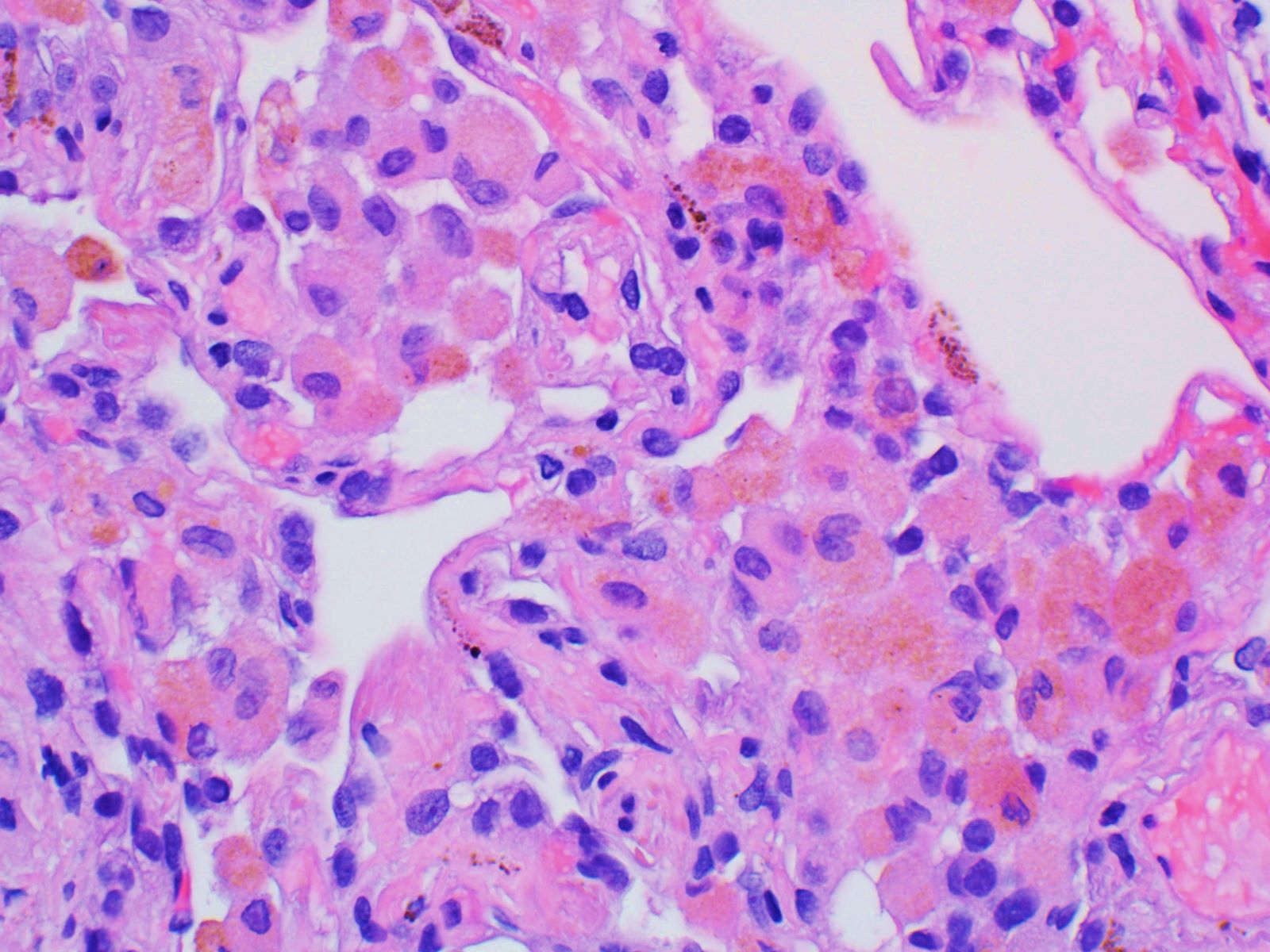
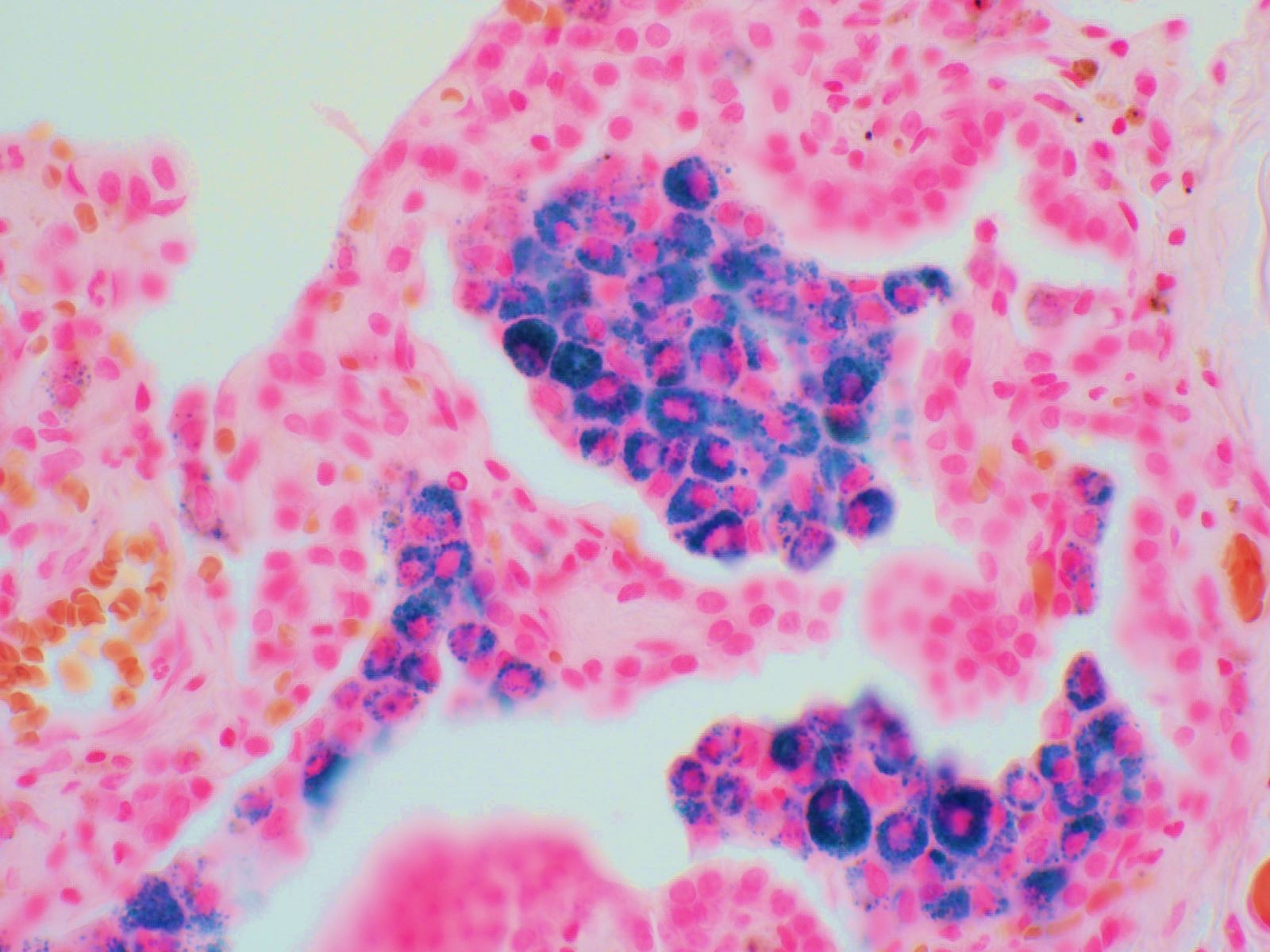
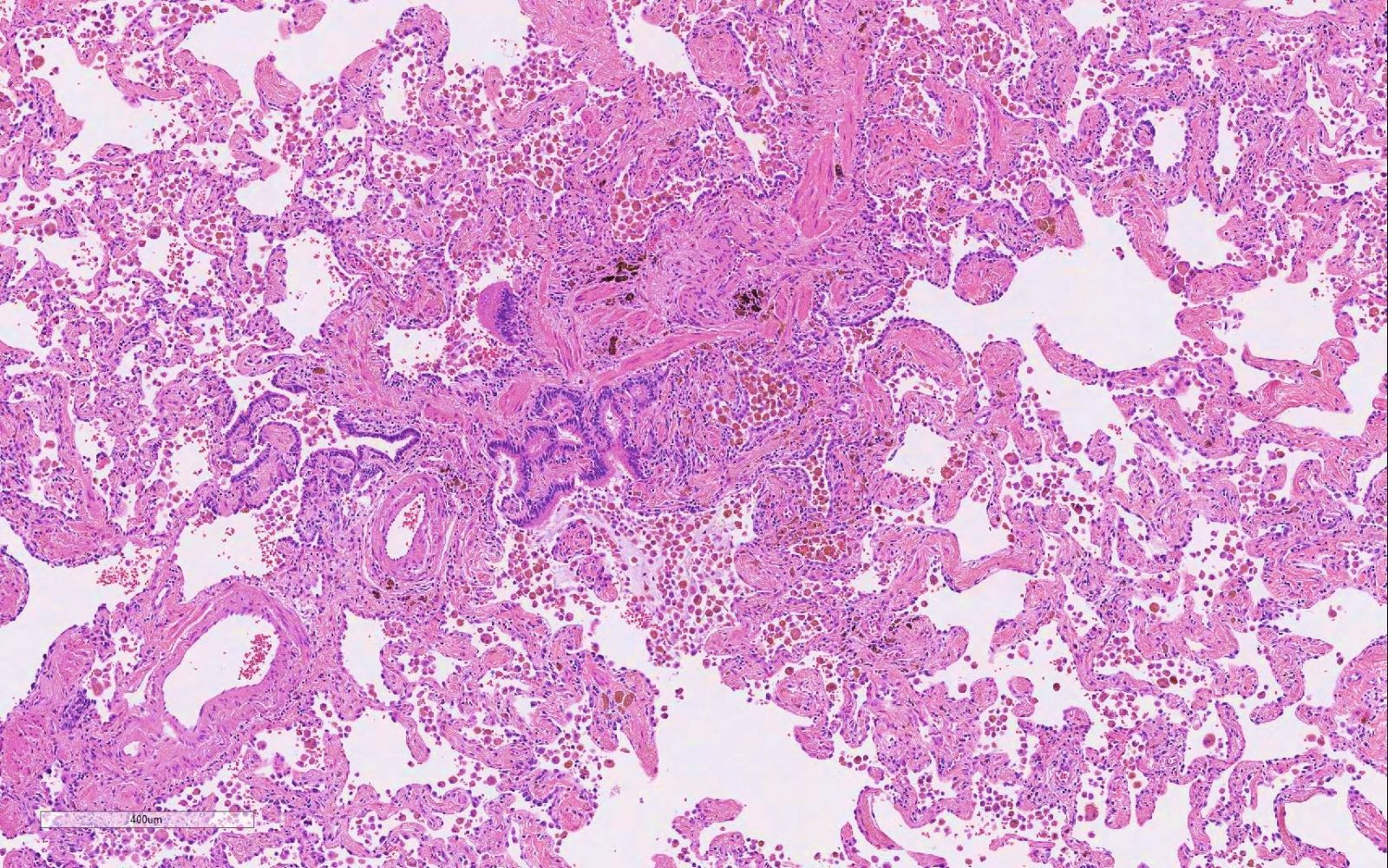
- Lightly pigmented (smoker's) macrophages limited to distal airspaces and peribronchiolar airspaces
- Pigment within macrophage cytoplasm is yellow to light brown and finely granular
- Minimal to absent peribronchiolar interstitial thickening by fibrosis
- No diffuse interstitial fibrosis or inflammation
Microscopic (histologic) images
Positive stains
- Iron (e.g. Prussian blue)
Negative stains
- None relevant to this diagnosis
Sample pathology report
- Lung, right upper, middle and lower lobes, wedge biopsies:
- Respiratory bronchiolitis (see comment)
- Comment: Respiratory bronchiolitis (RB) is a common incidental finding in current or former smokers and is usually of little clinical consequence. In a subset of patients, however, this is the only pathologic finding and seems to account for clinical interstitial lung disease. In this scenario, a diagnosis of respiratory bronchiolitis interstitial lung disease may be applicable.
Differential diagnosis
- Desquamative interstitial pneumonia (DIP):
- Substantial histologic overlap with respiratory bronchiolitis interstitial lung disease
- Diffuse accumulation of pigmented macrophages beyond the peribronchiolar airspaces into the distal airspaces
- Degree of interstitial fibrosis and inflammation usually greater than in respiratory bronchiolitis interstitial lung disease
- Hemosiderosis:
- Potential etiologies: diffuse alveolar hemorrhage or chronic passive vascular congestion
- Hemosiderin pigment darker and coarser than smoker's pigment
- Iron stain can help in highlighting iron encrustation of vascular elastica (endogenous pneumoconiosis), a finding seen in chronic hemorrhage or chronic passive congestion
Additional references
Board review style question #1
Board review style answer #1
B. Cigarette smoking. The image shows respiratory bronchiolitis, characterized by the accumulation of pigmented (smoker's) macrophages within distal airspaces. Aspiration usually results in amorphous or birefringent particulates within distal airspaces. Answer C is associated with hypersensitivity pneumonia, while type I hypersensitivity reactions are associated with atopic asthma. Respiratory bronchiolitis is a marker of current or former smoker status and is usually of no clinical consequence with no deaths attributable to it.
Comment Here
Reference: Respiratory bronchiolitis
Comment Here
Reference: Respiratory bronchiolitis
Board review style question #2
A 64 year old man with extensive smoking history undergoes lung wedge biopsy for evaluation of progressive exertional dyspnea and a restrictive defect on pulmonary function tests. Sections of the wedge biopsy show accumulation of lightly pigmented macrophages within distal airspaces. This is accompanied by patchy interstitial fibrosis that is associated with areas of architectural distortion and lung remodeling in the forms of scarring and honeycomb change. Based on these findings, which of the following is the best diagnosis?
- Desquamative interstitial pneumonia (DIP)
- Diffuse alveolar hemorrhage
- Respiratory bronchiolitis interstitial lung disease (RB-ILD)
- Smoking related interstitial fibrosis (SRIF)
- Usual interstitial pneumonia (UIP)
Board review style answer #2
E. Usual interstitial pneumonia (UIP). Although the features of respiratory bronchiolitis are present in the wedge biopsy sections and the patient has clinically significant interstitial lung disease, the diagnosis of respiratory bronchiolitis interstitial lung disease requires that other forms of diffuse lung disease have been ruled out. In this case, the findings of patchy interstitial fibrosis and honeycombing are consistent with usual interstitial pneumonia, which is the best explanation for this patient's symptoms and pulmonary function testing results.
Comment Here
Reference: Respiratory bronchiolitis
Comment Here
Reference: Respiratory bronchiolitis