Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Alrajjal A, Gabali A. Mycobacteria-atypical / other than TB or leprosy. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphnodesatypicalmycobacteria.html. Accessed April 16th, 2024.
Definition / general
- Common cause of granulomatous lymphadenitis in immunocompetent children and immunocompromised adults (Pediatr Int 2018;60:1062)
Essential features
- Diagnosis by excluding Mycobacterium tuberculosis and positive culture for atypical Mycobacterium or suggestive histology (Adv Exp Med Biol 2017;944:19)
- Lymph node partially or totally affected by sheets of foamy histiocytes
- Nonnecrotizing granulomas not needed for diagnosis
- Unilateral anterior neck lymph nodes in children (2 - 5 years) and immunocompromised adults
- Spontaneous regression may occur after 4 - 6 months
Terminology
- Atypical mycobacterial lymphadenitis
ICD coding
- ICD-10: A31.8 - Other mycobacterial infections
Epidemiology
- Children ages 2 - 5 are most susceptible
- Immunocompromised adults, HIV+
Sites
- Head and neck, usually unilateral anterior neck chain
Pathophysiology
- Mycobacterial, intracellular organisms, replicate within macrophages
- Macrophages antagonize bacterial growth via TNF dependent mechanisms
- Mycobacteria induce infected macrophage apoptosis
- Newly recruited macrophages engulf cell debris, contributing to granuloma expansion
- Newly infected macrophages can exit the primary granuloma and establish secondary granuloma in distal tissue (Cold Spring Harb Perspect Med 2014;5:a018499)
Etiology
- Most common causes are M. avium intracellulare complex, M. marinum, M. fortuitum, M. scrofulaceum, M. kansasii (Clin Infect Dis 1995;20:9549)
Clinical features
- Chronic, painless, lymphadenopathy
- Head and neck, unilateral
Diagnosis
- Culture: sensitivity 41%, specificity 100% (gold standard) (Int J Pediatr Otorhinolaryngol 2018;112:48)
- PCR: sensitivity 71.6%, specificity 100%
- Sensitivity of immunoassay: sensitivity 87.5 - 100%, specificity 81 - 100%
- Skin tests (PPD-S): sensitivity 70%, specificity of 94%
Laboratory
- Nucleic acid amplification (NAAT) only for Mycobacterium tuberculosis complex; tuberculosis and M. bovis: 90% sensitivity
- Good for diagnosis not follow up; could detect RNA 6 months after starting therapy
Radiology description
- Ultrasound: markedly decreased echogenicity, intranodal liquefactive / cystic necrosis, nodal matting and adjacent soft tissue edema (Pediatr Radiol 2006;36:1063)
Case reports
- 19 month old girl with the first reported case of human infection with Mycobacterium stomatepiae (JMM Case Rep 2018;5:e005146)
- 2 year old African American girl presented to the clinic with anterior ear lobe and submandibular lymphadenitis (Cureus 2016;8:e846)
- 46 year old man with necrotizing lymphadenitis during therapy for AML (Infect Chemother 2017;49:78)
- 67 year old man without immunodeficiency with right axillary lymphadenitis and lung right upper lobe nodule (Respir Med Case Rep 2019;28:100947)
Treatment
- Complete excision: highest cure rate and highest risk of facial nerve palsy
- Decision on excision versus long term antibiotics versus no treatment should be based on location and number of lymph nodes (J Infect 2015;71:9)
Gross description
- Enlarged rubbery lymph node, tan glistening surface with multifocal irregular necrotic soft tissue
Gross images
Frozen section description
- Identical to microscopic
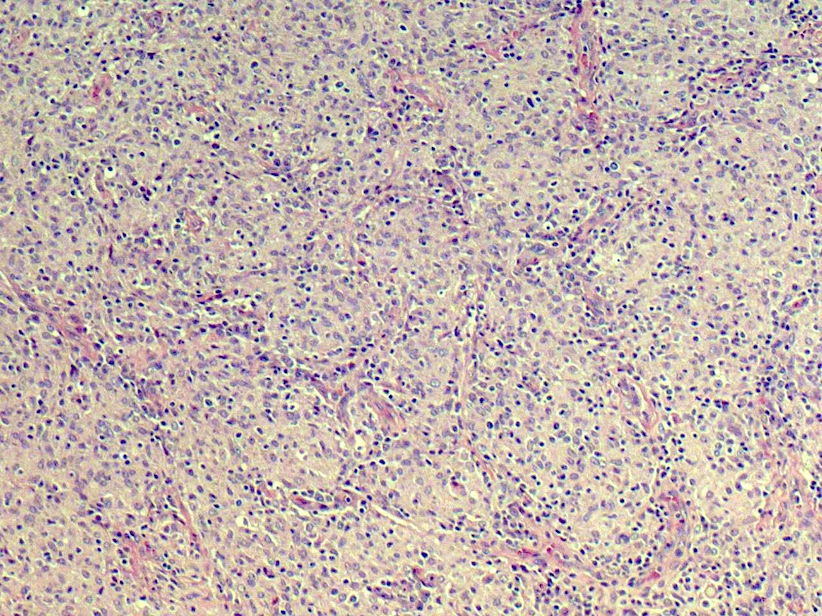
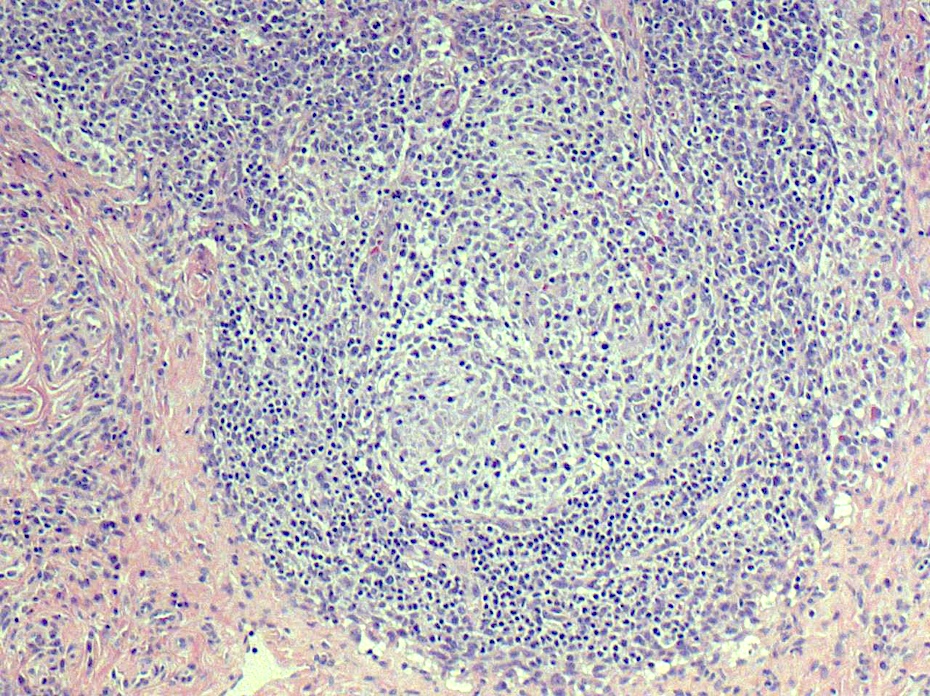
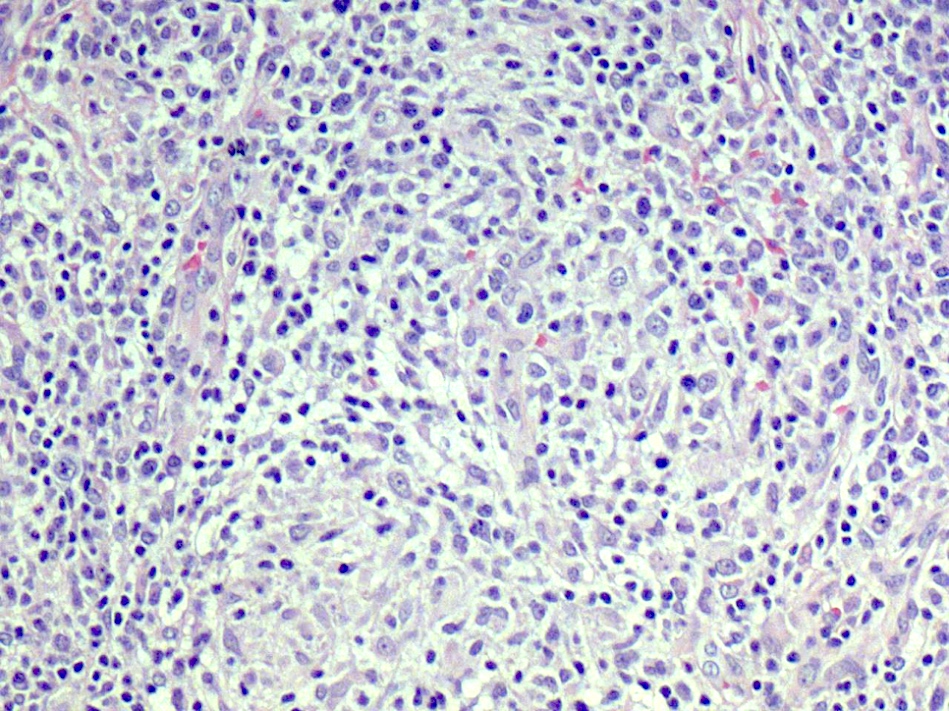
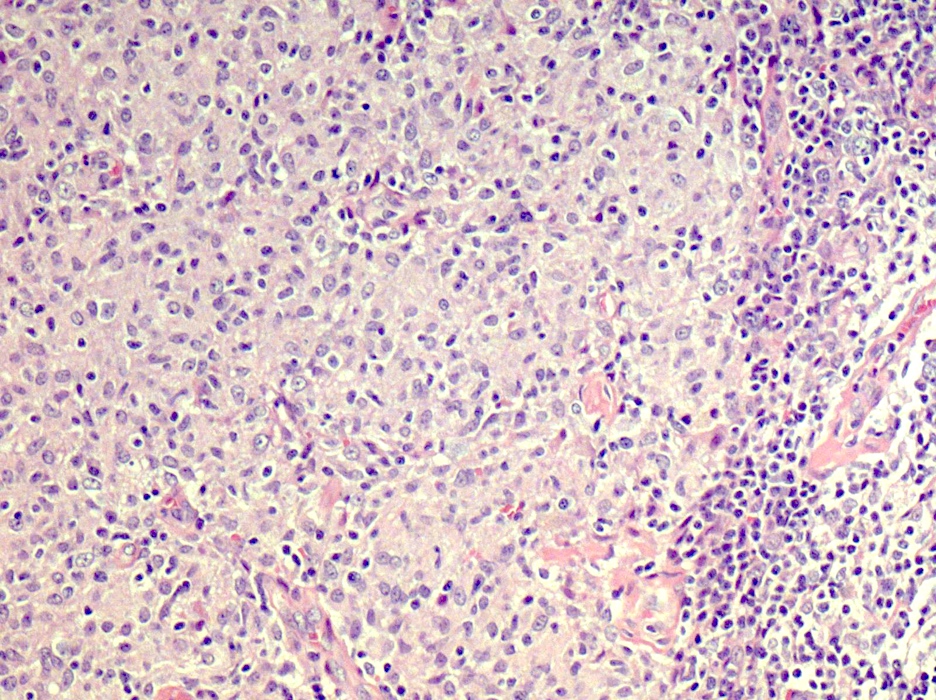
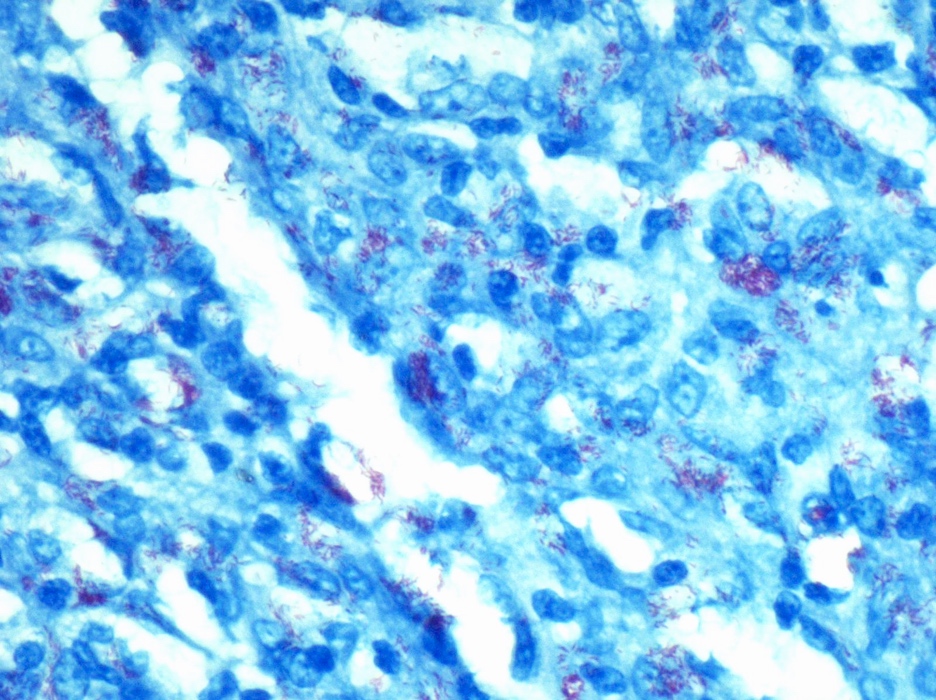
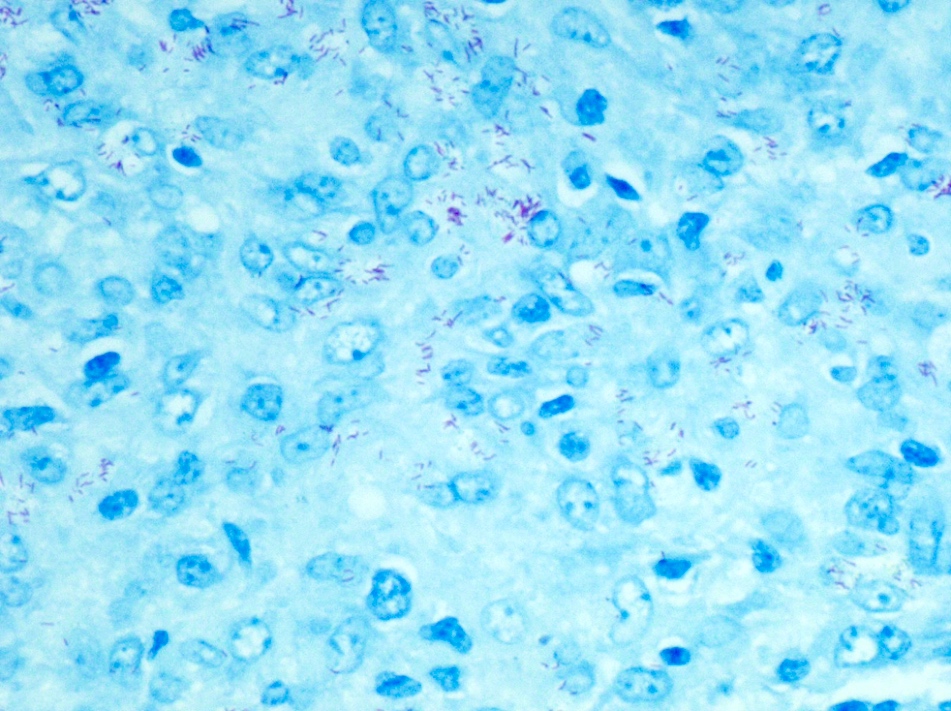
Microscopic (histologic) description
- Granulomatous inflammation with or without necrosis, the presence of microabscesses, ill defined granulomas, noncaseating granulomas and a small number of giant cells favors nontuberculous mycobacteria over tuberculosis (Histopathology 1999;35:534)
Microscopic (histologic) images
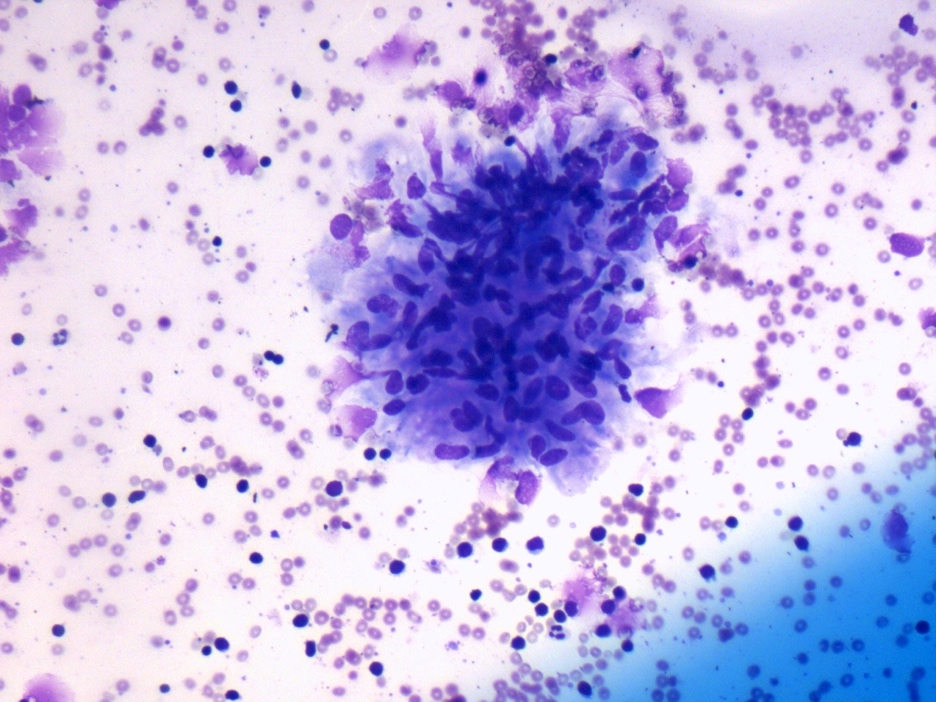
Cytology description
- Suppurative granulomas
- Necrotizing granulomas typical for tuberculosis infection; also seen in atypical mycobacterial infection
- Granulomas without necrosis can be suggestive of sarcoidosis
- Multiple passes for cultures or PCR testing are recommended
- Reference: BMC Infect Dis 2020;20:224
Cytology images
Positive stains
- Ziehl-Neelsen:
- Acid fast bacteria are red
- Growth only (hot stain)
- Kinyoun stain:
- Acid fast bacteria are red
- Growth and susceptibility (cold stain)
- Fite stain:
- Acid fast bacteria are red
- Modified Ziehl-Neelsen specifically for M. leprae
- Auramine O:
- Bright yellow luminous rods against a dark background with fluorescent microscope
- Increased sensitivity and speed
- Reference: Ann Clin Lab Sci Spring 2014;44:131
Negative stains
Molecular / cytogenetics description
- 16S rRNA sequencing (New Microbes New Infect 2017;22:24, J Clin Microbiol 2000;38:246)
- PCR restriction fragment length polymorphism (PCR-RFLP) procedure capable of rapidly identifying 28 species of clinically encountered mycobacteria (J Clin Microbiol 1997;35:79)
Sample pathology report
- Lymph node, left neck, excision:
- Nonnecrotizing granulomatous lymphadenitis (see comment)
- Comment: The lymph node architecture is partially affected by sheets of foamy histiocytes and multifocal granulomas. The granulomas are ill defined and composed of epithelioid histiocytes, lymphocytes and occasional plasma cells. No evidence of necrosis is noted. AFB Fite special stain is positive for mycobacterial organisms. Paraffin embedded block was sent for PCR analysis for strain identification and subspeciation and the results will be reported in an addendum.
Differential diagnosis
- Tuberculous mycobacterial infection:
- Usually necrotizing granuloma
- Few organisms are AFB stain positive
- Nucleic acid amplification and culture are positive for Mycobacterium tuberculosis
- Fungal infection:
- Foreign body reaction:
- Polarizable material may be present on tissue
- Sarcoidosis:
- Diagnosis of exclusion by definition
- Negative for cultures and stains
- Naked type granuloma with very few lymphocytes
Board review style question #1
What is the most common histologic finding in non-TB mycobacterial lymphadenitis caused by MAC infection in an immunocompromised patient?
- Necrotizing granulomatous inflammation
- Suppurative inflammation
- Follicular hyperplasia
- Nonnecrotizing granulomatous inflammation with sheets of foamy histiocytes
- Parafollicular hyperplasia
Board review style answer #1
D. Nonnecrotizing granulomatous inflammation with sheets of foamy histiocytes
Comment Here
Reference: Mycobacteria - atypical / other than TB or leprosy
Comment Here
Reference: Mycobacteria - atypical / other than TB or leprosy
Board review style question #2
An HIV positive 34 year old man has an enlarged painless lymph node. Nucleic acid amplification and culture are negative for mycobacterial tuberculosis organisms. What is the most common mycobacterial infection in immunocompromised patients such as this one?
- M. aortuitum
- M. avium intracellulare
- M. gordonae
- M. scrufulaceum
Board review style answer #2
B. M. avium intracellulare is the most common nontuberculous mycobacterial infection in immunocompromised patients.
Comment Here
Reference: Mycobacteria - atypical / other than TB or leprosy
Comment Here
Reference: Mycobacteria - atypical / other than TB or leprosy