Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Backer SA, Kitahara S. Granulomatous inflammation. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphnodesgranulomatous.html. Accessed April 25th, 2024.
Definition / general
- Specialized immune response against various inflammatory insults, involving chronic activation and organization of mononuclear phagocytic cells (macrophages) (J Clin Tuberc Other Mycobact Dis 2017;7:1)
- Histologically characterized by epithelioid histiocytes, with or without central necrosis, surrounded by acute or chronic inflammation
Essential features
- Specialized inflammatory response against various offending entities, including (StatPearls: Granuloma [Accessed 13 June 2022]):
- Infectious (usually necrotic, suppurative)
- Autoimmune / inflammatory
- Malignancy
- Others (see below)
- Histologically characterized by central epithelioid histiocytes surrounded by acute or chronic inflammation
- Microbiologic cultures of fresh sample, special stains / immunohistochemistry for microorganisms are essential when clinical history includes suspicion of infection or an immunocompromised / suppressed state
- Immunohistochemistry to evaluate for malignancies that arise as differential diagnoses (e.g., carcinoma [cytokeratin], melanoma [SOX10]) (O'Malley: Benign and Reactive Conditions of Lymph Node and Spleen, 1st Edition, 2009)
Terminology
- Lymphadenitis (LA), infectious lymphadenitis, granulomatous lymphadenitis (GLA)
ICD coding
Epidemiology
- May be associated with infectious disease or noninfectious disease (J Clin Tuberc Other Mycobact Dis 2017;7:1)
- No particular predilection for age / sex (StatPearls: Lymphadenopathy [Accessed 13 June 2022])
Sites
- Any lymph node site in the body
- Spleen (O'Malley: Benign and Reactive Conditions of Lymph Node and Spleen, 1st Edition, 2009)
- Certain etiologies have strong association with anatomical site (J Clin Tuberc Other Mycobact Dis 2017;7:1)
- Inguinal nodes in lymphogranuloma venereum
- Cervical and axillary nodes in tularemia and cat scratch disease
- Mesenteric lymph nodes in Yersinia lymphadenitis
- Pulmonary hilar lymph nodes in environmental, fungal, tuberculous lymphadenitis
Pathophysiology
- Dysregulation of immune response due to inability of macrophages to clear the offending agent (StatPearls: Granuloma [Accessed 13 June 2022])
- Results in chronic active inflammation, histologically characterized by (StatPearls: Granuloma [Accessed 13 June 2022]):
- Central collection of epithelioid histiocytes
- Rim of plasma cells and lymphocytes
- Central necrosis or suppuration, depending on etiology
- Can be conceptualized as consisting of 3 phases (J Clin Exp Hematop 2012;52:1):
- Initiation / accumulation, peak and late phase
- Initiation characterized by activation of T cells via MHC class II interactions with antigen presenting cells (APCs) (J Clin Tuberc Other Mycobact Dis 2017;7:1)
- Activated T helper 1 (Th1) cells stimulate and recruit macrophages via secretion of TNF alpha, IFN gamma, IL2, IL12 and chemokines
- Precise mechanism of defective downregulation of active inflammation is poorly understood
- With ensuing active inflammation, peak phase is characterized by rim of chronic inflammatory infiltrate consisting of:
- CD4+ T cells, CD8+ T cells, NK cells, plasma cells and occasional granulocytes
- Certain infectious GLA features prominent monocytoid B cell infiltrates (Toxoplasma lymphadenitis, Bartonella) (J Clin Exp Hematop 2012;52:1)
- Role poorly understood
- Late phase characterized by fibrosis and hyalinization
- Resolution occurs after clearance of antigenic stimulus and is characterized by a fibrous scar
Etiology
- Infectious:
- Suppurative (purulent):
- Tularemia lymphadenitis (Francisella tularensis)
- Cat scratch lymphadenitis (Bartonella henselae)
- Yersinia lymphadenitis (Yersinia enterocolitica)
- Various fungal infections
- Nonsuppurative:
- Tuberculous lymphadenitis (Mycobacterium tuberculosis spp.)
- Atypical mycobacterial infection
- Bacillus Calmette-Guérin (BCG) lymphadenitis
- Toxoplasma lymphadenitis
- Hansen disease or leprosy (M. leprae)
- Syphilis
- Brucellosis
- Fungal lymphadenitis (Coccidioides, Cryptococcus, Histoplasma, Pneumocystis)
- Suppurative (purulent):
- Noninfectious:
- Systemic sarcoidosis
- Foreign body (berylliosis, silicosis)
- Malignancies (lymphoma, carcinoma, especially breast, uterus, lung, stomach)
- Systemic inflammatory / autoimmune conditions (lupus [SLE], rheumatoid arthritis [RA], granulomatosis with polyangiitis [GPA])
- Toxic (chemotherapy, heavy metals, beryllium, zirconium, silicon)
- Histiocytic inflammatory (Rosai-Dorfman disease, Castleman disease)
- Reference: J Clin Tuberc Other Mycobact Dis 2017;7:1
Clinical features
- Painful / painless lymphadenopathy (StatPearls: Lymphadenopathy [Accessed 13 June 2022])
Diagnosis
- Clinical exam
- Imaging:
- CT
- Ultrasound
- Tissue biopsy:
- Excisional preferred over needle core biopsies, due to preservation of lymph node architecture; usually yields sufficient tissue to perform ancillary studies (microbiologic studies, special stains, immunostains)
- Fine needle aspiration (FNA):
- Can be ultrasound guided
- Reference: StatPearls: Lymphadenopathy [Accessed 13 June 2022]
Laboratory
- Dependent on suspected etiology but generally includes:
- Microbiologic studies (e.g., cultures, serology)
- Essential to obtain tissue cultures, as necrotic node usually contains high density of organisms
- Autoimmune / rheumatology workup
- Microbiologic studies (e.g., cultures, serology)
Prognostic factors
- Dependent on etiology (e.g., HIV, sarcoidosis, malignancy, infection)
Case reports
- 27 year old Greek man with suppurative necrotizing granulomatous lymphadenitis in adult onset Still disease (J Med Case Rep 2012;6:354)
- 29 year old man with necrotizing granulomatous sarcoidosis (Cureus 2020;12:e10220)
- 82 year old man with necrotizing granulomatous lymphadenitis (BMJ Case Rep 2011;2011:bcr1120103548)
Treatment
- Management of underlying disease (e.g., infection, neoplasm, inflammatory / autoimmune)
- Removal of offending agent (e.g., removal of foreign body)
Gross description
- Pale tan circumscribed nodules
- Fibrotic and firm compared to surrounding lymph node parenchyma
- Can show central necrosis, which can be dry and crumbly (caseating) or soft with a gelatinous consistency
- Can show gross suppuration
- Reference: Foucar: Tumors of the Bone Marrow, 1st Edition, 2016
Frozen section description
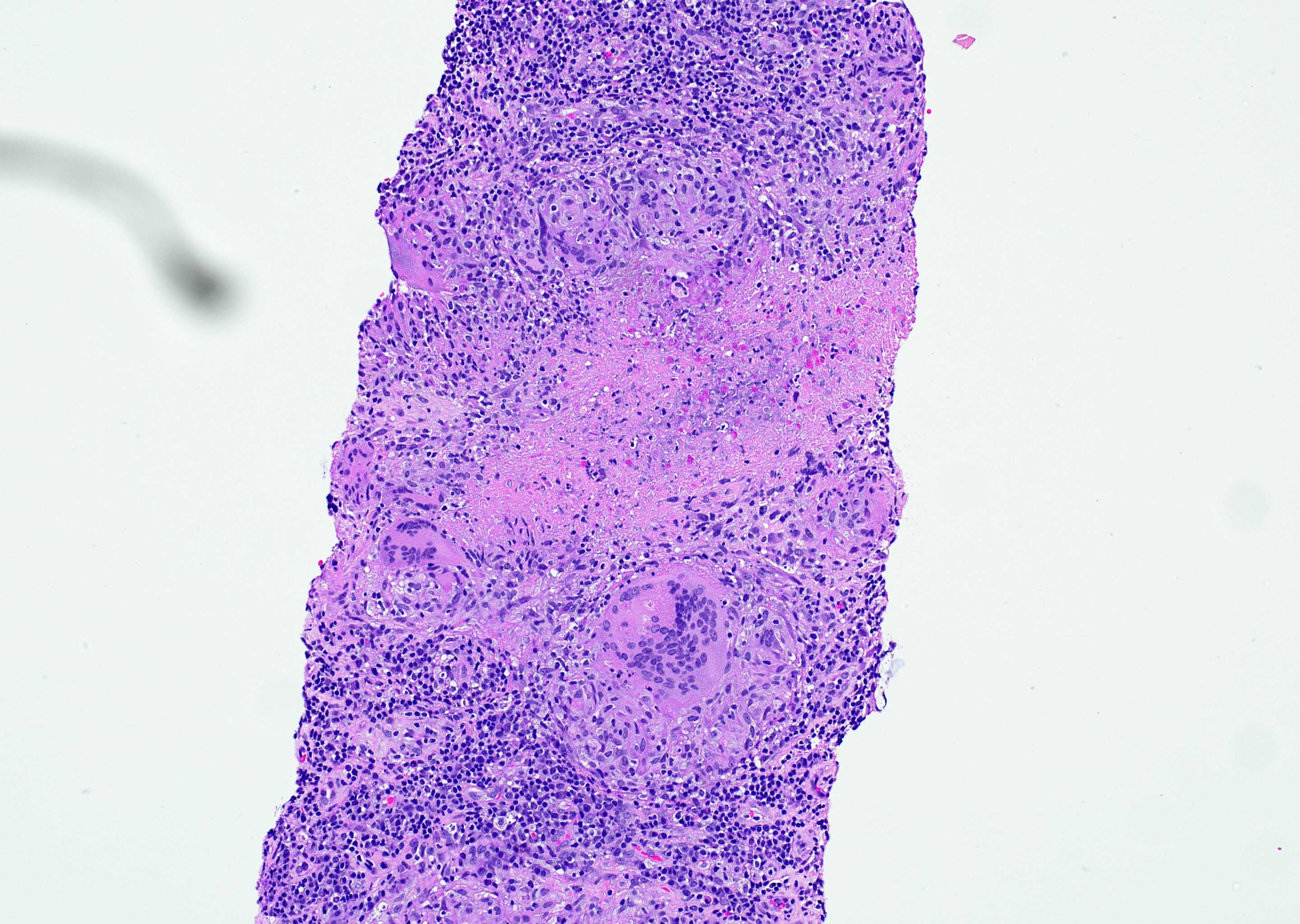
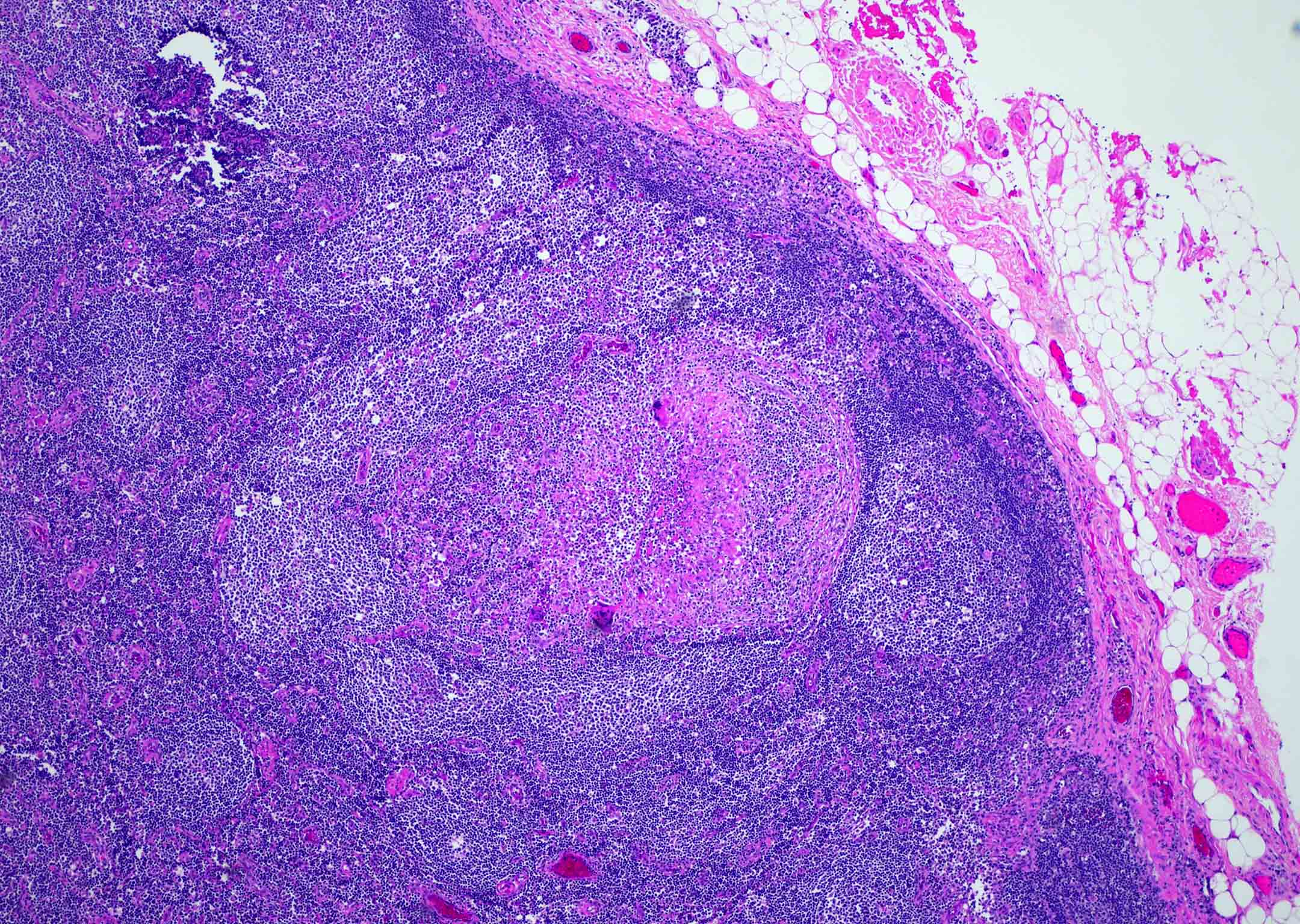
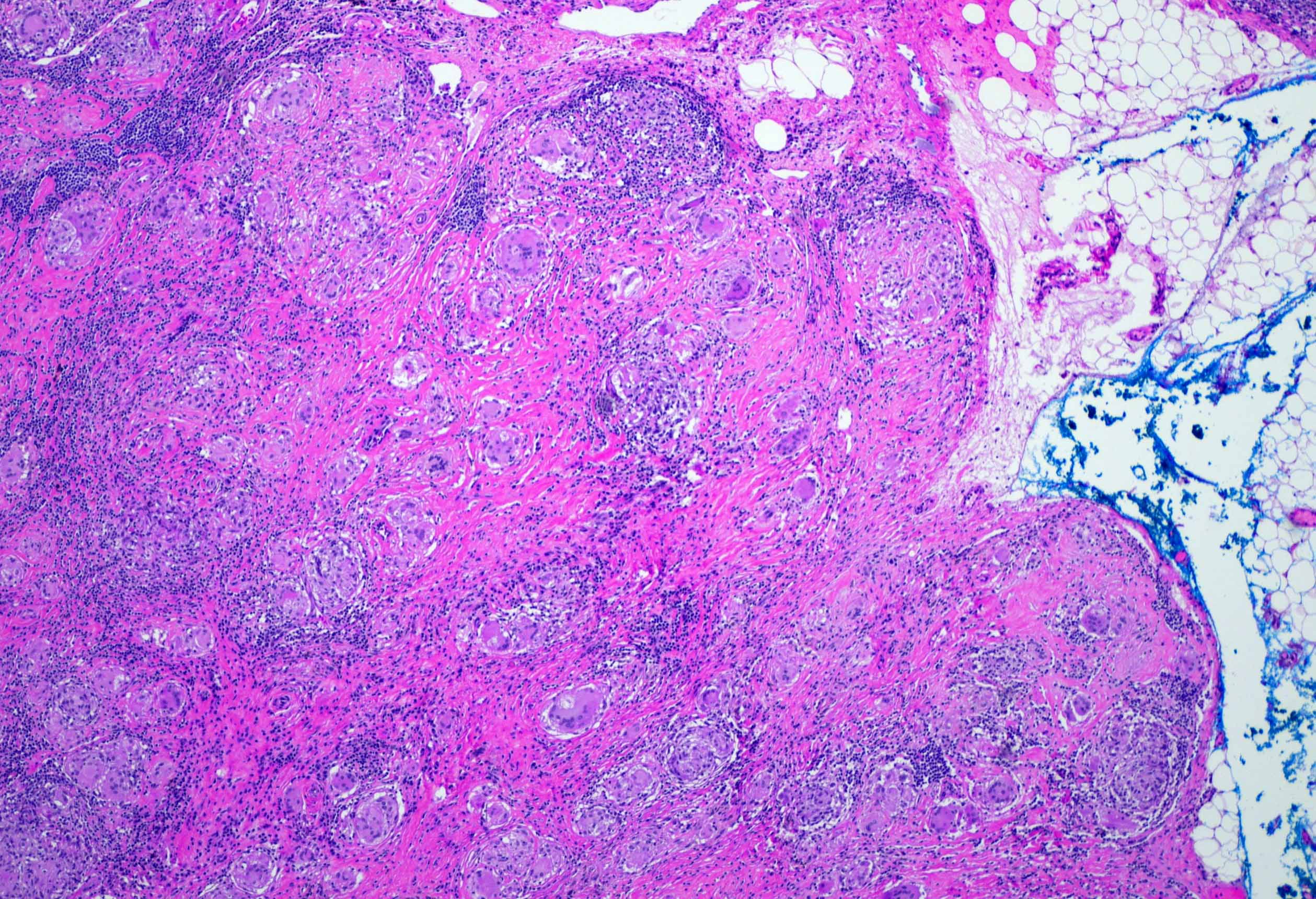
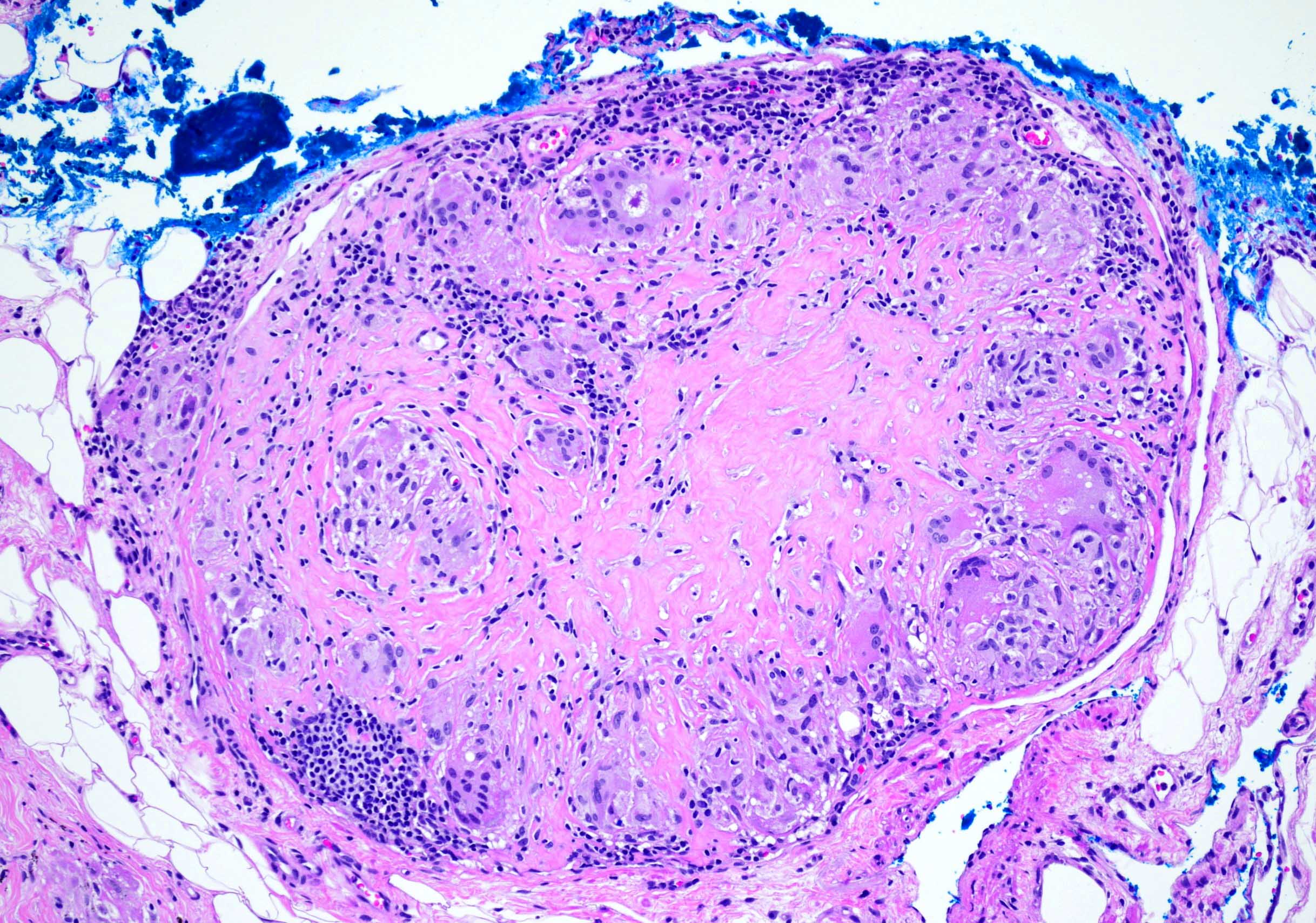
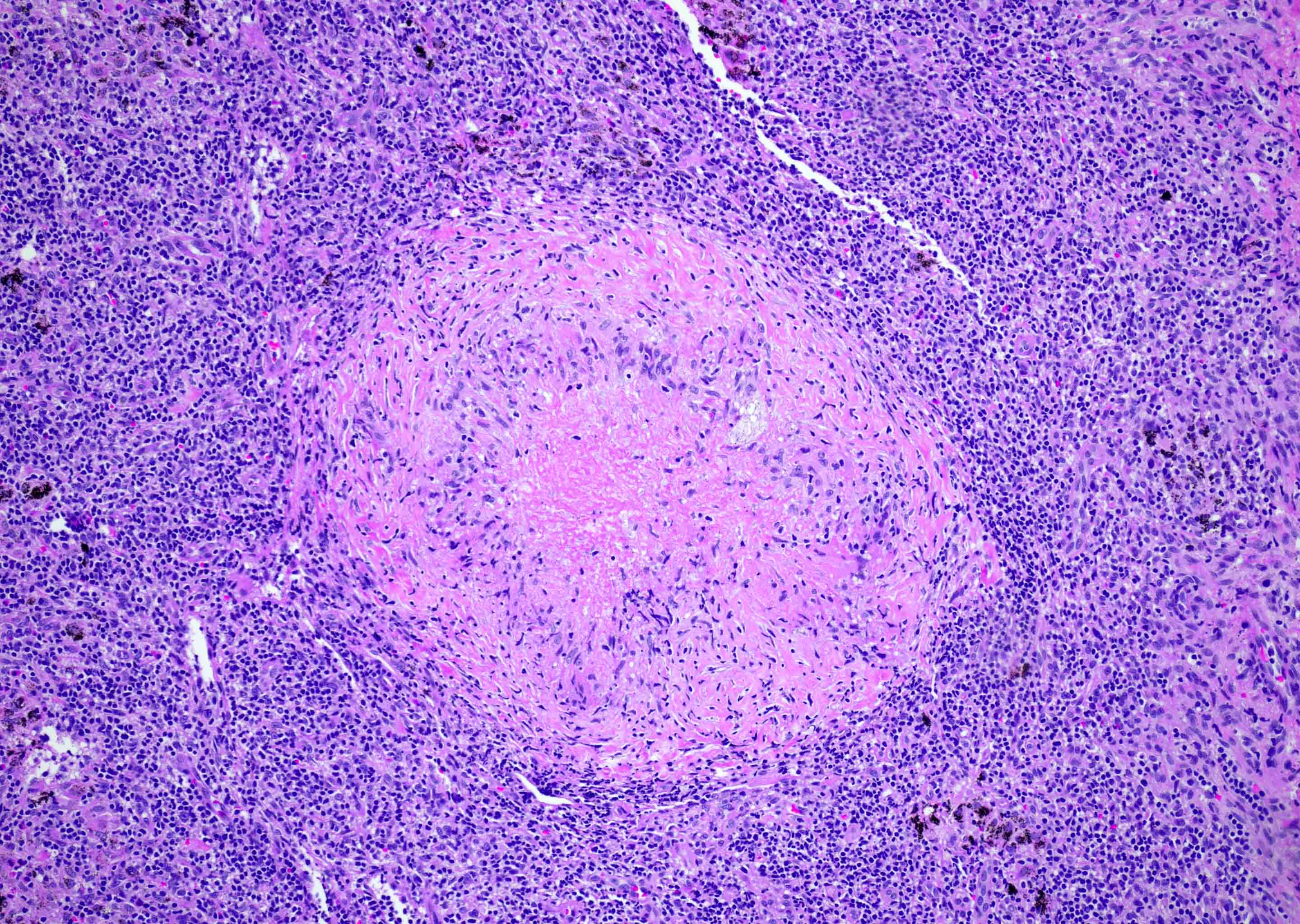
Microscopic (histologic) description
- Collection of epithelioid macrophages with abundant eosinophilic cytoplasm and indistinct cell borders (StatPearls: Granuloma [Accessed 13 June 2022])
- Surrounded by a rim of inflammatory cells, including lymphocytes, plasma cells and macrophages (StatPearls: Granuloma [Accessed 13 June 2022])
- Multinucleated giant cells are often present (StatPearls: Granuloma [Accessed 13 June 2022])
- Certain etiologies may demonstrate characteristic features
- May present as a characteristic triad of florid follicular hyperplasia, interfollicular monocytoid B cells and cortical / subcortical, ill defined aggregates of epithelioid cells (Toxoplasma lymphadenitis)
- Subtypes:
- Necrotizing granulomas (J Clin Exp Hematop 2012;52:1):
- Necrotic focus surrounded by a rim of chronic inflammatory cells, including epithelioid macrophages
- May show suppuration (acute inflammation) depending on etiology
- Usually associated with infectious agents (e.g., tuberculosis, lymphogranuloma venereum, tularemia, cat scratch disease, fungal)
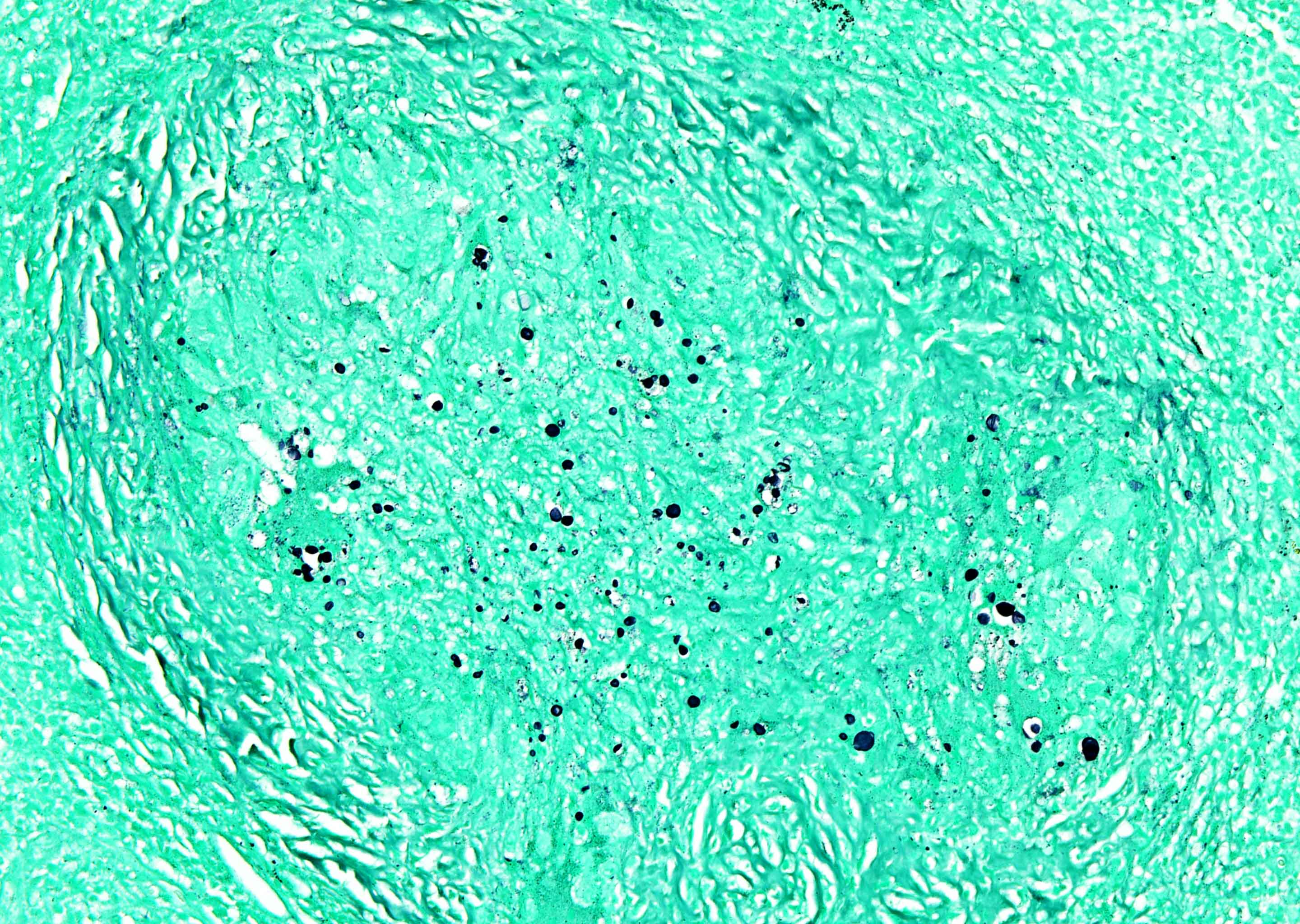
- Important to look for organisms within granulomas
- Use special stains to highlight
- Often essential for diagnosis as serology may have low sensitivity / specificity
- Obtain tissue culture
- Nonnecrotizing (sarcoid and sarcoid-like) granulomas (J Clin Exp Hematop 2012;52:1):
- Well defined borders, cohesive solid appearance, no central necrosis
- Various types of inclusions inside macrophages (e.g., asteroid bodies)
- Etiology includes
- Sarcoidosis containing Langhans type giant cells containing nuclei arranged in a horseshoe shape along cell periphery
- Systemic / autoimmune entities
- Foreign body type lymphadenitis containing giant cells with haphazardly arranged nuclei and engulfed foreign material
- Lipogranuloma (O'Malley: Benign and Reactive Conditions of Lymph Node and Spleen, 1st Edition, 2009):
- Frequently found in spleen; can be seen in lymph node
- Focus of macrophages with ingested fat surrounded by a rim of lymphocytes and plasma cells
- Etiology is unknown
- Has been associated with excessive topical application / ingestion of mineral oils
- Necrotizing granulomas (J Clin Exp Hematop 2012;52:1):
Microscopic (histologic) images
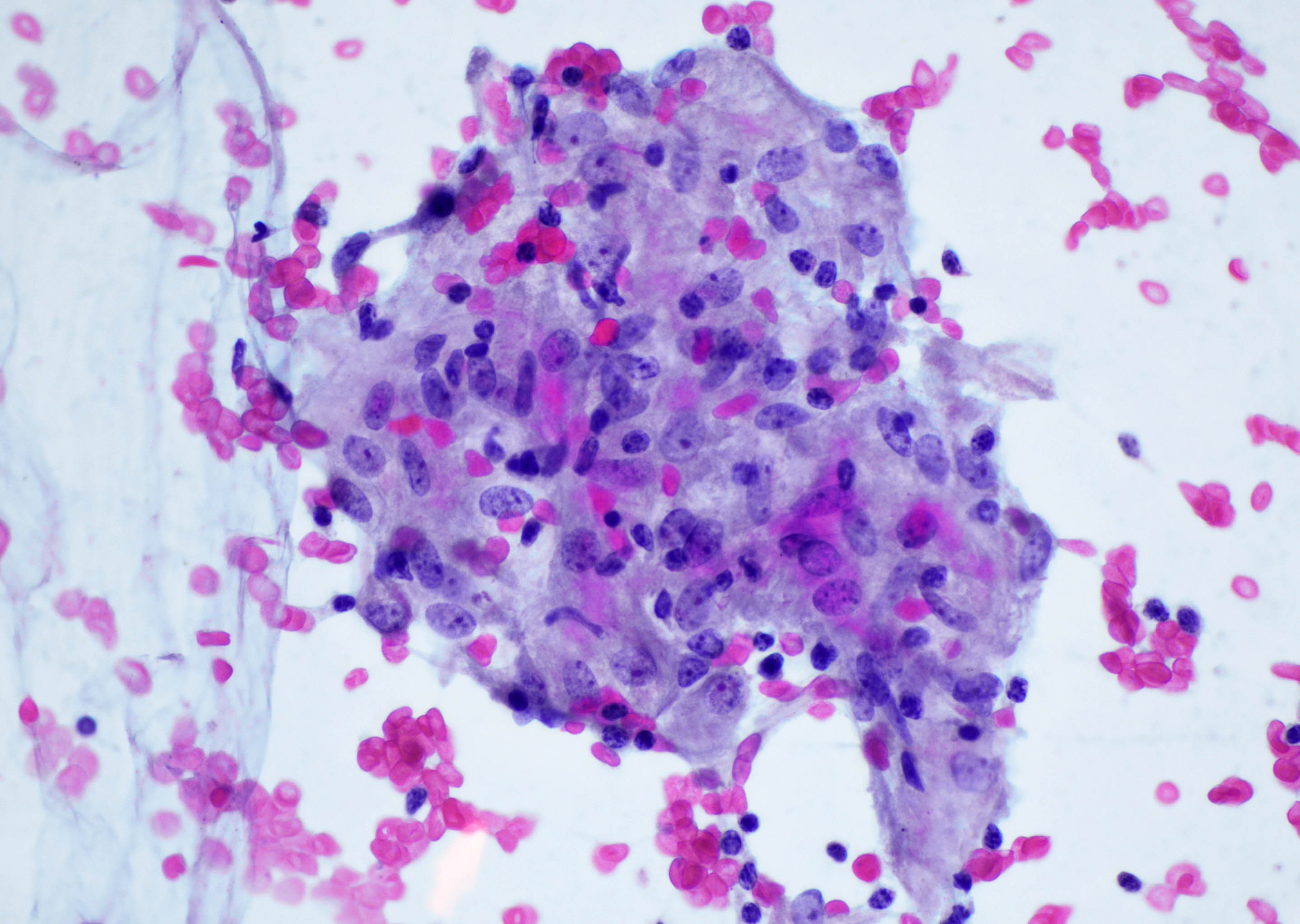
Cytology description
- Sarcoid granulomatous lymphadenitis:
- Tight collection of epithelioid histiocytes in syncytial arrangement with curved nuclei in horseshoe, C or V shape
- Infectious type granulomatous lymphadenitis:
- Histiocyte cluster may be loose or tight
- Usually surrounded by abundant acute inflammation
- Can show suppuration or necrosis, depending on infectious etiology
- Ultimately, findings are nonspecific and microbiologic, serologic studies are needed for a definitive etiology
- Reference: Cibas: Cytology - Diagnostic Principles and Clinical Correlates, 5th Edition, 2020
Positive stains
Negative stains
- Acid fast bacilli (AFB): positive in mycobacterial etiology
- Grocott methenamine silver (GMS) and periodic acid-Schiff (PAS): positive in fungal etiology
- Cytokeratin: positive in carcinoma
- SOX10: positive in melanoma
- CD30: positive in Hodgkin lymphoma
Sample pathology report
- R4 lymph node, excision:
- Nonnecrotizing granulomatous lymphadenitis (see comment)
- No evidence of malignancy identified
- Comment: The overall findings raise the possibility of sarcoidosis; infection remains in the differential diagnosis. AFB and GMS stains are negative for acid fast organisms and fungal forms. Clinical correlation with microbiologic studies is recommended.
Differential diagnosis
- Necrotizing granulomatous inflammation:
- Suppurative:
- Nonsuppurative:
- Nonnecrotizing granulomatous inflammation:
- Mycobacterium tuberculosis
- Nontuberculous mycobacterium (including Hansen disease)
- Salmonella typhi
- Rickettsia spp.
- Coxiella
- C. albicans
- C. immitis
- Viral (cytomegalovirus, herpes, hepatitides)
- Parasitic (toxoplasmosis, schistosomiasis)
- Noninfectious:
- Most noninfectious causes of granulomatous lymphadenitis present with nonnecrotizing granulomatous inflammation, including
- Autoimmune:
- Drugs:
- Bacillus Calmette-Guérin
- NSAIDs
- Antibiotics
- Methotrexate
- Malignancy associated:
- Carcinoma
- Melanoma
- Lymphoma (e.g., classic Hodgkin lymphoma, T cell lymphoma)
- Most noninfectious causes of granulomatous lymphadenitis present with nonnecrotizing granulomatous inflammation, including
- Foreign body:
- Talc, starch, suture, hyaluronic acid (and other injectable fillers):
- Foreign material may be visualized within granuloma
- May be polarizable
- Talc, starch, suture, hyaluronic acid (and other injectable fillers):
- Reactive conditions that present with granulomatous lymphadenitis:
- Kikuchi-Fujimoto disease:
- Predominance of CD8+ T cells surrounding necrotic center
- Histiocytes with C shaped nuclei
- Plasmacytoid dendritic cells
- Kimura disease:
- Hypereosinophilia and eosinophilic abscesses
- Preservation of follicles, hyperplastic follicles
- Stromal and perivascular sclerosis
- Kikuchi-Fujimoto disease:
- Rosai-Dorfman disease (also known as sinus histiocytosis with massive lymphadenopathy):
- Histiocytic neoplasms:
- Histiocytic sarcoma:
- Rarely affects lymph nodes (usually extranodal presentation)
- Diffuse infiltration by malignant, variably pleomorphic, mature appearing histiocytes
- Nodal architecture effacement, sparing of follicles
- No well formed granulomas
- Langerhans cell histiocytosis:
- Histiocytic sarcoma:
- Reference: J Clin Tuberc Other Mycobact Dis 2017;7:1
Board review style question #1
A 30 year old pregnant woman presents to her general practitioner complaining of mild flu-like symptoms. On physical examination, there is small but palpable, tender cervical lymphadenopathy. She states that her allergies seem to be acting up lately, which may be due to her new cat. She reports a family history of lymphoma in a grandparent and would like the lymph node biopsied. Sections of the node reveal secondary follicles of varying shapes and sizes, clusters of monocytoid lymphoid cells and cortical, loose collections of epithelioid histiocytes. Based on the clinical presentation and histologic findings, what is the most likely etiology for this patient's presentation?
- Cat scratch disease
- Follicular lymphoma
- Metastatic carcinoma
- Toxoplasmosis
- Tularemia
Board review style answer #1
Board review style question #2
You receive an excisional biopsy of an enlarged superficial neck lymph node from a 55 year old homeless man who was found obtunded. He is a poor historian and is unable to provide the duration of the adenopathy but he reports feeling unwell for quite some time. On physical examination, he has somewhat tender cervical adenopathy, as well as axillary and inguinal adenopathy. In addition, imaging studies show mediastinal and intra-abdominal adenopathy. Biopsy sections of the superficial cervical node show follicular hyperplasia with scattered epithelioid granulomas that are nonnecrotizing. The expanded follicles show a monotonous proliferation of small to medium lymphocytes, with variably irregular nuclear contours, condensed chromatin and scant cytoplasm. Occasional larger lymphoid cells are seen. Interfollicular plasma cells, eosinophils and scattered epithelioid histiocytes are also seen. What additional studies could narrow your differential diagnosis?
- AFB and GMS stains
- Immunostains to evaluate for both non-Hodgkin and Hodgkin lymphomas
- PCR studies for HIV
- Serologic studies for infectious etiologies
- Tissue culture of fresh tissue sent to the microbiology laboratory
Board review style answer #2
B. Immunostains to evaluate for both non-Hodgkin and Hodgkin lymphomas
Comment Here
Reference: Granulomatous inflammation
Comment Here
Reference: Granulomatous inflammation