Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Sites | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Flow cytometry description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Singh K, Ohgami R. Indolent T lymphoblastic proliferations. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphnodestlymphoblastic.html. Accessed April 18th, 2024.
Definition / general
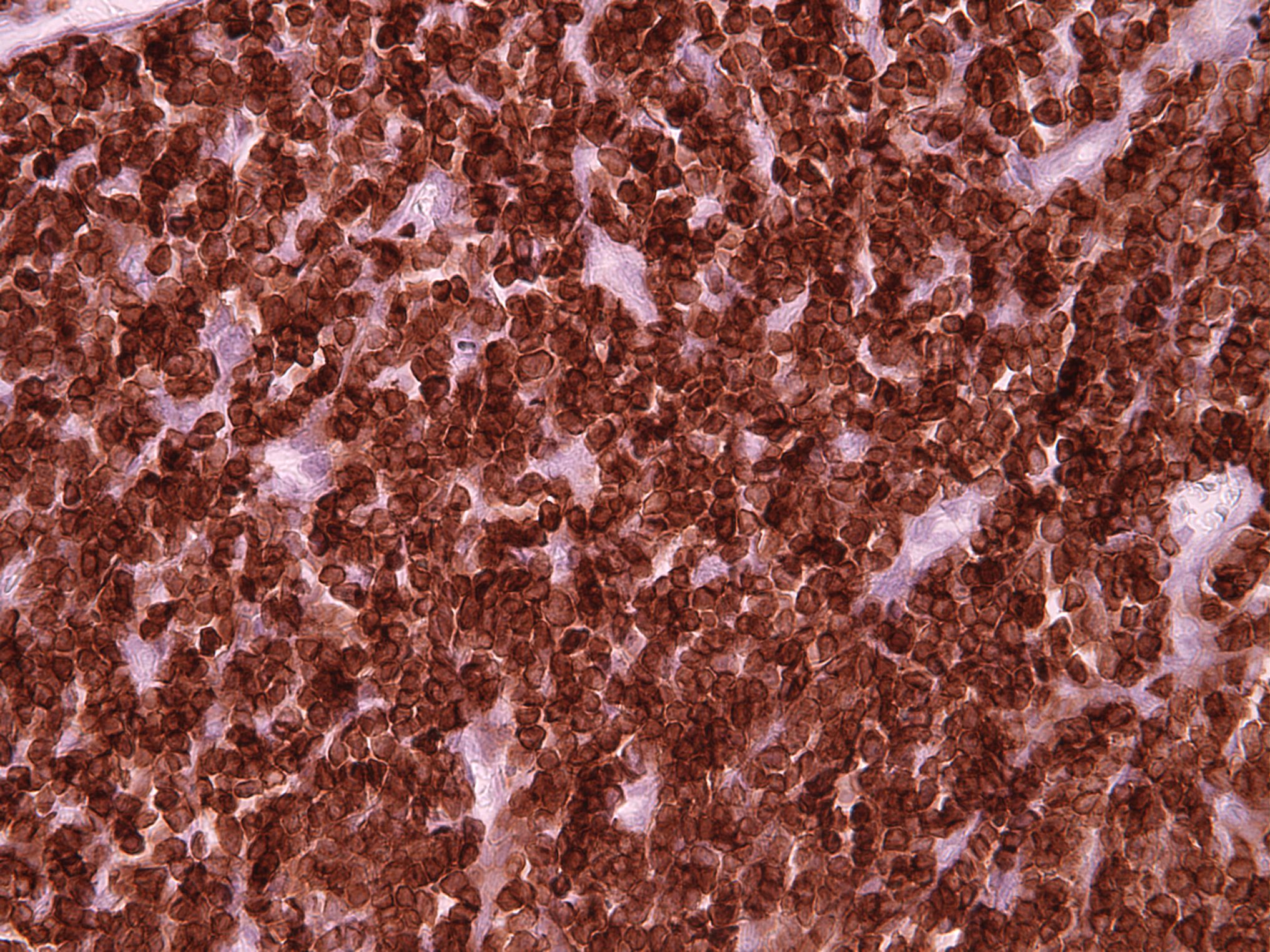
- Benign expansion of immature terminal deoxynucleotidyl transferase (TdT) positive T cells in extramedullary and extrathymic tissues
- Can be seen concurrently with other hematologic disorders or epithelial malignancies, such as Castleman disease, follicular dendritic cell sarcomas, angioimmunoblastic T cell lymphoma, hepatocellular carcinoma, acinic cell carcinoma, etc.
Essential features
- Benign proliferation of extrathymic immature T cells that lack significant morphologic atypia but mimic malignant T lymphoblastic lymphoma / leukemia
- Nonclonal process without evidence of TCR γ or β gene rearrangements
- Lack of aberrant immunophenotypic or karyotypic abnormalities
Terminology
- Immature T lymphoblastic proliferation
- iT-LBP
Epidemiology
- Age, gender, ethnicity, incidence / prevalence are undefined at this point
Sites
- Typically presents with localized lymphadenopathy or a discrete mass
- Common anatomical locations: mandible, cervical, supraclavicular, abdominal, retroperitoneal and oropharyngeal regions (Adv Anat Pathol 2013;20:137)
- Rare cases have shown disseminated multinodal involvement (Am J Surg Pathol 2014;38:1298)
- Does not involve mediastinum
- Peripheral blood and bone marrow are not involved
Clinical features
- Clinical presentation varies but patients are generally asymptomatic and healthy
- Can be associated with other underlying neoplastic pathologic conditions, such as carcinomas, Castleman disease, follicular dendritic cell tumors and angioimmunoblastic T cell lymphoma (Am J Surg Pathol 2012;36:1619)
Diagnosis
- Major criteria (Adv Anat Pathol 2013;20:137):
- No aberrant antigen expression (immunophenotype is of normal immature cortical thymocytes)
- Nonclonal TdT+ T cells
- No evidence of T cell gene rearrangements (TCR α and TCR β)
- Clinical evidence of indolence, > 6 months of follow up without progression in the absence of treatment
Prognostic factors
- Clinically indolent
- May persist in the involved tissue
Case reports
- 35 year old man with indolent T lymphoblastic proliferation associated with low grade follicular dendritic cell sarcoma and Castleman disease (Pathology 2018;50:351)
- 37 year old woman with an indolent T lymphoblastic proliferation involving the upper aerodigestive tract (Int J Clin Exp Pathol 2014;7:6350)
- 41 year old woman with pelvic pain found to have localized Castleman disease with concomitant iT-LBP (Ann Pathol 2019;39:29)
Treatment
- Typical lesions show no signs of progression and require no treatment
- Treatment for secondary disease (if present) may be needed
Gross description
- Typically forms a tumor mass, varies in size from ≤ 1 cm to ≥ 9 cm in greatest dimension
- External surface may be firm and fibrous or nonencapsulated
- Displays pink-tan firm fleshy cut surfaces
- Necrotic (yellow) areas may be seen in cases associated with hepatocellular carcinoma (HCC)
- Reference: Adv Anat Pathol 2013;20:137
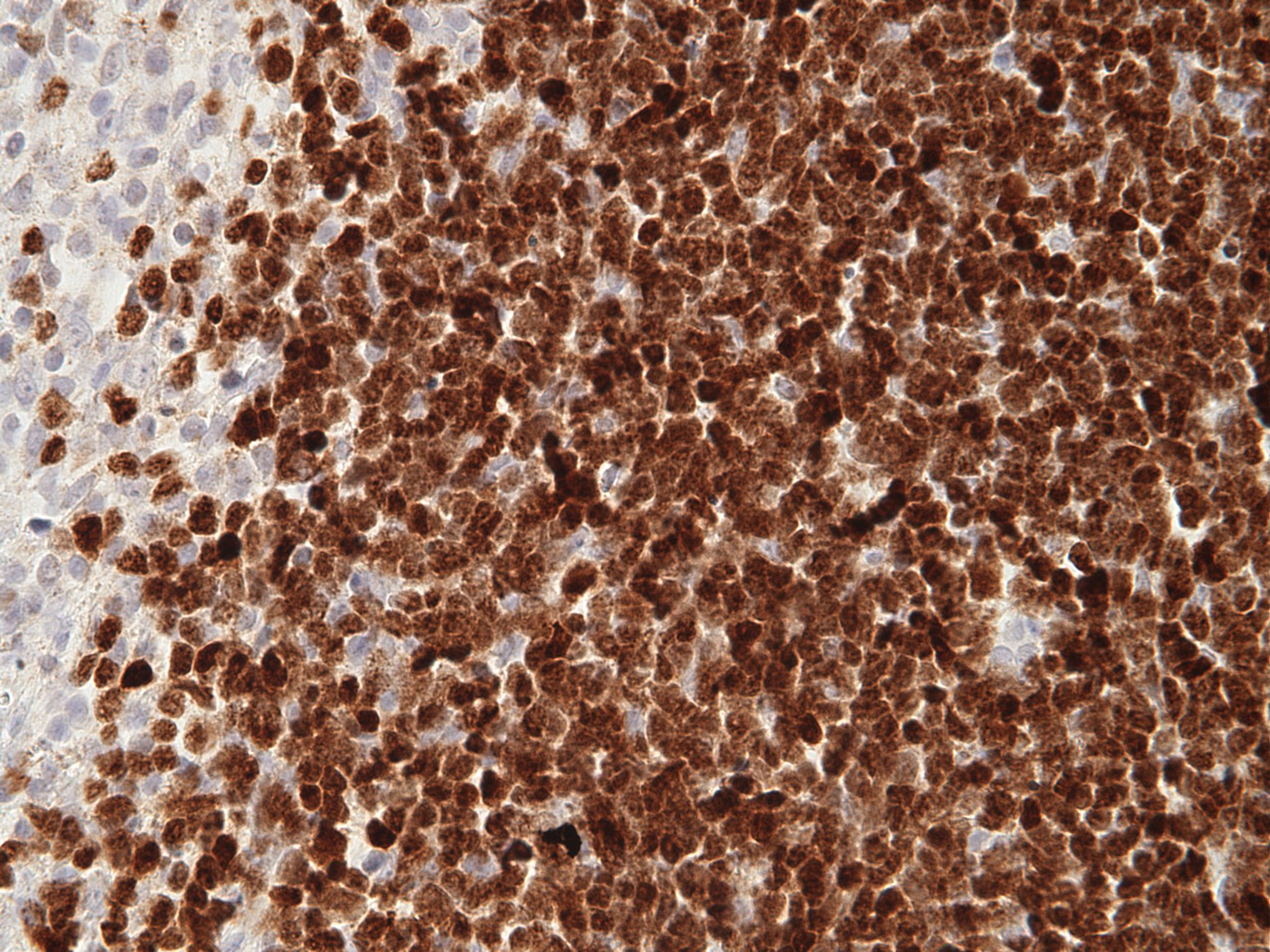
Microscopic (histologic) description
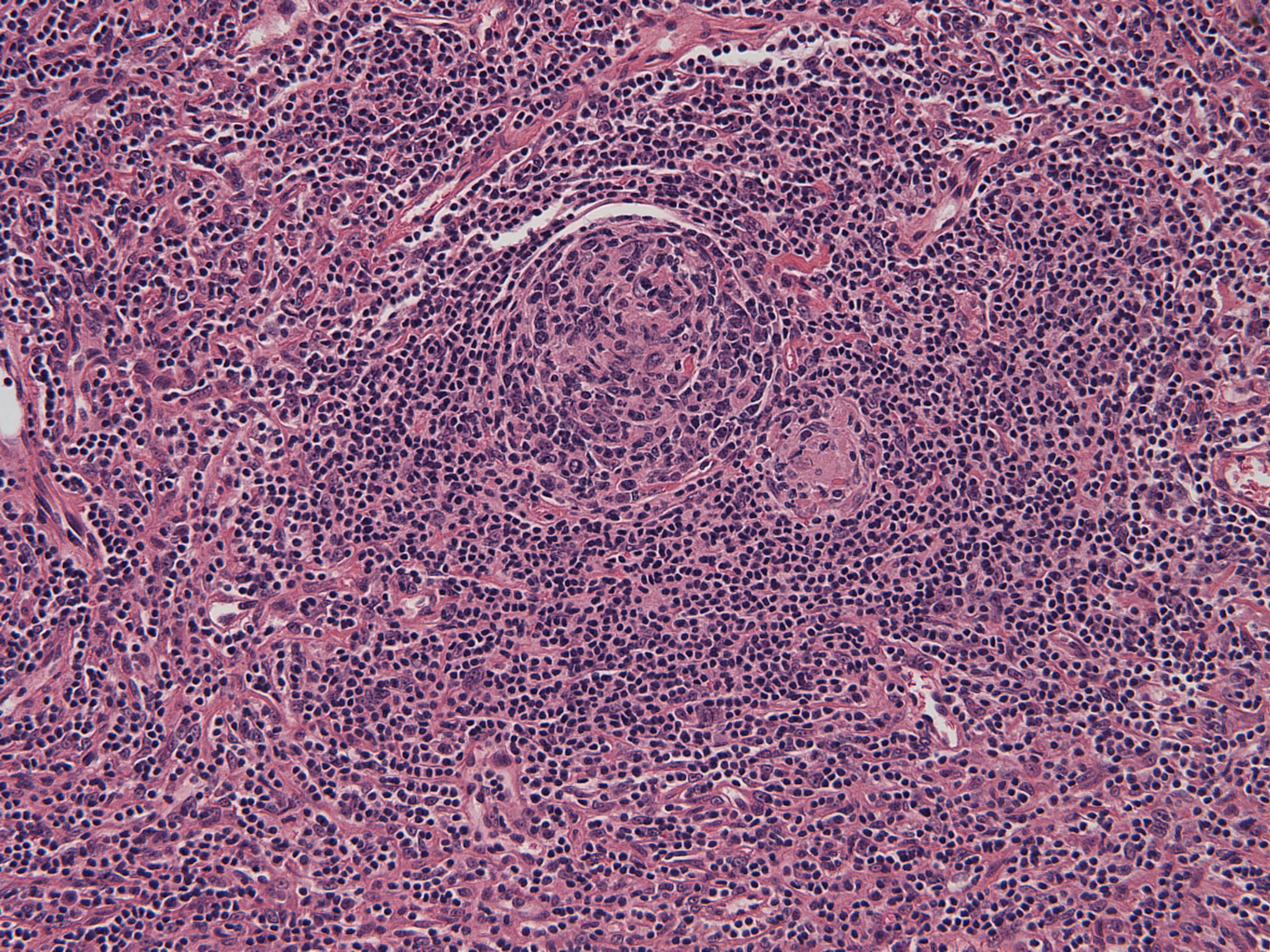
- Preservation of overall tissue architecture (Adv Anat Pathol 2013;20:137)
- Lymph nodes: benign lymphoblasts localize predominantly to interfollicular / paracortical regions
- Carcinomas: lymphoblasts are interspersed or clustered between malignant epithelial cells without definitive evidence of lymphoepithelial lesions
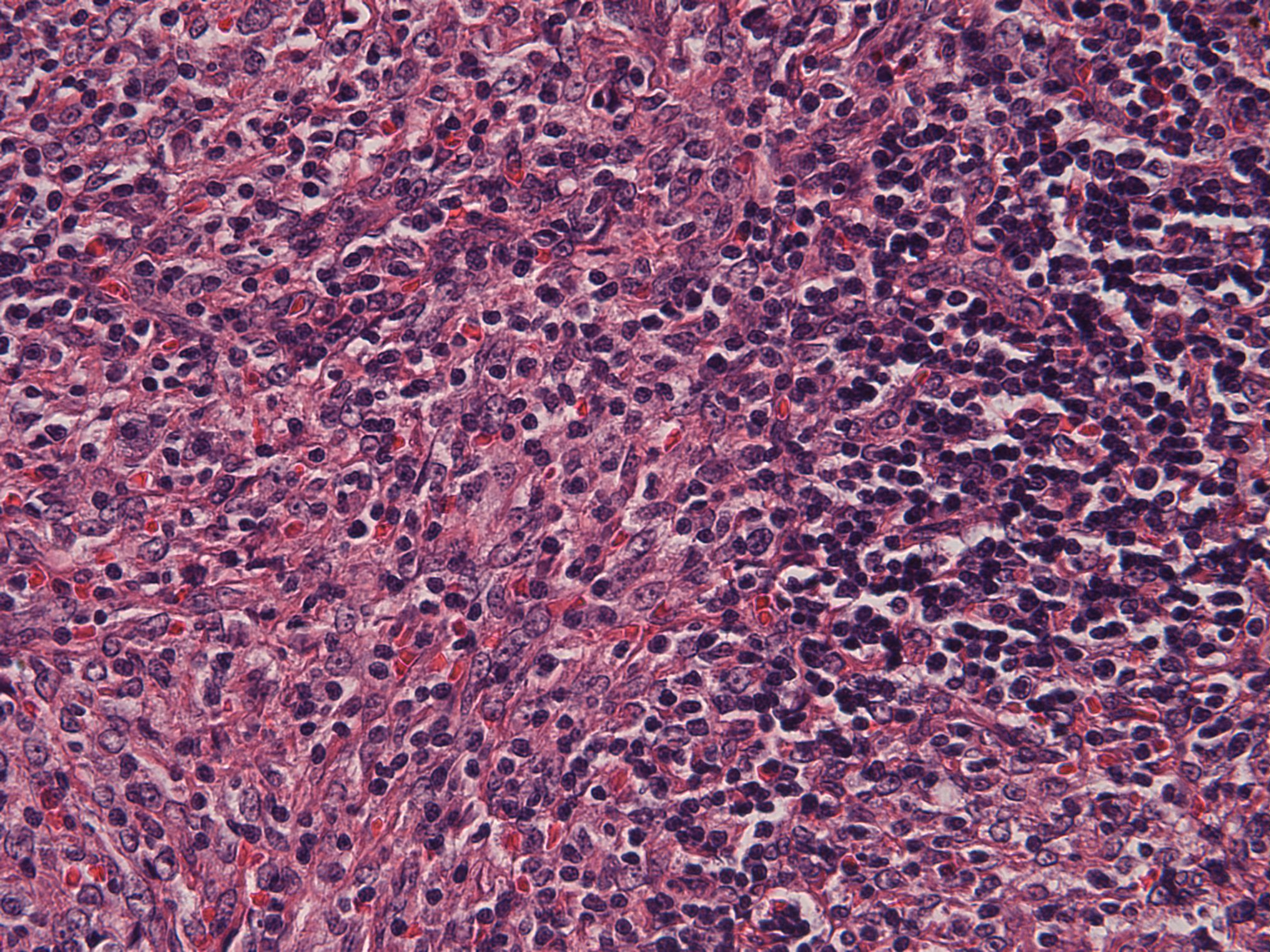
- Small to intermediate sized lymphoid cells with immature fine / blastoid chromatin lacking significant atypia
- Inconspicuous nucleoli
- Numerous mitotic figures may be present
- Histiocytes are interspersed evenly throughout the proliferation
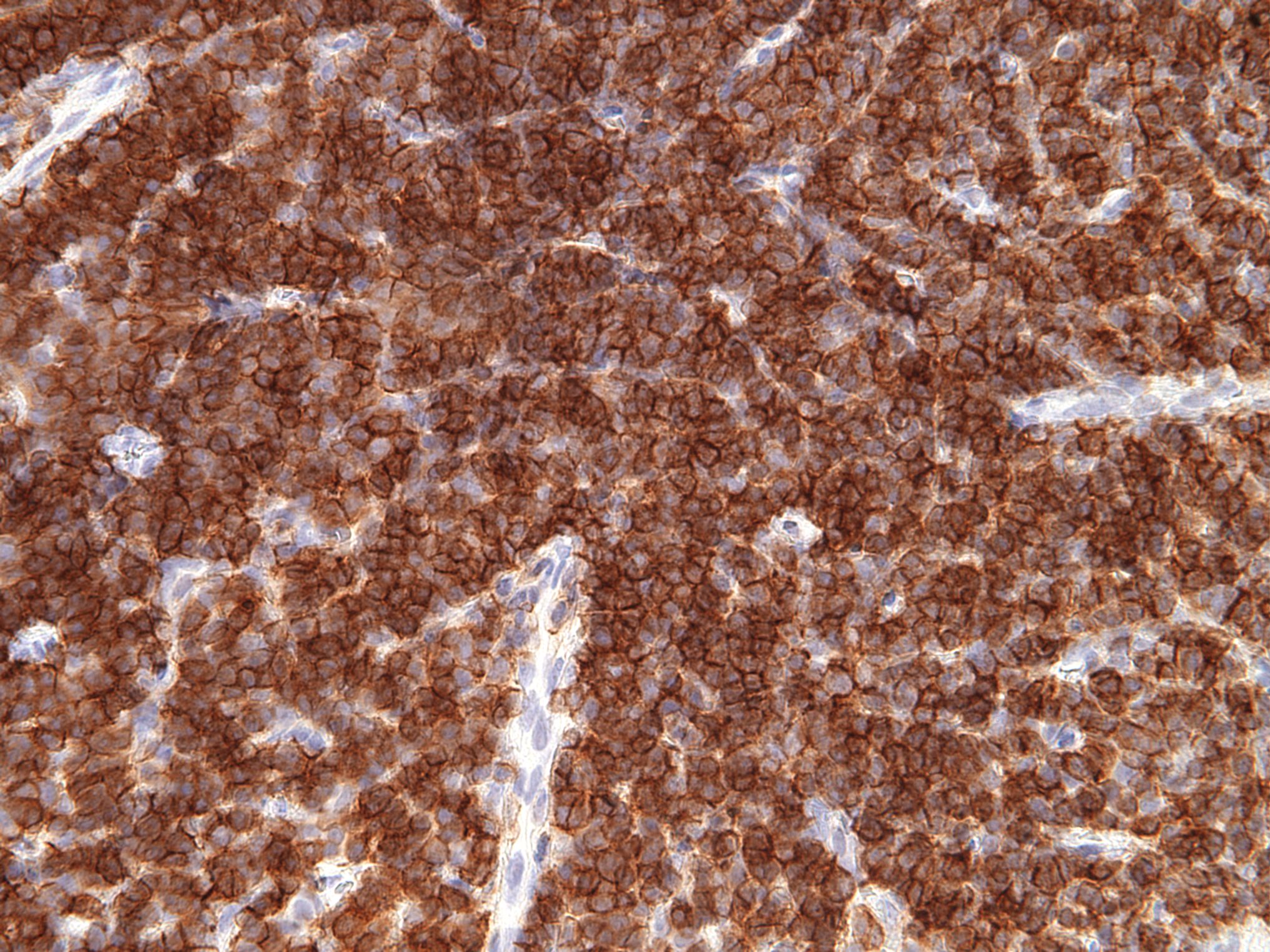
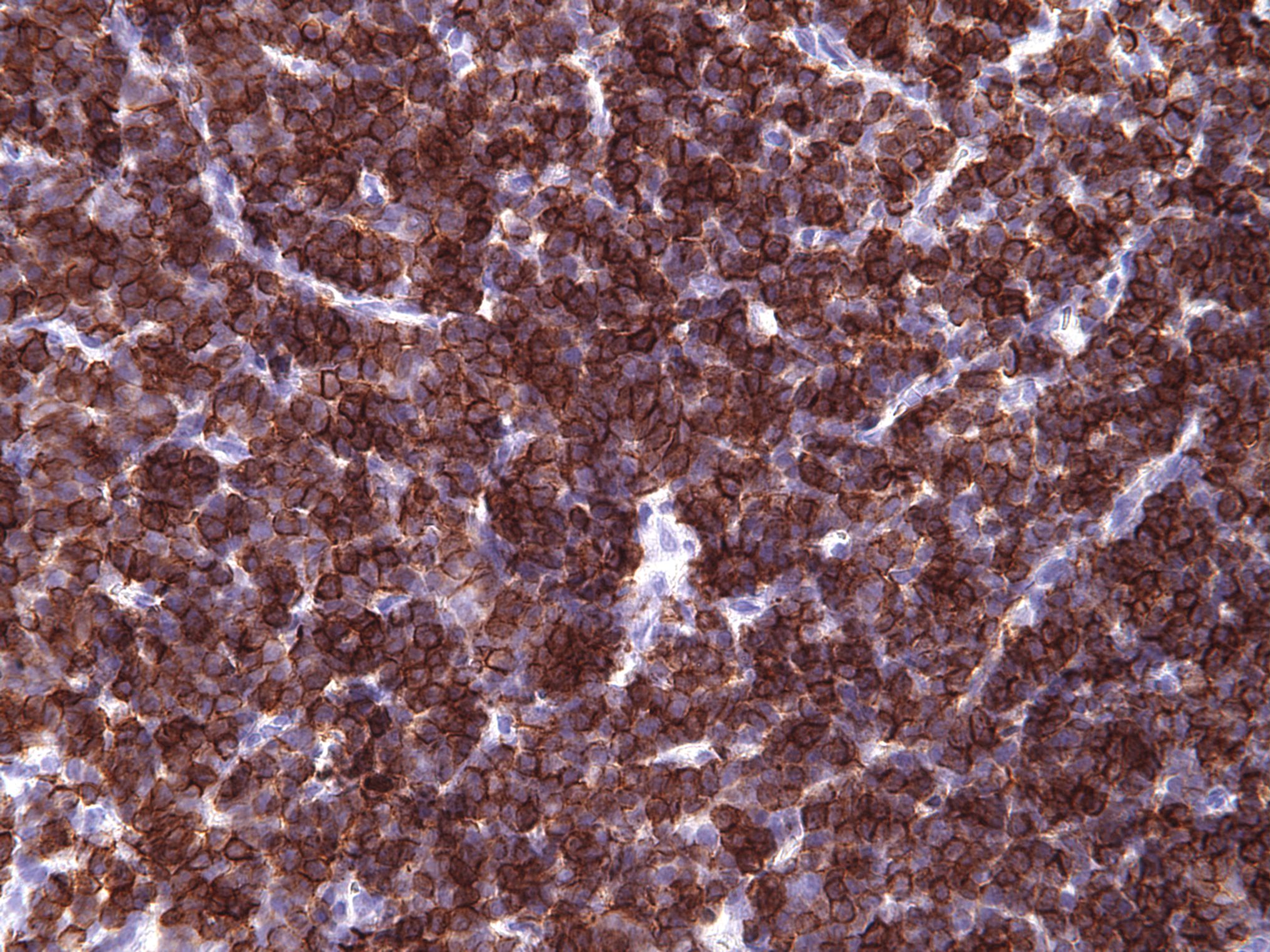
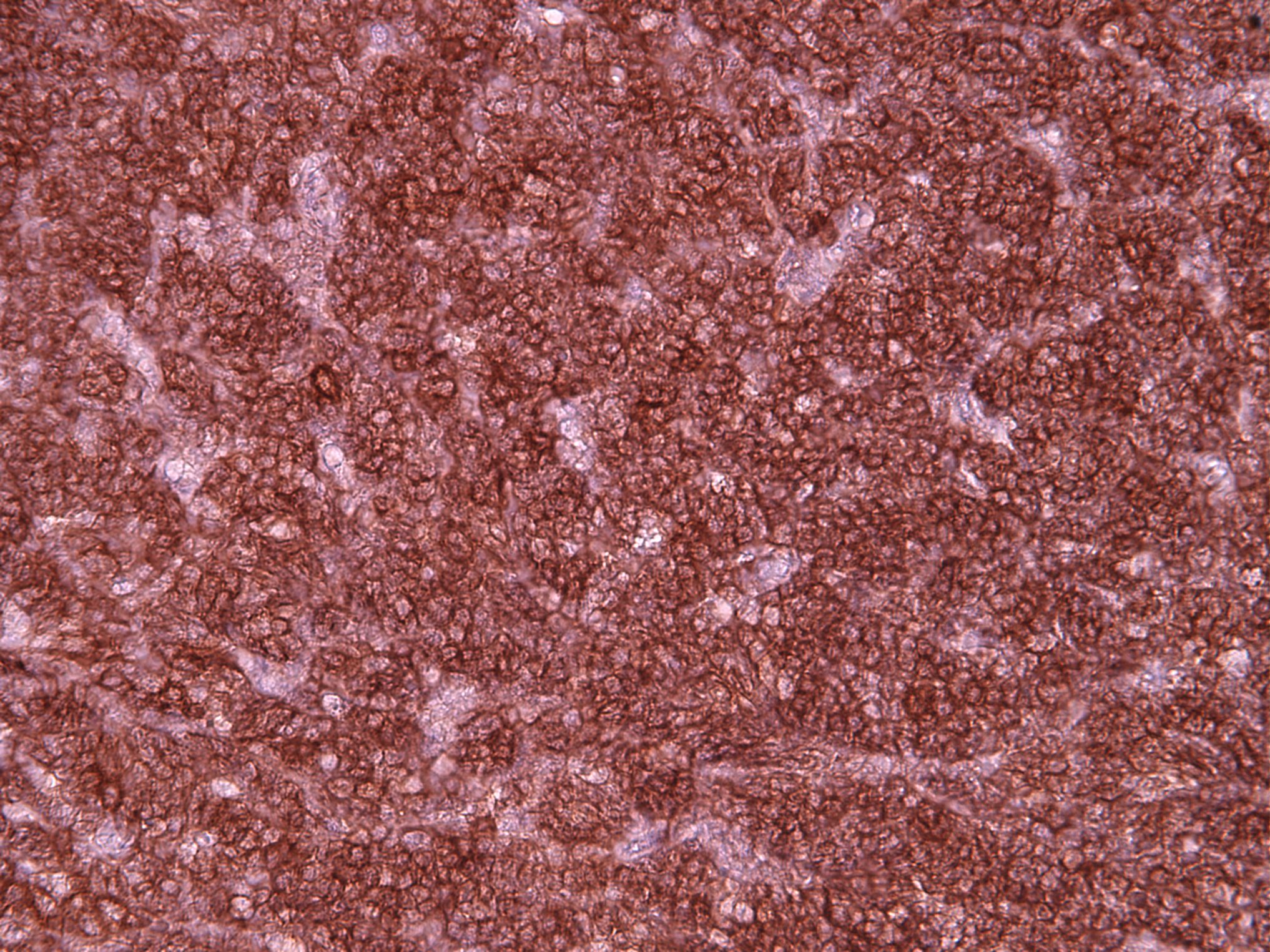
Microscopic (histologic) images
Cytology description
- Small to intermediate sized monotonous population with fine dispersed chromatin pattern and scant cytoplasm; occasional variably sized nucleoli may be present
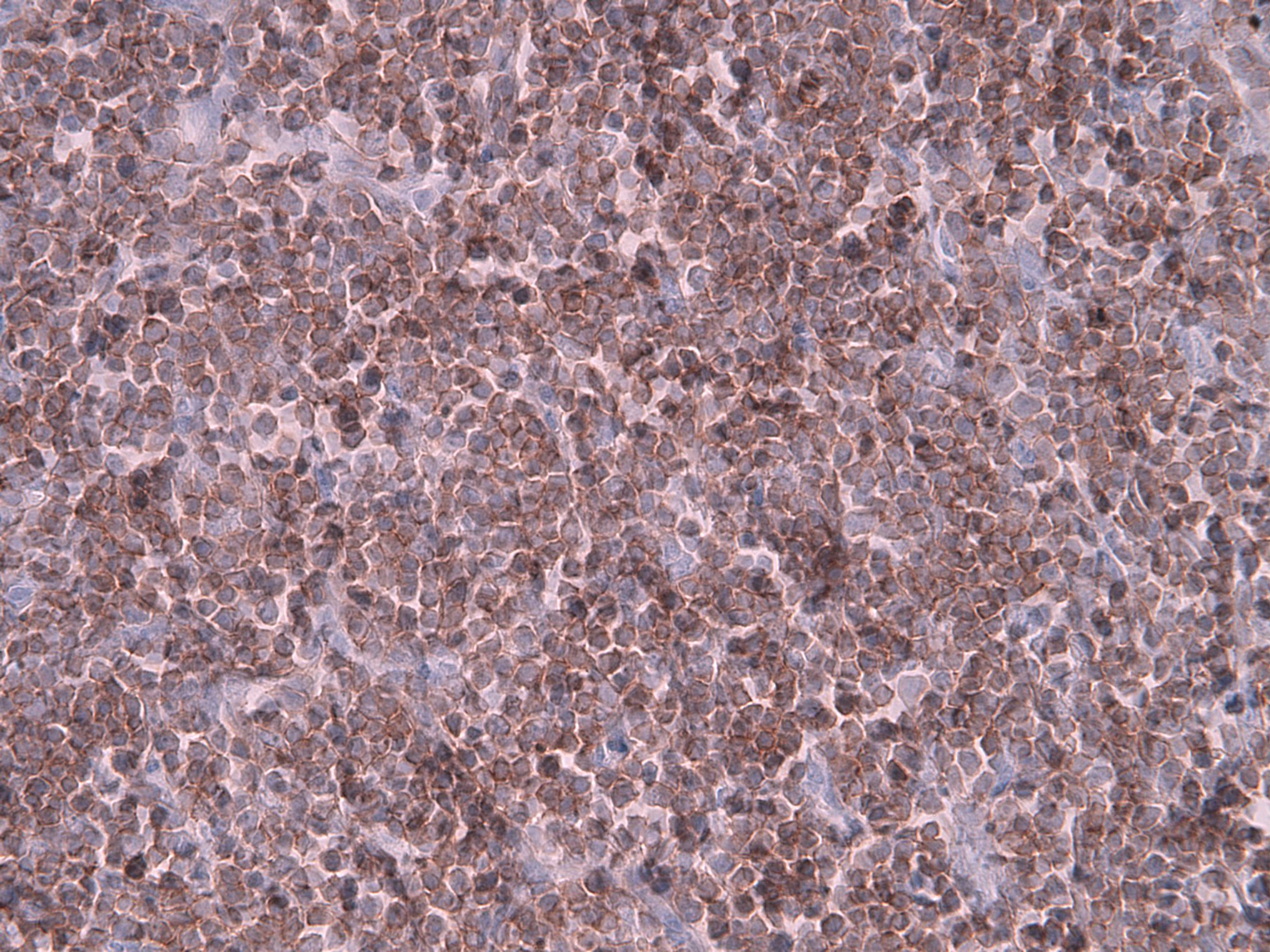
Positive stains
Flow cytometry description
- Incidental benign TdT+ T cell populations may be detected by flow cytometry
- Immunophenotype can show the entire range of T cell differentiation from the most immature dual CD4- / CD8- / CD7 bright+ / CD34+ / cytoplasmic CD3+ / surface CD3- forms to surface CD3+ forms with coexpression of CD4 and CD8 (Cytometry B Clin Cytom 2020;98:282)
- Proportion of T lymphoblasts (identified by cytoplasmic CD3 and TdT expression) can vary from < 1% of events to > 50% of events
Molecular / cytogenetics description
- iT-LBP have nonclonal T cell receptor (TCR) gene rearrangement studies (TCR γ or β)
- No definitive chromosomal abnormalities
- Initial reported case reported chromosome 9 inversion of uncertain significance (Am J Surg Pathol 1999;23:977)
Sample pathology report
- Lymph node, inguinal, excision:
- Castleman disease, hyaline vascular variant
- Indolent T lymphoblastic proliferation (see comment)
- Comment: Sections from the inguinal node show predominantly preserved nodal architecture with atretic follicles and increased vascularity with a subset of hyalinized vessels penetrating regressed germinal centers. Interspersed within the paracortical areas are increased CD3+ / TdT+ positive T cells without aberrant antigen expression. The presence of immature T cells in association with hyaline vascular Castleman disease has been reported and typically shows indolent behavior. Clinical correlation is recommended. (Am J Surg Pathol 2012;36:1619)
Differential diagnosis
- T lymphoblastic leukemia / lymphoma:
- Typically effaces nodal architecture or will infiltrate relatively nondiscriminately throughout entire node obliterating residual follicles
- Usually expresses LMO2 on malignant lymphoblasts (Histopathology 2020;77:984)
- Ectopic thymic tissue:
- Thymoma:
- Lobulated architecture
- Presence of thymic epithelial meshworks
- No expression of LMO2 on lymphoblasts
- Presence in the mediastinum
Additional references
Board review style question #1
Which of the following antigens do indolent T lymphoblastic proliferations lack?
- CD3
- CD20
- CD33
- CD45
- TdT
Board review style answer #1
B. CD20. CD20 is a B cell marker which is not expressed by T lymphoblasts. CD3 is incorrect as it is a T cell marker expressed by indolent T lymphoblastic proliferations. CD33 is a myeloid associated marker which has been described as expressed by a subset of indolent T lymphoblastic proliferations. CD45 is a pan-hematopoietic cell marker which is expressed by indolent T lymphoblastic proliferations. TdT is incorrect as it is an immature marker expressed by indolent T lymphoblastic proliferations.
Comment Here
Reference: Indolent T lymphoblastic proliferations
Comment Here
Reference: Indolent T lymphoblastic proliferations
Board review style question #2
Board review style answer #2
B. Indolent T lymphoblastic proliferation. This image shows a lymph node typical of Castleman disease. Indolent T lymphoblastic proliferations have been described in association with Castleman disease. Chronic lymphadenitis is incorrect as it is not a disease well known to occur in association with Castleman disease. Kikuchi-Fujimoto disease is incorrect as this is a necrotizing lymphadenitis of unknown etiology and association. Kimura disease is incorrect as it would show numerous eosinophils and eosinophilic granulomas and is not associated with Castleman disease. Rosai-Dorfman disease is incorrect as it shows large histiocytic cells with round to ovoid nuclei and distinct central nucleoli that exhibit emperipolesis.
Comment Here
Reference: Indolent T lymphoblastic proliferations
Comment Here
Reference: Indolent T lymphoblastic proliferations