Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Peripheral smear description | Peripheral smear images | Flow cytometry description | Flow cytometry images | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Hupp M, Courville E. B cell monoclonal lymphocytosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomaMBL.html. Accessed April 22nd, 2024.
Definition / general
- Circulating clonal B cells (< 5 x 109/L) in patients who have no other signs of a lymphoproliferative disorder
- Most common phenotype is chronic lymphocytic leukemia-like (CLL-like), though other phenotypes do exist (atypical CLL and non-CLL phenotypes) (Blood 2015;126:454)
Essential features
- Monoclonal B cell lymphocytosis (MBL): monoclonal population of B cells in the blood of < 5 x 109/L
- Asymptomatic and without extramedullary involvement
- Subtypes include CLL-like MBL, MBL with atypical CLL phenotype, MBL with non-CLL phenotype
- CLL-like subtype can be divided into low count monoclonal B cell lymphocytosis (< 0.5 x 109/L, progression to CLL is exceedingly rare) and high count monoclonal B cell lymphocytosis (> 0.5 x 109/L, progression to CLL 1 - 2% per year)
ICD coding
Epidemiology
- Prevalence: reported between < 1 - 18% (depending on assay sensitivity and populations studied)
- M:F = 1.5:1 (Blood 2014;123:1319)
- Incidence increases with age: < 1% at < 40 years to as high as 75% at > 90 years (Blood 2009;114:33)
- Possible risk factors for onset: family history of CLL, certain single nucleotide polymorphisms, infections (including hepatitis C, pneumonia, influenza, cellulitis, upper respiratory infections and herpes zoster)
- Reported lower incidence in those vaccinated for influenza or pneumonia (Blood 2015;126:454, Cytometry B Clin Cytom 2010;78:S61, PLoS One 2012;7:e52808)
Sites
- Blood
- Bone marrow: involvement is common (median of 20% of marrow cellularity composed of clonal B cells); in the absence of other criteria, the percentage of marrow infiltration does not change the diagnosis from monoclonal B cell lymphocytosis to CLL (Blood 2015;126:454)
Pathophysiology
- Proposed natural history: oligoclonal expansions of CD5+ B cells may progress to monoclonal B cell lymphocytosis, which may progress to CLL (J Exp Med 2012;209:2183)
- High count CLL-like monoclonal B cell lymphocytosis appears to be biologically similar to CLL, while low count is genetically different (based on biased usage of IGHV genes) (Leukemia 2010;24:512)
- Correlations with chronic infections suggest chronically stimulating the immune system may play a role in pathophysiology (Blood 2015;126:454)
- CLL-like monoclonal B cell lymphocytosis is considered a precursor lesion to CLL: virtually all CLLs evolve from monoclonal B cell lymphocytosis, though not all monoclonal B cell lymphocytosis cases progress to CLL (Blood 2011;118:6618)
Clinical features
- By definition, asymptomatic
- May be an incidental finding or identified in work up for lymphocytosis
Diagnosis
- Monoclonal population of B cells in the blood of < 5 x 109/L (Leukemia 2010;24:512, Blood 2015;126:454)
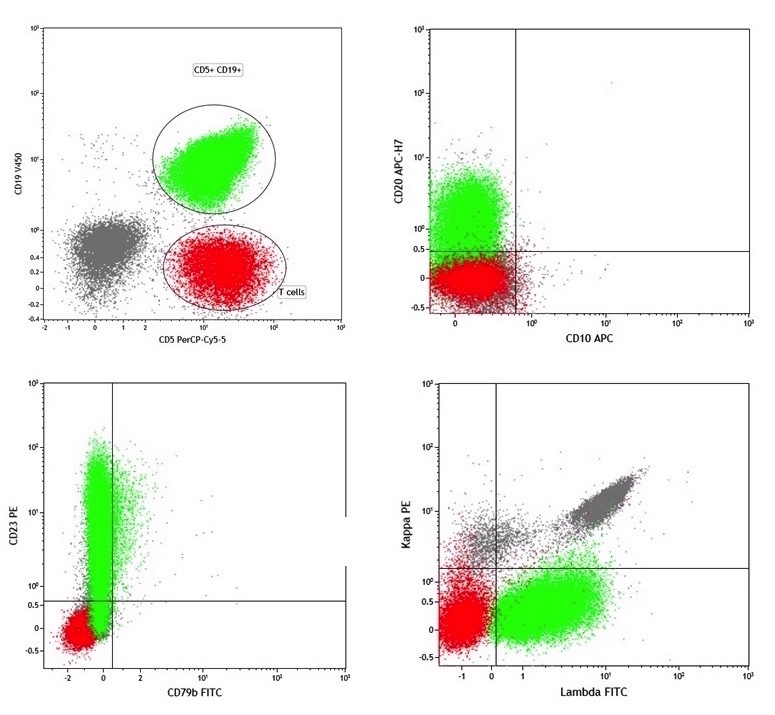
- CLL-like monoclonal B cell lymphocytosis: CD5+, CD19+, dim CD20+, CD23+, dim surface immunoglobulin (or lack surface immunoglobulin)
- Low count monoclonal B cell lymphocytosis: circulating population < 0.5 x 109/L
- High count monoclonal B cell lymphocytosis: circulating population > 0.5 x 109/L
- Monoclonal B cell lymphocytosis with atypical CLL phenotype: CD5+, CD19+, CD20+ (bright), CD23 variable, moderate to bright surface immunoglobulin
- Monoclonal B cell lymphocytosis with non-CLL phenotype: dim or negative CD5, CD19+, CD20+, moderate to bright surface immunoglobulin
- CLL-like monoclonal B cell lymphocytosis: CD5+, CD19+, dim CD20+, CD23+, dim surface immunoglobulin (or lack surface immunoglobulin)
- Asymptomatic and without lymph node, visceral or other extramedullary involvement
- No features of another B cell lymphoproliferative disorder
- While the diagnosis is based on absolute counts for clonal B cells, a standard method of determining such an absolute count does not currently exist
- One method is to use dual platform flow cytometry (using CBC parameters from the hematology instrument in conjunction with the flow cytometry percentage); however, there are numerous variables that affect the method’s accuracy and precision
- While single platform flow cytometric testing using beads or a volumetric approach can have improved accuracy and precision, the method is not widely available for leukemia / lymphoma type immunophenotyping assays (Cytometry B Clin Cytom 2021;100:142)
Prognostic factors
- Absolute monoclonal B cell count
- High count monoclonal B cell lymphocytosis shows progression to CLL at about 1 - 2% per year (Blood 2011;118:6618, Leukemia 2010;24:512)
- Low count monoclonal B cell lymphocytosis rarely has progression to CLL (Blood 2011;118:6618)
- CLL-like monoclonal B cell lymphocytosis is more likely to persist than atypical or non-CLL phenotypes (Blood 2011;118:6618)
- Mutated immunoglobulin heavy chain variable (IGHV) genes predict a longer time to first treatment and improved overall survival (Leukemia 2010;24:512)
Case reports
- 46 year old woman with subsequent CLL undergoing in vitro fertilization (Br J Haematol 2015;168:350)
- 61 year old woman with coexisting myelodysplastic syndrome (Clinics (Sao Paulo) 2012;67:1487)
- 66 year old male stem cell donor with coexisting hairy cell leukemia (Cytometry B Clin Cytom 2012;82:177)
- 69 year old man with coexisting rheumatoid arthritis on very low dose rituximab (Int J Rheum Dis 2013;16:764)
- 70 year old man with coexisting granulomatosis with polyangiitis (Chin Med J (Engl) 2016;129:2258)
Treatment
- Low count monoclonal B cell lymphocytosis: no specific clinical follow up
- High count monoclonal B cell lymphocytosis: annual complete blood count and periodic lymph node examination; no treatment (Leukemia 2010;24:512)
Microscopic (histologic) description
- A tissue equivalent of monoclonal B cell lymphocytosis has been described (Arch Pathol Lab Med 2021;145:1544, Haematologica 2011;96:1144)
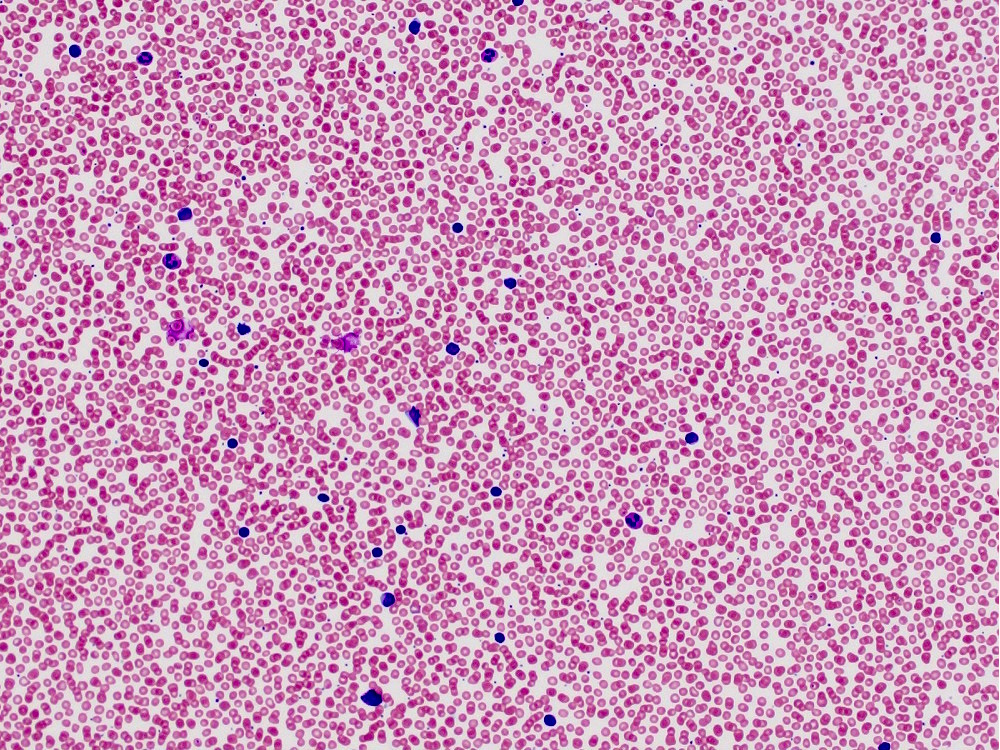
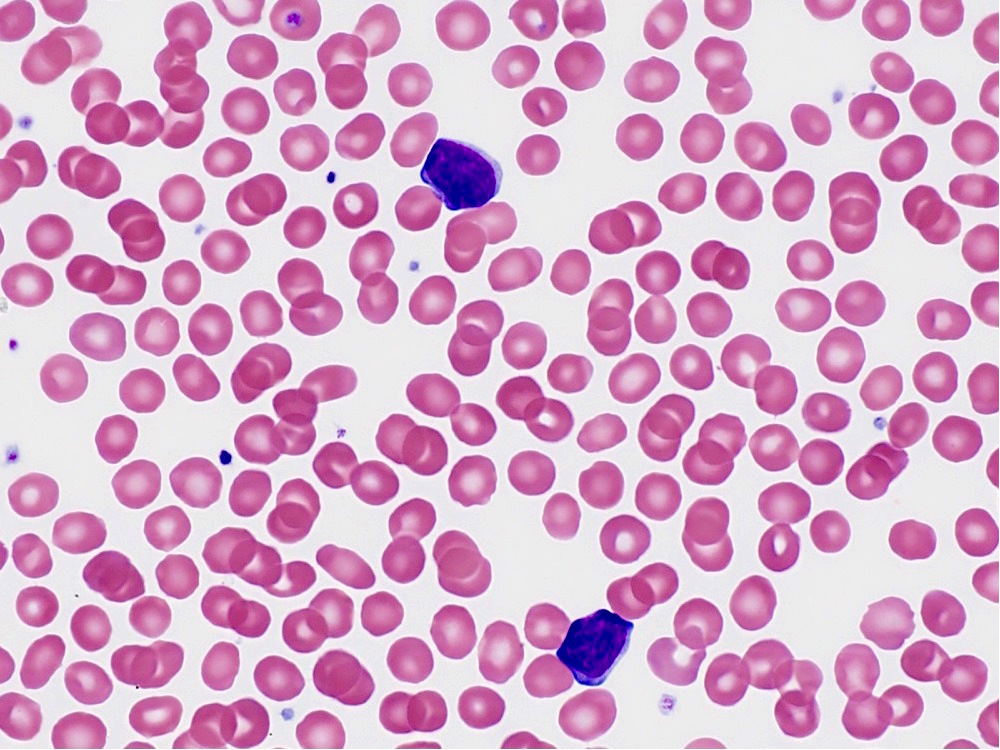
Peripheral smear description
- May or may not see an atypical lymphocyte population, depending on the number of monoclonal B cells
Peripheral smear images
Flow cytometry description
- CLL-like monoclonal B cell lymphocytosis:
- Monoclonal B cell lymphocytosis with atypical CLL phenotype:
- Positive CD5, CD19, CD20 (bright)
- Moderate to bright monotypic surface light chains
- Variable CD23 expression
- Monoclonal B cell lymphocytosis with non-CLL phenotype:
- Positive CD19 and CD20 (bright)
- Moderate to bright monotypic surface light chains
- Dim or negative CD5
- Reference: Blood 2015;126:454
Molecular / cytogenetics description
- Majority of CLL-like monoclonal B cell lymphocytosis cases have mutated IGHV genes (up to 90% in high count)
- CLL-like monoclonal B cell lymphocytosis cases can have similar cytogenetic alterations to that of CLL, although at different frequencies (Br J Haematol 2012;157:86)
- Genetic abnormalities frequently identified in chronic lymphocytic leukemia (deletion of the long arm of chromosome 13, deletion of the long arm of chromosome 11, deletion of the short arm of chromosome 17 and the presence of trisomy 12) are also seen in monoclonal B cell lymphocytosis
- In low count MBL, deletions of chromosome 13 long arm (deletion 13q) were most frequently identified (Blood 2011;118:6618)
- In contrast, by FISH, it appears that the distribution of genetic abnormalities in high count MBL is comparable to that of CLL (Blood 2015;126:454)
- Elucidation of underlying genetic differences between MBL and CLL is an area of active investigation (Semin Oncol 2016;43:201)
Sample pathology report
- Peripheral blood, flow cytometry:
- CD5 positive, kappa monotypic B cell population (see comment)
- Comment: This immunophenotypic assay identified a monotypic B cell population with a chronic lymphocytic leukemia / small lymphocytic lymphoma (CLL / SLL)-like immunophenotype. The main differential lies between CLL / SLL and monoclonal B cell lymphocytosis with a CLL-like immunophenotype. The monotypic B cell population comprises an estimated 10% of the total lymphocytes. Clinical correlation is recommended, including evaluation for lymphadenopathy / organomegaly.
Differential diagnosis
- Chronic lymphocytic leukemia:
- Monoclonal population absolute count will differentiate CLL from CLL-like monoclonal B cell lymphocytosis (≥ and < 5 x 109/L, respectively); the characteristic morphology and phenotype of CLL should be seen as well to make a CLL diagnosis
- Of note, some patients have counts that oscillate between monoclonal B cell lymphocytosis and CLL for some time
- Monoclonal population absolute count will differentiate CLL from CLL-like monoclonal B cell lymphocytosis (≥ and < 5 x 109/L, respectively); the characteristic morphology and phenotype of CLL should be seen as well to make a CLL diagnosis
- Small lymphocytic lymphoma with minimal peripheral blood involvement:
- Physical exam and imaging with or without biopsy to rule out extramedullary disease
-
Mantle cell lymphoma with peripheral blood involvement:
- Especially important to rule out in monoclonal B cell lymphocytosis with atypical CLL phenotype; the presence of t(11;14) may help distinguish
- Other small B cell lymphoma with low level peripheral blood involvement (particularly monoclonal B cell lymphocytosis with non-CLL phenotype or atypical CLL phenotype):
- Some cases of monoclonal B cell lymphocytosis with non-CLL phenotype have 7q aberrations and develop splenomegaly, suggesting a connection with splenic marginal zone lymphoma (Blood 2014;123:1199)
- Reactive (polyclonal) lymphocytosis:
- May be in the differential prior to flow cytometry evaluation
Additional references
Board review style question #1
A 65 year old woman has a flow cytometry study performed for lymphocytosis. She has a white blood cell count of 9.1 x 109/L with 58% lymphocytes. By flow cytometric immunophenotyping, a monoclonal B cell population is identified comprising 30% of leukocytes (absolute count of 2.73 x 109/L) with the following immunophenotype: CD5+, CD19+, CD20+ (moderate to bright), CD23 negative and moderate monotypic surface kappa light chain expression. Which of the following would be most helpful in establishing a diagnosis?
- Erythrocyte sedimentation rate and C reactive protein levels
- Fluorescence in situ hybridization to evaluate for t(11;14)
- Lumbar puncture with cell count
- Whole genome sequencing
Board review style answer #1
B. Fluorescence in situ hybridization. The patient has a CD5+ B cell clone with an absolute count of 2.73 x 109/L. The differential includes monoclonal B cell lymphocytosis with atypical CLL phenotype and mantle cell lymphoma with peripheral blood involvement. FISH for t(11;14) would assist in differentiating these 2 entities.
Comment Here
Reference: B cell monoclonal lymphocytosis
Comment Here
Reference: B cell monoclonal lymphocytosis
Board review style question #2
Which of the following is true regarding CLL-like monoclonal B cell lymphocytosis?
- It always progresses to chronic lymphocytic leukemia (CLL)
- It is associated with significant lymphadenopathy
- It is divided into low count and high count based on the absolute monoclonal B cell count
- The incidence decreases with age
Board review style answer #2
C. It is divided into low count and high count based on the absolute monoclonal B cell count
Comment Here
Reference: B cell monoclonal lymphocytosis
Comment Here
Reference: B cell monoclonal lymphocytosis