Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Gross description | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Peripheral smear description | Peripheral smear images | Positive stains | Negative stains | Flow cytometry description | Flow cytometry images | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Khanlari M, Ok CY. MCL-classic. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomaMCL.html. Accessed April 25th, 2024.
Definition / general
- Clinically aggressive, mature B cell lymphoma
- Small to medium sized lymphoid cells (monomorphic, except in pleomorphic variant)
Essential features
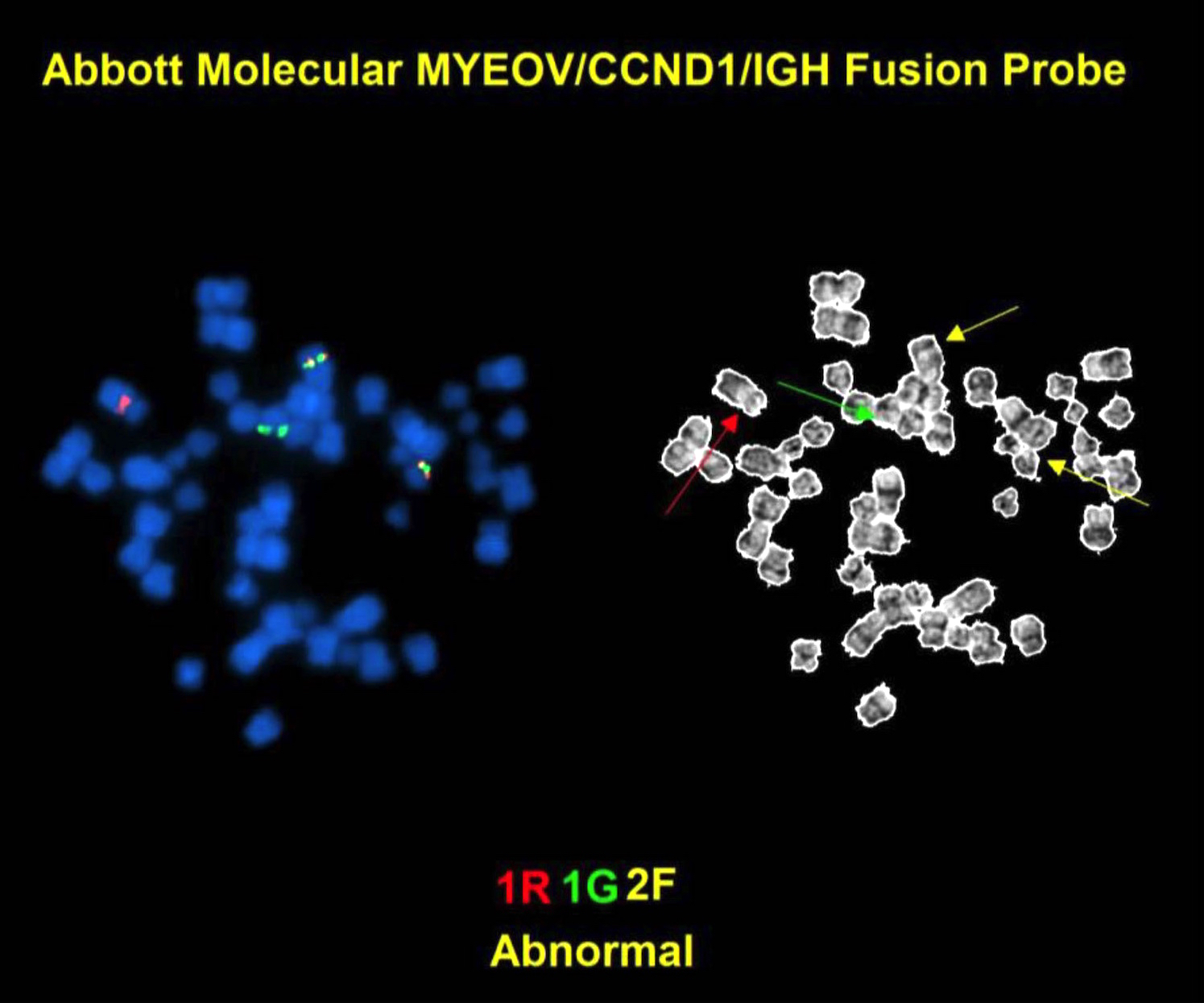
- Associated with t(11;14)(q13;q32) or IGH/CCND1 and cyclin D1 overexpression
Terminology
- Obsolete names:
- Centrocytic lymphoma (Br J Cancer Suppl 1975;2:29)
- Lymphocytic lymphoma of intermediate differentiation (Semin Diagn Pathol 2011;28:245)
- Mantle zone lymphoma (Cancer 1982;49:1429)
Epidemiology
- 7% of B cell lymphomas (Blood 1997;89:3909)
- ~10% of non-Hodgkin lymphomas
- Age adjusted incidence: 0.6/100,000 person years
- Median age: 68 years
- M:F = 2 - 3:1
Sites
- Lymph node, bone marrow (50 - 90%), peripheral blood (20 - 70%), spleen (50%), liver (20%) (Am J Clin Pathol 1996;106:196, Am J Clin Pathol 1997;108:302)
- Frequent extranodal site involvement : gastrointestinal tract, Waldeyer ring, lungs, pleura, skin, CNS
- Extranodal involvement without lymphadenopathies: 4 - 15%
Pathophysiology
- Virtually all mantle cell lymphomas have t(11;14) IGH/CCND1
- Promotes G1 to S phase progression during cell cycle
- References: Blood 2010;116:953, Kumar: Robbins and Cotran Pathologic Basis of Disease, 9th edition, 2014
Etiology
- Pregerminal center origin (SOX11+, unmutated IGHV)
- Postgerminal center origin, a subset (SOX11-, hypermutated IGHV)
- Reference: Cancer Res 2012;72:5307
Clinical features
- 70%: stage IV disease (at presentation)
- Two subtypes:
- One more aggressive with SOX11+, nodal presentation
- One more indolent with SOX11- disease, leukemic presentation, and non-nodal disease
- Generalized lymphadenopathies
- Hepatomegaly / splenomegaly
- Peripheral blood:
- Atypical lymphoid cells: present virtually in all cases by flow cytometry (Cancer 2007;109:2473)
- Leukemic involvement at diagnosis: 20 - 70% of patients
- Multiple intestinal polyps (lymphomatous polyposis)
- Progress to blastoid / pleomorphic variant
- In relapse (22%)
Diagnosis
- Tissue biopsy (lymph node / extranodal sites): monomorphic proliferation of small to intermediate sized B cells with overexpression of cyclin D1 or SOX11
- t(11;14)(q13;q32) IGH/CCND1
- Reference: Cancer Res 2012;72:5307
Laboratory
- Anemia and thrombocytopenia: 10 - 40%
- High LDH and β2 microglobulin: 50%
- A monoclonal serum component (low level): 10 - 30%
- Atypical lymphocytosis
- Reference: Cancer 1998;82:567
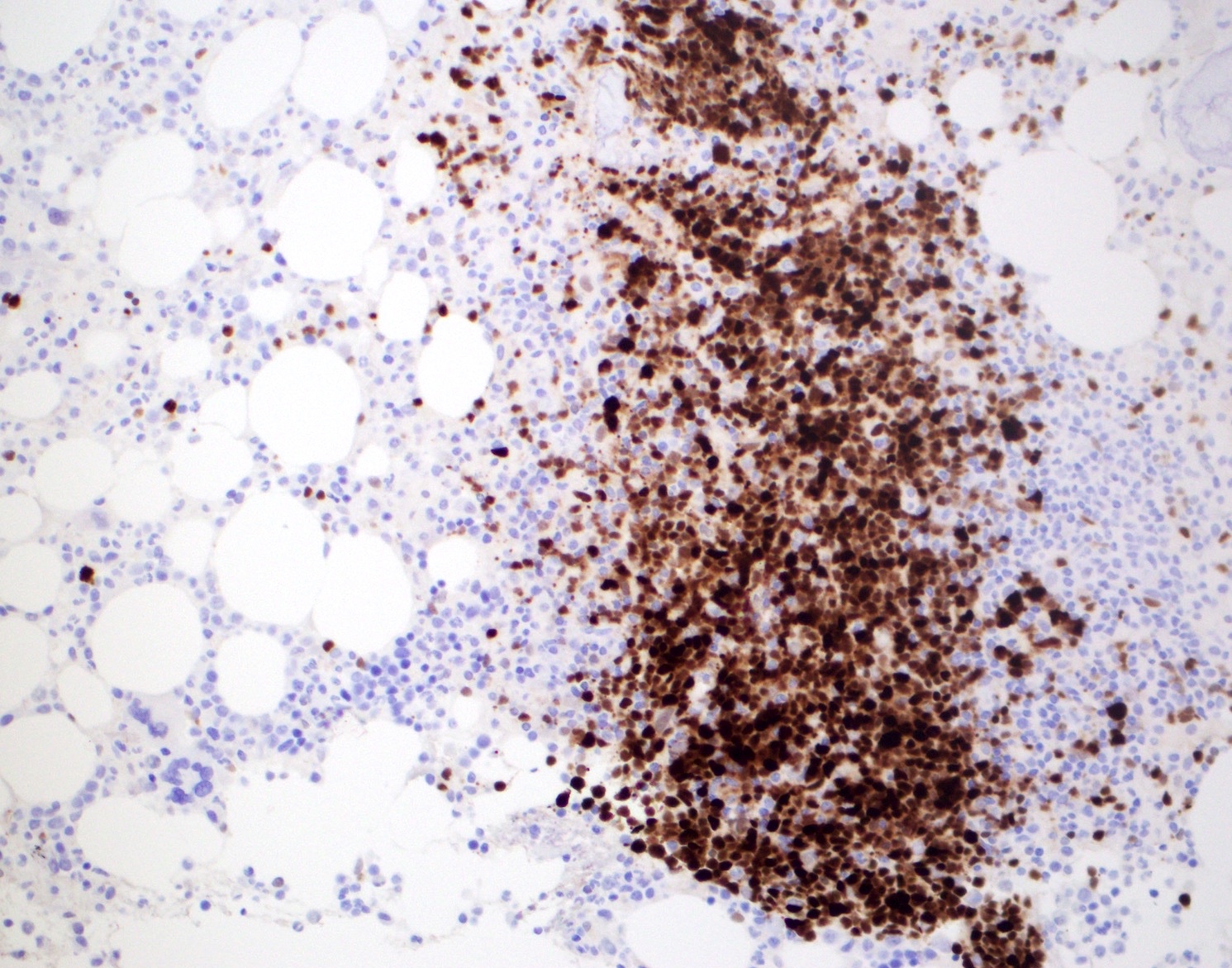
Prognostic factors
- Median survival: 5 - 7 years
- Mantle cell lymphoma international prognostic index (clinical) (Blood 2008 Jan;111:558)
- Age, performance status, lactate dehydrogenase, leukocyte count
- 3 morphologic groups with significantly different prognoses
- Adverse outcome (histopathology / molecular)
- High mitotic rate (> 50/mm2) (Br J Haematol 2005;131:29)
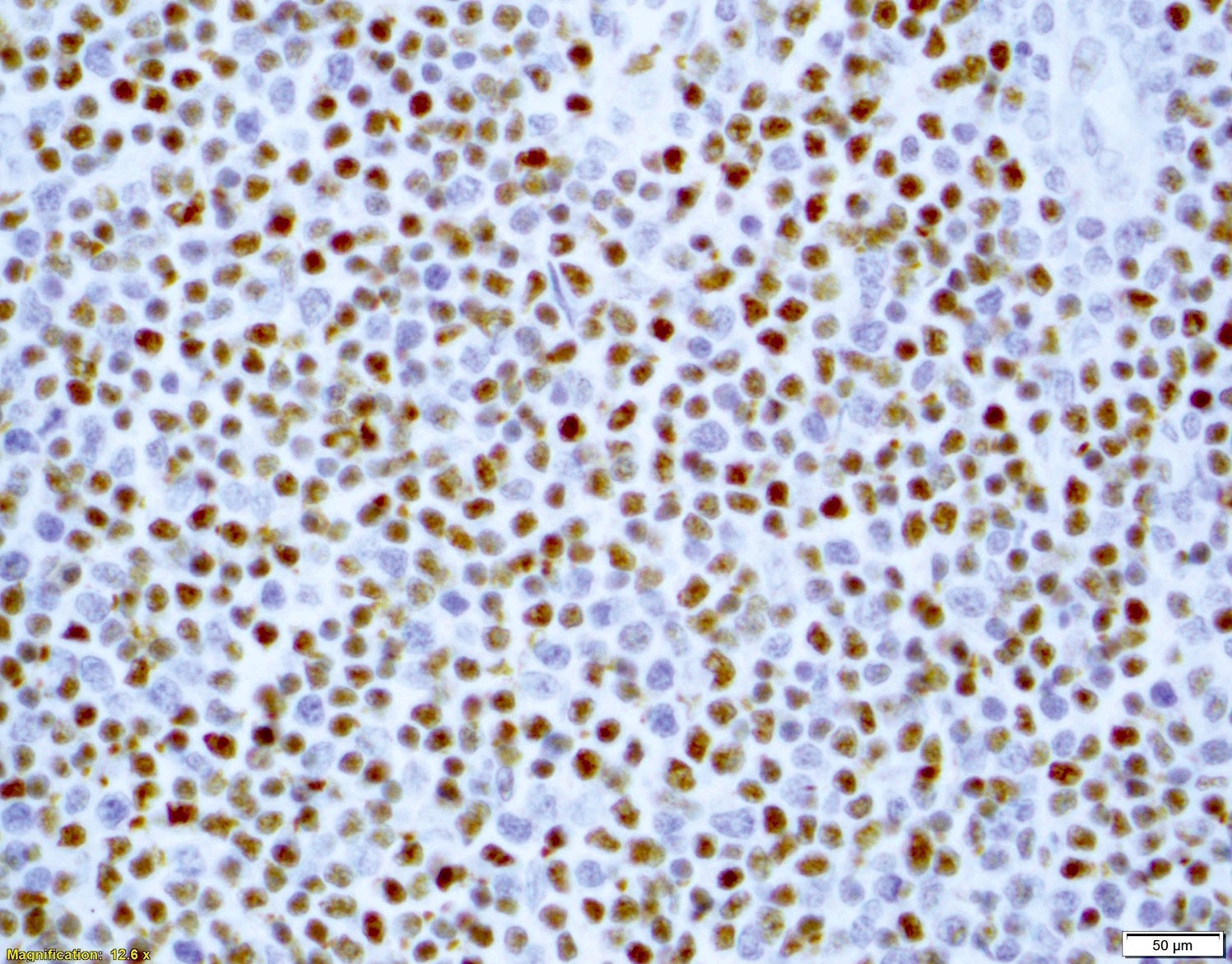
- Ki67 or MIB1 IHC stains (> 30%) (Histopathology 2013;62:334)
- Blastoid and pleomorphic variants (See Mantle cell lymphoma (MCL), aggressive variants)
- MYC rearrangement (Am J Surg Pathol 2017;41:216)
- TP53 mutation / overexpression / loss (17p) (Blood 2015;126:604)
- CDKN2A deletion (9p) (Blood 2015;126:604)
- Gains in 3q, deletions of 9q (J Clin Oncol. 2007;25:1216)
Case reports
- 60 year old man with mantle cell lymphoma involving the prostate with features of granulomatous prostatitis (Int J Surg Pathol 2012;20:610)
- 63 year old man with Hodgkin and Reed-Sternberg cells in a recurrent mantle cell lymphoma (Appl Immunohistochem Mol Morphol 2019;27:8)
- 64 year old man with right conjunctival mass as an initial presentation of mantle cell lymphoma (BMC Res Notes 2012;5:671)
- 69 year old man with a history of systemic nodal mantle cell lymphoma who presented with subcutaneous nodules on his lower extremities (J Cutan Pathol 2019;46:538)
- A case of mantle cell lymphoma showing cyclin D1 overexpression by immunohistochemistry and a t(11;12)(q13;p11.2) by conventional cytogenetic studies (Hum Pathol 2017;64:207)
Treatment
- Fit for high dose therapy
- Hyper CVAD chemotherapy or R-DHAP / R-CHOP with autologous stem cell transplantation
- Fit for conventional dose therapy
- Rituximab (R)-CHOP or R-bendamustine
- Unfit for conventional dose therapy
- R-bendamustine or R-lenalidomide
- Indolent disease (low risk)
- Watch and wait
- New biologic agents
- Ibrutinib (Bruton tyrosine kinase inhibitor)
- Idelalisib (phosphoinositide-3 kinase inhibitor)
- Bortezomib (proteasome inhibitors)
- Temsirolimus (mTOR inhibitors)
- Lenalidomide (immunomodulatory)
- References: F1000Res 2018;7:1136, Best Pract Res Clin Haematol 2018;31:99
Gross description
- Lymph node
- Generalized enlargement
- Homogenous tan cut surface
- With or without nodules
- Not distinctive
- Spleen
- Generalized micronodular pattern
- Perivascular infiltration
- GI
- Lymphomatoid polyposis
- Multiple lymphoid polyps, small and large bowel
- Ulcers, tumor masses and diffuse thickening of the mucosa (Histopathology 1995;26:413)
- Note: Microscopic infiltration without gross lesion is common (Cancer 2003;97:586)
Frozen section description
- Same criteria applied in microscopic evaluation
- Cytogenetics, flow cytometry, preparation of imprints should be considered
- The nuclear shape, size and chromatin structure are helpful in smears
- Reference: Jaffe: Hematopathology, 2nd Edition, 2016
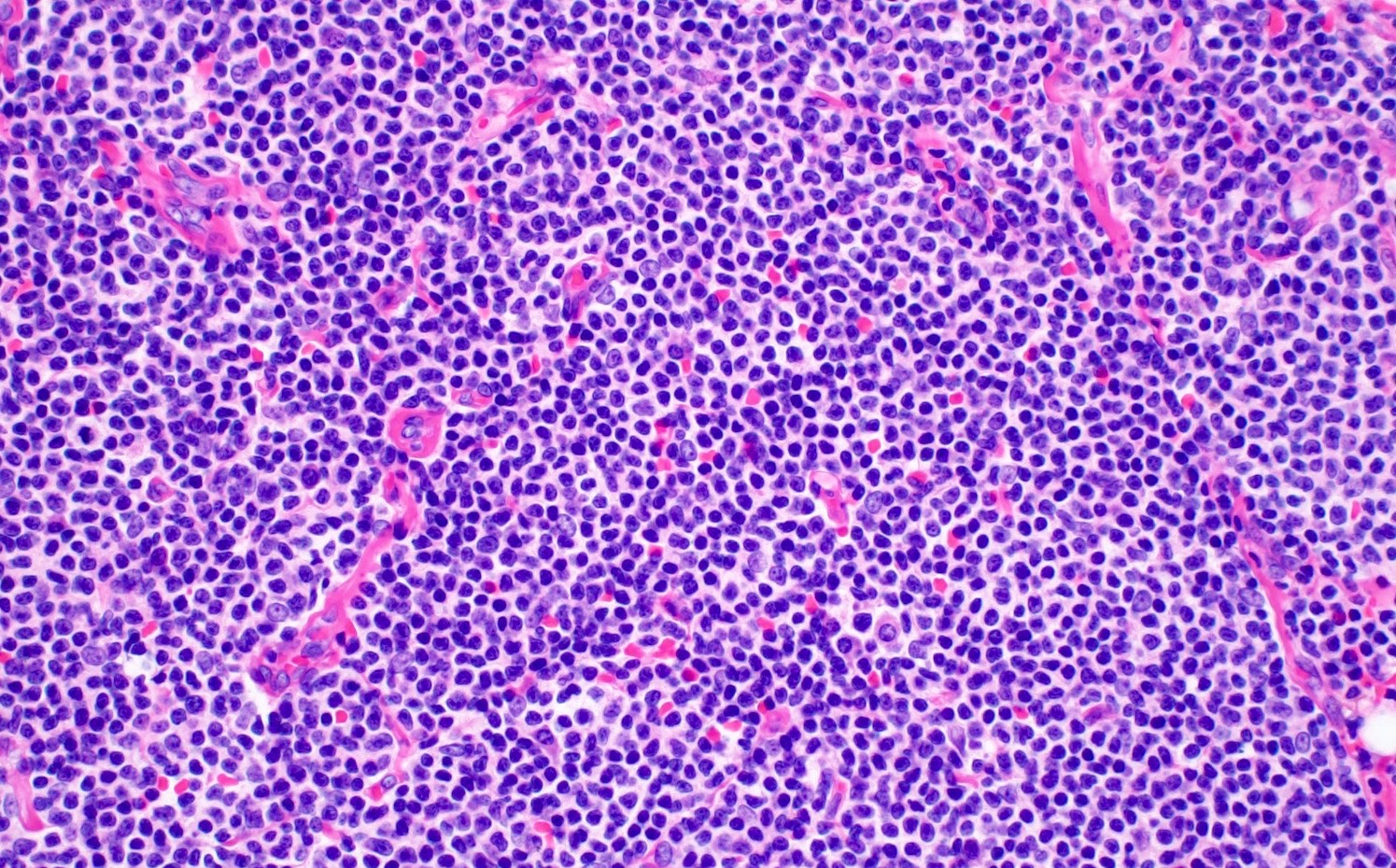
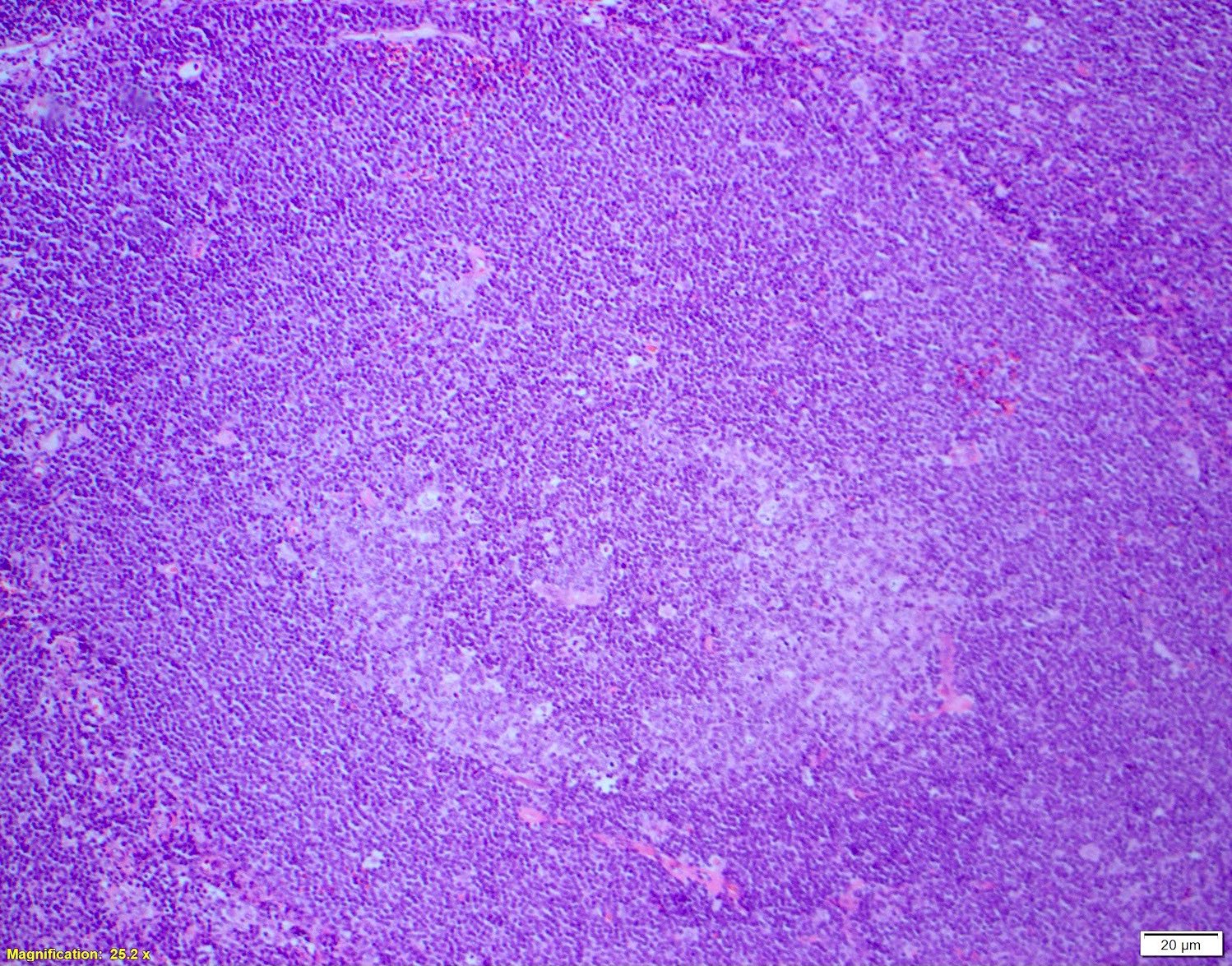
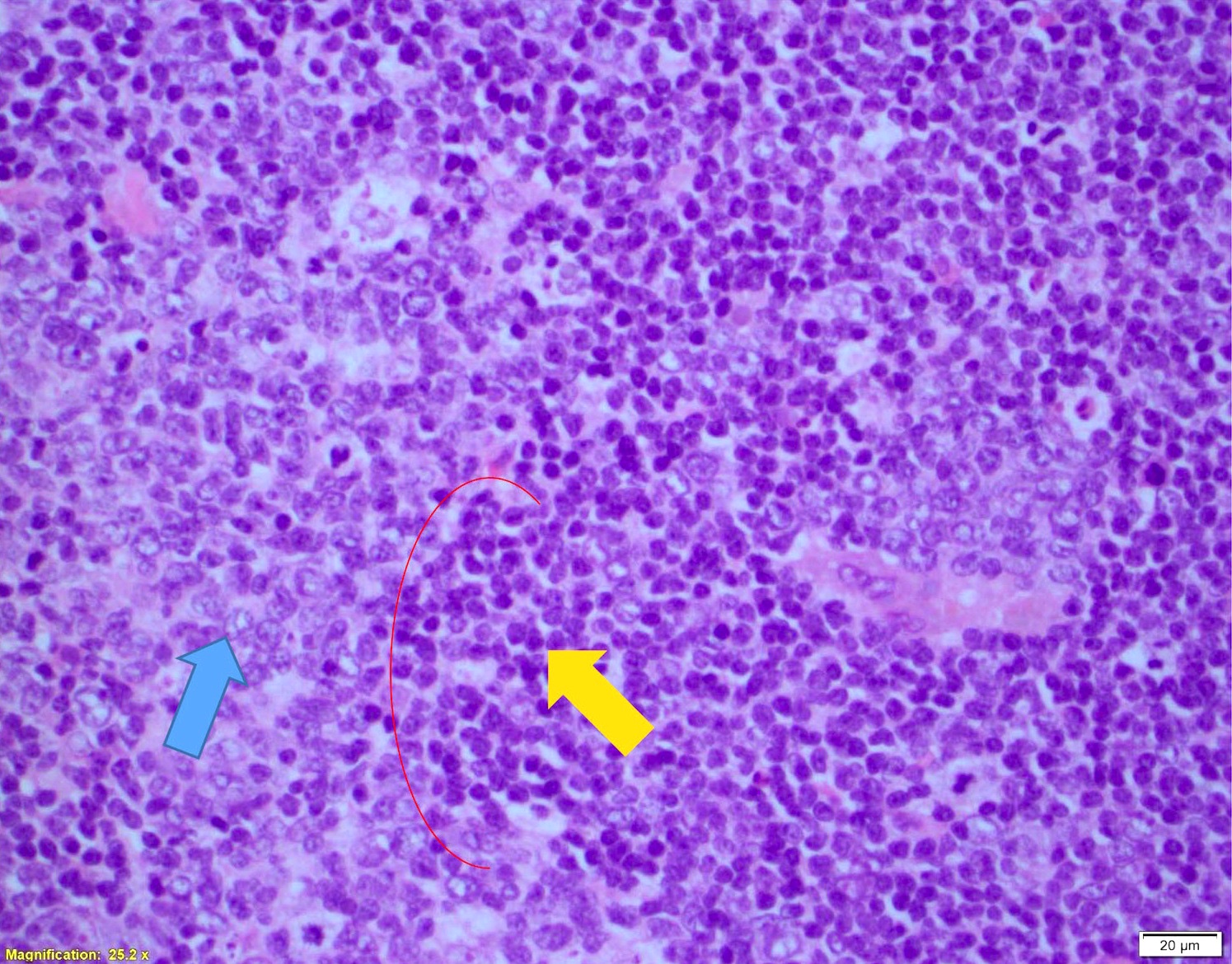
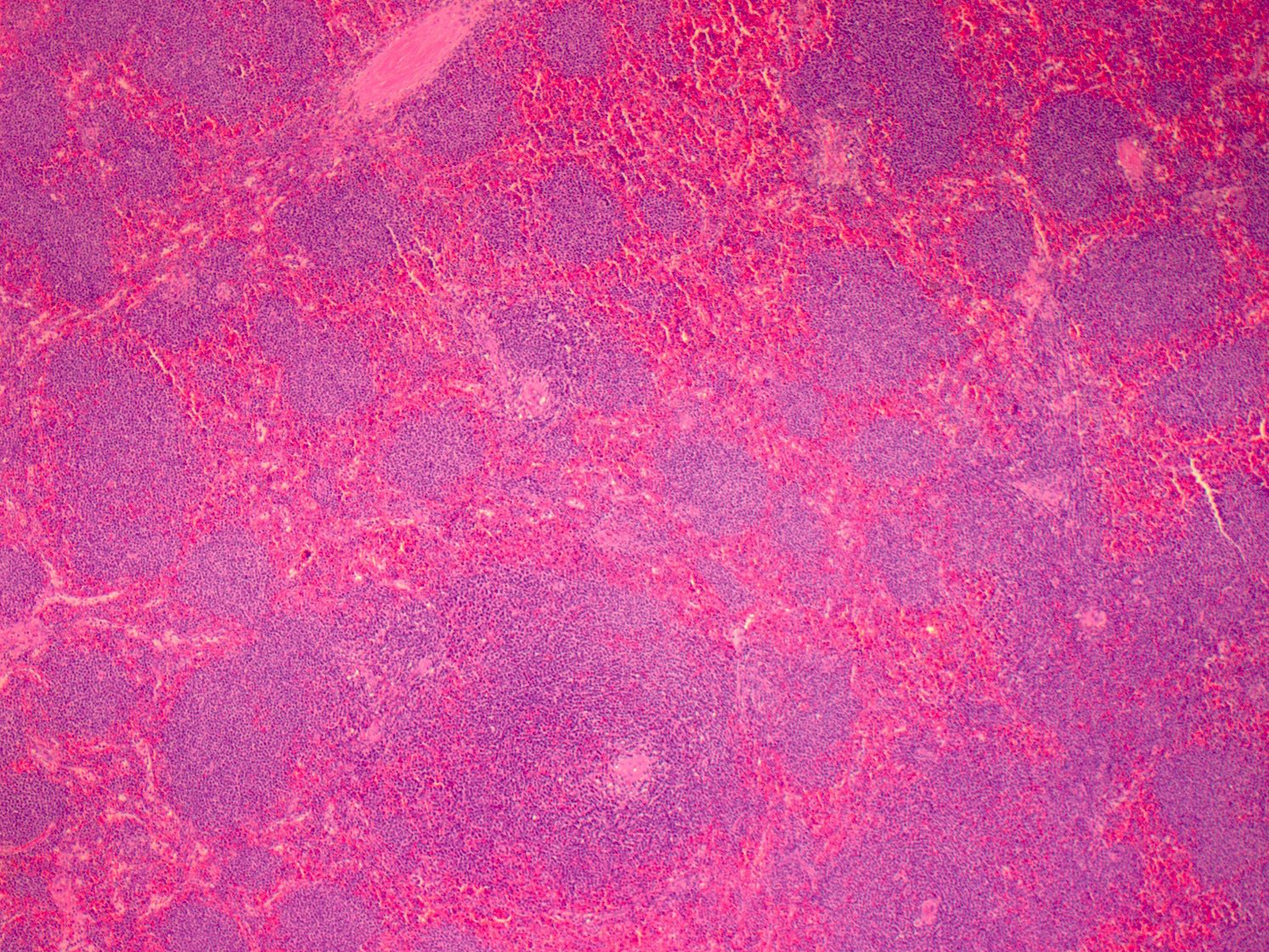
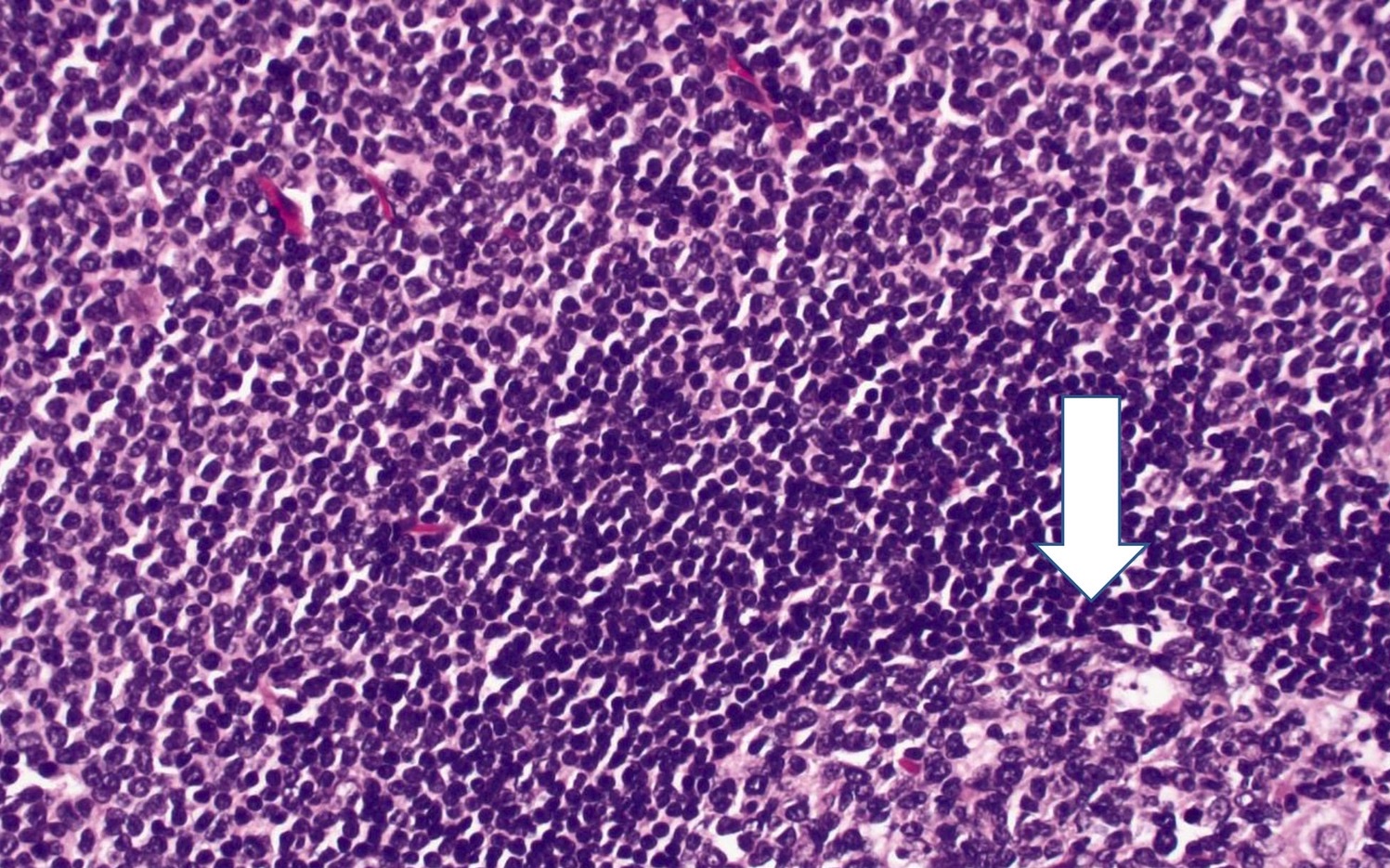
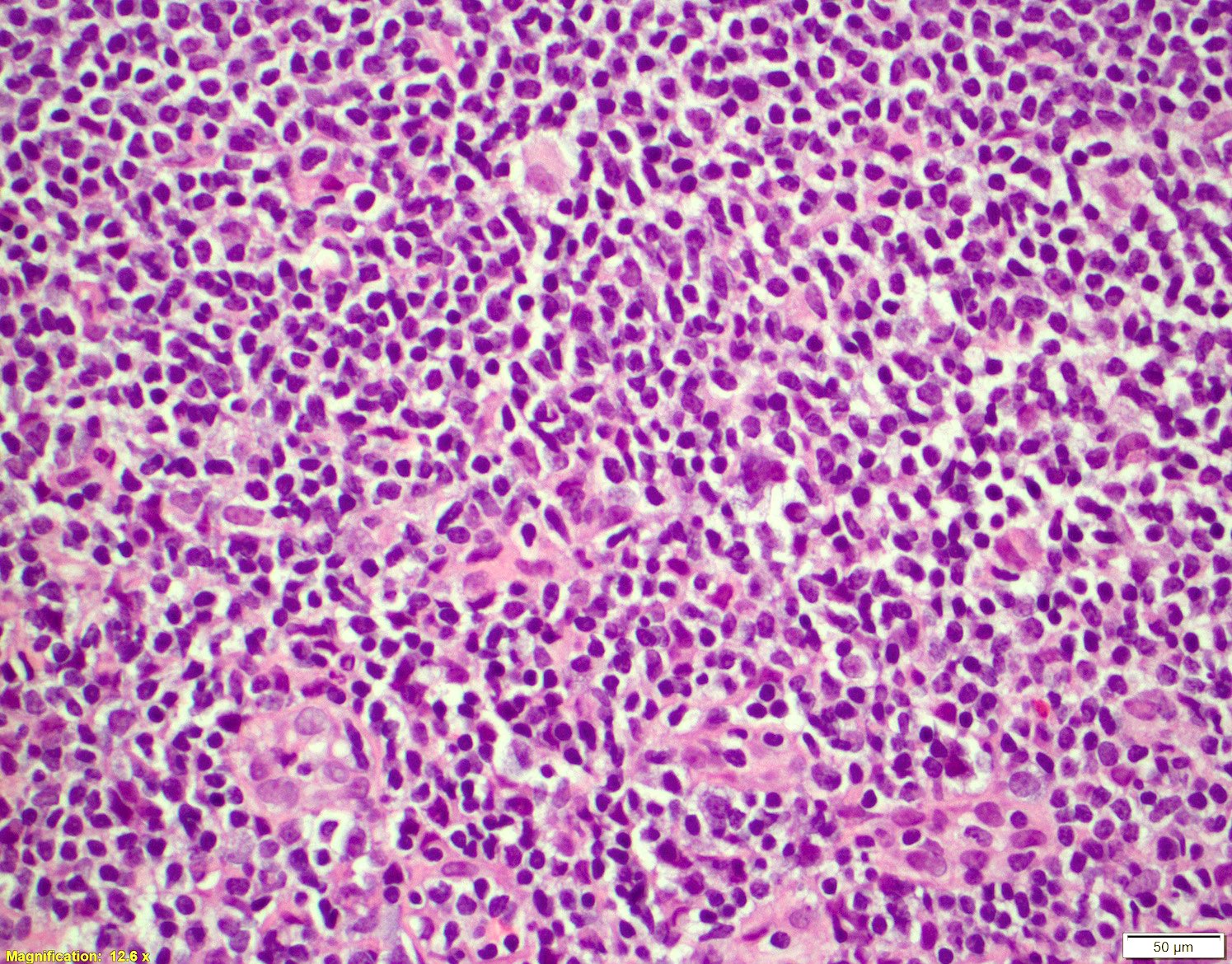
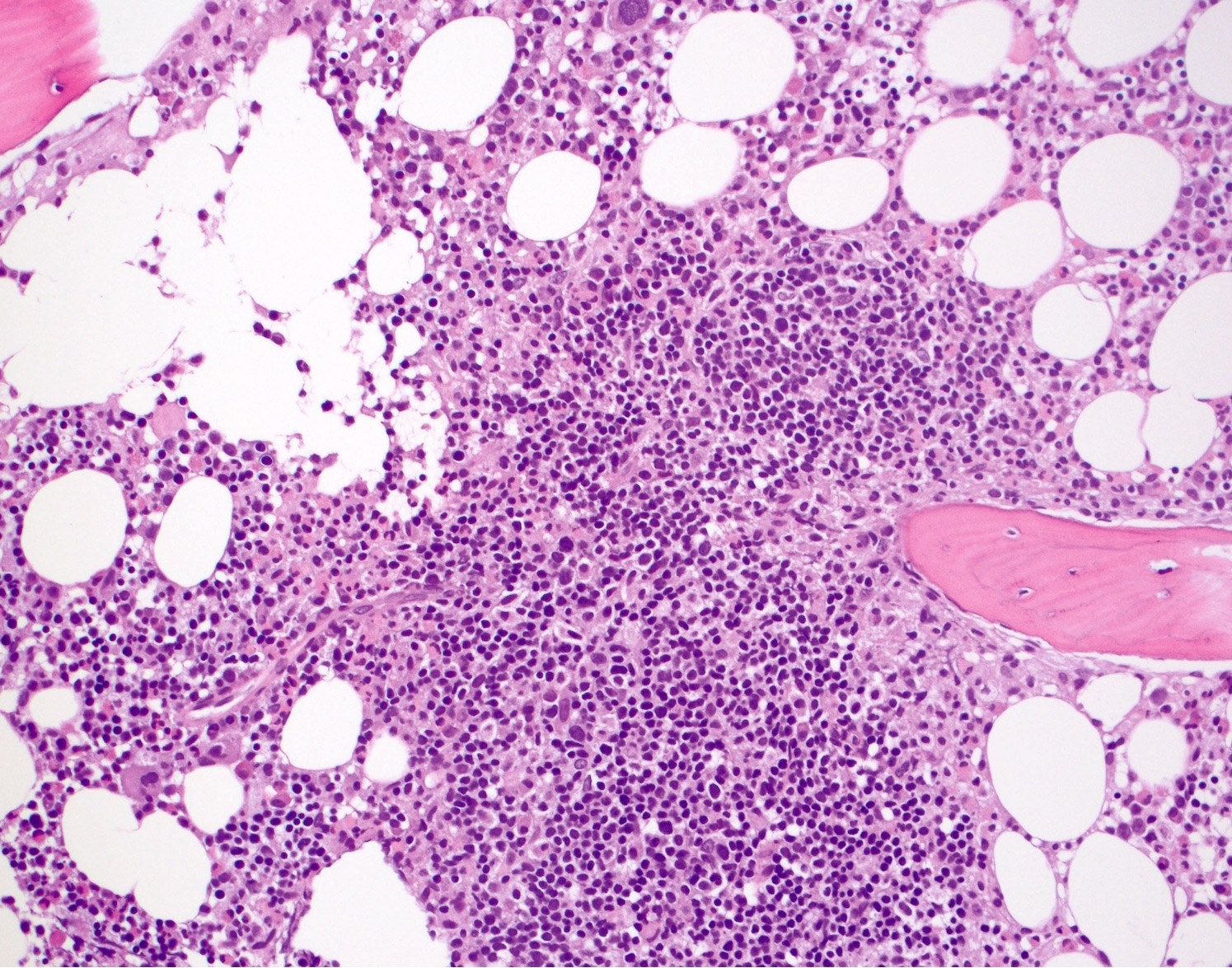
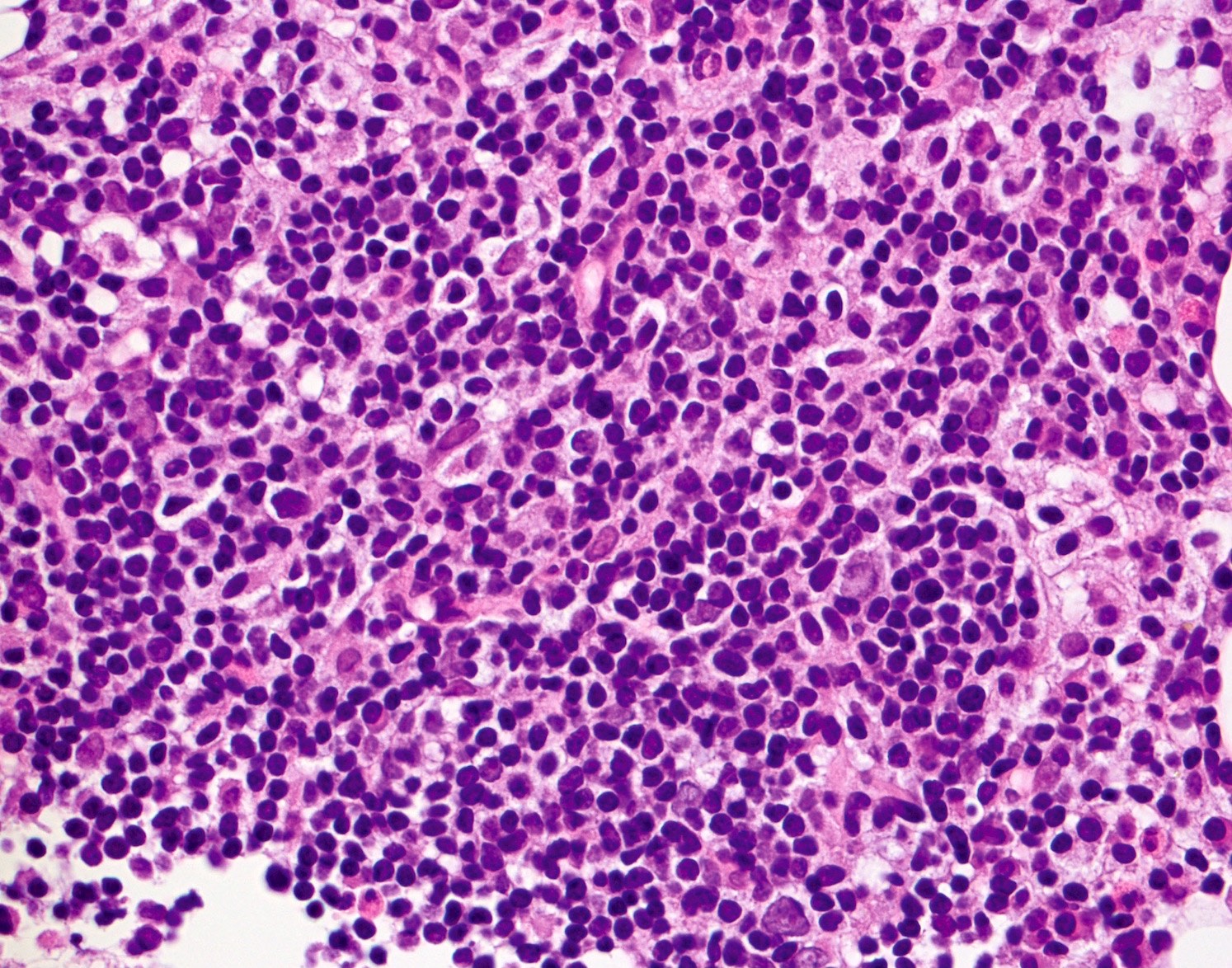
Microscopic (histologic) description
- Diffuse > nodular > mantle zone growth patterns
- Nodal (> 50% nodular), diffuse growth pattern (< 50% nodular)
- Small to medium monomorphic lymphoid neoplasm
- Irregular nuclear border, clumped chromatin and inconspicuous nucleoli
- No proliferation centers
- Centroblasts, immunoblasts or paraimmunoblasts are absent
- Hyalinized vessels
- Epithelioid histiocytes
- Variants
- Aggressive variants
- Blastoid: lymphoblast-like in appearance, monomorphism
- >20 - 30 mitoses per 10 high power fields
- Resemble lymphoblastic lymphoma
- Pleomorphic: large cells with irregular nuclear border, cerebriform nuclei, multinucleation, lack of monomorphism
- Prominent nucleoli and abundant pale cytoplasm
- Resemble DLBCL
- Blastoid: lymphoblast-like in appearance, monomorphism
- Other variants
- Small cell: small round lymphocytes with more clumped chromatin
- Resemble CLL
- Marginal zone-like: abundant pale cytoplasm
- Resembling marginal zone or monocytoid B cells
- Lymphoplasmacytic differentiation, some cases (Am J Surg Pathol 2006;30:954)
- Small cell: small round lymphocytes with more clumped chromatin
- Aggressive variants
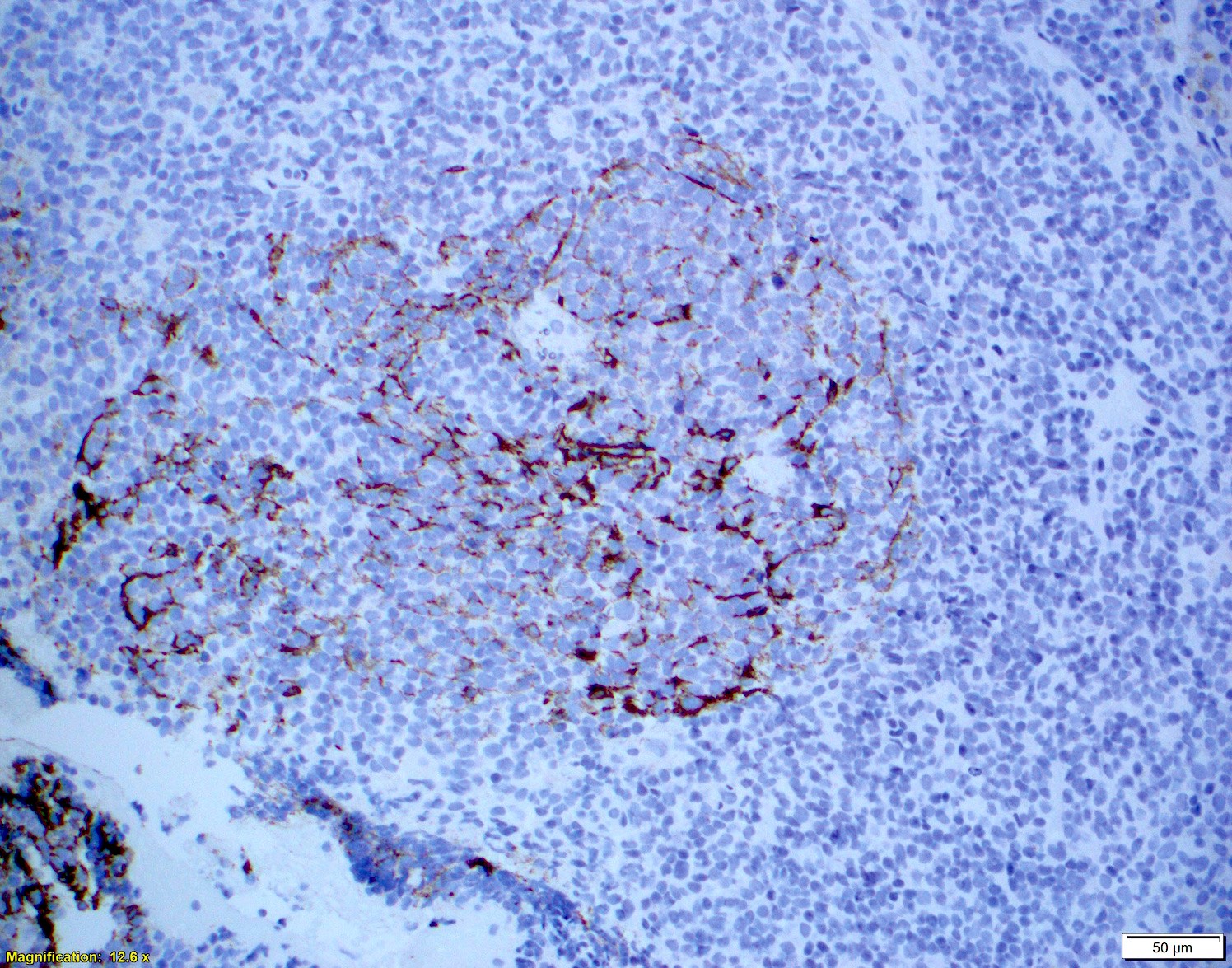
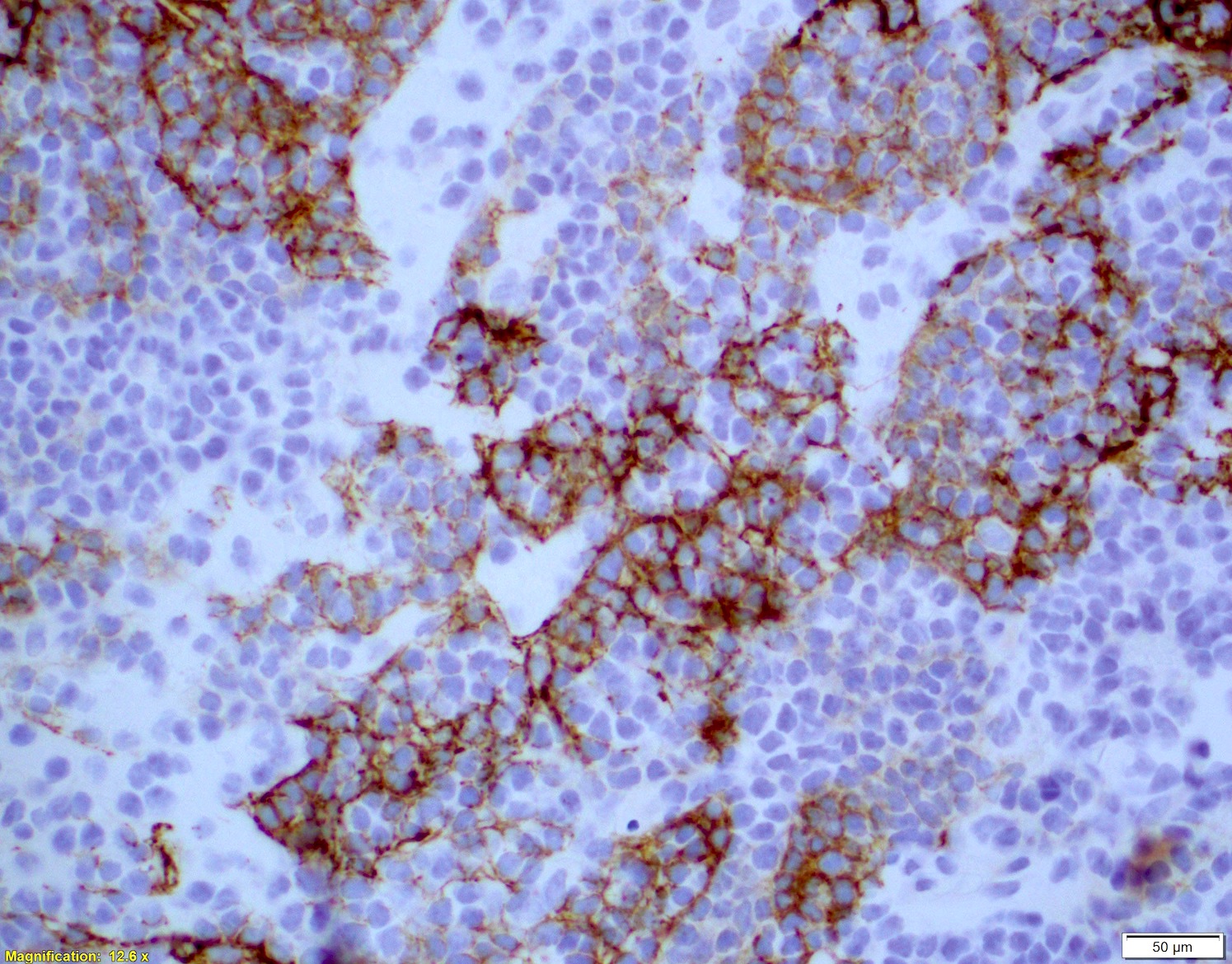
- Follicular dendritic cell (FDC) meshwork
- Nodular pattern
- Primary follicle-like pattern
- Germinal center-like pattern
- Diffuse pattern
- Nodular pattern
- Bone marrow
- Nodular, interstitial or paratrabecular or combination
- Peripheral blood (see below)
- Similar spectrum seen in tissue sample
- Nucleoli are sometimes more prominent
- Spleen
- White pulp nodules involved (enlarged)
- Variable involvement of the red pulp
- Residual naked germinal centers
- Tumor cells: similar monotonous morphology
- Some cases may show a marginal zone-like area (Histopathology 1998;33:230)
- GI
- May mimic lymphoepithelial lesions in marginal zone lymphoma (Histopathology 1995;26:413)
- Relapse
- Loss of a mantle zone growth pattern
- Increase in nuclear size
- Pleomorphism and chromatin dispersal
- Increase in mitotic activity and Ki67
- Cases that are blastoid at diagnosis may relapse with classic morphology (Histopathology 2013;62:334)
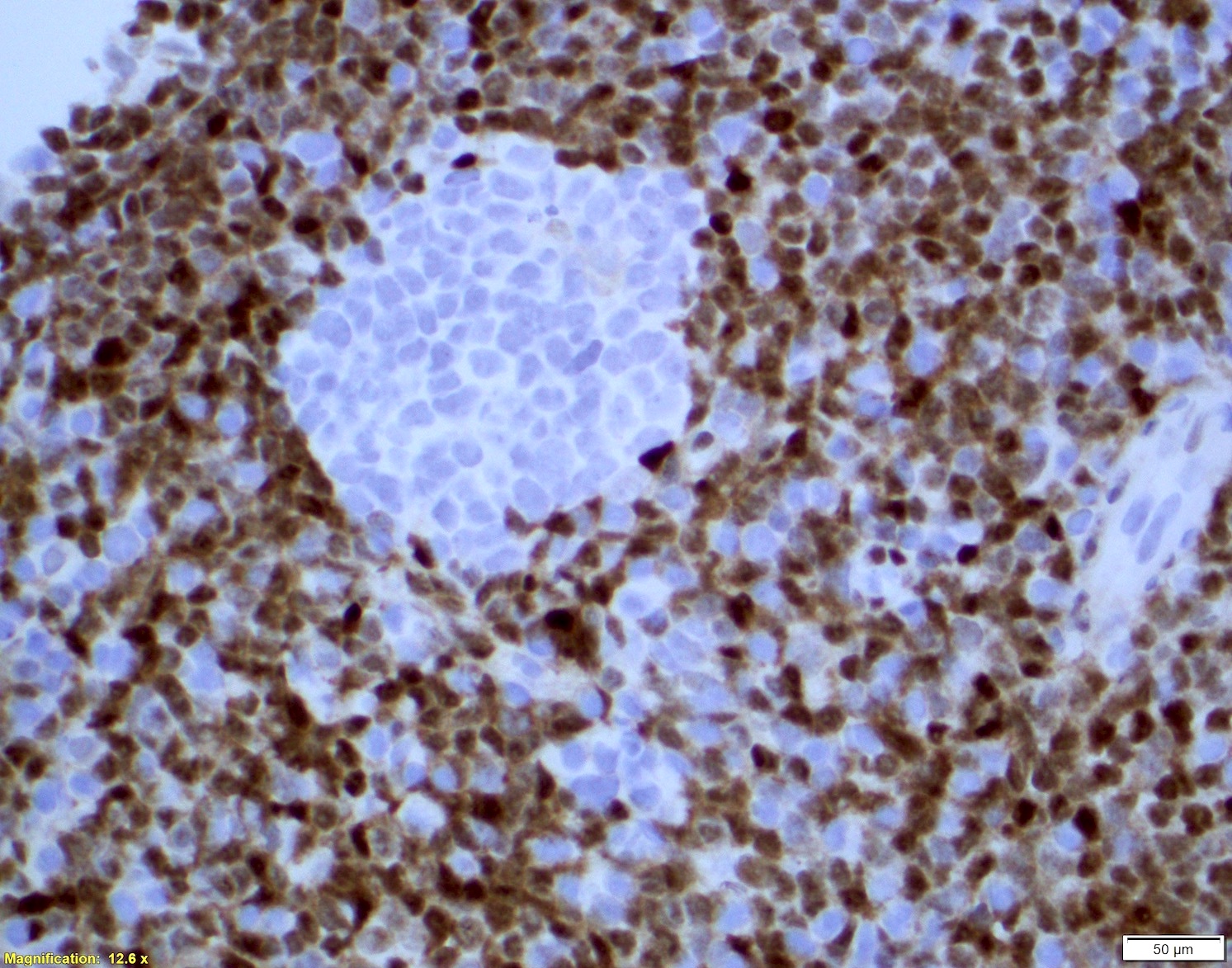
Microscopic (histologic) images
Contributed by Chi Young Ok, M.D.
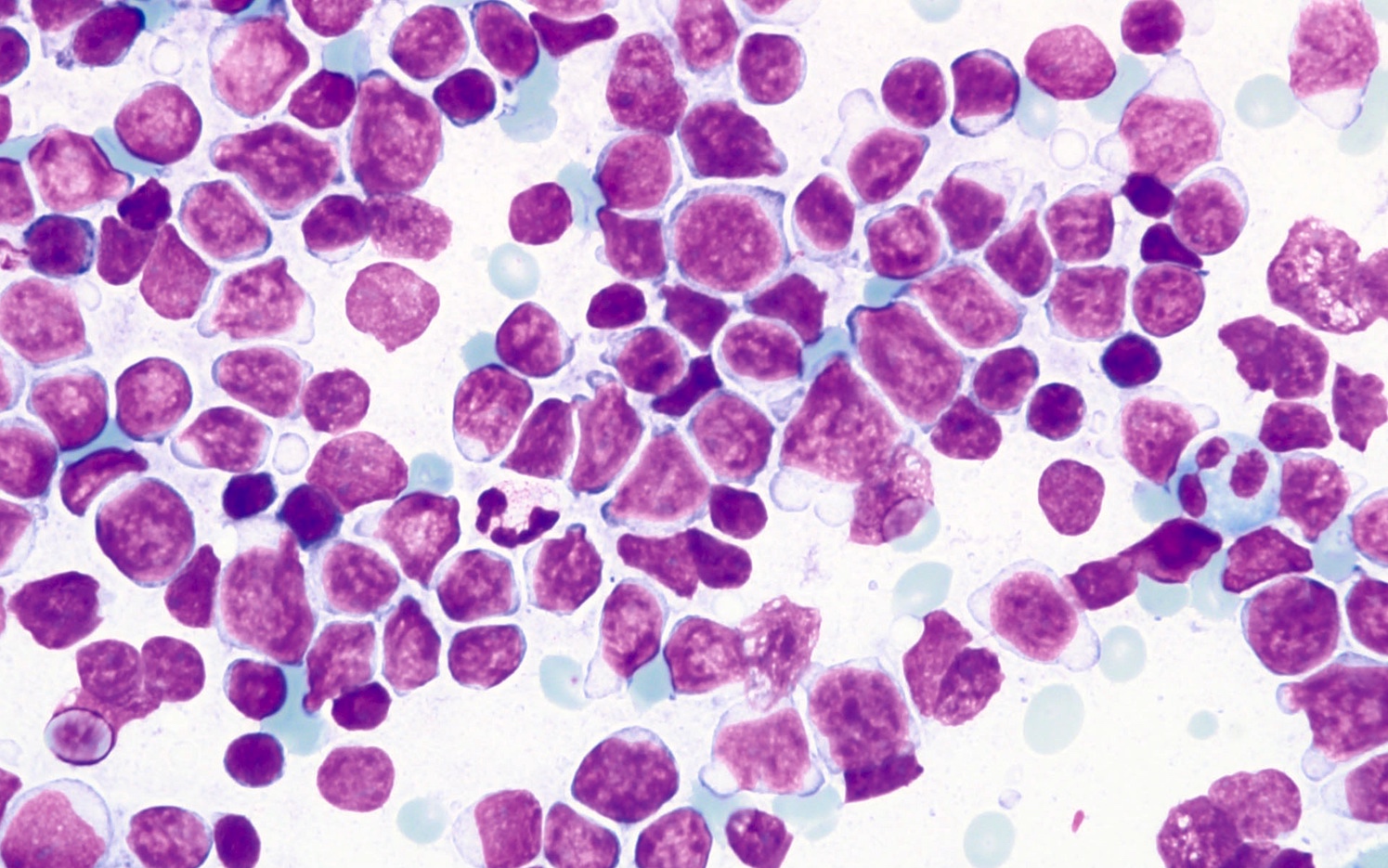
Cytology description
- A monotonous population of small to intermediate sized lymphoid cells
- Nuclear clefts with fine stippled chromatin
- Inconspicuous nucleoli
- Distinct pale or basophilic cytoplasm
- Reference: Jaffe: Hematopathology, 2nd Edition, 2016
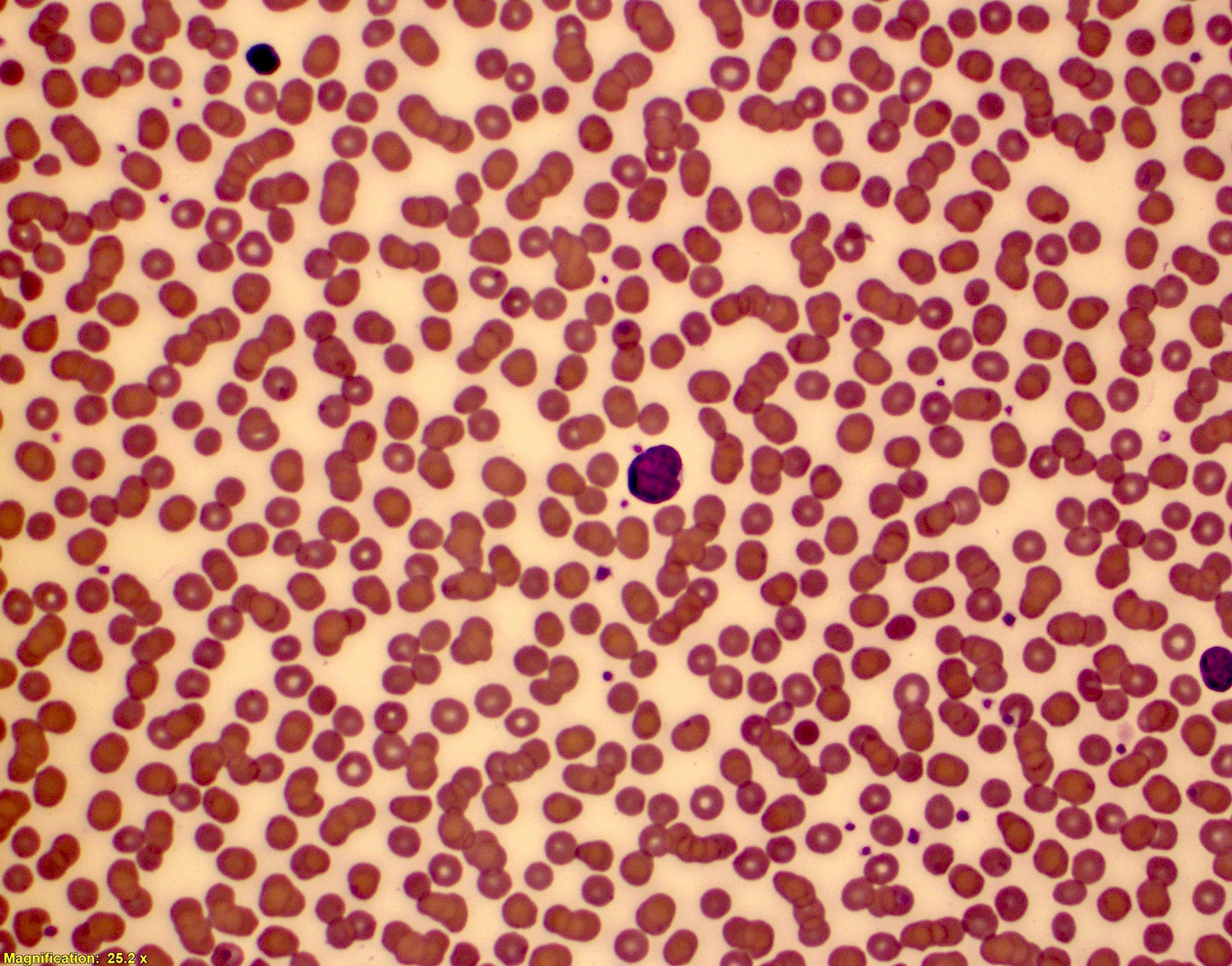
Peripheral smear description
- Mantle cell lymphoma cells may be polymorphous (in contrast to tissue)
- Nuclear size and shape vary
- Chromatin has a reticulated pattern
- Nucleoli can be prominent
- May mimic B cell chronic lymphocytic leukemia
- Reference: Wang: Diagnosis of Blood and Bone Marrow Disorders, 1st Edition, 2018
Positive stains
- Cyclin D1
- CD19+, CD20+, sIg+, IgM with or without IgD
- CD43
- CD5+ (> 95%), SOX11+ (> 90%)
- Exceptions:
- SOX11 negative cases
- More indolent
- Leukemic / non-nodal involvement (Am J Surg Pathol 2019;43:710)
- Mutated IGHV
- CD5 negative cases (Am J Surg Pathol 2019;43:1052)
- Cyclin D1 positive
- Cyclin D1 negative cases
- SOX11 positive
- SOX11 negative cases
- MUM1/ IRF4 (50% in small subset of cells)
- BLIMP1 (50%) and XBP1 (30%)
- Small number of mantle cell lymphomas are positive for CD10 (Oncotarget 2017;9:11441)
- Ki67 count (J Hematop 2009;2:103)
- Five independent high power fields count
- Avoidance of residual germinal centers, hot spots and proliferating T cells
- CD23 and CD21 highlight FDC meshwork (see microscopic description)
Negative stains
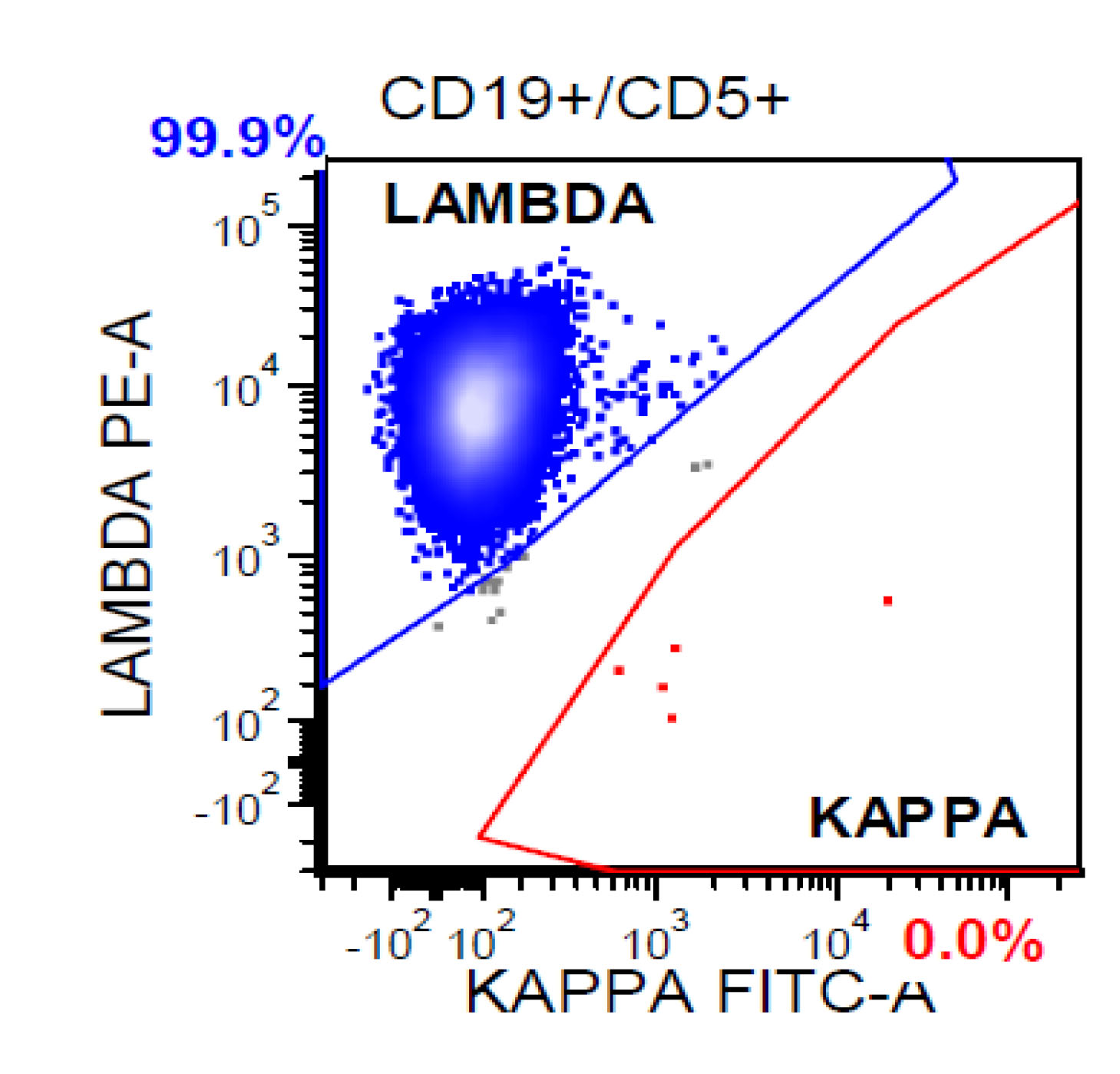
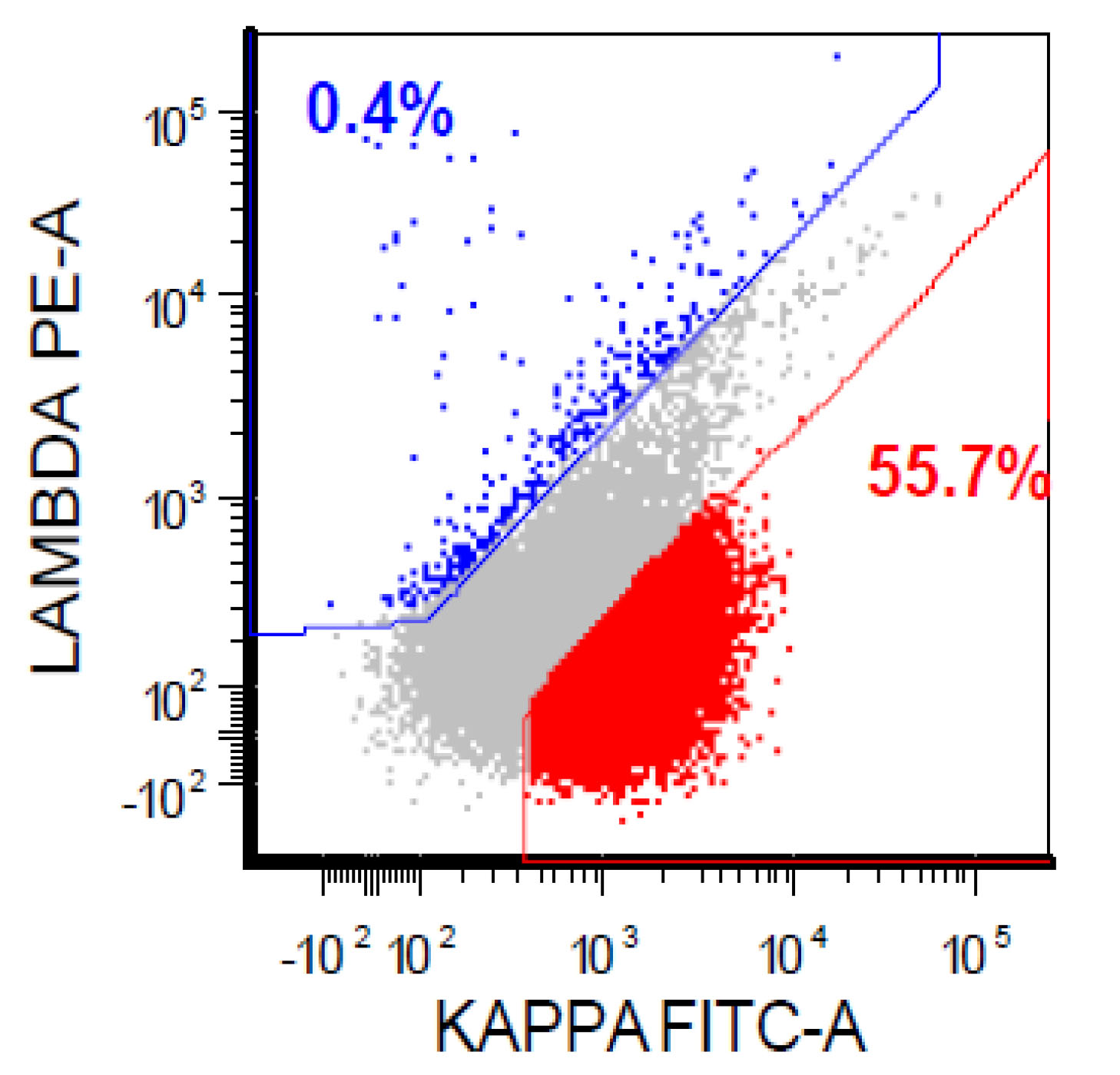
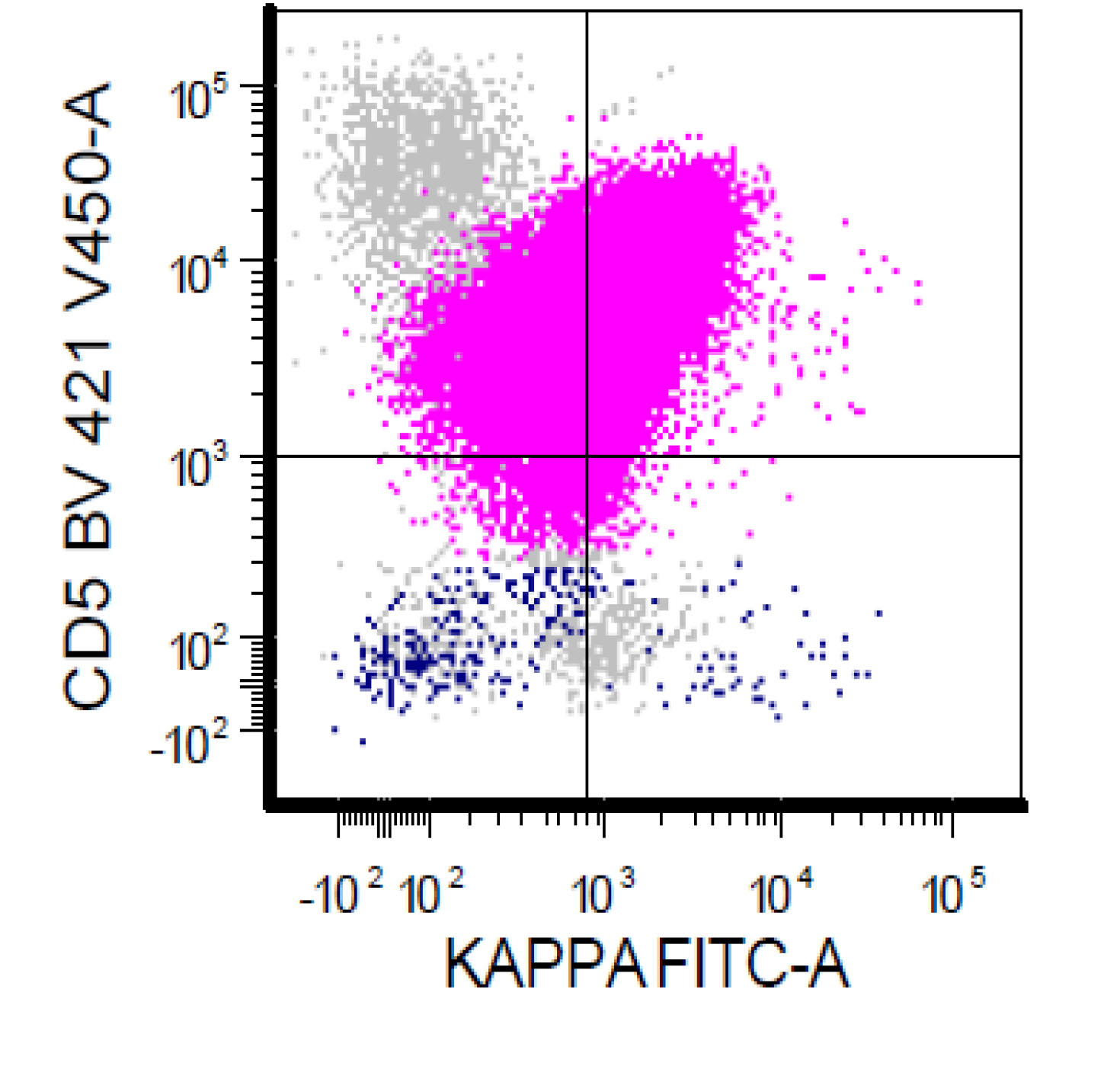
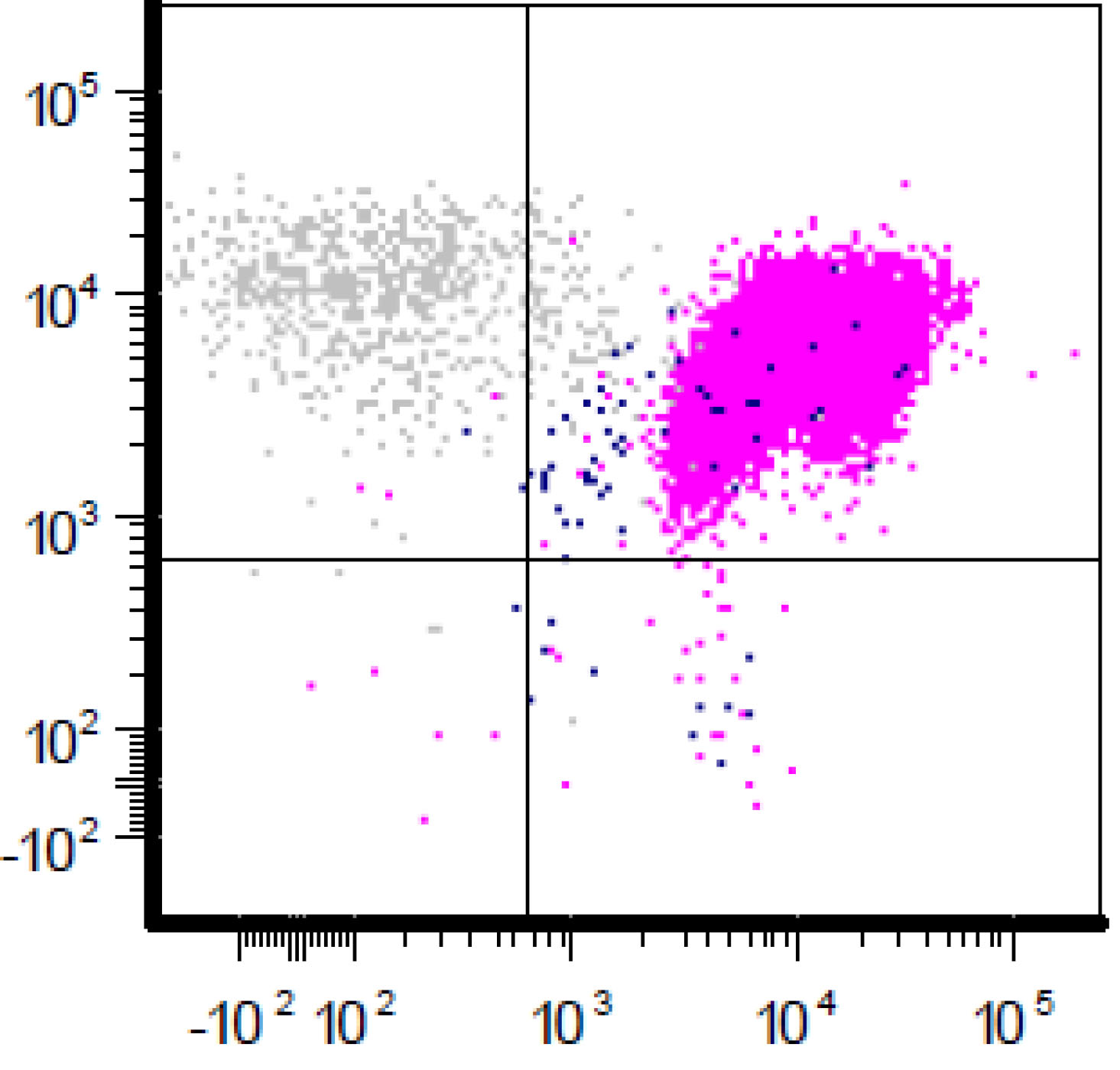
Flow cytometry description
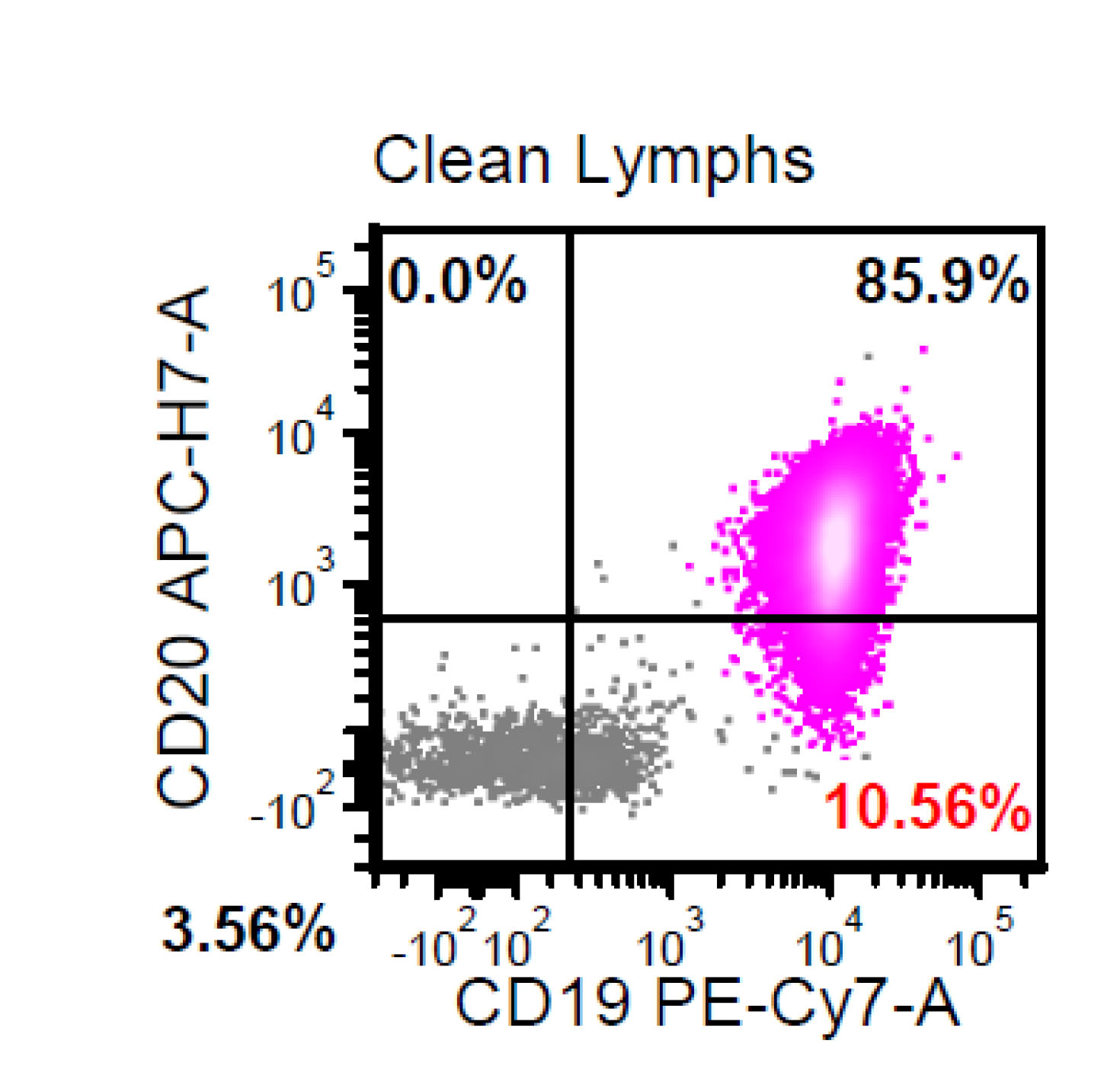
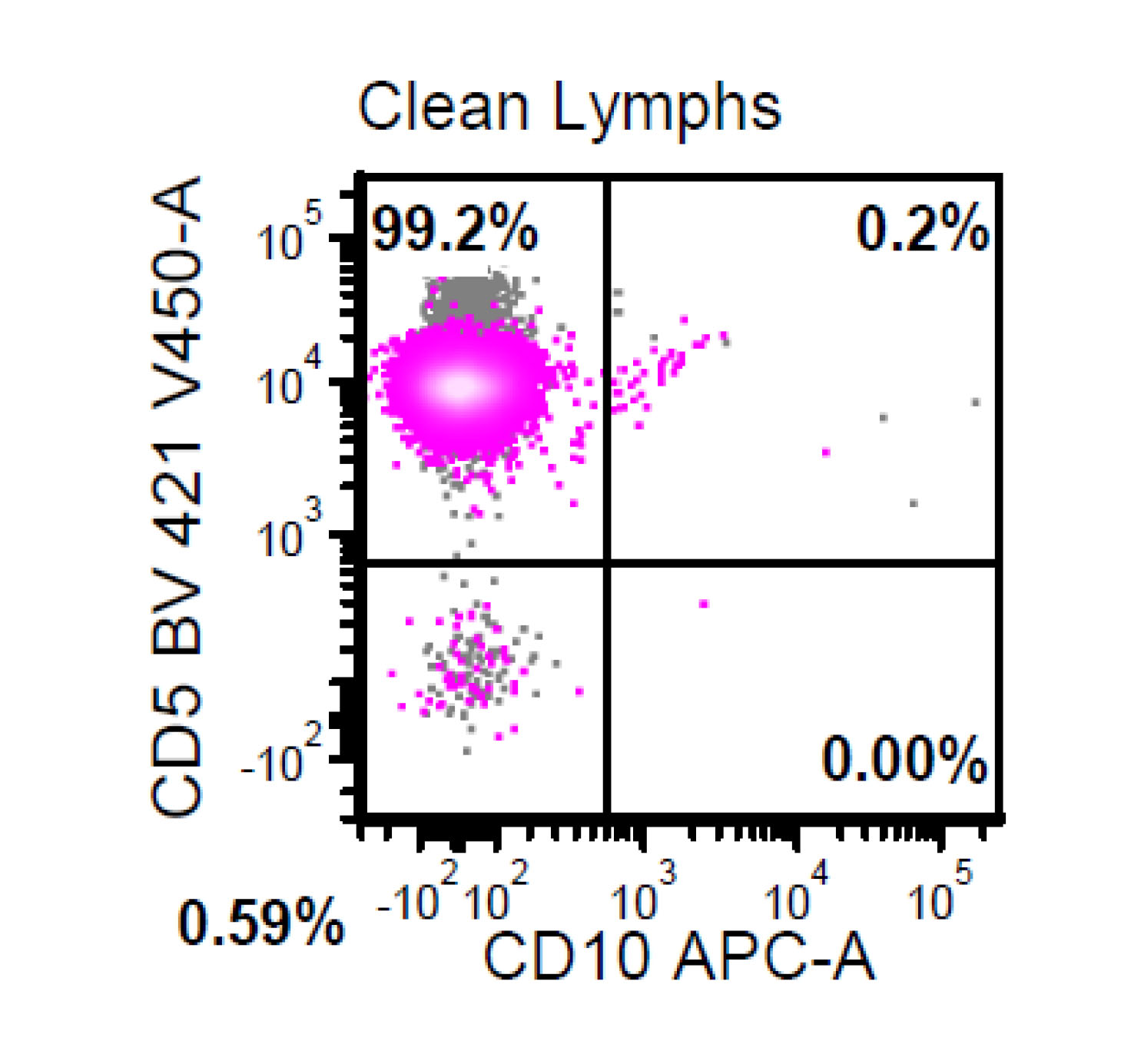
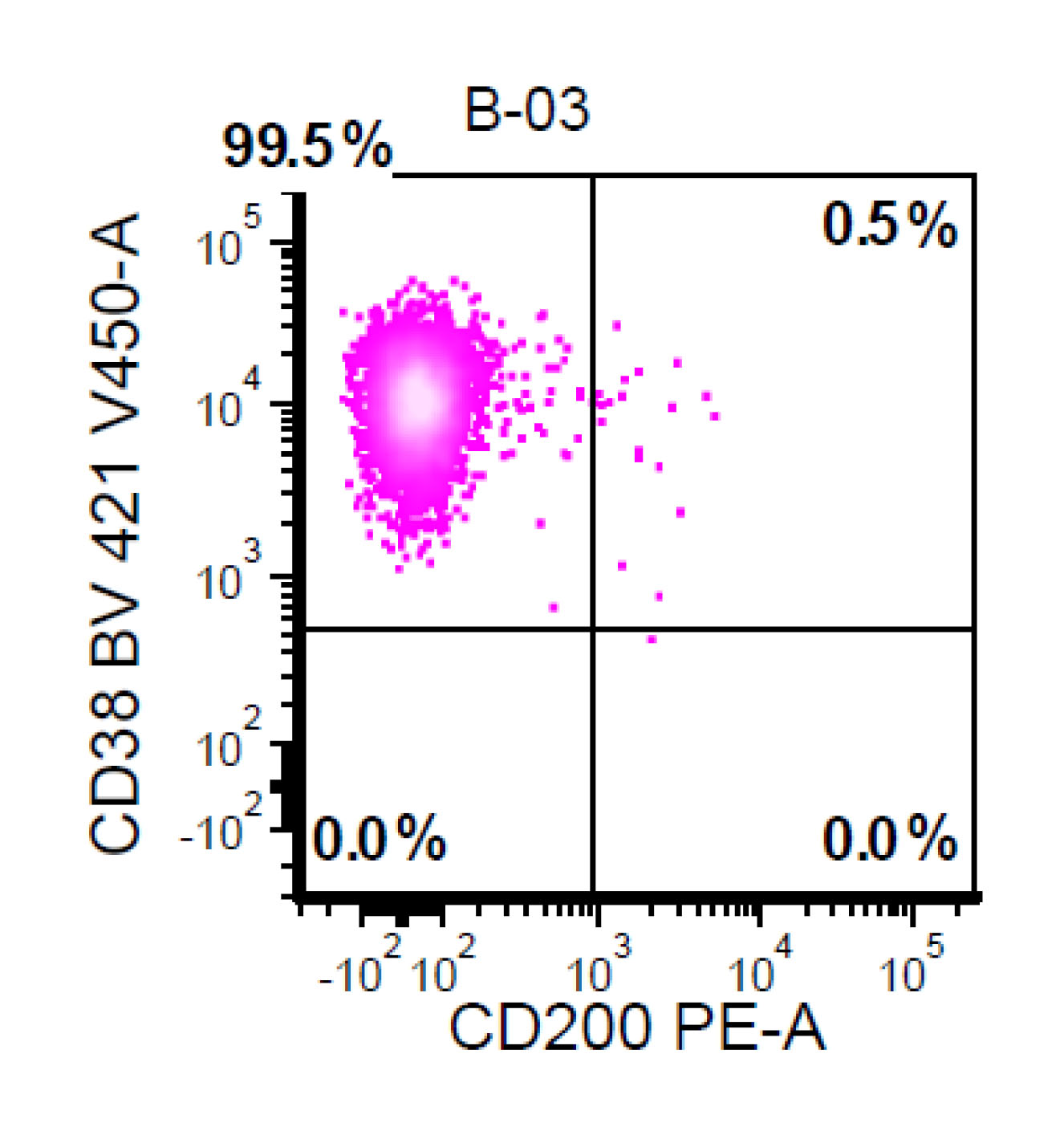
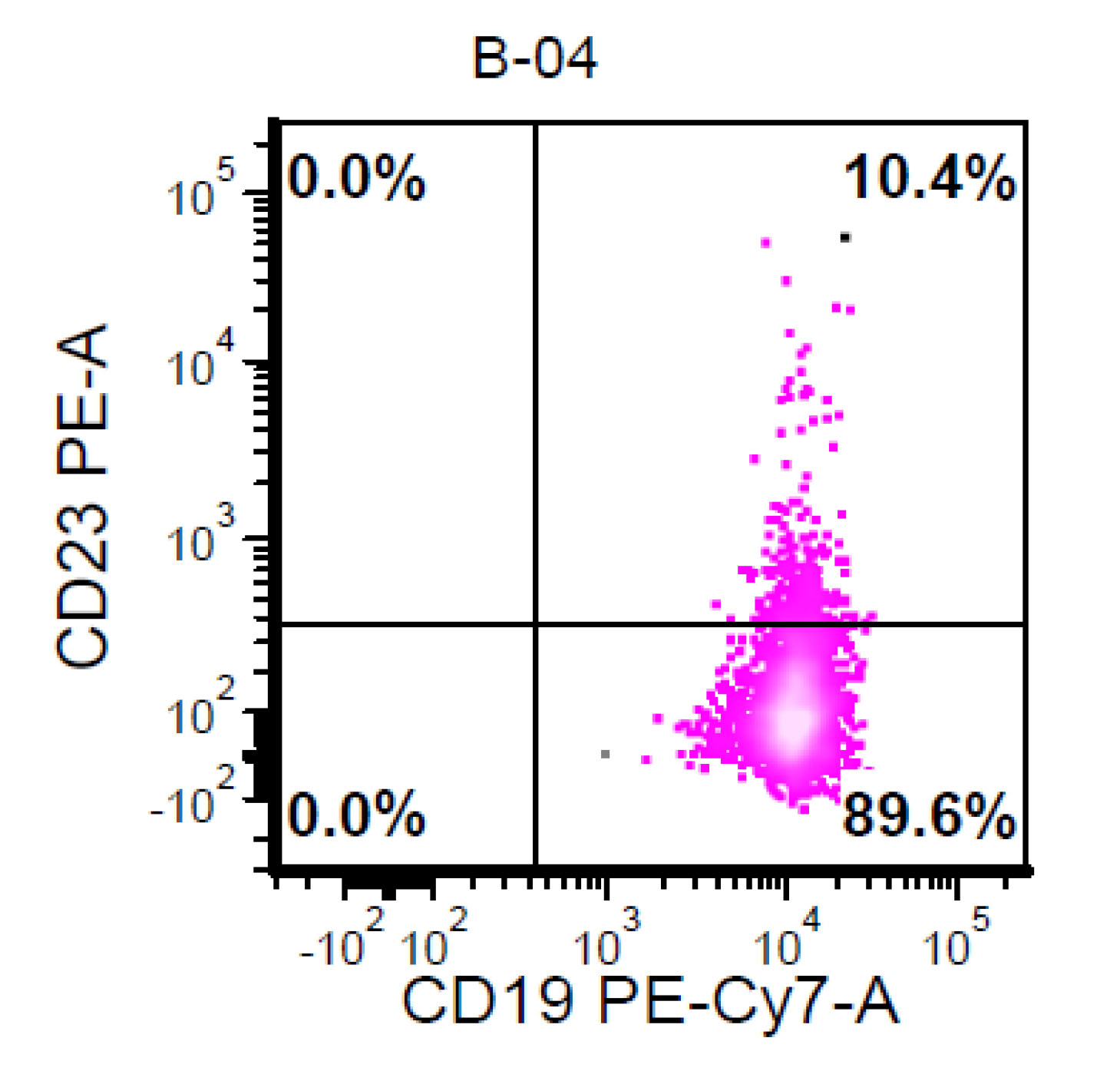
- CD5+, CD19+, CD20+, CD22+, CD79b+, FMC7+
- Monotypic Ig (usually moderate intensity)
- CD3-, CD10-, CD11c+/-, CD23-, CD43+/-, CD200-/+
- Rare cases have atypical immunophenotype: CD5- or CD10+, CD200+ or CD23+ (dim ~ 10%)
- Reference: Wang: Diagnosis of Blood and Bone Marrow Disorders, 1st Edition, 2018
Flow cytometry images
Molecular / cytogenetics description
- IG genes are clonally rearranged
- IGHV genes are unmutated or minimally mutated in most cases
- t(11;14)(q13;q32)
- FISH is convenient because it can be performed on fixed tissue sections
- Conventional cytogenetics if fresh material available
- Most PCR assays usually detect 1 major breakpoint region in mantle cell lymphoma
- Cyclin D2 rearrangements by FISH in some of cyclin D1(-) cases
- Secondary chromosomal aberrations
- Gains of 3q26 (in 31 - 50%)
- 7p21 (16 - 34%),
- 8q24 (MYC, 16 - 36%)
- 13q31 (24%)
- Losses of 1 p13-31 (29 - 52%)
- 6q23-27 (TNFAIP3, 23 - 38%)
- 9p21 (CDKN2A which codes for p16 INK4a and p14 ARF, 18 - 31%)
- 11q22-23 (ATM, 21 - 59%)
- 13q11-13 (22 - 55%)
- 13q14-34 (43 - 51%)
- 17p13 (TP53, 21 - 45%) (Blood 1999;93:436, Blood 2005;105:4445, Oncogene 1992;7:1401)
Molecular / cytogenetics images
Sample pathology report
- Inguinal lymph node, left, needle biopsies:
- Mantle cell lymphoma, diffuse pattern, classic variant (see comment)
- Comment: Histologic sections show needle core shaped lymphoid tissue. Lymph node architecture is entirely effaced by malignant lymphoma. The lymphoma demonstrates a diffuse pattern and the lymphoma cells are intermediate sized. Lymphoma cells have irregular nuclear contours, relatively closed chromatin, inconspicuous nucleolus and moderate to large amount of cytoplasm. Scattered epithelioid histiocytes with eosinophilic cytoplasm (“pink histiocytes”) are seen in the background. No sheets of large cells or necrosis are seen. Mitotic figures are rarely present.
Flow cytometric analysis using concurrent cytologic sample demonstrates clonal B cells with surface kappa light chain expression, positive for CD5, CD19, CD20, CD22 ,CD38, CD43 (partial), CD44, CD79b, while they are negative for CD3, CD4, CD8, CD10, CD11c, CD23, CD30, CD34, CD56 and CD200. The clonal B cells comprise approximately 62.4% of total analyzed cellular events and 70.7% of the lymphoid population.
Immunohistochemical studies were performed on formalin fixed, paraffin embedded tissue. Lymphoma cells are positive for CD20, PAX5, cyclin D1 and SOX11. They are negative for CD3 and p53. Ki67 proliferation rate is estimated at 10 - 20%.
In summary, morphologic, flow cytometric and immunohistochemical studies are diagnostic of mantle cell lymphoma, classic variant.
Differential diagnosis
- Nodal mantle cell lymphoma
- Chronic lymphocytic leukemia / small lymphocytic lymphoma (CLL / SLL)
- Follicular lymphoma
- Nodal marginal zone B cell lymphoma
- Splenic marginal zone lymphoma (SMZL)
- A micronodular pattern of splenic involvement are seen in both mantle cell lymphoma and splenic marginal zone lymphoma
- Villous cells in PB may be seen in mantle cell lymphoma
- Mantle cell lymphoma expresses CD5 and cyclin D1
- 7q deletion is a relatively specific marker for splenic marginal zone lymphoma (40% of cases)
- Reactive follicular hyperplasia
- Thinner mantle zones
- Composed of small, round, mature lymphocytes
- Prominent germinal centers
- No evidence of monoclonality
- Castleman disease, hyaline vascular type
- Large localized mass in a young person
- Architecture not entirely effaced
- Hyaline vascular follicles
- Onion skin lymphocytes around germinal centers
- Leukemic mantle cell lymphoma
- Hairy cell leukemia (HCL)
- Hairy cell leukemia may be cyclin D1 positive
- Refer to flow cytometry section for more detail
- Chronic lymphocytic leukemia / small lymphocytic lymphoma (CLL / SLL)
- Prolymphocytic leukemia
- Many B-PLL cases may actually be leukemic mantle cell lymphoma
- This is especially likely in cases that are either cyclin D1 positive or t(11;14) IGH/CCND1 positive (Am J Clin Pathol 2001;115:571)
- Lymphoblastic leukemia
- Mostly in DDx with blastoid mantle cell lymphoma (refer to mantle cell lymphoma variants)
- Hairy cell leukemia (HCL)
Additional references
- Jaffe: Hematopathology, 2nd Edition, 2016
- Hsi: Hematopathology - Foundations in Diagnostic Pathology, 3rd Edition, 2017
- Swerdlow: WHO Classification of Tumors of Hematopoietic and Lymphoid Tissues, 4th Edition, 2017
- Aster: Hematopathology - High Yield Pathology, 1st Edition, 2013
- Medeiros: Diagnostic Pathology - Lymph Nodes and Extranodal Lymphomas, 2nd Edition, 2017
- Kumar: Robbins and Cotran pathologic basis of disease, 9th edition, 2015
- Wang: Diagnosis of blood and bone marrow disorders, 1st Edition, 2018
Board review style question #1
- Which of the following translocations is characteristic of mantle cell lymphoma?
- t(14;18)
- t(11;18)
- t(11;14)
- t(8;14)
Board review style answer #1
Board review style question #2
- A 74 year old man has presented with an absolute lymphocytosis (6 - 7 x 103/μL) for about 6 months. You are screening the peripheral blood with a preliminary flow cytometry that is provided in the first three plots. You decide to extend the flow cytometry markers. Which combination of markers in the last plot (plot 4) will more likely represent CLL phenotype rather than MCL phenotype?
- CD79a / CD45
- CD43 / CD200
- CD79a / FMC7
- CD5 / CD79a
Board review style answer #2