Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Crane GM. Heavy chain disease. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomaheavychain.html. Accessed April 17th, 2024.
Definition / general
- Rare B cell neoplasm characterized by production of monoclonal heavy chain unable to bind light chain (truncated or mutated)
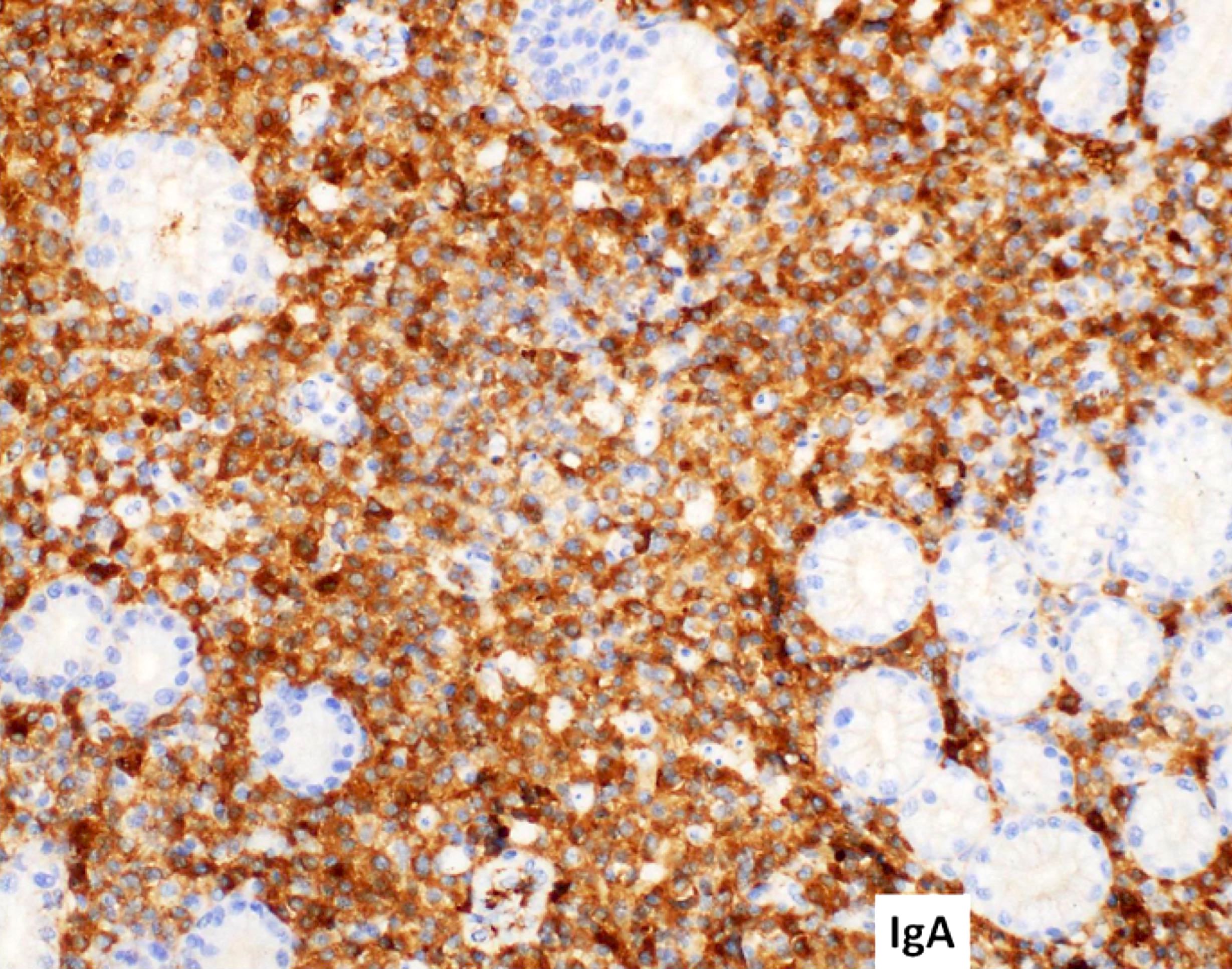
- Alpha heavy chain disease is the most common; it is also known as immunoproliferative small intestinal disease (IPSID), a variant of extranodal marginal zone lymphoma of mucosa associated lymphoid tissue (MALT lymphoma)
Essential features
- 3 main types: alpha (IgA), gamma (IgG) and mu (IgM)
- Resultant lymphoma resembles other lymphoma types with each heavy chain disease associated with distinct features
- Must demonstrate free heavy chain by protein electrophoresis / immunofixation
- Alpha heavy chain disease is the most common, presents in younger patients, marginal zone phenotype
- Gamma is often associated with autoimmune disease, may be polymorphic
- Mu may resemble chronic lymphocytic leukemia (CLL) with mix of lymphocytes and characteristic vacuolated plasma cells
Terminology
- Alpha heavy chain is also known as immunoproliferative small intestinal disease (IPSID)
ICD coding
- ICD-10: C88.2 - heavy chain disease
Epidemiology
- Alpha: younger age, peak incidence in 20s and 30s, equal prevalence in men and women, more common in areas neighboring Mediterranean Sea, most prevalent in Africa and the Middle East, associated with factors linked to low socioeconomic status (poor hygiene, malnutrition, frequent intestinal infections)
- Gamma: rare, ~150 cases reported, median age 60, female predominance
- Mu: extremely rare, 30 - 40 cases reported, median age 60, equal prevalence in men and women
Sites
- Alpha: mainly small intestine, mesenteric lymph nodes; gastric and colonic mucosa may be involved, rarely respiratory tract and thyroid; usually not bone marrow or other organs
- Gamma: lymph nodes or extranodal, Waldeyer ring, gastrointestinal tract, bone marrow, liver, spleen, peripheral blood, skin, subcutaneous tissue
- Mu: spleen, liver, bone marrow, blood, usually not lymphadenopathy
Pathophysiology
- All: deletions in heavy chain gene result in defective heavy chain protein that cannot bind to light chain to form complete Ig molecule
Etiology
- Alpha: chronic intestinal infection (e.g. Campylobacter jejuni) may underlie development of the disease
Clinical features
- Alpha: typically presents with malabsorption, diarrhea, hypocalcemia, abdominal pain, wasting, fever; patients may die from malnutrition, intestinal obstruction, sepsis or other complications due to massive bowel involvement
- Gamma: typically associated with systemic symptoms (anorexia, weakness, fever, weight loss, bacterial infections), concurrent autoimmune disease, generalized disease (hepatomegaly, splenomegaly, lymphadenopathy); rarely transforms to large cell lymphoma; disease patterns range from indolent to aggressive
- Mu: may resemble chronic lymphocytic leukemia (CLL) but differs in the high frequency of hepatosplenomegaly and absence of peripheral lymphadenopathy; has mixture of plasma cells and B lymphocytes with monoclonal cytoplasmic mu heavy chain; similar slow progression
Diagnosis
- Combination of histopathologic features and detection of serum heavy chain by immunofixation
Laboratory
- Variably sized heavy chains may be produced, which may NOT produce characteristic monoclonal peak on serum protein electrophoresis
- Immunofixation may be critical for detection
- Gamma: may detect IgG without light chain in blood or urine
- Mu: mu heavy chain not detected in urine but Bence Jones light chains may still be detected (especially kappa) (Am J Hematol 1992;40:56)
Prognostic factors
- Alpha: early stages may respond to antibiotic therapy; more advanced disease requires multiagent chemotherapy
Case reports
- 48 year old woman with gamma heavy chain disease and a history of seronegative rheumatoid arthritis (Biochem Med (Zagreb) 2012;22:373)
- 48 year old woman with Hodgkin lymphoma and gamma heavy chain disease (Arch Pathol Lab Med 2001;125:803)
- 59 year old woman with immunotactoid glomerulopathy, follicular lymphoma and gamma heavy chain disease (Arch Pathol Lab Med 2004;128:689)
- 64 year old patient with mu heavy chain disease (Blood 2017;130:558)
- Man with 30 year course of immunoproliferative small intestinal disease (IPSID) without development of lymphoma (Am J Gastroenterol 2001;96:2769)
Treatment
- Alpha: early disease may respond to antibiotic therapy; for more advanced immunoproliferative small intestinal disease, anthracycline containing regimens have been reported to result in remission and longterm survival
Microscopic (histologic) description
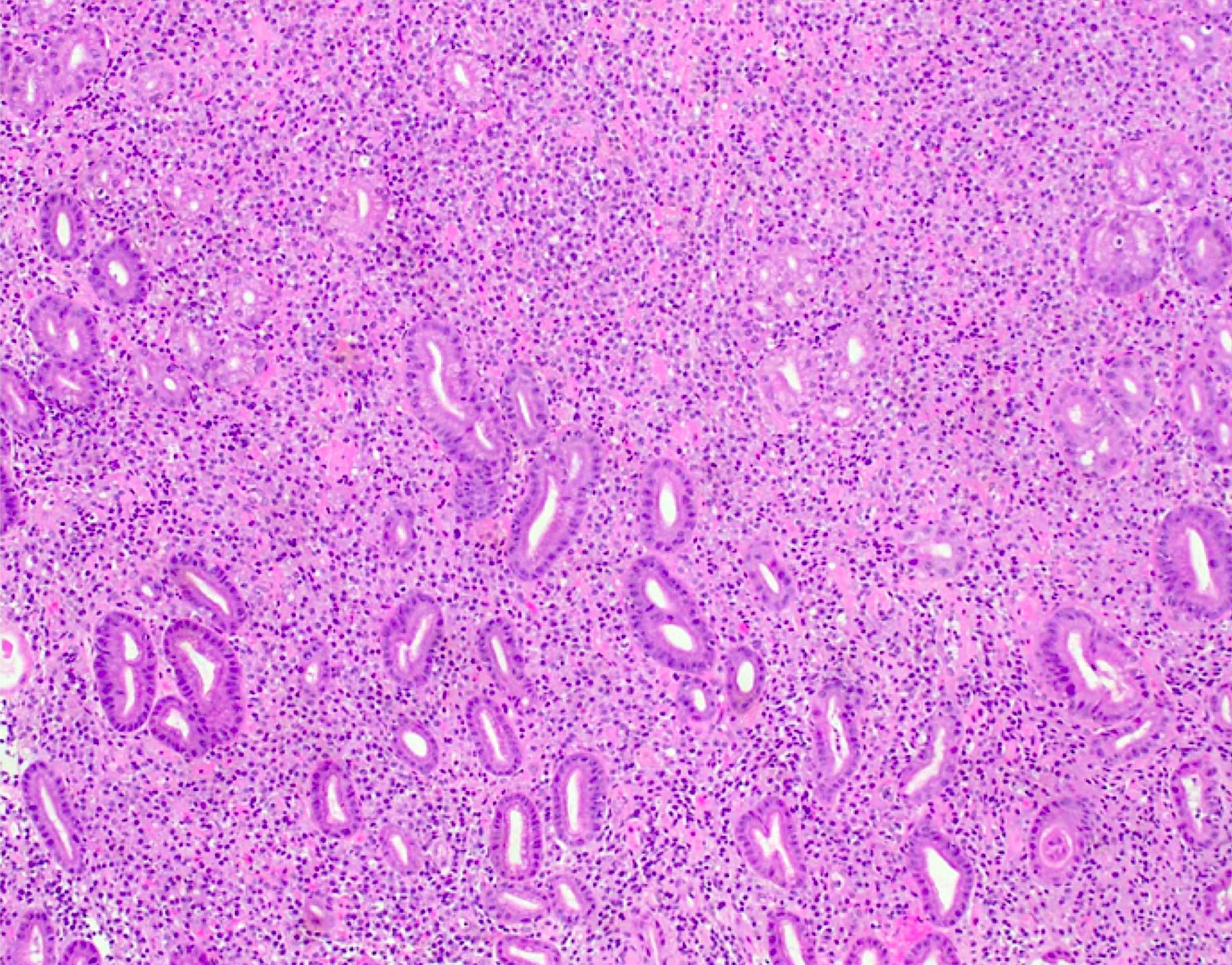
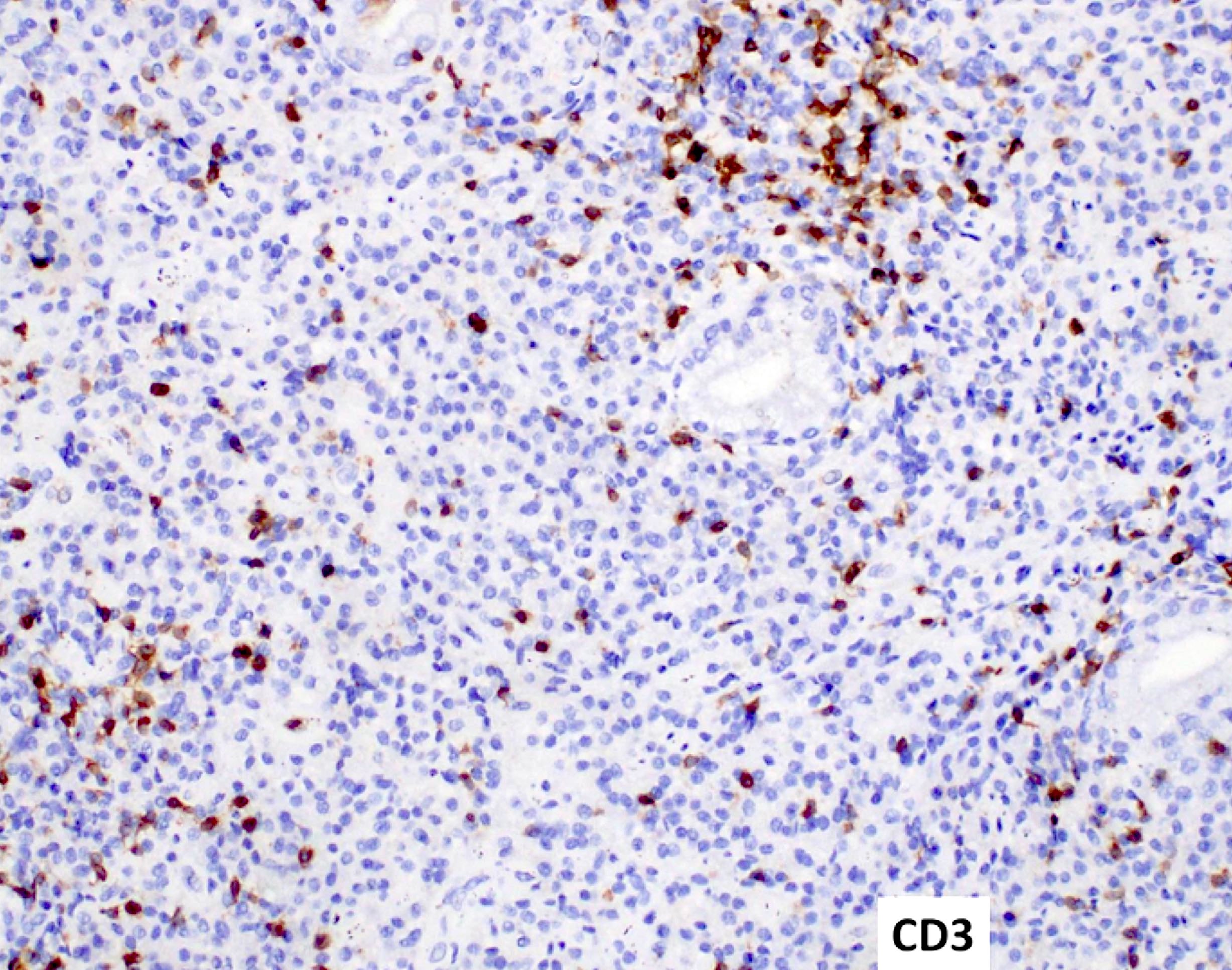
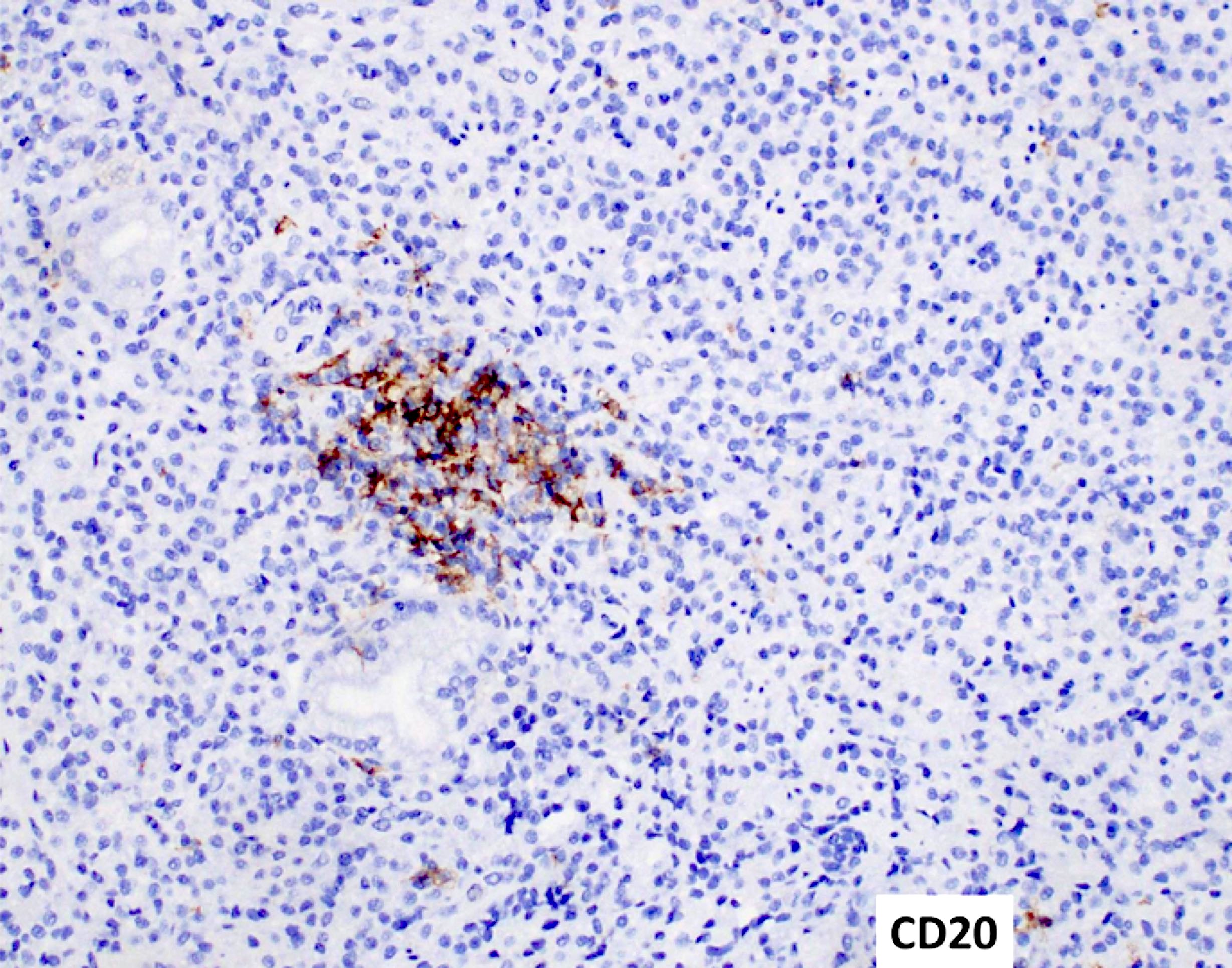
- Alpha: lamina propria of bowel mucosa heavily infiltrated with plasma cells and admixed lymphocytes which separate the crypts; may have marginal zone B cells, lymphoepithelial lesions and villous atrophy; progression to diffuse large B cell lymphoma may be characterized by destructive sheets of large plasmacytoid cells, immunoblasts and ulceration
- Gamma: circulating plasma cells, may resemble splenic marginal zone or MALT lymphoma; polymorphous proliferation with lymphocytes, plasma cells, immunoblasts, histiocytes, eosinophils
- Mu: bone marrow contains vacuolated plasma cells admixed with small lymphocytes
Microscopic (histologic) images
Contributed by Genevieve M. Crane, M.D., Ph.D.
Images hosted on other servers:
Positive stains
Molecular / cytogenetics description
- All have clonally rearranged IGH
- Deletions / insertions in the IGHV or CH1 domain result in defective or truncated heavy chain that cannot bind light chain to form a complete immunoglobulin molecule
- Alpha: case reports of cytogenetic abnormalities but not the t(11;18)(q21;q21) (BIRC3 / MALT1) translocation associated with gastric and pulmonary MALT lymphoma
- Gamma: abnormal karyotype in 50% of cases, MYD88 mutation is absent
- Mu: immunoglobulin genes show high levels of somatic mutation
Differential diagnosis
May resemble other lymphoma subtypes:
- Alpha: a variant of MALT lymphoma, suspicion based on location demographics, clinical features
- Gamma:
- If more monomorphic, may resemble:
- If polymorphous, may resemble:
- Mu: typically resembles chronic lymphocytic leukemia (CLL)
Additional references
Board review style question #1
The presence of a mixed population of vacuolated plasma cells and lymphocytes in the bone marrow is most characteristic of which process?
- Lymphoplasmacytic lymphoma
- MALT variant immunoproliferative small intestinal disease
- Mu heavy chain disease
- Myeloma with a t(11;14) translocation
- Splenic marginal zone lymphoma
Board review style answer #1
C. It is characteristic of mu heavy chain disease, a very rare disease.
Comment Here
Reference: Heavy chain disease
Comment Here
Reference: Heavy chain disease
Board review style question #2
Which heavy chain disease is most likely to be associated with underlying autoimmune disease?
- Alpha heavy chain disease
- Gamma heavy chain disease
- Mu heavy chain disease
- None of the above
Board review style answer #2