Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Marques-Piubelli ML, Ferrufino-Schmidt MC, Miranda RN. Primary cutaneous CD8+ aggressive epidermotropic cytotoxic T cell lymphoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomanonBCD8epidermotropic.html. Accessed April 16th, 2024.
Definition / general
- Cutaneous T cell lymphoma (CTCL) with marked epidermotropism by CD8+ cytotoxic T cells and aggressive clinical behavior (J Am Acad Dermatol 2012;67:748, Mod Pathol 2017;30:761, Am J Clin Pathol 2013;139:491, Histopathology 2015;67:425, Radiology 1991;178:907, Am J Pathol 1999;155:483)
- Included as provisional entity in 2008 and maintained as provisional in the 2017 revised WHO; first described in 1999 (Elder: WHO Classification of Skin Tumours, 4th Edition, 2018, Histopathology 2015;67:425, Am J Pathol 1999;155:483)
Essential features
- Cutaneous T cell lymphoma (CTCL) with marked epidermotropism by CD8+ cytotoxic T cells and aggressive clinical behavior (J Am Acad Dermatol 2012;67:748, Mod Pathol 2017;30:761, Am J Clin Pathol 2013;139:491, Histopathology 2015;67:425, J Am Acad Dermatol 2010;62:300, Am J Pathol 1999;155:483)
- Usually have generalized skin involvement (J Am Acad Dermatol 2012;67:748, Am J Clin Pathol 2013;139:491, Mod Pathol 2017;30:761, Histopathology 2015;67:425)
- Unfavorable prognosis and aggressive clinical course (J Am Acad Dermatol 2012;67:748, Mod Pathol 2017;30:761, Histopathology 2015;67:425, J Am Acad Dermatol 2010;62:300, Am J Pathol 1999;155:483)
ICD coding
- ICD-O: 9709/3 - Cutaneous T cell lymphoma, NOS
Epidemiology
- Rare, < 1% of all cutaneous T cell lymphoma (J Am Acad Dermatol 2012;67:748, J Am Acad Dermatol 2010;62:300)
- More common in elderly: sixth and seventh decade (J Am Acad Dermatol 2012;67:748, Mod Pathol 2017;30:761, Histopathology 2015;67:425, Am J Pathol 1999;155:483)
- M:F = 3:1 (J Am Acad Dermatol 2012;67:748, Mod Pathol 2017;30:761, Histopathology 2015;67:425, Am J Pathol 1999;155:483)
- No predisposing factors (Mod Pathol 2017;30:761)
Sites
- Usually have generalized skin involvement (J Am Acad Dermatol 2012;67:748, Am J Clin Pathol 2013;139:491, Mod Pathol 2017;30:761, Histopathology 2015;67:425)
- Variable distribution in cases with localized involvement: upper / lower extremities, trunk, head and neck (Mod Pathol 2017;30:761)
- Oral mucosa or perioral skin involvement may be present (J Am Acad Dermatol 2012;67:748, Am J Clin Pathol 2013;139:491, Histopathology 2015;67:425, J Am Acad Dermatol 2010;62:300, Am J Pathol 1999;155:483)
- High tendency to spread to extranodal sites (J Am Acad Dermatol 2012;67:748, Am J Clin Pathol 2013;139:491, Histopathology 2015;67:425, J Am Acad Dermatol 2010;62:300, Am J Pathol 1999;155:483)
- Lung, testis, CNS, liver, spleen and heart
- Lymph node and bone marrow involvement are rare (J Am Acad Dermatol 2012;67:748, Am J Clin Pathol 2013;139:491, Histopathology 2015;67:425, Am J Pathol 1999;155:483)
Clinical features
- Rapidly progressive (J Am Acad Dermatol 2012;67:748, Mod Pathol 2017;30:761, Histopathology 2015;67:425, J Am Acad Dermatol 2010;62:300, Am J Pathol 1999;155:483)
- Diffuse eruptive papules, patches, plaques, nodules and tumors with central ulceration and necrosis (J Am Acad Dermatol 2012;67:748, Mod Pathol 2017;30:761, Histopathology 2015;67:425, J Am Acad Dermatol 2010;62:300, Am J Pathol 1999;155:483)
- Uncommon presentation as superficial hyperkeratotic patches and plaques clinically resembling pagetoid reticulosis of the Ketron-Goodman type (J Am Acad Dermatol 2012;67:748, Mod Pathol 2017;30:761, J Am Acad Dermatol 2010;62:300)
Diagnosis
- Combination of clinical, histopathological and immunohistochemical features (J Am Acad Dermatol 2012;67:748)
- Diagnostic criteria (J Am Acad Dermatol 2012;67:748)
- Constant features
- Aggressive clinical course with few weeks evolution
- Widespread ulcerated papules, plaques and tumors without precursor lesion
- Epidermotropism and nodular or diffuse dermal pleomorphic T cell infiltrate
- CD8+ / CD4-
- Variable features
- Pyoderma gangrenosum-like, pagetoid reticulosis-like and annular erythematous scaling patches
- Spongiosis, blisters and necrosis
- Deep lymphoid infiltrate, angiocentrism and angiodestruction
- Variable expression of CD2, CD7, CD15, CD45 and CD56
- Constant features
Prognostic factors
- Unfavorable prognosis and aggressive clinical course (J Am Acad Dermatol 2012;67:748, Mod Pathol 2017;30:761, Histopathology 2015;67:425, J Am Acad Dermatol 2010;62:300, Am J Pathol 1999;155:483)
- Median survival: 22 - 32 months
- 5 year overall survival: 18 - 32%
- Worst prognosis in patients presenting with tumors at diagnosis (Mod Pathol 2017;30:761)
- Survival not influenced by cell size (small versus large), distribution (localized versus disseminated) or immunophenotype groups (Mod Pathol 2017;30:761)
Case reports
- 16 year old boy with primary cutaneous aggressive epidermotropic CD8+ T cell lymphoma with cerebral infiltration and treated with cord blood stem cell transplant (SCT) (Intern Med 2018;57:2051)
- 19 year old woman with primary cutaneous aggressive epidermotropic CD8+ T cell lymphoma simulating pyoderma gangrenosum (Clin Exp Dermatol 2009;34:e261)
- 29 year old woman with primary cutaneous aggressive epidermotropic CD8+ T cell lymphoma and homozygous mutation in SAMHD1 (JAAD Case Rep 2015;1:227)
- 47 year old man with primary cutaneous aggressive epidermotropic CD8+ T cell lymphoma and complete durable remission after autologous and allogeneic hematopoietic stem cell transplantation (JAAD Case Rep 2017;3:196)
- 61 year old man with primary cutaneous aggressive epidermotropic CD8+ T cell lymphoma and history of psoriasis (Ann Dermatol 2018;30:255)
- 68 year old man with lupus-like initial clinical presentation (Indian Dermatol Online J 2019;10:298)
- 72 year old man with primary cutaneous aggressive epidermotropic CD8+ cytotoxic T cell lymphoma of the ear (J Laryngol Otol 2007;121:503)
Treatment
- No definite successful therapy available
- Multiagent chemotherapy: CHOP (cyclophosphamide, hydroxydorubicin, vincristine and prednisone), CHOEP (cyclophosphamide, hydroxydorubicin, vincristine, etoposide and prednisone), hyper-CVAD (hyper-cyclophosphamide, vincristine, doxorubicin, dexamethasone, methotrexate and cytarabine) and MACOP-B (methotrexate, doxorubicin, cyclophosphamide, vincristine, prednisone and bleomycin) (J Am Acad Dermatol 2012;67:748, Mod Pathol 2017;30:761)
- Unsatisfactory and usually partial response
- Total skin electron beam therapy with or without oral retinoid (e.g. bexarotene) (J Am Acad Dermatol 2012;67:748, J Am Acad Dermatol 2010;62:300)
- Partial response and some cases with complete clearance
- Allogeneic or autologous stem cell transplant (SCT) (J Am Acad Dermatol 2012;67:748, Mod Pathol 2017;30:761, J Am Acad Dermatol 2010;62:300)
- Setting of unresponsive or relapse after multiagent chemotherapy or early use of combined intensive chemotherapy and SCT
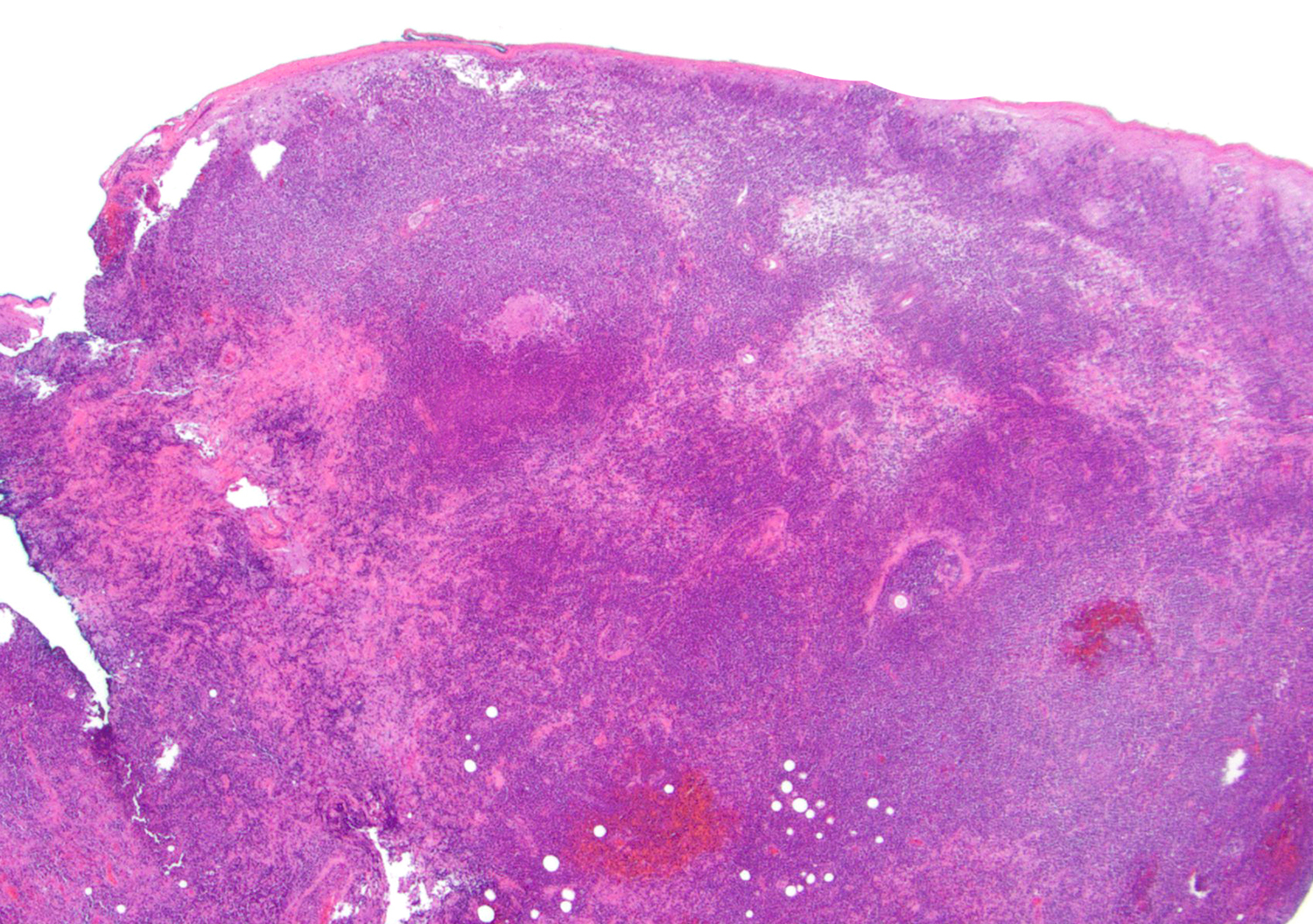
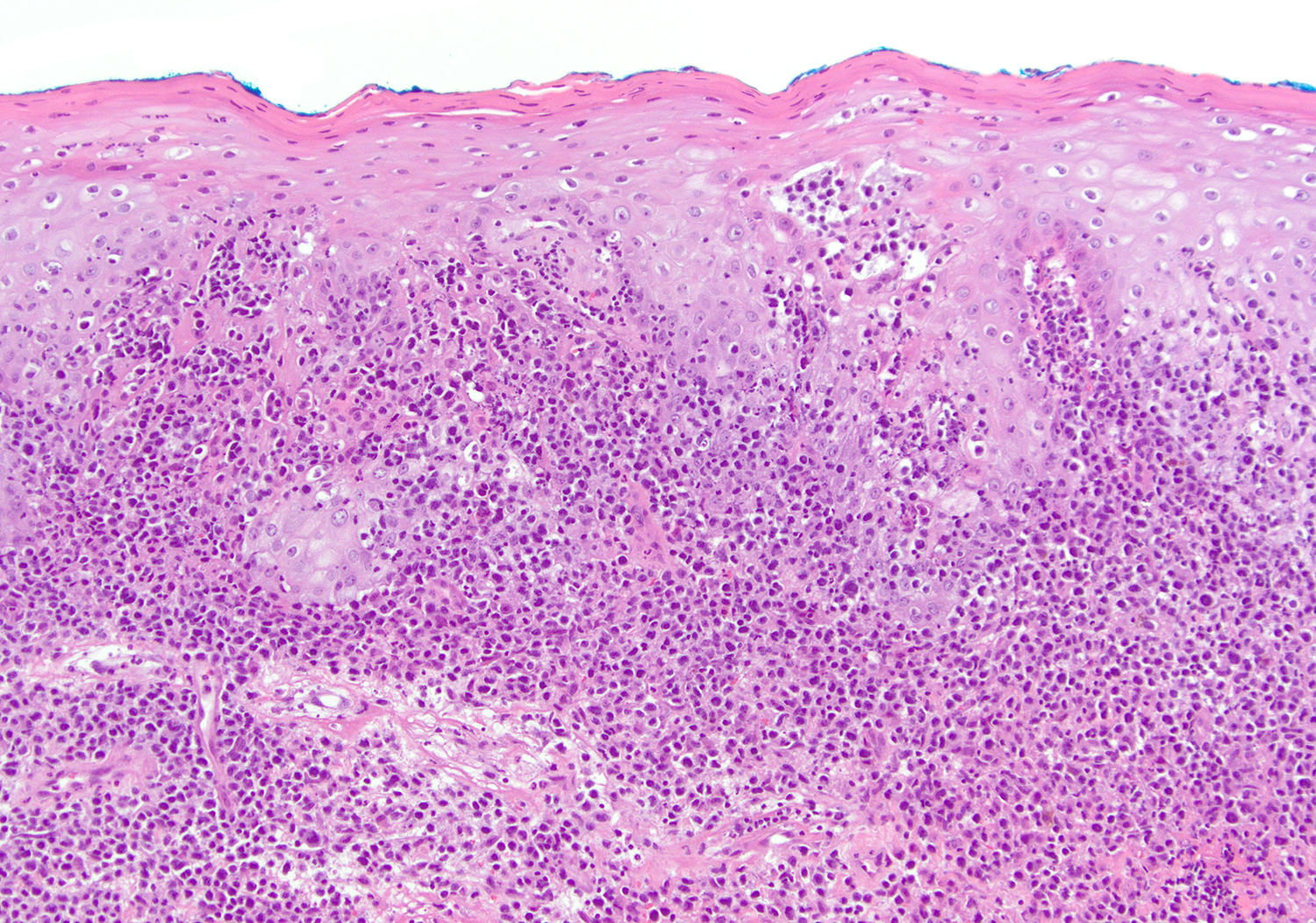
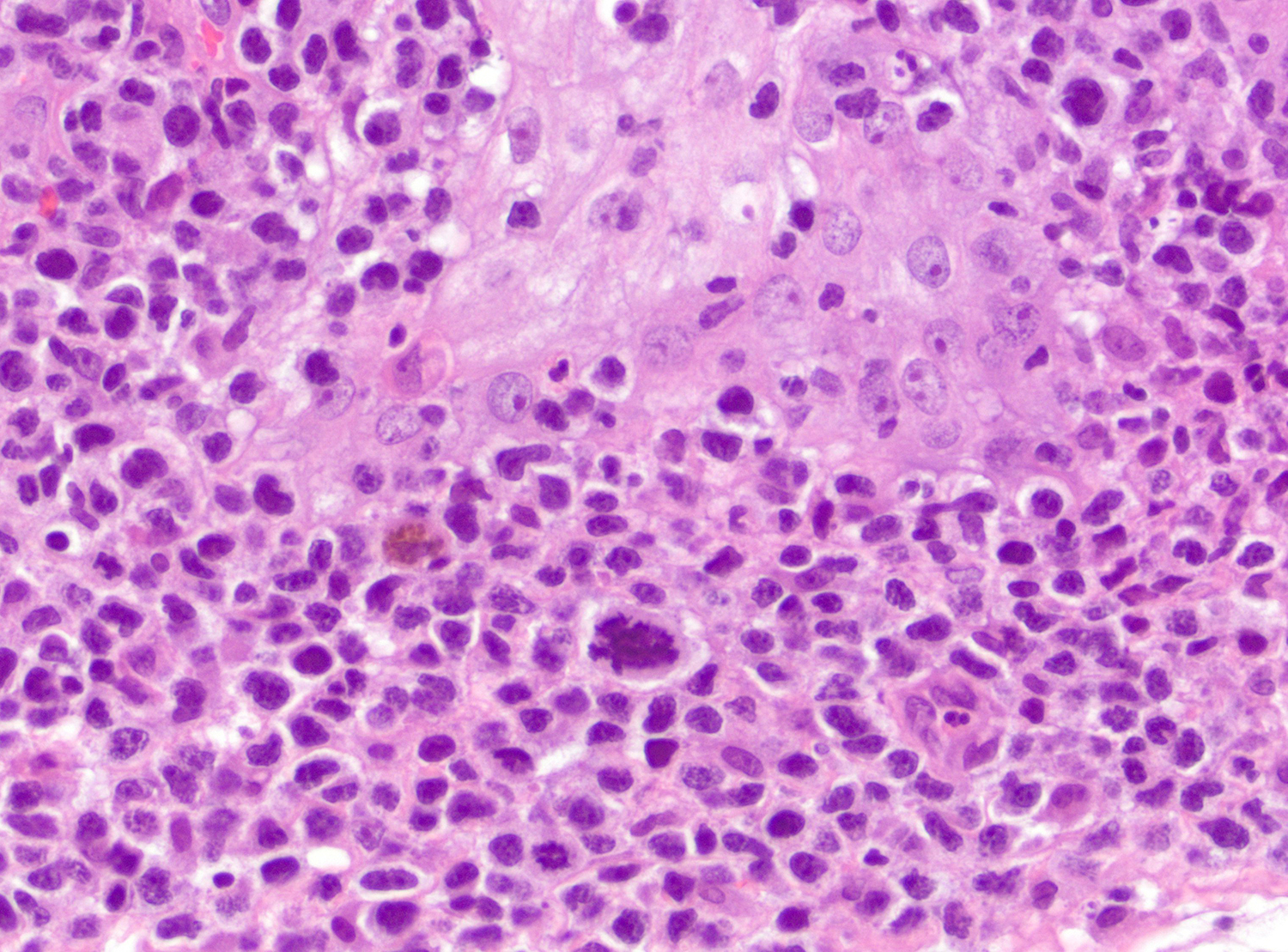
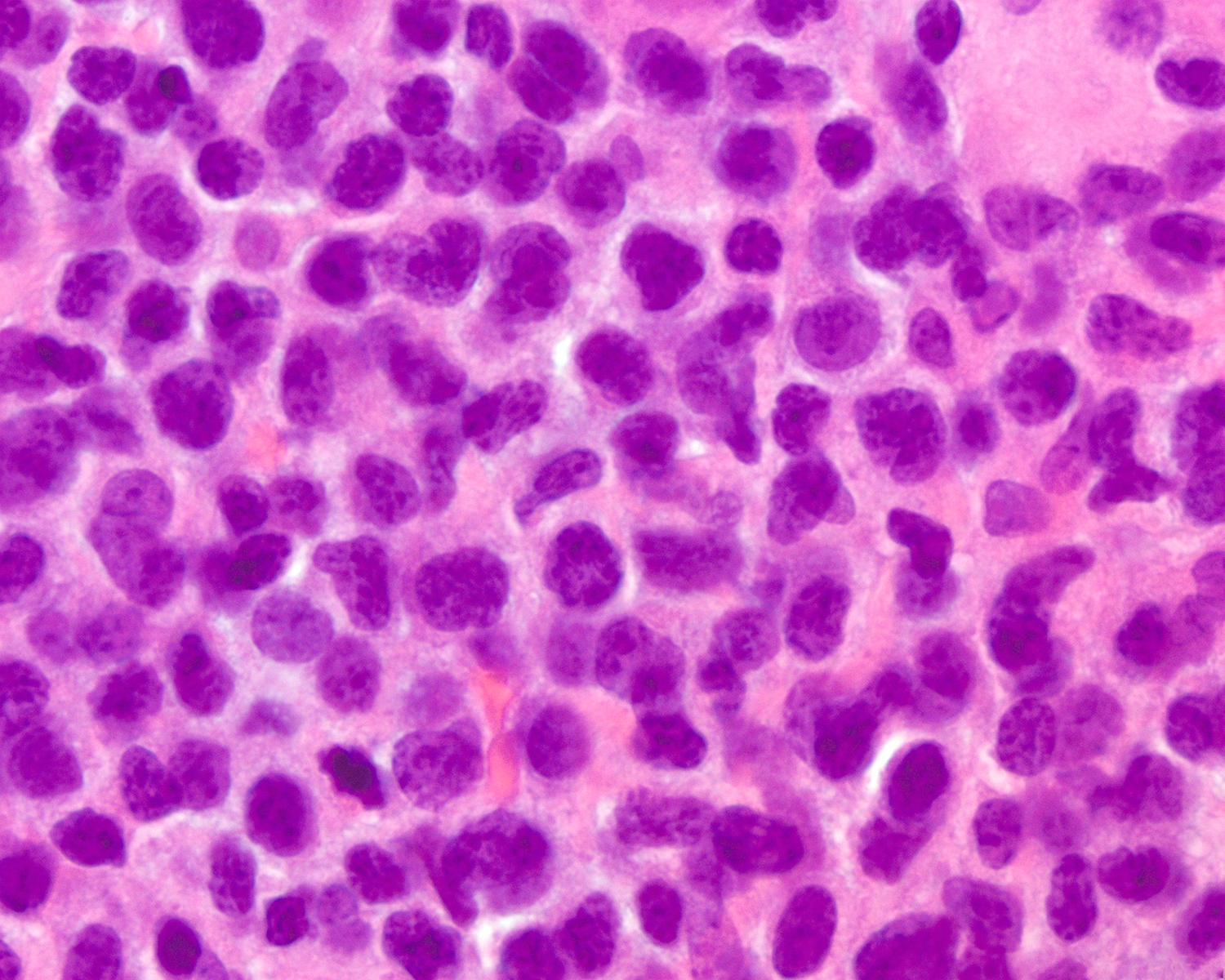
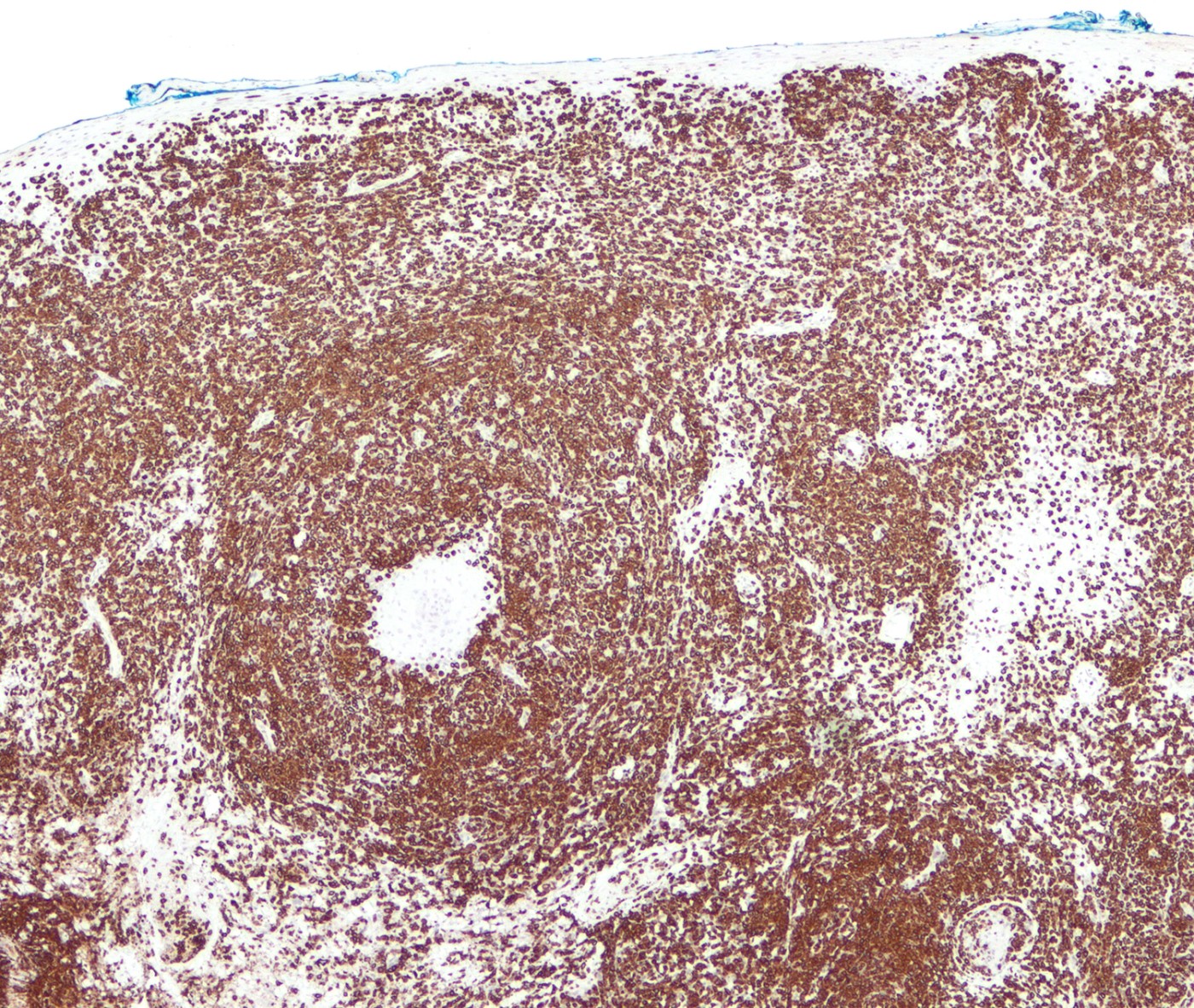
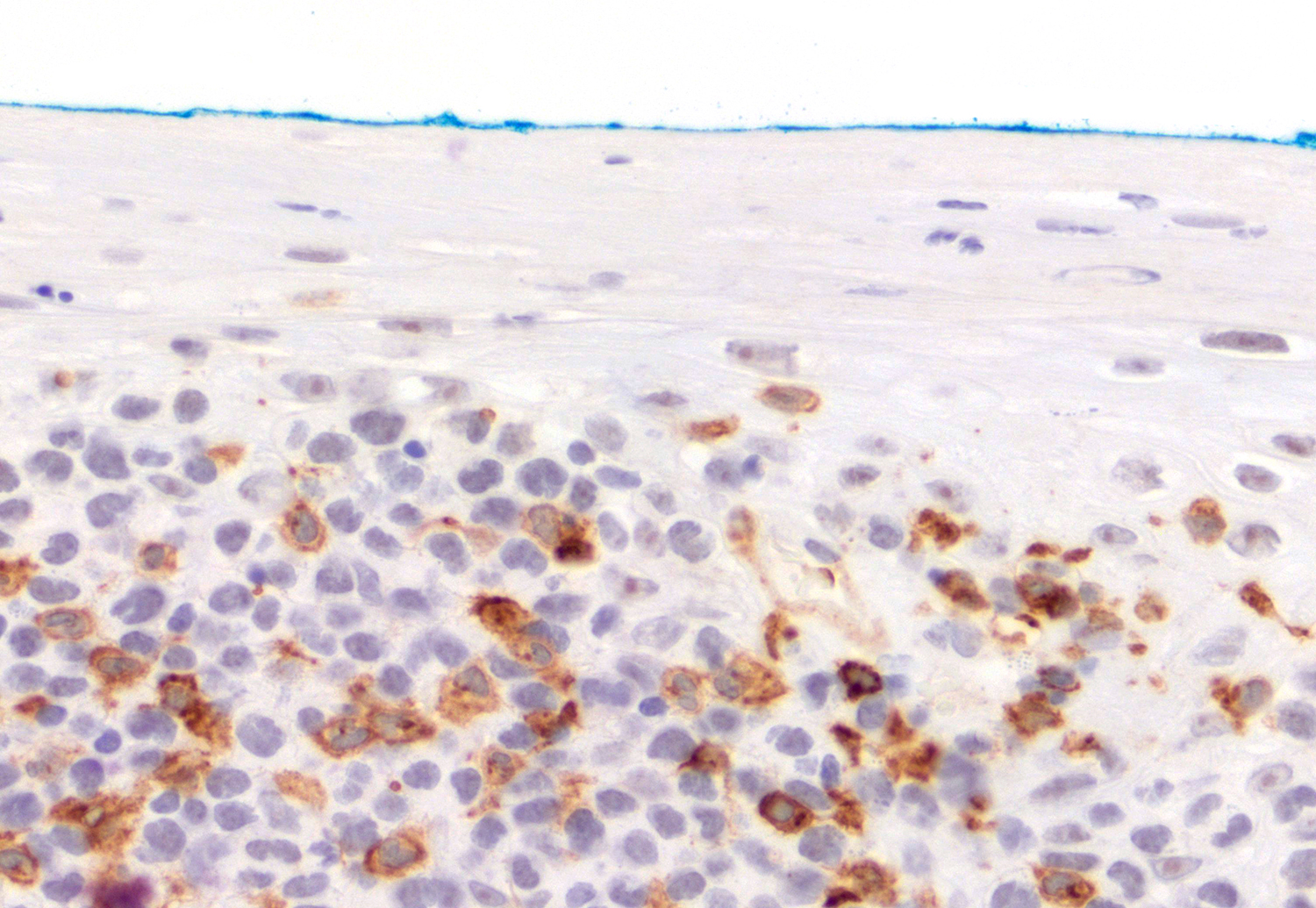
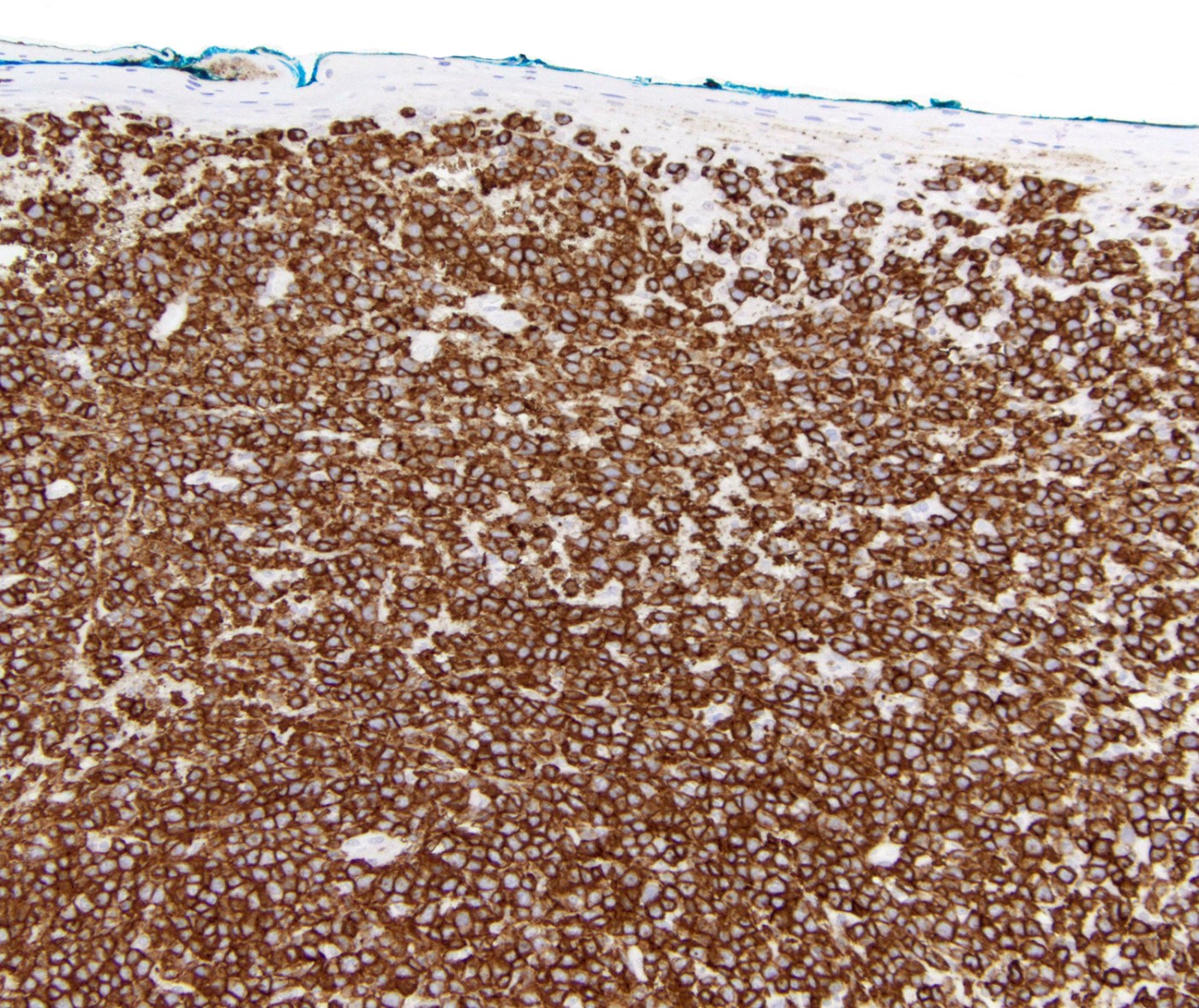
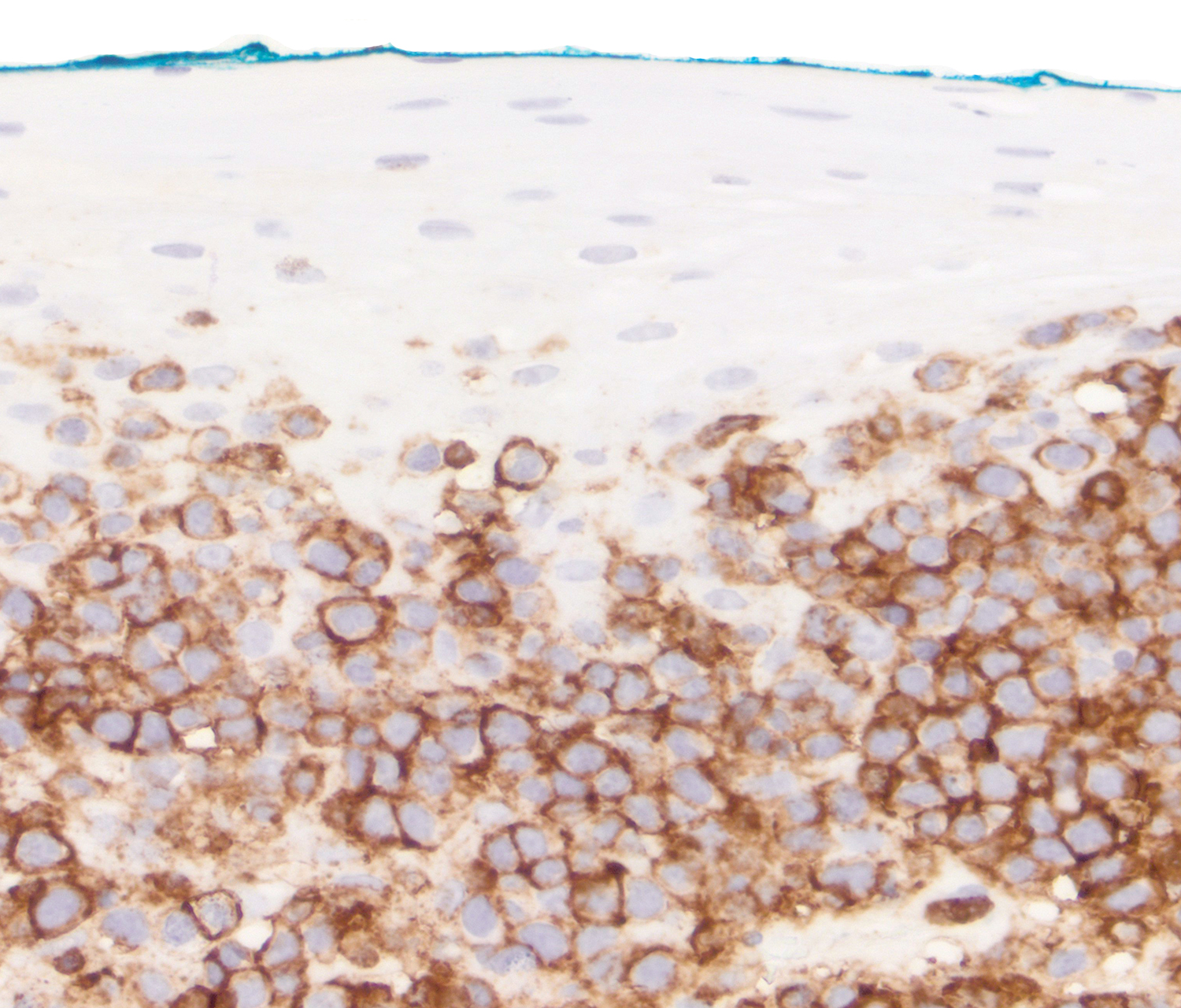
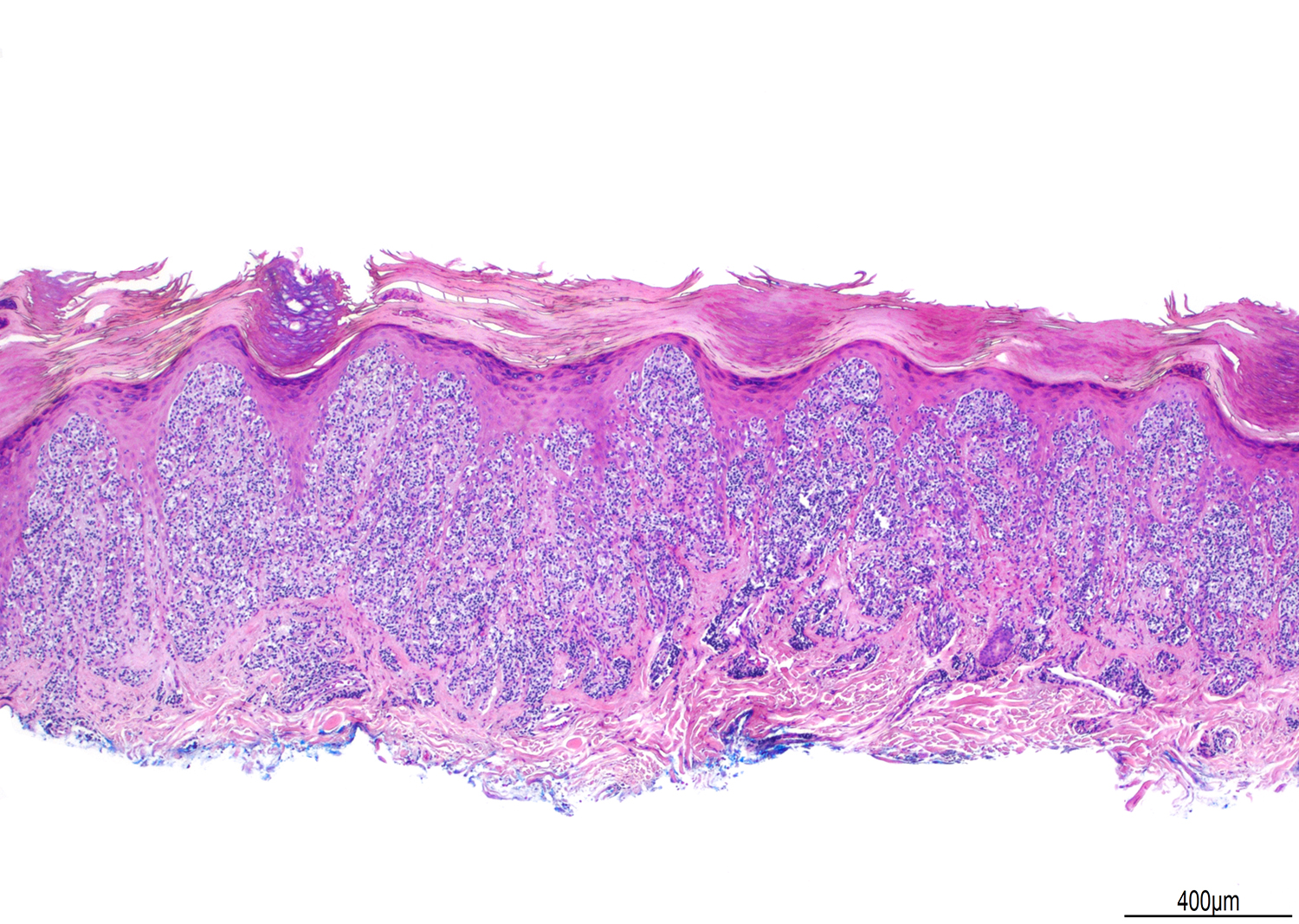
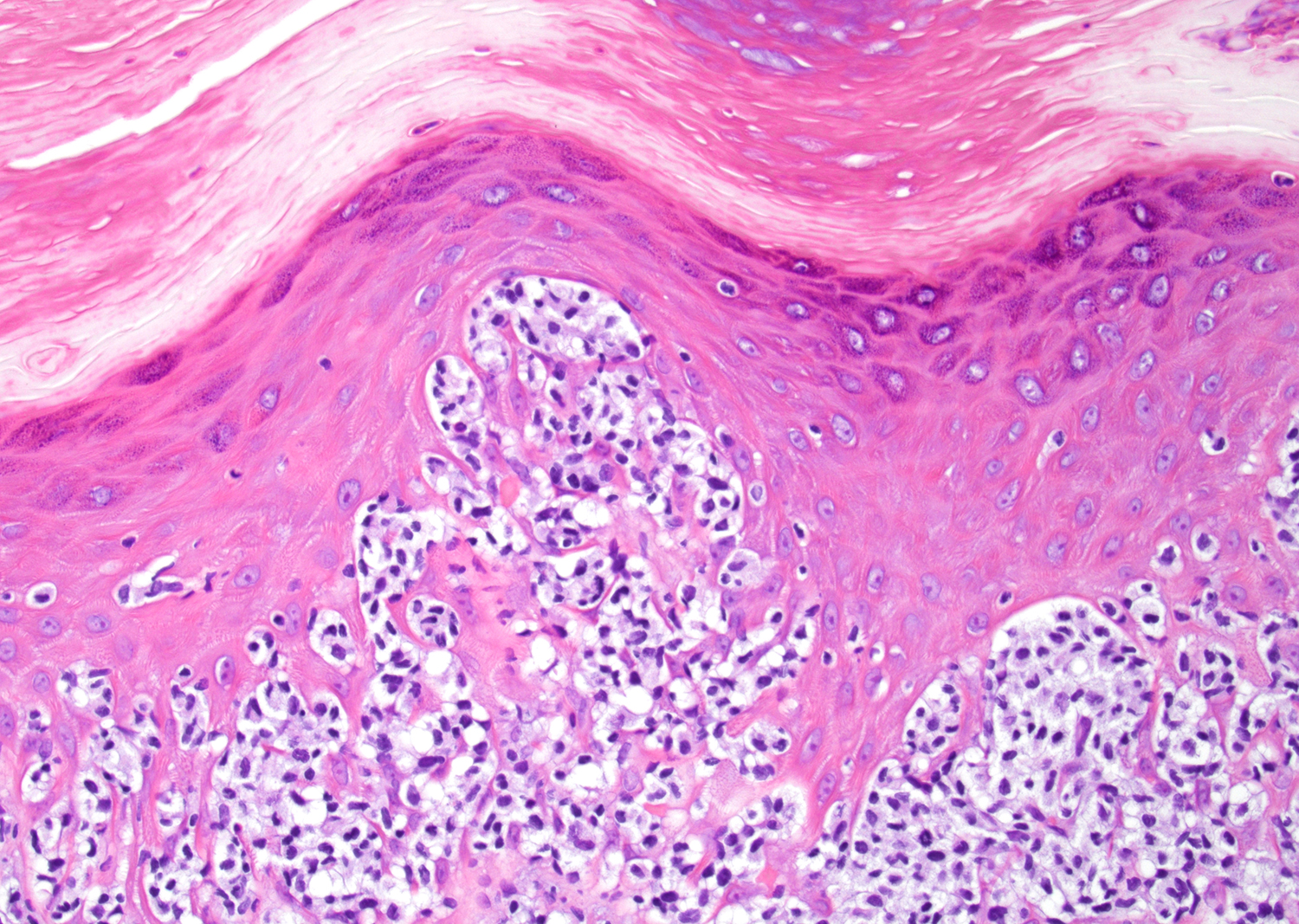
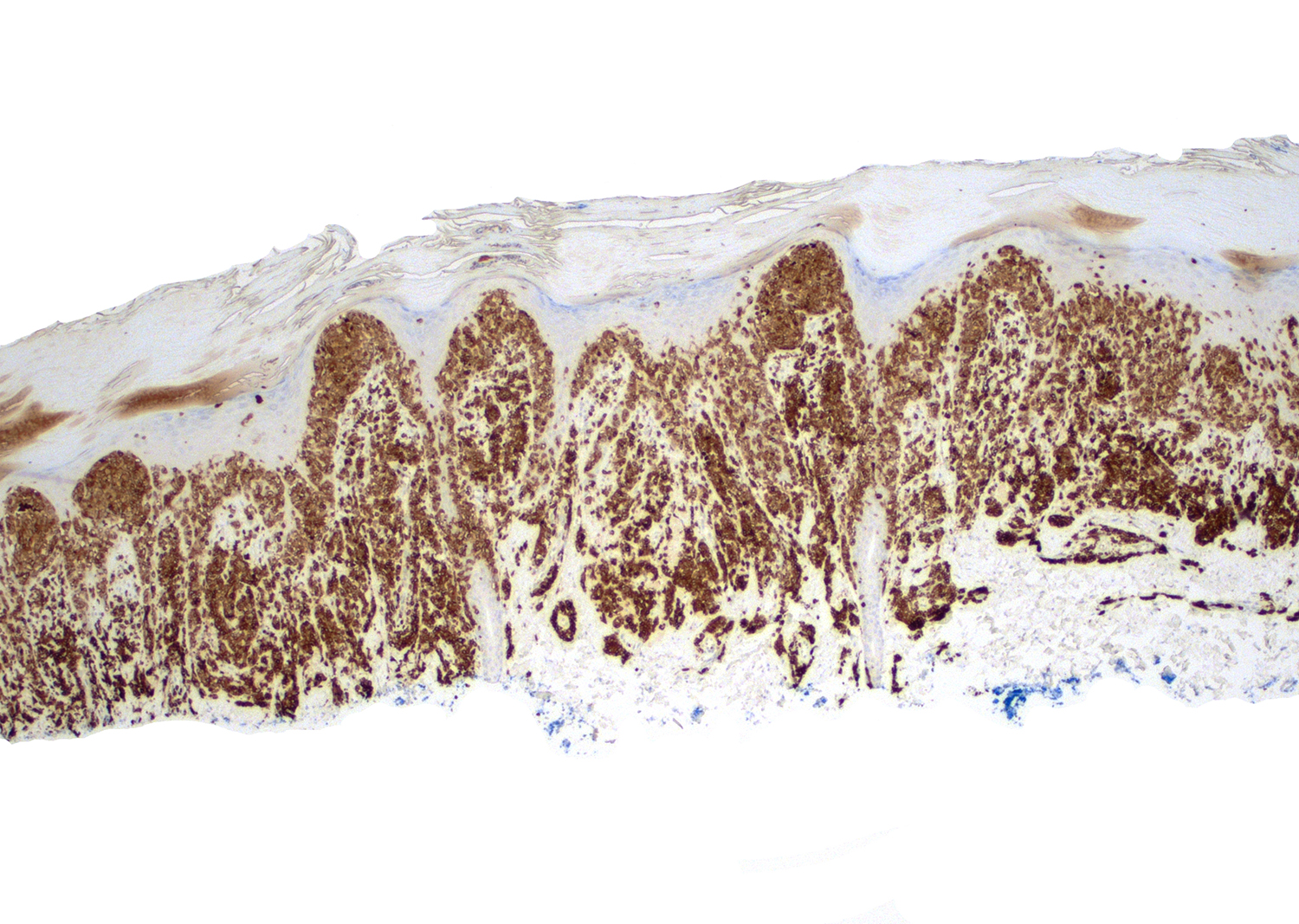
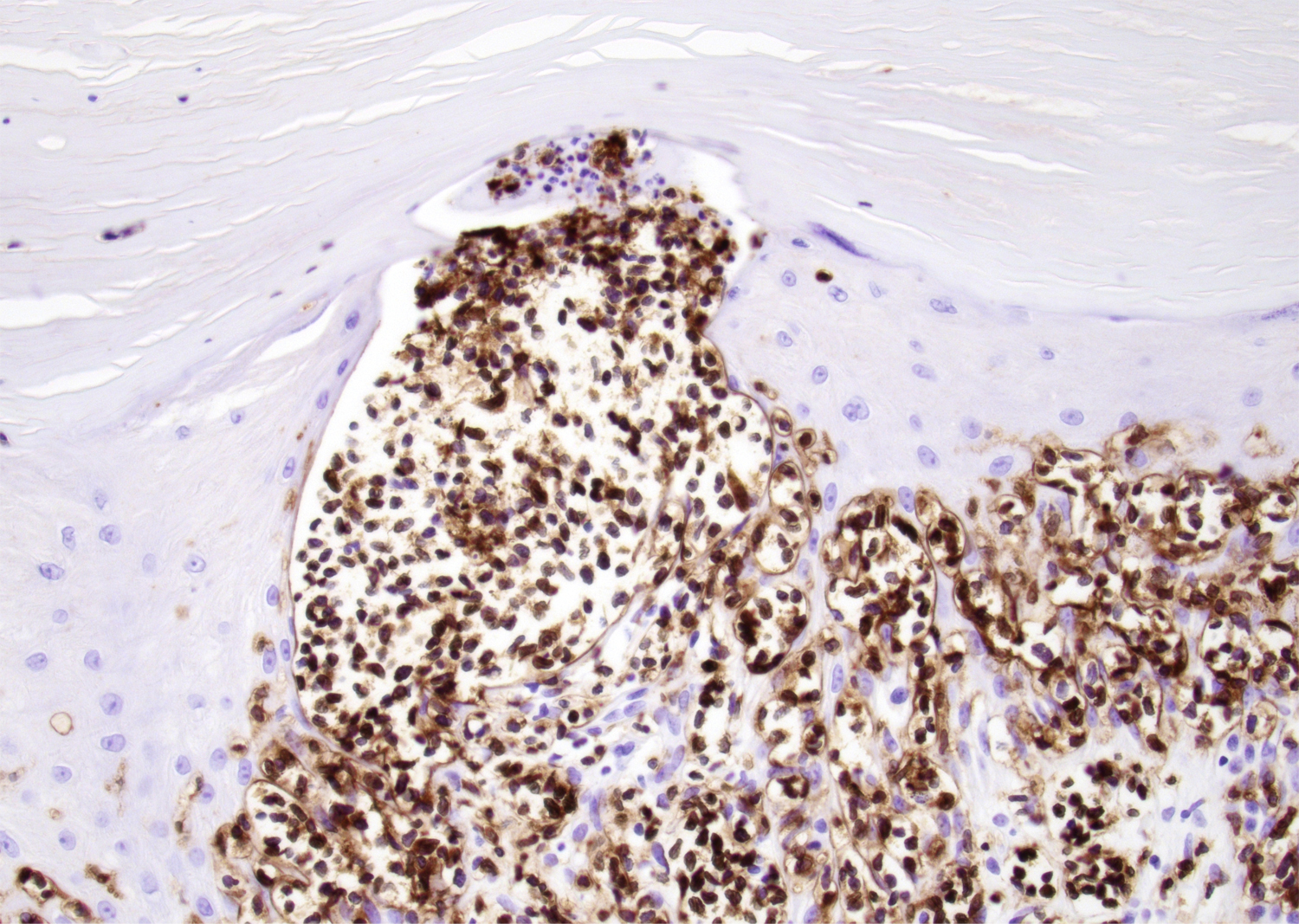
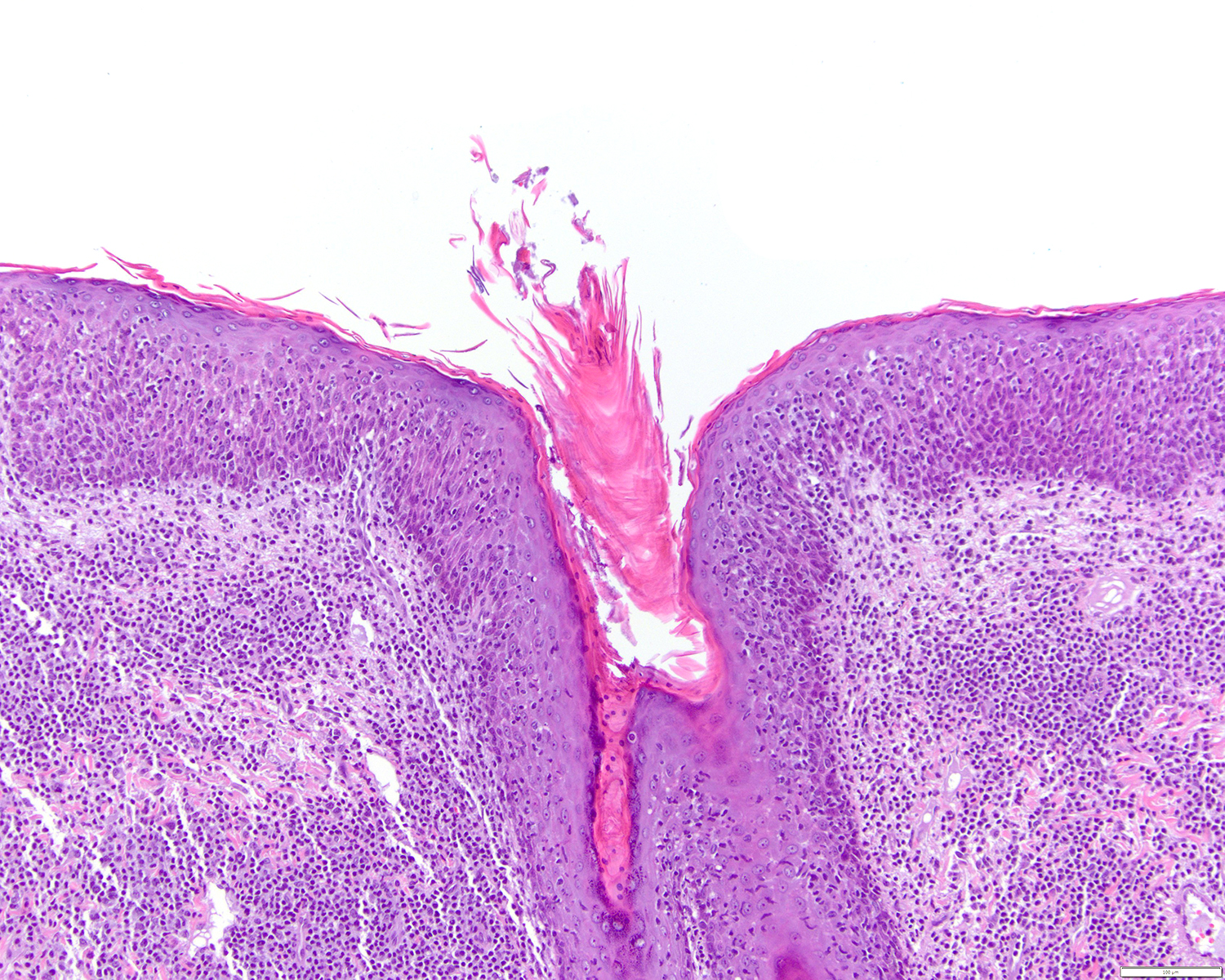
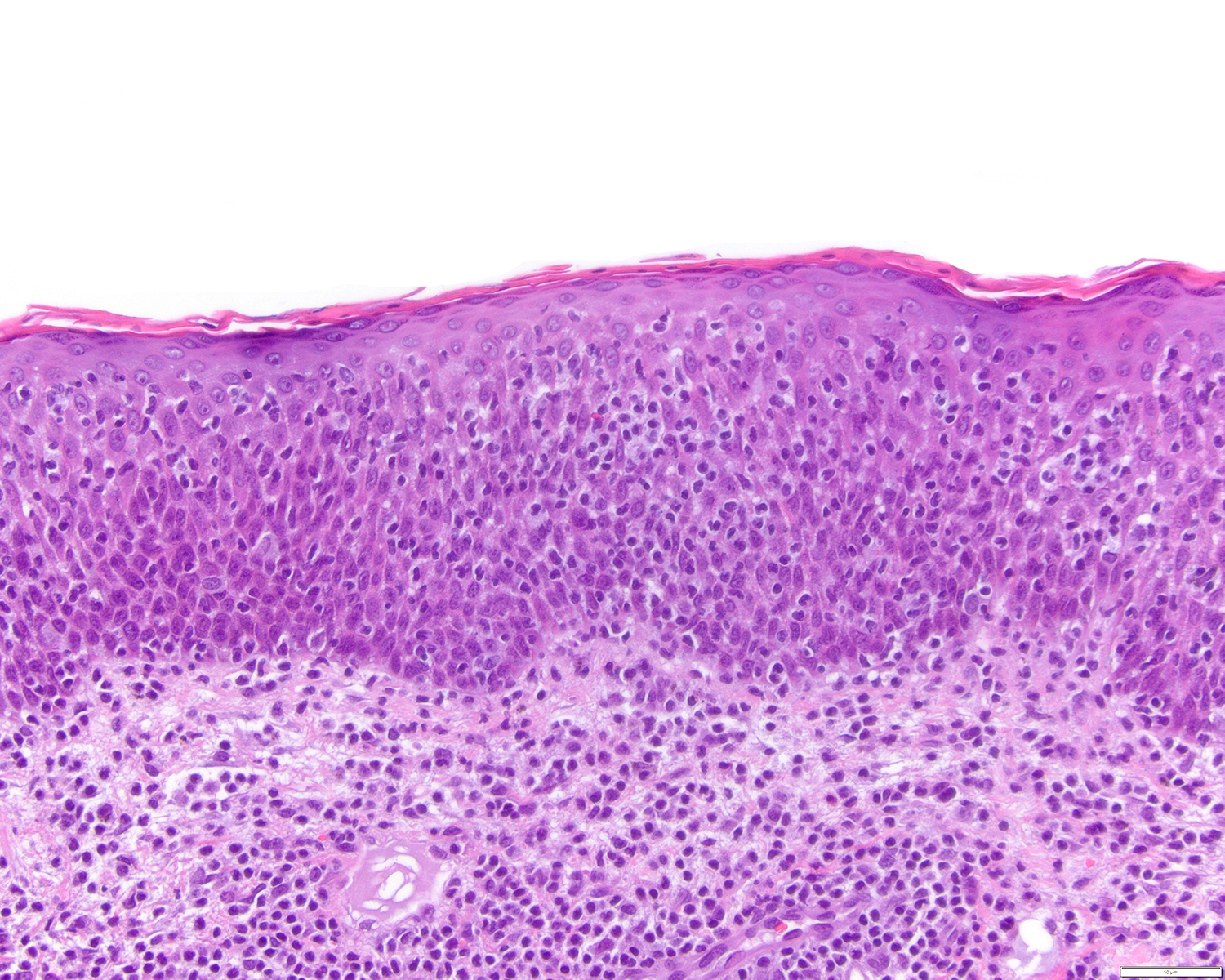
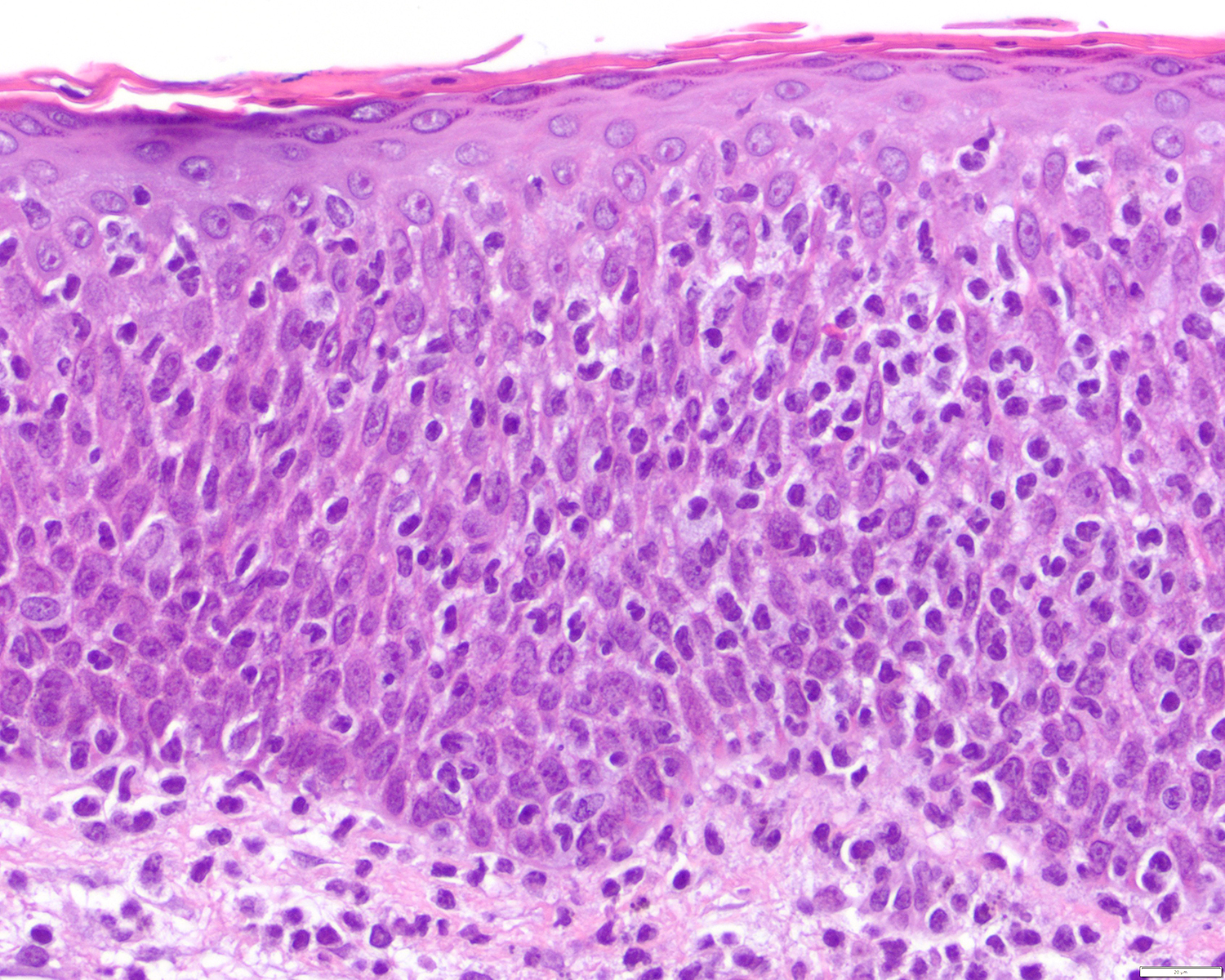
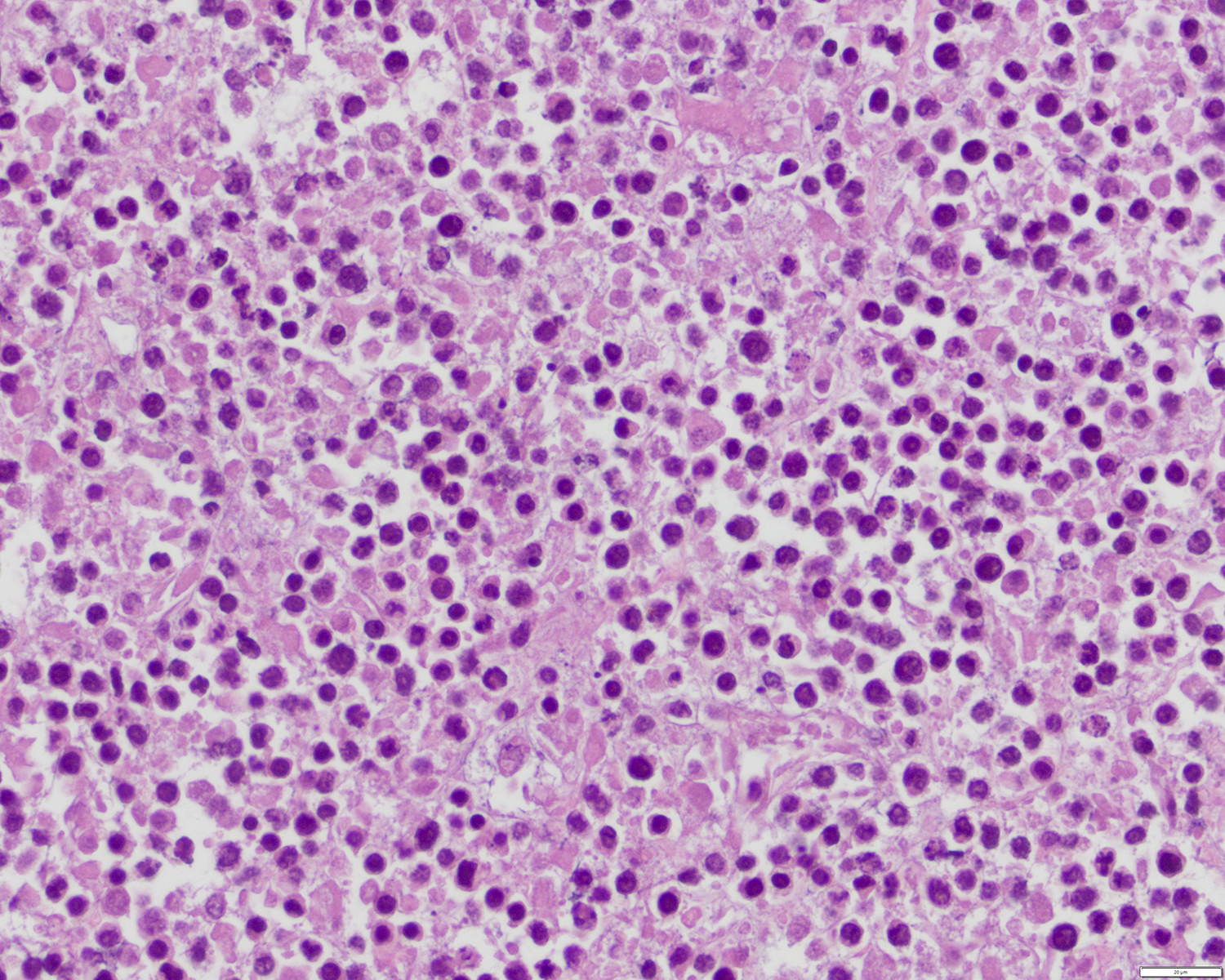
Microscopic (histologic) description
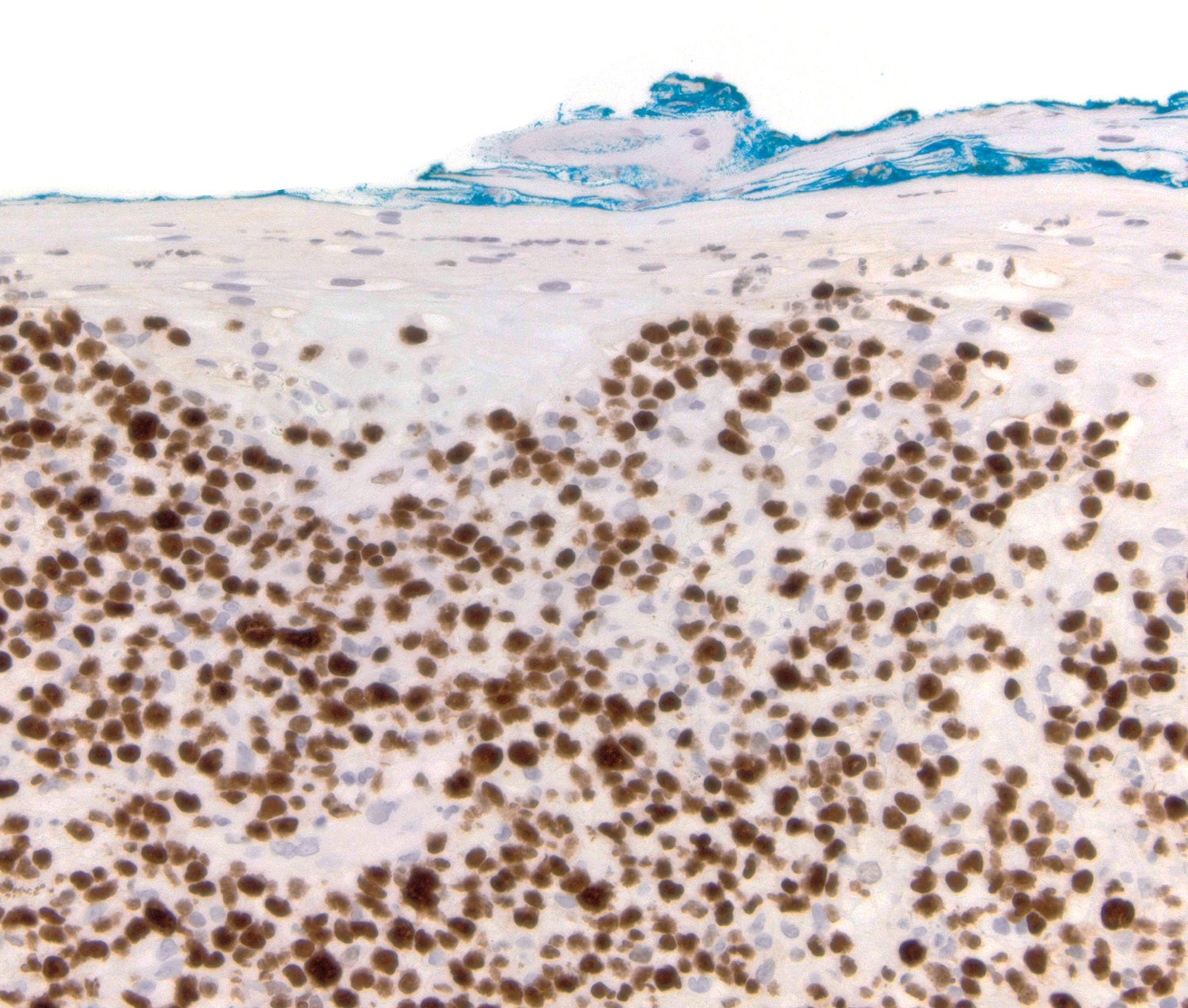
- Epidermotropism (particularly in basal layer) usually followed by a pagetoid or lichenoid pattern (J Am Acad Dermatol 2012;67:748, Am J Clin Pathol 2013;139:491, Mod Pathol 2017;30:761, Histopathology 2015;67:425, Am J Pathol 1999;155:483)
- Rare cases with absence of epidermotropism (J Am Acad Dermatol 2012;67:748)
- Dermal infiltrate with lymphocytes of variable size (small to large), pleomorphic cytology, nodular or diffuse pattern and deep extension into dermis down to subcutaneous (J Am Acad Dermatol 2012;67:748, Mod Pathol 2017;30:761, Histopathology 2015;67:425, Am J Pathol 1999;155:483)
- Folliculotropism, syringotropism, angiocentrism and angioinvasion may be present (J Am Acad Dermatol 2012;67:748, Am J Clin Pathol 2013;139:491, Mod Pathol 2017;30:761, Histopathology 2015;67:425, J Am Acad Dermatol 2010;62:300)
- Other findings: acanthosis, spongiosis, blistering and necrosis (J Am Acad Dermatol 2012;67:748, Mod Pathol 2017;30:761, Histopathology 2015;67:425, J Am Acad Dermatol 2010;62:300, Am J Pathol 1999;155:483)
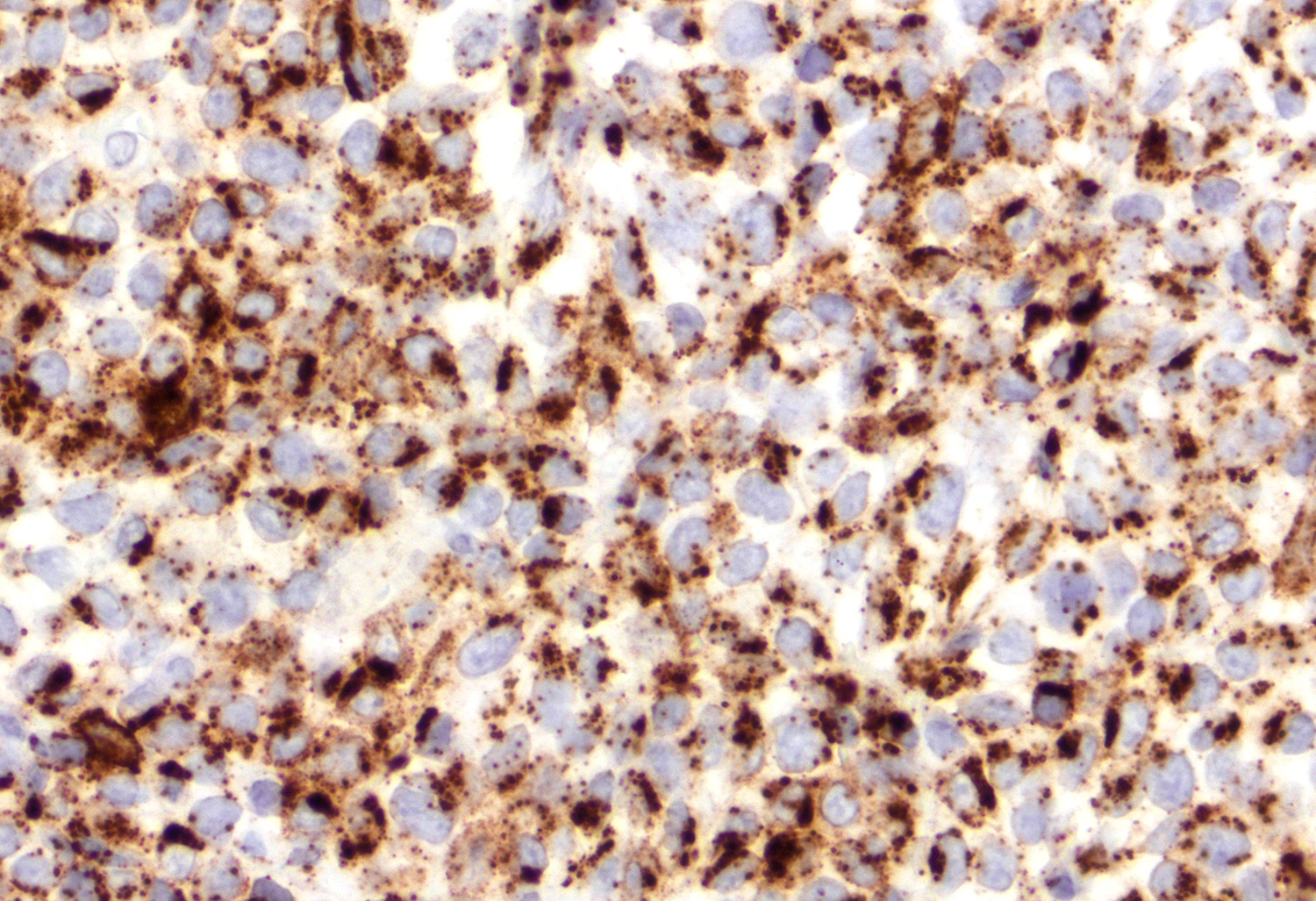
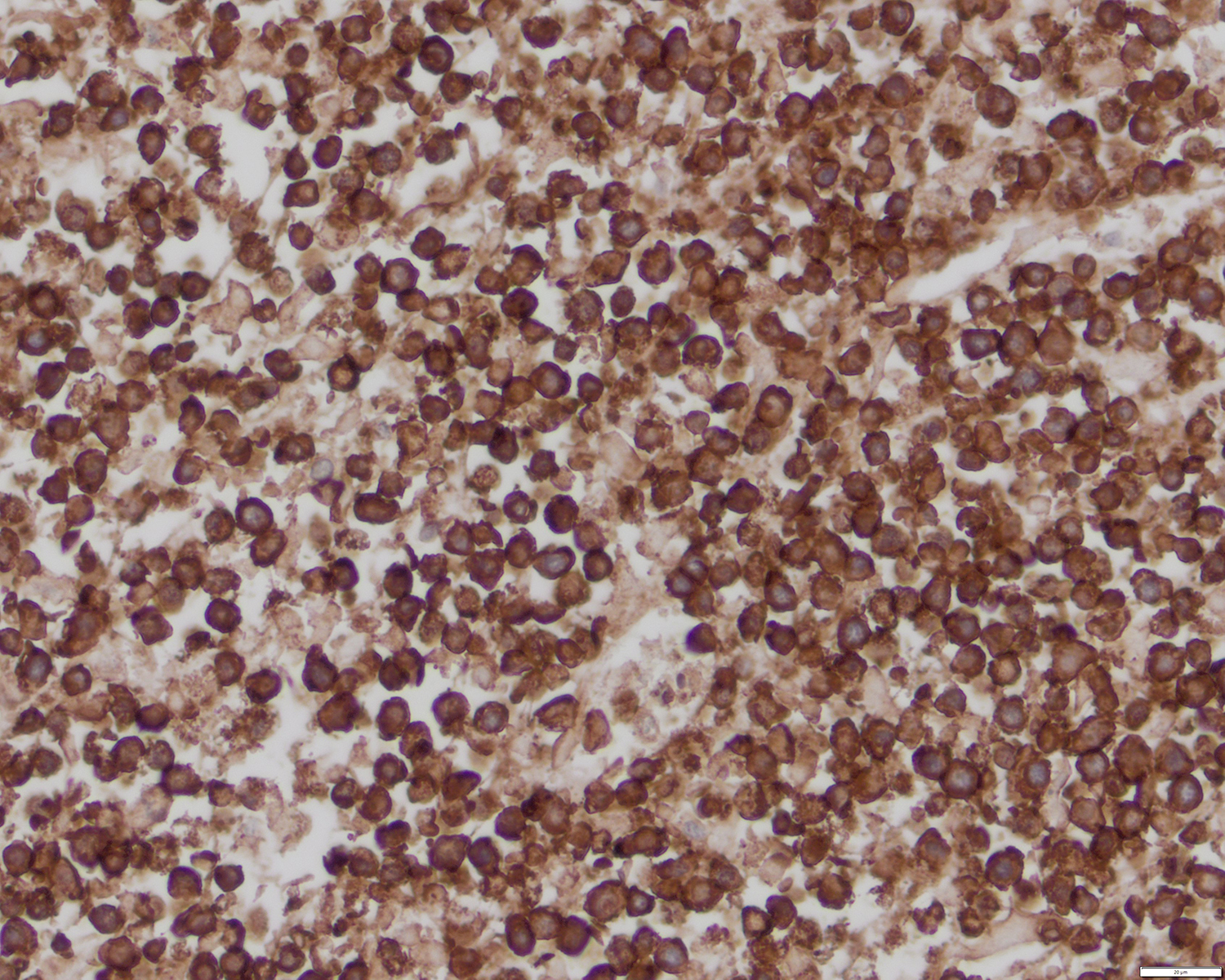
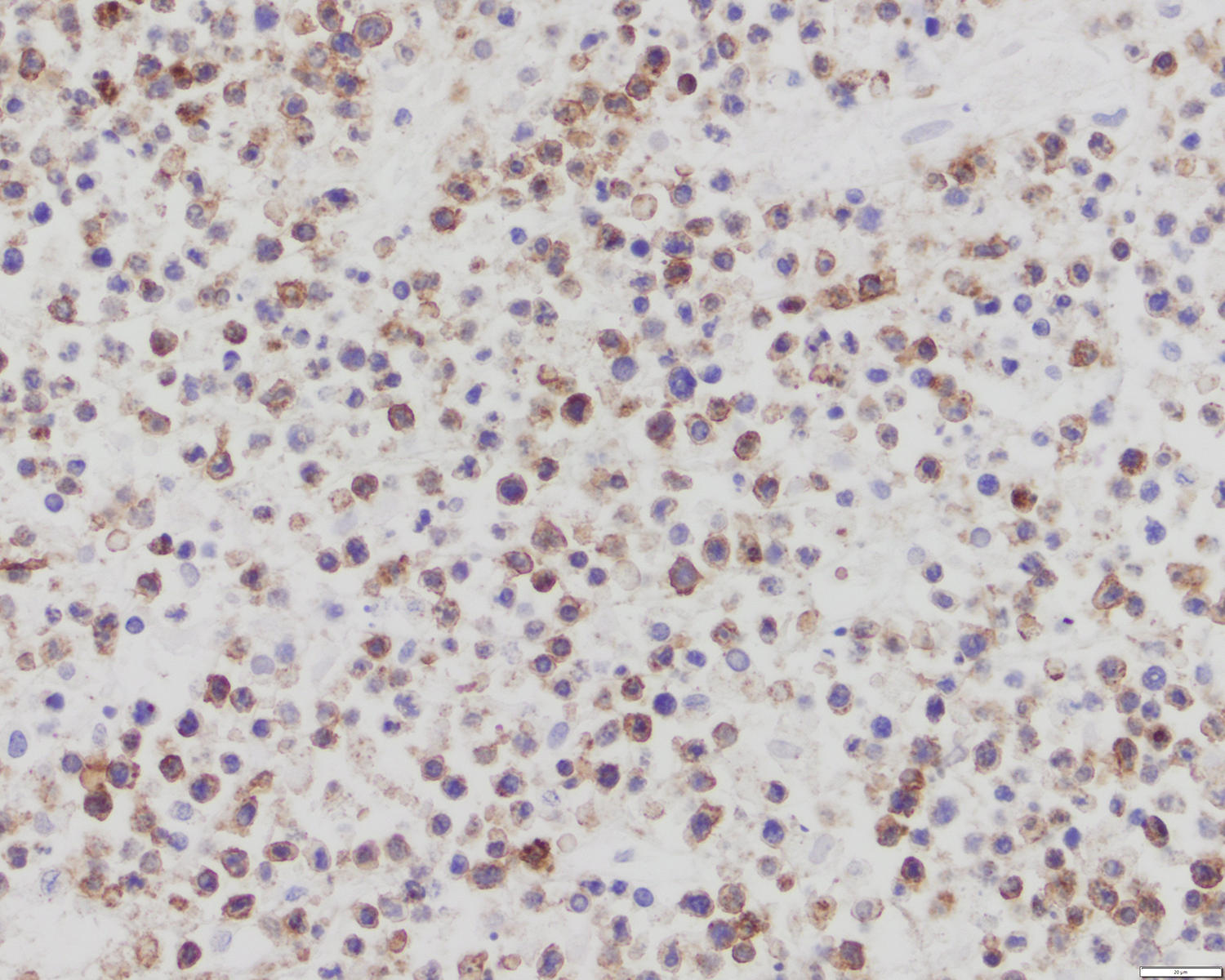
Microscopic (histologic) images
Contributed by Roberto N. Miranda, M.D.
Positive stains
- CD3, CD8 and CD45RA (J Am Acad Dermatol 2012;67:748, Am J Clin Pathol 2013;139:491, Mod Pathol 2017;30:761, J Am Acad Dermatol 2010;62:300, Am J Pathol 1999;155:483)
- Very rare cases of double CD4 / CD8 negativity (Mod Pathol 2017;30:761)
- Cytotoxic granules: TIA1, granzyme B and perforin (Am J Clin Pathol 2013;139:491, Mod Pathol 2017;30:761, Histopathology 2015;67:425, J Am Acad Dermatol 2010;62:300, Am J Pathol 1999;155:483)
- Variable CD2 and CD7 (J Am Acad Dermatol 2012;67:748, Am J Clin Pathol 2013;139:491, Mod Pathol 2017;30:761, Histopathology 2015;67:425, J Am Acad Dermatol 2010;62:300, Am J Pathol 1999;155:483, Oncol Ther 2016;4:199)
- BCL2 (Am J Pathol 1999;155:483)
- βF1 (Am J Clin Pathol 2013;139:491, Mod Pathol 2017;30:761, Histopathology 2015;67:425, J Am Acad Dermatol 2010;62:300, Am J Pathol 1999;155:483)
- Ki67 (often > 75%) (J Am Acad Dermatol 2012;67:748, Am J Clin Pathol 2013;139:491, Histopathology 2015;67:425)
Negative stains
- CD4, CD5 and CD15 (J Am Acad Dermatol 2012;67:748, Mod Pathol 2017;30:761, J Am Acad Dermatol 2010;62:300, Oncol Ther 2016;4:199)
- CD30 (J Am Acad Dermatol 2012;67:748, Am J Clin Pathol 2013;139:491, Mod Pathol 2017;30:761, Histopathology 2015;67:425)
- Rare cases of partial positivity (Mod Pathol 2017;30:761)
- CD25 (Am J Pathol 1999;155:483)
- CD1a (Am J Pathol 1999;155:483)
- ALK1 (J Am Acad Dermatol 2010;62:300)
- CD56 and CD57 (J Am Acad Dermatol 2012;67:748, Mod Pathol 2017;30:761, Histopathology 2015;67:425, J Am Acad Dermatol 2010;62:300)
- CD45RO (J Am Acad Dermatol 2012;67:748, Am J Clin Pathol 2013;139:491, Histopathology 2015;67:425, J Am Acad Dermatol 2010;62:300)
- Epstein-Barr virus: EBER, EBNA2 and LMP1 (J Am Acad Dermatol 2012;67:748, Am J Clin Pathol 2013;139:491, Mod Pathol 2017;30:761, Histopathology 2015;67:425, J Am Acad Dermatol 2010;62:300, Am J Pathol 1999;155:483)
Molecular / cytogenetics description
- Clonal TR rearrangement (J Am Acad Dermatol 2012;67:748, Mod Pathol 2017;30:761, J Am Acad Dermatol 2010;62:300, Am J Pathol 1999;155:483)
- Haploinsufficiency for TP53 (Ann Dermatol 2018;30:255)
Sample pathology report
- Ulcerated plaque of the trunk, skin punch biopsy:
- Primary cutaneous T cell lymphoma, most consistent with primary cutaneous CD8+ aggressive epidermotropic cytotoxic T cell lymphoma (see comment)
- Comment: Section shows an adequate skin punch biopsy with intense epidermotropism, focal epidermal necrosis, acanthosis and spongiosis. There is an extensive, nodular and diffuse dermal infiltrate composed of variably sized, pleomorphic lymphocytes with irregular nuclear contours, hyperchromatic nuclei and scant cytoplasm. Immunohistochemical studies show that the abnormal lymphocytes are diffusely positive for CD3, CD7, CD8, CD45RA, TIA1, T cell receptor beta (βF1) and granzyme B. The atypical cells are negative for CD2, CD4, CD5, CD56, EBER, CD30, T cell receptor gamma / delta and ALK1. The Ki67 proliferation index is approximately 70%. According to clinical notes, the patient is a 63 year old man with history of hypertension. The patient presented to the department of dermatology with a 5 week history of ulcerated plaques, papules and nodules in the upper and lower limbs, trunk, head, neck, tongue and perioral area. A computed tomography (CT) showed multiple nodules in liver, without evidence of lymphadenopathy. The final diagnosis is most consistent with primary cutaneous CD8+ aggressive epidermotropic cytotoxic T cell lymphoma.
Differential diagnosis
- Lymphomatoid papulosis (LyP) type D (Am J Clin Pathol 2013;139:491, Histopathology 2015;67:425):
- Clinical presentation as waxing and waning papules and nodules
- Some cases are histologically indistinguishable from primary cutaneous CD8+ aggressive epidermotropic cytotoxic T cell lymphoma
- Wedge shaped infiltrate of medium size pleomorphic T cells with cytotoxic phenotype
- Large cells with strong and uniform expression of CD30
- May be associated or preceded by other lymphoid malignancies such as mycosis fungoides
- Good prognosis
- Primary cutaneous anaplastic large cell lymphoma (Am J Clin Pathol 2013;139:491):
- Large cells with strong and uniform expression of CD30
- Localized disease
- Subcutaneous panniculitis-like T cell lymphoma (Am J Clin Pathol 2013;139:491, Am J Surg Pathol 2004;28:719):
- Solitary or multiple infiltrated subcutaneous nodules or deeply seated plaques
- Dissemination to extracutaneous sites is rare
- Overlying dermis and epidermis typically uninvolved
- Pleomorphic cells admixed with histiocytes
- Excellent prognosis
- Primary cutaneous acral CD8+ T cell lymphoma (Oncol Ther 2016;4:199):
- Extranodal NK / T cell lymphoma, nasal type (Am J Clin Pathol 2013;139:491, Am J Surg Pathol 2004;28:719):
- Solitary pagetoid reticulosis (Woringer-Kolopp disease) (Histopathology 2015;67:425):
- Primary cutaneous γδ T cell lymphoma (Am J Clin Pathol 2013;139:491, Mod Pathol 2017;30:761, Am J Surg Pathol 2004;28:719):
- Composed of mature γδ T cells
- Uncommon epidermotropism
- Medium to large shape with clumped chromatin
- No involvement of mucosae; rare involvement of extranodal sites
- Mycosis fungoides (J Am Acad Dermatol 2012;67:748, Histopathology 2015;67:425, J Am Acad Dermatol 2010;62:300, Oncol Ther 2016;4:199):
- Longer clinical history with typical progression: patch → plaque → tumor
- Cerebriform morphology
- Frequent lack of CD7
- Rare mucosal involvement
- Common lymph node involvement with variable histologic appearance and pathologic staging
- Rare ulceration, angiocentricity and angioinvasion
- Needs systemic chemotherapy in longstanding and advanced disease
- Good prognosis
- Secondary cutaneous involvement of peripheral T cell lymphoma
(Am J Clin Pathol 2013;139:491):
- Exclusion diagnostic: always rule out the other defined entities
- Small size morphology and CD4+
- Secondary skin involvement; unusual confined to cutaneous sites
Additional references
Board review style question #1
- What immunophenotype is more commonly expressed by primary cutaneous CD8+ aggressive epidermotropic cytotoxic T cell lymphoma?
- CD3+ / CD4- / CD7- / CD8+ / CD30- / EBER-
- CD3+ / CD4- / CD7+ / CD8+ / CD30- / EBER+
- CD3+ / CD4+ / CD7+ / CD8+ / CD30- / EBER+
- CD3+ / CD4+ / CD7+ / CD8+ / CD30+ / EBER-
Board review style answer #1
A. CD3+ / CD4- / CD7- / CD8+ / CD30- / EBER-
Comment Here
Reference: Primary cutaneous CD8+ aggressive epidermotropic T cell lymphoma
Comment Here
Reference: Primary cutaneous CD8+ aggressive epidermotropic T cell lymphoma
Board review style question #2
- What is a consistent feature for the diagnostic criteria of primary cutaneous CD8+ aggressive epidermotropic T cell lymphoma?
- Pyoderma gangrenosum-like
- Spongiosis, blistering and necrosis
- Variable expression of CD2, CD4, CD5, CD7 and CD8
- Widespread ulcerated papules, plaques and tumors without precursor lesion
Board review style answer #2
D. Widespread ulcerated papules, plaques and tumors without precursor lesion
Comment Here
Reference: Primary cutaneous CD8+ aggressive epidermotropic T cell lymphoma
Comment Here
Reference: Primary cutaneous CD8+ aggressive epidermotropic T cell lymphoma