Table of Contents
Definition / general | Major updates | Diagrams / tables | Microscopic (histologic) images | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Deng T, Tsang P. WHO 2022 & ICC-T / NK cell. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomaWHOHAEM5ICCTcell.html. Accessed April 24th, 2024.
Definition / general
- 2 new classification systems for T / NK cell lymphoid neoplasms emerged in 2022 and evolved from the previous WHO revised 4th edition of 2016 (WHO HAEM4R)
- WHO 5th edition (WHO HAEM5) (Leukemia 2022;36:1720)
- International Consensus Classification (ICC) (Blood 2022;140:1229)
- Putative new entities with limited data are designated as provisional in the WHO HAEM4R and ICC while no provisional designation exists in WHO HAEM5 (see table 1)
- Updates include newly defined entities, more encompassing umbrella terms, deletion of old entities and modified nomenclature
Major updates
- Certain newly incorporated entities are unique to one or the other of the updated classifications (see table 1)
- Tumor-like lesions with T cell predominance (Kikuchi-Fujimoto disease, indolent T lymphoblastic proliferation and autoimmune lymphoproliferative syndrome) are included only in WHO HAEM5
- Primary cutaneous peripheral T cell lymphoma, NOS is a newly introduced term in WHO HAEM5 to describe rare cases of cutaneous T cell lymphoma that do not fit into existing entities
- Type II refractory celiac disease is recognized as an entity in ICC as a precursor of enteropathy associated T cell lymphoma (EATL)
- New entities have been added concurrently to WHO HAEM5 and ICC
- Indolent NK cell lymphoproliferative disorder (LPD) of the gastrointestinal (GI) tract, previously thought to be reactive, is newly recognized as neoplastic by WHO HAEM5 and ICC
- Formerly named lymphomatoid gastropathy or NK cell enteropathy
- Somatic mutations (e.g., JAK3) are present in a subset (Histopathology 2023;82:567)
- Lacks EBV
- May display a high proliferative fraction (Semin Diagn Pathol 2021;38:21)
- Previously included as a variant of peripheral T cell lymphoma, not otherwise specified (PTCL, NOS), EBV positive nodal T and NK cell lymphoma is a distinct entity in WHO HAEM5, that is equivalent to primary nodal EBV positive T / NK cell lymphoma in ICC (provisional entity)
- Indolent NK cell lymphoproliferative disorder (LPD) of the gastrointestinal (GI) tract, previously thought to be reactive, is newly recognized as neoplastic by WHO HAEM5 and ICC
- Breast implant associated anaplastic large cell lymphoma (ALCL): upgraded from provisional status (WHO HAEM4R) to a definite entity (J Clin Oncol 2020;38:1102)
- Can harbor JAK::STAT3 gain of function mutations (Am J Pathol 2020;190:2)
- Most patients present with localized disease that may be amenable to surgical excision; hence, margin evaluation and TNM staging are important (Cancer Treat Rev 2020;84:101963)
- Certain T / NK cell neoplastic entities have new nomenclature
- Indolent T cell LPD of the GI tract has been renamed as indolent T cell lymphoma of the GI tract (WHO HAEM5) or indolent clonal T cell LPD of the GI tract (ICC) due to its potential for disease dissemination, associated morbidity and monoclonal nature
- Symptoms may mimic inflammatory bowel disease (Front Oncol 2020;10:1276)
- Recurrent STAT3::JAK2 fusion can be seen in CD4+ cases (Blood 2018;131:2262)
- Category of nodal lymphomas of T follicular helper (TFH) origin is now unified into a single entity comprising 3 subtypes with new nomenclature
- Angioimmunoblastic T cell lymphoma (WHO HAEM4R) is now nodal TFH cell lymphoma, angioimmunoblastic type (WHO HAEM5) or follicular helper T cell lymphoma, angioimmunoblastic type (ICC)
- Follicular T cell lymphoma (provisional, WHO HAEM4R) is now nodal TFH cell lymphoma, follicular type (WHO HAEM5) or follicular helper T cell lymphoma, follicular type (ICC)
- Nodal peripheral T cell lymphoma with TFH phenotype (provisional, WHO HAEM4R) has been renamed nodal TFH cell lymphoma, NOS (WHO HAEM5) or follicular helper T cell lymphoma, NOS (ICC)
- Chronic LPD of NK cells, a provisional entity in WHO HAEM4R, has been upgraded to NK large granular lymphocytic leukemia (WHO HAEM5) to reflect the clonal nature of the NK cells
- Shares certain similarities with T large granular lymphocytic leukemia (e.g., cytologic features and recurrent STAT3 mutations) (Cancers (Basel) 2022;14:5236)
- Nomenclature and provisional status remain the same under ICC
- Primary cutaneous acral CD8 positive T cell lymphoma has been downgraded to an LPD in WHO HAEM5 and ICC due to its indolent nature
- Extranodal NK / T cell lymphoma, nasal type is known simply as extranodal NK / T cell lymphoma under the WHO HAEM5
- Hydroa vacciniforme-like LPD, an indolent EBV related lesion seen mostly in children, has been renamed hydroa vacciniforme LPD under both classifications
- Chronic active EBV infection of T and NK cell type, systemic form has been upgraded to systemic chronic active EBV disease (WHO HAEM5) or chronic active EBV disease (ICC)
- Premalignant, potentially life threatening condition with clonal proliferation of EBV infected T or NK cells that can cause systemic inflammation and organ failure (Immunol Med 2018;41:162)
- Indolent T cell LPD of the GI tract has been renamed as indolent T cell lymphoma of the GI tract (WHO HAEM5) or indolent clonal T cell LPD of the GI tract (ICC) due to its potential for disease dissemination, associated morbidity and monoclonal nature
- While NK lymphoblastic leukemia / lymphoma, a provisional entity in WHO HAEM4R, remains provisional under ICC, it has been eliminated from WHO HAEM5 (Virchows Arch 2023;482:11)
- Biologically heterogeneous; overlaps other CD56+ neoplastic entities (e.g., blastic plasmacytoid dendritic cell neoplasm, T lymphoblastic leukemia / lymphoma, acute myeloid leukemia and acute undifferentiated leukemia)
Diagrams / tables
Table 1: T / NK cell entities - comparison of WHO (2016), WHO (2022) and ICC (2022)
| WHO HAEM4R | WHO HAEM5 | ICC |
| Precursor T cell neoplasms | ||
| T lymphoblastic leukemia / lymphoma | T lymphoblastic leukemia / lymphoma, NOS | T lymphoblastic leukemia / lymphoma |
Early T cell precursor lymphoblastic leukemia / lymphoma | Early T cell precursor lymphoblastic leukemia | Early T cell precursor acute lymphoblastic leukemia, NOS |
| Early T cell precursor acute lymphoblastic leukemia, BCL11B activated | ||
| NK lymphoblastic leukemia / lymphoma* | [Entity removed] | NK cell acute lymphoblastic leukemia* |
| Tumor-like lesions with T cell predominance | ||
| [Not included] | Kikuchi-Fujimoto disease | [Not included] |
| [Not included] | Indolent T lymphoblastic proliferation | [Not included] |
| [Not included] | Autoimmune lymphoproliferative syndrome | [Not included] |
| Mature T / NK cell leukemias | ||
| T prolymphocytic leukemia | T prolymphocytic leukemia | T cell prolymphocytic leukemia |
| T cell large granular lymphocytic leukemia | T large granular lymphocytic leukemia | T cell large granular lymphocytic leukemia |
| Chronic lymphoproliferative disorder of NK cells* | NK large granular lymphocytic leukemia | Chronic lymphoproliferative disorder of NK cells* |
| Adult T cell leukemia / lymphoma | Adult T cell leukemia / lymphoma | Adult T cell leukemia / lymphoma |
| Sézary syndrome | Sézary syndrome | Sézary syndrome |
| Aggressive NK cell leukemia | Aggressive NK cell leukemia | Aggressive NK cell leukemia |
| Primary cutaneous T cell lymphomas | ||
| Primary cutaneous CD4 positive small or medium T cell LPD* | Primary cutaneous CD4 positive small or medium T cell LPD | Primary cutaneous small or medium CD4 positive T cell LPD |
| Primary cutaneous acral CD8 positive T cell lymphoma* | Primary cutaneous acral CD8 positive lymphoproliferative disorder | Primary cutaneous acral CD8 positive lymphoproliferative disorder |
| Mycosis fungoides | Mycosis fungoides | Mycosis fungoides |
| Primary cutaneous CD30 positive T cell LPD: lymphomatoid papulosis | Primary cutaneous CD30 positive T cell LPD: lymphomatoid papulosis | Primary cutaneous CD30 positive T cell LPD: lymphomatoid papulosis |
| Primary cutaneous CD30 positive T cell LPD: primary cutaneous anaplastic large cell lymphoma | Primary cutaneous CD30 positive T cell LPD: primary cutaneous anaplastic large cell lymphoma | Primary cutaneous CD30 positive T cell LPD: primary cutaneous anaplastic large cell lymphoma |
| Subcutaneous panniculitis-like T cell lymphoma | Subcutaneous panniculitis-like T cell lymphoma | Subcutaneous panniculitis-like T cell lymphoma |
| Primary cutaneous gamma / delta T cell lymphoma | Primary cutaneous gamma / delta T cell lymphoma | Primary cutaneous gamma / delta T cell lymphoma |
| Primary cutaneous CD8 positive aggressive epidermotropic cytotoxic T cell lymphoma* | Primary cutaneous CD8 positive aggressive epidermotropic cytotoxic T cell lymphoma | Primary cutaneous CD8 positive aggressive epidermotropic cytotoxic T cell lymphoma |
| [Not included] | Primary cutaneous peripheral T cell lymphoma, NOS | [Not included] |
| Intestinal T cell and NK cell lymphoid proliferations and lymphomas | ||
| Indolent T cell lymphoproliferative disorder of the gastrointestinal tract* | Indolent T cell lymphoma of the gastrointestinal tract | Indolent clonal T cell LPD of the gastrointestinal tract |
| [Not included] | Indolent NK cell LPD of the gastrointestinal tract | Indolent NK cell LPD of the gastrointestinal tract |
| Enteropathy associated T cell lymphoma | Enteropathy associated T cell lymphoma | Enteropathy associated T cell lymphoma |
| Type II refractory celiac disease | ||
| Monomorphic epitheliotropic intestinal T cell lymphoma | Monomorphic epitheliotropic intestinal T cell lymphoma | Monomorphic epitheliotropic intestinal T cell lymphoma |
| Intestinal T cell lymphoma, NOS | Intestinal T cell lymphoma, NOS | Intestinal T cell lymphoma, NOS |
| Hepatosplenic T cell lymphoma | ||
| Hepatosplenic T cell lymphoma | Hepatosplenic T cell lymphoma | Hepatosplenic T cell lymphoma |
| Anaplastic large cell lymphoma | ||
| Anaplastic large cell lymphoma, ALK positive | ALK positive anaplastic large cell lymphoma | Anaplastic large cell lymphoma, ALK positive |
| Anaplastic large cell lymphoma, ALK negative | ALK negative anaplastic large cell lymphoma | Anaplastic large cell lymphoma, ALK negative |
| Breast implant associated anaplastic large cell lymphoma* | Breast implant associated anaplastic large cell lymphoma | Breast implant associated anaplastic large cell lymphoma |
| Nodal T follicular helper (TFH) cell lymphoma | ||
| Angioimmunoblastic T cell lymphoma | Nodal TFH cell lymphoma, angioimmunoblastic type | Follicular helper T cell lymphoma, angioimmunoblastic type |
| Follicular T cell lymphoma* | Nodal TFH cell lymphoma, follicular type | Follicular helper T cell lymphoma, follicular type |
| Nodal peripheral T cell lymphoma (PTCL) with TFH phenotype* | Nodal TFH cell lymphoma, NOS | Follicular helper T cell lymphoma, NOS |
| Other peripheral T cell lymphomas | ||
| Peripheral T cell lymphoma, NOS | Peripheral T cell lymphoma, NOS | Peripheral T cell lymphoma, NOS |
| EBV positive NK / T cell lymphomas | ||
| [Not included] [variant of PTCL, NOS] | EBV positive nodal T and NK cell lymphoma | Primary nodal Epstein-Barr virus positive T / NK cell lymphoma* |
| Extranodal NK / T cell lymphoma, nasal type | Extranodal NK / T cell lymphoma | Extranodal NK / T cell lymphoma, nasal type |
| EBV positive T and NK cell lymphoid proliferations and lymphomas of childhood | ||
| Severe mosquito bite allergy | Severe mosquito bite allergy | Severe mosquito bite allergy |
| Hydroa vacciniforme-like lymphoproliferative disorder | Hydroa vacciniforme lymphoproliferative disorder, classic or systemic | Hydroa vacciniforme lymphoproliferative disorder, classic or systemic |
| Chronic active EBV infection of T and NK cell type, systemic form | Systemic chronic active EBV disease | Chronic active EBV disease (T and NK cell phenotype) |
| Systemic EBV positive T cell lymphoma of childhood | Systemic EBV positive T cell lymphoma of childhood | Systemic EBV positive T cell lymphoma of childhood |
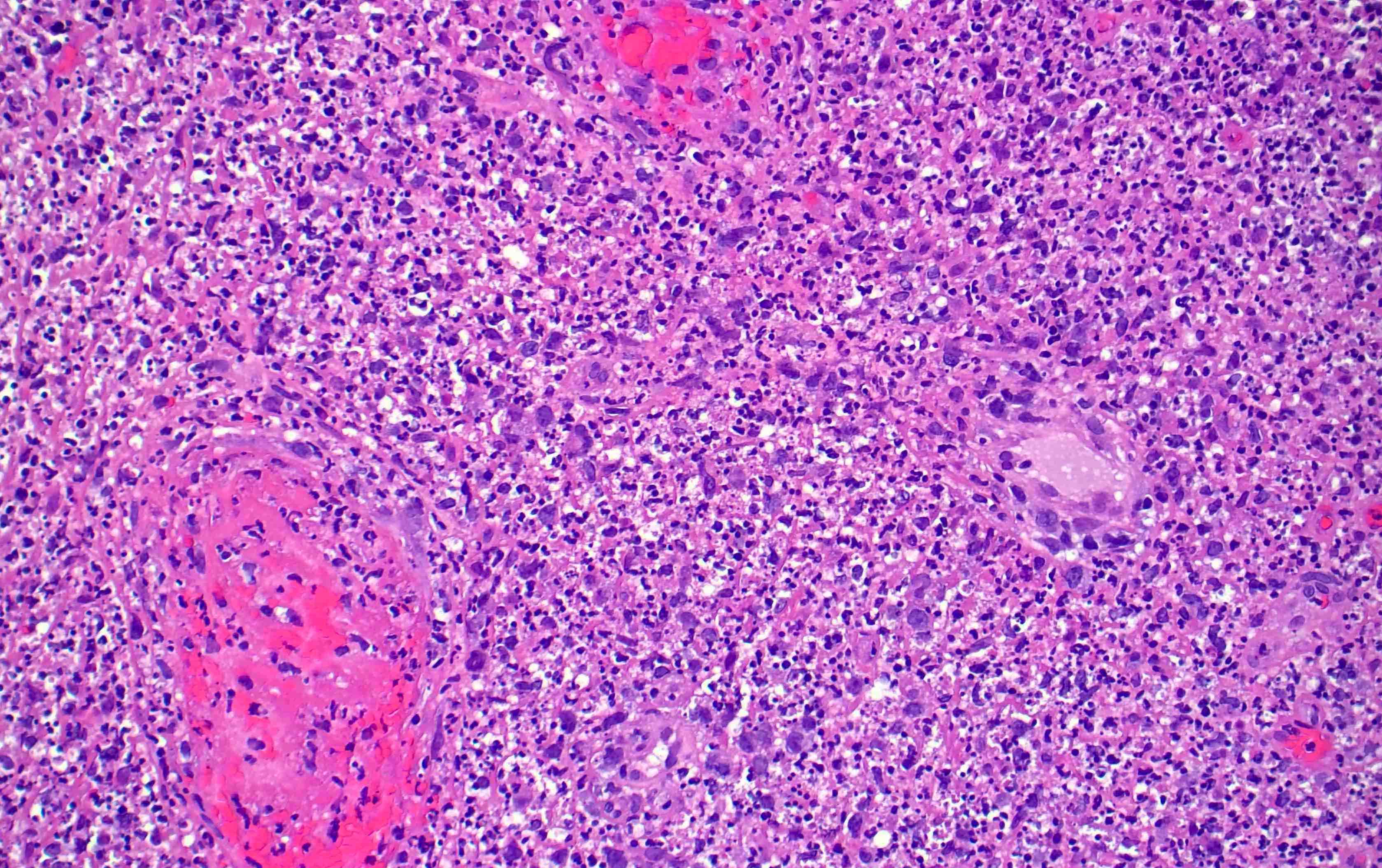
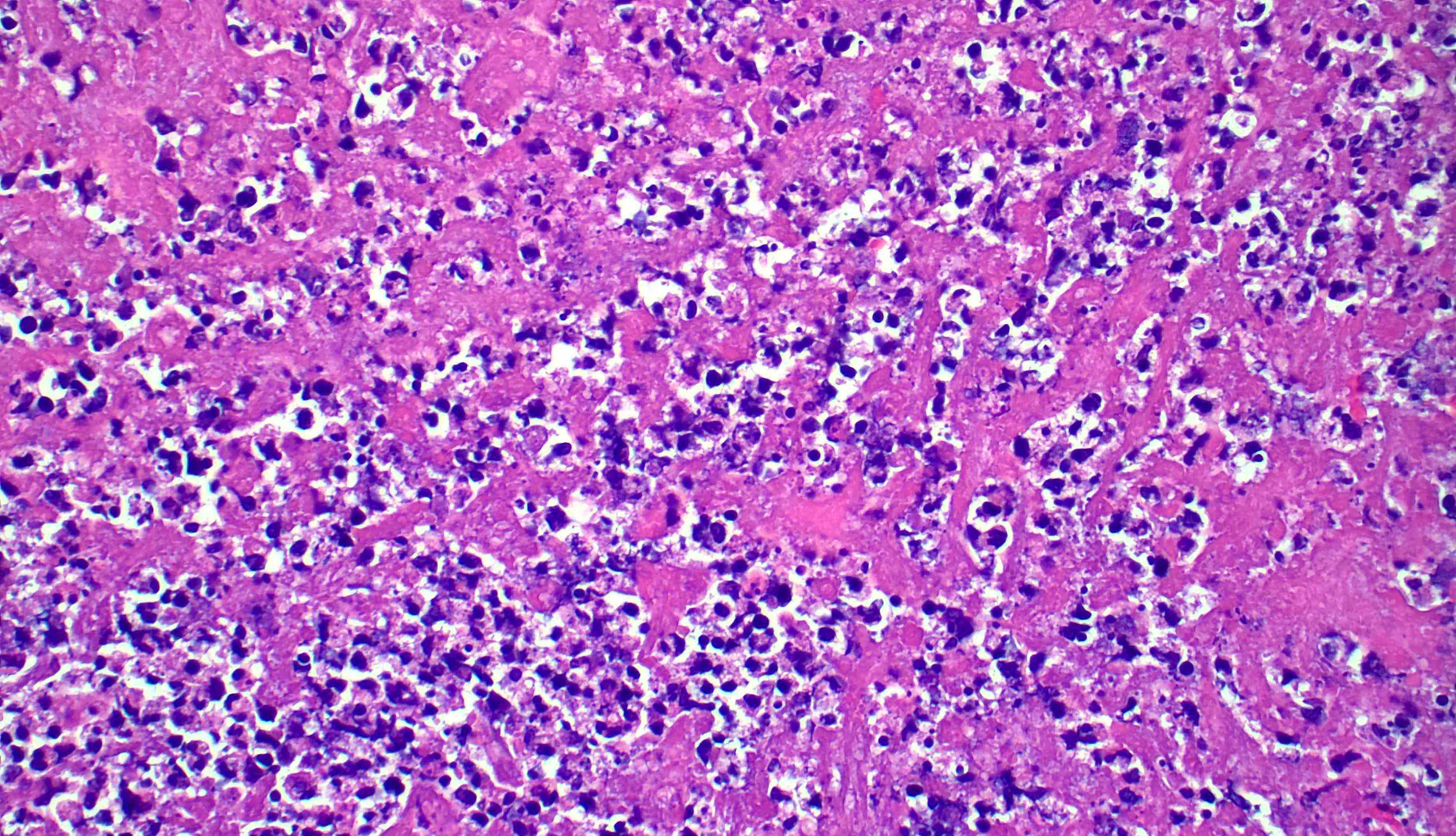
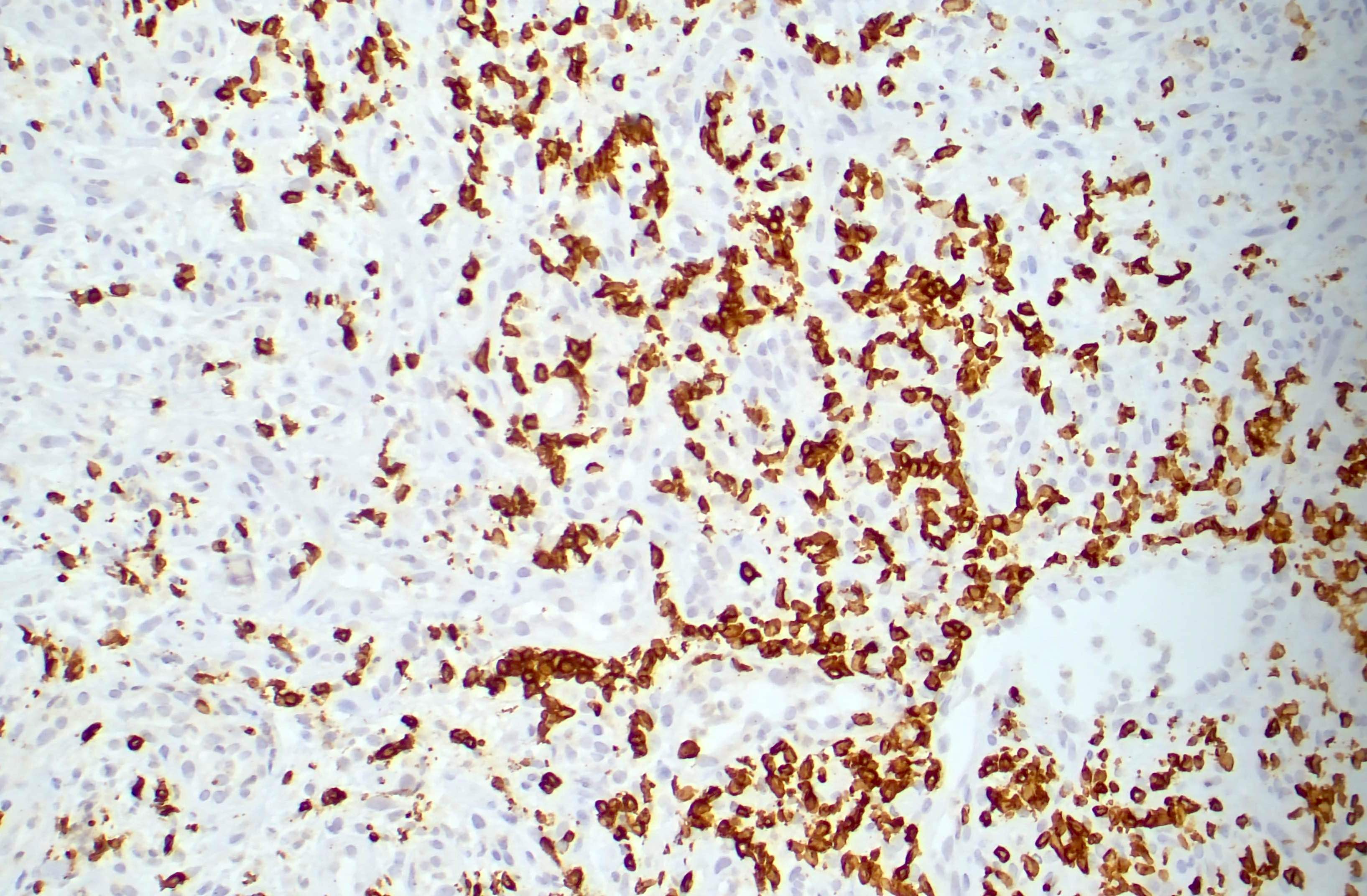
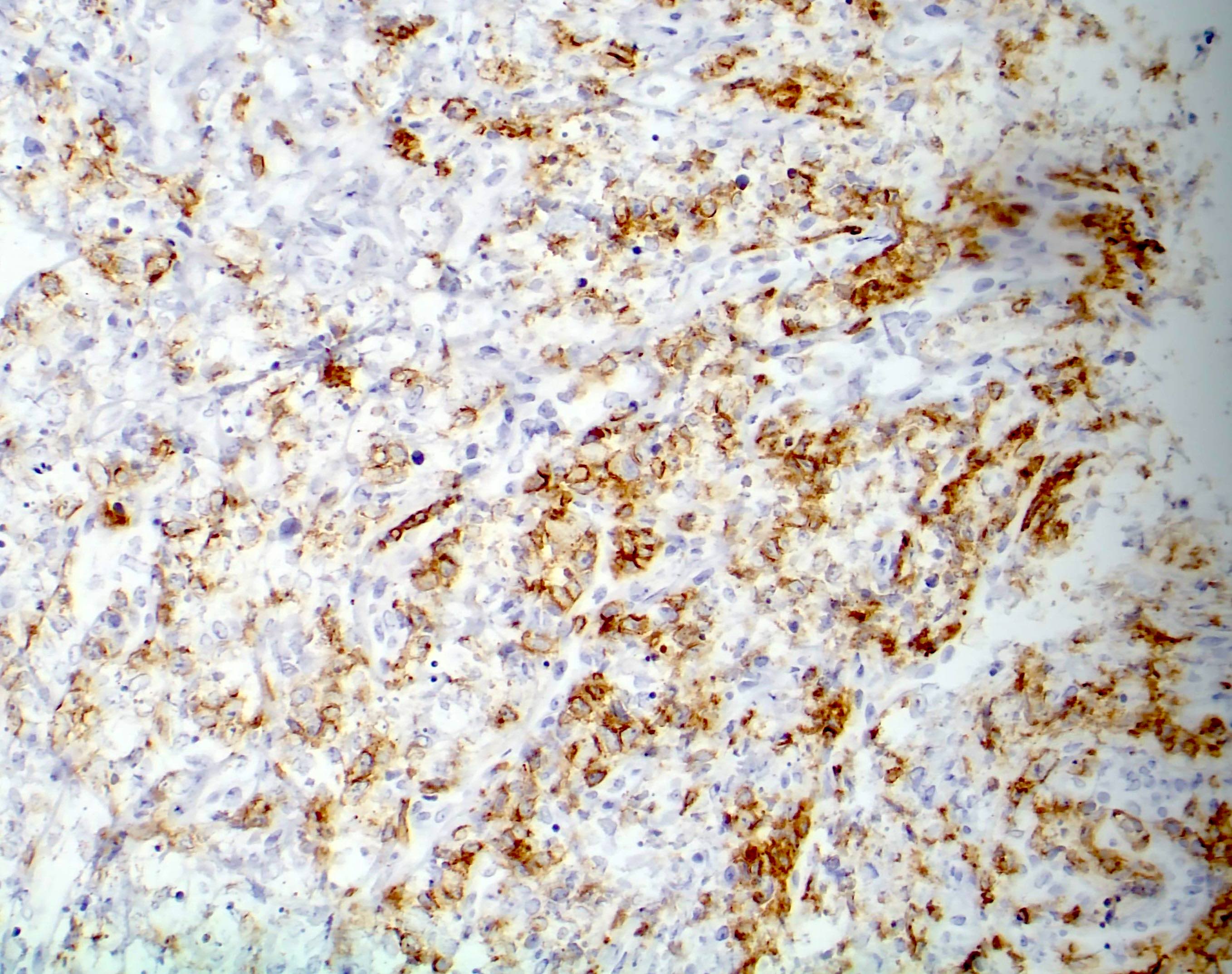
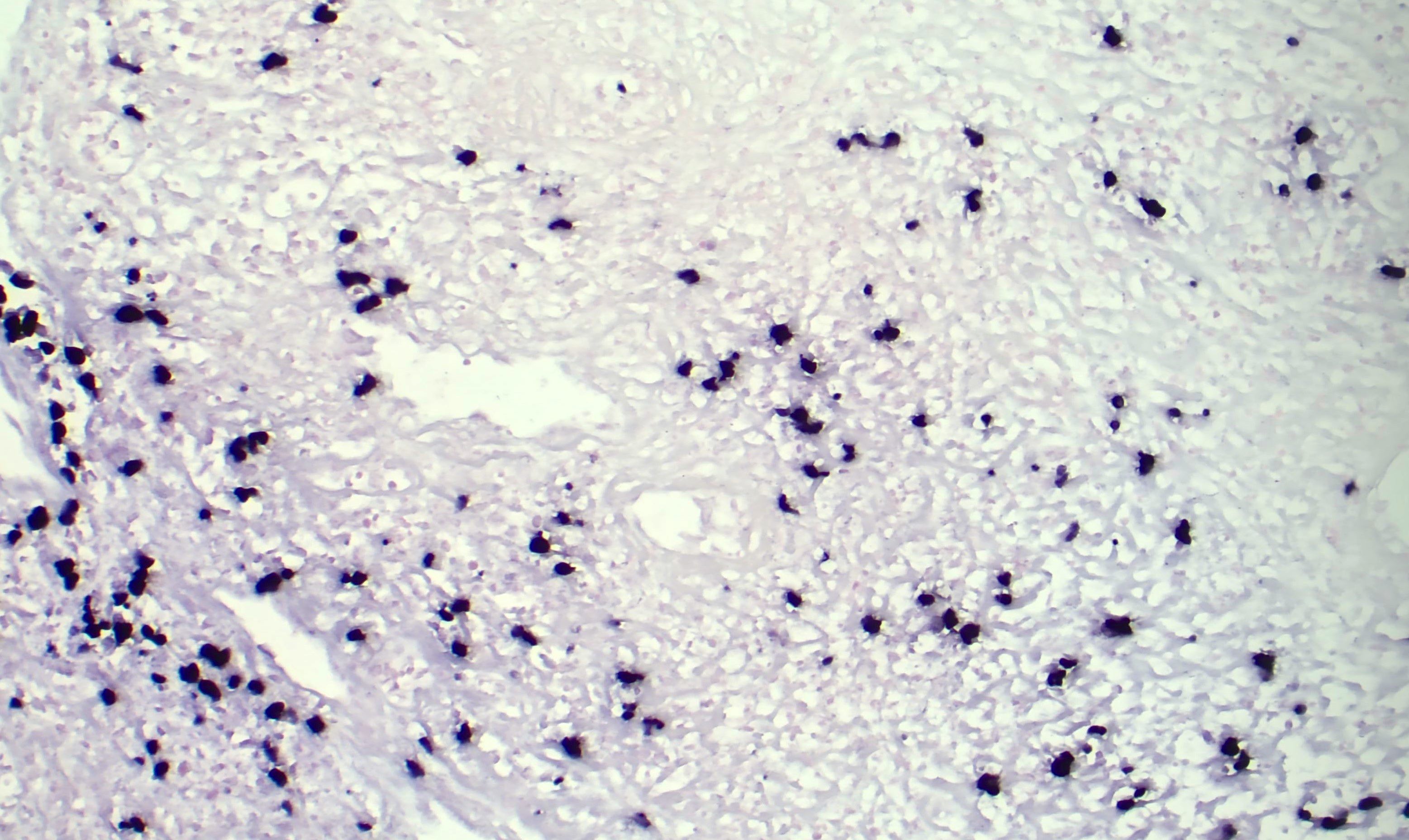
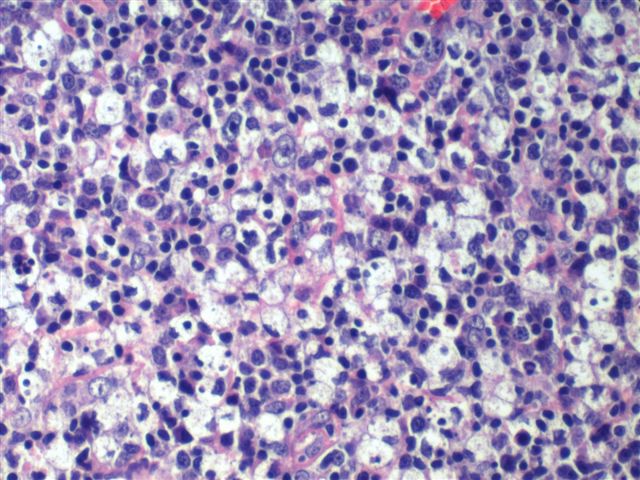
Microscopic (histologic) images
Board review style question #1
Board review style answer #1
D. Kikuchi-Fujimoto disease is considered as a tumor-like condition with T cell predominance, which is a newly defined category in the WHO 5th edition (2022). Answers C and B are incorrect because Erdheim-Chester disease is a histiocytic lesion while cold agglutinin disease is predominated by plasma cells. Answer A is incorrect because Castleman disease is a proliferation of mostly B cells or plasma cells.
Comment Here
Reference: WHO 2022 & ICC-T / NK cell
Comment Here
Reference: WHO 2022 & ICC-T / NK cell
Board review style question #2
Which of the following conditions is newly recognized by the WHO 5th edition (2022) and International Consensus Classification as neoplastic?
- Indolent NK cell lymphoproliferative disorder of the gastrointestinal tract
- Indolent T lymphoblastic proliferation
- NK lymphoblastic leukemia / lymphoma
- Primary cutaneous acral CD8 positive lymphoproliferative disorder
Board review style answer #2
A. Indolent NK cell lymphoproliferative disorder of the gastrointestinal tract, previously thought to be reactive, is newly recognized as neoplastic. Answer B is incorrect because indolent T lymphoblastic proliferation is not considered neoplastic under WHO 5th edition (2022) but a tumor-like lesion with T cell predominance. Answer C is incorrect because NK lymphoblastic leukemia / lymphoma, a provisional entity under the WHO 4th revised edition, is no longer considered a distinct entity. Answer D is incorrect because primary cutaneous acral CD8 positive lymphoproliferative disorder has been downgraded from lymphoma due to its indolent clinical course.
Comment Here
Reference: WHO 2022 & ICC-T / NK cell
Comment Here
Reference: WHO 2022 & ICC-T / NK cell