Table of Contents
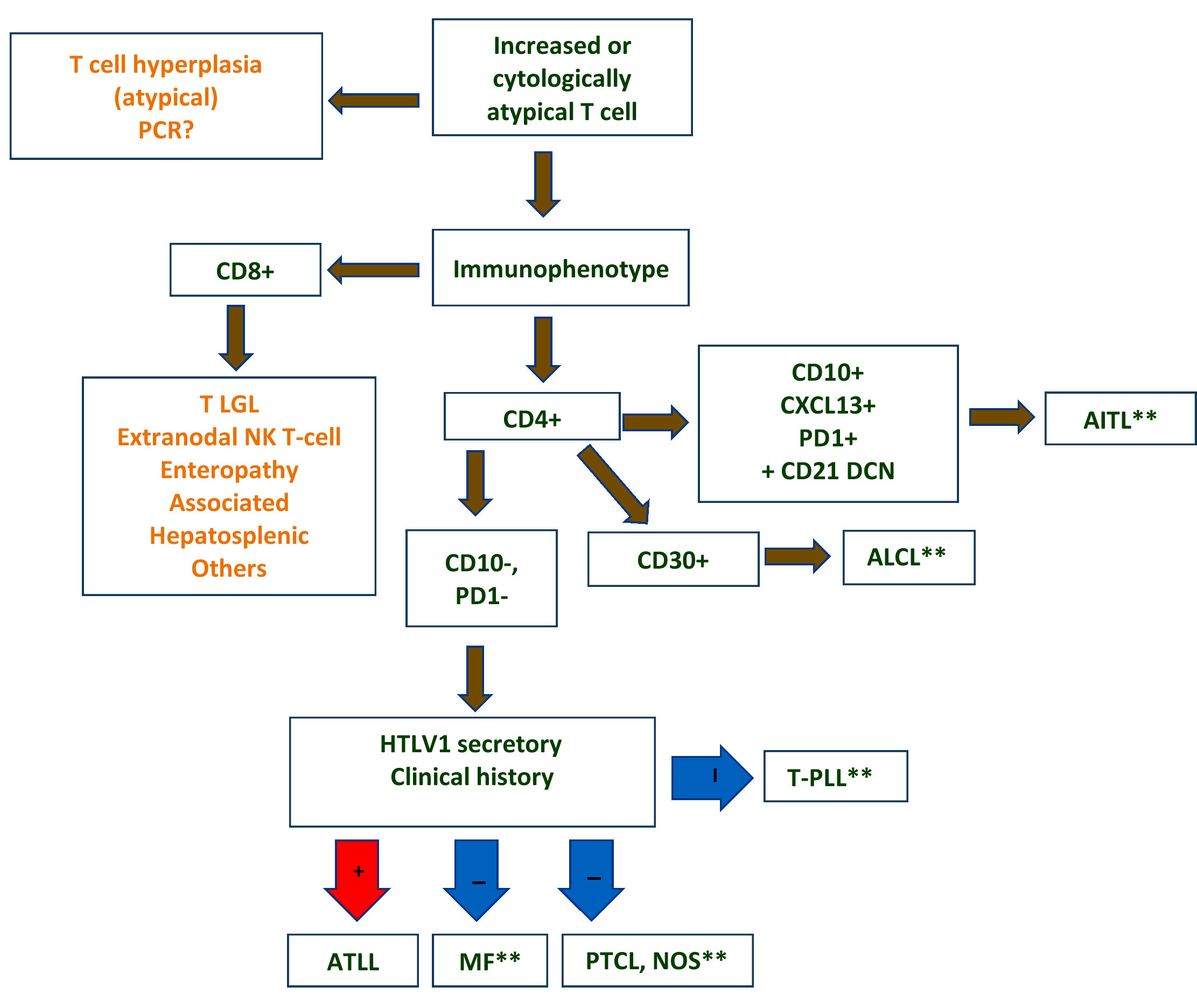
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnostic criteria | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Peripheral smear description | Peripheral smear images | Positive stains | Negative stains | Flow cytometry description | Flow cytometry images | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Khanlari M, Chapman J. ATLL. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomanonBatlv.html. Accessed April 28th, 2024.
Definition / general
- Aggressive T cell malignancy of mature CD4+ T cells causally associated with human T lymphotropic virus 1 (HTLV-1; also called human T cell leukemia virus) (Blood 2017;129:1071)
Essential features
- Lymphoma cells show monoclonal integration of HTLV-1 (Blood 2017;129:1071)
- Occurs in regions endemic for HTLV-1 (~ 2.5% in HTLV-1 carriers) (Int J Hematol 2002;76:240)
- Affected individuals are usually exposed to HTLV-1 very early in life (Front Microbiol 2018;9:461)
- Develops after a long latency (therefore occurs in adults)
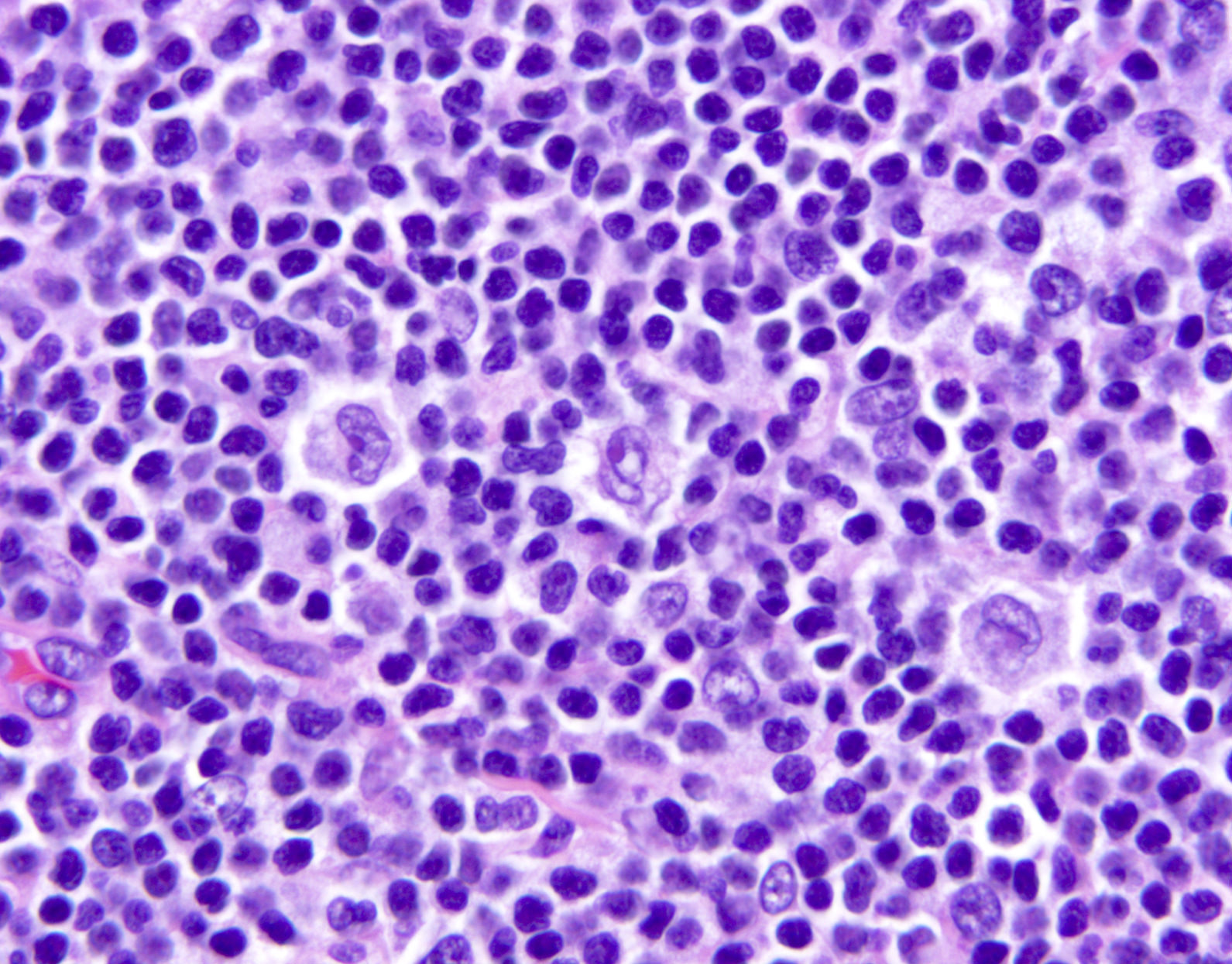
- Most often composed of highly pleomorphic small to medium sized lymphoid cells
- Widely disseminated and clinically aggressive
- Clinical spectrum of HTLV-1 associated diseases is wide and includes neoplastic and nonneoplastic disorders (Clin Microbiol Rev 2010;23:577)
Terminology
- Abbreviation: adult T cell leukemia / lymphoma (ATLL)
- Synonyms: adult T cell leukemia, adult T cell lymphoma, adult T cell leukemia / lymphoma (HTLV-1+)
ICD coding
Epidemiology
- HTLV-1 virus is endemic in Southwestern Japan, the Caribbean basin, sub-Saharan Africa, South America and parts of the Middle East and Australo-Melanesia (Front Microbiol 2012;3:388)
- Third to ninth decade, mean 58 years
- M:F = 1.5:1
- Transmission: requires the presence of living HTLV-1 infected cells
- Mother to infant (mainly by lymphocytes in breast milk) (J Pediatric Infect Dis Soc 2018;7:350)
- Sexual fluids
- Blood and blood products (not transmitted in fresh frozen plasma)
Sites
- Widespread lymph node involvement in most
- Systemic: spleen and extranodal sites including the skin, lungs, liver, gastrointestinal tract and central nervous system
- Main extranodal sites: skin (involved in > 50% of cases) and peripheral blood
Pathophysiology
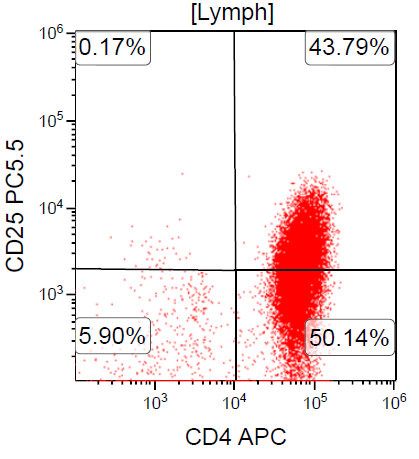
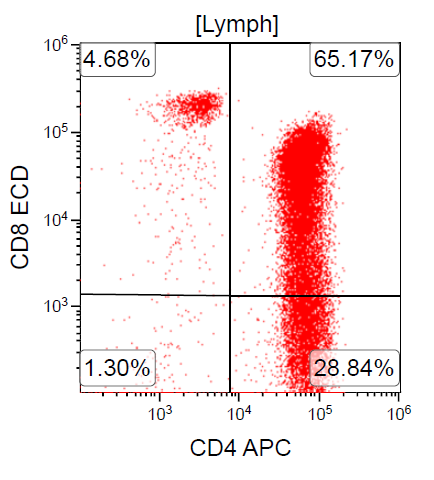
- Cell of origin is peripheral CD4+ T regulatory αβ T cell (CD4+ CD25+ FoxP3+ T regulatory cells are the closest normal counterpart)
- ATLL patients suffer from profound immunodeficiency; the concept that the cell of origin of ATLL is a T regulatory T cell provides a biologic basis for disease associated immunodeficiency
Etiology
- ATLL is uniformly causally associated with HTLV-1 infection
- HTLV was the first human retrovirus to be identified, isolated from a patient derived T cell lymphoma cell line (Proc Natl Acad Sci USA 1980;77:7415)
- HTLV-1 is a type C retrovirus, Deltaretrovirus genus
- Single strand of RNA is converted into double strand of DNA in host via reverse transcriptase enzyme (Viruses 2010;2:2037)
- Monoclonal, randomly integrates into host cell genome (Oncology 2015;89:7)
- Infection alone is not sufficient to result in neoplastic transformation of infected cells
- HTLV-1 can infect immature thymocytes and mature CD4+ T cells
- Enters by cell to cell contact via 3 cellular molecules: neuropilin 1, heparan sulfate proteoglycan (HSPGs) and GLUT1 (J Virol 2006;80:6844)
- Tax protein and HTLV-1 basic leucine zipper factor (HBZ): two major oncoproteins with key role in the development of ATLL in chronically infected individuals
- Tax (p40): activates viral promoter, the cyclic AMP response element binding transcription factor (CREB) and nuclear factor κβ pathways (Retrovirology 2004;1:20)
- HBZ: consistently expressed in all cases of ATLL; contributes to cellular proliferation and survival of the neoplastic clone (Retrovirology 2016;13)
- Epigenetic alterations and hypermethylation are also involved in the development and disease progression (Nat Genet 2015;47:1304, Am J Pathol 2010;176:402)
Clinical features
- 4 clinically defined variants in Shimoyama classification: acute, lymphomatous, chronic and smoldering (Br J Haematol 1991;79:428)
- Acute variant: ~ 55 to 60% of cases, survival usually < 1 year
- Leukocytosis (often greater than 100 x 109/L)
- Peripheral blood involvement with numerous flower cells
- Skin rash and lymphadenopathy
- Hepatosplenomegaly
- Hypercalcemia
- Elevated serum LDH
- Rapidly progressive course and frequent opportunistic infections
- Lymphomatous variant: ~ 20% of cases, survival usually < 1 year
- Lymphadenopathy
- Skin lesions
- No / minimal peripheral blood involvement
- Hypercalcemia is less frequent (compared with acute variant)
- Chronic variant: ~ 15 to 20% of cases, survival > 2 years but < 5 years due to progression to acute or lymphomatous ATLL
- Lymphocytosis
- Exfoliative skin lesions
- Lymphocyte count is much lower than in the acute variant
- Few atypical lymphocytes in peripheral smear review
- Mild hepatosplenomegaly
- Mild lymphadenopathy
- No hypercalcemia
- Smoldering variant: ~ 5% of cases, survival > 2 years but < 10 years due to progression to
acute ATLL or infectious complications
- Skin or lung lesions
- More than 5% atypical lymphocytes in absence of leukocytosis
- No hepatosplenomegaly, hypercalcemia or lymphadenopathy
- Primary cutaneous tumoral type
- No leukemic phase, lymphadenopathy, hepatosplenomegaly or hypercalcemia
- Proposed as a fifth clinical type in the Shimoyama classification (Int J Dermatol 2010;49:1099)
- Nonneoplastic HTLV-1 associated diseases
- Tropical spastic paraparesis / HTLV-1 associated myelopathy (TSP / HAM) (Rev Neurol (Paris) 2012;168:257)
- HTLV-1-associated infective dermatitis
- Uveitis
- Thyroiditis
- Pneumonitis
- Myositis
| Comparison of clinical forms of adult T cell leukemia / lymphoma | ||||
|---|---|---|---|---|
| Clinical manifestation | Acute | Lymphomatous | Smoldering | Chronic |
| Lymphocytosis | Increased | No | No | Mildly increased |
| Blood abnormal lymphocyte | Increased | No* | > 5% | Mildly increased |
| Increased LDH | Yes | No | No | Minimal |
| Hypercalcemia | Yes | Variable | No | No |
| Skin rash | Variable: > 50% | Variable: > 50% | Erythematous rash | Rash, papules |
| Lymphadenopathy | Usually present | Yes | No | Mild |
| Hepatosplenomegaly | Usually present | Often present | No | Mild |
| Bone marrow infiltration | May be present | No | No | No |
| Median survival | < 1 year | < 1 year | > 2 years | > 2 years |
Diagnostic criteria
- Strongest support for a diagnosis of ATLL: demonstration of viral integration in the tumor cells
- Clinical features favoring the diagnosis: appropriate patient demographic (patient derived from HTLV-1 endemic area), hypercalcemia, skin lesions and a leukemic phase
- Histologic features favoring the diagnosis: pleomorphic T cell lymphoma, leukemic phase, CD4+ αβ type with T regulatory immunophenotype, expression of CD25
Laboratory
- Evidence of HTLV-1 or 2 sequences at the molecular level
- Seropositivity for anti-HTLV-1 antibody as surrogate for demonstration of monoclonal integration of virus
- Only useful in areas with low prevalence of HTLV-1 infection
- In areas of high HTLV-1 prevalence, viral integration must be demonstrated
- Expression of CD25 by lymphoma cells
- Other laboratory tests / results:
- CBC: elevated leukocyte count and circulating neoplastic lymphocytes (leukemic phase)
- Elevated serum LDH level reflects disease burden / activity
- Hypercalcemia: more common in patients with acute variant; variably associated with lytic bone lesions
- Eosinophilia and neutrophilia are common
- Elevated soluble IL-2 receptor α chain levels in patients with aggressive ATLL
Radiology description
- May have lytic bone lesions
- Skull, pelvis, spine and long bones can be affected
- Punched out lesions similar to those seen in plasma cell myeloma can be found
- F-18 deoxyglucose PET / CT is usually positive in sites of disease activity
- CT detects sites of nodal and extranodal disease
Prognostic factors
- Clinical variant, age, performance status, serum calcium and LDH levels are major prognostic factors
- Death often stems from opportunistic infections
- Acute and lymphomatous variants:
- Aggressive clinical course
- Recurrent infection: parasitic (Strongyloides stercoralis) and viral infections (Parasite Immunol 2004;26:487)
- p16 gene deletion and p53 mutation: more aggressive clinical course
- Chronic and smoldering variants:
- More protracted clinical course
- Progression to an acute phase with an aggressive course in ~25%
- p16 gene deletion and chromosomal deletion detected via comparative genomic hybridization (CGH) in the chronic phase is a negative prognostic factor (J Clin Oncol 1997;15:1778)
Case reports
- 49 year old man with multiple cranial nerve palsies and meningeal lymphoma (Am J Hematol 2017;92:397)
- 50 year old woman with rheumatoid arthritis and panbronchitis-like pulmonary lesions (J UOEH 2017;39:55)
- 58 year old woman with erythematous and itchy plaques (Br J Haematol 2017;177:507)
- 70 year old man with TCL-1 positive lymphoma (Mod Pathol 2018;31:1046)
- 73 year old woman with unilateral conjunctival infiltration (J Clin Exp Hematop 2017;57:143)
Treatment
- Chronic or smoldering ATLL: observation may be appropriate for patients who are asymptomatic
- ATLL is resistant to most chemotherapy
- No standard chemotherapy regimen
- Intensive high dose combination chemotherapy and bone marrow transplantation have been used in limited numbers of patients (Blood 2010;116:1369)
- Monoclonal antibody based therapies have been attempted directed against:
- IL-2R (anti-Tac)
- CCR4 (mogamulizumab)
- CD52 (alemtuzumab)
- Recent clinical trials use arsenic trioxide, interferon α and zidovudine (Adv Ther 2018;35:135)
Gross description
- Skin lesions have been classified as erythema, papules or nodules
- Rare cases show tumor-like lesions or erythroderma as seen in mycosis fungoides / Sézary syndrome
- Enlarged and effaced lymph node
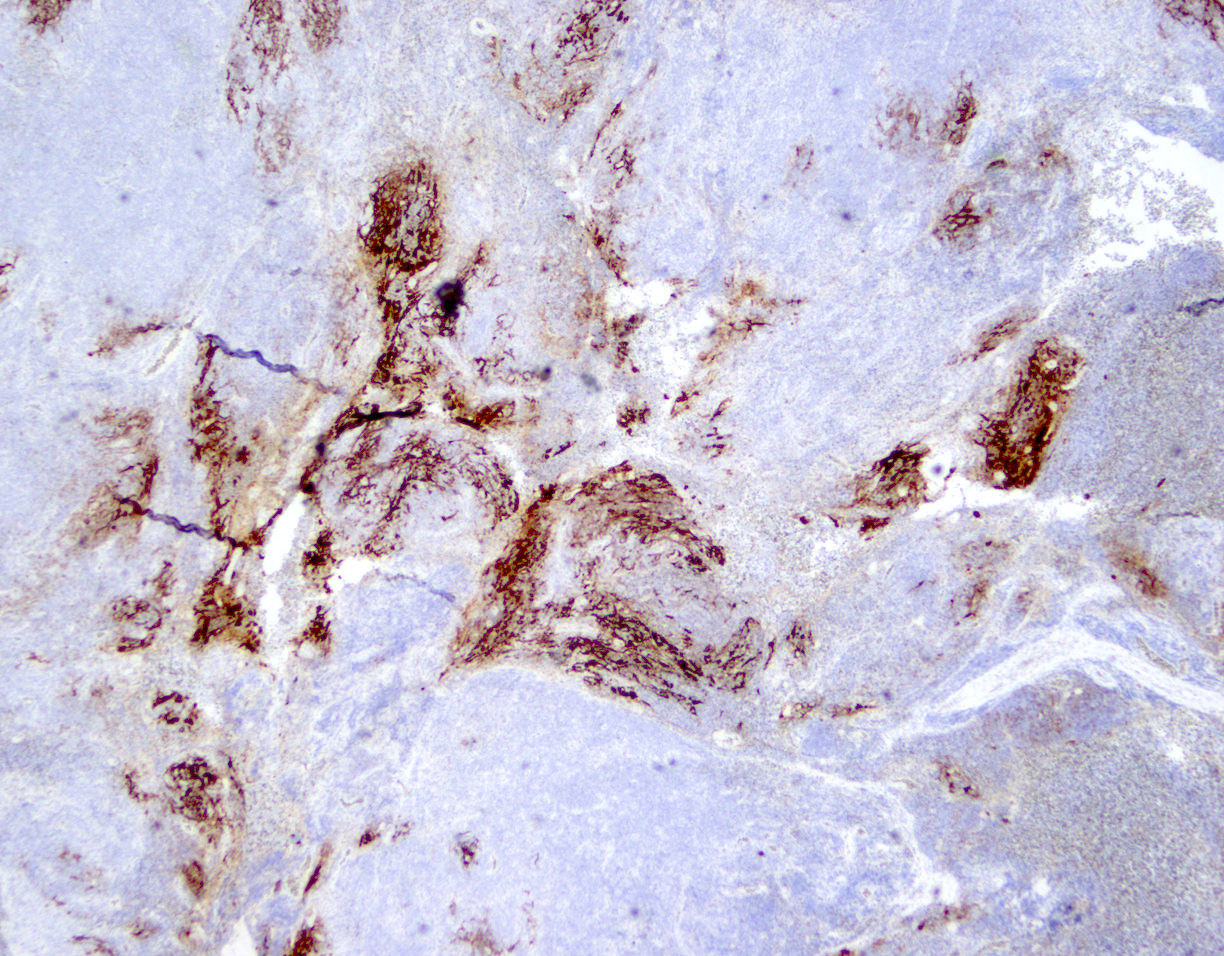
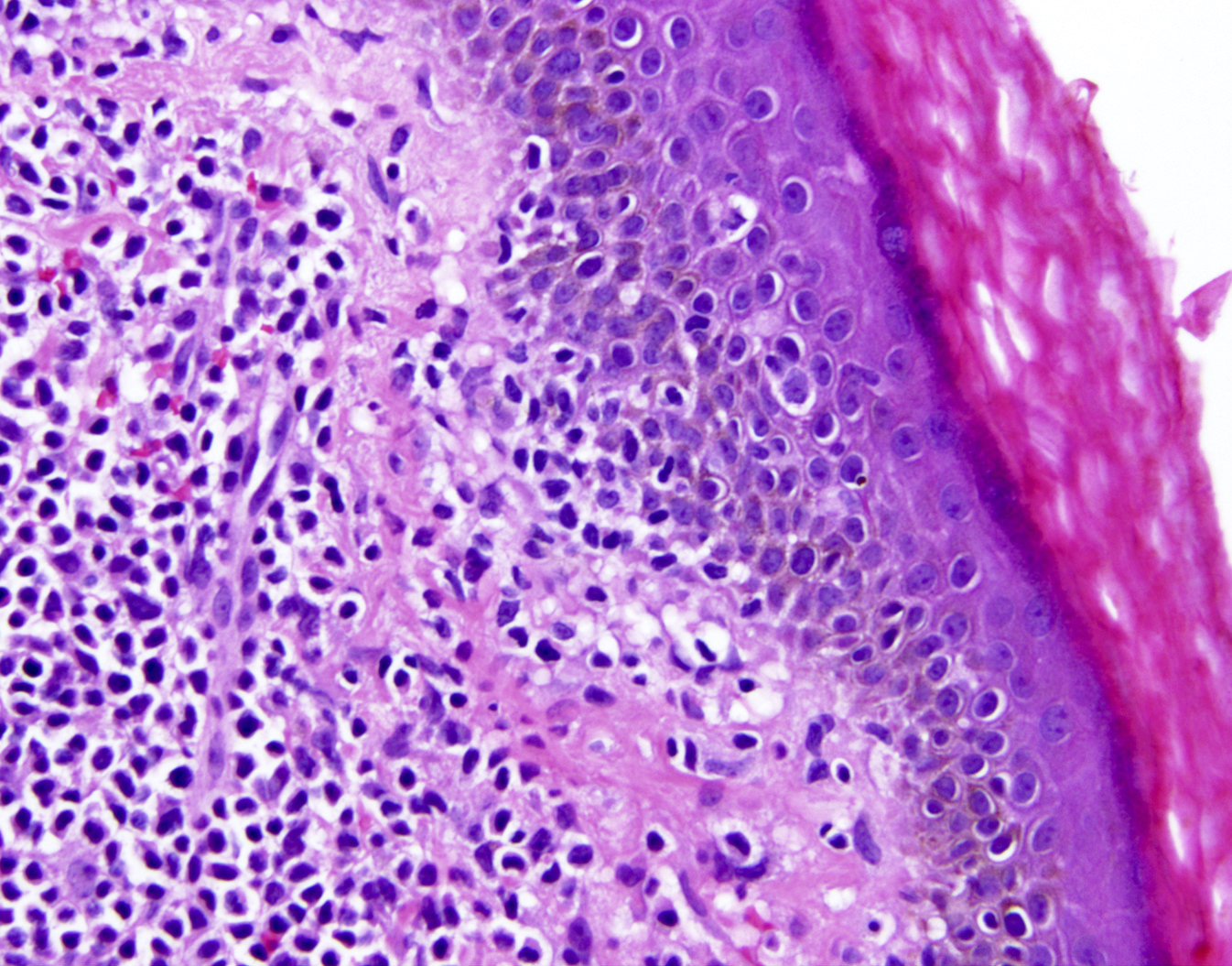
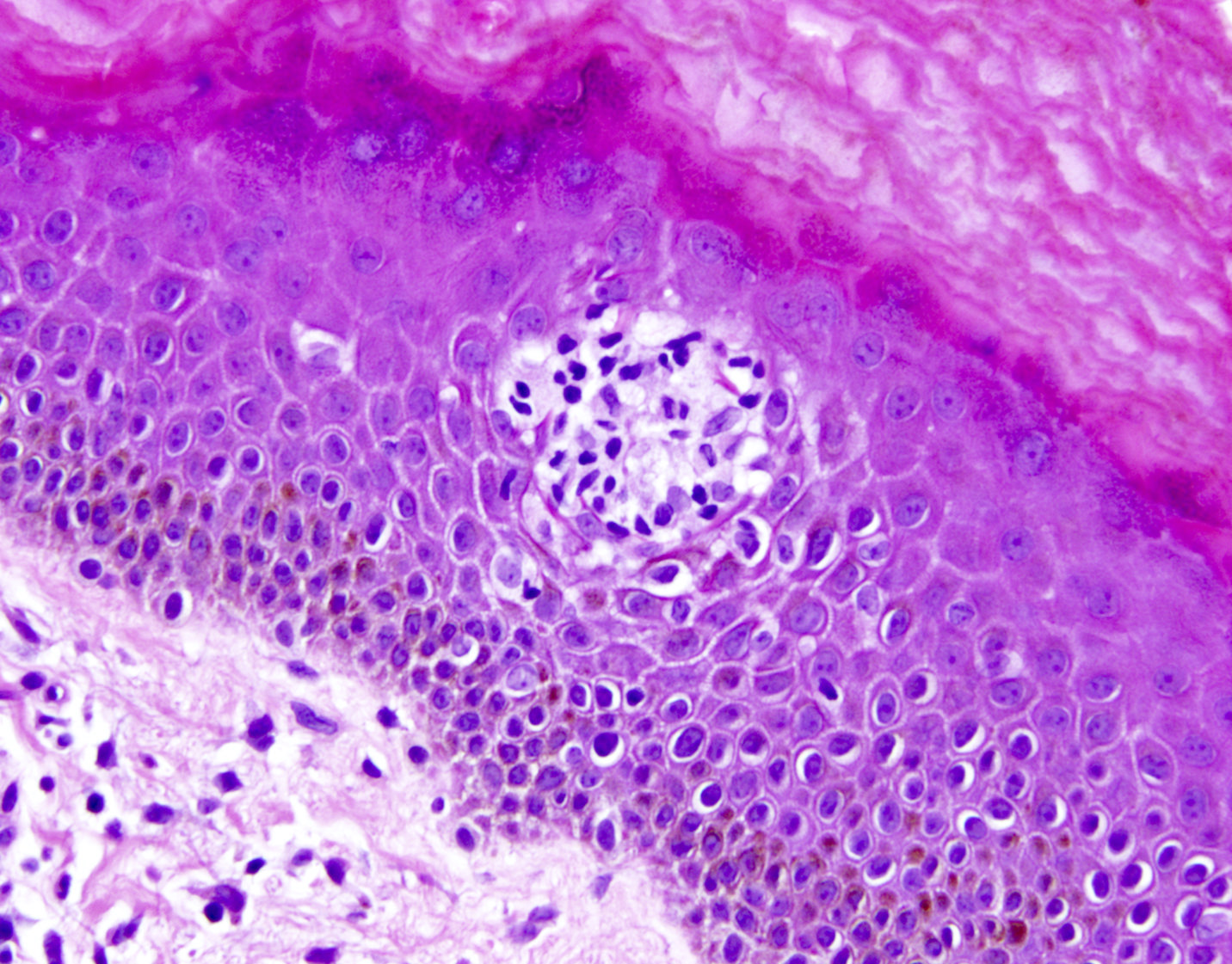
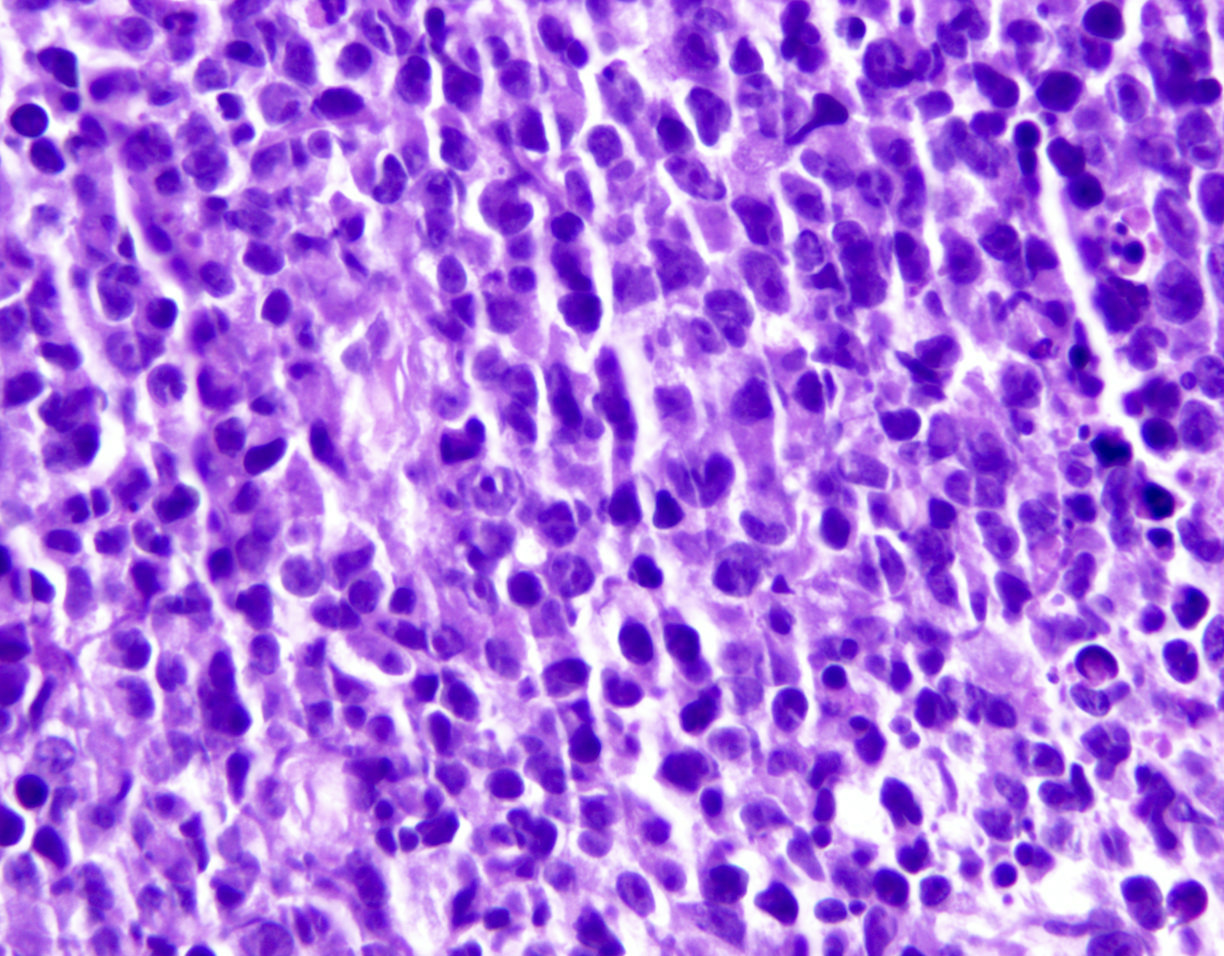
Microscopic (histologic) description
- Bone marrow:
- Degree of bone marrow infiltration is less than expected, given the marked lymphocytosis that is often present
- Pattern of marrow involvement can be diffuse, interstitial or sinusoidal
- Often evidence of bone resorption and osteoclastic activity
- Bone trabeculae: may show remodeling
- Lytic bone lesions can be present even in the absence of tumoral bone infiltration
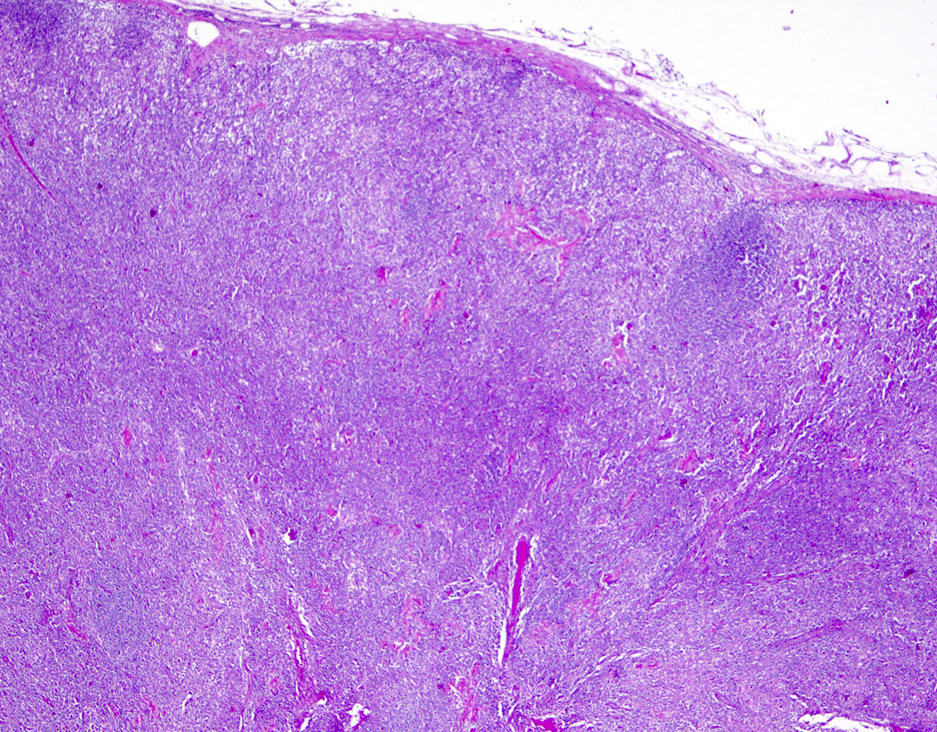
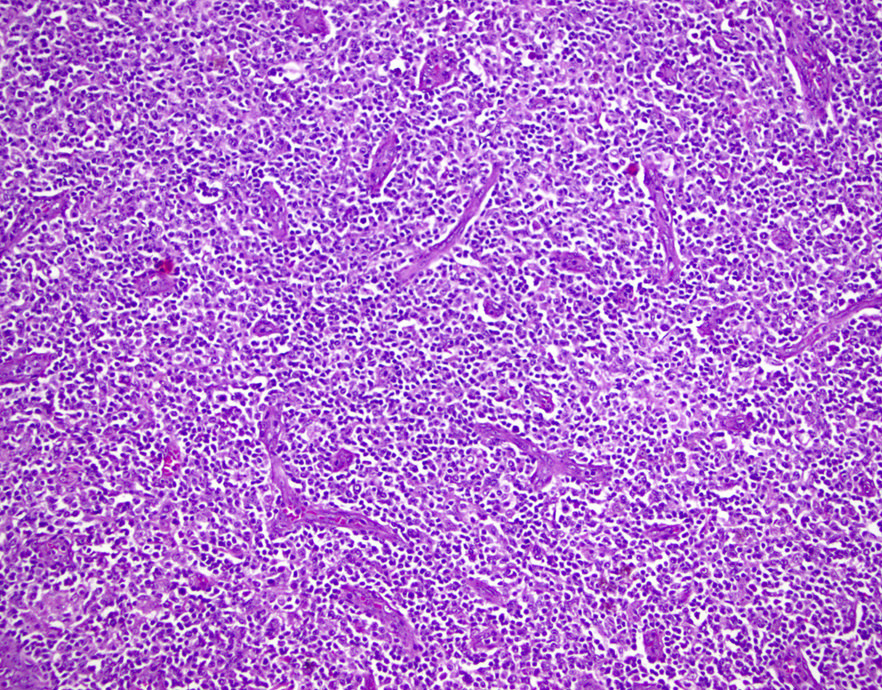
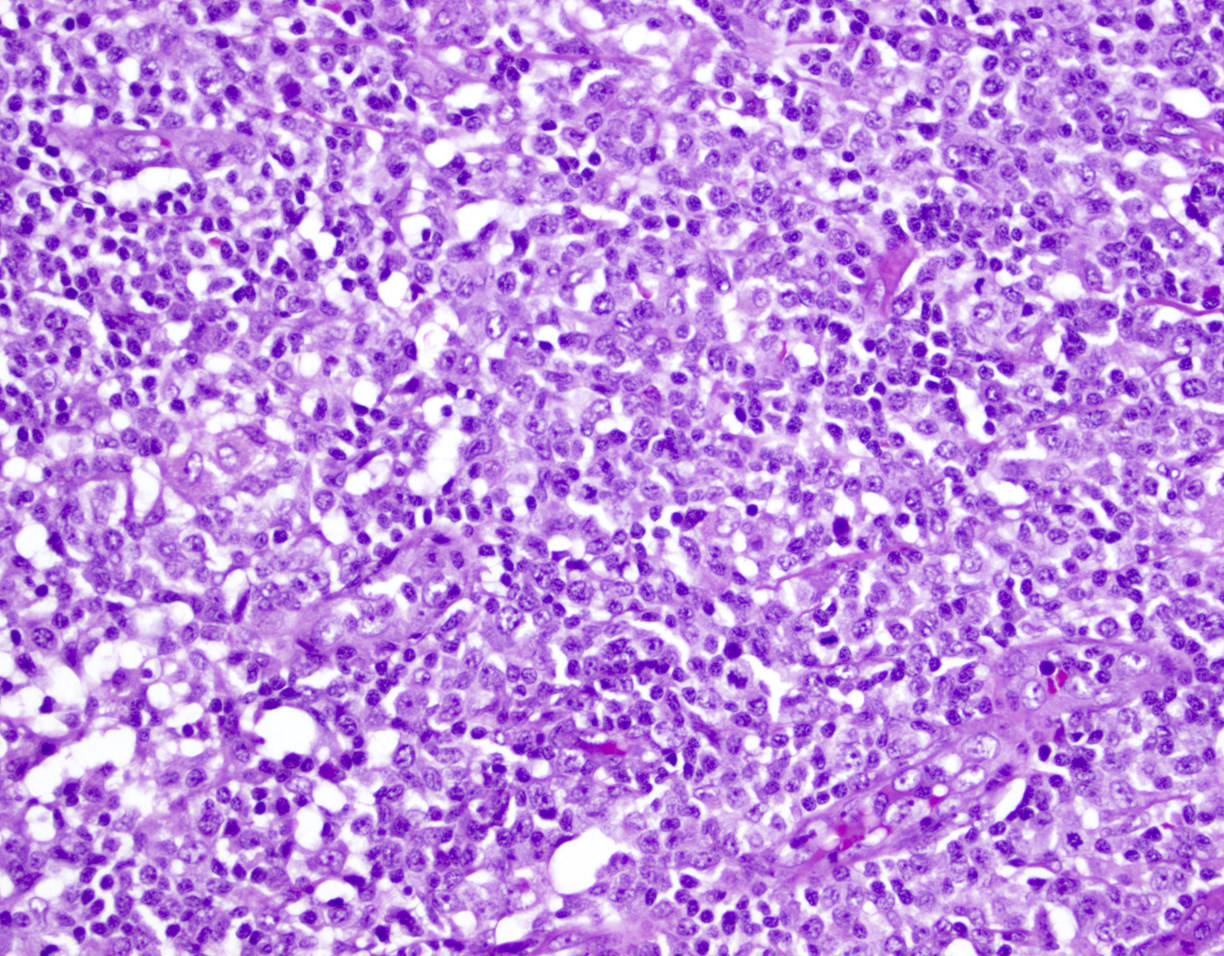
- Lymph nodes:
- Involves paracortical T cell zones
- Typically show diffuse architectural effacement
- May be subdivided according to cell type and pattern into:
- Pleomorphic small cell
- Pleomorphic medium and large cell type / pattern (most common)
- Anaplastic large cell-like [resembling anaplastic large cell lymphoma (ALCL)]
- Angioimmunoblastic T cell lymphoma-like (AITL)
- Hodgkin lymphoma-like: seen in early phase of some adult T cell lymphoma
- Leukemic pattern of infiltration with preservation or dilation of lymph node sinuses that contain malignant cells
- Size or shape of the neoplastic cells or identification / classification of the above patterns does not impact the clinical course
- Skin lesions:
- Epidermal infiltration with Pautrier-like micro-abscesses is common (Mod Pathol 2018;31:1046)
- Hyperparakeratosis is variably present in the overlying epidermis
- Dermal infiltration: mainly perivascular but larger tumor nodules with extension to subcutaneous fat may be observed
- Erythematous lesions: composed of smaller cells in perivascular pattern in dermis
- Papules and nodules: composed of larger cells that replace dermis
- Other sites commonly involved by ATLL include: liver, spleen, lungs and central nervous system
- Grading: there is no formal grading system for ATLL
Note: ATLL should be strongly considered in any T cell lymphoma developing in a patient from an endemic area regardless of histopathologic features and anti-HTLV-1 serology testing should be performed
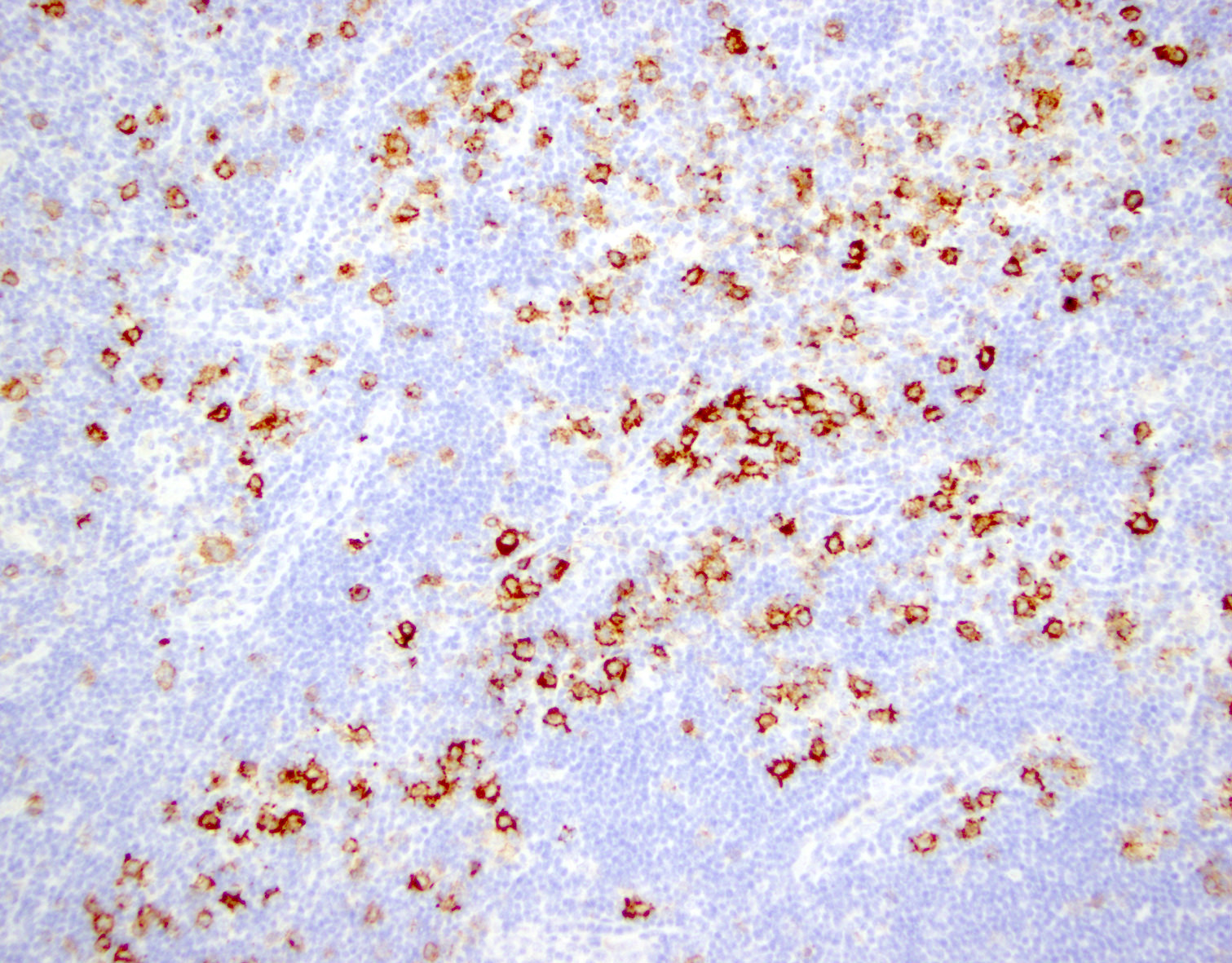
Microscopic (histologic) images
Cytology description
- ATLL cells show variable appearances
- Irregular / polylobulated nuclei, homogeneous, condensed chromatin, small nucleoli
- Agranular basophilic cytoplasm
- Tumor cells in lymph nodes are frequently pleomorphic and most cases have a mixture of small to large pleomorphic cells
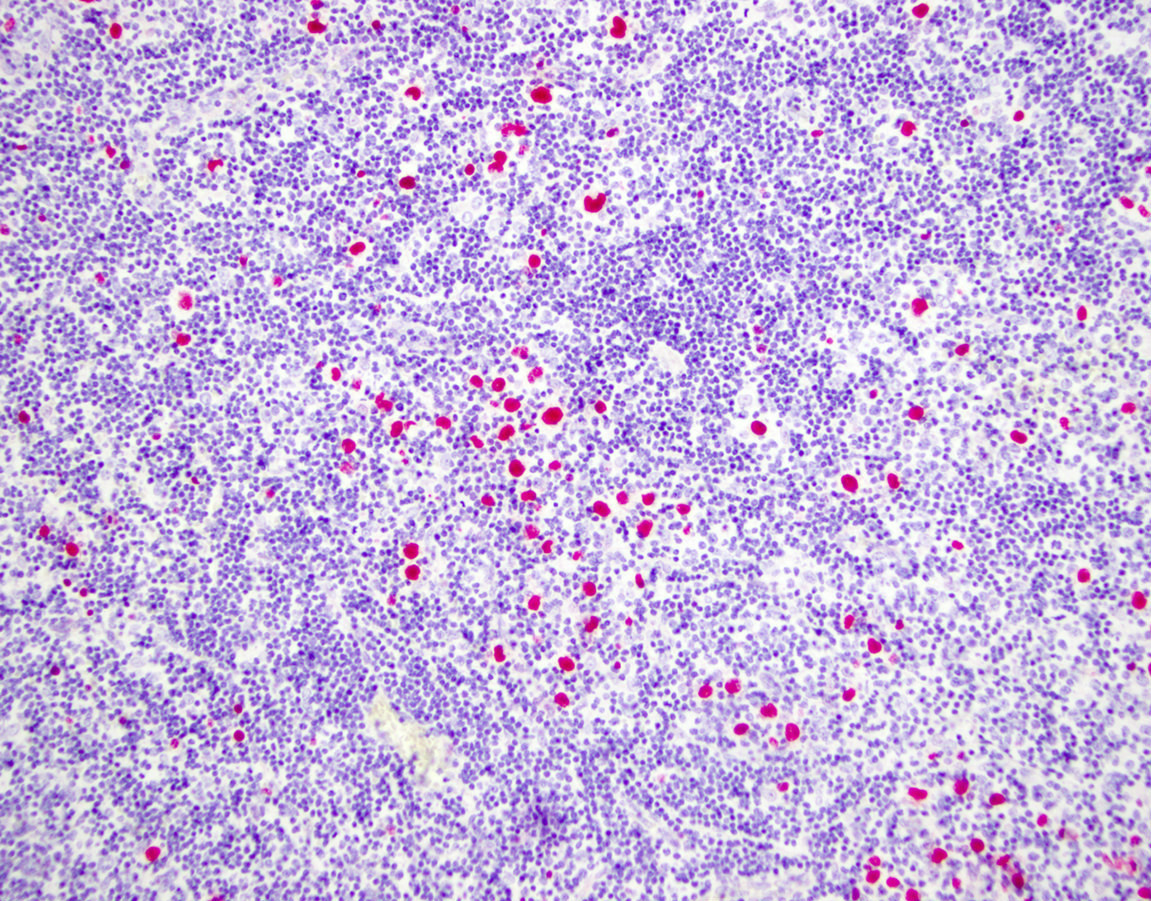
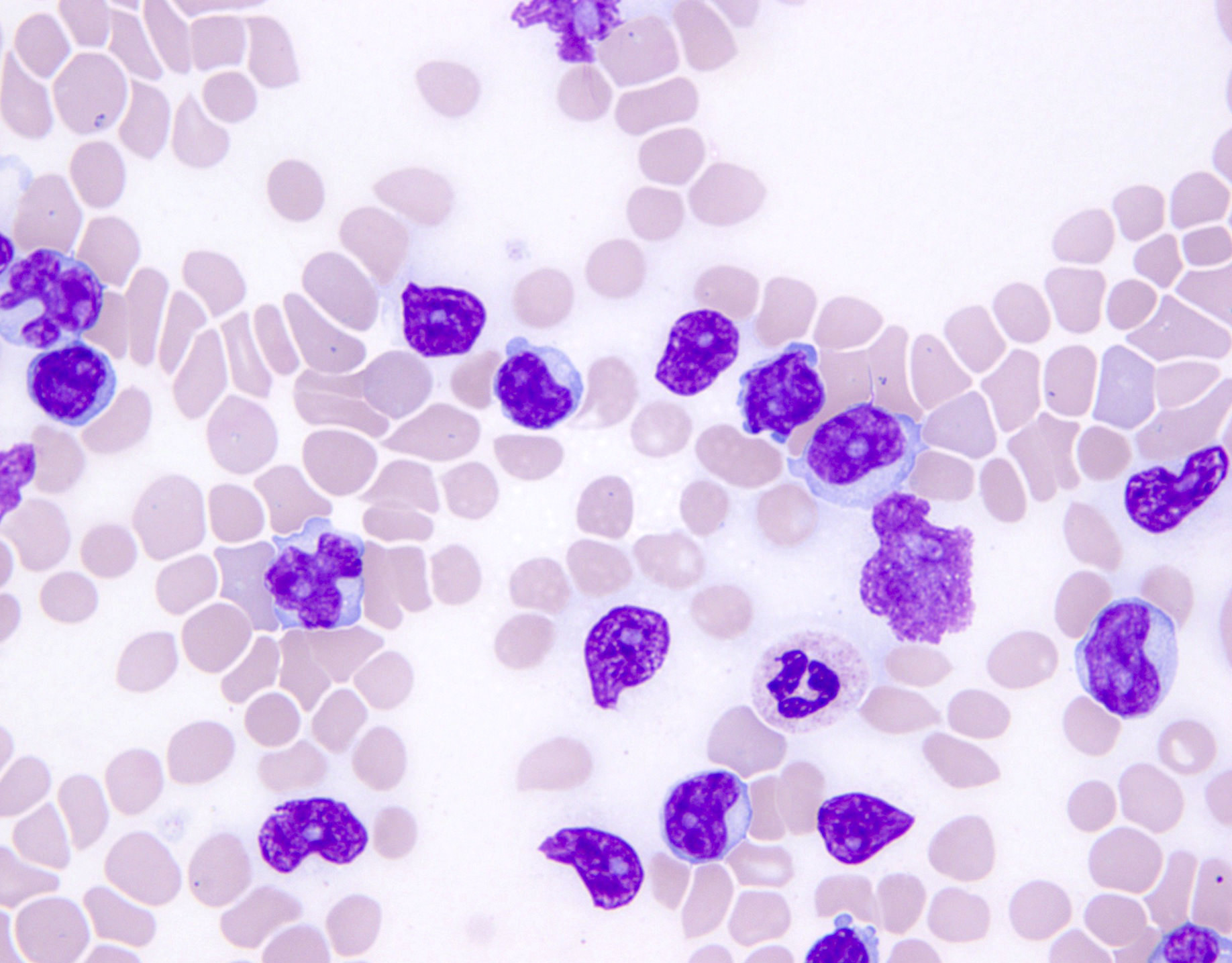
Peripheral smear description
- Medium to large sized lymphocytes with multilobulated nuclei (flower cells) in the peripheral blood of acute (leukemic) ATLL
- Slightly larger than normal peripheral blood lymphocytes with moderately condensed chromatin, absent or small nucleoli, scant slightly basophilic cytoplasm and some with multilobulated nuclei in chronic ATL
Peripheral smear images
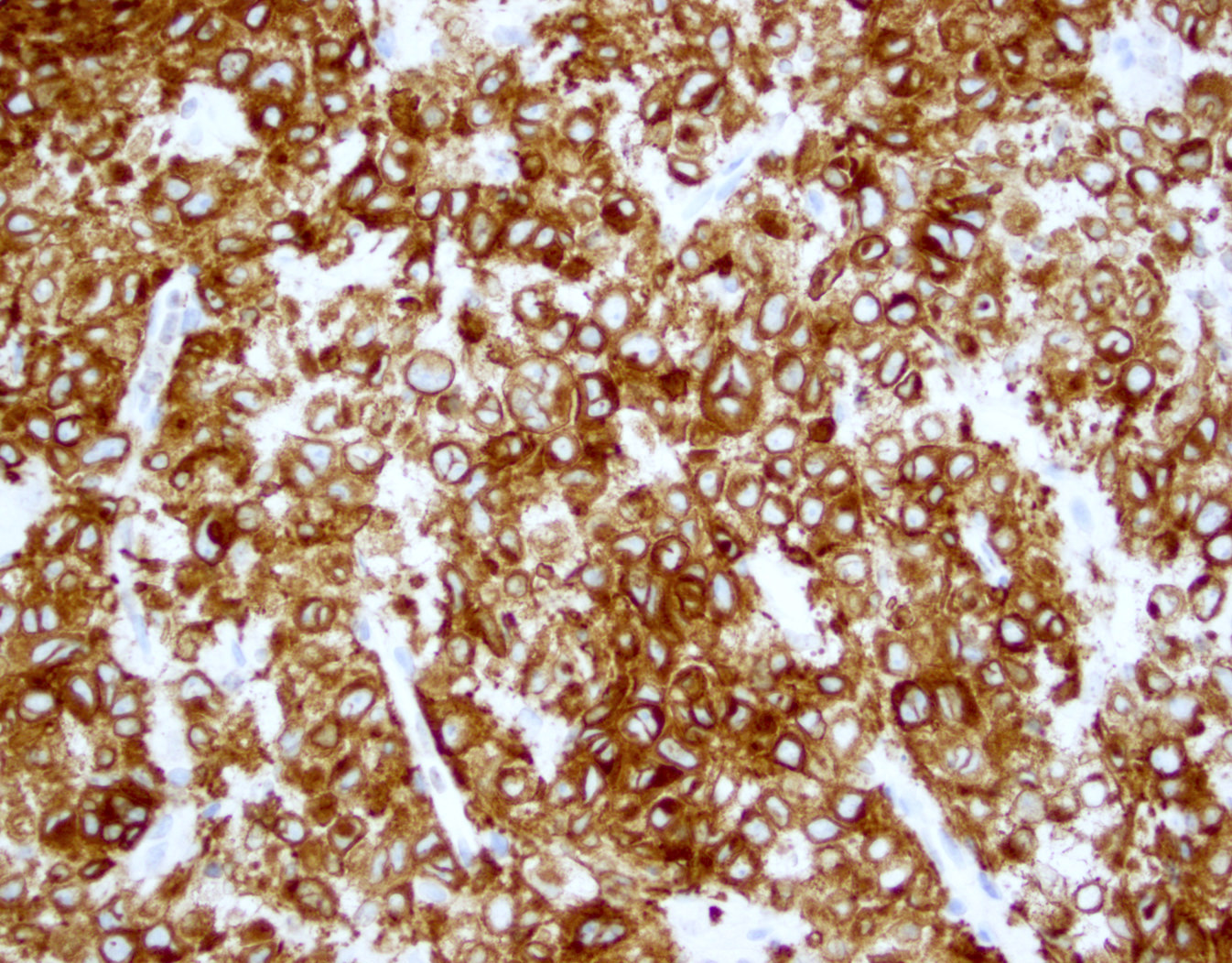
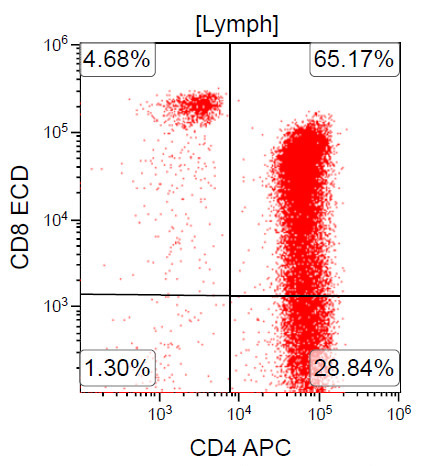
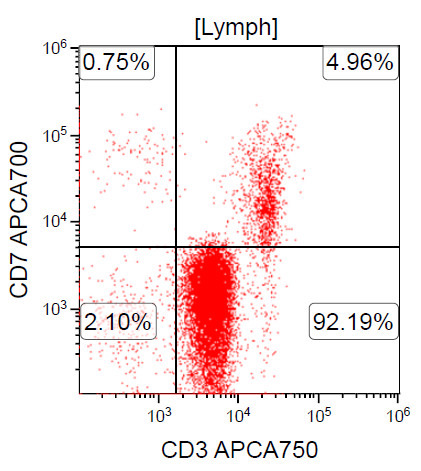
Positive stains
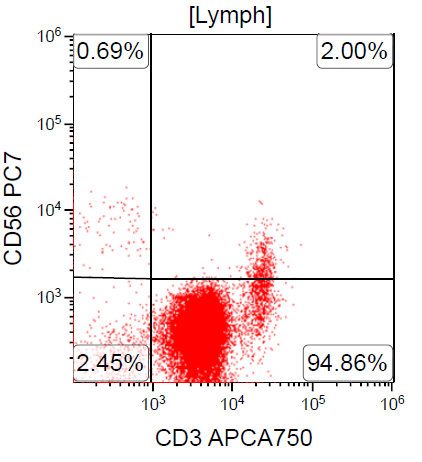
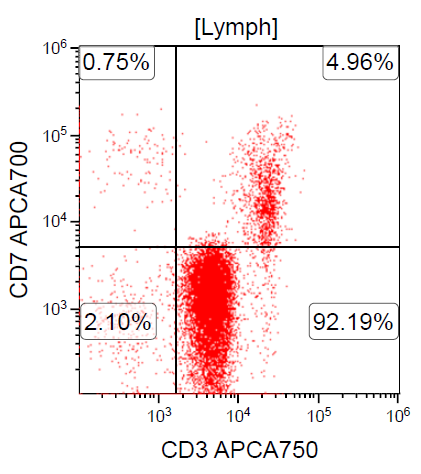
- CD2, CD3, CD4 (most), CD5, CD25 (IL-2R), T cell receptor (TCR) αβ, CD45RO, HLA-DR variable, FOXP3 (68%), CD52 variable, CD62 / selectin L variable and CCR4 (88%) (Leukemia 2005;19:2247, Clin Cancer Res 2003;9:3625)
- Frequent expression of IRF4 / MUM1
- Can be negative for CD30 or can express weak or diffuse and strong CD30 (in large transformed cells)
- EBV+ reactive B cells (immunoblasts) may be present in the background
Negative stains
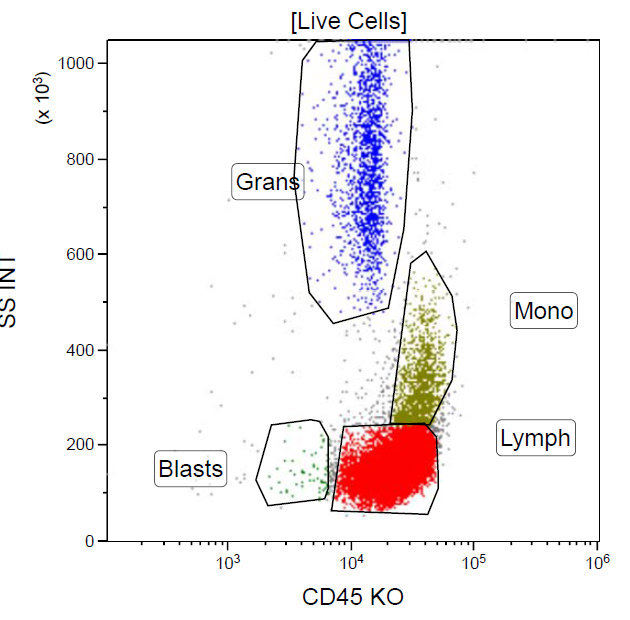
Flow cytometry description
Flow cytometry images
Electron microscopy description
- Viral particles, 80 to 120 nm, are present in both cytoplasm and extracellular space
Molecular / cytogenetics description
- Clonal integration of HTLV-1 genome can be demonstrated
- PCR assays are positive for clonal T cell receptor gene rearrangement
- Quantitative HTLV-1 levels
- CCR4 mutations in ~25% of cases (Nat Genet 2015;47:1304)
- RHOA mutations detected in ~15% of cases (Blood 2016;127:596)
- Tumor suppressor genes are inactivated either by mutation or epigenetic silencing
- Numerous complex chromosomal abnormalities are frequent, especially in acute and lymphomatous variants
- Clonal chromosome abnormalities are frequent but not specific
Differential diagnosis
- Peripheral T cell lymphoma, not otherwise specified (PTCL-NOS)
- Patient from Western hemisphere
- Background of reactive cells, including eosinophils, plasma cells and histiocytes
- Negative serologic studies or lack of molecular evidence of HTLV-1
- Angioimmunoblastic T cell lymphoma (AITL)
- Anaplastic large cell lymphoma (ALCL)
- Sinusoidal distribution in partially involved lymph nodes
- Lymphoma cells are strongly CD30+ (ATLL with strong CD30 expression in 100% of lymphoma cells are reported)
- Expression of cytotoxic granule associated proteins (can be seen in ATLL)
- Translocations involving ALK gene and / or ALK1 protein expression
- ALK- ALCL cases are difficult to differentiate from ATLL without HTLV-1 testing
- Classic Hodgkin lymphoma (HL)
- Background T cells are immunophenotypically normal
- Lacks clonal T cell gene rearrangement
- Lacks malignant cells in peripheral blood, rare reports of skin lesions and hypercalcemia
- Cutaneous T cell lymphoma / mycosis fungoides (CTCL MF / SS)
- T cell prolymphocytic leukemia (T-PLL)
- Involves blood at presentation with ↑ WBC
- Some nuclear irregularity but no flower cell morphology as in ATLL
- Lack of anti-HTLV-1 positive serology
- T lymphoblastic leukemia / lymphoma (T-LBL)
- T cell large granular lymphocytic leukemia (LGL)
Additional references
- Swerdlow: WHO Classification of Tumours of Haematopoietic and Lymphoid Tissue, 4th Edition, 2008, His: Hematopathology - Foundations in Diagnostic Pathology series, 3rd Edition, 2017, Orazi: Knowles Neoplastic Hematopathology, 3rd Edition, 2013, Jaffe: Hematopathology 2nd, Edition, 2016, Medeiros: Diagnostic Pathology - Lymph Nodes and Extranodal Lymphomas, 2nd Edition, 2017
Board review style question #1
Which of the following is the most common site of extranodal involvement in adult T cell
leukemia / lymphoma (ATLL)?
- Central nervous system
- Heart
- Liver
- Skin
Board review style answer #1
Board review style question #2
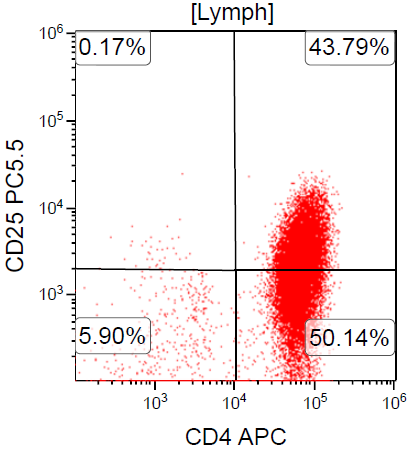
A 67 year old Haitian man with hepatitis B presents with fatigue and weakness. No other symptoms are present. Laboratory work up shows leukocytosis (55 x 109/L) and thrombocytopenia (100 x 109/L). Physical examination and imaging studies show massive splenomegaly with no lymphadenopathy. There was no hypercalcemia or increased in serum LDH. Peripheral smear review showed abnormal lymphocytosis with circulating lymphoma cells having mature nuclear features and highly lobulated nuclei. Flow cytometry performed in bone marrow aspirate is provided above. Serology for anti HTLV-1 antibody is positive. Which of the following is the most accurate statement?
- Dual positivity for CD4 and CD8 is uncommon in adult T cell leukemia / lymphoma
- Expression of CD25 is specific for ATLL among T cell lymphomas / leukemias
- Patient has acute myeloid leukemia with maturation (NK / myeloid type)
- Patient has T cell large granular lymphocytic leukemia (LGL)
Board review style answer #2
A. Dual positivity for CD4 and CD8 is uncommon in adult T cell leukemia / lymphoma
Comment here
Reference: ATLL
Comment here
Reference: ATLL