Table of Contents
Definition / general | Major updates | WHO (2016), WHO (2022) and ICC (2022) | Microscopic (histologic) images | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Nithagon P, Tsang P. WHO 2022 & ICC-B cell. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomaWHOHAEM5ICCBcell.html. Accessed April 16th, 2024.
Definition / general
- 2 new classification systems for B cell lymphoid neoplasms have emerged in 2022:
- WHO 5th edition (WHO HAEM5) (Leukemia 2022;36:1720)
- International Consensus Classification (ICC) (Blood 2022;140:1229)
- Evolution from the 2016 WHO revised 4th edition (WHO HAEM4R) classification system to the new version reflects advancements in genomic profiling and evidence based clinical data
- Updates include newly defined subtypes, more encompassing umbrella terms, deletion of old entities and modified nomenclature
- Putative new entities with limited data are designated as provisional in WHO HAEM4 and ICC but no provisional designation exists in WHO HAEM5 (see tables 1 and 2)
Major updates
- Certain newly added categories are specific to only one classification system (table 1), e.g.:
- Newly included nonneoplastic tumor-like lesions in WHO HAEM5 include IgG4 related disease and 2 additional types of Castleman disease (unicentric and idiopathic multicentric)
- EBV+ polymorphic B cell lymphoproliferative disorder, NOS is a new entity under ICC to describe EBV+ B cell lesions with altered nodal architecture that are not diagnostic of lymphoma
- Multiple myeloma (MM) is categorized by ICC into MM with recurrent genetic abnormalities (based on interphase FISH) and MM, NOS
- B prolymphocytic leukemia (B PLL) is no longer defined as an entity in WHO HAEM5 based on the notion that it represents prolymphocytoid transformation of various small B cell lymphoma entities (Ann Diagn Pathol 2021;54:151790)
- Under WHO HAEM5, previous cases of B PLL are categorized as one of the following entities:
- Mantle cell lymphoma with IGH::CCND1
- CD5 positive nonmantle B cell neoplasm with elevated prolymphocytes in peripheral blood or bone marrow
- Splenic B cell lymphoma / leukemia with prominent nucleoli
- ICC continues to recognize B PLL as a neoplasm after excluding transformation from other B cell entities
- Under WHO HAEM5, previous cases of B PLL are categorized as one of the following entities:
- Splenic B cell lymphoma / leukemia with prominent nucleoli (SBLPN):
- Corresponds to hairy cell leukemia (HCL) variant (rare, provisional entity) in WHO HAEM4R and ICC
- Newly created terminology under WHO HAEM5 reflects its biologic distinction from typical hairy cell leukemia (Expert Rev Hematol 2021;14:355)
- Includes previous cases of CD5 negative B PLL under WHO HAEM4R
- Marginal zone lymphomas:
- WHO HAEM5 and ICC both recognize pediatric nodal marginal zone lymphoma (pNMZL) as a separate entity from nodal marginal zone lymphoma (NMZL)
- WHO HAEM5 and ICC both recognize primary cutaneous marginal zone lymphoma / lymphoproliferative disorder as distinct from extranodal marginal zone lymphoma of MALT of other sites
- Follicular lymphoma:
- WHO HAEM5 recognizes 3 subsets of follicular lymphoma based on BCL2 gene rearrangement:
- Classic follicular lymphoma (cFL) with BCL2 rearrangement
- Follicular large B cell lymphoma (FLBL) without BCL2 rearrangement
- Follicular lymphoma with uncommon features (uFL) without BCL2 rearrangement
- Histologic grading of cFL is no longer mandatory
- ICC proposes a new provisional entity based on absence of BCL2 rearrangement
- BCL2 rearrangement negative, CD23 positive follicle center lymphoma (provisional): often diffuse
- Continues with grading of follicular lymphoma with emphasis on 3A and 3B
- ICC recognizes testicular follicular lymphoma as a new entity that is distinct from pediatric type follicular lymphoma
- WHO HAEM5 recognizes 3 subsets of follicular lymphoma based on BCL2 gene rearrangement:
- New large B cell lymphoma entities:
- Fibrin associated large B cell lymphoma (both WHO HAEM5 and ICC)
- Fluid overload associated large B cell lymphoma (WHO HAEM5) overlaps with HHV8 and EBV negative primary effusion based lymphoma (provisional entity in ICC); distinct from primary effusion lymphoma that is HHV8 associated
- Primary large B cell lymphomas of immune privileged site:
- New umbrella term in WHO HAEM5 encompassing diffuse large B cell lymphoma (DLBCL) of the following extranodal sites: CNS, vitreoretina compartment and testis
- ICC maintains that each should remain as distinct entities to facilitate further research
- Nodular lymphocyte predominant Hodgkin lymphoma (NLPHL):
- Known as NLPHL in WHO HAEM4R, it has been renamed under ICC as nodular lymphocyte predominant B cell lymphoma (NLPBL), in recognition of its overlap with T cell / histiocyte rich large B cell lymphoma (Pathology 2020;52:142)
- Under WHO HAEM5, the terminology remains unchanged and continues to list NLPHL under the family of Hodgkin lymphoma to avoid potential disruption of clinical trials
- However, WHO HAEM5 also recognizes it may be more accurately called nodular lymphocyte predominant B cell lymphoma (based on the neoplastic cells having a functional B cell program) and also accepts this term in preparation for future adoption
- Importance of different morphologic growth patterns (variant histology) in relation to clinical behavior is recognized by both ICC and WHO HAEM5 (Am J Surg Pathol 2003;27:1346)
- High grade B cell lymphomas (HGBCL):
- Previously a single entity, HGBCL with MYC and BCL2 or BCL6 rearrangement (double / triple hit lymphomas) has been categorized into 2 entities under WHO HAEM5:
- B cell lymphomas with dual MYC and BCL2 rearrangements are considered a homogenous entity and have been renamed as diffuse large B cell lymphoma / high grade B cell lymphoma with MYC and BCL2 rearrangements (DLBCL / HGBCL MYC / BCL2)
- B cell lymphomas with MYC and BCL6 rearrangements are biologically distinct from those with MYC / BCL2 rearrangements and are designated as DLBCL, NOS or HGBCL, NOS based on cytomorphology
- ICC recognizes 2 subtypes of HGBCL double hit:
- HGBCL with MYC and BCL2 rearrangements (with or without BCL6), an aggressive lymphoma of germinal center B cell origin
- HGBCL with MYC and BCL6 rearrangements, a provisional entity that has shown heterogeneous biology based on relatively small sample sizes (J Hematol Oncol 2022;15:26)
- Previously a single entity, HGBCL with MYC and BCL2 or BCL6 rearrangement (double / triple hit lymphomas) has been categorized into 2 entities under WHO HAEM5:
- Burkitt lymphoma:
- WHO HAEM5 recommends subtyping Burkitt lymphomas based on EBV status rather than epidemiologic context
- Under ICC, previous rare cases of TdT positive Burkitt lymphomas with IG::MYC translocation should be designated as B lymphoblastic leukemia / lymphoma with MYC rearrangement
- Burkitt-like lymphoma with 11q aberration:
- Provisional under WHO HAEM4R; resembling Burkitt lymphoma but lacking MYC rearrangement
- Under WHO HAEM5: renamed as high grade B cell lymphoma with 11q aberration
- Under ICC: renamed as large B cell lymphoma with 11q aberration, in recognition of its genetic profile being closer to DLBCL than Burkitt and occasional cases with predominantly large cell morphology
- Lymphoplasmacytic lymphoma (LPL):
- MYD88 p.L265P mutation (> 90%)
- CXCR4 mutations (30 - 40%), associated with drug resistance and increased bone marrow disease (J Clin Oncol 2020;38:1198)
- WHO HAEM5 recognizes 2 subsets of LPL:
- IgM LPL / Waldenström macroglobulinemia
- Non-Waldenström macroglobulinemia (includes IgG / IgA cases, nonsecretory LPL and IgM LPL without bone marrow involvement)
- IgM monoclonal gammopathy of undetermined significance (MGUS):
- ICC recognizes 2 distinct subtypes of IgM MGUS:
- IgM MGUS of plasma cell type (precursor of MM)
- IgM MGUS, NOS (may show MYD88 mutation or monoclonal B cells)
- ICC recognizes 2 distinct subtypes of IgM MGUS:
- Monoclonal gammopathy of renal significance (MGRS):
- WHO HAEM5 defines MGRS as a new entity
- ICC considers MGRS as a clinical description of the underlying MGUS rather than a distinct entity
- Cold agglutinin disease or primary cold agglutinin disease:
- A new diagnostic category in both WHO HAEM5 and ICC
- Clonal B cell proliferation usually of IgM isotype, distinct from IgM MGUS and LGL and lacking MYD88 L265P mutation (Clin Adv Hematol Oncol 2020;18:35)
- Plasma cell neoplasms with associated paraneoplastic syndrome:
- WHO HAEM5 recognizes a new syndrome: adenopathy and extensive skin patch overlying a plasmacytoma (AESOP) (Blood Cancer J 2022;12:58)
- Lymphoid proliferations / lymphomas with immune deficiency or dysregulation:
- WHO HAEM4R: categorization based on underlying etiology (primary immune disorders, HIV, posttransplant status and iatrogenic agents / immunosuppressants)
- WHO HAEM5: new integrated approaches with 3 components
- Histologic diagnosis (hyperplasia, polymorphic lymphoproliferation, mucocutaneous ulcer or lymphoma)
- Oncologic viral association (EBV or KSHV / HHV8)
- Immune deficiency / dysregulation (HIV, inborn error of immunity, posttransplant, autoimmune, iatrogenic or immune senescence)
- ICC: retains posttransplant lymphoproliferative disorders (PTLD) as a subgroup of iatrogenic lymphoid lesions with distinct clinical management
- B lymphoblastic leukemia / lymphoma (B ALL) (see table 2):
- WHO HAEM5 uses shorter nomenclature consisting of gene names of molecular drivers but excluding the cytogenetic changes that appeared in the WHO HAEM4R nomenclature (e.g., B ALL with BCR::ABL1 fusion in WHO HAEM5 is equivalent to B ALL with t(9;22)(q34;q11.2); BCR-ABL1 in WHO HAEM4R)
- Under WHO HAEM5, B ALL with BCR::ABL1-like features is no longer considered a provisional entity as in WHO HAEM4R
- 2 new entities are recognized in WHO HAEM5:
- B ALL with ETV6::RUNX1-like features (distinct from B ALL with ETV6::RUNX1 fusion)
- B ALL with TCF3::HLF fusion (associated with aggressive behavior)
- No major reclassification of most B ALL entities in WHO HAEM5
WHO (2016), WHO (2022) and ICC (2022)
Table 1: Mature B cell entities - comparison of 3 classification systems
| WHO HAEM4R | WHO HAEM5 | ICC |
| Tumor-like lesions with B cell proliferation | ||
| Not included | Reactive B cell rich lymphoid proliferations that can mimic lymphoma | |
| Not included | IgG4 related disease | |
| Not included | Unicentric Castleman disease | |
| Not included | Idiopathic multicentric Castleman disease | |
| Multicentric Castleman disease | KSHV / HHV8 associated multicentric Castleman disease | Multicentric Castleman disease |
| Not included | EBV positive polymorphic B cell lymphoproliferative disorder, NOS | |
| Neoplastic and preneoplastic small lymphocytic proliferation | ||
| Chronic lymphocytic leukemia / small lymphocytic lymphoma (CLL / SLL) | Chronic lymphocytic leukemia / small lymphocytic lymphoma (CLL / SLL) | Chronic lymphocytic leukemia / small lymphocytic lymphoma (CLL / SLL) |
Monoclonal B cell lymphocytosis
| Monoclonal B cell lymphocytosis
| Monoclonal B cell lymphocytosis
|
| B prolymphocytic leukemia (B PLL) | Not a distinct entity but heterogeneous | B prolymphocytic leukemia (B PLL) |
Lymphoplasmacytic lymphoma
| Lymphoplasmacytic lymphoma
| Lymphoplasmacytic lymphoma
|
| Marginal zone lymphoma | ||
| Nodal marginal zone lymphoma | Nodal marginal zone lymphoma | Nodal marginal zone lymphoma |
| Pediatric nodal marginal zone lymphoma* | Pediatric nodal marginal zone lymphoma | Pediatric nodal marginal zone lymphoma* |
| Extranodal marginal zone lymphoma of mucosa associated lymphoid tissue (MALT) | Extranodal marginal zone lymphoma of mucosa associated lymphoid tissue (MALT) | Extranodal marginal zone lymphoma of mucosa associated lymphoid tissue (MALT) |
| Not included; part of extranodal marginal zone lymphoma of MALT | Primary cutaneous marginal zone lymphoma | Primary cutaneous marginal zone lymphoproliferative disorder |
| Splenic B cell lymphoma / leukemia | ||
| Splenic marginal zone lymphoma | Splenic marginal zone lymphoma | Splenic marginal zone lymphoma |
| Hairy cell leukemia | Hairy cell leukemia | Hairy cell leukemia |
| Hairy cell leukemia variant* | Splenic B cell lymphoma / leukemia with prominent nucleoli (distinct from HCL and includes all previous CD5 negative B PLL) | Hairy cell leukemia variant* |
| Splenic diffuse red pulp small B cell lymphoma* | Splenic diffuse red pulp small B cell lymphoma | Splenic diffuse red pulp small B cell lymphoma* |
| Follicular lymphoma | ||
| In situ follicular neoplasia | In situ follicular B cell neoplasm | In situ follicular neoplasia |
| Follicular lymphoma (FL) | Follicular lymphoma (grading of cFL not mandatory)
| Follicular lymphoma (continue grading FL with emphasis on 3A and 3B)
|
| Pediatric type follicular lymphoma | Pediatric type follicular lymphoma | Pediatric type follicular lymphoma |
| Not included | Testicular follicular lymphoma | |
| Duodenal type follicular lymphoma | Duodenal type follicular lymphoma | Duodenal type follicular lymphoma |
| Primary cutaneous follicle center lymphoma | Primary cutaneous follicle center lymphoma | Primary cutaneous follicle center lymphoma |
| Mantle cell lymphoma | ||
| In situ mantle cell neoplasia | In situ mantle cell neoplasia | In situ mantle cell neoplasia |
| Mantle cell lymphoma | Mantle cell lymphoma | Mantle cell lymphoma |
| Leukemic nonnodal mantle cell lymphoma | Leukemic nonnodal mantle cell lymphoma | Leukemic nonnodal mantle cell lymphoma |
| Aggressive lymphomas transformed from low grade B cell lymphomas | ||
| Not included | Transformations of indolent B cell lymphomas | |
| Large B cell lymphoma | ||
| Diffuse large B cell lymphoma (DLBCL), NOS | Diffuse large B cell lymphoma, NOS | Diffuse large B cell lymphoma, NOS |
| EBV positive mucocutaneous ulcer* | EBV positive mucocutaneous ulcer | EBV positive mucocutaneous ulcer |
| EBV positive diffuse large B cell lymphoma, NOS | EBV positive diffuse large B cell lymphoma | EBV positive diffuse large B cell lymphoma, NOS |
| Diffuse large B cell lymphoma associated with chronic inflammation | Diffuse large B cell lymphoma associated with chronic inflammation | Diffuse large B cell lymphoma associated with chronic inflammation |
| Primary large B cell lymphoma of the central nervous system | Primary large B cell lymphoma of immune privileged sites (new umbrella term for DLBCL arising in the CNS, vitreoretina and testis) | Primary diffuse large B cell lymphoma of central nervous system |
| Not included | Primary diffuse large B cell lymphoma of testis | |
| Primary cutaneous diffuse large B cell lymphoma, leg type | Primary cutaneous diffuse large B cell lymphoma, leg type | Primary cutaneous diffuse large B cell lymphoma, leg type |
| Intravascular large B cell lymphoma | Intravascular large B cell lymphoma | Intravascular large B cell lymphoma |
| ALK positive large B cell lymphoma | ALK positive large B cell lymphoma | ALK positive large B cell lymphoma |
| Plasmablastic lymphoma | Plasmablastic lymphoma | Plasmablastic lymphoma |
| Large B cell lymphoma with IRF4 rearrangement | Large B cell lymphoma with IRF4 rearrangement | Large B cell lymphoma with IRF4 rearrangement |
| Primary mediastinal large B cell lymphoma | Primary mediastinal large B cell lymphoma | Primary mediastinal large B cell lymphoma |
| B cell lymphoma, unclassified with features intermediate between DLBCL and classic Hodgkin lymphoma | Mediastinal gray zone lymphoma (cases without mediastinal involvement are classified as DLBCL, NOS) | Mediastinal gray zone lymphoma |
| Not included | Fibrin associated large B cell lymphoma | Fibrin associated large B cell lymphoma |
| Not included | Fluid overload associated large B cell lymphoma (previously included in primary effusion lymphoma) | HHV8 and EBV8 negative primary effusion based lymphoma* |
| T cell / histiocyte rich large B cell lymphoma | T cell / histiocyte rich large B cell lymphoma | T cell / histiocyte rich large B cell lymphoma |
| See Hodgkin lymphomas | See Hodgkin lymphomas | Nodular lymphocyte predominant B cell lymphoma (renamed from nodular lymphocyte predominant Hodgkin lymphoma) |
| Lymphomatoid granulomatosis | Lymphomatoid granulomatosis | Lymphomatoid granulomatosis |
| KSHV / HHV8 associated B cell lymphoid proliferation / lymphoma | ||
| Primary effusion lymphoma | Primary effusion lymphoma | Primary effusion lymphoma |
| HHV8 positive diffuse large B cell lymphoma, NOS | HHV8 positive diffuse large B cell lymphoma | HHV8 positive diffuse large B cell lymphoma, NOS |
| HHV8 positive germinotropic lymphoproliferative disorder | KSHV / HHV8 positive germinotropic lymphoproliferative disorder | HHV8 positive germinotropic lymphoproliferative disorder |
| High grade B cell lymphomas | ||
| High grade B cell lymphoma, NOS | High grade B cell lymphoma, NOS | High grade B cell lymphoma, NOS |
| High grade B cell lymphoma with MYC and BCL2 or BCL6 rearrangements | Diffuse large B cell lymphoma / high grade B cell lymphoma with MYC and BCL2 rearrangements (previous high grade B cell lymphoma with MYC and BCL6 rearrangements is designated as DLBCL, NOS) | High grade B cell lymphoma with MYC and BCL2 rearrangements |
| High grade B cell lymphoma with MYC and BCL6 rearrangements* | ||
| Burkitt lymphoma | Burkitt lymphoma (EBV status supersedes epidemiologic subtyping) | Burkitt lymphoma |
| Burkitt-like lymphoma with 11q aberration* | High grade B cell lymphoma with 11q aberration | Large B cell lymphoma with 11q aberration* |
| Hodgkin lymphomas | ||
Classic Hodgkin lymphoma
| Classic Hodgkin lymphoma
| Classic Hodgkin lymphoma
|
| Nodular lymphocyte predominant Hodgkin lymphoma | Nodular lymphocyte predominant Hodgkin lymphoma | Renamed as nodular lymphocyte predominant B cell lymphoma; categorized as non-Hodgkin lymphoma |
| Plasma cell neoplasms and entities with paraproteins | ||
| Solitary plasmacytoma of bone | Solitary plasmacytoma of bone | Solitary plasmacytoma of bone |
| Extraosseous plasmacytoma | Extraosseous plasmacytoma | Extraosseous plasmacytoma |
| Plasma cell myeloma | Plasma cell myeloma | Multiple myeloma (MM), NOS |
MM with recurrent genetic abnormality
| ||
Plasma cell neoplasm with associated paraneoplastic syndrome
| Plasma cell neoplasm with associated paraneoplastic syndrome
| |
| IgM monoclonal gammopathy of undetermined significance | IgM monoclonal gammopathy of undetermined significance | IgM monoclonal gammopathy of undetermined significance
|
| Non-IgM monoclonal gammopathy of undetermined significance | Non-IgM monoclonal gammopathy of undetermined significance | Non-IgM monoclonal gammopathy of undetermined significance |
| Not included | Monoclonal gammopathy of renal significance | Not a separate entity; clinical descriptor of the underlying diagnosis (e.g., MGUS) |
| Not included | Cold agglutinin disease | Primary cold agglutinin disease |
| Primary amyloidosis | Immunoglobulin related (AL) amyloidosis | Immunoglobulin light chain (AL) amyloidosis |
| Localized AL amyloidosis | ||
| Light chain and heavy chain deposition disease | Monoclonal immunoglobulin deposition disease (renamed) | Light chain and heavy chain deposition |
| Mu heavy chain disease | Mu heavy chain disease | Mu heavy chain disease |
| Gamma heavy chain disease | Gamma heavy chain disease | Gamma heavy chain disease |
| Alpha heavy chain disease | Alpha heavy chain disease | Alpha heavy chain disease |
| Lymphoid proliferations / lymphomas with immune deficiency or dysregulation | ||
| Nondestructive PTLD | Hyperplasias arising in immune deficiency / dysregulation | Plasmacytic hyperplasia PTLD |
| Florid follicular hyperplasia PTLD | ||
| Infectious mononucleosis PTLD | ||
| Polymorphic PTLD | Polymorphic lymphoproliferative disorders arising in immune deficiency / dysregulation (new term that includes various etiologies) | Polymorphic PTLD |
| Other iatrogenic immunodeficiency associated lymphoproliferative disorders | Other iatrogenic immunodeficiency associated lymphoproliferative disorders | |
| Monomorphic PTLD | Lymphomas arising in immune deficiency / dysregulation (new umbrella term that includes monomorphic PTLD, lymphomas associated with HIV infection, etc.) | Monomorphic PTLD |
| Classic Hodgkin lymphoma PTLD | Classic Hodgkin lymphoma PTLD | |
| Lymphomas associated with HIV infection | ||
| Lymphoproliferative diseases associated with primary immune disorders | Inborn error of immunity associated lymphoid proliferations and lymphomas | |
Table 2: Precursor B cell neoplasms - comparison of WHO 4th and 5th edition classification systems
| WHO HAEM4R | WHO HAEM5 | ||||||||||||
| B lymphoblastic leukemia / lymphoma, NOS | B lymphoblastic leukemia / lymphoma, NOS | ||||||||||||
| B lymphoblastic leukemia / lymphoma with hyperdiploidy | B lymphoblastic leukemia / lymphoma with high hyperdiploidy | ||||||||||||
| B lymphoblastic leukemia / lymphoma with hypodiploidy | B lymphoblastic leukemia / lymphoma with hypodiploidy | ||||||||||||
| B lymphoblastic leukemia / lymphoma with iAMP21 | B lymphoblastic leukemia / lymphoma with iAMP21 | ||||||||||||
| B lymphoblastic leukemia / lymphoma with t(9;22)(q34;q11.2); BCR-ABL1 | B lymphoblastic leukemia / lymphoma with BCR::ABL1 fusion | ||||||||||||
| B lymphoblastic leukemia / lymphoma, BCR-ABL1-like* | B lymphoblastic leukemia / lymphoma with BCR::ABL1-like features | ||||||||||||
| B lymphoblastic leukemia / lymphoma with t(12;21)(p13.2;q22.1); ETV6-RUNX1 | B lymphoblastic leukemia / lymphoma with ETV6::RUNX1
| Not included
| B lymphoblastic leukemia / lymphoma with ETV6::RUNX1-like feature
| B lymphoblastic leukemia / lymphoma with t(1;19)(q23;p13.3); TCF3-PBX1 | B lymphoblastic leukemia / lymphoma with TCF3::PBX1 fusion
| Not included
| B lymphoblastic leukemia / lymphoma with TCF3::HLF fusion
| B lymphoblastic leukemia / lymphoma with t(v;11q23.3); KMT2A rearranged | B lymphoblastic leukemia / lymphoma with KMT2A rearrangement
| B lymphoblastic leukemia / lymphoma with t(5;14)(q31.1;q32.1); IGH / IL3 | B lymphoblastic leukemia / lymphoma with IGH::IL3 fusion
| B lymphoblastic leukemia / lymphoma with other defined genetic abnormalities | B lymphoblastic leukemia / lymphoma with other defined genetic abnormalities
| |
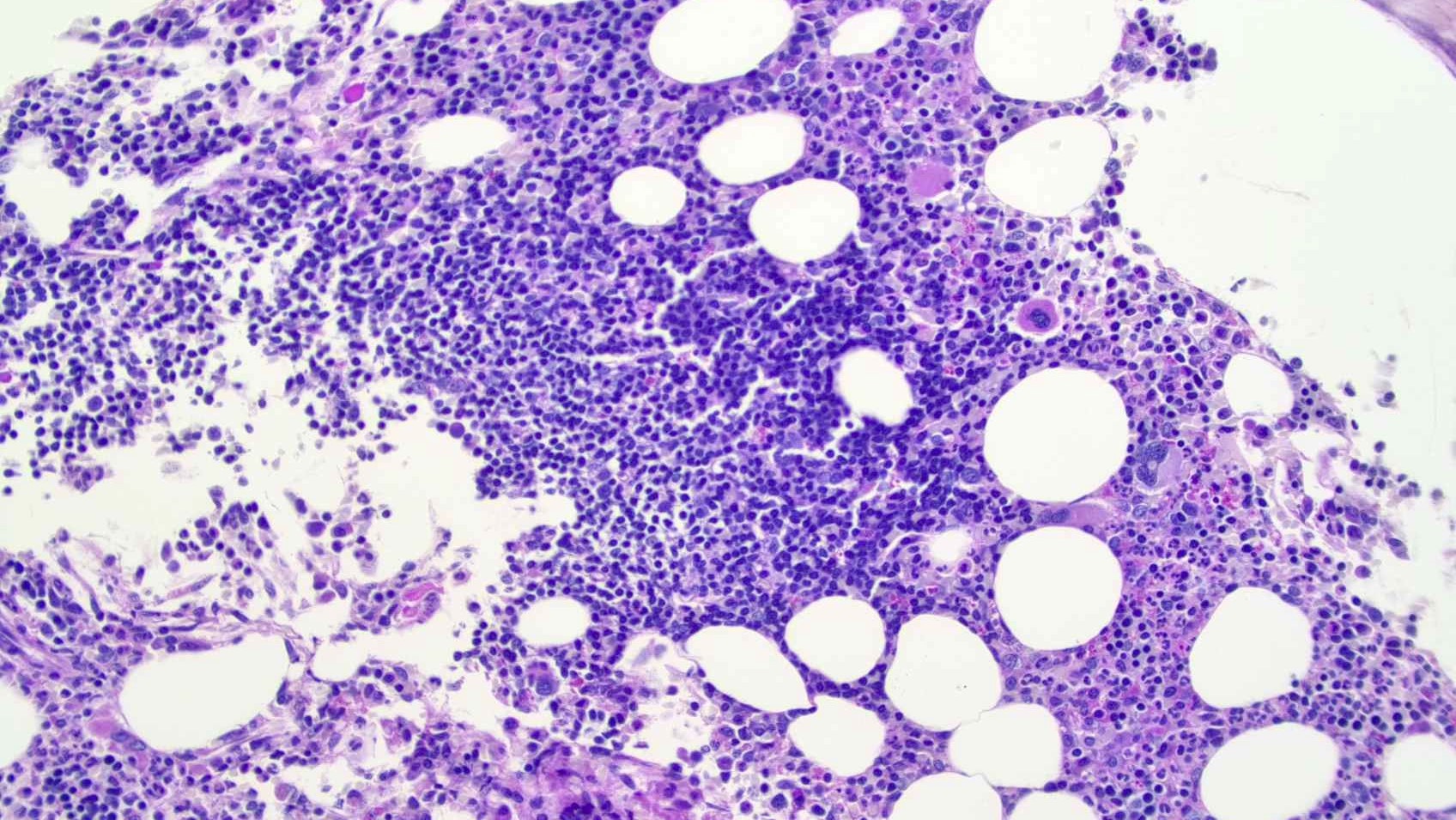
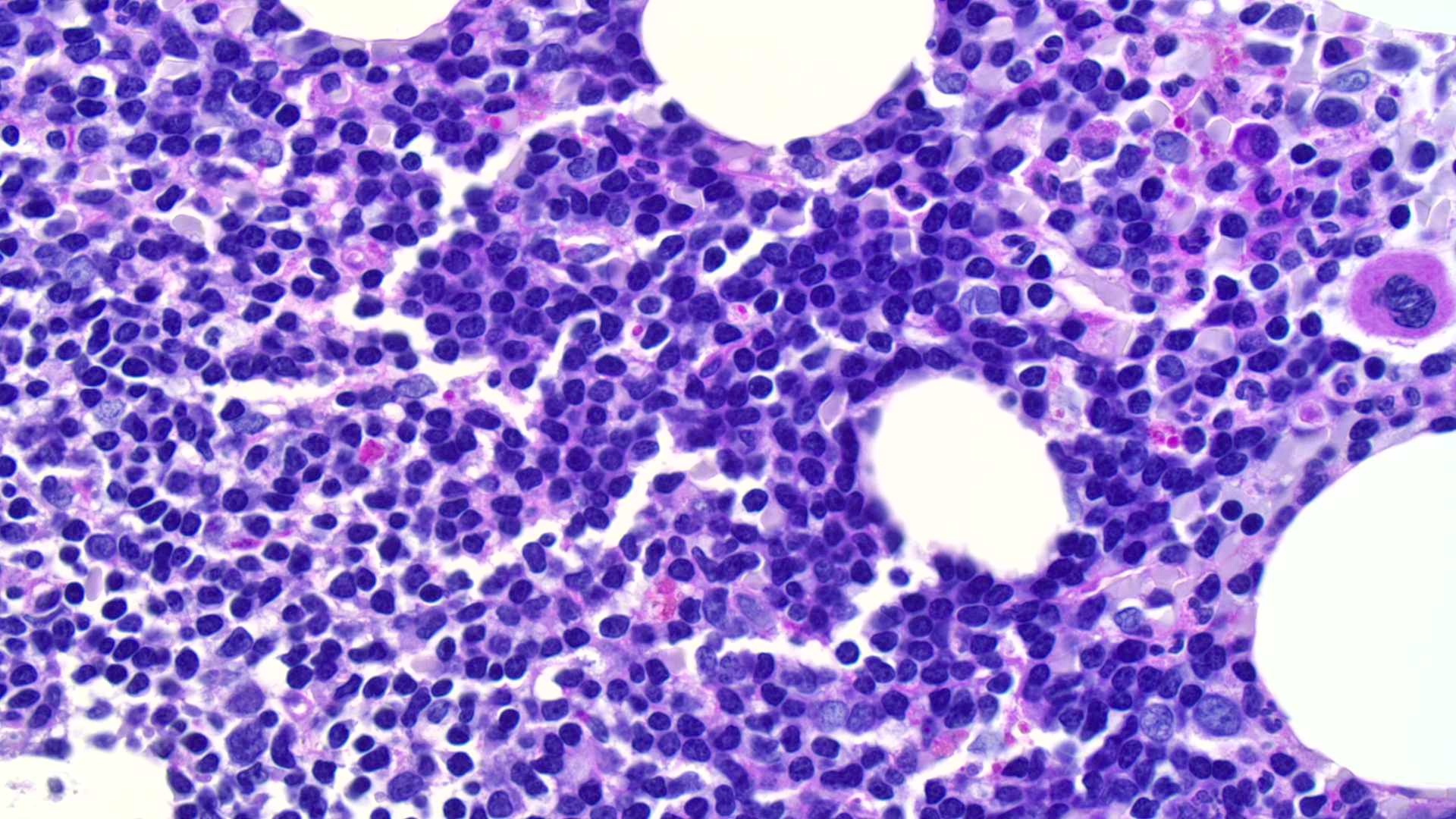
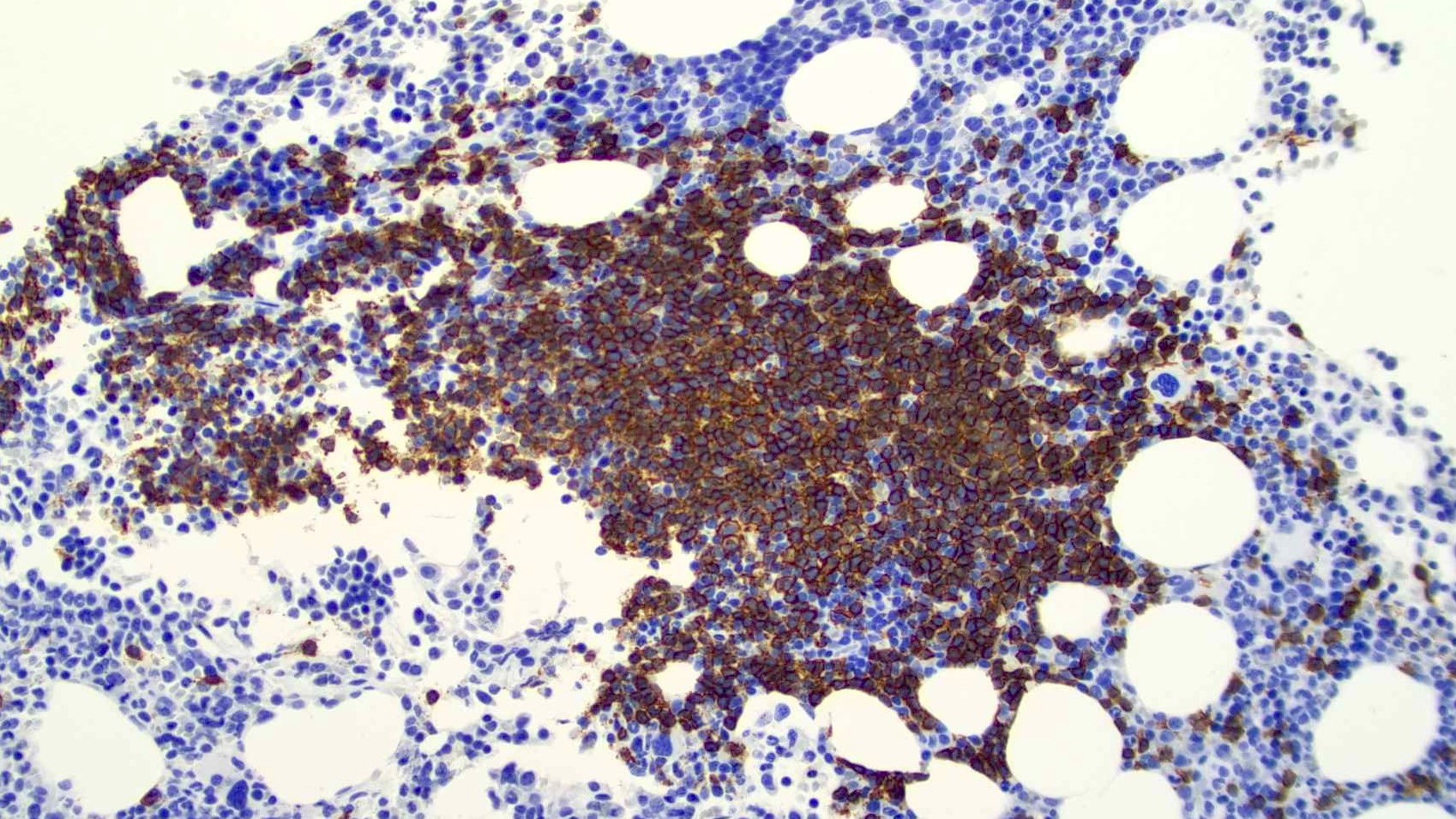
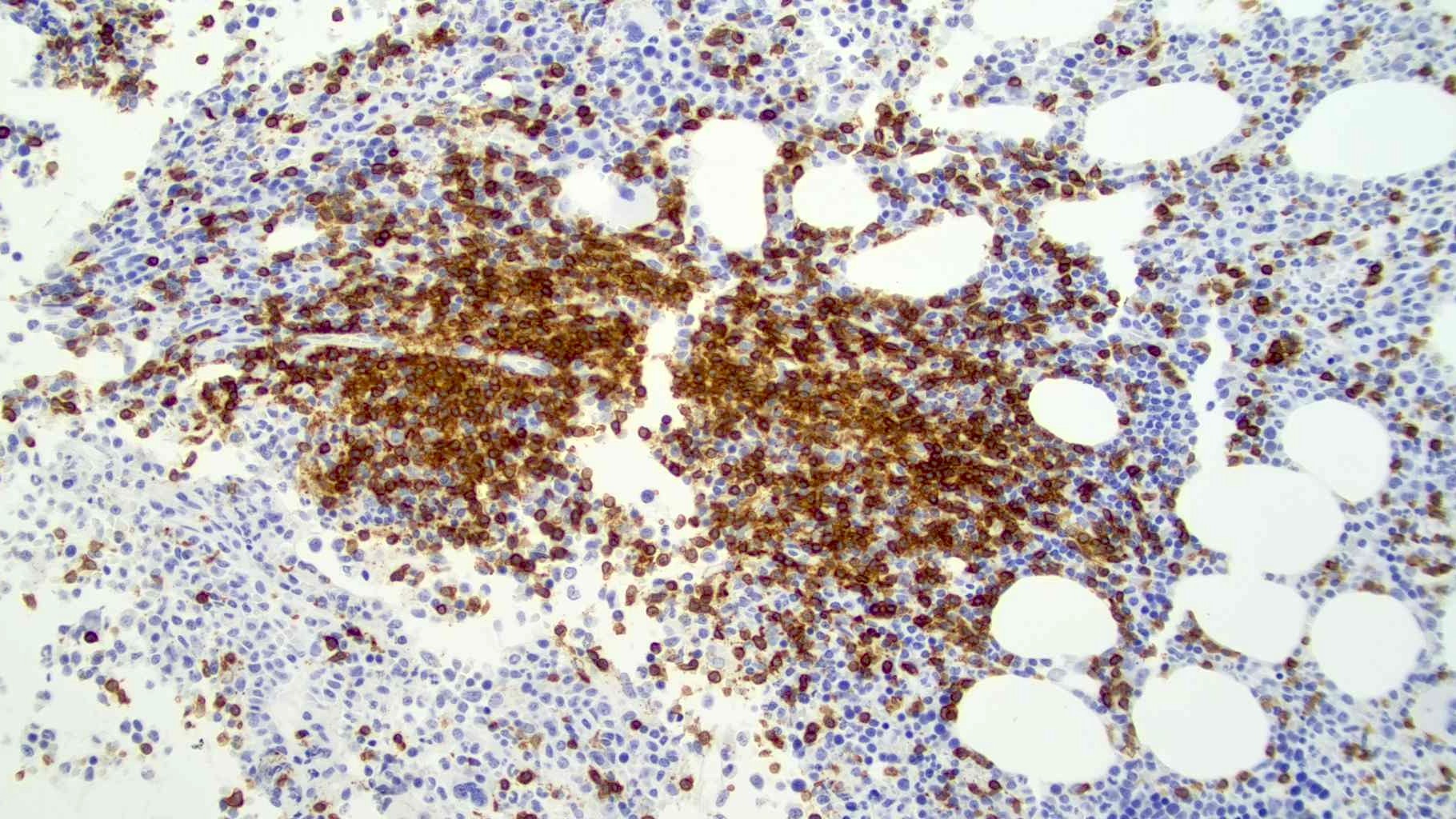
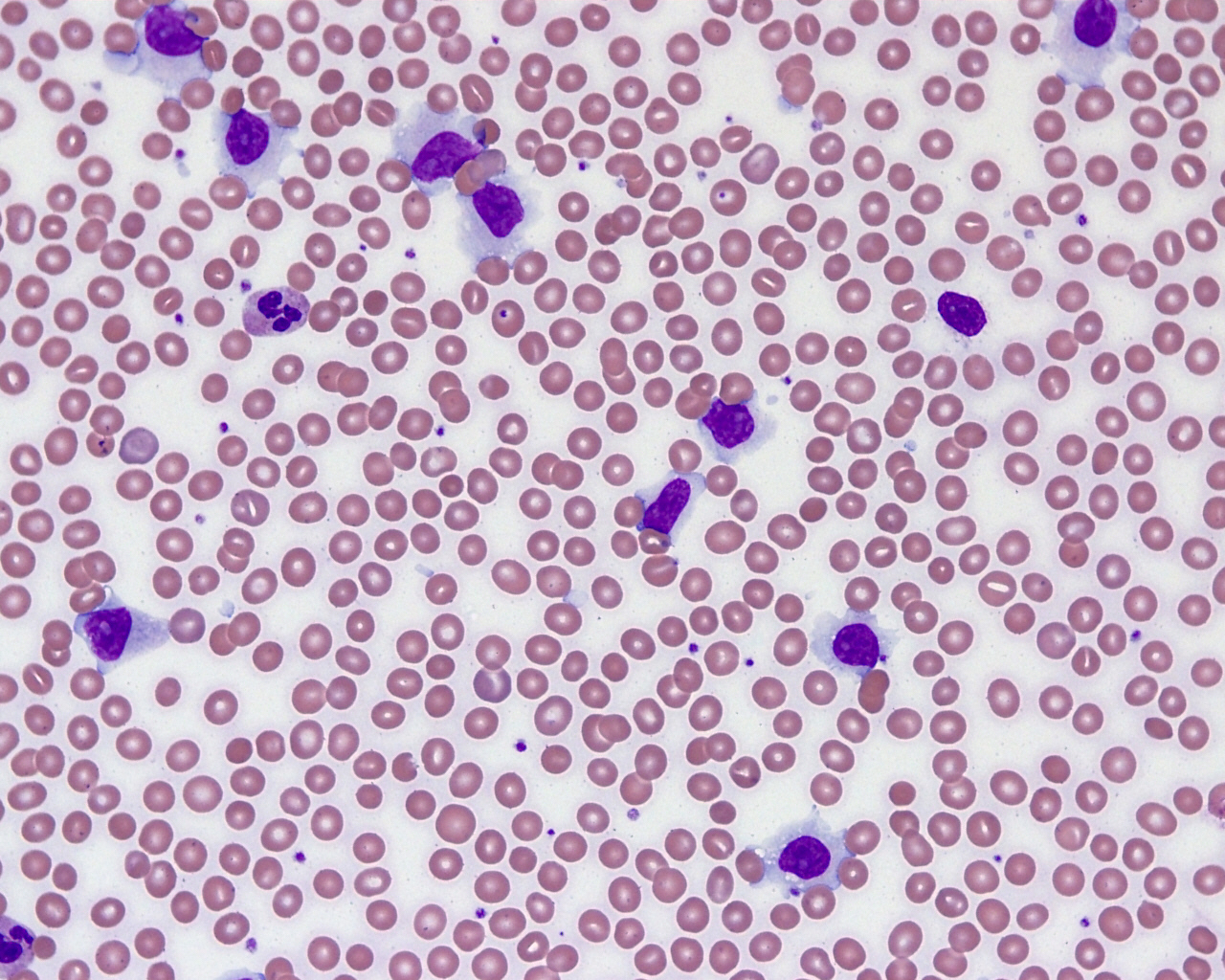
Microscopic (histologic) images
Additional references
Board review style question #1
Which of the following is a characteristic of splenic B cell lymphoma / leukemia with prominent nucleoli as defined in the WHO classification of hematolymphoid neoplasms, 5th edition (WHO HAEM5)?
- Classified as an immature B cell lymphoid neoplasm
- Considered as a subtype of diffuse large B cell lymphoma originating from the spleen
- Corresponds to hairy cell leukemia variant under the WHO classification, 4th edition
- Shares a similar genetic profile with hairy cell leukemia
- Tumor cells characteristically coexpress CD5
Board review style answer #1
C. Corresponds to hairy cell leukemia variant under the WHO classification, 4th edition. This entity is a mature B cell neoplasm that is biologically distinct from both hairy cell leukemia and diffuse large B cell lymphoma and typically lacks CD5 coexpression.
Comment Here
Reference: WHO HAEM5 and ICC-B cell
Comment Here
Reference: WHO HAEM5 and ICC-B cell
Board review style question #2
Which of the following is true regarding B cell or plasma cell neoplasms as defined by the International Consensus Classification (ICC) system?
- B cell prolymphocytic leukemia is the counterpart of Richter transformation of small lymphocytic lymphoma
- Lymphoplasmacytic lymphoma can manifest clinically as primary cold agglutinin disease
- Multiple myeloma with recurrent genetic abnormality is a newly added category
- Nodular lymphocytic predominant B cell lymphoma is renamed from nodular sclerosis Hodgkin lymphoma
- Testicular follicular lymphoma is a provisional subtype of pediatric type follicular lymphoma
Board review style answer #2
C. Multiple myeloma with recurrent genetic abnormality is a newly added category in the International Consensus Classification system.
Comment Here
Reference: WHO HAEM5 and ICC-B cell
Comment Here
Reference: WHO HAEM5 and ICC-B cell