Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1Cite this page: Goksu BB, Murga-Zamalloa CA. Primary cutaneous acral CD8+ lymphoproliferative disorder. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomanonbacraltcell.html. Accessed April 19th, 2024.
Definition / general
- Rare indolent lymphoproliferative disorder characterized by slow growing papules or nodules in acral sites with a dermal infiltrate of CD8+ T lymphocytes
Essential features
- Mostly characterized by a solitary, slow growing nodule (Am J Surg Pathol 2007;31:1887, Mod Pathol 2020;33:83)
- Typically occurs in adults older than 50 years, with a male predominance (Arch Pathol Lab Med 2017;141:1469, Br J Dermatol 2022;186:887)
- Dense, diffuse dermal infiltrate with sparing of the epidermis
- CD8 and CD3 positive staining
Terminology
- Primary cutaneous acral CD8+ lymphoproliferative disorder (Leukemia 2022;36:1720)
ICD coding
- ICD-10: C84.A0 - cutaneous T cell lymphoma, unspecified, unspecified site
Epidemiology
- Fewer than 100 cases have been reported
- Male predilection (M:F = 1.7:1) (J Cutan Pathol 2016;43:125, Br J Dermatol 2022;186:887)
- Median age of diagnosis is 54 years (Br J Dermatol 2022;186:887)
Sites
- Usually localized to the dermis in the ear (Br J Dermatol 2022;186:887)
- Multiple sites of involvement may be present
- Other sites may include the nose, hands, elbows and feet
- No extracutaneous involvement is present
Pathophysiology
- Pathophysiology is not known
Etiology
- Cell of origin is activated mature T lymphocyte, CD3+ / CD8+ type
Clinical features
- Painful, slowly growing single papule or nodule localized in the ear
- Always an indolent course (Blood 2016;127:2375)
- Cure is expected after local excision or localized therapy in 70% of patients; persistent disease in 20%
Diagnosis
- Biopsy or excision
Radiology description
- Single lesion localized to dermis
- No systemic dissemination
- Rare multifocal
Prognostic factors
- Recurrences are rare and are limited to the dermis
- Surgical excision or radiotherapy usually result in cure (70%) with an overall low relapse rate (20%) (Br J Dermatol 2022;186:887)
- Relapsing / progressing disease more frequent in younger patients (Br J Haematol 2019;185:598)
Case reports
- 16 year old boy with an enlarging solitary lesion on the right lower eyelid of 1 month duration and presence of CD56 expression and high Ki67 proliferation (J Cutan Pathol 2021;48:1489)
- 35 year old man and 45 year old woman with nasal involvement and similar clinical and histomorphological features (J Cutan Pathol 2010:37;977)
- 52 year old man and 41 year old man with indolent CD8+ lymphoid proliferation of the ear (J Cutan Pathol 2011:38;209)
- 53 year old woman with a 12 month history of an asymptomatic solitary right leg nodule with atypical BCL6 / GATA3 positivity (Am J Dermatopathol 2021;43:137)
- 57 year old man with history of slowly growing ear nodule with signet ring features (Histopathology 2009;55:468)
- 69 year old man with a 10 year history of a solitary slow growing plaque on the left ear and a 4 year history of an identical plaque on the right ear with presence of double positive CD8 / CD4 and associated with thymic carcinoma (J Cutan Pathol 2019;46:231)
- 69 year old man with history of relapsing asymptomatic nodules confined to the left ear with extracutaneous involvement (J Cutan Pathol 2017;44:964)
- 3 cases with largest review of the literature, including 52 additional cases (J Cutan Pathol 2016;43:125)
- 3 cases with ear involvement and review of the literature (Am J Dermatopathol 2019;41:644)
- First report defining the entity included 4 cases with ear involvement (Am J Surg Pathol 2007:31:1887)
Treatment
- Surgical excision or radiotherapy
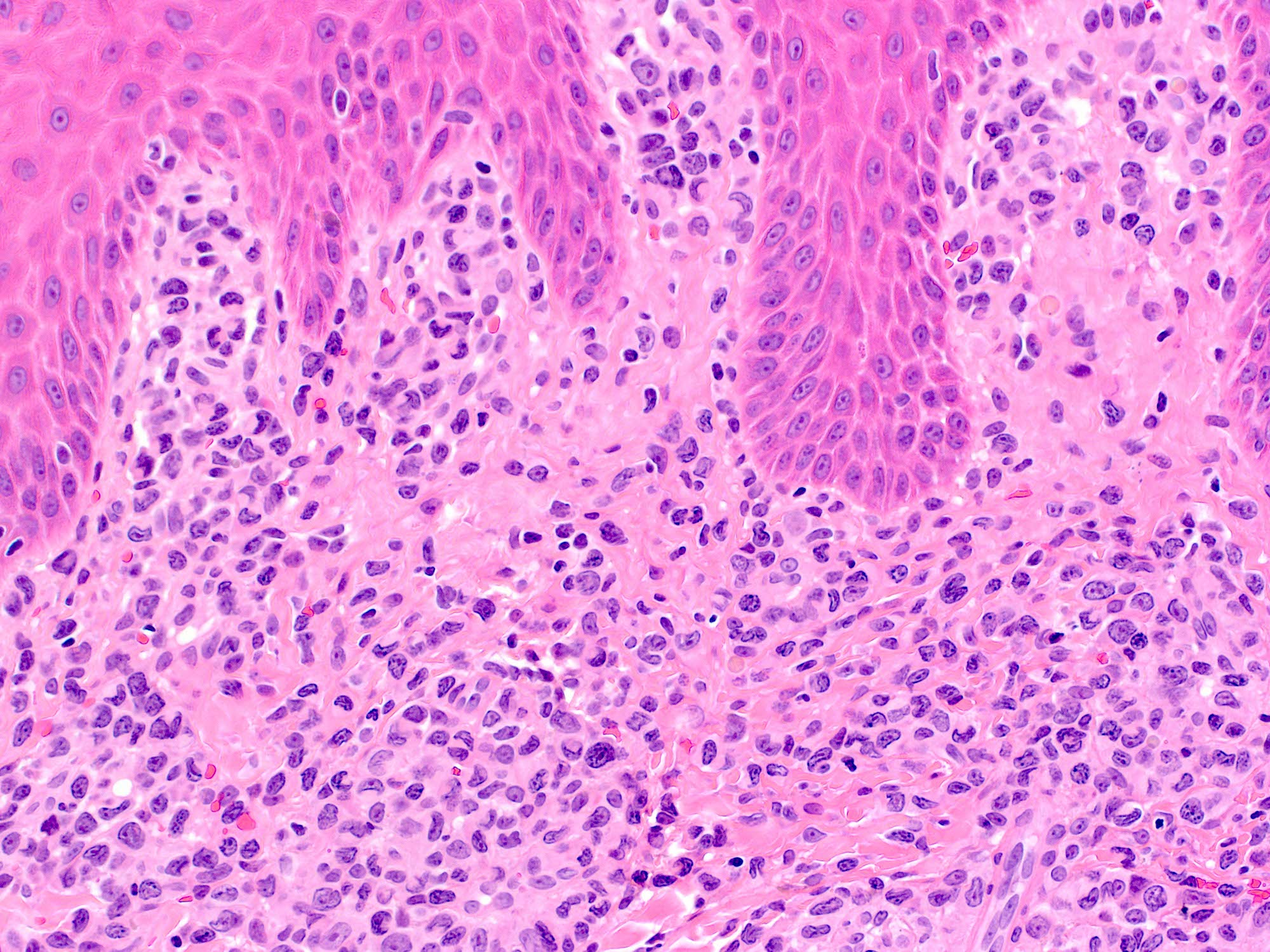
Microscopic (histologic) description
- Dense, diffuse dermal infiltrate with sparing of the epidermis and presence of a thin grenz zone
- Infiltrate is composed of medium to large size atypical lymphocytes (blast-like) with irregular nuclear membranes, small nucleoli and scant cytoplasm; signet ring cells can be present
- No fat rimming, angiodestruction or necrosis is identified
- Focal epidermotropism and exocytosis of atypical lymphocytes have been noted in rare cases
- References: Arch Pathol Lab Med 2017;141:1469, Br J Dermatol 2022;186:887
Microscopic (histologic) images
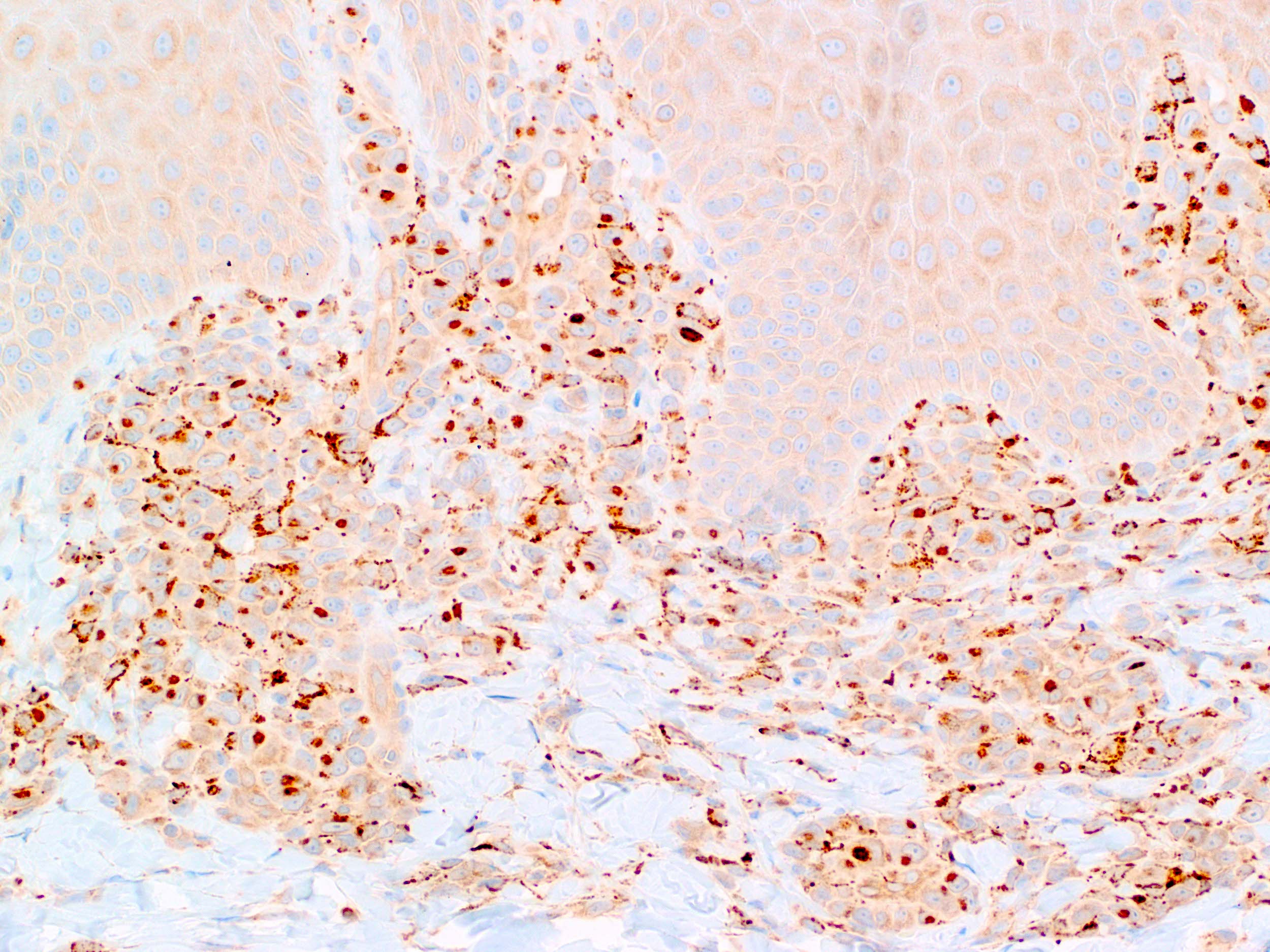
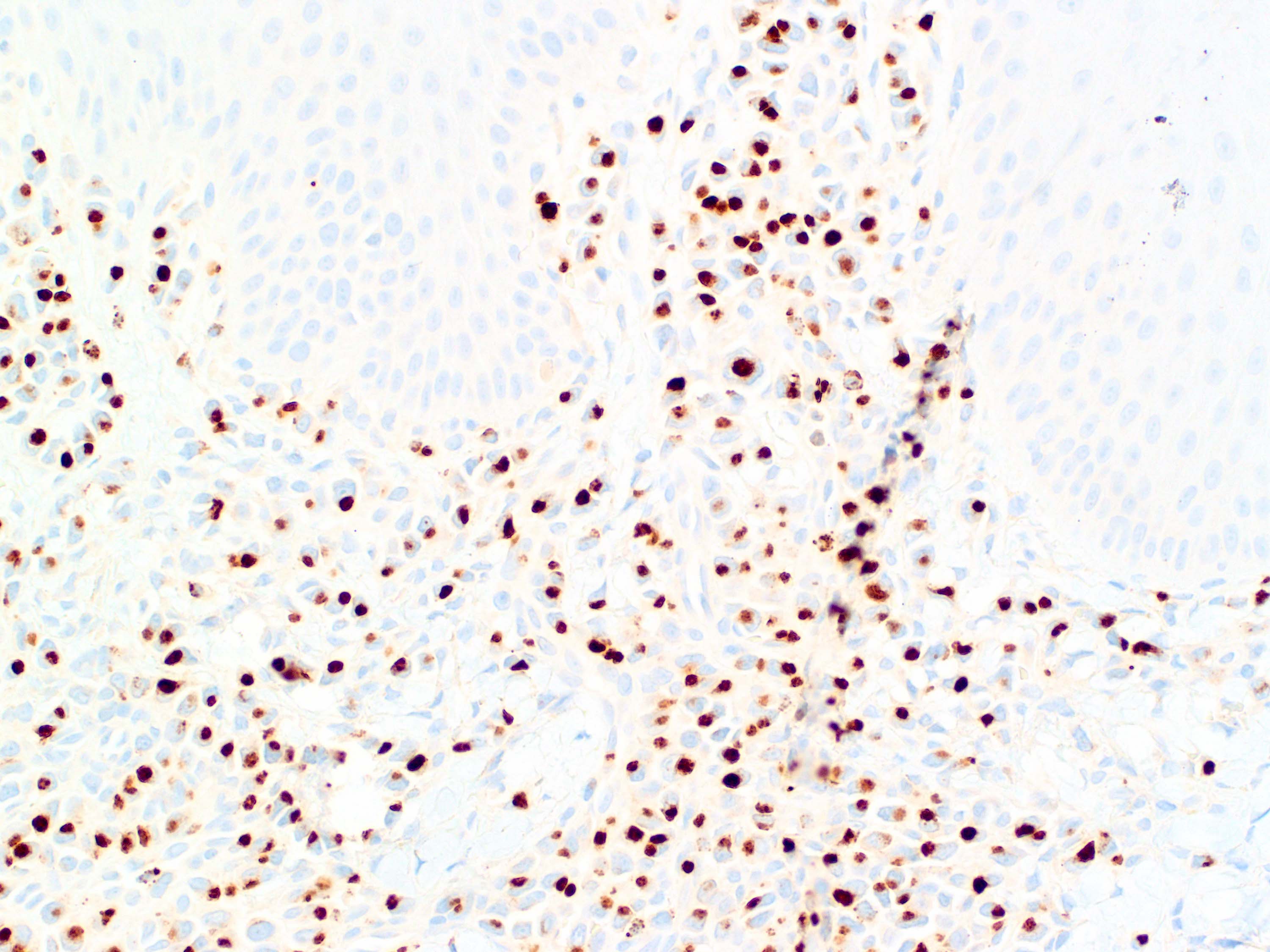
Positive stains
- CD8, CD3, TIA1 (focal), granzyme B (commonly negative; focal occasionally), T cell receptor BF1
- Characteristic dot-like pattern of CD68 expression (negativity doesn't exclude the diagnosis) (Br J Dermatol 2022;186:887)
- Aberrant loss of CD2, CD5 and CD7 may be present in a proportion of the atypical lymphocytes
- Ki67 expression is frequently low (< 10%); some low moderate (20 - 30%) (Arch Pathol Lab Med 2017;141:1469)
Negative stains
- CD30, EBV, CD56, CD4, granzyme B
Molecular / cytogenetics description
- Clonal TCR gene rearrangements present by PCR testing in almost 100% of cases
Sample pathology report
- Skin, left ear, punch biopsies:
- CD8+ positive cutaneous lymphoproliferative disorder (see comment)
- Comment: The morphological features and immunohistochemical findings are most consistent with a low grade CD8+ cutaneous lymphoproliferative disorder. If the lesion is unique and localized to the ear, the findings are most consistent with primary cutaneous acral CD8+ lymphoproliferative disorder (Leukemia 2022;36:1720).
Differential diagnosis
- Hydroa vacciniforme-like lymphoma:
- Primary cutaneous CD8+ aggressive epidermotropic cytotoxic T cell lymphoma:
- Features skin papules or nodules with an aggressive clinical course, characterized by rapid progression, ulceration, poor response to chemotherapy and a 5 year overall survival rate of 32% (Mod Pathol 2017;30:761)
- Morphologically characterized by full thickness pagetoid epidermotropism
- Occasional cases show predominant dermal infiltrates; however, this is associated with atrophic epidermis and infiltration of adjacent adnexal structures (Mod Pathol 2017;30:761)
- Tumor cells display a high Ki67 proliferation index (more than 50%)
- Primary cutaneous gamma delta T cell lymphoma:
- Subcutaneous panniculitis-like T cell lymphoma:
- Mycosis fungoides, cytotoxic:
- Rare variant of mycosis fungoides
- Presents as other cases of MF, with generalized, scaly patches and plaques, ulcerated nodules
- Predilection for buttocks and sun protected areas
- Morphologically has epidermotropism and shows Pautrier microabscesses, as well as intraepidermal vesiculation
- Primary cutaneous peripheral T cell lymphoma, unspecified:
- Solitary or multiple ulcerating nodules
- Medium to large sized cells with moderate to marked pleomorphism
- Positive expression of T cell markers, including loss of antigens; may coexpress TIA1, granzyme B or perforin
- Aggressive clinical behavior
Board review style question #1
Which of the following statements is correct regarding primary cutaneous acral CD8+ lymphoproliferative disorder?
- Characterized by aggressive course with progressive disease and resistance to therapy
- Epidermotropism is usually absent
- Loss of expression of pan-T cell markers CD2, CD5 and CD7 is rarely observed
- Neoplastic cells feature a Ki67 proliferation index that ranges from 50 to 90%
- Restricted to the skin of the ear
Board review style answer #1
B. Epidermotropism is usually absent
Comment Here
Reference: Primary cutaneous acral CD8+ lymphoproliferative disorder
Comment Here
Reference: Primary cutaneous acral CD8+ lymphoproliferative disorder