Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Flow cytometry description | Molecular / cytogenetics description | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Crane GM. Plasmacytoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomaplasmacytoma.html. Accessed April 19th, 2024.
Definition / general
- Solitary lesion of clonal plasma cells that are cytologically, immunophenotypically and genetically similar to plasma cell myeloma
- Solitary plasmacytoma of bone: localized bone tumor consisting of monoclonal plasma cells with no other radiographic lesions and no evidence of other bone marrow involvement
- Extraosseous (extramedullary) plasmacytoma: localized tumor of plasma cells (not in bone)
Essential features
- Monoclonal plasma cells, no associated clonal B cell population, isolated lesion without evidence of additional bone marrow plasmacytosis
Terminology
- Solitary plasmacytoma of bone
- Extraosseous (extramedullary) plasmacytoma
ICD coding
Epidemiology
- Bone and extramedullary tumors each comprise 3 - 5% of plasma cell neoplasms
- Both are more common in men (65%), median age 55 years
Sites
- Extraosseous: 80% in upper respiratory tract (15% spread to cervical lymph nodes)
- Other: GI, lymph nodes (Am J Clin Pathol 2001;115:119), bladder, CNS, breast, thyroid, testis, parotid, skin
- Bone:
- Areas of active hematopoiesis
- In order of decreasing frequency: vertebrae, ribs, skull, pelvis, femur, clavicle, scapula, rare in distal long bones
Clinical features
Bone:
Extraosseous (clinical features depend on site):
- Most present with bone pain
- Vertebral lesions may cause cord compression
- Palpable mass due to soft tissue extension
- Up to 2/3 progress to myeloma or additional plasmacytomas; 1/3 remain disease free for > 10 years following local (radiation) control
- 5% may have multiple or recurrent plasmacytomas but no evidence of myeloma
Extraosseous (clinical features depend on site):
- Rhinorrhea, epistaxis, nasal obstruction
- Approximately 15% progress to myeloma, 70% are disease free at 10 years
- 25% have local recurrence, may spread to regional lymph nodes or metastasize to distant sites
Diagnosis
- Monoclonal plasma cells, less frequently plasmablastic or anaplastic morphology
- Histologic findings are combined with laboratory and radiographic findings (below) showing absence of additional disease
Laboratory
- M protein in serum or urine (absent or lower than in myeloma):
- Bone: approximately 50%, usually IgG
- Extraosseous: 20%, often small, IgA
- No CRAB (hypercalcemia, renal failure, anemia, additional bone lesions)
- Unlike myeloma, normal levels of uninvolved immunoglobulins
- Monitor free light chain to measure progression
Radiology description
- MRI may be preferred method to exclude additional bone lesions
- Solitary bone lesions are usually purely lytic with a narrow zone of transition to normal bone
- Abnormalities may persist after successful treatment
Prognostic factors
Bone - poor prognostic features (in some series):
- Older patients
- Plasmacytoma > 5 cm
- Persistence of M protein following radiotherapy
- Low polyclonal immunoglobulins (also raises concern for myeloma)
- Osteopenia
Case reports
- 52 year old man with plasmacytoma involving a lymph node that evolved to plasma cell myeloma (N Engl J Med 1950;243:335)
- 67 year old African American man with extramedullary plasmacytoma associated with amyloidoma (Arch Pathol Lab Med 2002;126:969)
Treatment
- Local radiation therapy
Microscopic (histologic) description
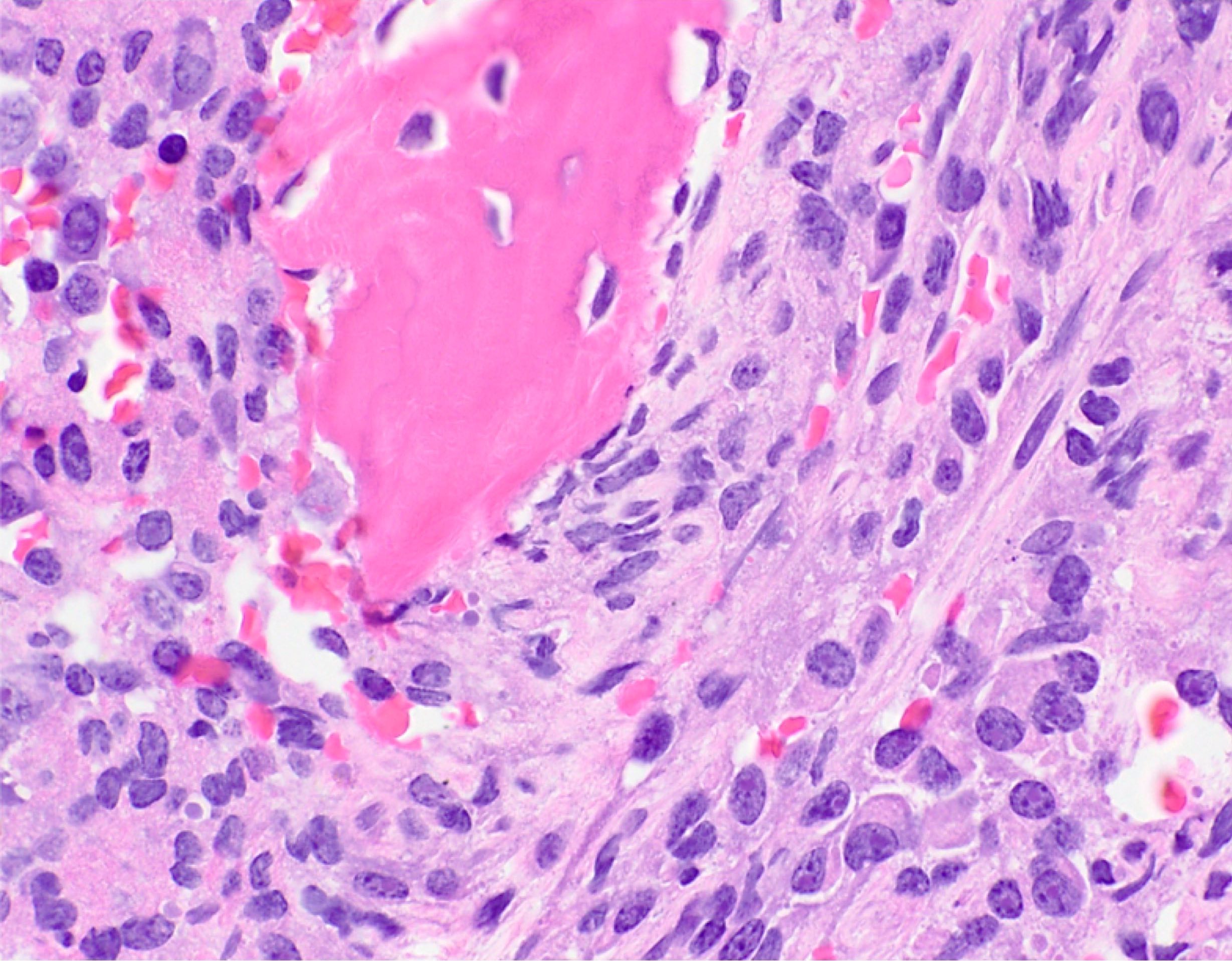
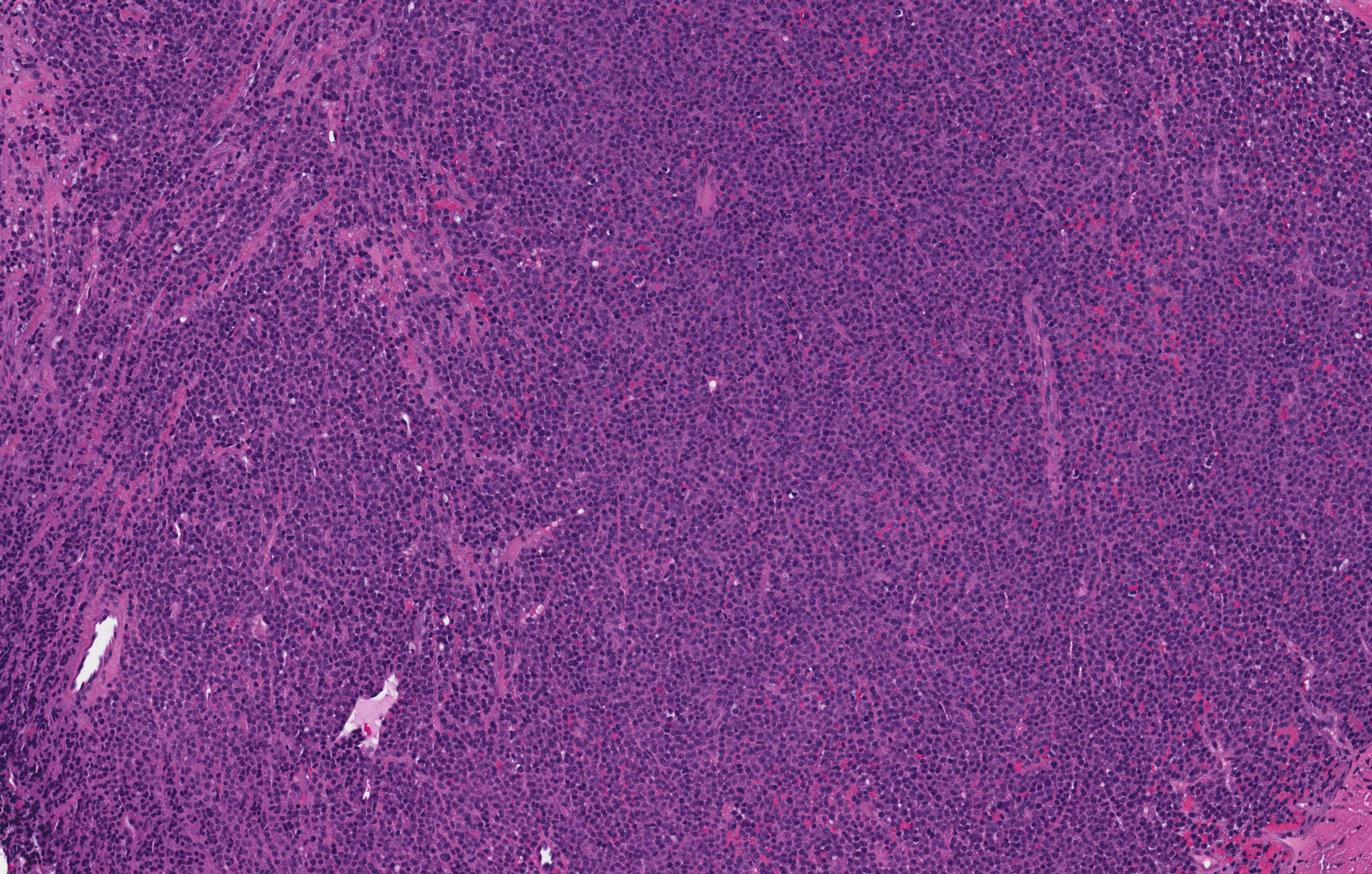
- Similar to myeloma, may contain mature, immature, plasmablastic or anaplastic plasma cells
- Amyloid deposits may appear in extraosseous tumors as pink amorphous material with scattered multinucleated giant cells
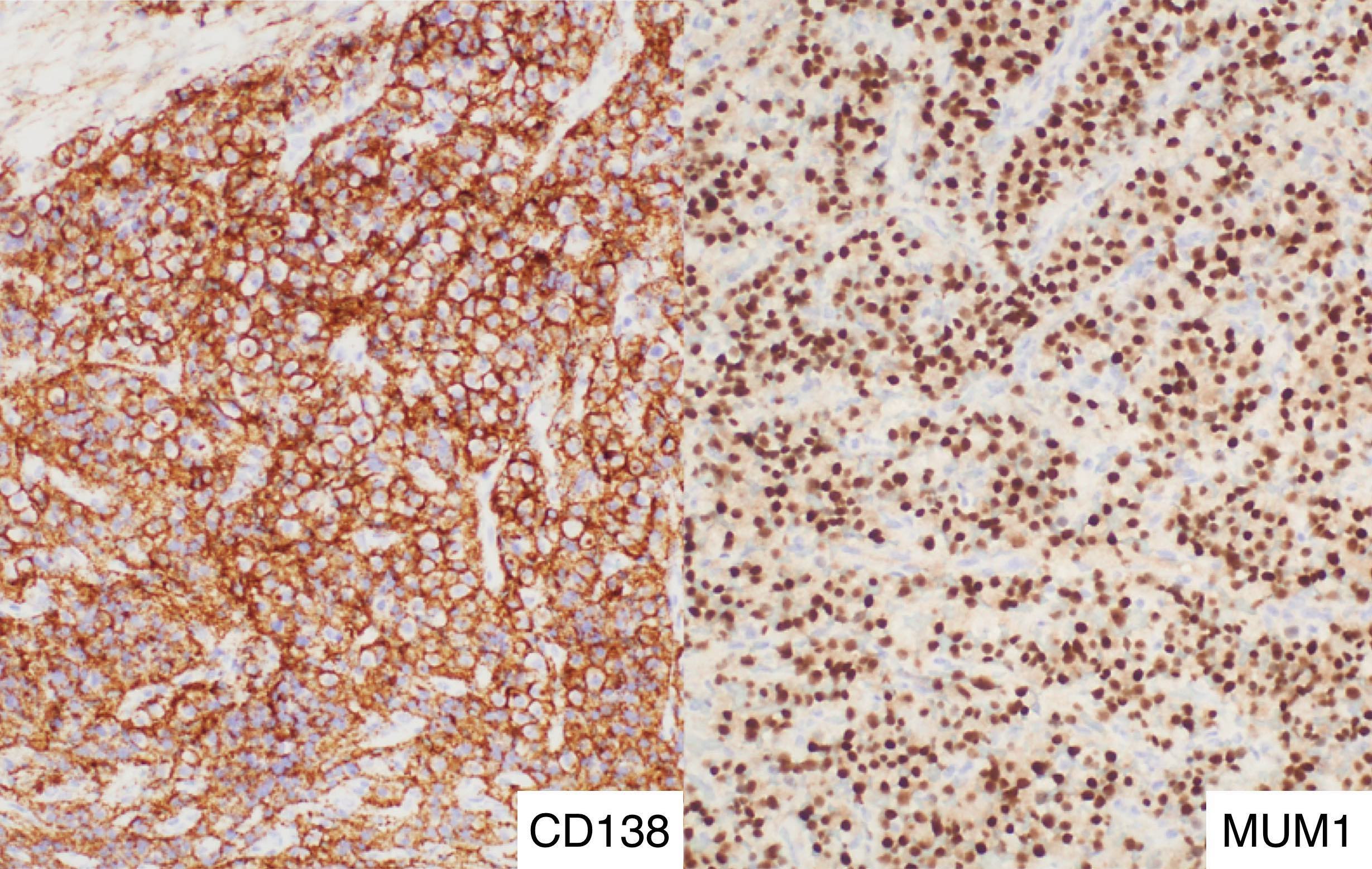
Microscopic (histologic) images
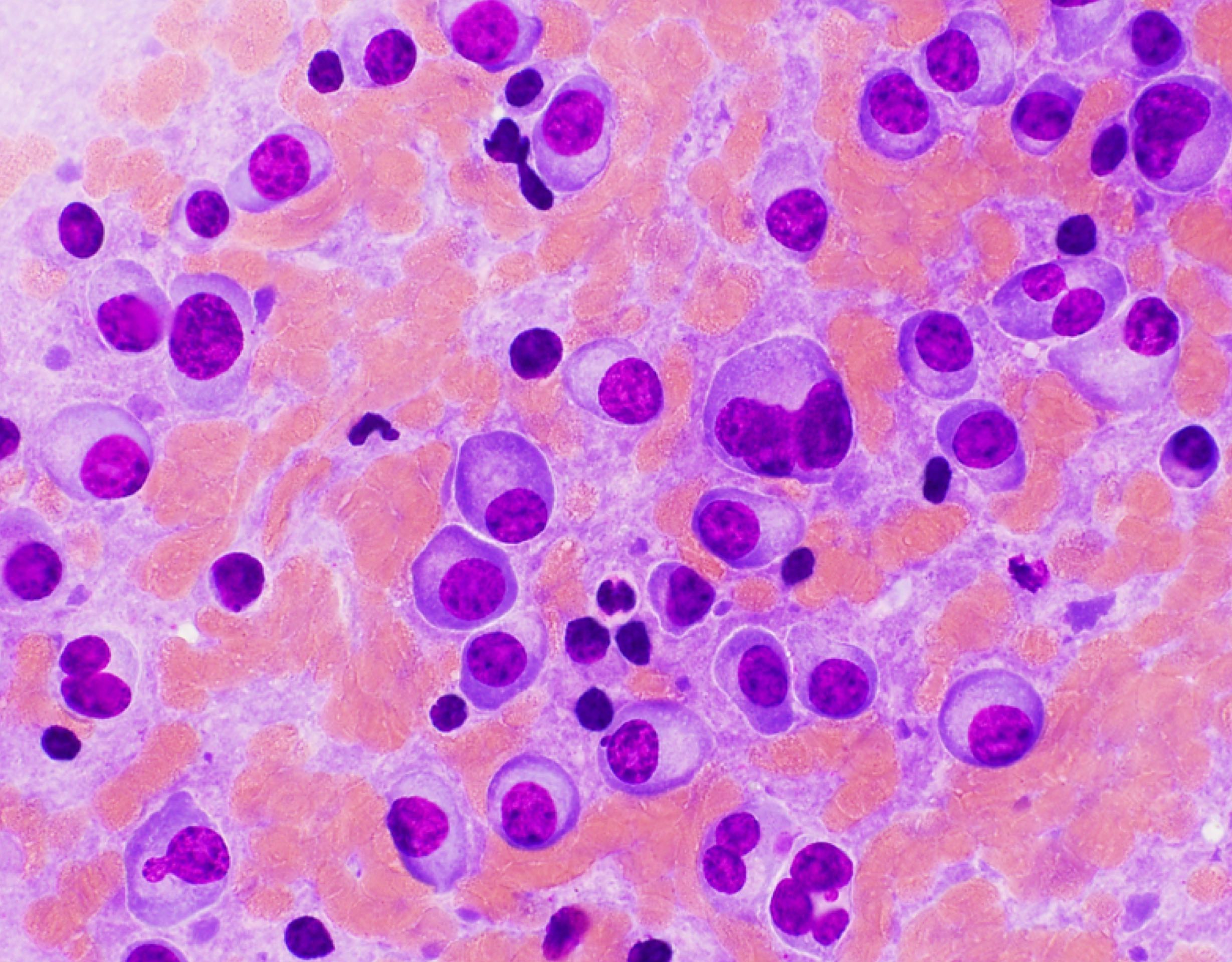
Cytology description
- Similar to myeloma
- Mature plasma cells: oval with abundant basophilic cytoplasm, perinuclear hof, round eccentric nuclei, "clock face" chromatin and indiscernible nucleoli
- Immature plasma cells: higher nuclear / cytoplasmic ratio, more abundant cytoplasm and hof region compared to plasmablastic, more dispersed chromatin, often prominent nucleoli
- Plasmablastic: less abundant cytoplasm with little or no hof region, fine reticular chromatin, large nucleus ( > 10 microns) or large nucleolus ( > 2 microns) (Blood 1998;91:2501)
- Pleomorphic: multinucleated, polylobated
- Rare cases may have small, lymphoid appearing plasma cells or plasma cells with marked nuclear lobation
- Morphologic features:
- Mott cells / morula cells: multiple grape-like cytoplasmic inclusions comprised of crystalized Ig
- Russell bodies: hyaline intracytoplasmic and intranuclear inclusions
- Flame cells: vermillion staining glycogen rich IgA in cytoplasmic projections
- Gaucher-like cells / thesaurocytes: overstuffed fibrils
- Cytoplasmic crystals: occasional in myeloma, common in adult Fanconi syndrome
- Dutcher bodies: pale staining nuclear inclusions, single and usually large, more common in IgA myeloma
Flow cytometry description
- Similar to plasma cell myeloma
Molecular / cytogenetics description
- In bone, genetics similar to plasma cell myeloma, extraosseous not extensively studied
Differential diagnosis
- Cutaneous or GI plasmacytoma:
- Particularly difficult to differentiate from marginal zone lymphoma, may not be possible
- Large cell lymphoma:
- With immunoblastic or plasmablastic features
- Marginal zone lymphoma, lymphoplasmacytic lymphoma:
- May have plasmacytoid features but more extensive sampling may reveal B cell component
- CD20 expression by lymphocytes or plasmacytoid cells
- Clonal B cell population by flow; molecular or cytogenetic features of marginal zone or lymphoplasmacytic lymphoma
- Plasma cell myeloma:
- Must be excluded by radiographs, bone marrow biopsy
- Radiographically, may mimic metastatic tumor, Langerhans cell histiocytosis
- Reactive plasma cell infiltrate:
Additional references
Board review style question #1
What is the best way to distinguish plasma cell myeloma from solitary plasmacytoma?
- CD19 expression
- Cytogenetics demonstrating a t(11;14) translocation
- Plasmablastic features
- Radiographs
Board review style answer #1
Board review style question #2
When considering the diagnosis of a solitary plasmactyoma in a cervical lymph node, which factor(s) are most important to consider?
- Lymph node involvement by myeloma
- Nodal marginal zone lymphoma with extensive plasmacytic differentiation
- Potential spread from the upper respiratory tract
- All of the above
Board review style answer #2