Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: McLean-Holden AC, Magliocca K. Ameloblastoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/mandiblemaxillaameloblastoma.html. Accessed April 26th, 2024.
Definition / general
- Odontogenic epithelial neoplasm characterized by slow, expansile growth
- Classified as a benign neoplasm; ameloblastoma behaves in a locally aggressive manner with a tendency to recur
Essential features
- Slow growing, locally aggressive odontogenic epithelial neoplasm
- Most commonly occurs in mandible
- Multiple microscopic variants
- Treatment most often involves loss of bone and teeth
Terminology
- Adamantinoma (previous name): proposed early on by Malassez in 1885; subsequently abandoned as the term largely implies formation of hard tissues, which would be unexpected in ameloblastoma
- Ameloblastoma, conventional: name changed from solid / multicystic ameloblastoma to conventional ameloblastoma in WHO 2017, 4th edition, to avoid confusion with unicystic ameloblastoma
- Cystic ameloblastoma: conventional ameloblastoma with macrocystic change variably referred to as cystic ameloblastoma in the past; term is discouraged as it may be confused with unicystic ameloblastoma
- Desmoplastic ameloblastoma: previously classified as a separate and distinct subtype of ameloblastoma in WHO 2005, 3rd edition; no longer classified as distinct, now considered a microscopic variant of conventional ameloblastoma within WHO 2017, 4th edition
- Metastasizing ameloblastoma: previously classified as metastasizing (malignant) ameloblastoma, a malignant odontogenic tumor in WHO 2005, 3rd edition; removed from classification of malignant odontogenic tumors and reclassified in the spectrum of benign odontogenic tumors in WHO 2017, 4th edition
ICD coding
Epidemiology
- Represents 1% of all jaw cysts and tumors
- Most common odontogenic neoplasm
- Incidence: 0.5 cases per million population
- No sex predilection
- Majority of ameloblastomas are conventional type, followed by unicystic, peripheral
- Broad age range, narrowed somewhat by tumor type:
- Ameloblastoma, conventional type: peak incidence in fourth to fifth decades of life
- Ameloblastoma, unicystic type: peak incidence in second to third decades of life
- Ameloblastoma, extraosseous / peripheral type: peak incidence in fifth to seventh decades of life
Sites
- Intraosseous gnathic ameloblastoma (conventional and unicystic)
- ~80% cases occur in mandible
- ~20% cases occur in maxilla
- Desmoplastic ameloblastoma has predilection for anterior jaws, especially anterior maxilla
- Ameloblastoma, extraosseous / peripheral type (Head Neck Pathol 2010;4:192)
- Found in soft tissue of posterior gingiva and retromolar area
- Predilection for lingual side of mandible
- Other head and neck sites reported (all very rare):
- Sinonasal tract (Cancer 1998;82:667)
- Middle ear (J Int Adv Otol 2019;15:173)
- Temporal bone (J Oral Maxillofac Surg 2017;75:1300.e1)
- Infratemporal fossa; most commonly occurs in this location in the form of recurrent disease (Dentomaxillofac Radiol 2007;36:416)
Etiology
- Intraosseous gnathic ameloblastoma originates from:
- Remnants of the enamel organ or dental lamina
- Reported to rarely arise within odontogenic cyst
- Ameloblastoma, extraosseous / peripheral type: arises from rests of Serres (dental lamina remnants in gingiva)
Clinical features
- Ameloblastoma, conventional:
- Most commonly grossly solid / multicystic, expansile, locally aggressive, requiring resection with uninvolved margins
- May show macrocystic change grossly
- Microscopic variants include follicular, plexiform, basal, acanthomatous, granular and desmoplastic
- Usually asymptomatic; may be found incidentally on radiographic exam
- When symptoms present, they are usually limited or nonspecific
- Slow growing, painless expansion of the involved jaw
- Increased size often related to more clinically significant symptoms
- Malocclusion
- Loose teeth
- Pain possible if infected or hemorrhaging into tissues
- Very large tumors may cause facial deformity, restrict mouth opening and eventually lead to airway obstruction
- Ameloblastoma, unicystic type:
- Occurs as single cystic cavity with or without intramural growth
- Microscopic variants include luminal, intraluminal and mural; luminal and intraluminal considered a less aggressive variant of ameloblastoma, amenable to more conservative treatment
- Natural history and treatment of mural unicystic ameloblastoma remains controversial
- Usually asymptomatic; may be found incidentally on radiographic exam
- When symptoms present, they are usually limited or nonspecific
- Slow growing, painless expansion of the involved jaw
- Increased size often related to more clinically significant symptoms
- Malocclusion
- Loose teeth
- Pain possible if infected or hemorrhaging into tissues
- Very large tumors may cause facial deformity, restrict mouth opening and eventually lead to airway obstruction
- Possible rare association with nevoid basal cell carcinoma (Gorlin) syndrome, among other inherited conditions (Fam Cancer 2012;11:411, J Stomatol Oral Maxillofac Surg 2020;121:146)
- Ameloblastoma, extraosseous / peripheral type:
- Most commonly occurs within gingiva
- Peripheral ameloblastoma accounts for 1% of ameloblastoma cases and is amenable to conservative surgical treatment and show low recurrence rates (J Oral Maxillofac Pathol 2018;22:396)
- Usually asymptomatic
- Found in soft tissue of posterior gingiva and retromolar area
- Predilection for lingual side of mandible
- Gingival lesions showing radiographic cupping of bone may represent a peripherally placed intraosseous ameloblastoma that has perforated cortical bone (Head Neck Pathol 2010;4:192)
- Cross sectional imaging essential to exclude small intraosseous ameloblastoma with a prominent extraosseous component
- Metastasizing ameloblastoma:
- Rare
- Usually metastasizes to lymph nodes or lung, other sites possible with organ associated symptoms
- Associated with longstanding tumors, multiple surgical procedures, radiation therapy
Diagnosis
- Based on clinical, radiologic and pathologic correlation
- Ameloblastoma, extraosseous / peripheral type: requires exclusion of an intraosseous tumor with extraosseous extension mimicking a gingival lesion (Head Neck Pathol 2010;4:192)
- Metastasizing ameloblastoma can only be diagnosed retrospectively
- Ameloblastoma reported very rarely to occur in nongnathic sites (sinonasal, ear / temporal bone) and diagnosed only after:
- Sinonasal: requires exclusion of tumor extension into sinonasal tract from a maxillary alveolar bone location
- Ear / temporal bone: requires exclusion of competing differential diagnoses such as:
- Nonkeratinizing carcinoma (Am J Surg Pathol 2020;44:1244)
- Primary basal cell carcinoma of middle ear (J Int Adv Otol 2020;16:291)
Laboratory
- Hypercalcemia, rarely documented and is thought to be related to 1 or both of the following mechanisms:
- Increased parathyroid hormone related peptide (PTHrP)
- Osteolytic hypercalcemia: tumor invades bone and in combination with local inflammatory response, results in excessive calcium release from bone
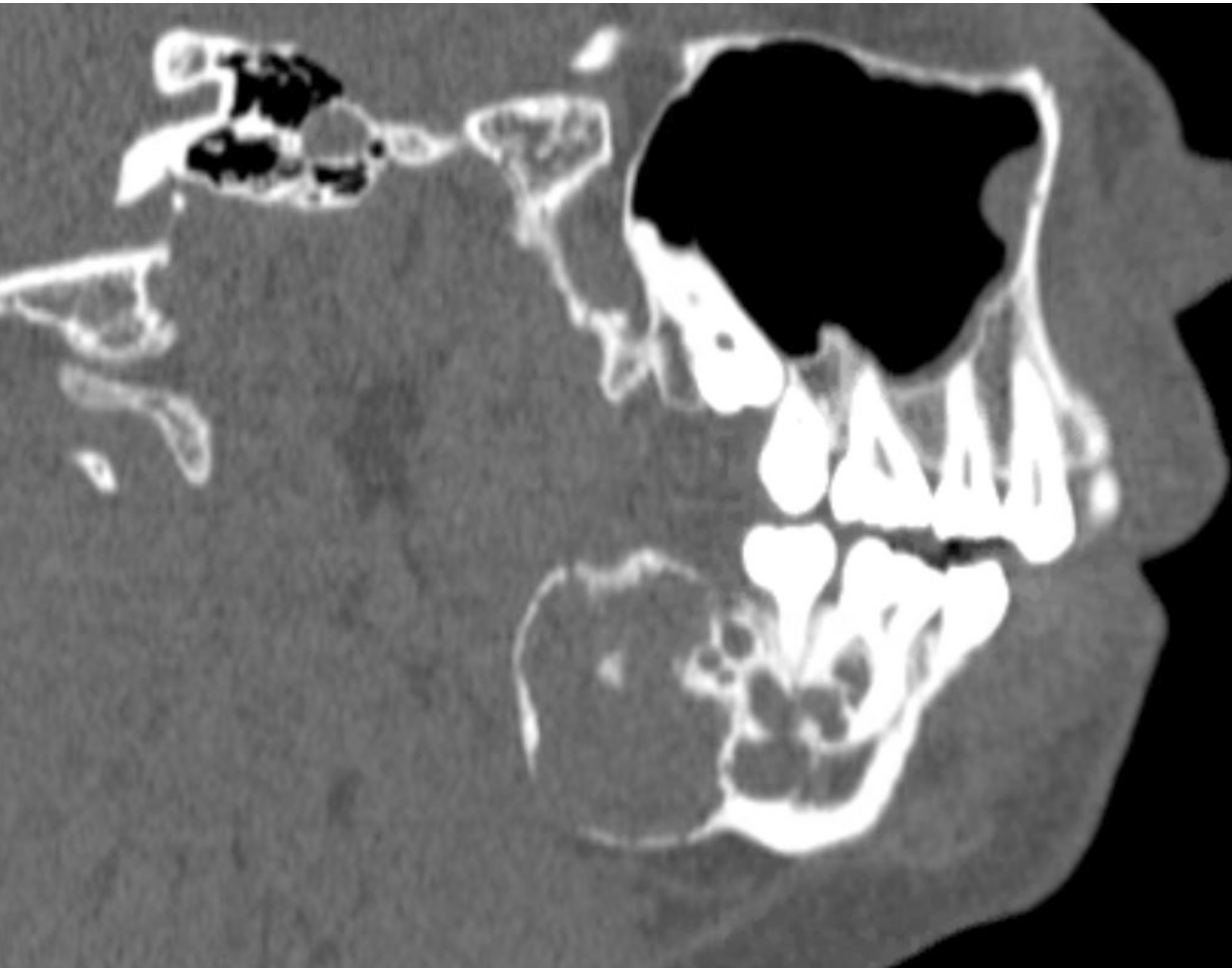
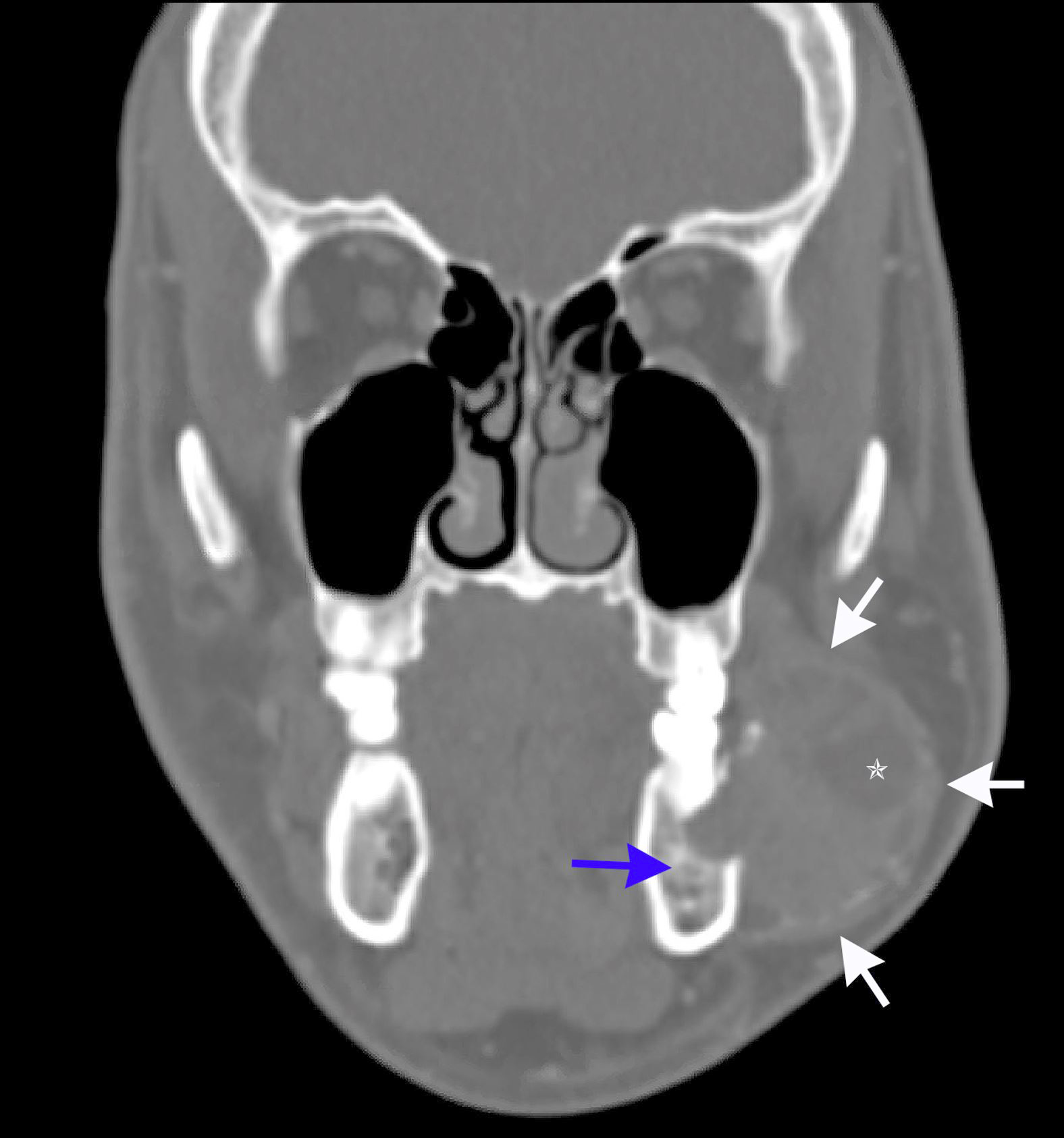
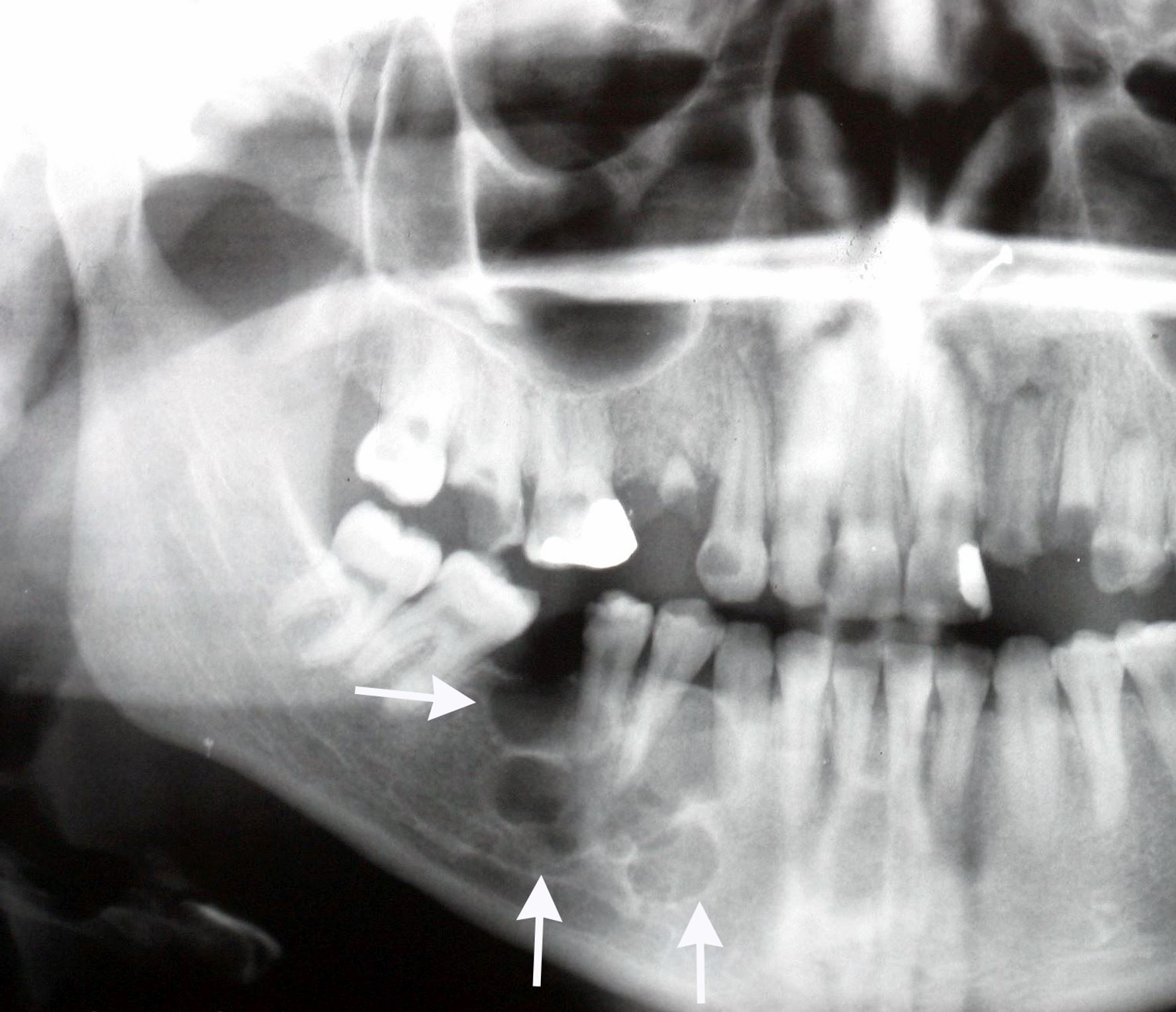
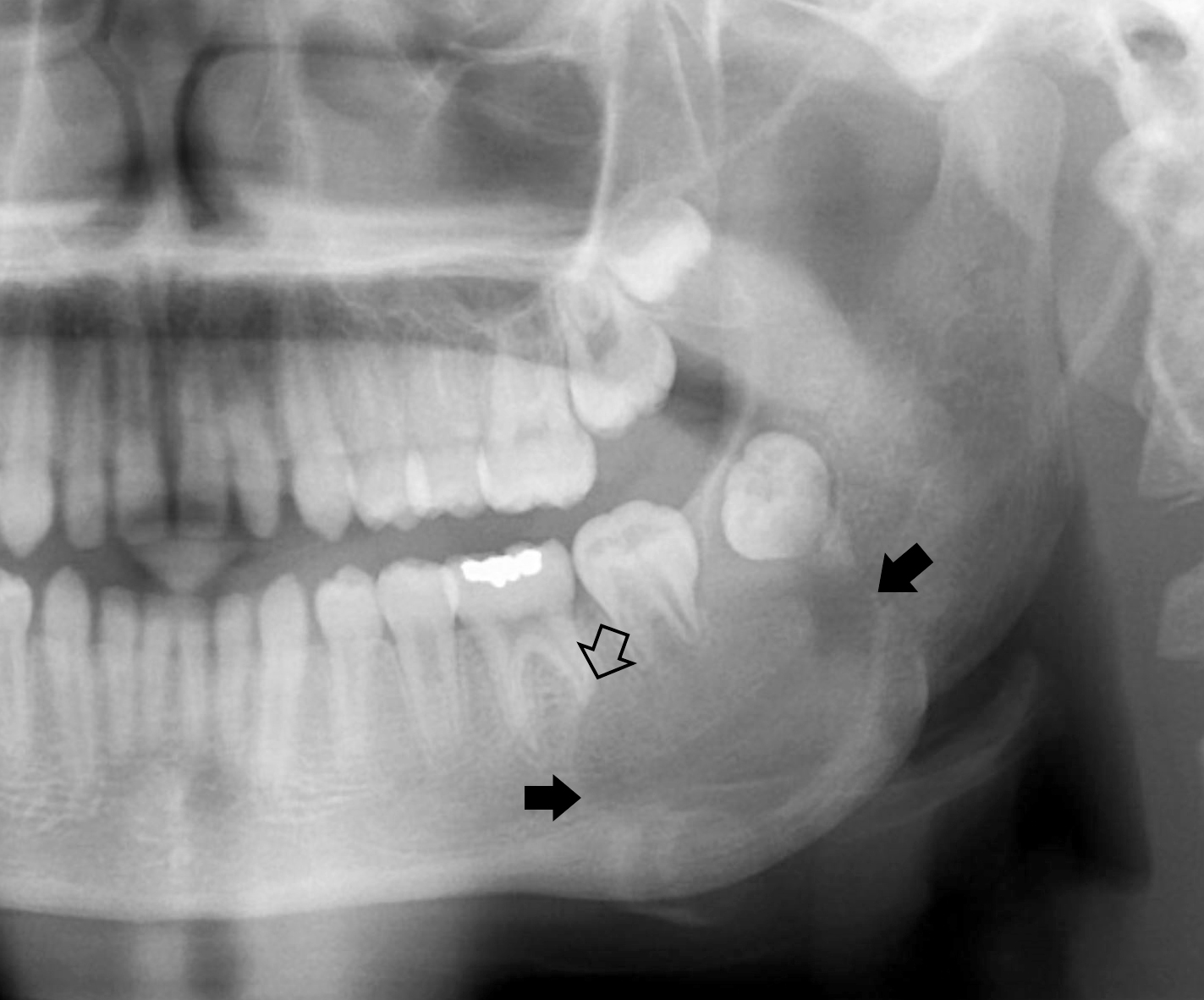
Radiology description
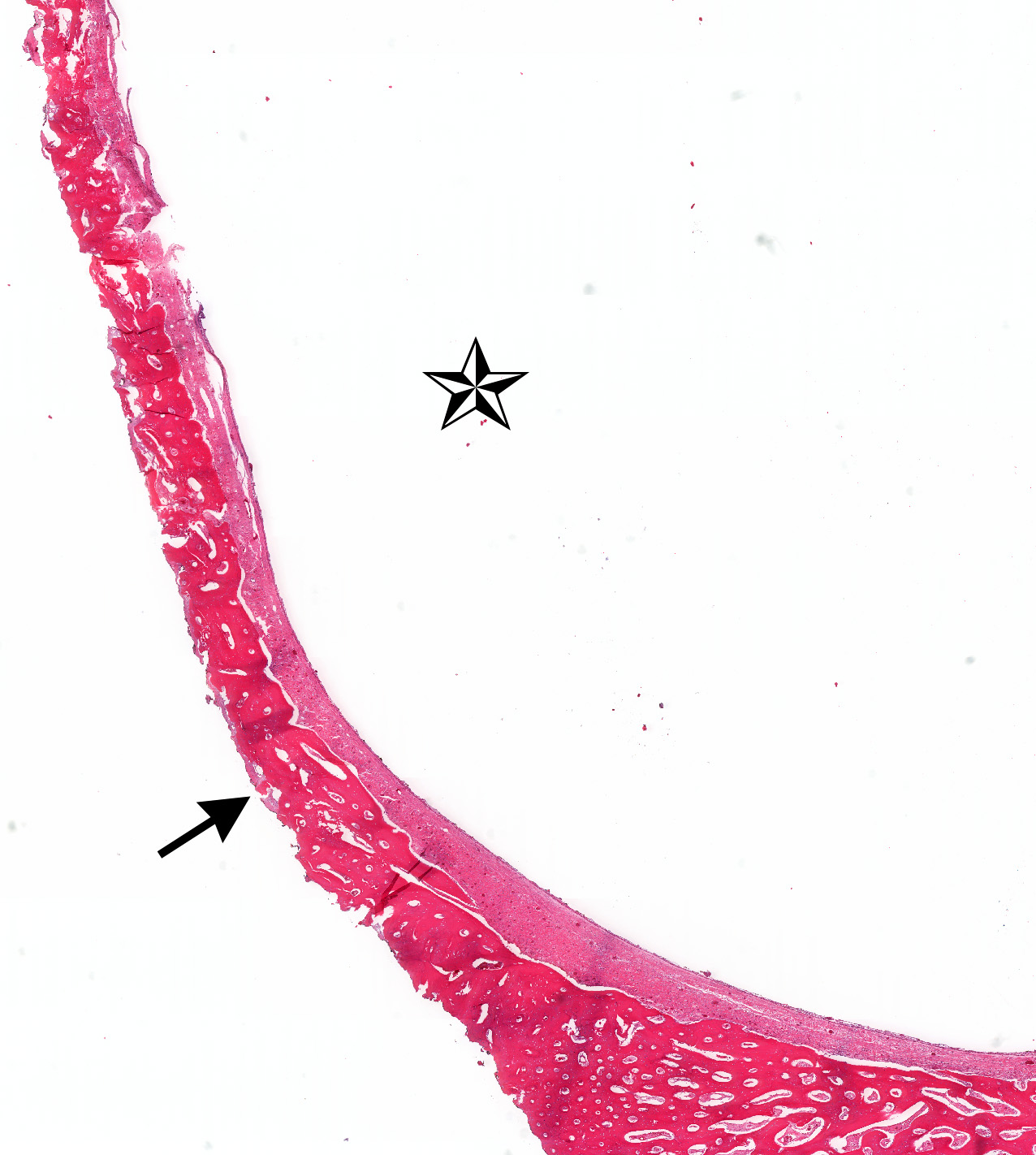
- Ameloblastoma, conventional
- Expansile multilocular radiolucency, well defined, corticated border
- Some cases exhibit classic soap bubble appearance
- May or may not be associated with impacted tooth / teeth
- Resorption or displacement of tooth roots
- Reactive bone formation may occur, most commonly in desmoplastic ameloblastoma, which may resemble a fibro-osseous lesion radiographically due to the presence of osteoplasia
- May have a unicystic radiographic appearance on plain images; requires microscopic examination for distinction from ameloblastoma, unicystic type (Dentomaxillofac Radiol 2018;47:20170288)
- Ameloblastoma, unicystic type
- Unilocular radiolucency, well defined, corticated border
- Often associated with an impacted tooth, specifically mandibular third molar
- Root resorption may occur
- Cortical perforation in 33% of cases
- Ameloblastoma, extraosseous / peripheral type
- Radiographic cupping of bone described but may represent a peripherally placed intraosseous ameloblastoma that has expanded and subsequently perforated through cortical bone to mimic a peripheral gingival based lesion; requires close clinicoradiographic correlation
- Cross sectional imaging needed to exclude intraosseous ameloblastoma with a prominent extraosseous component
Radiology images
Prognostic factors
- Ameloblastoma, conventional type (Oral Dis 2019;25:1683)
- Surgery type:
- Curettage associated with high recurrence rate (60 - 80%)
- Marginal or segmental resection in mandible with planned 1 cm margins reduces rate of recurrence
- Histologic type: histologic type does not affect prognosis
- Tumor anatomic location: maxilla, higher recurrence rate
- BRAF tumor status:
- Some studies note that ameloblastoma lacking BRAF V600E mutations associated with an increased rate of local recurrence (P = 0.0003)
- Surgery type:
- Ameloblastoma, unicystic type
- Treatment and recurrence depend on pattern and extent of tumor proliferation
- When mural involvement is present, the tumor may behave like conventional ameloblastoma; clarification needed
- Overall recurrence rate of 5 - 10%
- Ameloblastoma, extraosseous / peripheral type
- If tumor represents a peripherally placed intraosseous ameloblastoma that has perforated cortical bone and mimics a gingival based lesion, then tumor will recur if intraosseous component not removed (Head Neck Pathol 2010;4:192)
Case reports
- 14 year old boy with Gardner syndrome has unusual case of a unicystic ameloblastoma mimicking a dentigerous cyst (Dentomaxillofac Radiol 2018;47:20170288)
- 15 year old girl with mandibular unicystic ameloblastoma presenting in Gardner syndrome (Head Neck Pathol 2014;8:239)
- 20 year old woman with large mandibular ameloblastoma and hypercalcemia (BMJ Case Rep 2014;2014:bcr2014205491)
- 52 year old man with multiply recurrent ameloblastoma and delayed pulmonary metastases (Respirology 2009;14:1208)
- 72 year old woman with large mandibular ameloblastoma and hypercalcemia (Consultant 2018;58:124 )
Treatment
- Ameloblastoma, conventional type:
- Mandible: usually treated with a segmental resection (marginal if small), which includes at least 1 cm bone margins and at least 1 adjacent uninvolved anatomic barrier
- Maxilla: resected en bloc via various midface approaches, at least 1 cm margins and at least 1 adjacent uninvolved anatomic barrier
- Curettage associated with high recurrence rate (60 - 80%)
- Nonsurgical therapy: although BRAF inhibitors have been used, no advantage over traditional surgical treatment for a previously untreated, intraosseous gnathic ameloblastoma has been documented
- Ameloblastoma, unicystic type: enucleation or resection
- Ameloblastoma, extraosseous / peripheral type: conservative excision
- Metastasizing ameloblastoma: extremely rare and there is currently no established treatment protocol; to be distinguished from ameloblastic carcinoma, an overtly malignant odontogenic neoplasm
- Longterm follow up is recommended for all types of ameloblastoma due to the potential for delayed presentation of recurrent disease; recurrent ameloblastoma may be difficult to treat (Oral Dis 2019;25:1683)
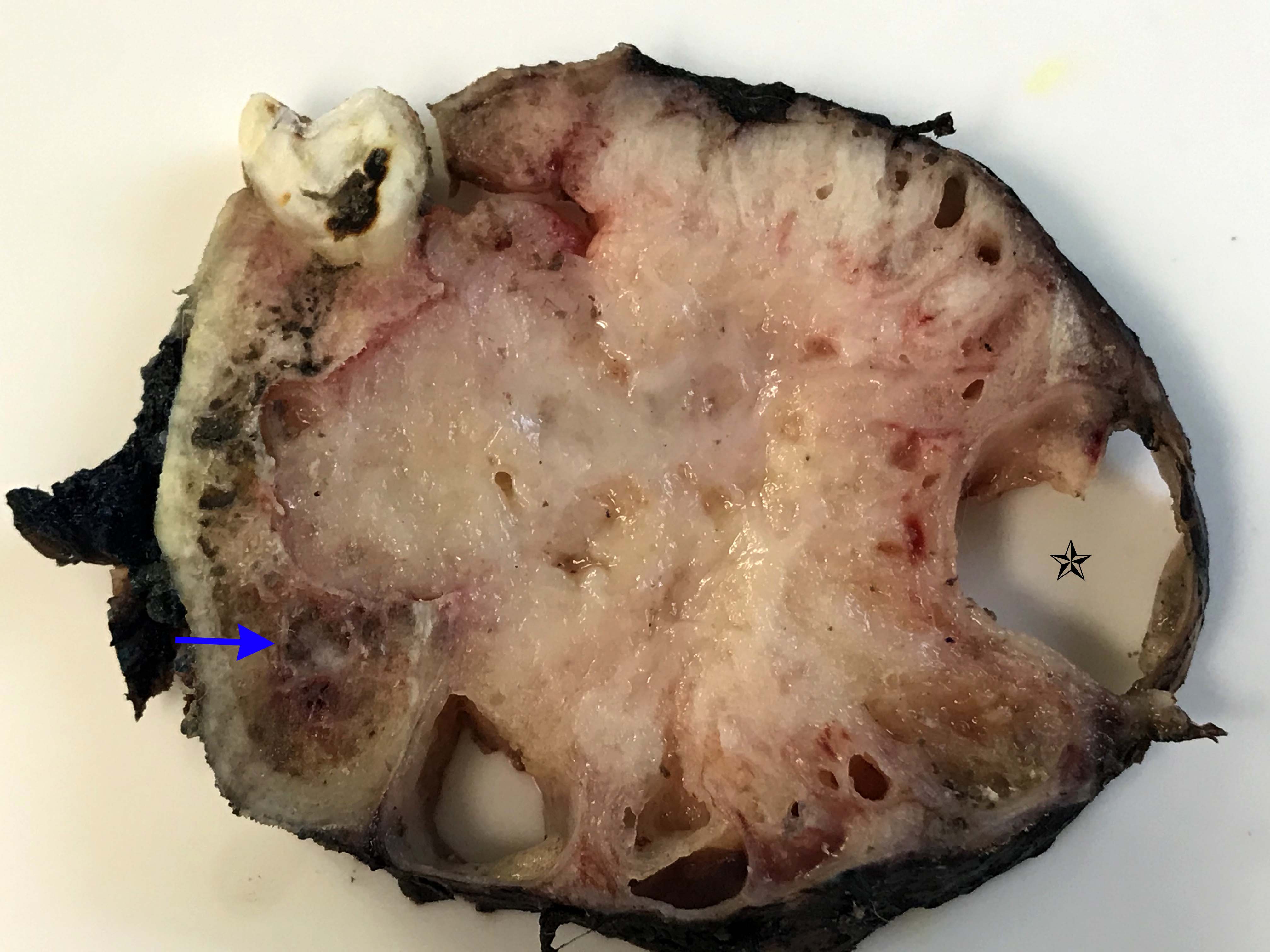
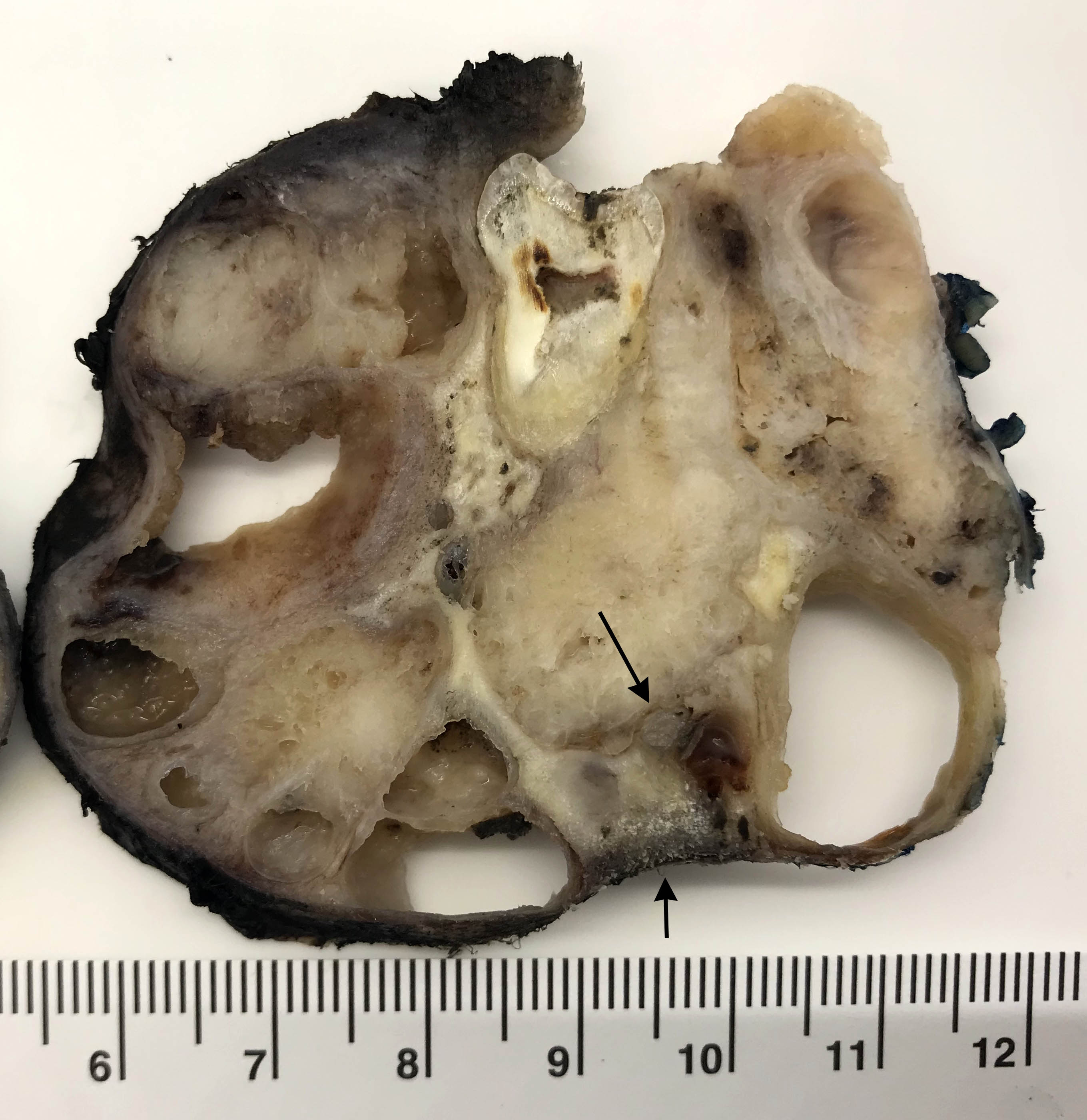
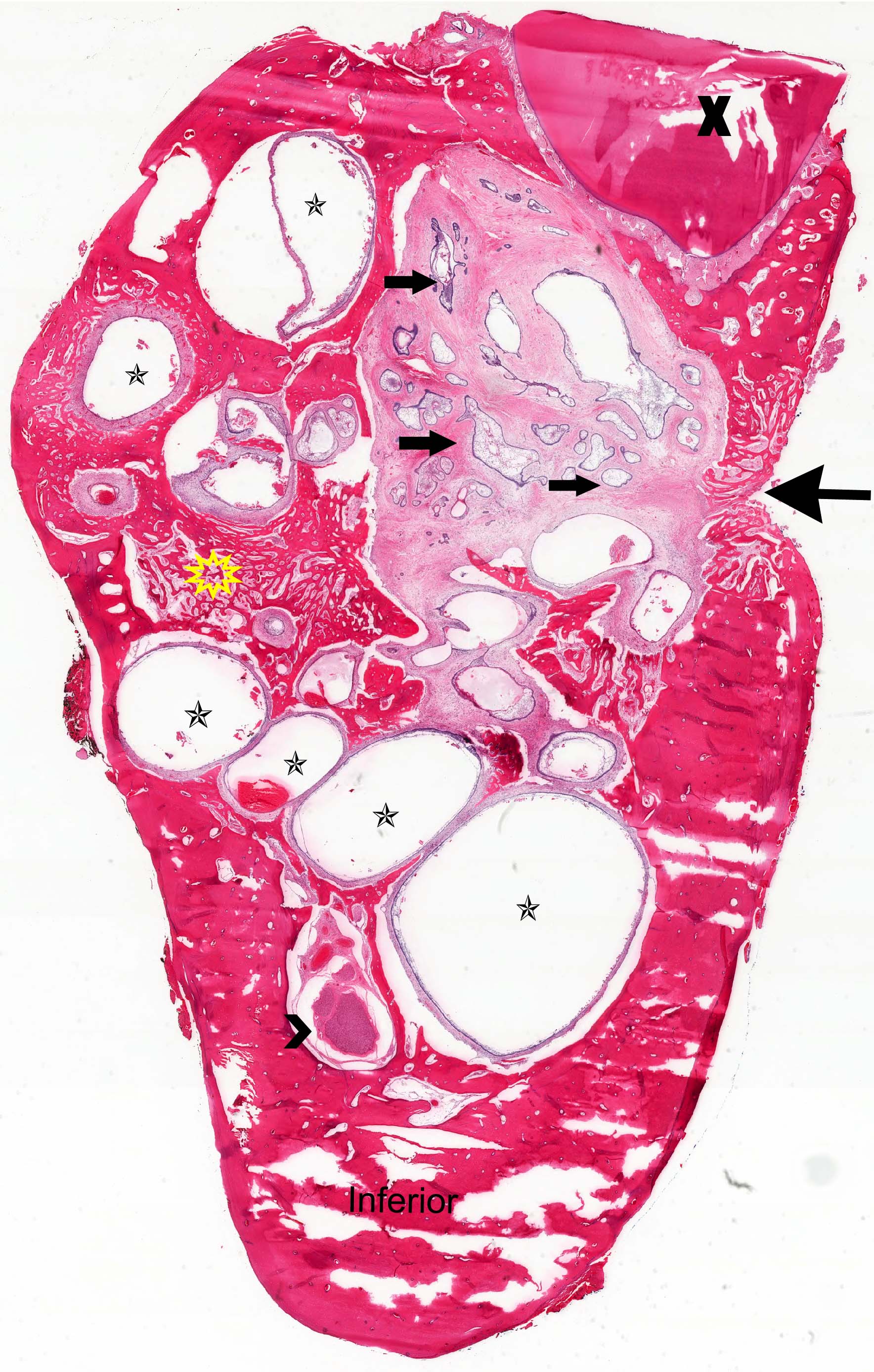
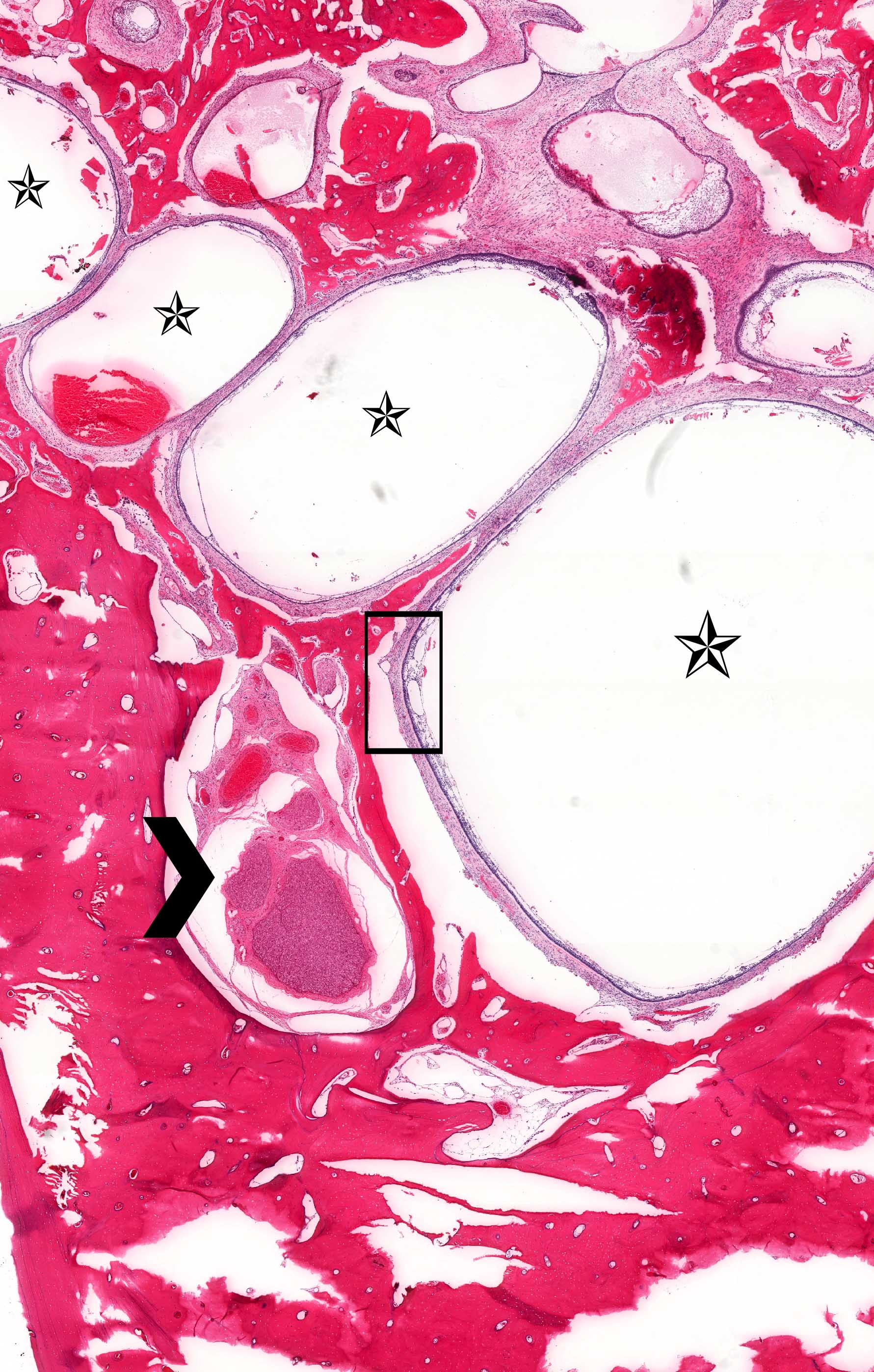
Gross description
- General grossing tips for intraosseous ameloblastoma:
- Prior to sectioning bone, review preoperative radiograph to evaluate for presence and location of any pre-existing metal hardware, titanium dental implants or impacted teeth that could interfere with bone sectioning, could increase difficulty with bone sectioning and be potentially hazardous if unexpectedly encountered
- If possible, recommend submitting at least 1 block as nondecalcified tumor specimen for immunohistochemistry or molecular studies
- Grossly exposed tumor or tumor fragmentation should be documented
- Shaving bone margins for odontogenic neoplasms discouraged:
- Difficulty in measuring extent of tumor from bone margins
- Incidental histologic findings can confound bone margin assessment (Int J Surg Pathol 2020;28:507)
- Ameloblastoma, conventional type:
- Viscous mucoid fluid present on cut surface
- Macrocystic degeneration: larger cystic spaces, may contain clear or red-brown fluid
- Solid, multiple cystic spaces or a combination thereof
- Resorbs tooth roots
- Note expansion or extension beyond bone
- May be associated with impacted tooth
- In mandible, note relation to inferior alveolar nerve if applicable
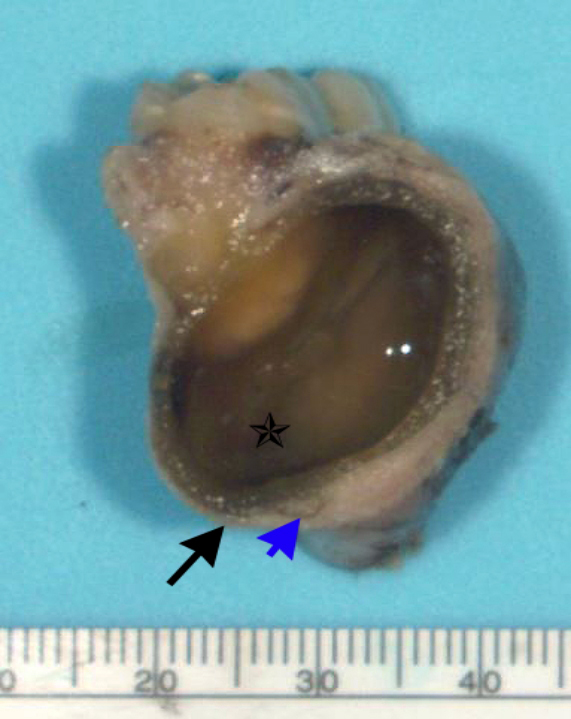
- Ameloblastoma, unicystic type:
- If surgically removed by enucleation, very little bone may present
- Evaluation of margins precluded by enucleation or curettage type of treatment
- When resected for margins with surrounding bone, unicystic gross appearance is conspicuous and may contain red-brown fluid
- If no mural growth identified on representative sections, consider submitting entire lesion
Gross images
Frozen section description
- Architectural organization preserved
- Subnuclear vacuolization difficult to appreciate
Frozen section images
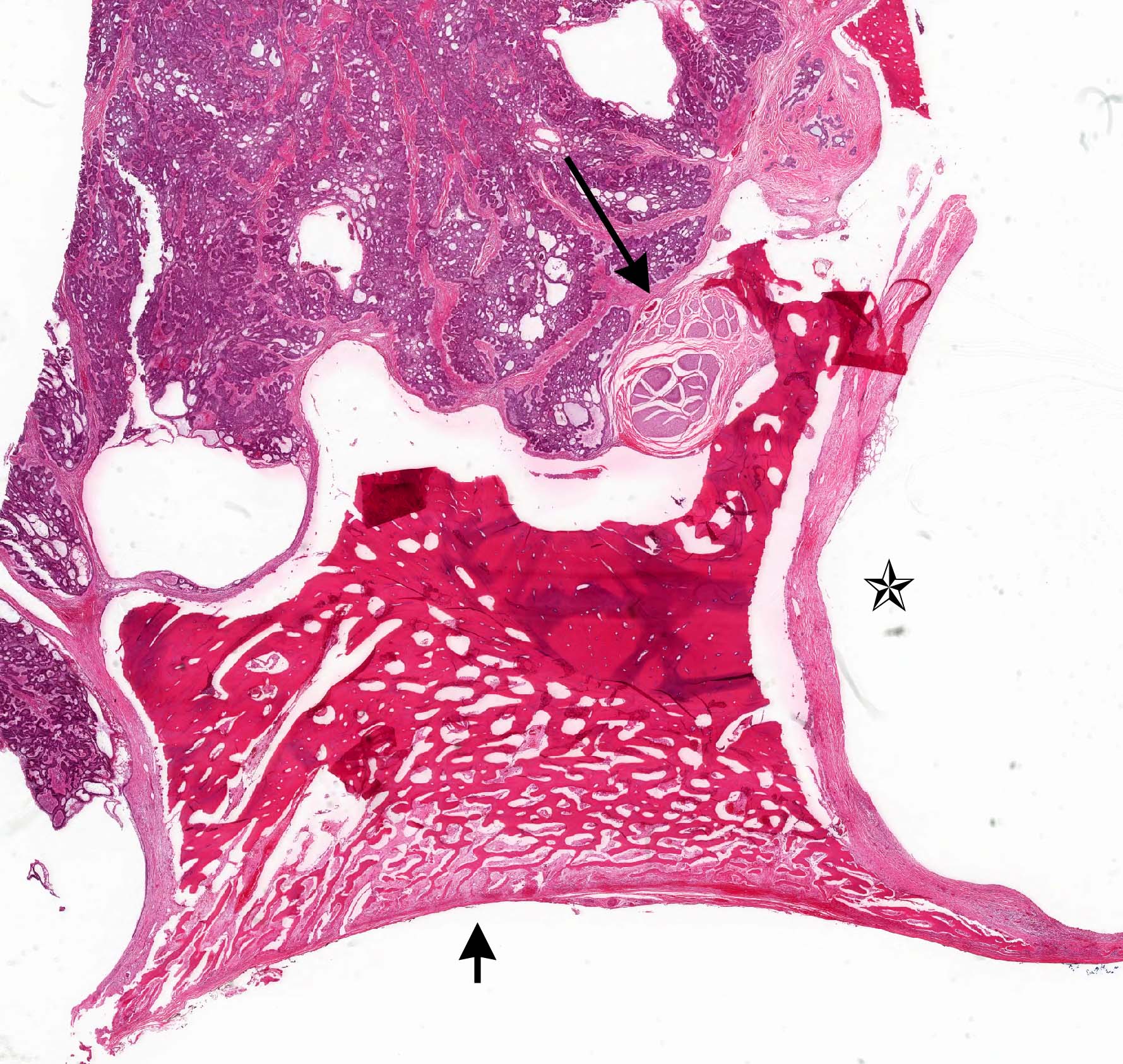
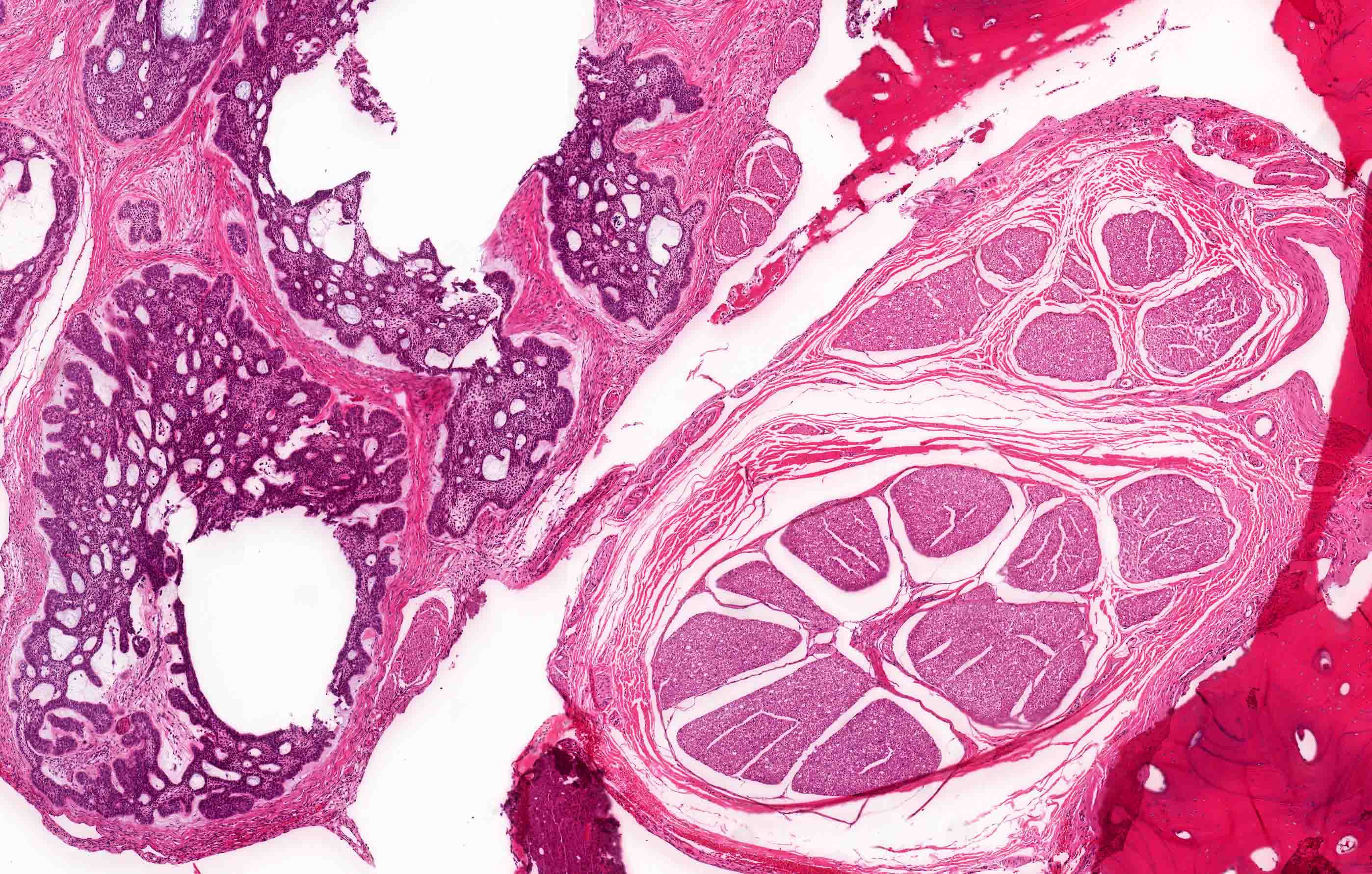
Microscopic (histologic) description
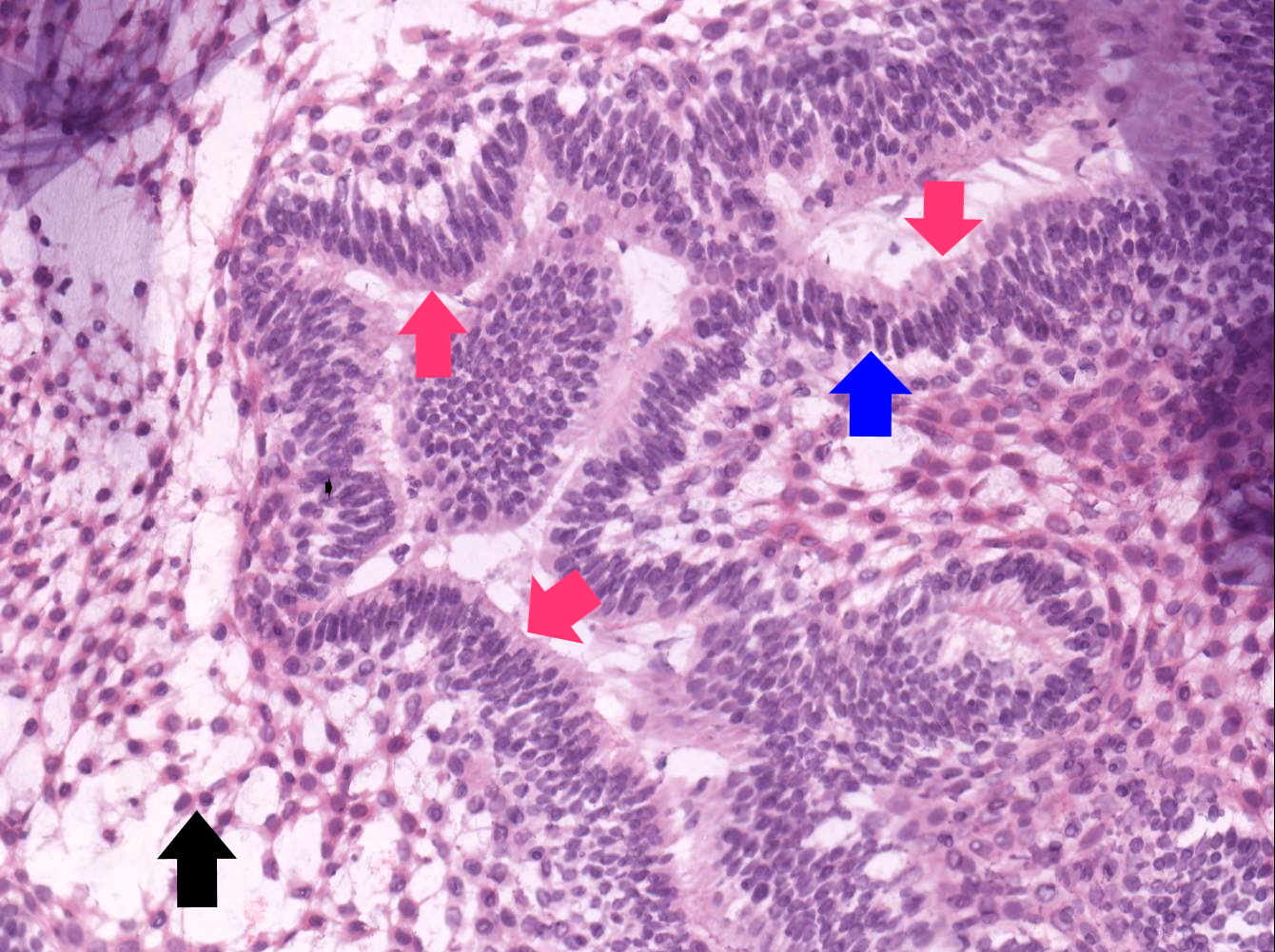
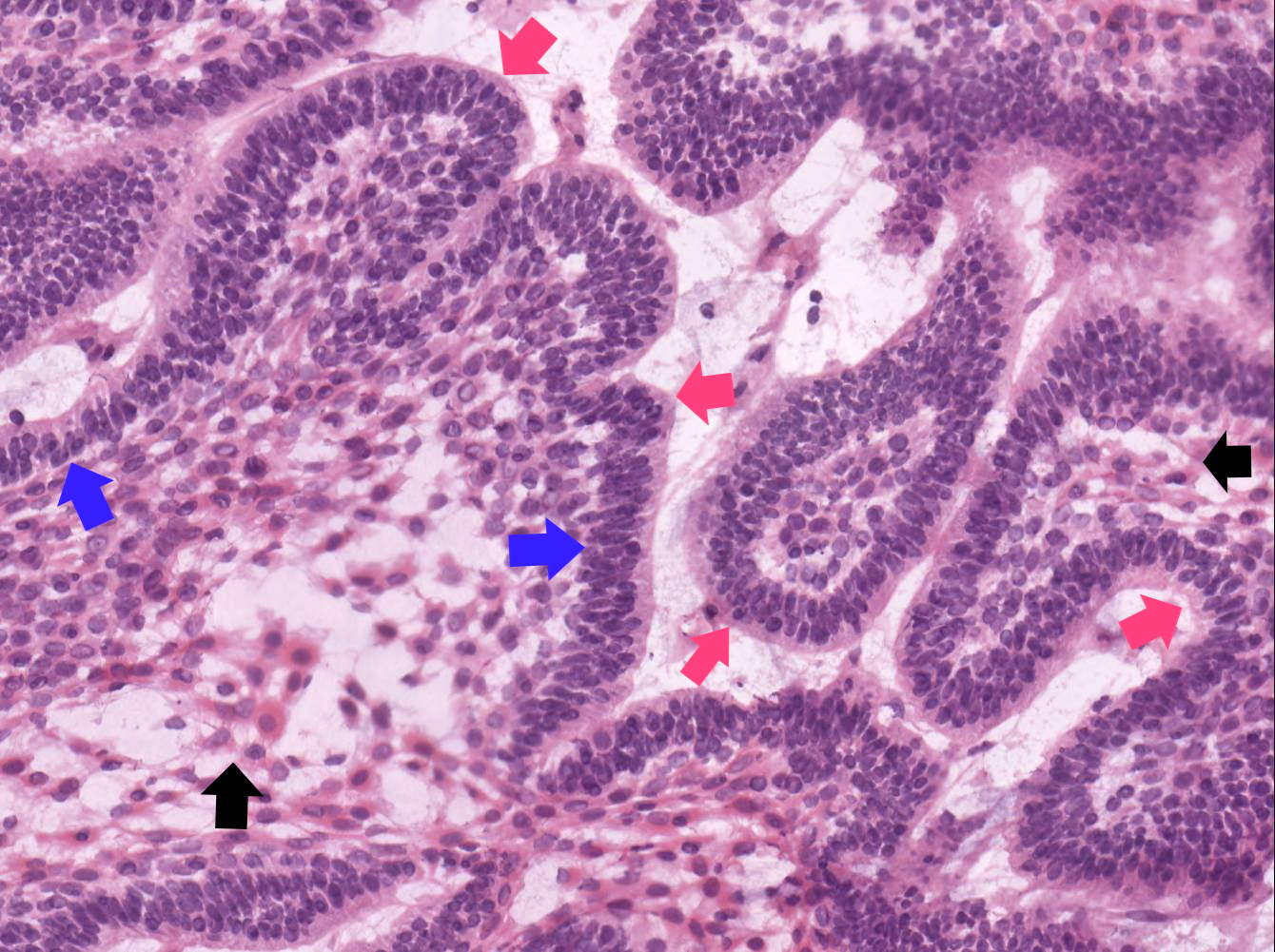
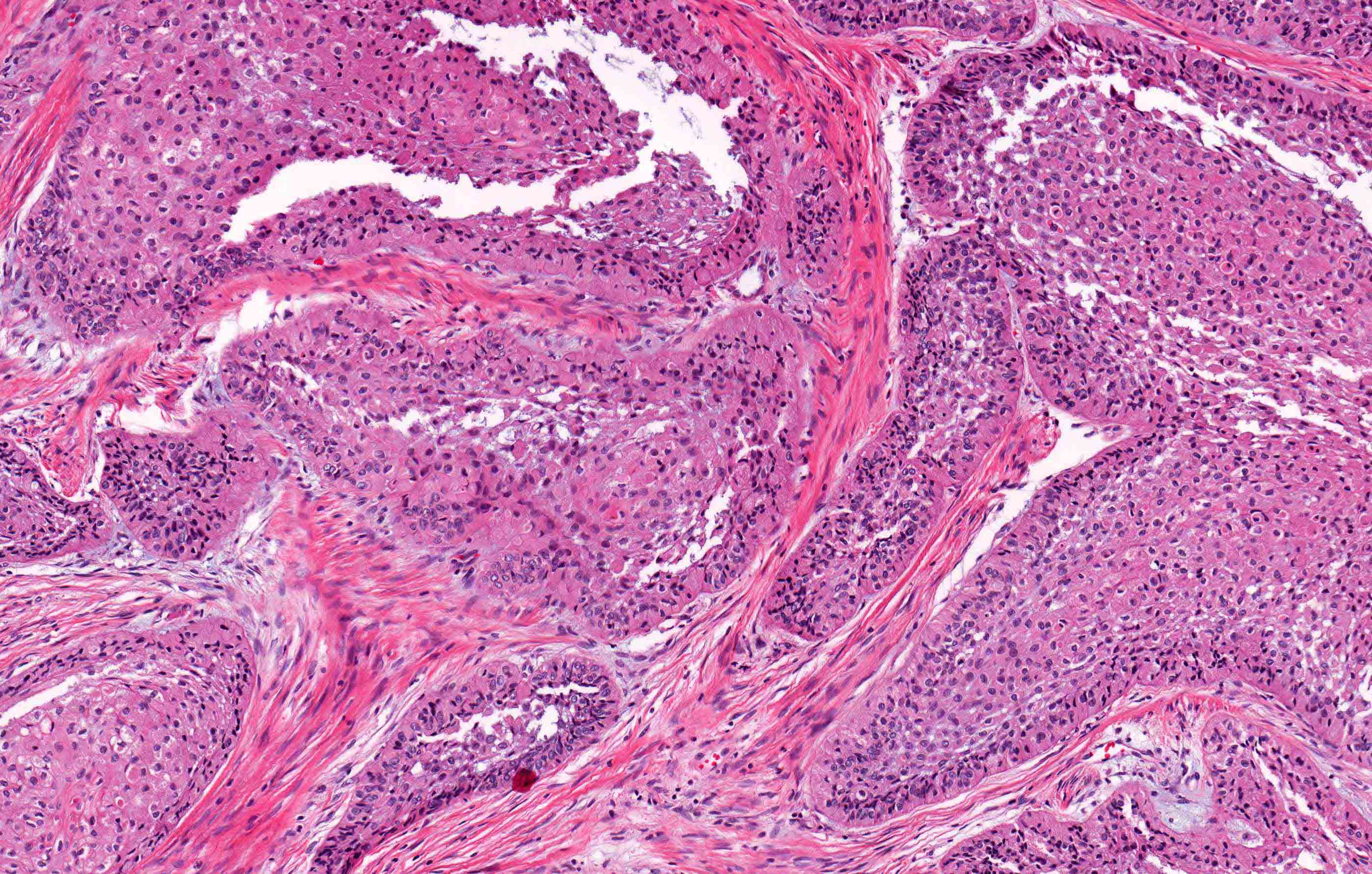
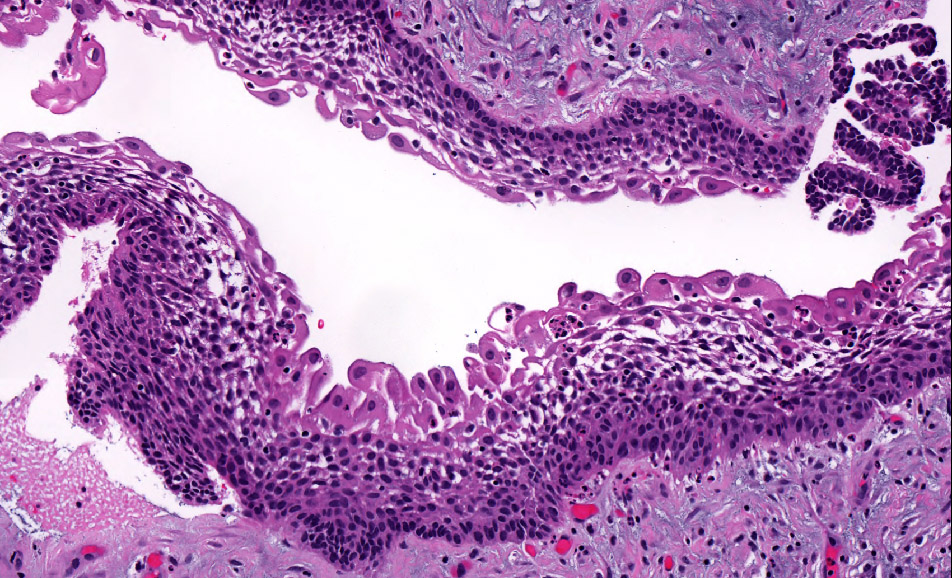
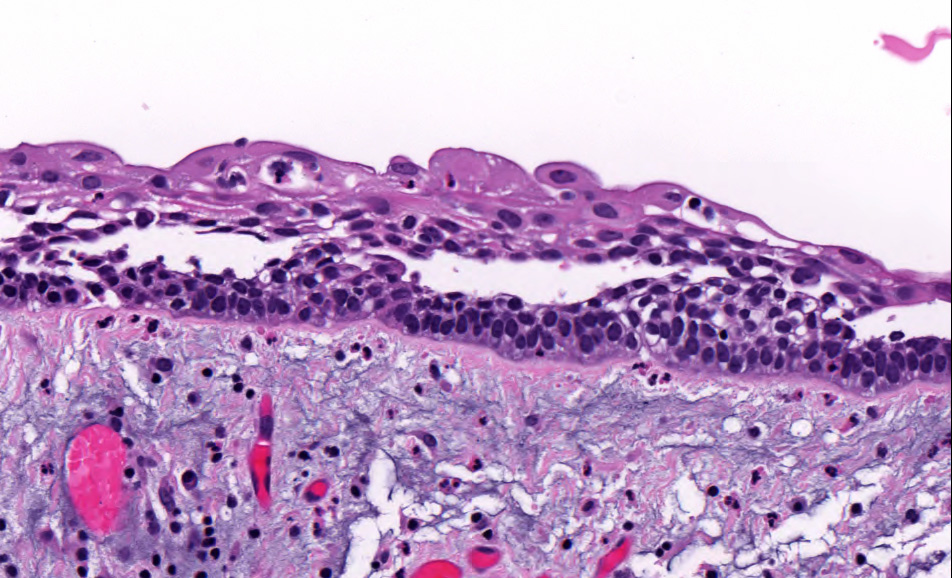
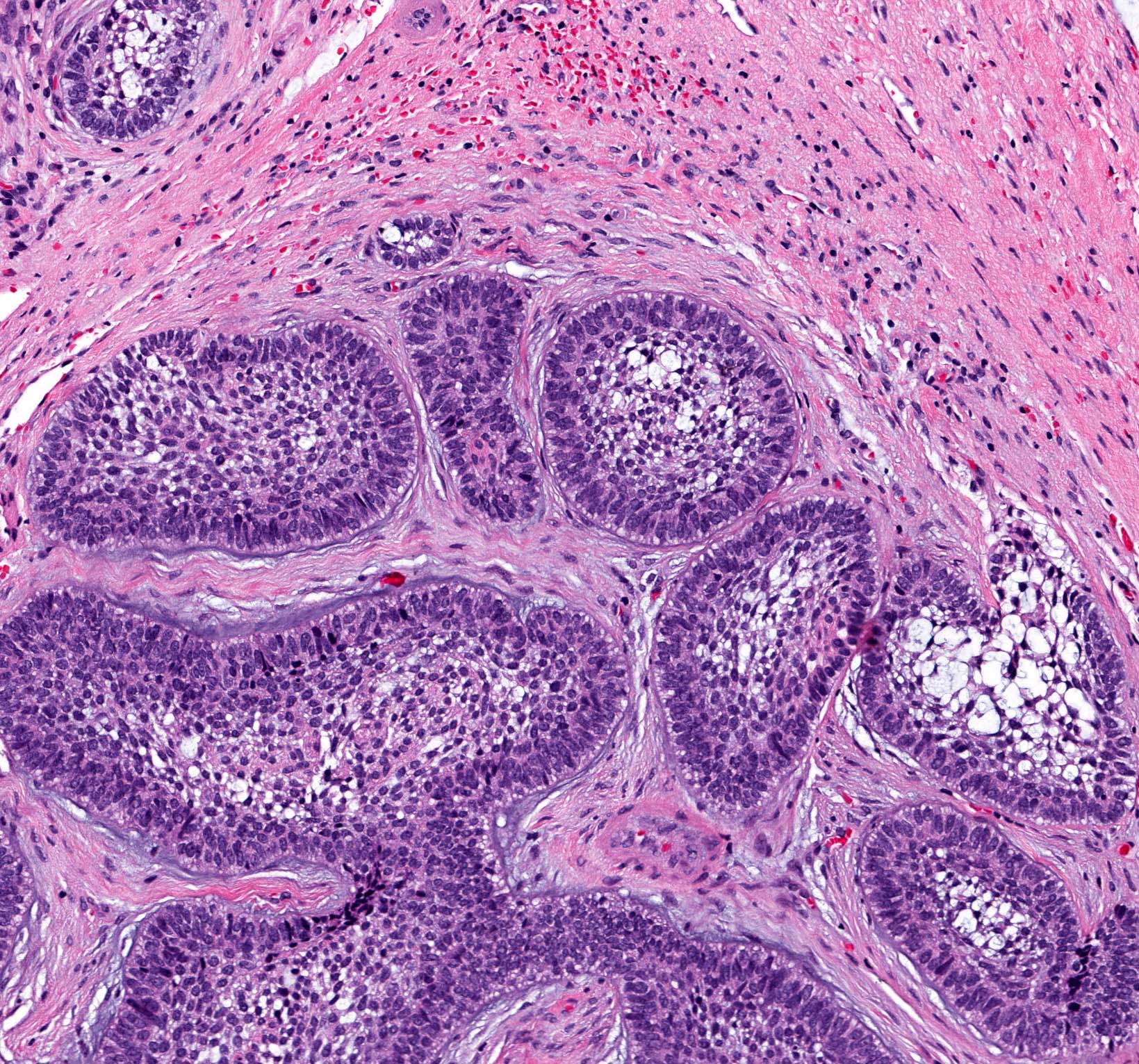
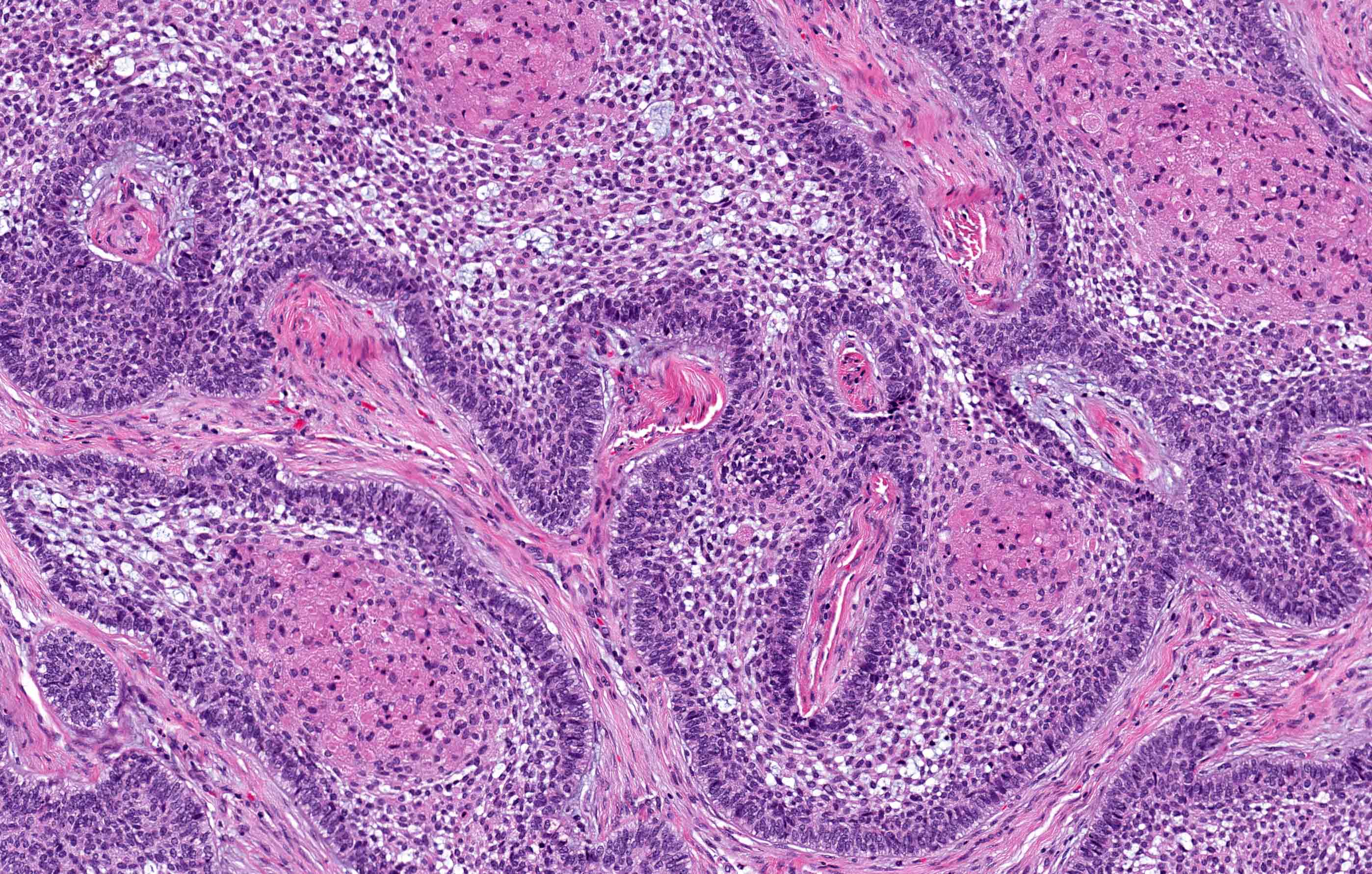
- Within the epithelial islands and cords of conventional ameloblastoma and the cystic epithelial lining of unicystic ameloblastoma, the odontogenic epithelium shows similar changes:
- Columnar cells with hyperchromatic nuclei at basal layer, exhibiting peripheral palisading
- Cells show reverse polarization away from basement membrane (Vickers-Gorlin change)
- Subnuclear vacuolization
- Suprabasal cells with a loose, network-like arrangement, recapitulating stellate reticulum formation seen in normal odontogenesis
- No dentin or enamel formation
- Ameloblastoma, conventional type may show macrocystic change of the tumor islands; when a limited portion of this phenomenon is sampled at initial biopsy, the appearance may suggest an odontogenic cyst, NOS or ameloblastoma, unicystic type
- Rarely, involvement of the inferior alveolar nerve has been reported in benign, conventional ameloblastoma (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001;91:557, Br J Oral Maxillofac Surg 2013;51:757)
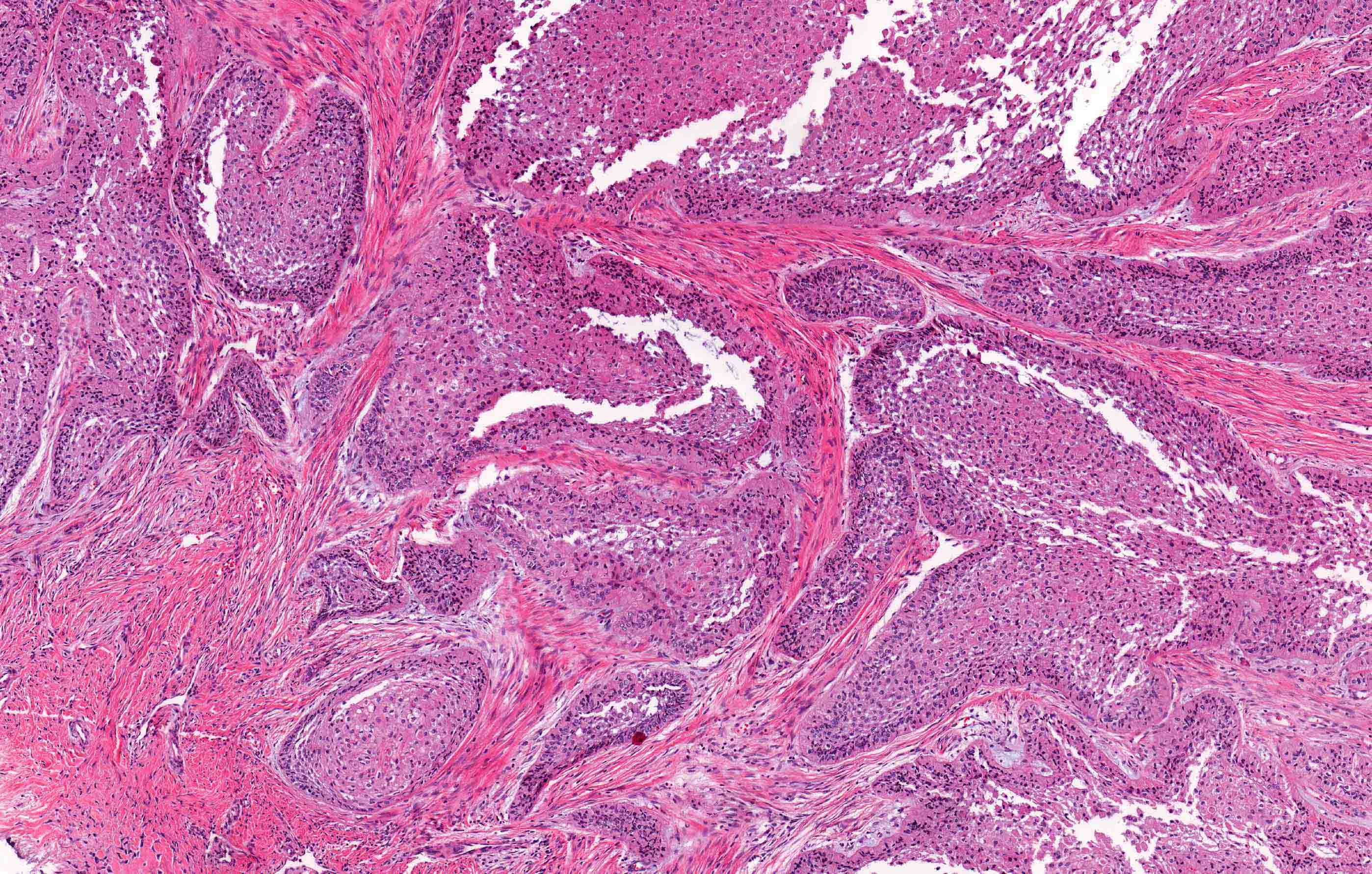
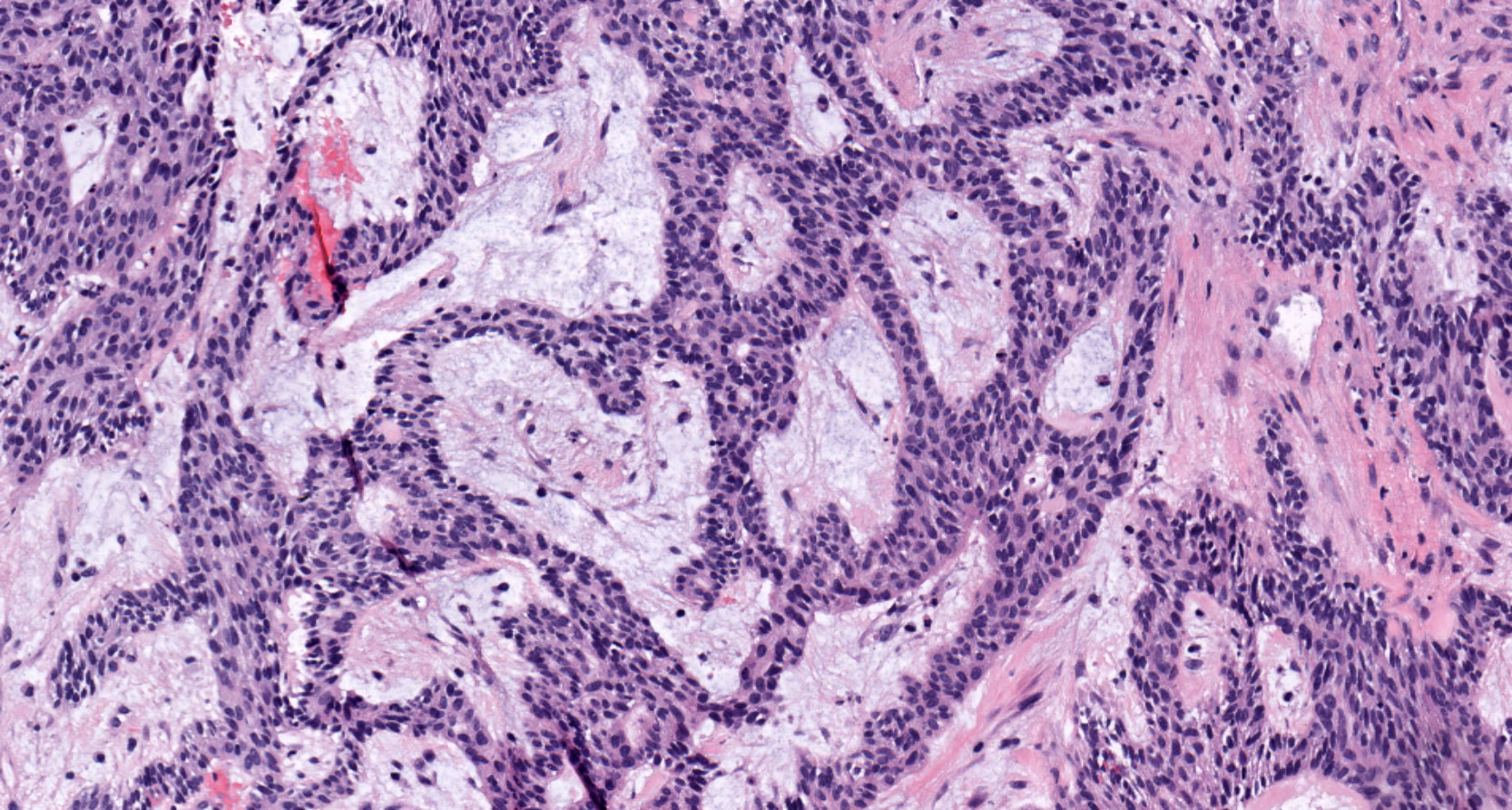
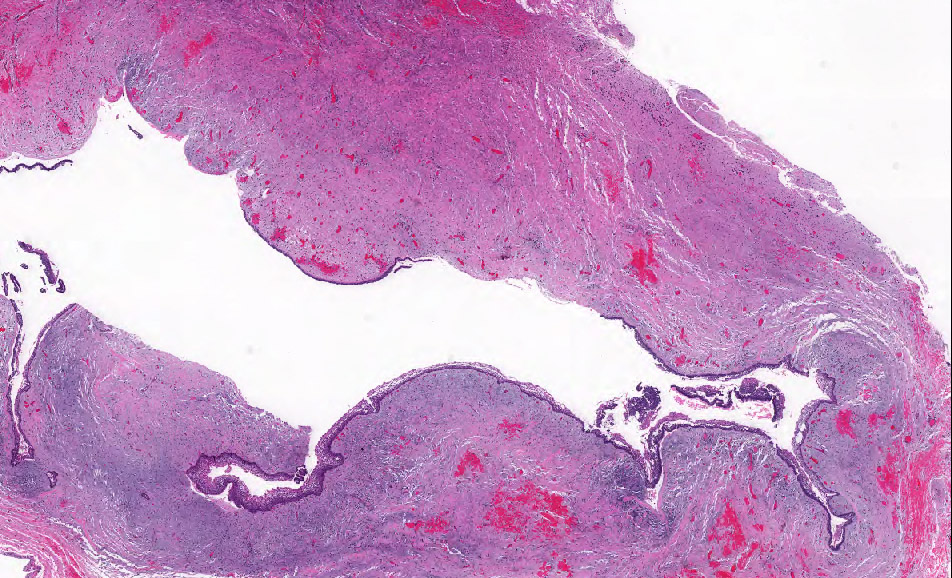
- Ameloblastoma, conventional type has at least 6 histopathological patterns
- Single patterns may predominate within a given lesion, often mixed with 1 or more patterns
- Microscopic pattern has no documented prognostic significance
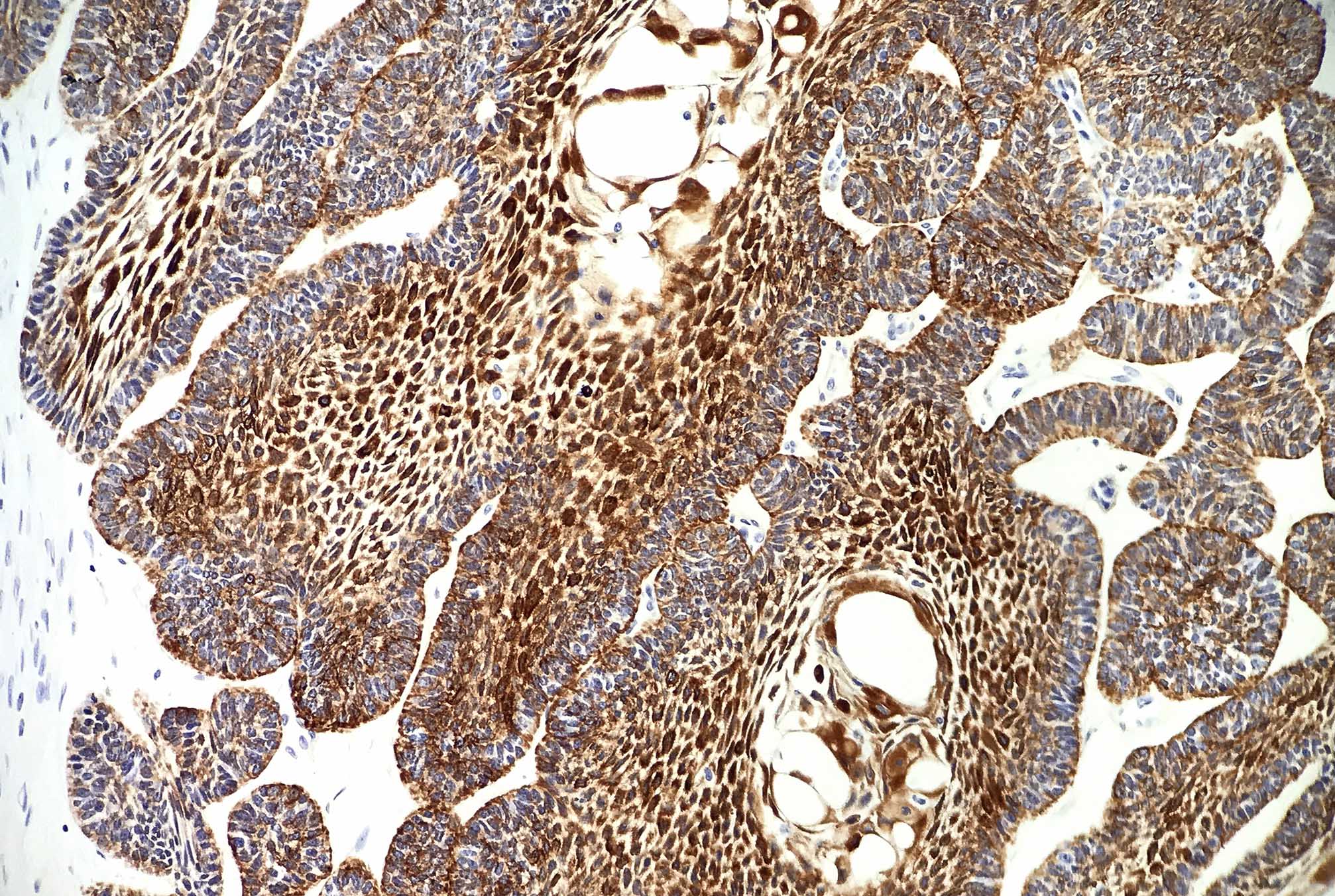
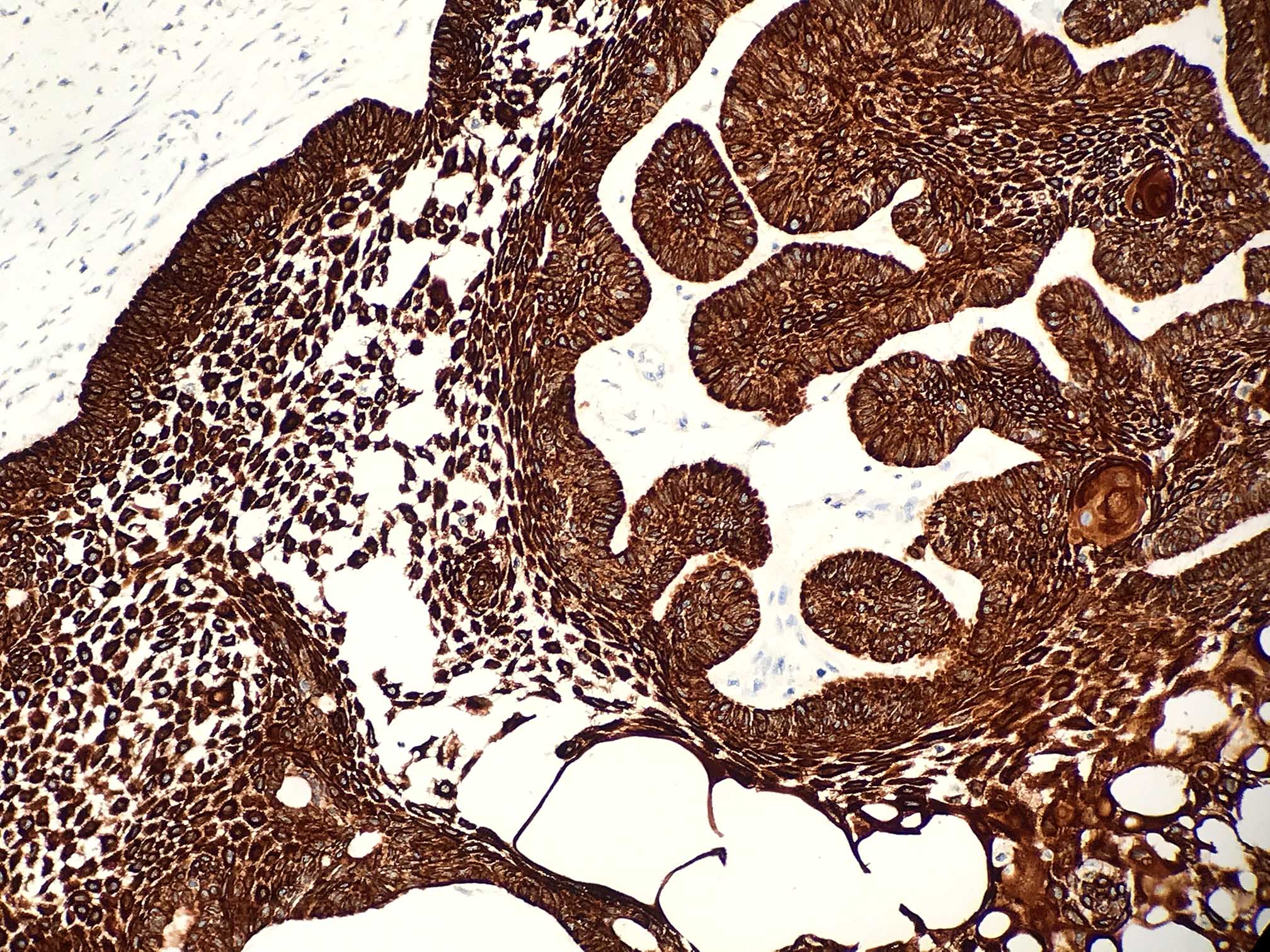
- Follicular: most common subtype; islands of odontogenic epithelium in fibrous connective tissue; may be cystic; classic peripheral palisading and stellate reticulum-like areas
- Plexiform: cords and sheets of anastomosing odontogenic epithelial cells; classic peripheral palisading and reverse polarity not always obvious
- Acanthomatous: squamous metaplasia and variable keratinization of stellate reticulum-like cells
- Granular cell: stellate reticulum-like cells have granular eosinophilic cytoplasm; less commonly involves cells at periphery of nests
- Basal cell / basaloid: least common histologic subtype; islands of hyperchromatic basal cells without stellate reticulum-like areas
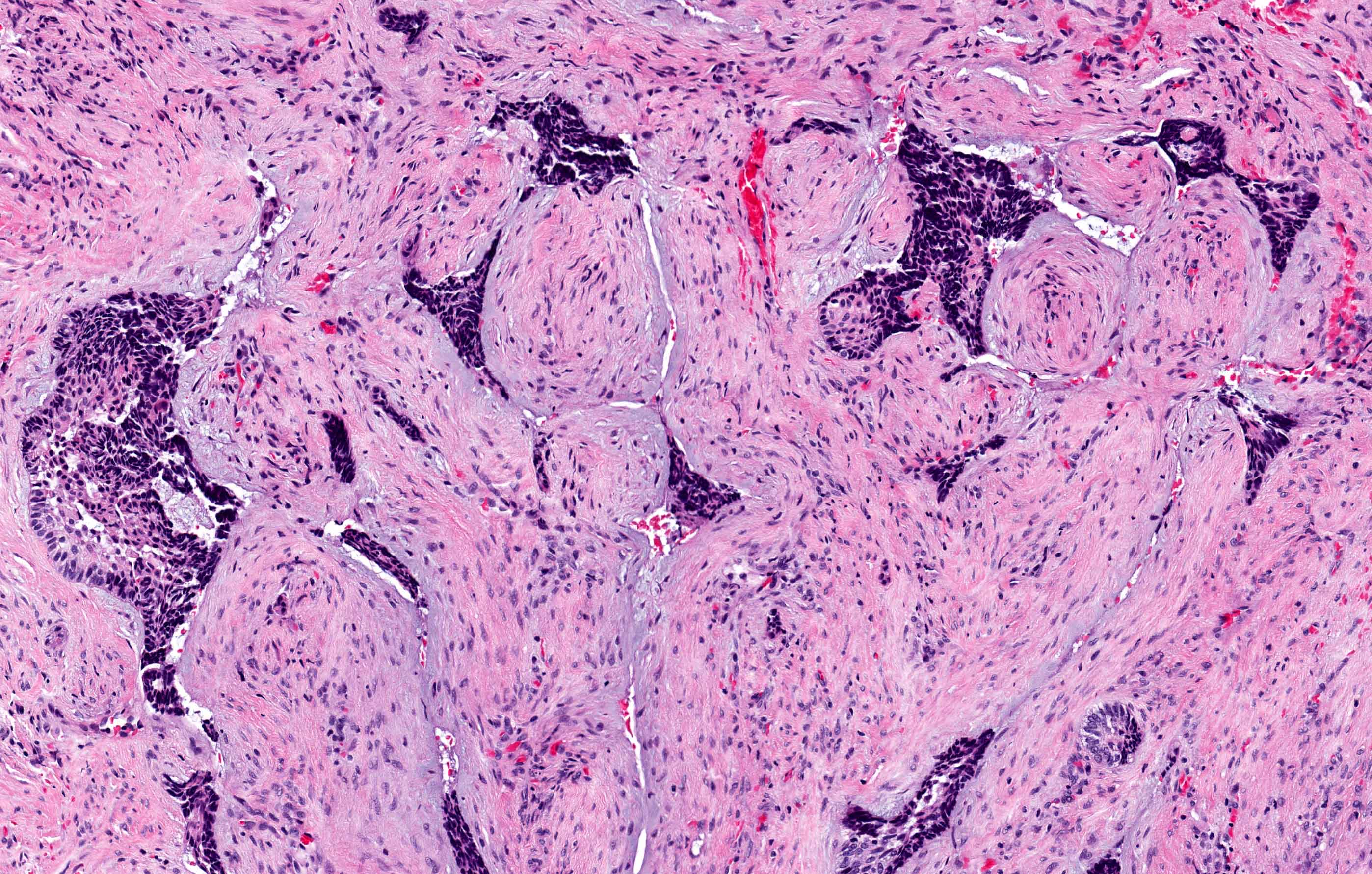
- Desmoplastic: compressed and angular islands of epithelial tumor cells with dense moderately cellular fibrous connective tissue or collagenous stroma; the formation of metaplastic bone trabeculae is also described
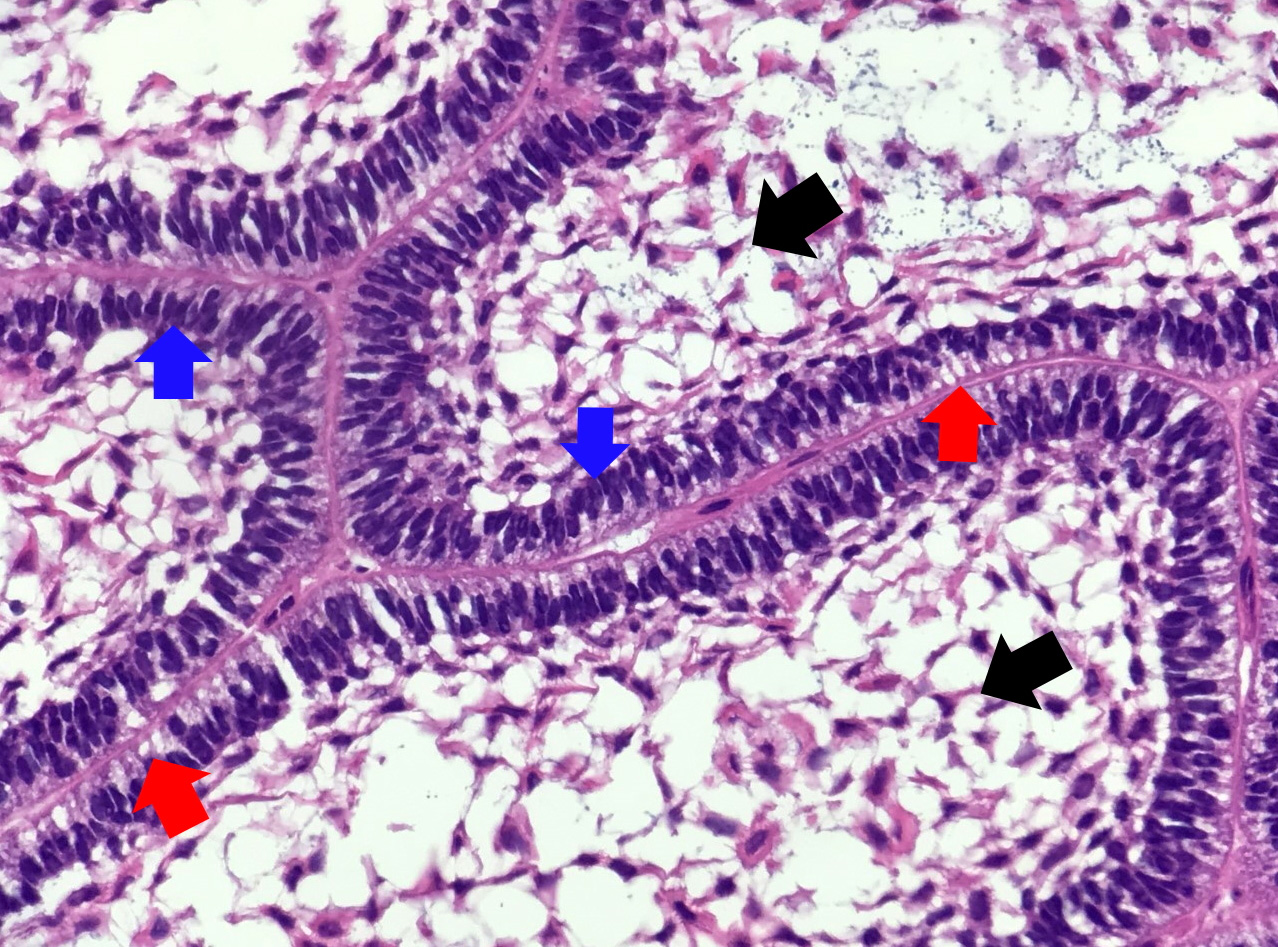
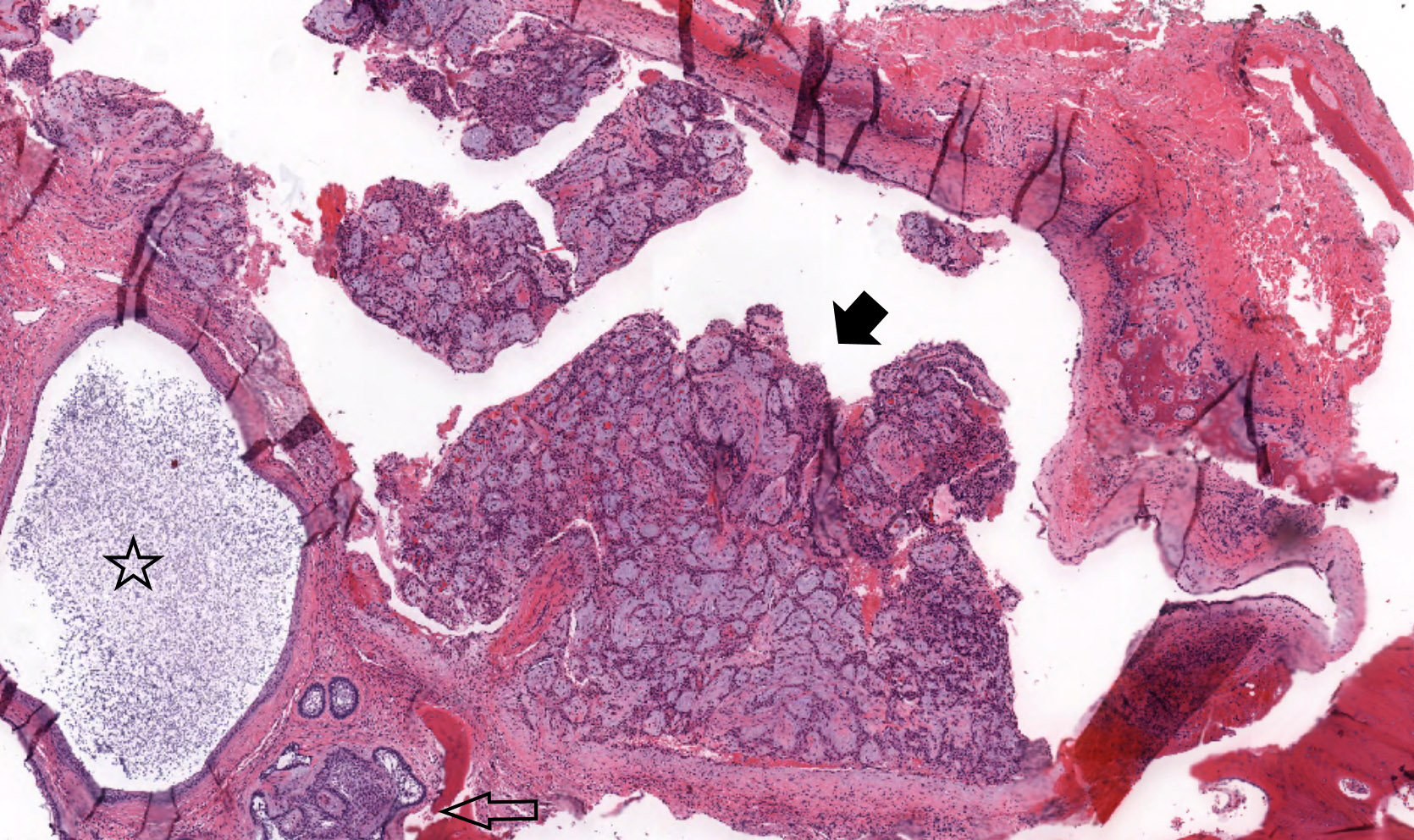
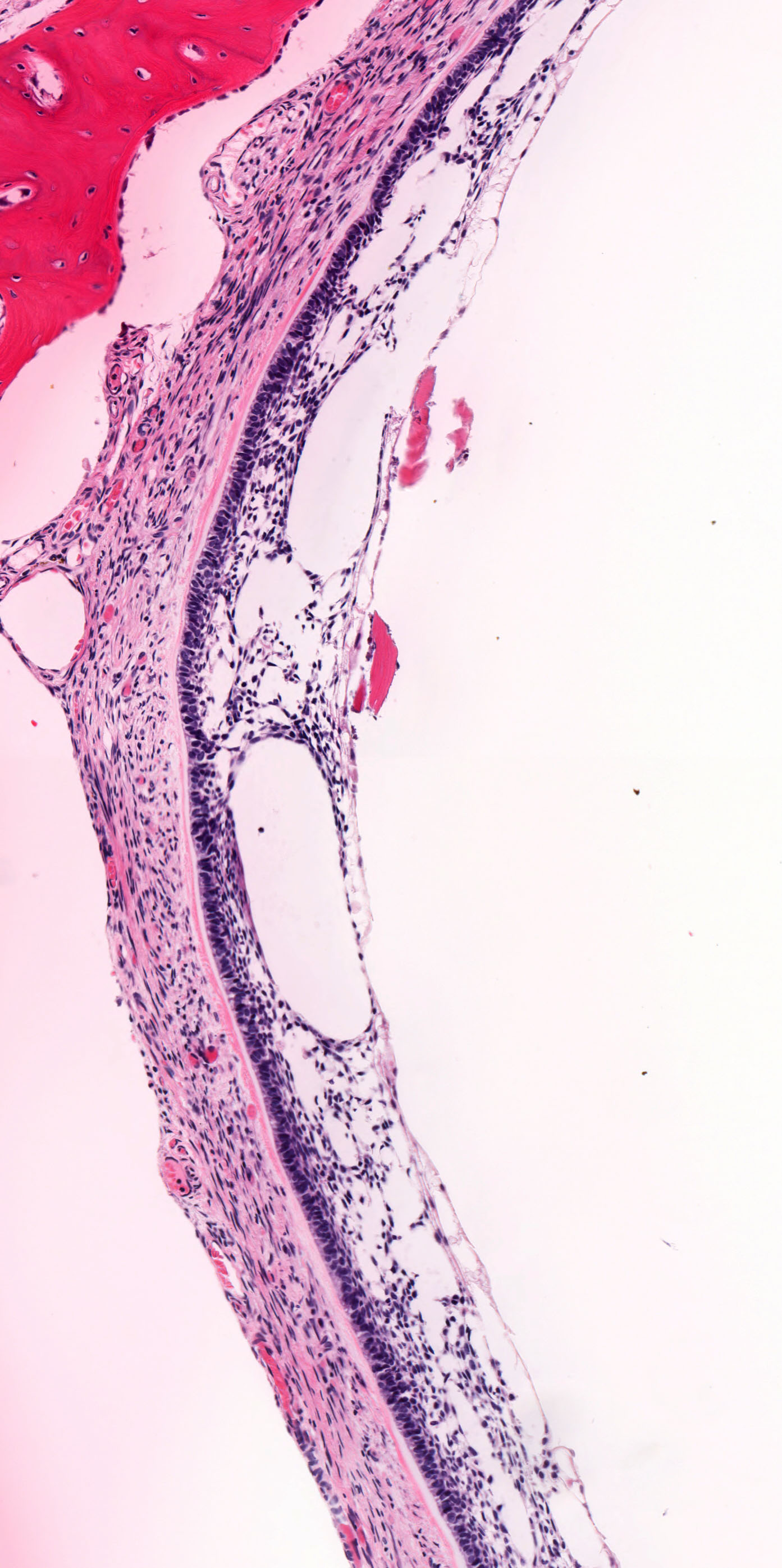
- Ameloblastoma, unicystic type has 3 histopathological patterns
- Single cystic lesion lined by ameloblastic epithelium that shows typical features of ameloblastoma in some areas, including columnar basal cells in palisading arrangement with vacuolated cytoplasm, hyperchromatic nuclei polarized away from basement membrane
- Suprabasal cells loosely textured and noncohesive resembling stellate reticulum, epithelial invagination, epithelial edema and separation
- Microscopic variants (may result in treatment differences - controversial)
- Luminal: cystic odontgenic epithelium with characteristic features (above) lining fibrous connective tissue wall
- Intraluminal: cystic odontgenic epithelium with characteristic features (above) lining fibrous connective tissue wall, with tumor extending into the cystic luminal space; may have intraluminal plexiform patterns
- Mural: cystic odontgenic epithelium with characteristic features (above) lining fibrous connective tissue wall but with the additional finding of definite ameloblastoma tumor islands within the fibrous connective tissue wall
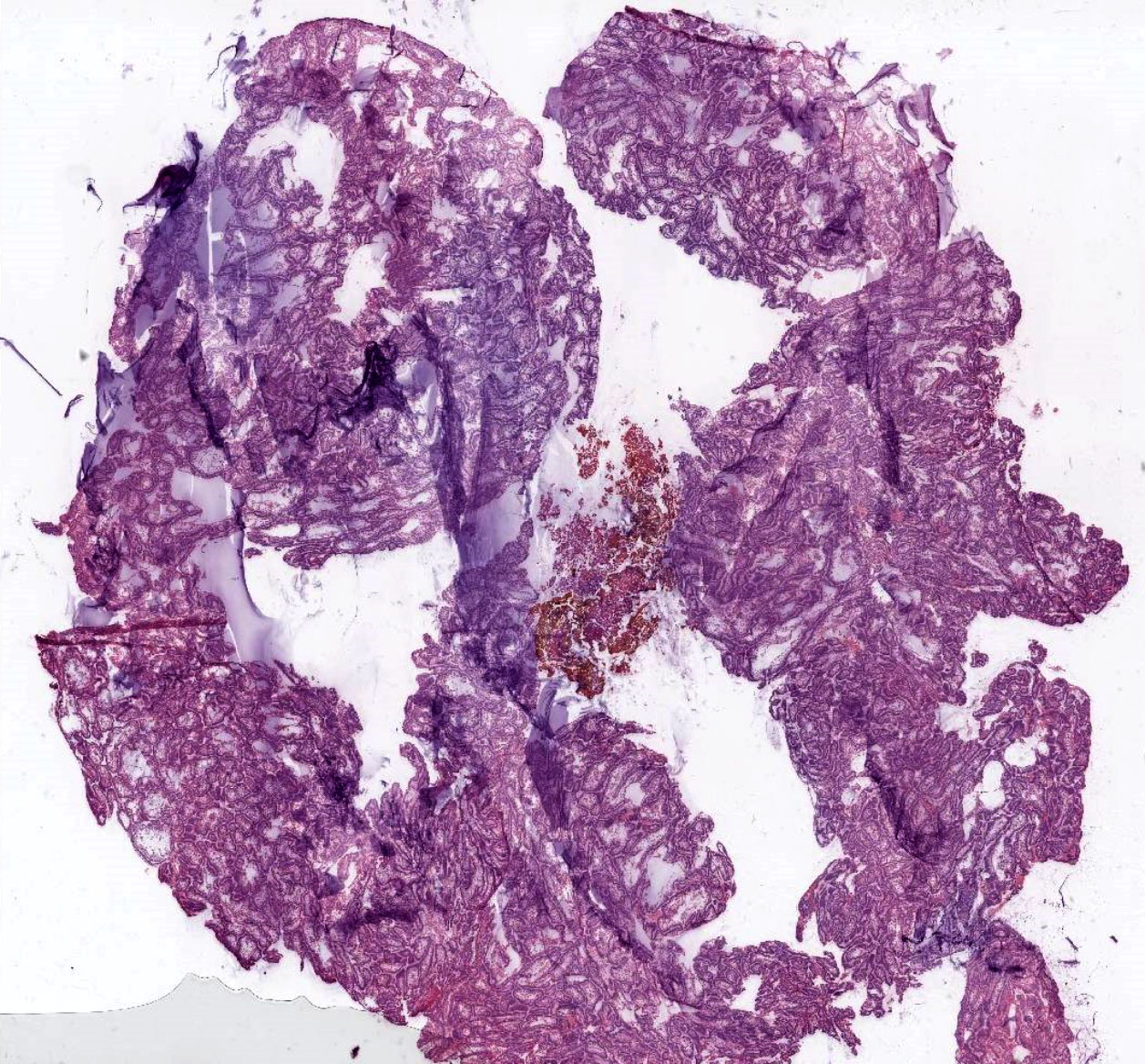
Microscopic (histologic) images
Contributed by Kelly Magliocca, D.D.S., M.P.H. and Anne C. McLean-Holden, D.M.D., M.S.
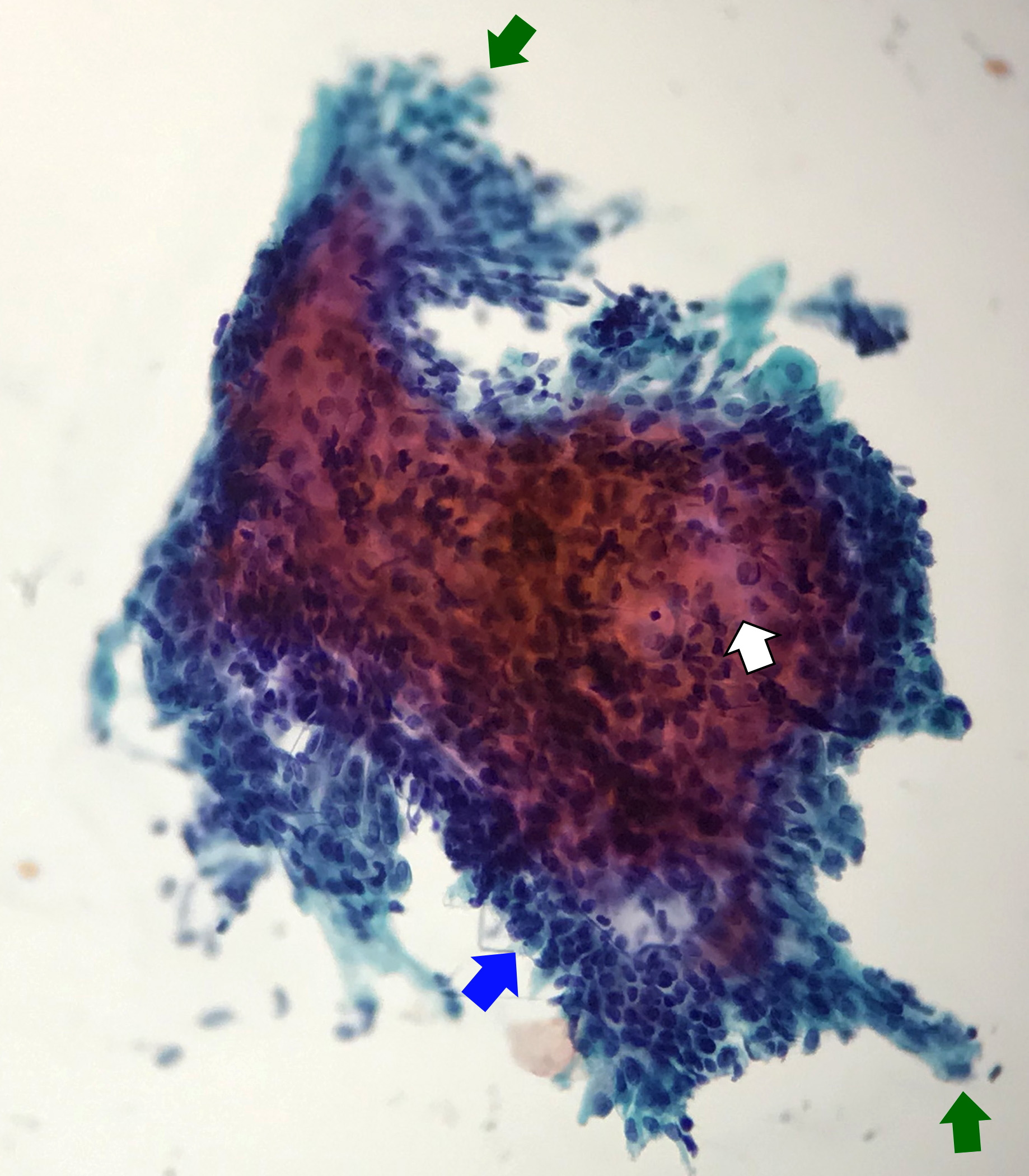
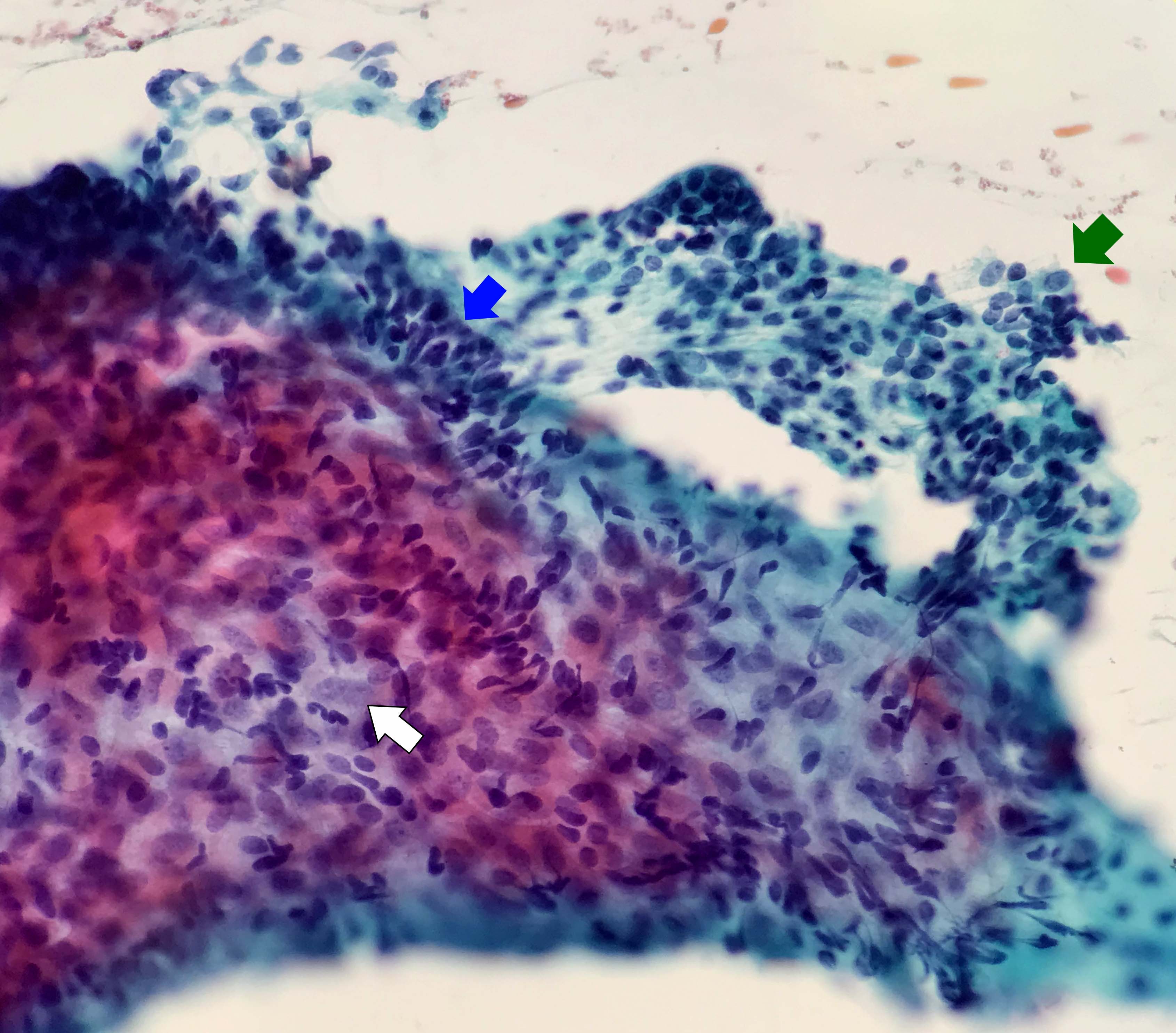
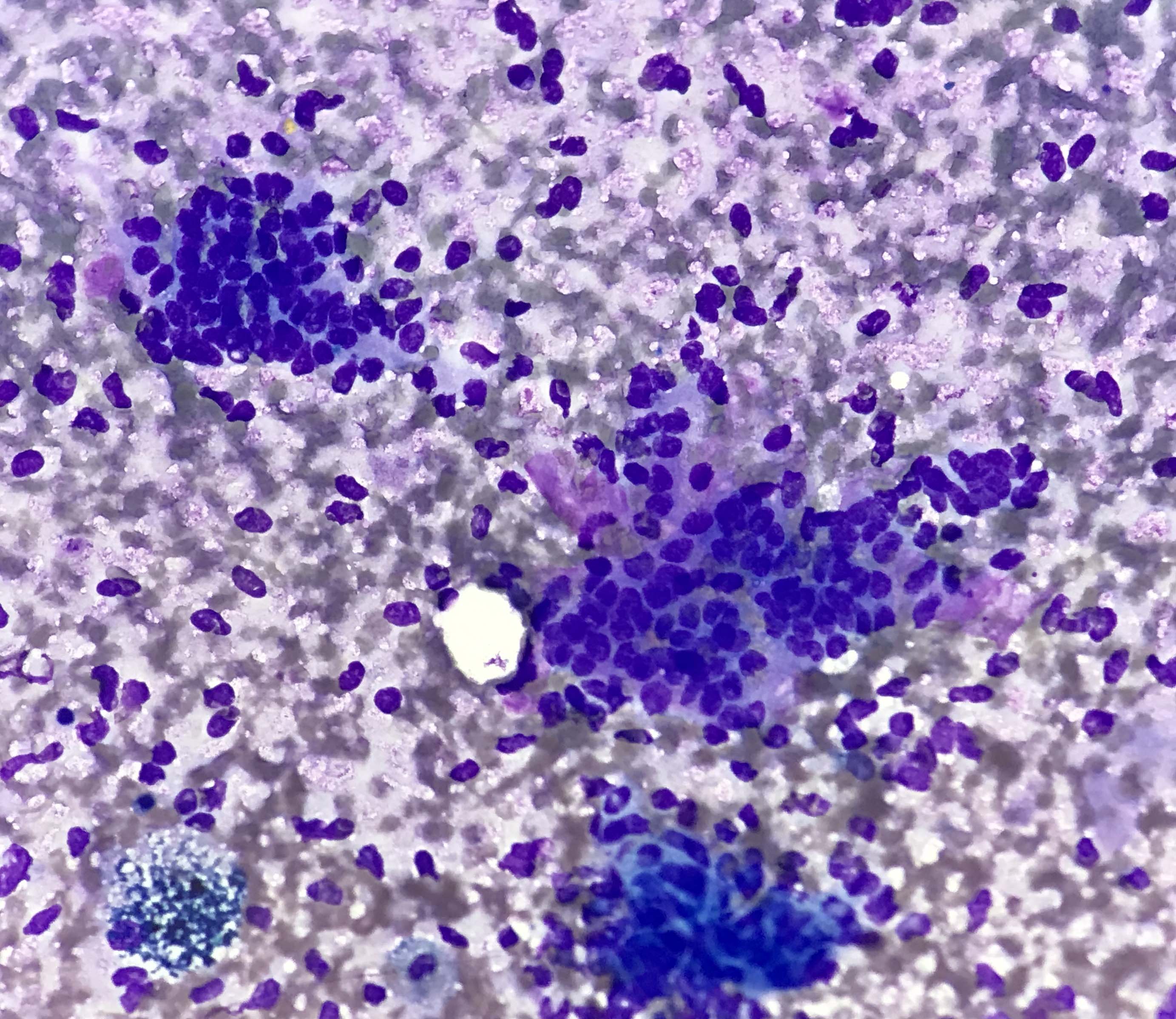
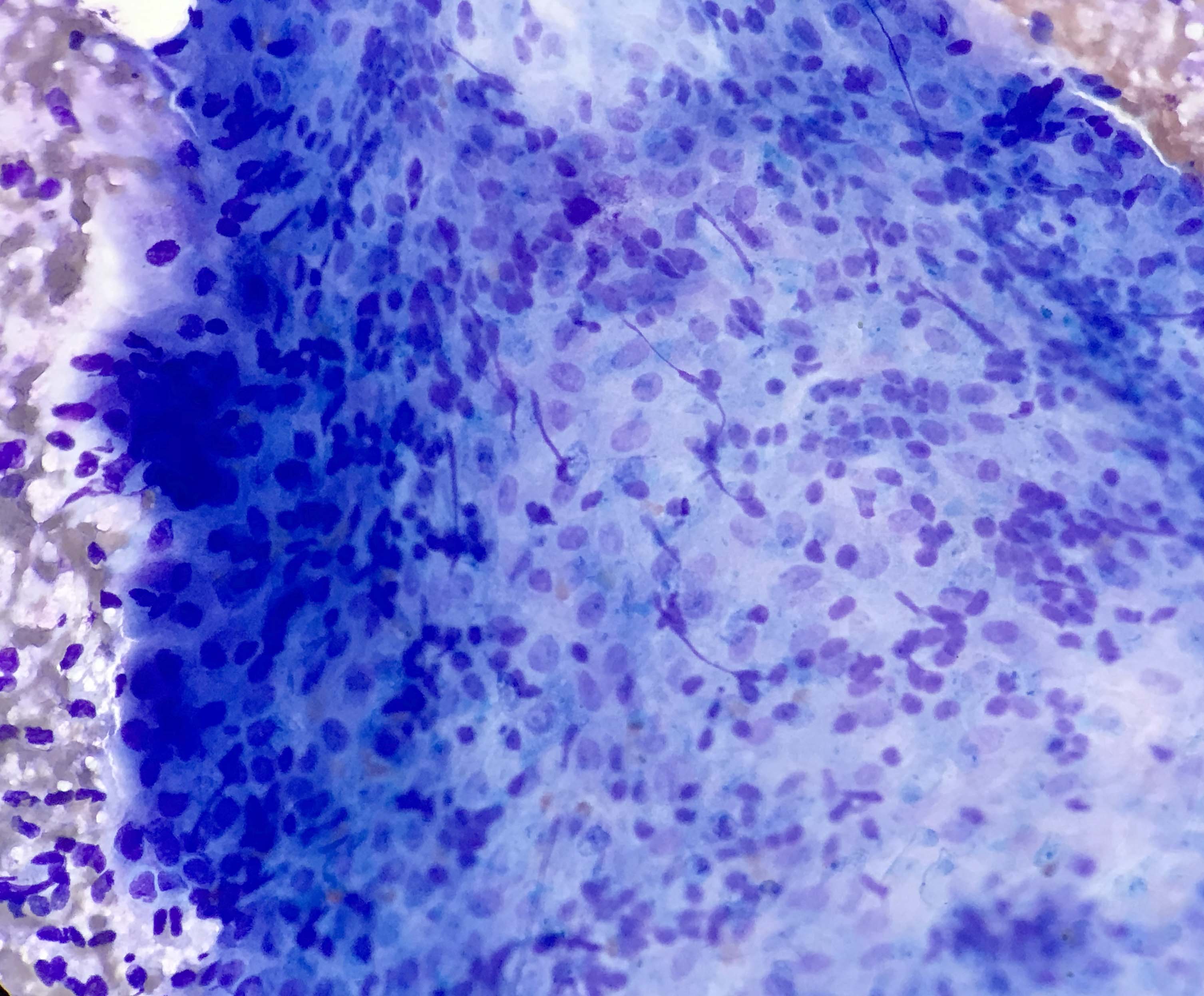
Cytology description
- Compact and cohesive cell clusters with areas of short branching of tumor cells along the periphery (Diagn Cytopathol 2013;41:206)
- Oval to round basaloid cells with high nuclear to cytoplasmic ratios, fine powdery chromatin, nucleoli with small peripheral nucleoli to inconspicuous nucleoli
- Squamous cells centrally with more abundant cytoplasm (particularly in acanthomatous variant)
- Possible limitations to FNA
- Inadequate sampling due to extensive cyst formation within the tumor
- Inability to distinguish ameloblastoma with macrocystic degeneration from ameloblastoma, unicystic type
- Inability to distinguish ameloblastoma from metastatic ameloblastoma without prior knowledge of metastatic disease
- Inability to distinguish ameloblastoma from other benign odontogenic tumors that are managed with curettage (e.g. adenomatoid odontogenic tumor, ameloblastic fibroma) (Diagn Cytopathol 2013;41:206)
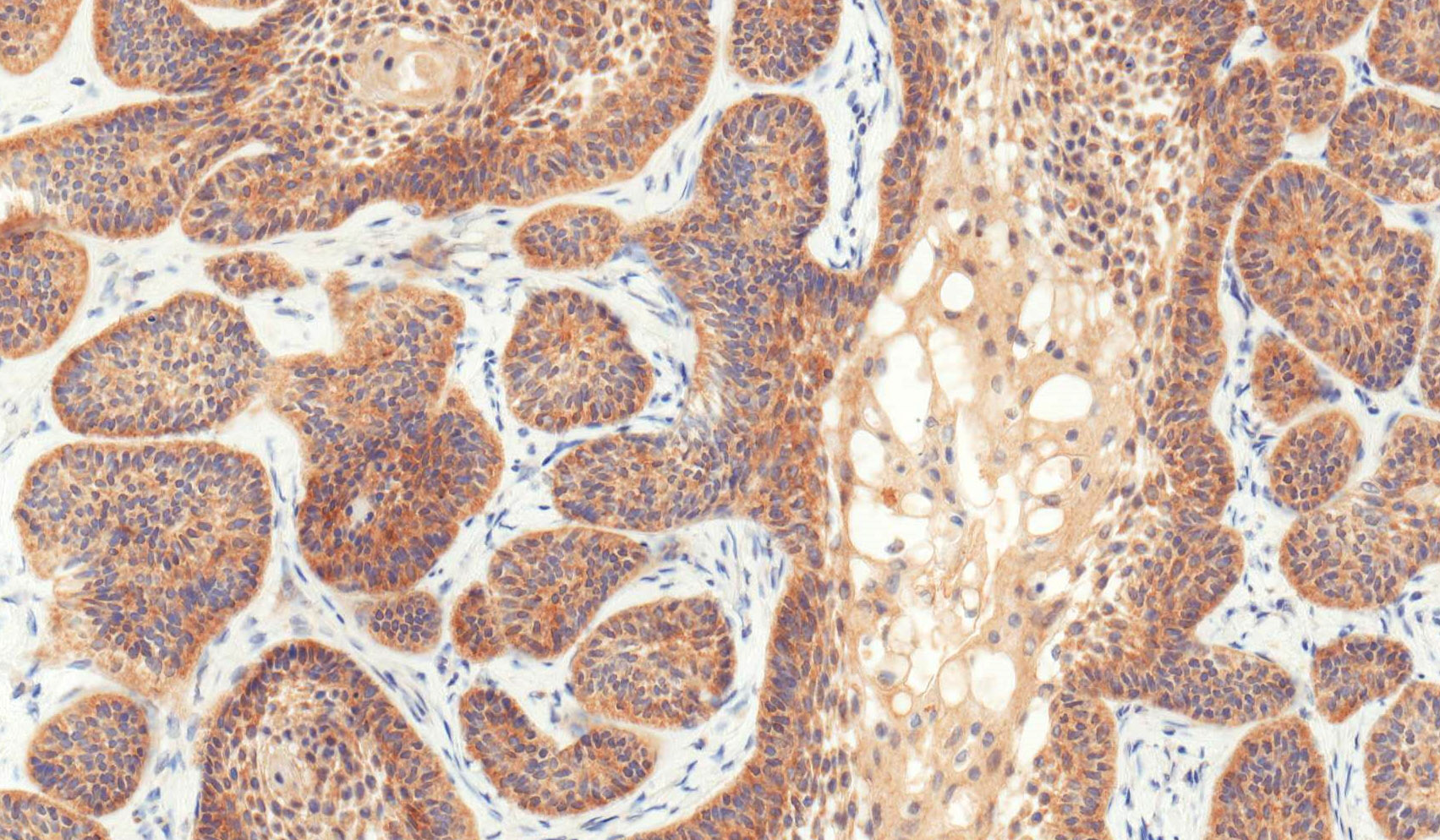
Positive stains
- CK19 and CK14 (J Oral Pathol Med 2016;45:704)
- CK5 (J Oral Pathol Med 2008;37:177)
- CD56 (Histopathology 2010;57:544)
- Calretinin (Histopathology 2001;38:312, Histopathology 2000;37:27)
- BRAF V600E (VE1) (Clin Oral Investig 2019;23:779)
- Beta catenin nuclear positive exceptionally rare (PLoS One 2017;12:e0180224)
- p63 and p40 (Oral Surg Oral Med Oral Pathol Oral Radiol 2018;126:506)
- FOXP1 (Am J Surg Pathol 2020;44:665)
Negative stains
- Uniformly SOX10 negative (Am J Surg Pathol 2020;44:665)
Electron microscopy description
- Epithelial differentiation (tonofilaments, complex desmosomes)
- Ultrastructural analyses have previously shown the presence of lysosomal aggregates in the cytoplasm of granular cells and apoptotic cell fragments were detected between these cells within the neoplastic clusters, corroborating this hypothesis (J Oral Pathol Med 2001;30:245)
Molecular / cytogenetics description
- Recurrent somatic and activating mutations in mitogen activated protein kinase (MAPK) pathway present in ~80% ameloblastomas identified in 2014 by 3 separate groups
- BRAF V600E (most common mutation; at least 60%)
- RAS and FGFR2
- Hedgehog signaling pathway; appear mutually exclusive from MAPK
- In a recent study, 94% of the mandibular unicystic ameloblastomas revealed BRAF V600E mutations; in 1 BRAF wild type mandibular tumor, an SMO p.L412F mutation was identified
Videos
Overview of odontogenic tumors by Dr. Khurram
Sample pathology report
- Mandible, left segmental mandibulectomy:
- Ameloblastoma (2.3 cm), confined to bone (see comment)
- Comment: Tumor measures 0.9 cm from anterior bone margin and 0.6 cm from posterior bone margin.
Differential diagnosis
- Differential diagnosis of ameloblastoma, conventional type
- Odontogenic fibroma:
- Short cords of odontogenic epithelium embedded in a moderately cellular fibrous / fibroblastic stroma
- No perineural or skeletal muscle invasion is seen
- Ameloblastic fibroma:
- Odontogenic epithelial component may exhibit peripheral palisading, reverse polarization and stellate reticulum-like areas
- Primitive appearance to stroma is essential to the diagnosis; evenly dispersed delicate spindled cells in an amphophilic background
- BRAF pV600E mutations described (Oral Oncol 2015;51:e77)
- Most common in children
- Adenomatoid odontogenic tumor:
- Benign odontogenic epithelial tumor with basaloid duct-like structures, lined by cuboidal or columnar cells
- May show focal reverse polarity
- Duct-like spaces contain eosinophilic secretions
- Amyloid-like material may be present
- Predilection for anterior maxilla, often associated with unerupted tooth
- 67% of patients are female
- Adenomatoid odontogenic tumor usually occurs in second decade
- See Case #490
- Squamous odontogenic tumor:
- Benign odontogenic epithelial tumor with squamous differentiation
- Jigsaw puzzle-like proliferation of squamous epithelial islands without atypia
- Lacks peripheral palisading or stellate reticulum-like areas
- Very rare; thought to arise from rests of Malassez in periodontal ligament
- Dentinogenic ghost cell tumor:
- Can have histologic features overlapping with ameloblastoma; is a solid proliferation of odontogenic epithelium with peripheral columnar or cuboidal basal cells with stellate reticulum-like central areas
- Will have ghost cells or anucleate epithelial cells
- Dentinoid present
- Beta catenin immunohistochemical stain positive
- BRAF pV600E has not been detected
- Sclerosing odontogenic carcinoma:
- Short epithelial nests and thin epithelial cords consisting of bland cuboidal or polygonal epithelial cells with cytoplasmic clearing within sclerotic stroma
- Mitoses are difficult to find; however, infiltration of skeletal muscle and perineural invasion is conspicuous
- Clear cell odontogenic carcinoma:
- 3 histopathologic patterns have been described for clear cell odontogenic carcinoma: clear cell, squamoid appearing and ameloblastoma-like
- Classically, a monophasic, clear cell population of epithelial cells are arranged in nests and cords
- Hyalinized connective tissue often separate the clear cell nests
- Eosinophilic cells represent the dominant cell type within the squamoid variant
- Third pattern has a resemblance to ameloblastoma, since peripheral cells within tumor islands may demonstrate palisading
- EWSR1 mutated in majority of cases
- 3 histopathologic patterns have been described for clear cell odontogenic carcinoma: clear cell, squamoid appearing and ameloblastoma-like
- Ameloblastic carcinoma:
- May show features of amelobastoma, such as peripheral palisading, reverse polarity of basal cells, stellate reticulum-like areas
- Features of malignancy include cytologic atypia, high N/C ratio, increased mitotic figures with atypical forms or necrosis
- Odontogenic fibroma:
- Differential diagnosis of ameloblastoma, unicystic type
- Dentigerous cyst:
- Benign odontogenic epithelial cyst
- Inflamed, stratified squamous epithelial lining, versus 2 - 4 layers of cuboidal epithelium, devoid of superficial keratinization (uninflamed dentigerous cyst)
- No rete ridges, flat interface
- Fibrous to fibromyxoid connective tissue
- BRAF negative (J Oral Pathol Med 2016;45:780)
- Reference: J Investig Clin Dent 2014;5:220
- Odontogenic keratocyst (OKC):
- Benign odontogenic epithelial cyst
- Stratified squamous epithelial lining characterized by palisaded hyperchromatic basal cell layer comprised of cuboidal cells
- Uniform epithelial lining 6 - 8 cells thick lacking rete ridges
- May have areas of budding growth from the basal cells
- Luminal surface has wavy ("corrugated") parakeratotic epithelial cells
- Lumen may contain keratinaceous debris
- May have artifactual clefting between epithelium and underlying fibroconnective tissue
- In contrast to unicystic ameloblastoma, BRAF pV600E mutations would be considered rare, if ever, in bona fide OKC
- Calcifying odontogenic cyst:
- Benign odontogenic epithelial cyst
- Well defined layer of palisading basal cells, loosely arranged suprabasal epithelial cells, resembling stellate reticulum similar to ameloblastoma
- Unlike ameloblastoma, variable numbers of lesional epithelial cells undergo ghost cell change in suprabasilar epithelium
- Epithelium also contains pale, eosinophilic ghost cells that may keratinize or calcify; variable foreign body reaction
- Ghost cells: altered epithelial cells with preservation of basic cell outline, eosinophilic cytoplasm but loss of nucleus
- Dentinoid present to a variable degree; paucicellular, eosinophilic calcified material considered to represent dysplastic dentin
- Beta catenin nuclear positive
- BRAF negative (immunohistochemistry and molecular)
- Limited biopsy sampling of the macrocystic degeneration component of ameloblastoma, conventional type:
- Basal palisading with reverse polarity, hyperchromatic basal layer
- Stellate reticulum-like layer
- Larger sample can be helpful in distinguishing type
- Dentigerous cyst:
Additional references
Board review style question #1
Which of the following is true about microscopic variants of ameloblastoma?
- Multiple microscopic variants possible in the same tumor
- Multiple microscopic variants unlikely to occur in the same tumor
- Multiple microscopic variants within the same tumor is associated with hypercalcemia
- Multiple microscopic variants within same tumor suggests high grade transformation has occurred
Board review style answer #1
A. Multiple microscopic variants possible in the same tumor, as described in WHO 4th edition
Comment Here
Reference: Ameloblastoma
Comment Here
Reference: Ameloblastoma
Board review style question #2
Which of the following histologic patterns of ameloblastoma is most likely to be misidentified as an odontogenic cyst?
- Ameloblastoma, extraosseous peripheral type with follicular growth
- Ameloblastoma, granular cell variant histology
- Ameloblastoma, unicystic type with luminal growth
- Ameloblastoma with acanthomatous variant histology
Board review style answer #2
C. Ameloblastoma, unicystic type with luminal growth. Ameloblastoma, unicystic type lacks mural island formation, thus mimicking a cyst.
Comment Here
Reference: Ameloblastoma
Comment Here
Reference: Ameloblastoma