Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Laboratory | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Electron microscopy images | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Lieberman JA. Clostridioides difficile. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/microbiologycdifficile.html. Accessed April 19th, 2024.
Definition / general
- Gram positive, strict anaerobe bacteria causing pseudomembranous colitis
- Ranges from normal flora of neonates, to asymptomatic carriage in children and adults, to diarrheagenic pathogen
- Transmissible, hand washing necessary (alcohol based sanitizers insufficient to remove spores) and contact precautions are standard
Essential features
- Gram positive bacteria important in antibiotic associated (pseudomembranous) colitis with marked diarrhea
- Anaerobic growth, spore formation
- Morphology (Anaerobe 2016;40:95):
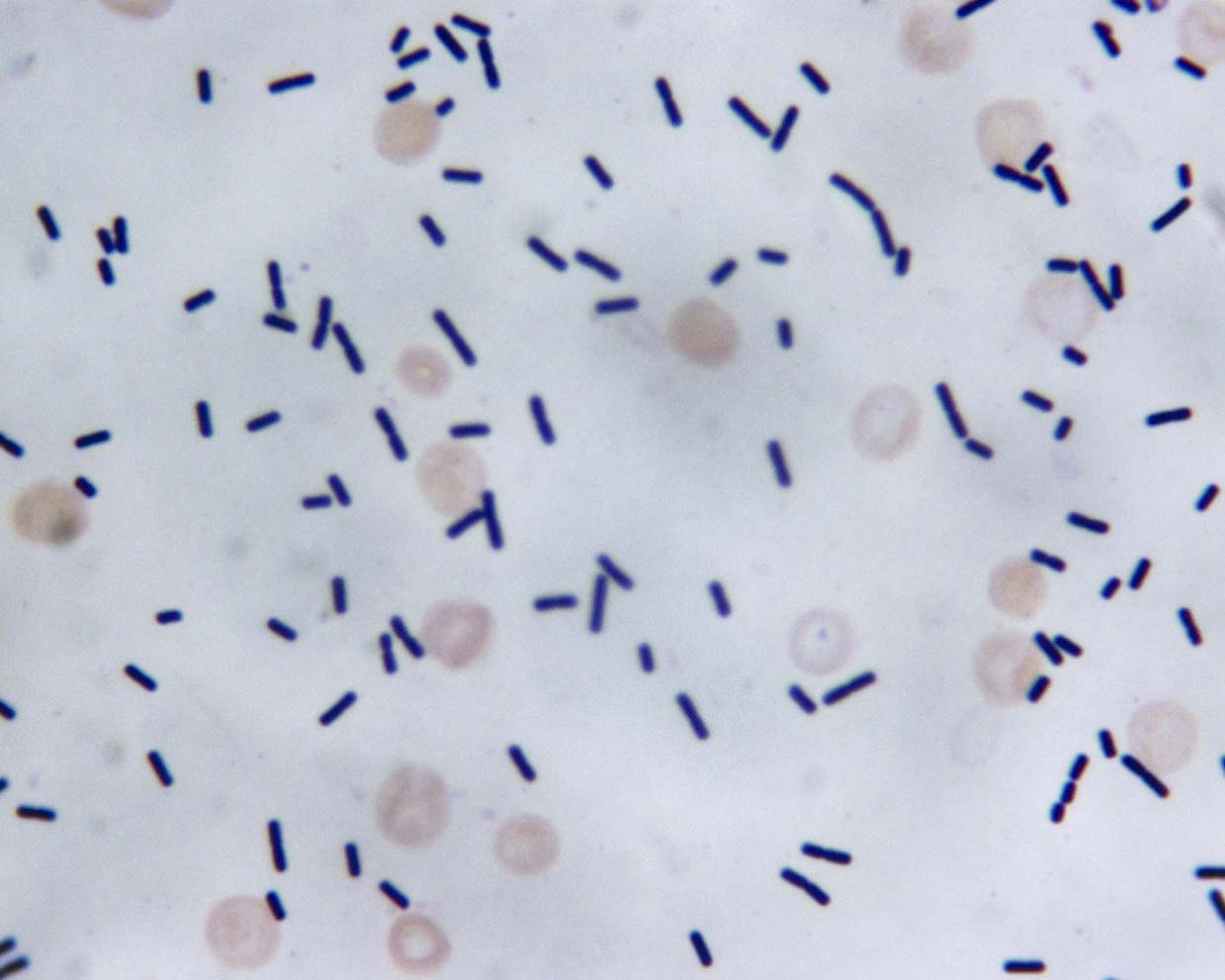
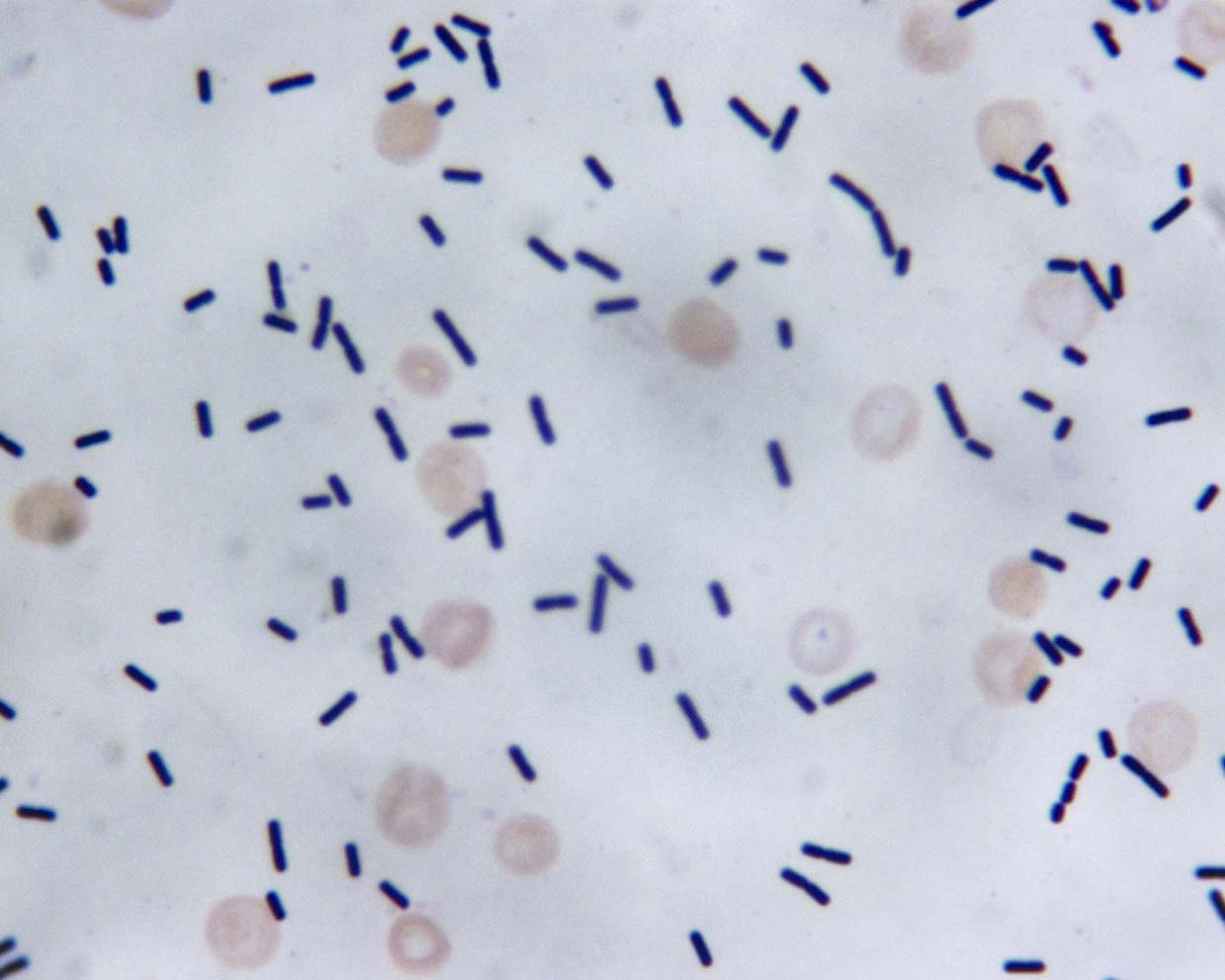
- Microscopic: rods, box car shaped, occasionally in chains
- Colonies: gray-white, low convex, 2 - 5 mm, matte to glossy, pale green fluorescence under UV light (traditional culture rarely employed for ID)
- Toxins required for disease and molecular detection: toxin A, toxin B and regulatory protein TcdC (J Clin Microbiol 2009;47:3729, J Clin Microbiol 2010;48:4519, Nature 2010;467:711)
- Epidemic strains (ribotype 027) have a third binary toxin, C. difficile transferase (CDT) that contributes to virulence (J Infect Dis 2014;209:83)
Terminology
- Previously Clostridium difficile but phylogenetically distant from Clostridium sensu strictu and therefore renamed Clostridioides (Anaerobe 2016;40:95)
- Jargon: C. diff
- CDI – Clostridioides difficile infection; CDAD – Clostridioides difficile associated disease / diarrhea
- Causes pseudomembranous colitis
ICD coding
- A04.7: enterocolitis due to Clostridium difficile
Epidemiology
- Causes illness in ~ 500,000 Americans per year; 15 - 30,000 deaths per year (Clin Infect Dis 2018;66:987)
- Incidence:
- 147/100,000 (Clin Infect Dis 2018;66:987)
- Highest incidence at age 65+
- > 60% of cases are health care associated
- Patients with inflammatory bowel disease, immunocompromise (post solid organ or bone marrow transplant) are at increased risk
- Antibiotic use is a major risk factor due to disruption of gut
microbiota (Clin Infect Dis 2018;66:987)
- Prior antibiotic use may be less of a factor in pediatric populations (Pediatr Infect Dis 1982;1:336)
- Major nosocomial pathogen; patient isolation, hand washing and proper use of gown / gloves important interventions (Clin Infect Dis 2018;66:987)
- Rare cause of illness in children under 2 years; testing not recommended unless noninfectious and other infectious causes excluded (Clin Infect Dis 2018;66:987)
Sites
- Colon
Pathophysiology
- Bacterial proliferation when gut microbial population structure is perturbed
- Toxin production (Gut Microbes 2014;5:579, Nat Rev Microbiol 2016;14:609)
- TcdA and TcdB are secreted, inactivate Rho GTPases and lead to actin depolymerization, cell rounding, apoptosis and loss of epithelial barrier function, as well as inflammasome activation
- CDT is not cytotoxic, is associated with virulence and can also disrupt colonocyte cytoskeleton
- Endospore formation permits persistence (Gut Microbes 2014;5:579, Nat Rev Microbiol 2016;14:609)
- Type IV pilus production promotes epithelial adhesion and may have role in biofilm formation (Nat Rev Microbiol 2016;14:609)
Laboratory
- Molecular diagnostic testing is mainstay of detection; multiple
assays available and perform better than cytotoxin neutralization
assay or enzyme immunoassay
- PCR assays detect either single organism versus multi organism panel
- Example of single organism: Cepheid GeneXpert has primers to multiple targets: tcdB, tcdC, cdtA and cdtB loci with ≥ 97% sensitivity and ≥ 90% specificity (J Clin Microbiol 2010;48:4519, J Clin Microbiol 2009;47:3729)
- Example of multiplex panel: Biofire FilmArray GI Panel detects by qPCR and also has high sensitivity (≥ 94%) and specificity (≥ 97%) for C. difficile (J Clin Microbiol 2015;53:915)
- Molecular assays are not tests of cure as DNA can persist in stool after disease resolution
- Institutional guidelines limiting molecular testing important to avoid overdiagnosis (e.g., detection of C. difficile in patients without diarrhea, indicating carrier state) (Clin Infect Dis 2018;66:987)
- Minimum time for retesting after positive test (i.e., do not use as test of cure due to persistence of DNA)
- Laboratories typically only accept nonformed stool for diagnostic testing
- If no preset institutional nucleic acid amplification testing guidelines, recommendation is to use a stool toxin test as part of multistep algorithm
- Gram stain and culture are rarely used in diagnosis
- Bacteria are gram positive, albeit frequently with variable gram staining
- Requires specific culture conditions; typically see anaerobic growth within 48 hours
- Morphology / colonies: see gross and microscopic descriptions
Case reports
- 28 year old man with chronic refractory ulcerative colitis (J Crohns Colitis 2015;9:367)
- 78 year old woman successfully treated using a combination of fecal microbiota therapy and fidaxomicin (Med Princ Pract 2017;26:182)
- Woman with fulminant pseudomembranous colitis caused by Clostridium difficile PCR ribotype 027 (J Infect Chemother 2014;20:729)
Treatment
- Antibiotic treatment is oral vancomycin or fidaxomicin (not absorbed
and thus no systemic exposure)
- Add IV metronidazole if severe, fulminant infection including ileus or megacolon
- Oral metronidazole if vancomycin or fidaxomicin are unavailable
- Surgical management (subtotal colectomy) may be necessary for severe infections
- Fecal microbiota transplant for patients with ≥ 2 recurrences and for whom medical therapy has not worked (Mayo Clin Proc 2017;92:1617, Am J Transplant 2018 Aug 7 [Epub ahead of print], Anaerobe 2013;19:22)
- Pending FDA approval; interim guidance for use issued by FDA (FDA: Enforcement Policy Regarding Investigational New Drug Requirements [Accessed: August 15, 2018])
Gross description
- Colonies: gray-white, low convex, 2 - 5 mm, matte to glossy, pale green fluorescence under UV light (but traditional culture rarely employed for ID)
Microscopic (histologic) description
- Rods, box car shaped, 0.5 - 1.9 x 3 – 17 microns
- Subterminal spores may be evident as oval, intracellular clearings
- Occasional chains of 2 - 6 cells
Differential diagnosis
- Diarrheagenic E. coli
- Viral diarrheal agents
- Travel history, immunosuppression may point to more exotic pathogens including parasites
Board review style question #1
A 57 year old man with ulcerative colitis presents with 4 days of diarrhea and a
leukocytosis of 14,000 cells/μL two weeks after being treated for bacterial
sinusitis. The best laboratory test to diagnose his condition is:
- Anaerobic and aerobic bacterial culture
- Immunoassay for cytotoxin production
- Nucleic acid amplification testing (NAAT) targeted to toxin B and the CDT toxin of the suspected pathogen
- Stool examination for ova and parasites
Board review style answer #1
C. This patient has a recent history of antibiotic exposure and
ulcerative colitis, both risk factors for Clostridioides difficile infection (CDI).
Diarrhea with a high WBC and this history is strongly suggestive of active
CDI. Nucleic acid amplification testing (NAAT) is more sensitive than cytotoxin immunoassay and faster than
culture (turnaround ~1 hour). Rapid turnaround time is valuable when CDI is
suspected to guide isolation practices. The description does not indicate any clear risk factors for parasitic infection.
Comment Here
Reference: Clostridioides difficile
Comment Here
Reference: Clostridioides difficile
Board review style question #2
A patient with ulcerative colitis presented with diarrhea for 4 days after antibiotic treatment for sinusitis. NAAT and culture were performed. Gram stain showed the following:
After oral antibiotics, his diarrhea resolved, and his physicians want to repeat the NAAT as a test of cure. What do you recommend?
- Advocate against testing as bacterial DNA may persist after clinical symptoms resolve
- Advocate against testing because it is expensive
- Proceed with testing as a negative NAAT result can shorten the patient's antibiotic exposure
- Proceed with testing because a positive result should prompt fecal microbiota transplant
Board review style answer #2
A. This is Clostridioides difficile infection (CDI). Institutional guidelines are important to prevent repeat testing.
Bacterial DNA may persist longer than symptoms, thus proving a clinical
false positive result on nucleic acid amplification testing (NAAT) (albeit an analytical true positive result!).
Treatment is fairly protocolized with evidence based recommendations for
length of treatment. Fecal microbiota transplant is reserved for patients
with at least 2 recurrences of CDI who have failed medical therapy and
would not (yet) be indicated for this patient. In addition, a positive test after
only a few days of treatment would NOT constitute evidence of a
recurrence but most likely represents persistent C. difficile DNA in the
stool.
Comment Here
Reference: Clostridioides difficile
Comment Here
Reference: Clostridioides difficile






