Table of Contents
Definition / general | Essential features | Epidemiology | Sites | Pathophysiology | Clinical features | Laboratory | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Molecular / cytogenetics description | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Totten AH, Farr GA, Leal SM. M. pneumoniae. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/microbiologympneumoniae.html. Accessed April 23rd, 2024.
Definition / general
- Atypical bacterial pathogen, stained poorly by the dyes used in Gram stain due to the absence of a cell wall
- Taxonomy: class Mollicutes, order Mycoplasmatales, family Mycoplasmataceae
Essential features
- Common cause of community acquired pneumonia or walking pneumonia
- No cell wall; does not Gram stain
- Increasing rates of macrolide resistance (Clin Microbiol Rev 2017;30:747)
Epidemiology
- Leading bacterial cause of community acquired pneumonia; ~ 2 million cases/year in the U.S. (Clin Microbiol Rev 2004;17:697)
- Predominately affects children between 5 - 18 years old
- Disseminated infections in immunocompromised individuals
- Rapid spread via droplet contact and close community conditions (i.e. prisons, dormitories, barracks, etc.)
- As immunity wanes, cyclic increases in infection rates occur ~ 3 - 7 years
Sites
- Lung / atypical walking pneumonia (Clin Microbiol Rev 2017;30:747)
- Throat / upper respiratory tract / tracheobronchitis
- Disseminated infection
- Central nervous system complications (encephalitis), dermatologic manifestations, joint infections, bacteremia
Pathophysiology
- Adhesin, attachment to host cell vital for pathogenesis, initiation of infection (Clin Microbiol Rev 2004;17:697)
- Community acquired respiratory distress syndrome toxin mediates acute infection (Clin Microbiol Rev 2017;30:747)
- Lacks cell wall, therefore not susceptible to beta lactams
- Lipoproteins are main immunogens for immunologic responses
- Macrolide resistance increasing in U.S. (8 - 10%) and other parts of world (> 90% Japan, China), no widely known quinolone or tetracycline resistance reported
Clinical features
- Usually associated with mild disease but can develop serious complications, such as pneumonia, asthma attacks, hemolytic anemia and other organ system involvement
- Associated with I antigen positive on red blood cell cross match
- Can lead to immune mediated sequelae including Stevens-Johnson syndrome, cold agglutinins (I antigen)
- Coinfections are common (~ 20%); most commonly rhinovirus and enterovirus (N Engl J Med 2015;372:2167)
Laboratory
- Does not stain on Gram stain
- Requires special culture media which contain serum that provides fatty acids and cholesterol for mycoplasma membrane synthesis
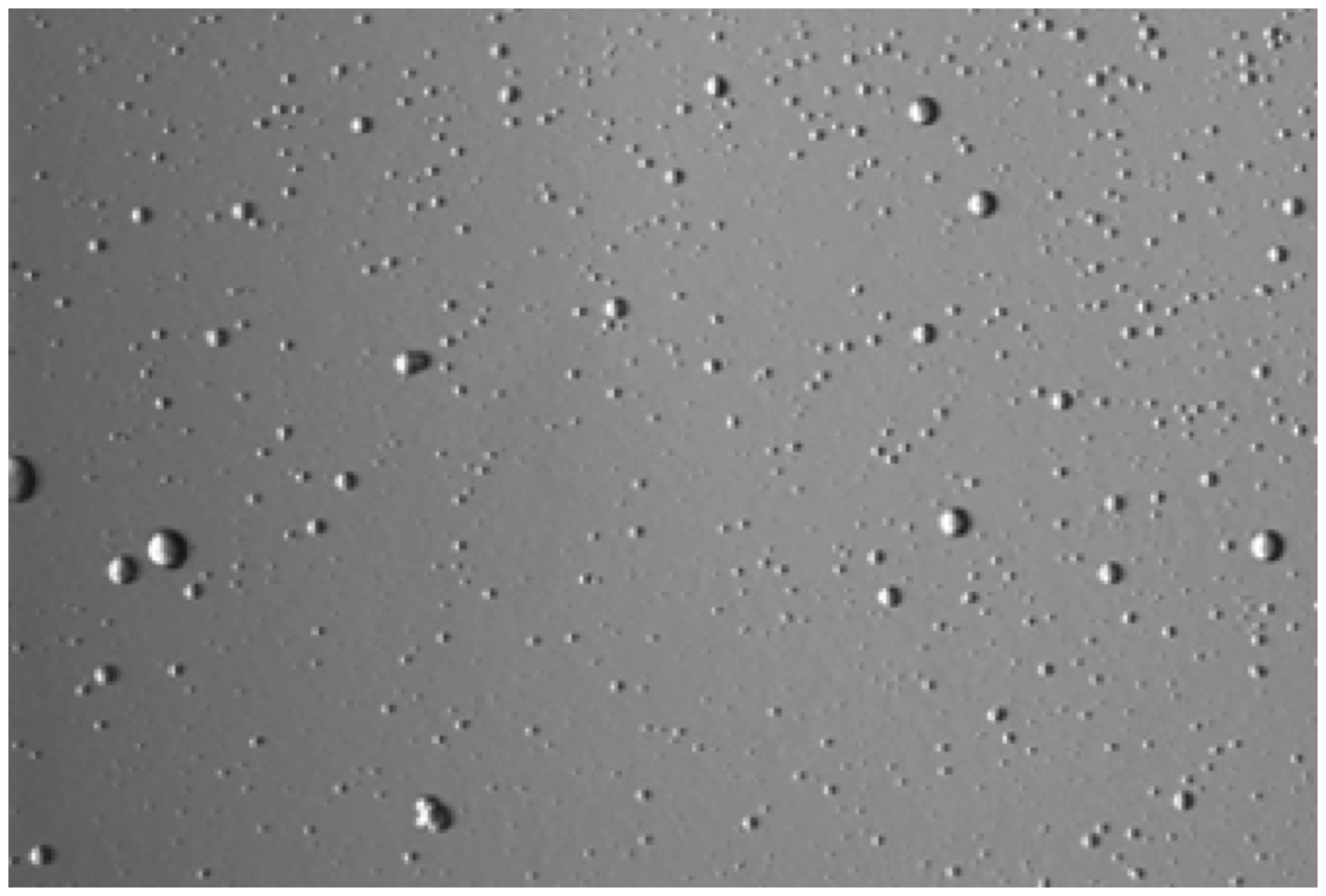
- Forms small, colorless, punctate colonies (dissection scope needed) on SP4 agar within 5 - 14 days when cultured aerobically at 37°C (Clin Microbiol Rev 2004;17:697)
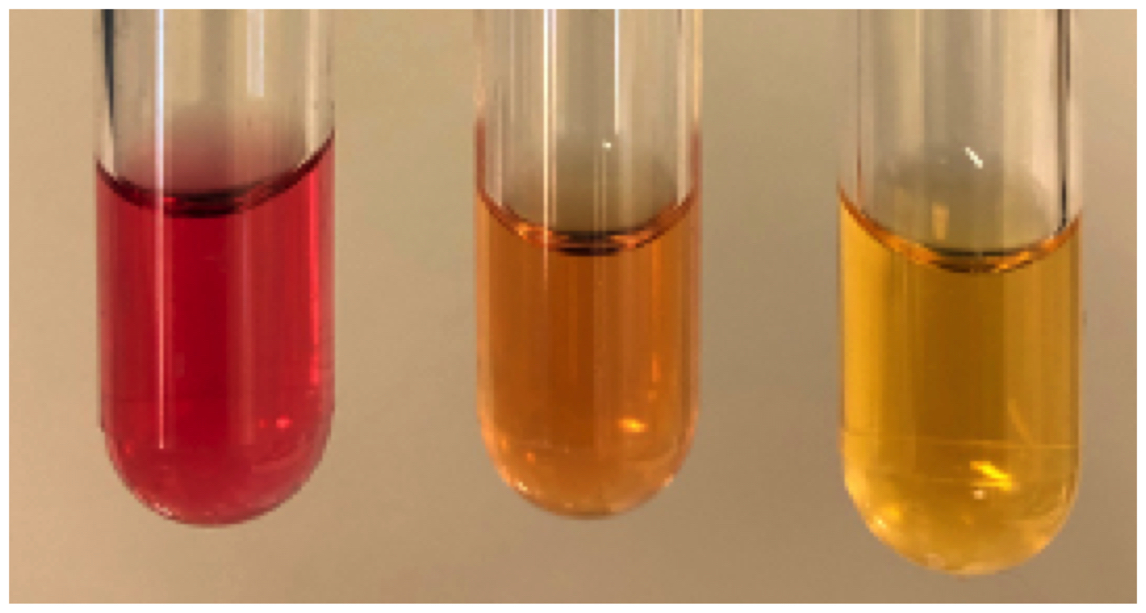
- Color change in liquid media due to glucose metabolism (red to yellow) is characteristic
- PCR testing (nucleic acid amplification) required to differentiate from other glucose utilizing mycoplasmas
- Serology testing performs poorly with respect to sensitivity and specificity (< 70 - 80%) for M. pneumoniae
- When utilized, acute and convalescent sera are vital, as antibodies persist in previously exposed hosts
- Acute sera is not sufficient for patient diagnosis
- Combination of paired sera and others methods has been shown to be potentially useful in acute diagnosis but not as accurate or sensitive as molecular (e.g. PCR) based detection (Eur J Clin Microbiol Infect Dis 2011;30:439)
Case reports
- Pediatric patient with acute lymphoblastic leukemia and M. pneumoniae carriage with reemergent, drug resistant pneumonia (Pediatrics 2019;144:e20191642)
- 6 year old child with severe M. pneumoniae pneumonia (J Paediatr Child Health 2019;55:107)
- 33 year old man with neurologic complications from M. pneumoniae infection (Respir Med Case Rep 2019;27:100859)
- 39 year old woman with macrolide resistant M. pneumoniae infection (BMC Infect Dis 2019;19:204)
- 39 year old man with meningoencephalitis secondary to disseminated M. pneumoniae infection (BMJ Case Rep 2018;2018:bcr-2017-221831)
Treatment
- Most can recover with medication; however, antibiotics are usually prescribed when pneumonia develops (Centers for Disease Control and Prevention: Mycoplasma pneumoniae Infections - Treatment and Complications [Accessed 26 May 2020])
- Pediatric patients mostly treated with the macrolide azithromycin (Z-pak)
- Adults can be treated with macrolides, quinolones or tetracyclines
- Empiric treatment is common but up to 7 - 10% of U.S. isolates are macrolide resistant (J Clin Microbiol 2019;57:e00968)
Clinical images
Microscopic (histologic) description
- M. pneumoniae is not visualized on H&E or other histologic stains (Carroll: Manual of Clinical Microbiology, 12th Edition, 2019)
- 16S sequencing may be helpful to identify M. pneumoniae infection in FFPE tissues
- Immunologic patterns consistent with infection include: acute peribronchial neutrophilic infiltrates and chronic lymphoplasmacytic inflammation with pneumocyte hyperplasia and intraalveolar proteinaceous material
- Organisms can be visualized by electron microscopy
Molecular / cytogenetics description
- Most FDA approved multiplex respiratory pathogen panels target M. pneumoniae (J Clin Microbiol 2018;56:e01658)
- PCR is the most common and accurate means of diagnosis:
- PCR for adhesin or high copy genomic targets are the most accurate (P1 adhesin, repMp1 genomic repeat regions, CARDS toxin) (J Clin Microbiol 2007;45:2726, J Clin Microbiol 2019;57:e00287, Methods Mol Biol 2013;943:149)
- Macrolide resistance can be determined in specialized laboratories via PCR (23S rRNA PCR), Sanger sequencing or antimicrobial susceptibility testing (UAB Research: Diagnostic Mycoplasma Lab [Accessed 20 March 2020]), Pediatr Infect Dis J 2009;28:693)
Differential diagnosis
- Viral respiratory infection:
- Influenza, parainfluenza, adenovirus and human metapneumovirus
- Atypical bacterial infections:
- Chlamydia pneumoniae
- Legionella pneumophila
Board review style question #1
- A pediatric patient has presented to an outpatient clinic with persistent cough and fever. All typical microbiologic tests return no identifiable agent and empiric diagnosis with Mycoplasma pneumoniae is made. What is the main class of antibiotic for adequate treatment of this pathogen?
- Cephalosporins
- Macrolide
- Penicillin
- Tetracycline
Board review style answer #1
B. Macrolides are the main means of treatment for M. pneumoniae in pediatric patients, as tetracyclines and quinolones are contraindicated in this patient population. Macrolide resistance is increasing and drug options may be limited in the near future.
Comment Here
Reference: M. pneumoniae
Comment Here
Reference: M. pneumoniae
Board review style question #2
- A patient with immunodeficiency has reported pain in a knee joint and inflammation upon usage of the limb. Previous pulmonary infection had been reported without an identifiable pathogen on typical microbiologic media / culturing. Synovial fluid analysis additionally revealed no pathogens upon Gram stain analysis. What pathogen is the most likely cause of this disseminated infection?
- Chlamydia pneumoniae
- Clostridium perfringens
- Mycoplasma pneumoniae
- Staphylococcus aureus
Board review style answer #2
C. Mycoplasma pneumoniae spreads from the lungs to various tissues, particularly in immunocompromised individuals, causing syndromes like septic arthritis. C. pneumoniae is rare and not known to cause significant systemic disease. C. perfringens and S. aureus would be detected as on Gram stain.
Comment Here
Reference: M. pneumoniae
Comment Here
Reference: M. pneumoniae