Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Holloman AM, Mohila CA. Polymyositis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/musclepolymyositis.html. Accessed April 25th, 2024.
Definition / general
- Very rare idiopathic inflammatory myopathy; often overdiagnosed (Neurology 2003;61:316)
- Many cases previously diagnosed as polymyositis may be classified as dermatomyositis, inclusion body myositis, immune mediated necrotizing myopathy or antisynthetase syndrome based on serologic testing for myositis specific autoantibodies (J Neuromuscul Dis 2015;2:13, JAMA Neurol 2018;75:1528, Curr Opin Neurol 2019;32:704)
- Existence of polymyositis as a distinct entity has been questioned and may not be included in some idiopathic inflammatory myopathy classification systems (JAMA Neurol 2018;75:1528, Rheumatol Int 2015;35:915)
Essential features
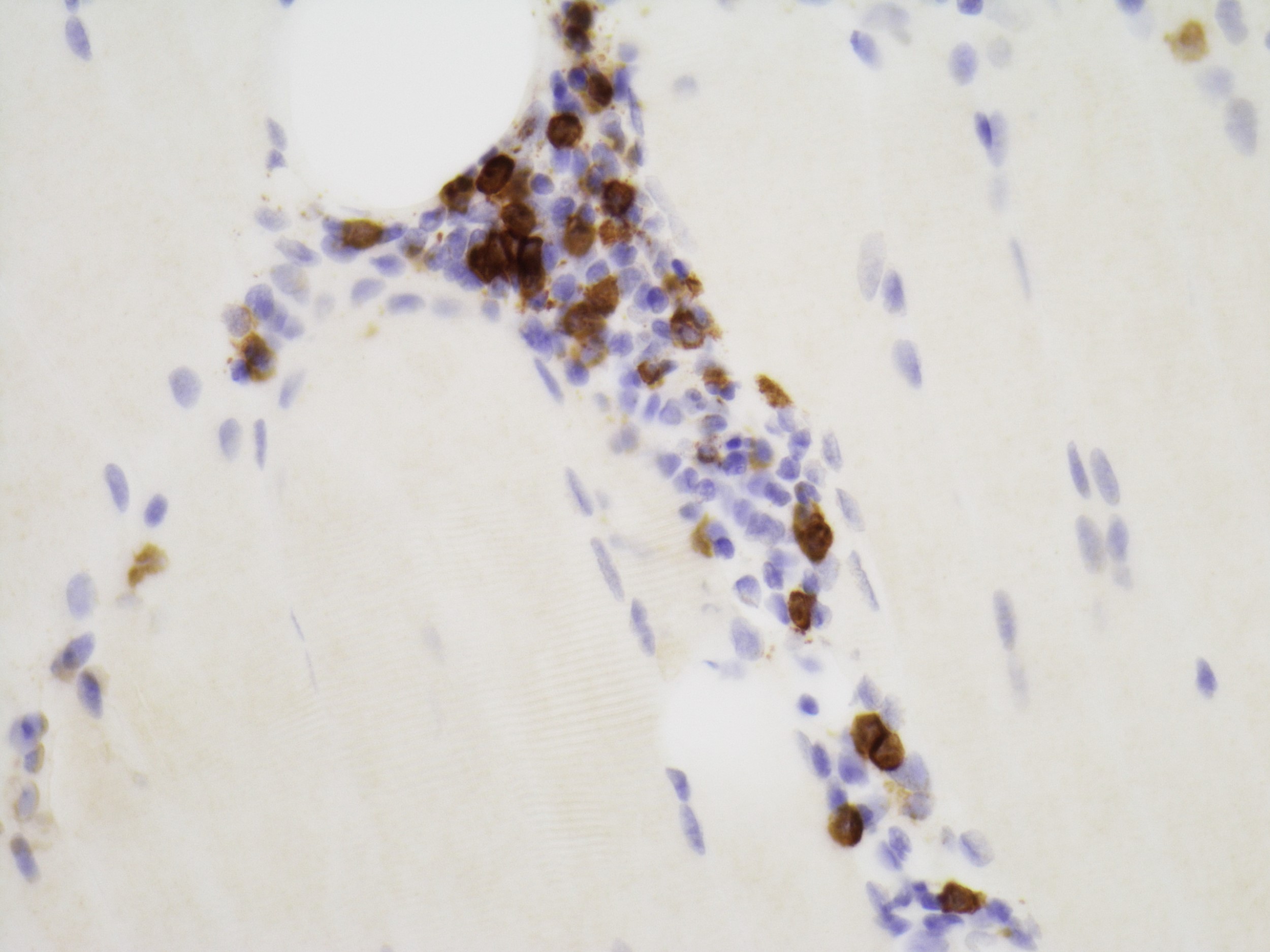
- Myopathic features with endomysial inflammatory infiltrate of predominantly CD8+ T cells surrounding and invading nonnecrotic muscle fibers expressing MHC I antigen (J Neuromuscul Dis 2018;5:109)
- Diagnosis of exclusion made after all other inflammatory disorders have been ruled out, including other idiopathic inflammatory myopathies (dermatomyositis, inclusion body myositis, antisynthetase syndrome and immune mediated necrotizing myopathy), toxin / drug induced myopathies and muscular dystrophies
Terminology
- Polymyositis, idiopathic inflammatory polymyositis, idiopathic polymyositis, pure polymyositis
ICD coding
Epidemiology
- Incidence of 3.8 per 100,000 in U.S. (J Neuromuscul Dis 2018;5:109, Muscle Nerve 2012;45:676)
- < 5% of all inflammatory myopathies (Arthritis Rheumatol 2017;69:878)
- Predominantly affects adults (N Engl J Med 2015;372:1734)
- More common in women
Sites
- Predominantly affects proximal muscles of the extremities (N Engl J Med 2015;372:1734)
Pathophysiology
- Clonal expansion of CD8+ T cells that expand and destroy myocytes via perforin and granzyme B (Rheum Dis Clin North Am 2011;37:159)
Etiology
- Exact etiology unknown
- Known association with human leukocyte antigen (HLA) DRB1*03:01 and HLA-B*08:01 (Ann Rheum Dis 2016;75:1558)
- PTPN22 gene single nucleotide polymorphisms (SNPs) associated with increased susceptibility to development of polymyositis (Muscle Nerve 2017;55:270, Ann Rheum Dis 2016;75:1558)
Clinical features
- Subacute onset of proximal muscle weakness
- Extramuscular manifestations include systemic symptoms (e.g. fever, weight loss) and Raynaud phenomenon
- May be associated with other connective tissue disorders such as rheumatoid arthritis and Sjögren syndrome
- May also be associated with cardiac and pulmonary dysfunction including arrhythmias and interstitial lung disease, respectively
- References: Lancet 2003;362:971, Clin Exp Rheumatol 2014;32:188, RMD Open 2017;3:e000507
Diagnosis
- Diagnosis of exclusion after other inflammatory myopathies have been ruled out
- Diagnosis of definite polymyositis requires the demonstration of CD8+ lymphocytes surrounding and invading nonnecrotic muscle fibers that express MHC class I antigen in the absence of rimmed vacuoles (Neuromuscul Disord 2015;25:268, Neuromuscul Disord 2004;14:337)
- In the absence of endomysial inflammation, a diagnosis of probable polymyositis can be made if there is ubiquitous expression of MHC class I antigen, in the absence of rimmed vacuoles and dystrophic changes (Neuromuscul Disord 2015;25:268, Neuromuscul Disord 2004;14:337)
- The European League Against Rheumatism / American College of Rheumatology (EULAR / ACR) Classification criteria may clinically help distinguish major subgroups of idiopathic inflammatory myopathies and distinguish them from mimicking conditions (Arthritis Rheumatol 2017;69:2271)
- Score based on age of onset, muscle weakness, skin manifestations, dysphagia or esophageal dysmotility, laboratory measurements (anti-Jo1 autoantibodies; elevated serum creatine kinase [CK], lactate dehydrogenase [LDH], aspartate aminotransferase [AST] or alanine aminotransferase [ALT]), with or without muscle biopsy findings
Laboratory
- Elevated creatine kinase (CK) and aldolase
- Elevated aspartate aminotransferase (AST) and alanine aminotransferase (ALT)
- Elevated lactate dehydrogenase (LDH)
- Positive human leukocyte antigen (HLA) DRB1*03:01 and HLA-B*08:01 haplotypes (Ann Rheum Dis 2016;75:1558)
- References: Lancet 2003;362:971, Clin Exp Rheumatol 2014;32:188, RMD Open 2017;3:e000507
Radiology description
- T2 weighted MRI may show muscle edema and fatty infiltration (Mod Rheumatol 2018;28:913)
Prognostic factors
- 10 year survival rate of 90% (Clin Exp Rheumatol 2014;32:188)
- Age > 60 and malignancy are associated with worse survival (Mod Rheumatol 2016;26:115)
- 1 study found that intravenous corticosteroid use was associated with worse prognosis when compared to oral corticosteroids, likely secondary to disease severity (Arthritis Res Ther 2012;14:R22)
Case reports
- 51 year old man with polymyositis presenting with acute heart failure and rhabdomyolysis (Reumatismo 2017;69:78)
- 54 year old man with concomitant polymyositis, myasthenia gravis and aplastic anemia treated with bone marrow transplantation (Case Rep Neurol 2018;10:108)
- 73 year old woman with polymyositis and elevated serum IgG4 (Medicine (Baltimore) 2017;96:e8710)
Treatment
- Oral glucocorticosteroids are first line therapy
- Intravenous (IV) steroids, immunosuppressants, intravenous immunoglobulin (IVIG) and immunomodulators may be considered in cases which do not respond to initial therapy (Arthritis Rheumatol 2018;70:1532)
Gross description
- Skeletal muscle usually submitted as 1 large piece but may also be submitted in small, multiple pieces
- Gross findings are nonspecific
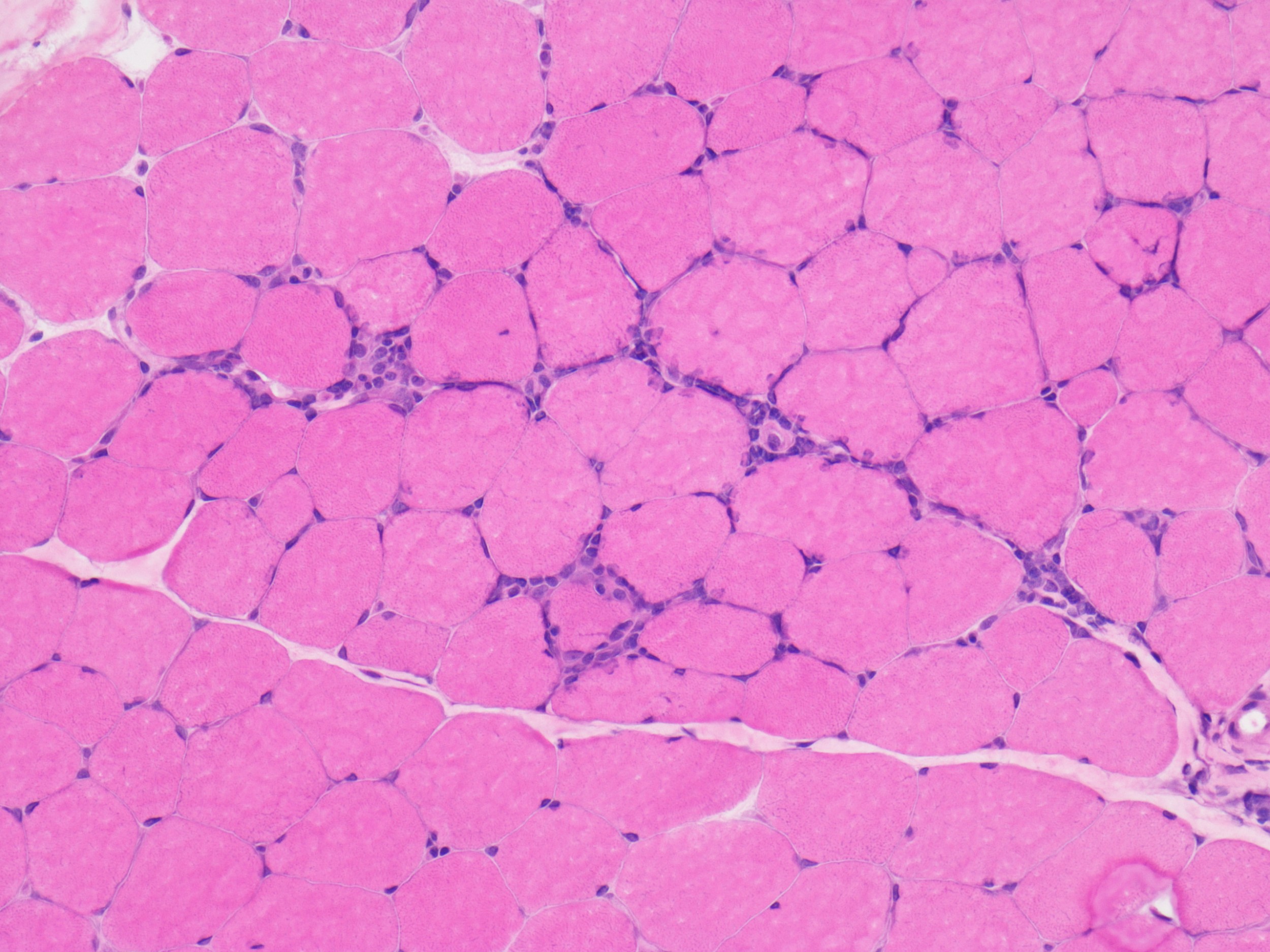
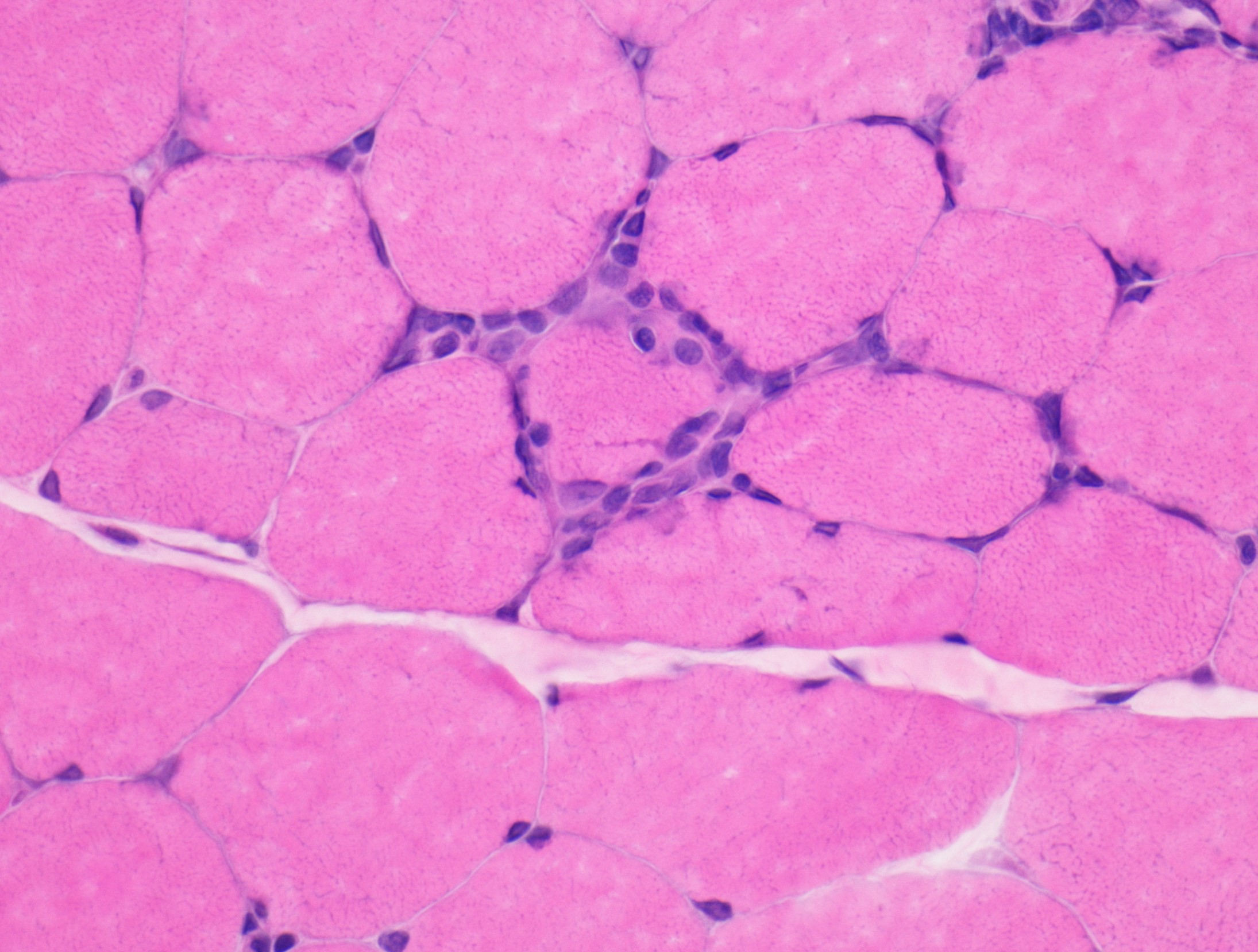
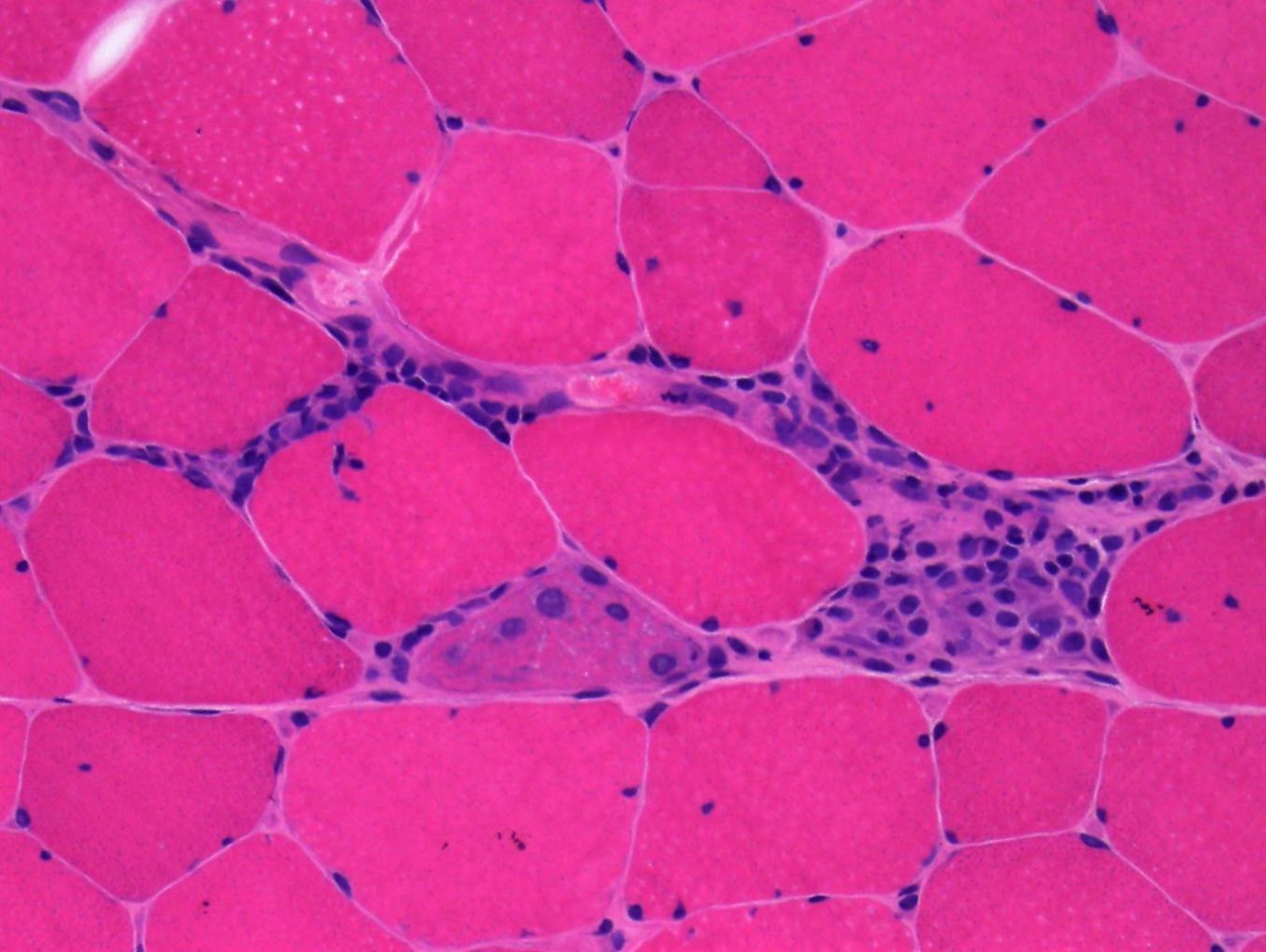
Microscopic (histologic) description
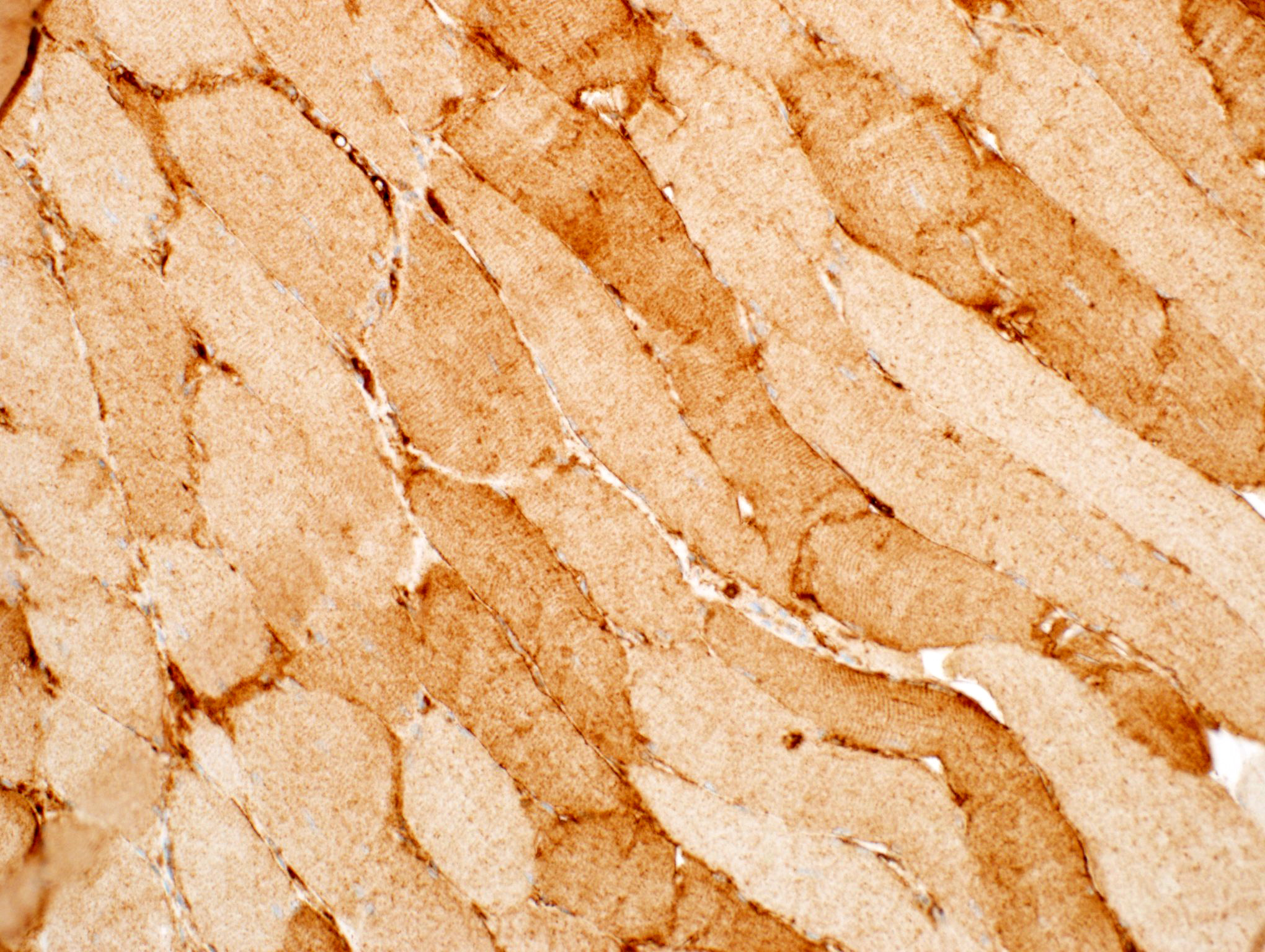
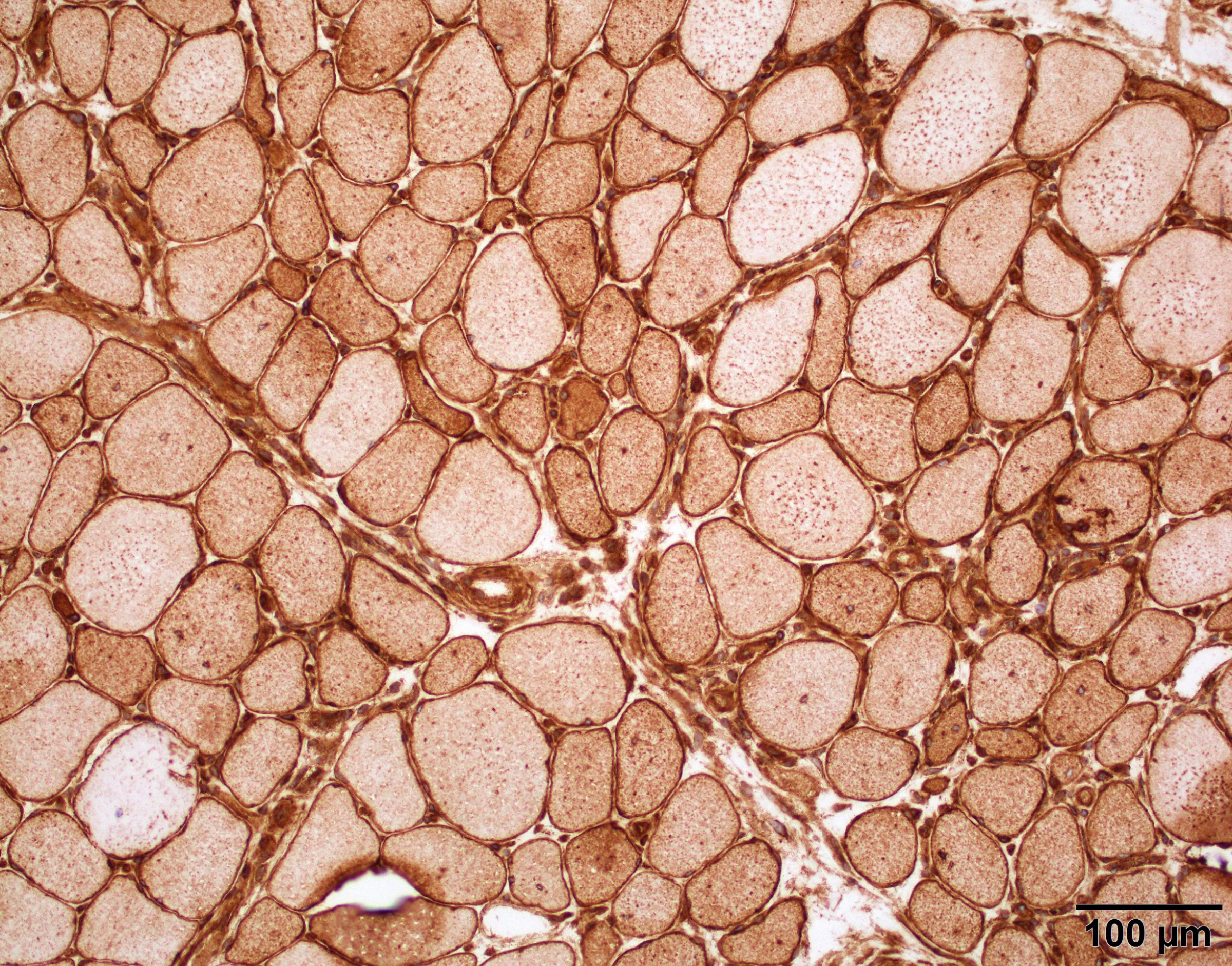
- Myopathic changes including myofiber size variation with small rounded myofibers and increased internalized nuclei
- Endomysial lymphocytic inflammation surrounding and invading nonnecrotic myofibers
- Lymphocytic infiltrate may be accompanied by macrophages
- Degenerating and basophilic regenerating myofibers with large nuclei with prominent nucleoli
- May see rare necrotic myofibers with phagocytosis
- Lacks perifascicular atrophy
- Lacks rimmed vacuoles
- References: Lancet 2003;362:971, Clin Exp Rheumatol 2014;32:188, RMD Open 2017;3:e000507
Microscopic (histologic) images
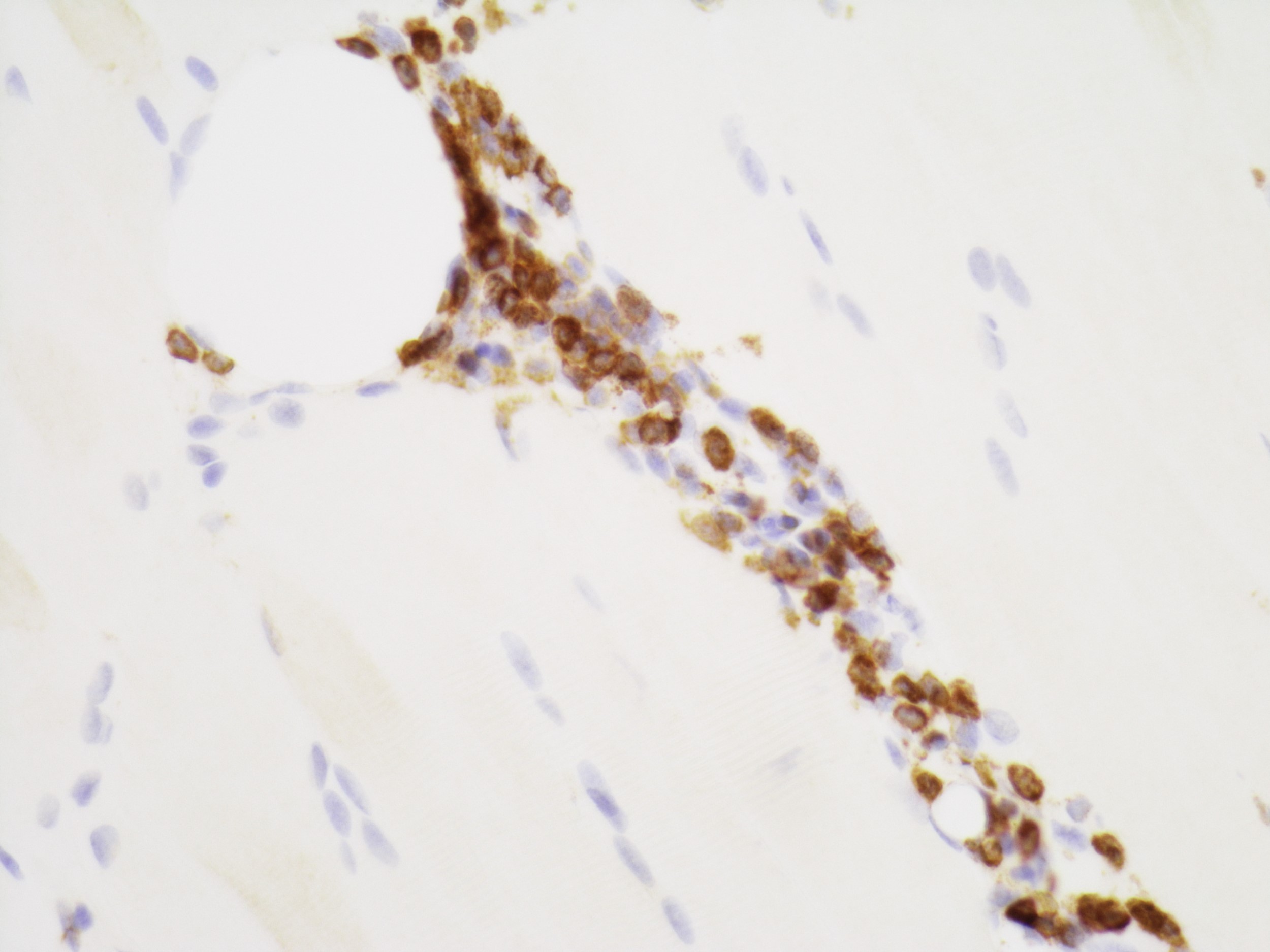
Positive stains
- CD3+, CD8+ T lymphocytes
- Myofibers with sarcolemmal and sarcoplasmic immunostaining for MHC class I antigen (nonspecific)
- References: Lancet 2003;362:971, Clin Exp Rheumatol 2014;32:188, RMD Open 2017;3:e000507
Negative stains
- No rimmed vacuoles identified on Gomori trichrome
- No loss of dystrophy associated proteins (e.g. dystrophin) on immunohistochemistry
- Absence of C5b9 (terminal complement complex / membrane attacking complex) on capillaries or sarcolemma of nonnecrotic fibers (Neuromuscul Disord 2004;14:337)
- References: Lancet 2003;362:971, Clin Exp Rheumatol 2014;32:188, RMD Open 2017;3:e000507
Electron microscopy description
- Lack of rimmed vacuoles and tubuloreticular inclusions
Sample pathology report
- Skeletal muscle, left vastus lateralis, biopsy:
- Inflammatory myopathy compatible with polymyositis (see comment)
- Comment: This biopsy shows myopathic changes associated with a lymphocytic inflammatory infiltrate of CD8 positive T cells invading nonnecrotic muscle fibers that express MHC class I antigens. There is no evidence of perifascicular atrophy, capillary loss or tubuloreticular inclusions on electron microscopy to suggest dermatomyositis. Rimmed vacuoles are not present. There are no dystrophic features. In the correct clinical setting, this biopsy is compatible with polymyositis. Correlation of biopsy findings with clinical features and myositis specific autoantibodies is required to exclude other idiopathic inflammatory myopathies.
Differential diagnosis
- Inclusion body myositis:
- Endomysial CD8+ lymphocytic inflammatory infiltrate
- Rimmed vacuoles present on H&E and Gomori trichrome
- Does not respond to typical steroid or immunosuppressive treatments as seen in other myopathies
- May show tau, p62, alpha synuclein and amyloid beta positive immunohistochemistry staining (Acta Neuropathol 2009;118:407, Presse Med 2011;40:e219, J Neuropathol Exp Neurol 2012;71:680)
- Immune mediated necrotizing myopathy:
- Necrotic and regenerating myofibers
- Minimal lymphocytic infiltration
- Associated with autoantibodies including anti-SRP, anti-HMGCR; may also be negative for autoantibodies
- p62+ myofibers may be present (Muscle Nerve 2019;60:315)
- Drug induced myopathy:
- Statin induced myopathy may show similar histologic findings to polymyositis
- Review of medications is required
- Dermatomyositis (Lancet Neurol 2018;17:816):
- Often associated with skin rash (heliotrope rash) or Gottron papules (CMAJ 2013;185:148)
- Perivascular and perimysial B cell lymphocytic inflammatory infiltrate
- Perifascicular atrophy is characteristic
- Tubuloreticular inclusions in vascular endothelial cells on electron microscopy
- Associated with dermatomyositis specific autoantibodies including Mi2, TIF1y, NXP2, MDA5 or SAE
Additional references
Board review style question #1
Which of the following statements is true regarding the skeletal muscle biopsy image shown above?
- CD20+ B cells are the predominant inflammatory component
- CD8+ T cells are the predominant inflammatory component
- Histologic findings are classic for dermatomyositis
- IVIG is the first line therapy
- Presence of rimmed vacuoles favors polymyositis
Board review style answer #1
Board review style question #2
Which of the following statements is true regarding the diagnosis of polymyositis?
- Histologic findings alone are characteristic and diagnostic of disease
- Patients often present with skin rash
- Polymyositis is a diagnosis of exclusion
- Polymyositis is associated with a specific autoantibody
- Sarcolemmal staining for MHC class I antigen is specific for polymyositis
Board review style answer #2