Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Lai J. Sinonasal glomangiopericytoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/nasalHPC.html. Accessed April 24th, 2024.
Definition / general
- Uncommon soft tissue tumor of perivascular myoid differentiation with hemangiopericytoma-like vasculature
Essential features
- Also called glomangiopericytoma, sinonasal type
- Nasal cavity is usually affected, present with nasal obstruction, mass, epistaxis and sinusitis
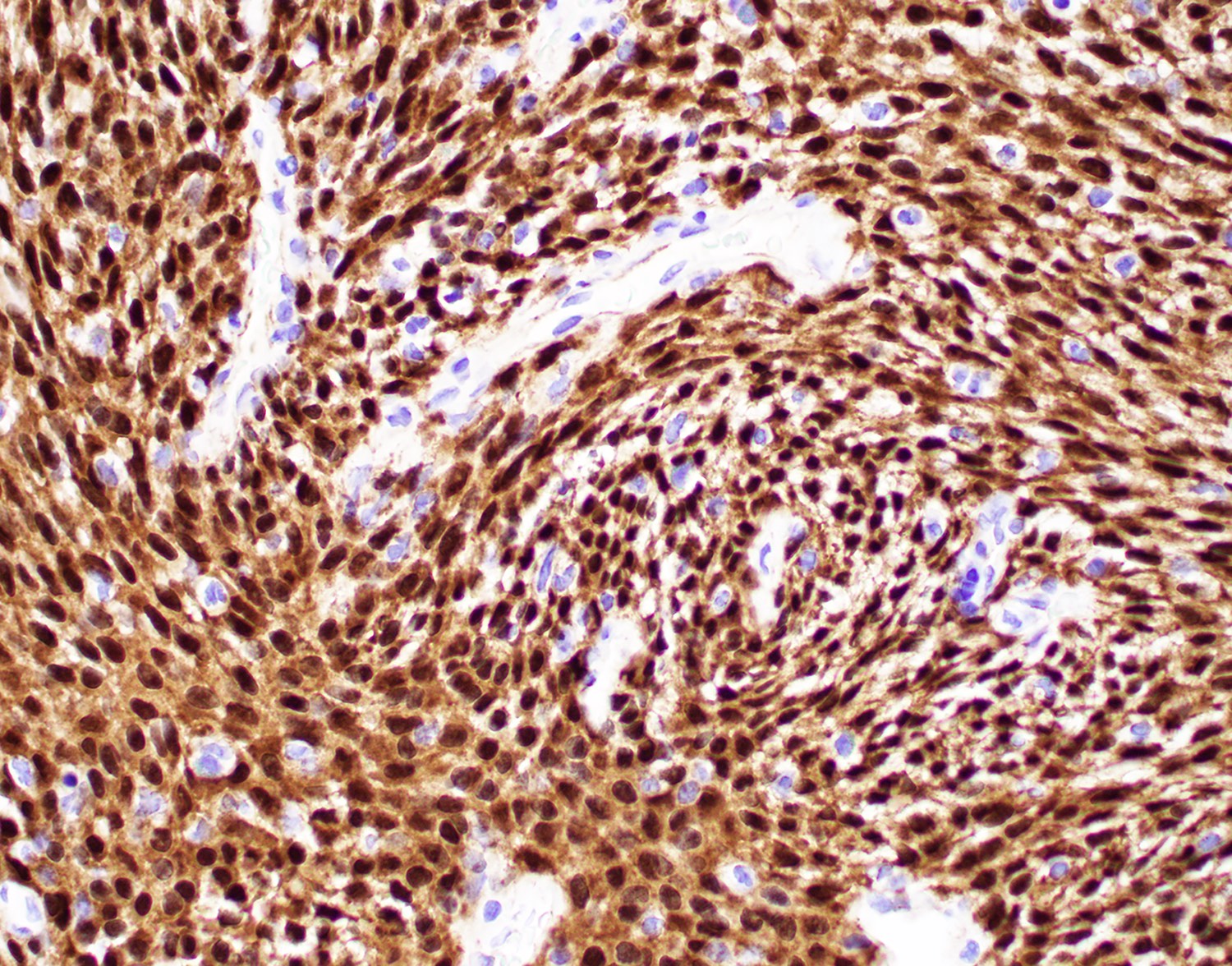
- CTNNB1 mutation with beta catenin oncogenic activation (beta catenin nuclear staining on IHC) (Head Neck Pathol 2019;13:298, Yale J Biol Med 2021;94:593)
- Excellent long term outcome with surgery alone, recurrence rate ~27%
Terminology
- Previous name: sinonasal type hemangiopericytoma
- Glomus tumor
- Intranasal myopericytoma
ICD coding
- ICD-10: D38.5 - neoplasm of uncertain behavior of other respiratory organs
Epidemiology
- Rare, comprising < 0.5% of sinonasal primary neoplasms (Thompson: Diagnostic Pathology - Head and Neck, 2nd Edition, 2016)
- Broad age range (5 - 90 years); mean in seventh decade
- F > M (1.2:1)
- No difference in outcome based on gender after surgery
Sites
- Nasal cavity is usually affected, turbinate and septum occasionally affected in isolation (Thompson: Diagnostic Pathology - Head and Neck, 2nd Edition, 2016)
- Maxillary and ethmoid sinuses may also be affected in conjunction with nasal cavity
- Bilateral tumor uncommon (~5%)
Pathophysiology
- May arise from pericytes associated with vessels of nasal cavity
- Mutational activation of beta catenin (Head Neck Pathol 2019;13:298, Yale J Biol Med 2021;94:593)
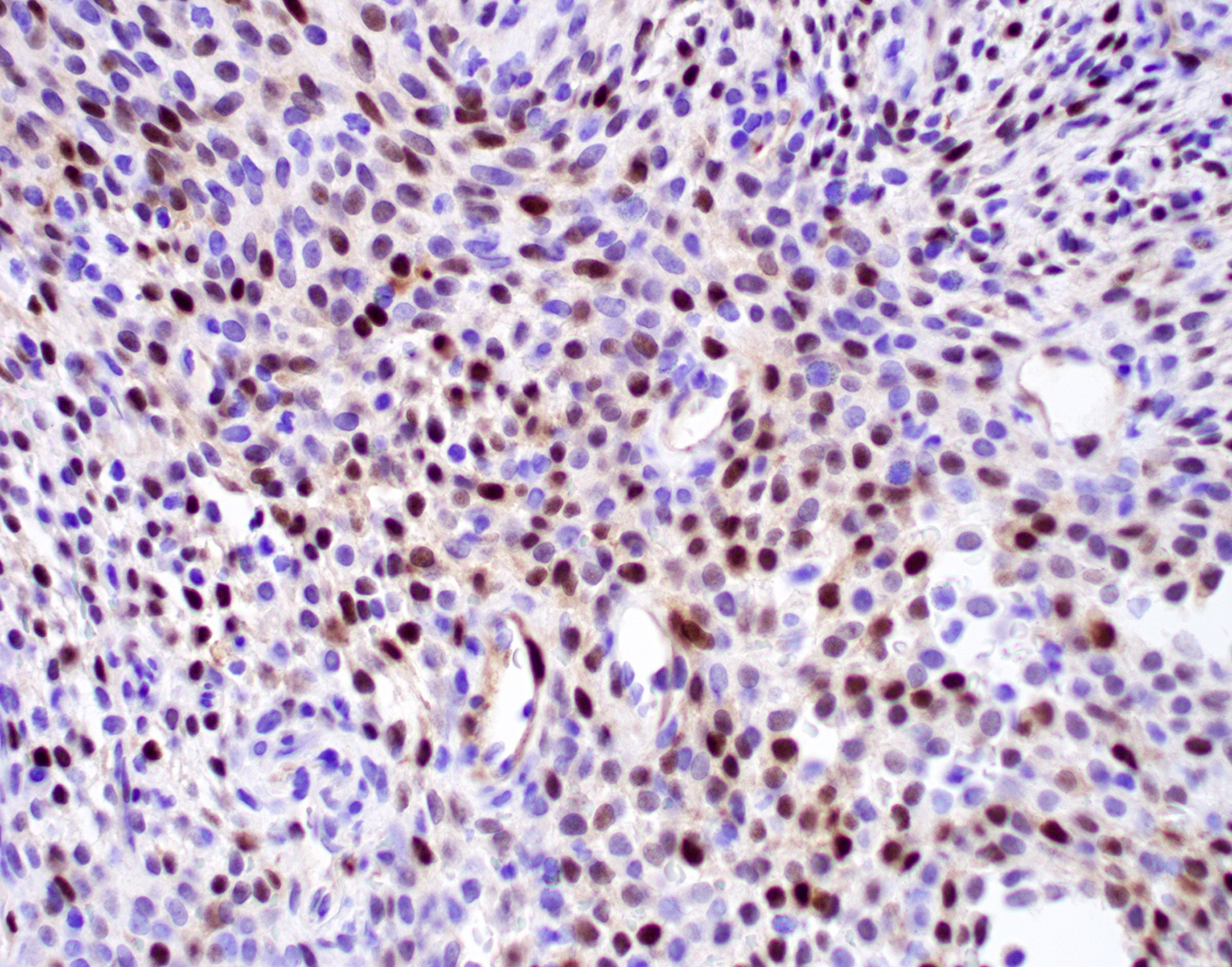
- Associated with cyclin D1 overexpression (Pathol Res Pract 2019;215:983)
Etiology
- CTNNB1 mutations
Clinical features
- Nasal obstruction, mass, polyps, difficulty breathing
- Sinusitis, discharge, change in smell
- Nasal bleeding (J Pak Med Assoc 2020;70:2469)
- Headache
- Rare association with oncogenic osteomalacia (BMC Endocr Disord 2022;22:31)
Diagnosis
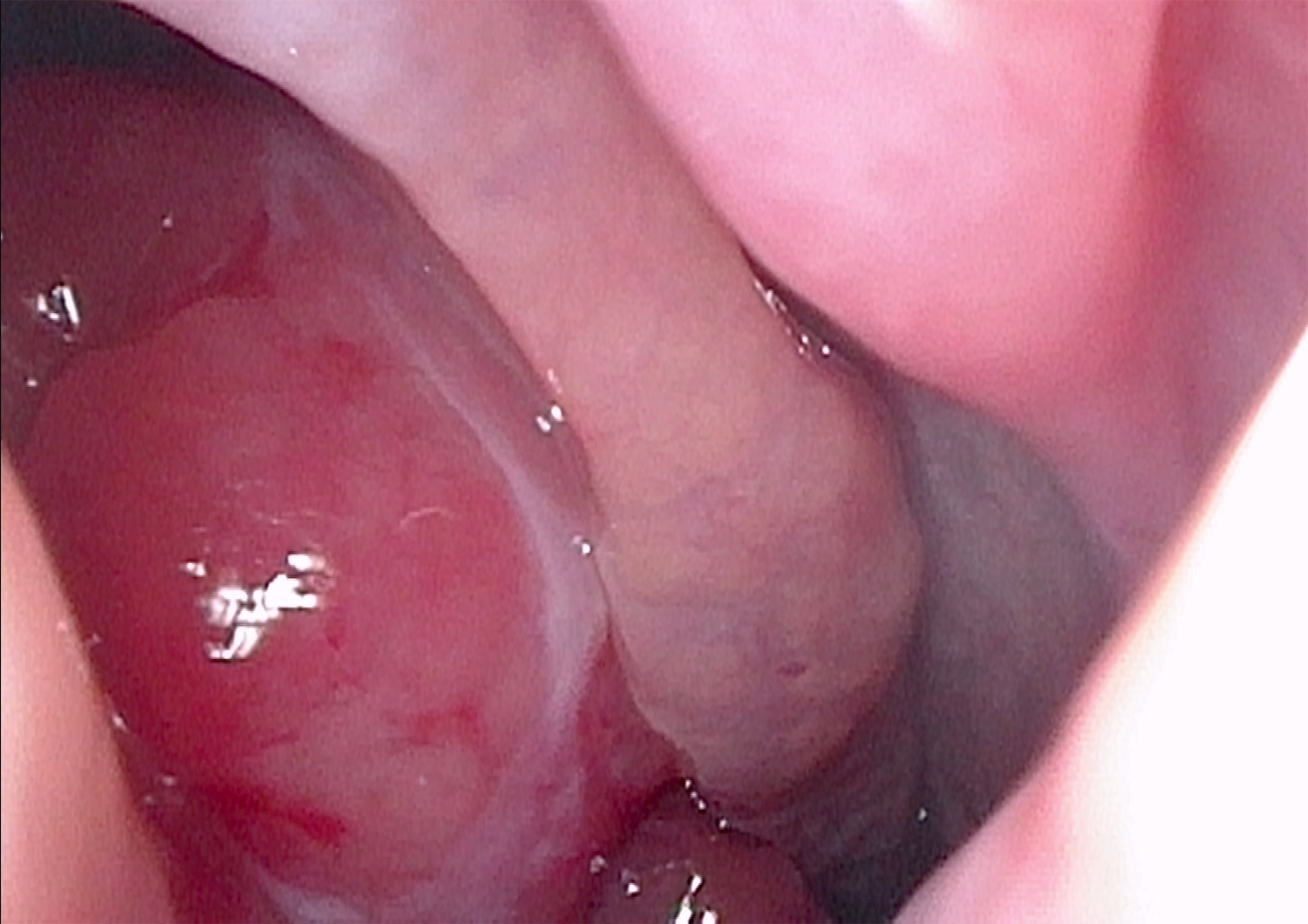
- Clinical symptoms and polypoid mass identified in the nasal cavity
- CT and MRI showing a polypoid mass of nasal cavity (paranasal sinus) accompanied with bone erosion or sclerosis
- Biopsy showing soft tissue with perivascular myoid differentiation, positive for beta catenin nuclear staining, cyclin D1 and SMA, negative for vascular markers in the tumor cells (Pathol Res Pract 2019;215:983)
Laboratory
- In the majority of cases, lab tests do not help
- In rare cases, associated with osteomalacia: serum hypophosphatemia and elevated alkaline phosphatase (BMC Endocr Disord 2022;22:31)
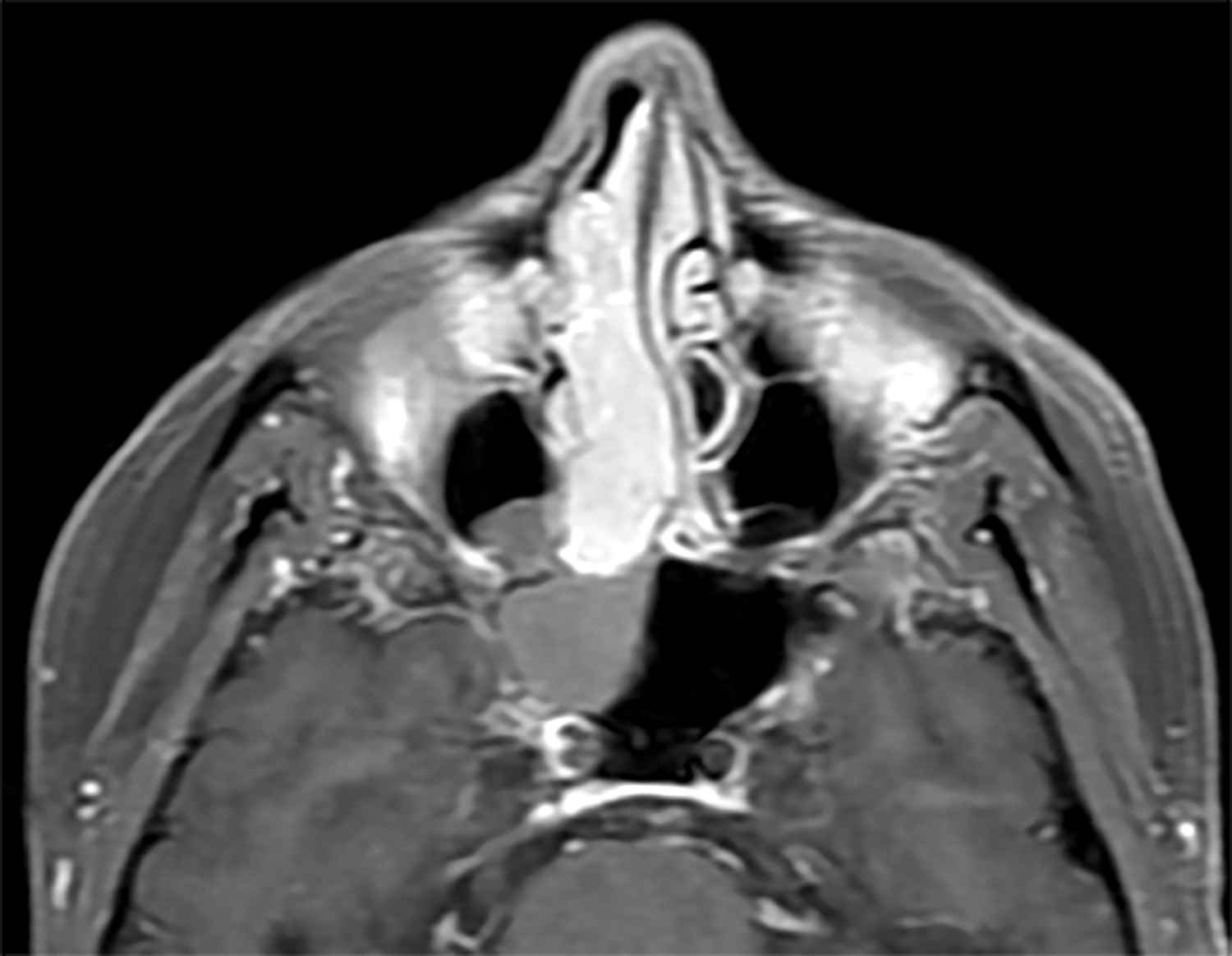
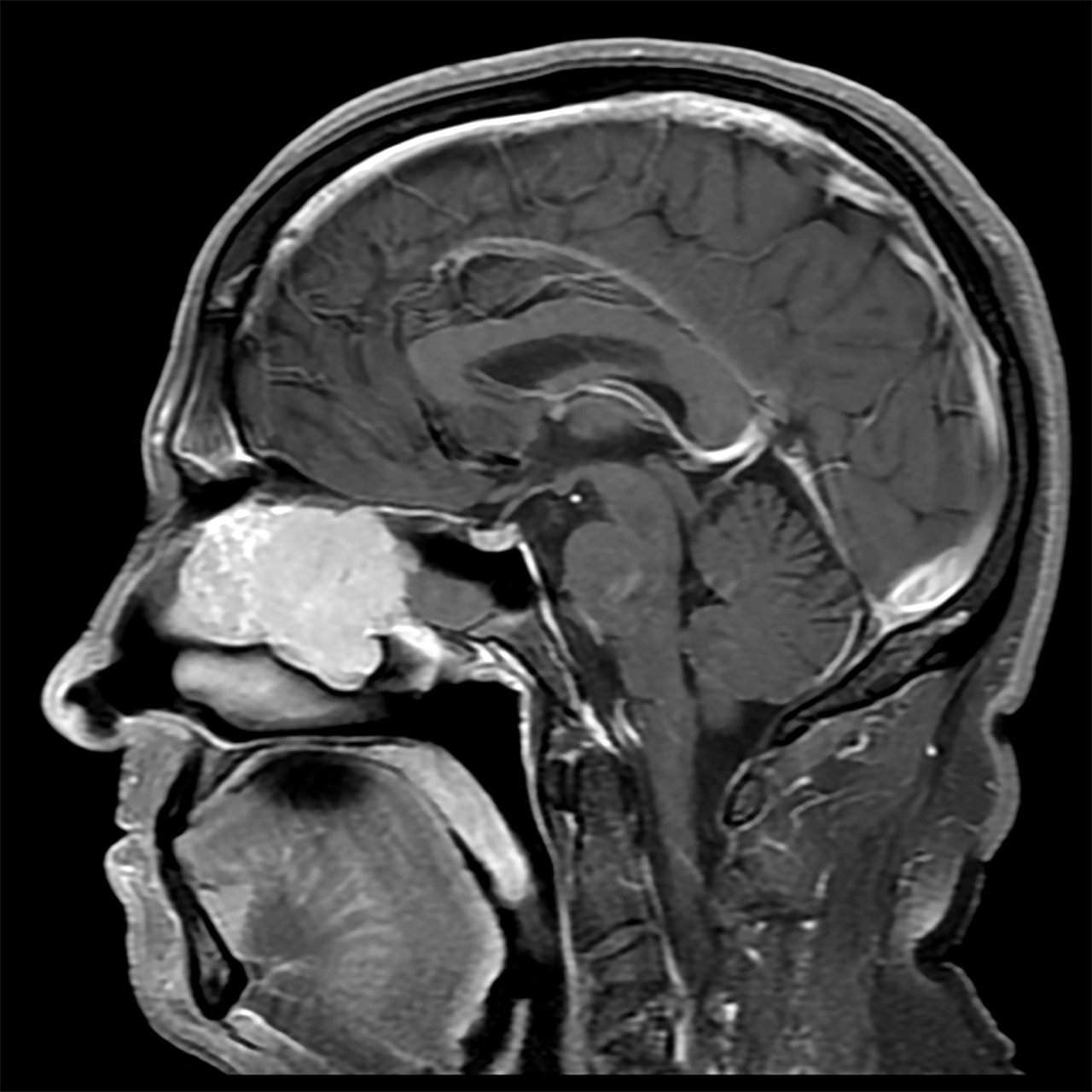
Radiology description
- CT and MRI showing a mass of nasal cavity (paranasal sinus), could be lobulated
Radiology images
Prognostic factors
- Excellent prognosis after surgery (5 year survival ~90%)
- Recurrence rate ~27%, long term clinical follow up advocated as recurrences may develop late (Thompson: Diagnostic Pathology - Head and Neck, 2nd Edition, 2016)
- Recurrences are associated with long duration of the symptoms, bone invasion and profound nuclear pleomorphism
Case reports
- 42 year old woman with osteomalacia caused by sinonasal glomangiopericytoma and coexisting parathyroid adenoma (BMC Endocr Disord 2022;22:31)
- 57 year old man with sinonasal FUS::ERG rearranged Ewing sarcoma mimicking glomangiopericytoma (Case Rep Oncol 2020;13:1393)
- 60 year old man with new onset, right arm and leg weakness / numbness, was found to have a left ethmoid sinus glomangiopericytoma with extension in the olfactory fossa (Yale J Biol Med 2021;94:593)
- 70 year old man with nasal blockage and epistaxis underwent endoscopic sinus surgery (J Pak Med Assoc 2020;70:2469)
- 74 year old man with a reddish nasal mass with CTNNB1 p.S37C mutation (Head Neck Pathol 2019;13:298)
Treatment
- Surgery (polypectomy or wide surgical resection) is the treatment of choice (J Pak Med Assoc 2020;70:2469)
- Radiation could be used for nonsurgical candidates
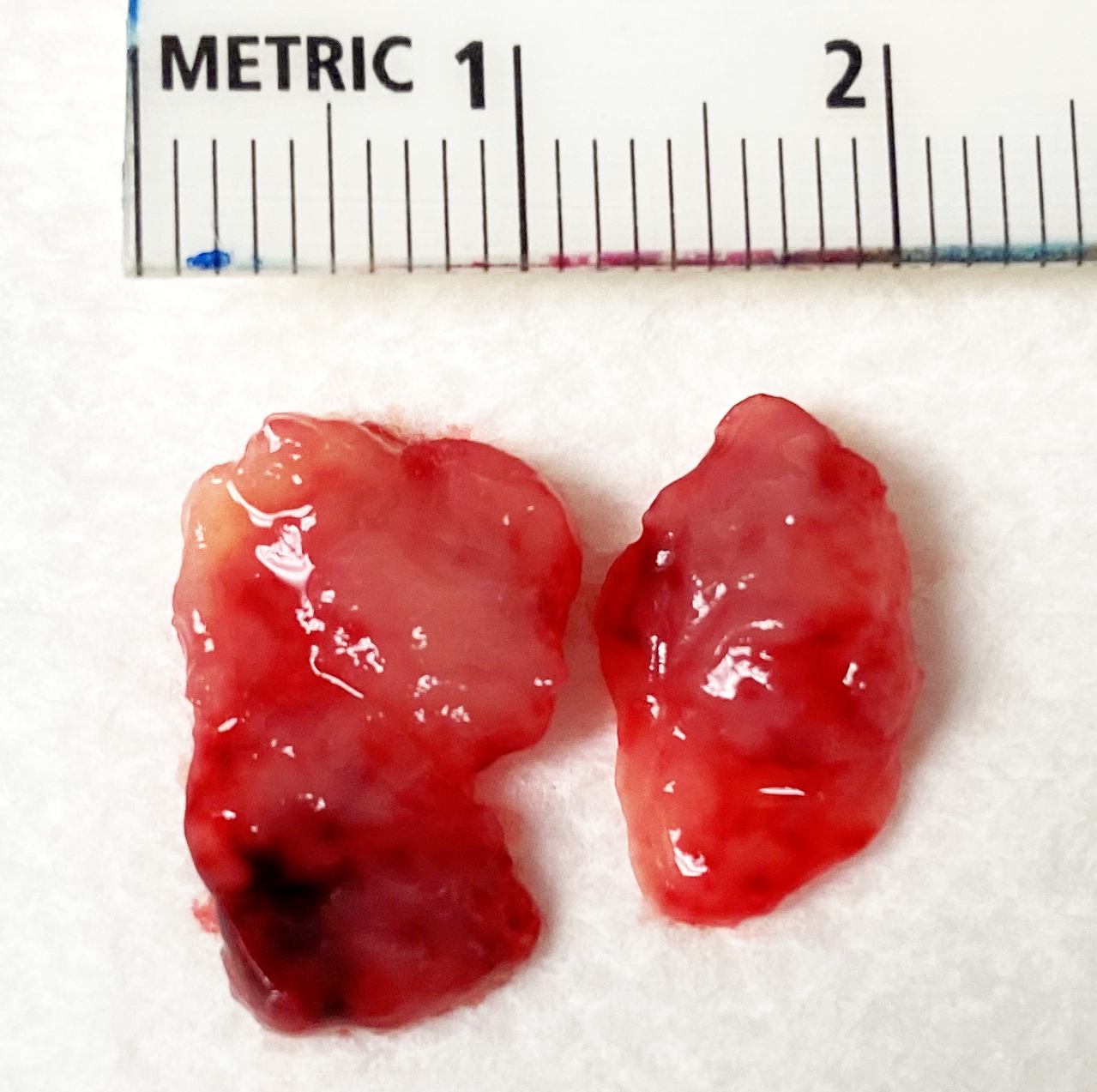
Gross description
- Polypoid mass, mean 3 cm, beefy red to grayish pink with hemorrhage
- Soft, edematous and fleshy cut surface
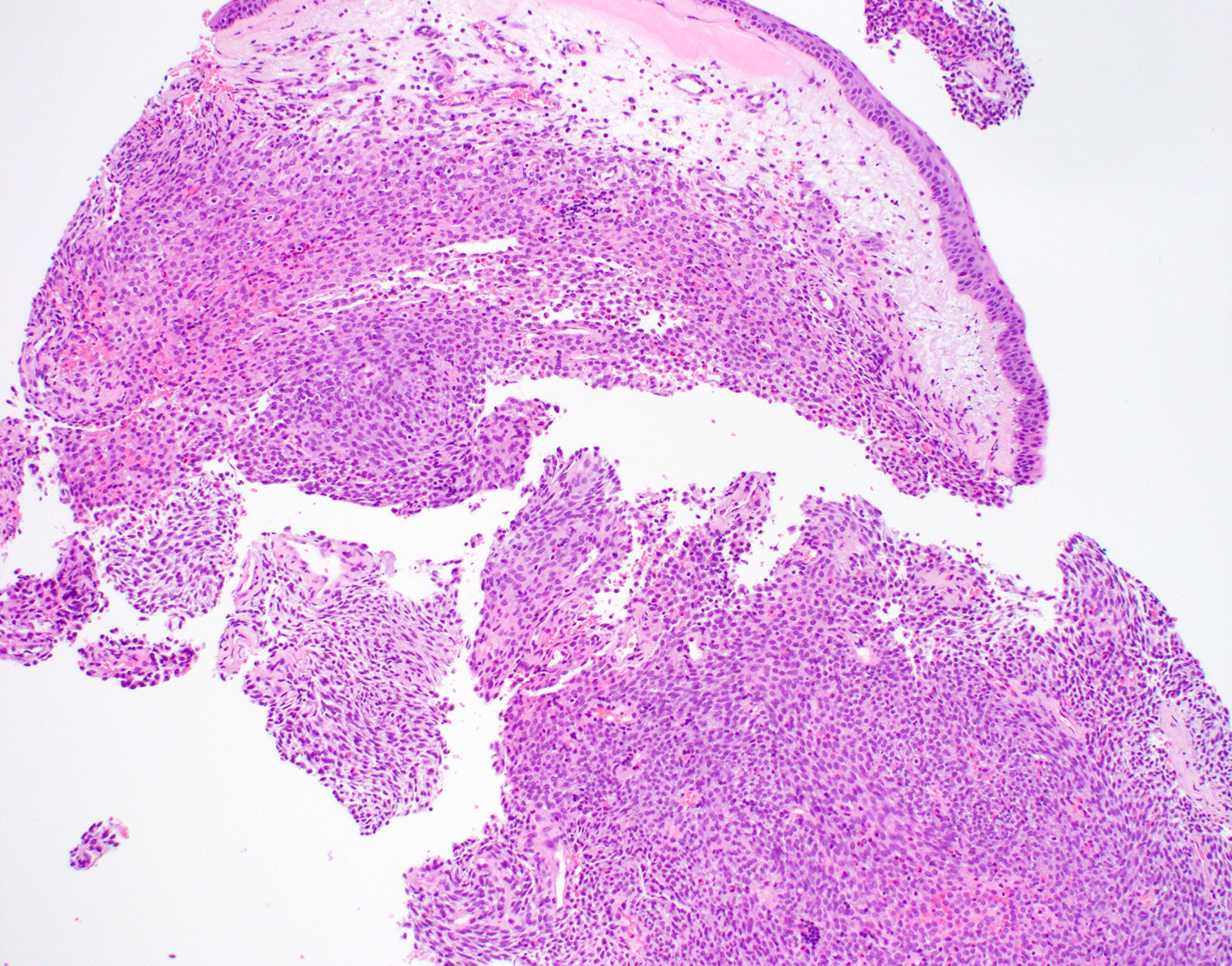
Frozen section description
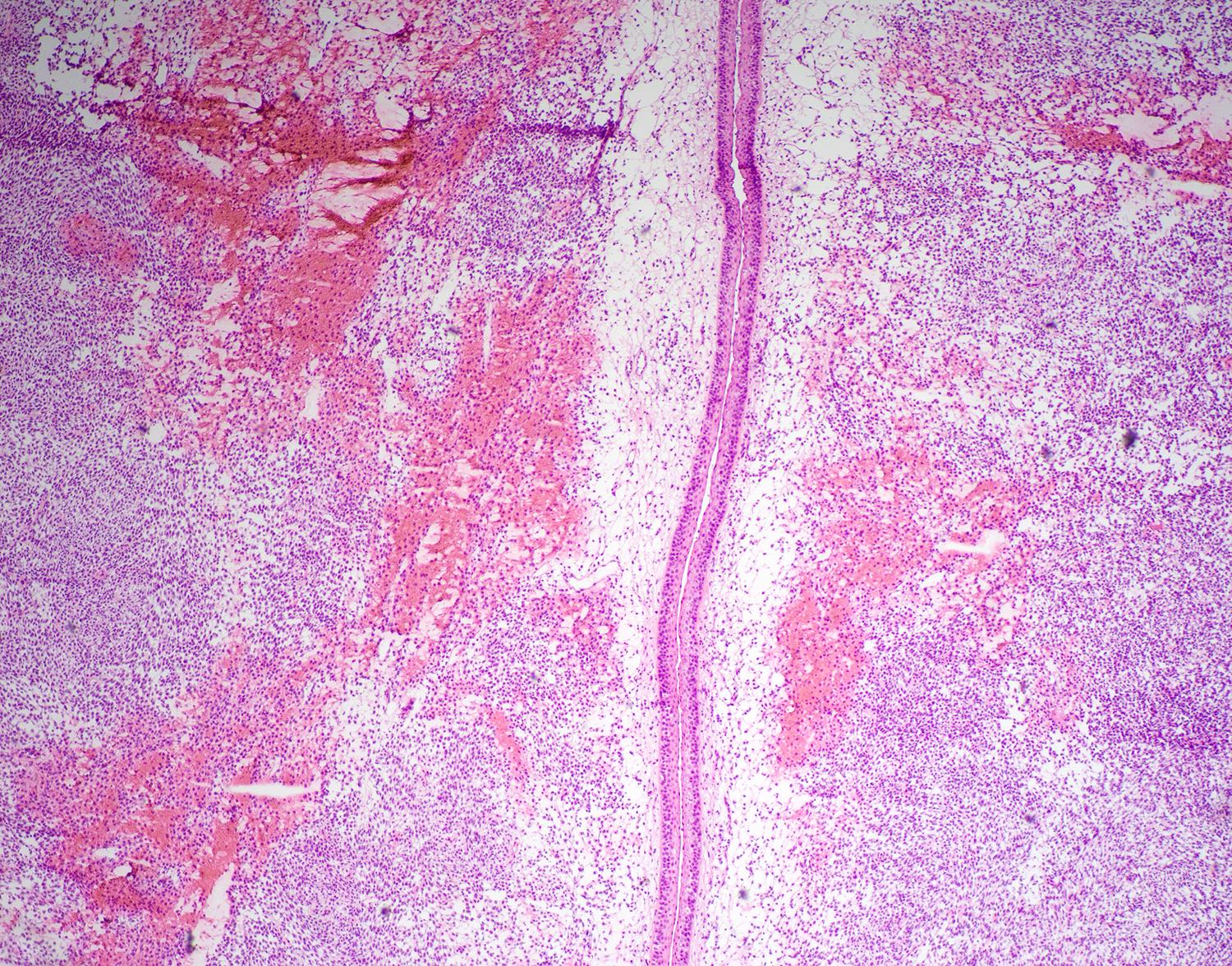
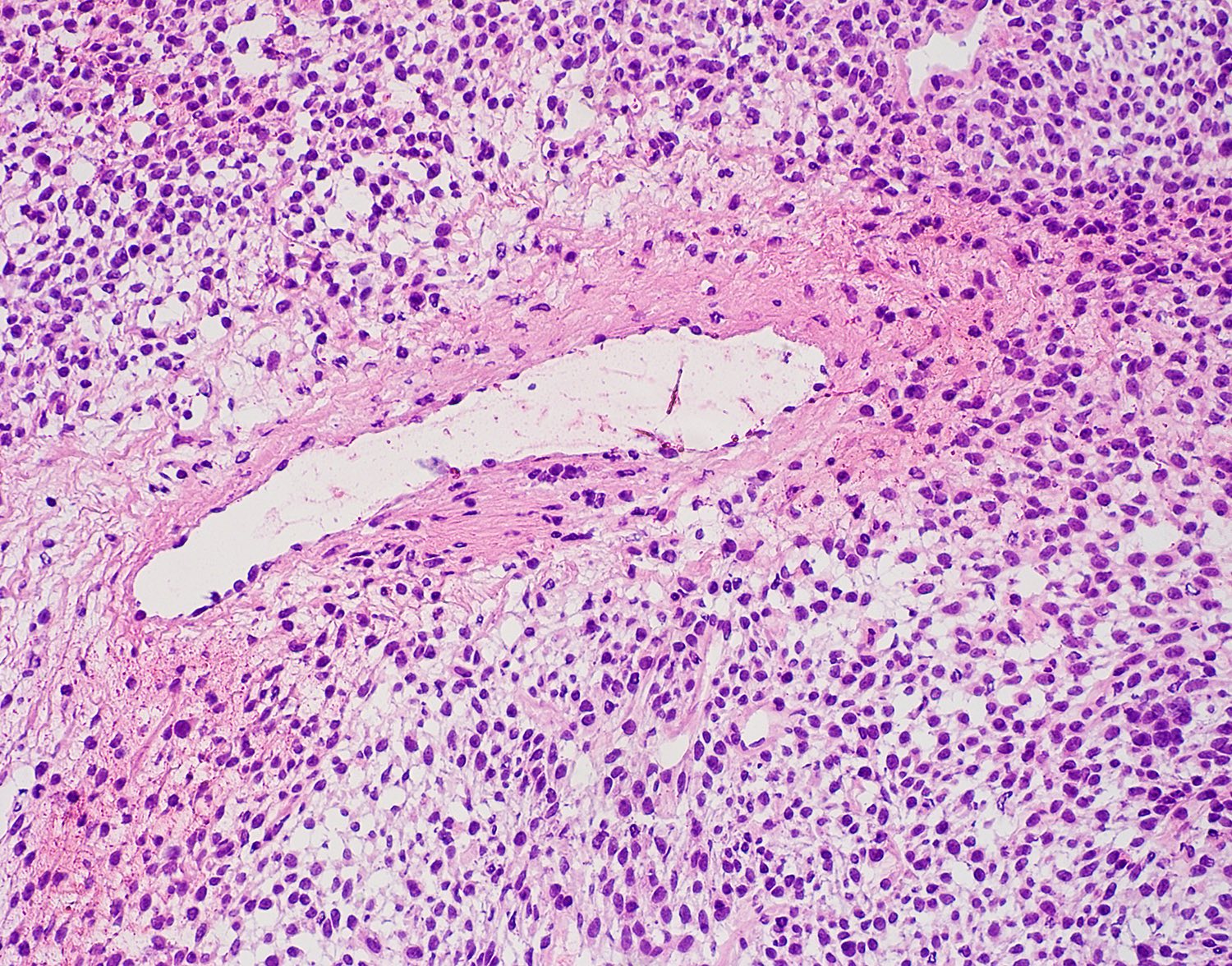
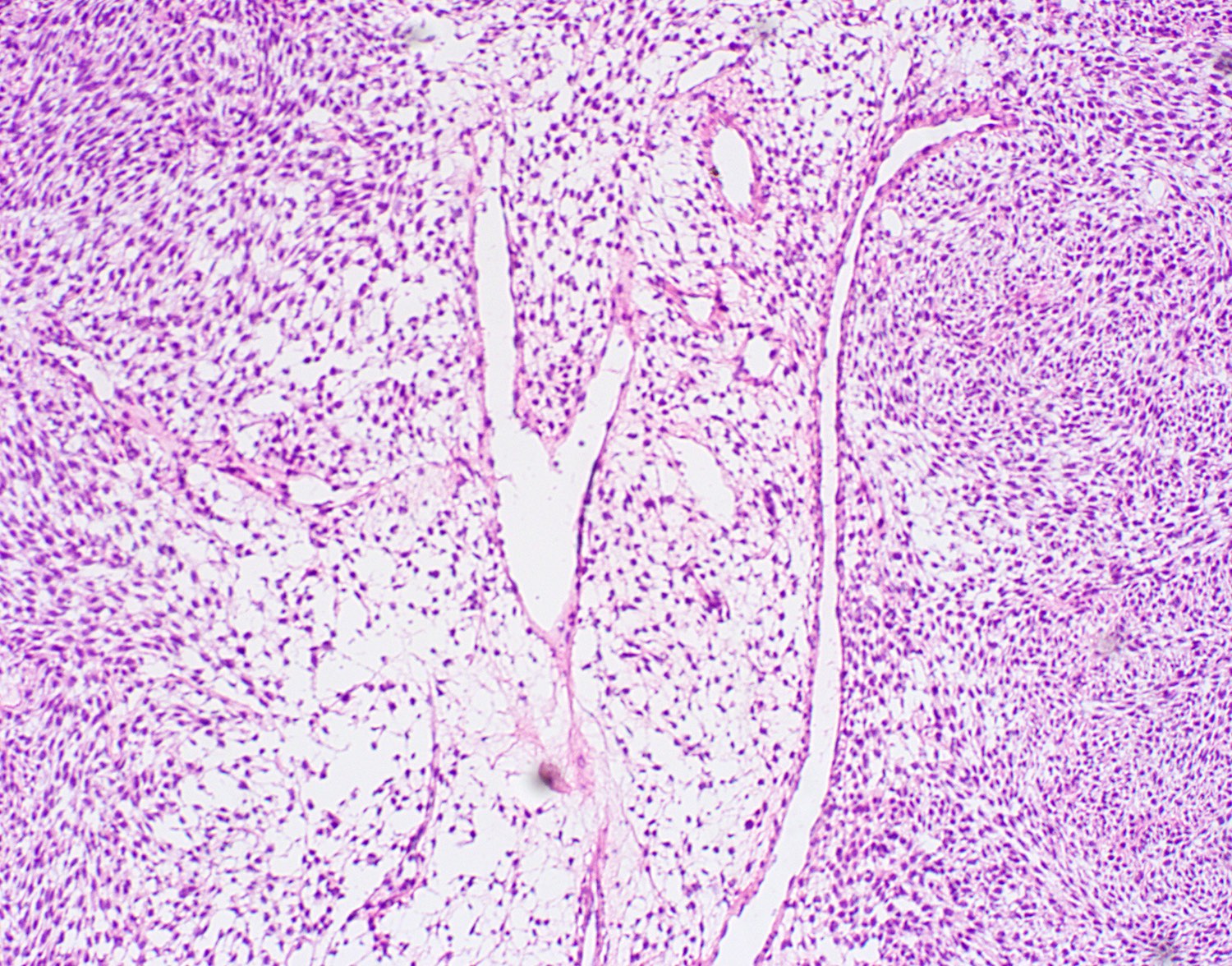
- Frozen sections of the tumor show subepithelial cytologically bland spindle and round cell proliferation separated from the surface respiratory epithelium, hemorrhagic stromal, perivascular hyalinization and staghorn vessels
Frozen section images
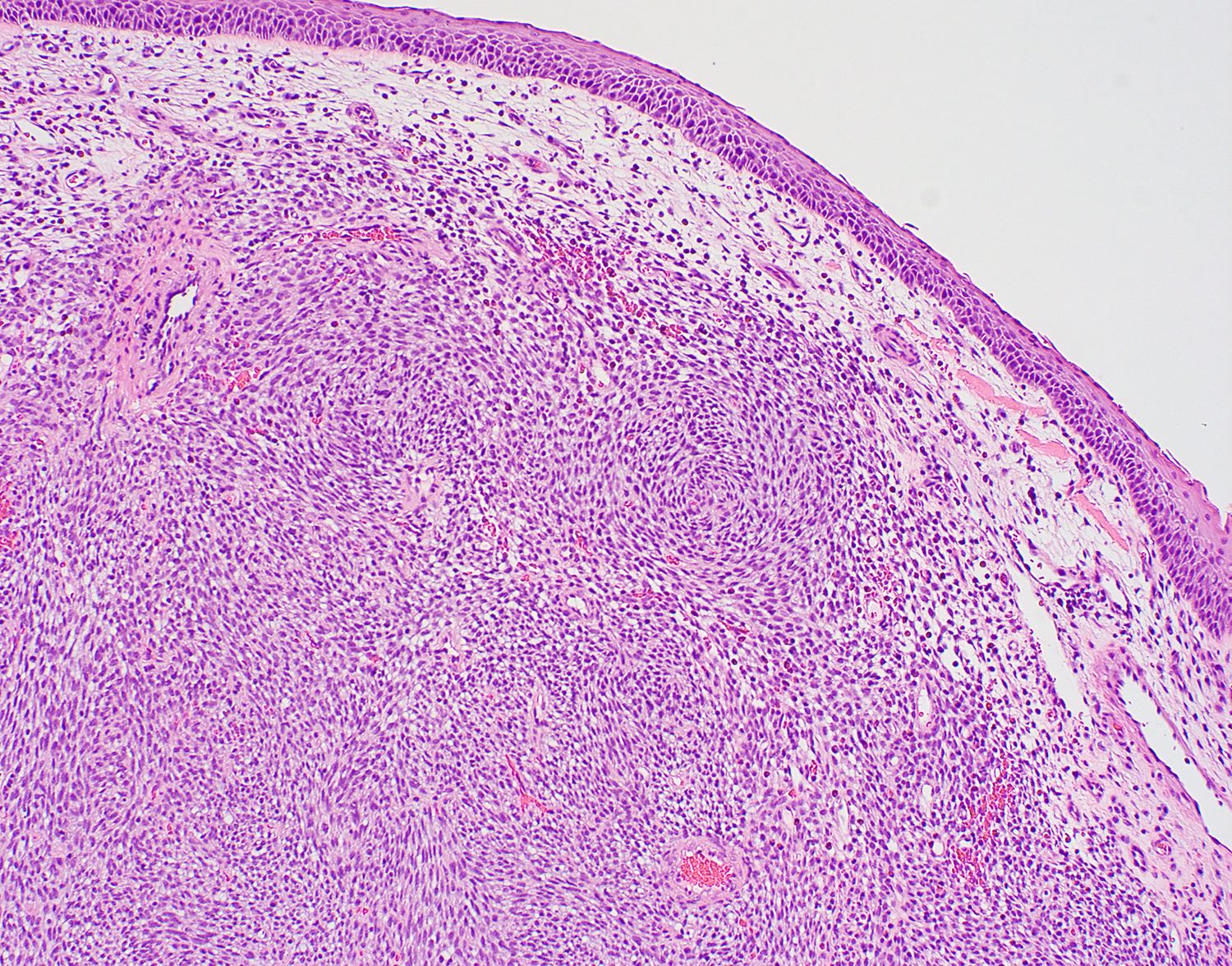
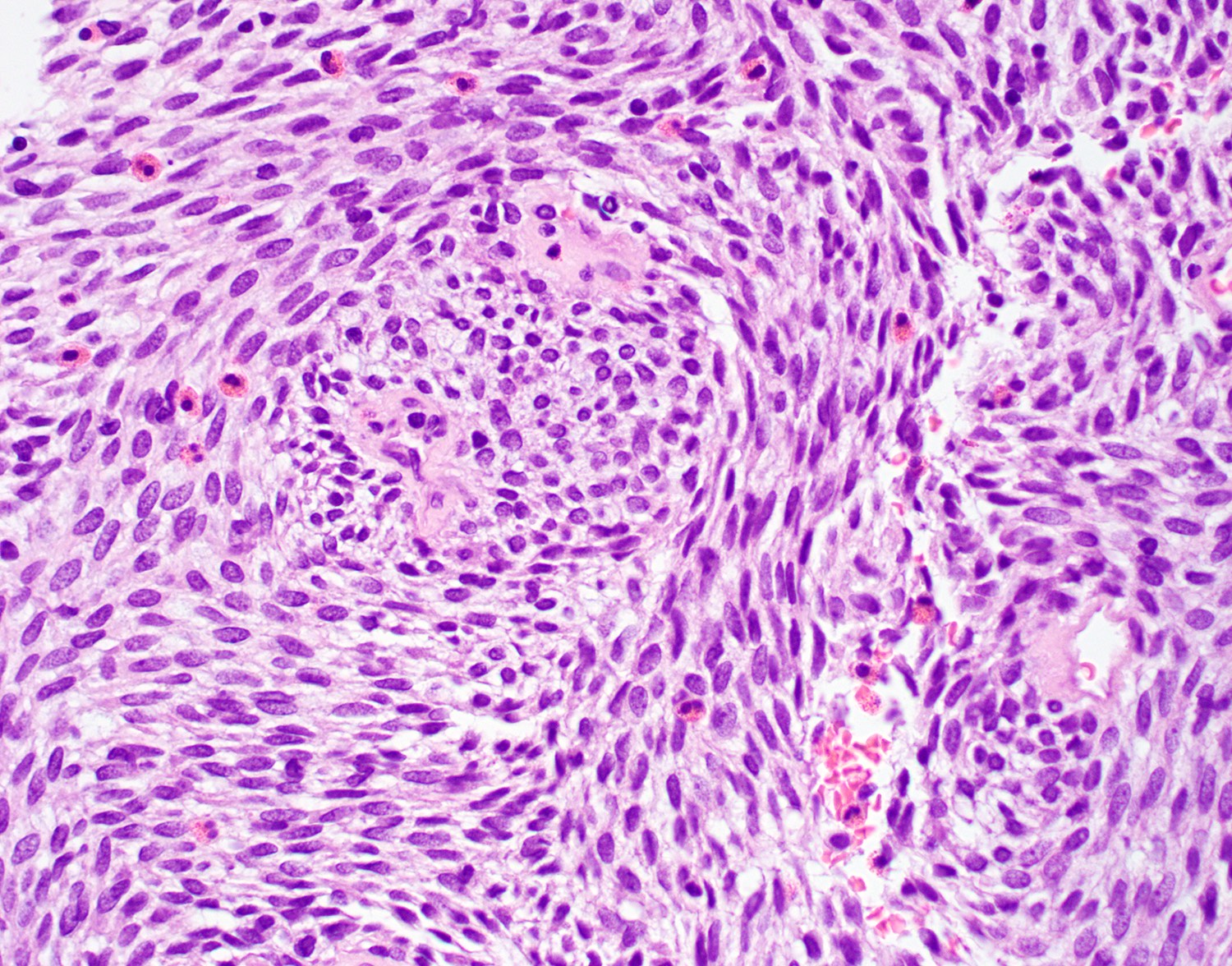
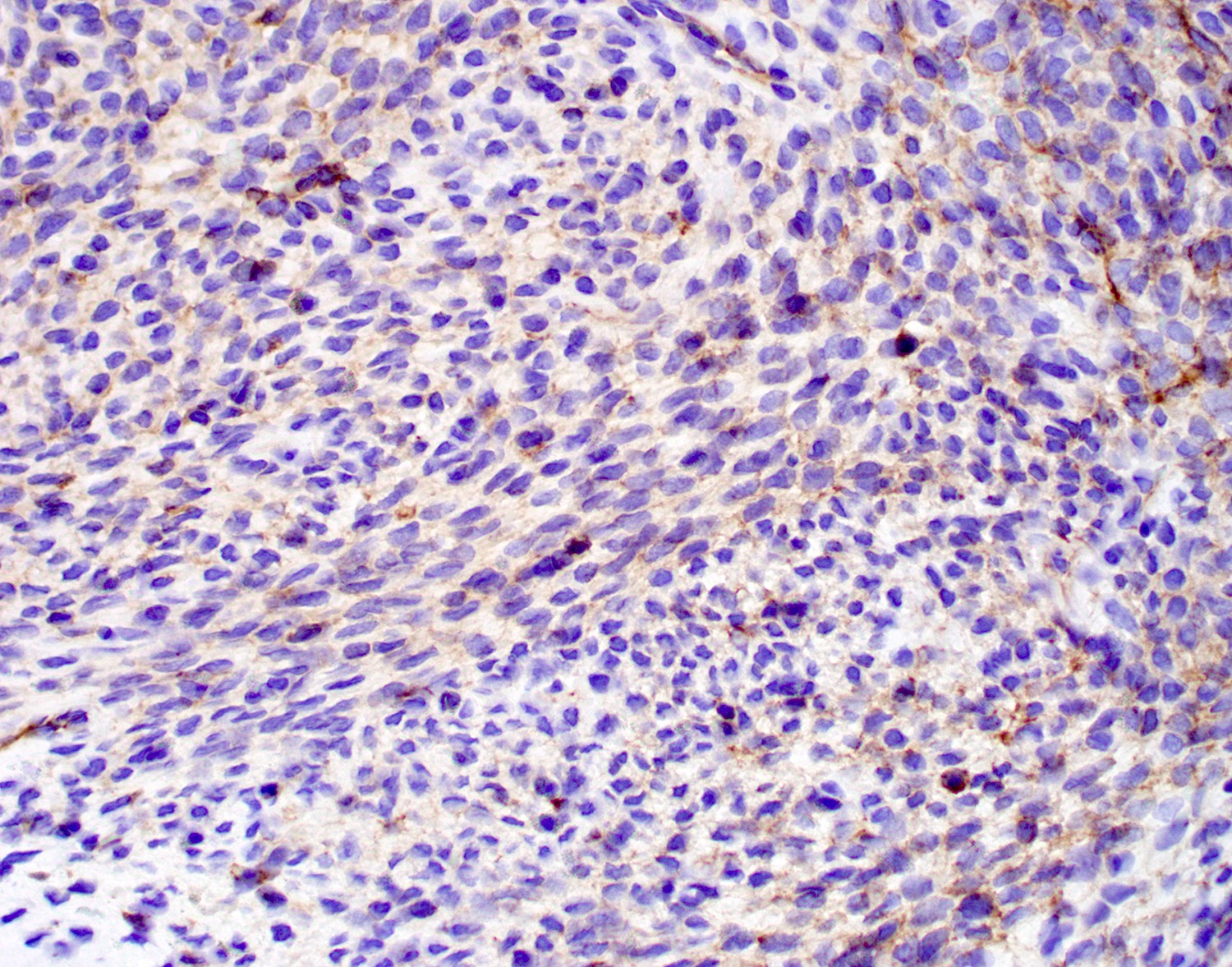
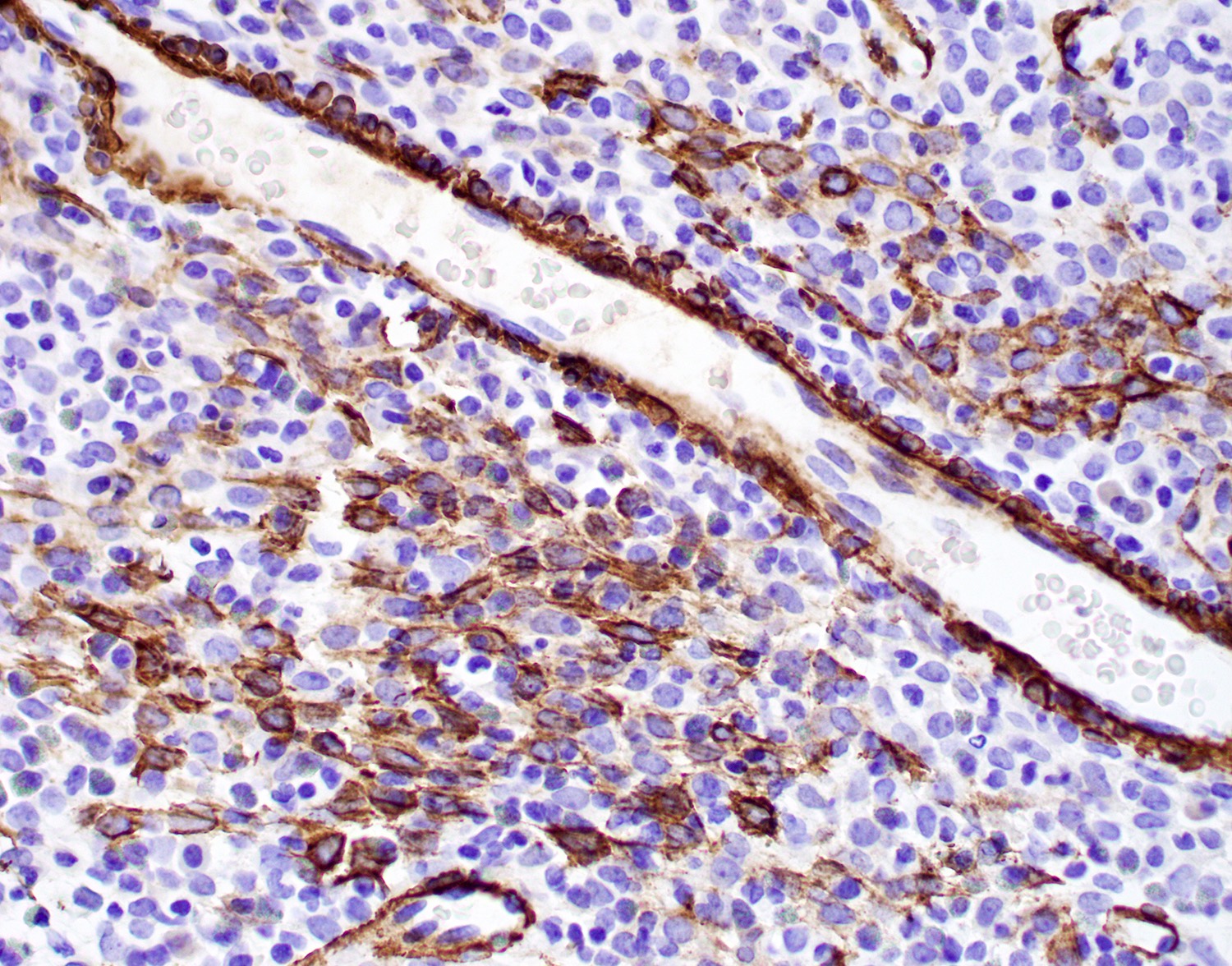
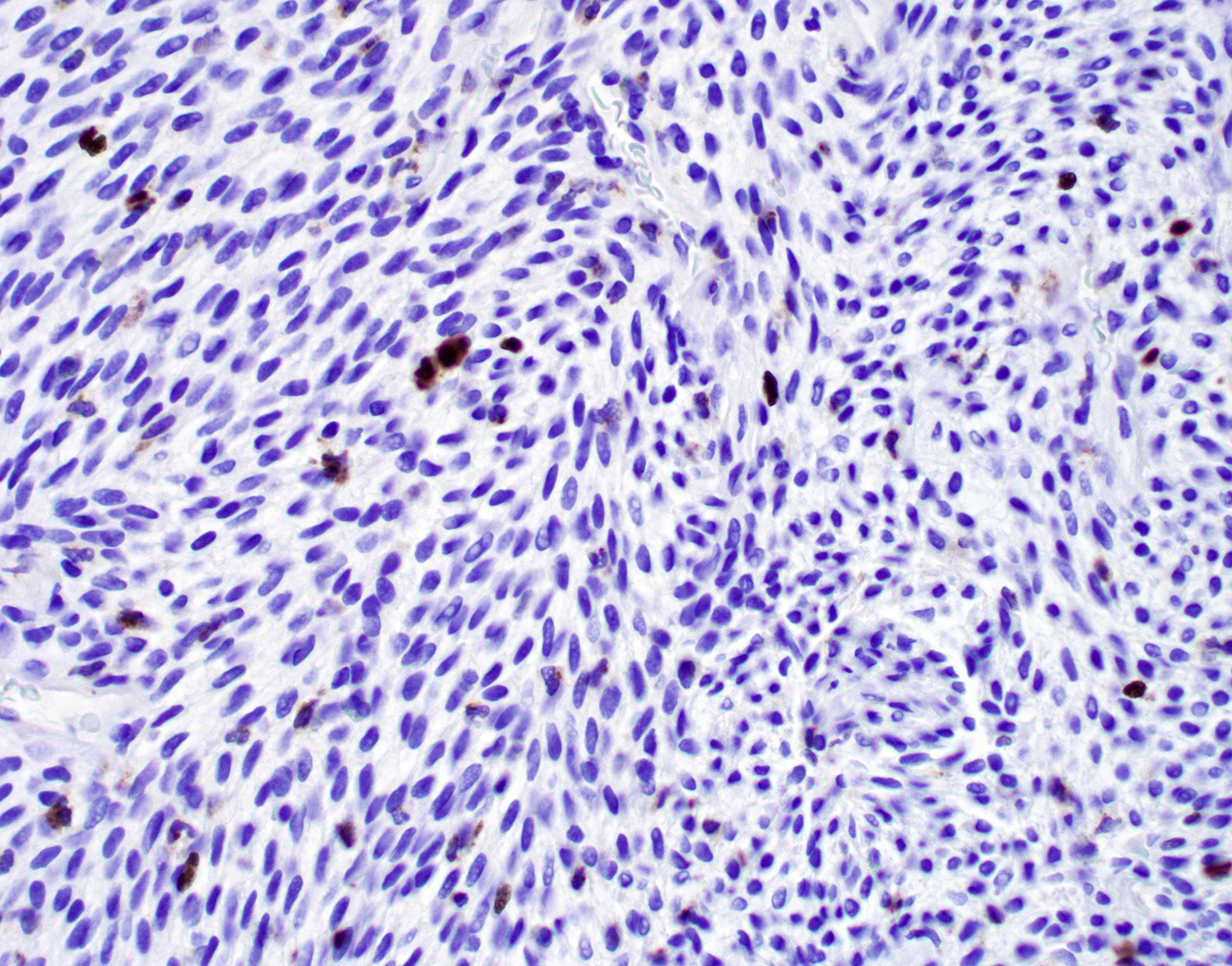
Microscopic (histologic) description
- Surface respiratory epithelium or metaplastic squamous epithelium is intact
- Subepithelial proliferation separated from surface (grenz zone)
- Diffuse growth with fascicular, solid or focally whorled pattern of spindled or round / oval tumor cells that arrange themselves around prominent, small, thin walled submucosal blood vessels
- Cells have variable cytoplasm and nuclei, indistinct cell borders and occasionally are multinucleated
- Minimal atypia, no necrosis, no / rare mitotic activity
- Vessels are prominent with staghorn appearance and perivascular hyalinization
- Inflammatory cells including mast cells and eosinophils are often present
Microscopic (histologic) images
Cytology description
- Smears show spindled, epithelioid or round cells with indistinct cell borders
Positive stains
- Beta catenin: nearly all tumor cells with nuclear and cytoplasmic staining (Pathol Res Pract 2019;215:983, Yale J Biol Med 2021;94:593)
- Cyclin D1, CD99 (Pathol Res Pract 2019;215:983)
- Vimentin (98%), smooth muscle actin (92%), muscle specific actin (77%), factor XIIIa (78%), laminin (52%)
- D2-40 (Virchows Arch 2006;448:459)
Negative stains
- ERG, CD31, CD34 (usually), factor VIII, keratin
Electron microscopy description
- Basal lamina surrounds individual cells, tapered cytoplasmic extensions, orderly bundles of filaments (Thompson: Diagnostic Pathology - Head and Neck, 2nd Edition, 2016)
Molecular / cytogenetics description
- CTNNB1 mutation: PCR and gene sequencing show single nucleotide substitutions with exon 3 codons of the CTNNB1 glycogen serine kinase 3 beta phosphorylation region
Sample pathology report
- Right nasal cavity mass, biopsy:
- Nasal glomangiopericytoma (see comment)
- Comment: Sections of the nasal mass biopsy show cytologically bland spindle cell proliferation with scattered staghorn vessels and perivascular hyalinization. The tumor cell proliferation is separated from the overlying respiratory epithelium. No mitotic figures or tumor necrosis is identified. The tumor cells are positive for beta catenin (nuclear staining), cyclin D1, CD99 and SMA, negative for desmin, CD31, ERG, CD34 and AE1 / AE3. The histologic features and immunoprofile support the diagnosis.
Differential diagnosis
- Glomus tumor:
- Also a pericytic tumor with similar staining but extremely rare in the sinonasal region
- Composed of compact epithelioid cells
- Positive for SMA but negative for beta catenin nuclear staining
- Lobular capillary hemangioma:
- Lobular pattern at low power
- Has spindled fibroblasts and prominent vessels but overall granulation tissue-like appearance with only small capillaries
- Positive for CD34 and CD31, negative for beta catenin nuclear staining
- Solitary fibrous tumor:
- Similar vascular pattern but tumor has patternless pattern, with ropy keloidal collagen and thin walled vascular spaces
- Positive for CD34 and STAT6, negative for beta catenin nuclear staining
- Ewing or Ewing-like sarcoma:
- Tumor cells have clear cytoplasm and similar histology with positive CD99 immunoreactivity
- Negative beta catenin nuclear staining and positive for EWSR1 rearrangement (Case Rep Oncol 2020;13:1393)
Additional references
Board review style question #1
Regarding sinonasal glomangiopericytoma, which of the following statements is true?
- Bilateral tumor is seen in 10% of patients
- It is much more common in male patients
- Majority of the tumors have a poor prognosis
- Maxillary sinus is the most affected
- Nasal cavity is usually affected
Board review style answer #1
E. Nasal cavity is usually affected; maxillary and ethmoid sinuses may also be affected in conjunction with nasal cavity. The female to male ratio is 1.2 to 1. Patients with bilateral tumor are uncommon (~5%). The majority of the tumors have a good prognosis.
Comment Here
Reference: Sinonasal glomangiopericytoma
Comment Here
Reference: Sinonasal glomangiopericytoma
Board review style question #2
A 50 year old woman presented with right nasal obstruction and occasional nose bleeding. Physical examination showed a red to grayish polypoid soft mass in her right nasal cavity and a biopsy was performed. A histology photo is shown above. Which of the following immunostains should be positive for the diagnosis of nasal glomangiopericytoma?
- Beta catenin nuclear staining
- CD31
- CD34
- S100 nuclear staining
- STAT6 nuclear staining
Board review style answer #2
A. Beta catenin nuclear staining should be positive in the tumor cells, as sinonasal glomangiopericytoma is related to mutational beta catenin activation. Positive CD34 and STAT6 are helpful for diagnosis of solid fibrous tumor. Positive S100 and muscular markers are helpful for diagnosis of biphenotypic sinonasal sarcoma.
Comment Here
Reference: Sinonasal glomangiopericytoma
Comment Here
Reference: Sinonasal glomangiopericytoma