Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Xu B, Mannan R, Yuan S. Nasopharyngeal carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/nasalnasopharyngealgeneral.html. Accessed April 27th, 2024.
Definition / general
- Nasopharyngeal carcinoma originates from the nasopharyngeal mucosa showing histologic or immunophenotypic evidence of squamous differentiation
- WHO classification of nasopharyngeal carcinoma:
- Nonkeratinizing squamous cell carcinoma
- Differentiated subtype
- Undifferentiated subtype
- Keratinizing squamous cell carcinoma
- Basaloid squamous cell carcinoma
- Nonkeratinizing squamous cell carcinoma
Essential features
- Originates from nasopharynx
- Showing squamous differentiation on H&E or immunohistochemistry
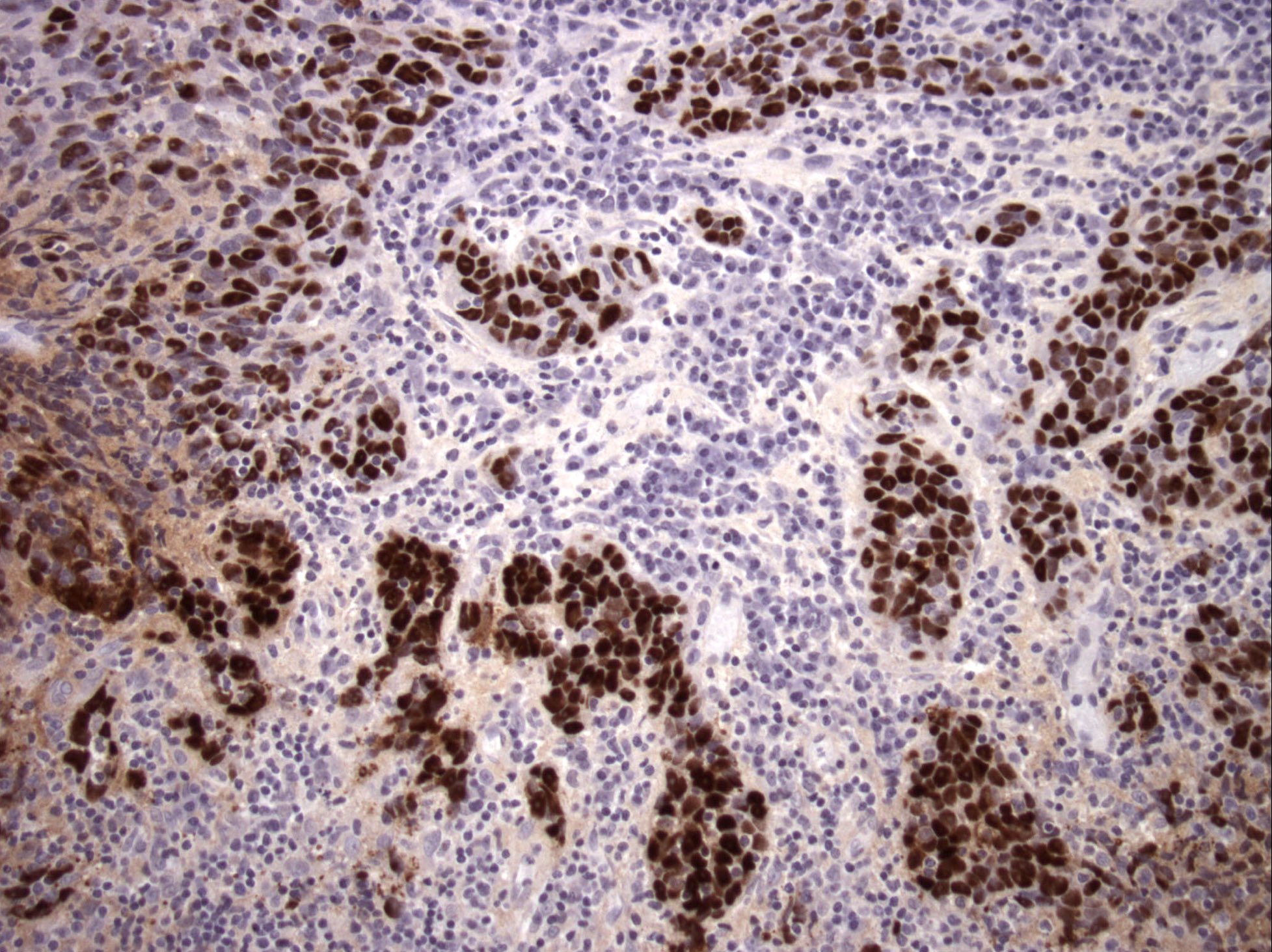
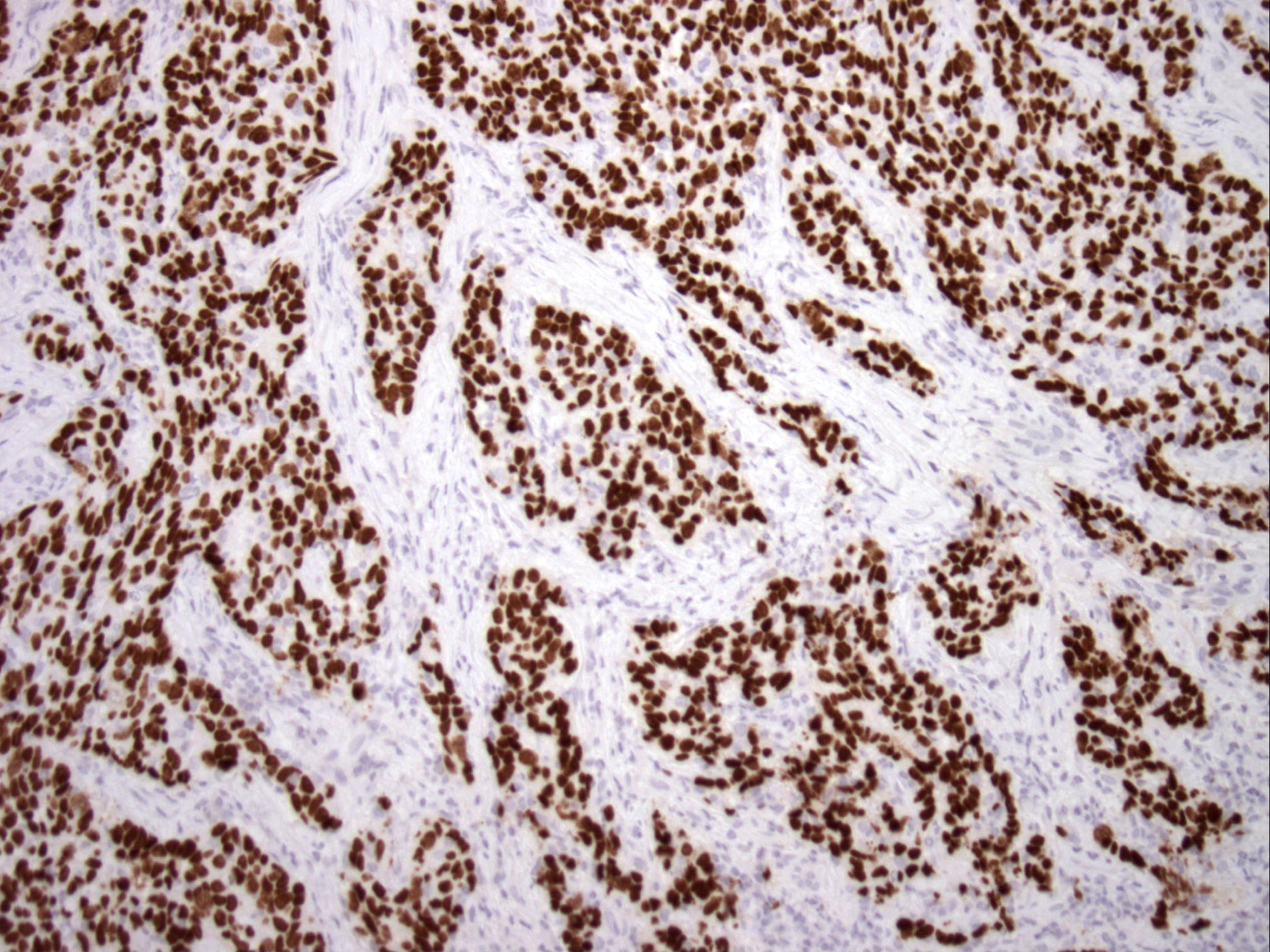
- Most are positive for Epstein-Barr virus (EBV) / Epstein-Barr encoded RNA (EBER) in endemic areas (China, Southeast Asia and North Africa)
- Nonkeratinizing, undifferentiated subtype is the most common, showing syncytial growth pattern, vesicular nuclei with prominent central nucleoli and reactive lymphoid stroma
Terminology
- Nonkeratinizing, undifferentiated: lymphoepithelioma, lymphoepithelial carcinoma, undifferentiated carcinoma
- Nonkeratinizing, differentiated: transitional carcinoma
- Keratinizing: squamous cell carcinoma
ICD coding
Epidemiology
- High Incidence in China, Southeast Asia, North Africa, natives of Arctic region and part of the Mediterranean Basin (Semin Diagn Pathol 2015;32:54, Surg Oncol Clin N Am 2015;24:547)
- Rare in US: incidence 0.2 to 0.5 per 100,000 (Semin Diagn Pathol 2015;32:54, Surg Oncol Clin N Am 2015;24:547)
- Undifferentiated is the most common subtype, accounting for > 60% of nasopharyngeal carcinoma
- It is also the most frequent pediatric subtype
- Other subtypes in a descending order of frequency are keratinizing, nonkeratinizing differentiated and basaloid
- Peak incidence in fourth to sixth decades; less than 20% occur in pediatric age group
Sites
- As the name implies, nasopharyngeal carcinoma affects nasopharynx, with nasopharyngeal recess (i.e. fossa of Rosenmüller) as the most common affected site, followed by superior posterior wall
- Extension to adjacent organs (e.g., nasal cavity, paranasal sinus, oropharynx, bone, orbit and infratemporal fossa) is common (Int J Radiat Oncol Biol Phys 2004;59:21)
Etiology
- Strongly associated with Epstein-Barr virus (EBV) in endemic regions (Semin Diagn Pathol 2015;32:54, Mod Pathol 2017;30:S68)
- Subset may be attributed to high risk human papillomavirus (HPV) in nonendemic and endemic regions (Head Neck 2014;36:511, Neoplasma 2016;63:107, Acta Virol 1988;32:261)
- Other risk factors (Semin Diagn Pathol 2015;32:54):
- Genetic susceptibility; e.g., certain human leukocyte antigen (HLA) class I genotypes (Semin Diagn Pathol 2015;32:54)
- High levels of nitrosamines in preserved food (e.g., salted fish)
- Cigarette smoking
- Occupational exposure to chemical fumes, smoke, formaldehyde and wood dust
- Keratinizing subtype can arise as secondary malignancy years after radiation therapy for nonkeratinizing nasopharyngeal carcinoma (Hum Pathol 2000;31:227)
Clinical features
- Commonly presents with painless upper cervical lymphadenopathy secondary to lymph node metastasis or obstructive symptoms related to nasopharyngeal mass (e.g., postnasal drip, nasal discharge, epistaxis, serous otitis media and tinnitus) (Hong Kong Med J 1997;3:355)
- Headache and symptoms of cranial nerve involvement in advanced disease with skull base involvement
Diagnosis
- Biopsies are recommended if diagnosis is suspected (70% sensitive)
Laboratory
- Positive Epstein-Barr virus (EBV) serology (Int J Cancer 2020;146:2923)
- Elevated circulating EBV DNA or RNA; e.g., plasma or serum EBV encoded small RNA (EBERs)
Radiology description
- MRI covering the nasopharynx and cervical regions is the preferred imaging modality to assess extent of disease and presence of intracranial extension (Radiopaedia: Nasopharyngeal Carcinoma [Accessed 5 April 2018])
Radiology images
Prognostic factors
- 5 year survival is ~ 65% for nonkeratinizing differentiated and undifferentiated subtypes
- Keratinizing type has a poorer outcome, with frequent nodal metastasis and high mortality (Semin Diagn Pathol 2015;32:54)
- Clinical stage is the most important prognostic factor: 5 year disease specific survival is 98% for stage I, 95% for stage II, 86% for stage III and 73% for stage IV
- Other adverse prognostic factors include older age, male gender, large tumor volume and cranial nerve palsy
Case reports
- 49 year old woman with breast metastasis from nasopharyngeal carcinoma (Oncol Lett 2013;5:1859)
- 50 year old man with bilateral enlarging neck masses for 10 months (Case #100)
- 56 and 58 year old men with glandular differentiation in EBV positive nasopharyngeal carcinoma (Arch Pathol Lab Med 2000;124:1369)
Treatment
- Radiation therapy is the mainstay of treatment for all histologic types of nasopharyngeal carcinoma (NCCN: NCCN Guidelines - Head and Neck Cancers [Accessed 14 October 2020])
- Surgery is reserved for patients who fail to respond to radiation therapy
Gross description
- Most specimens are endoscopic biopsy without specific gross findings
- In resection specimens, the gross appearance is variable: smooth mucosal bulge, raised nodule with or without surface ulceration, infiltrative mass lesion or occult lesion identified only on microscopy
Microscopic (histologic) description
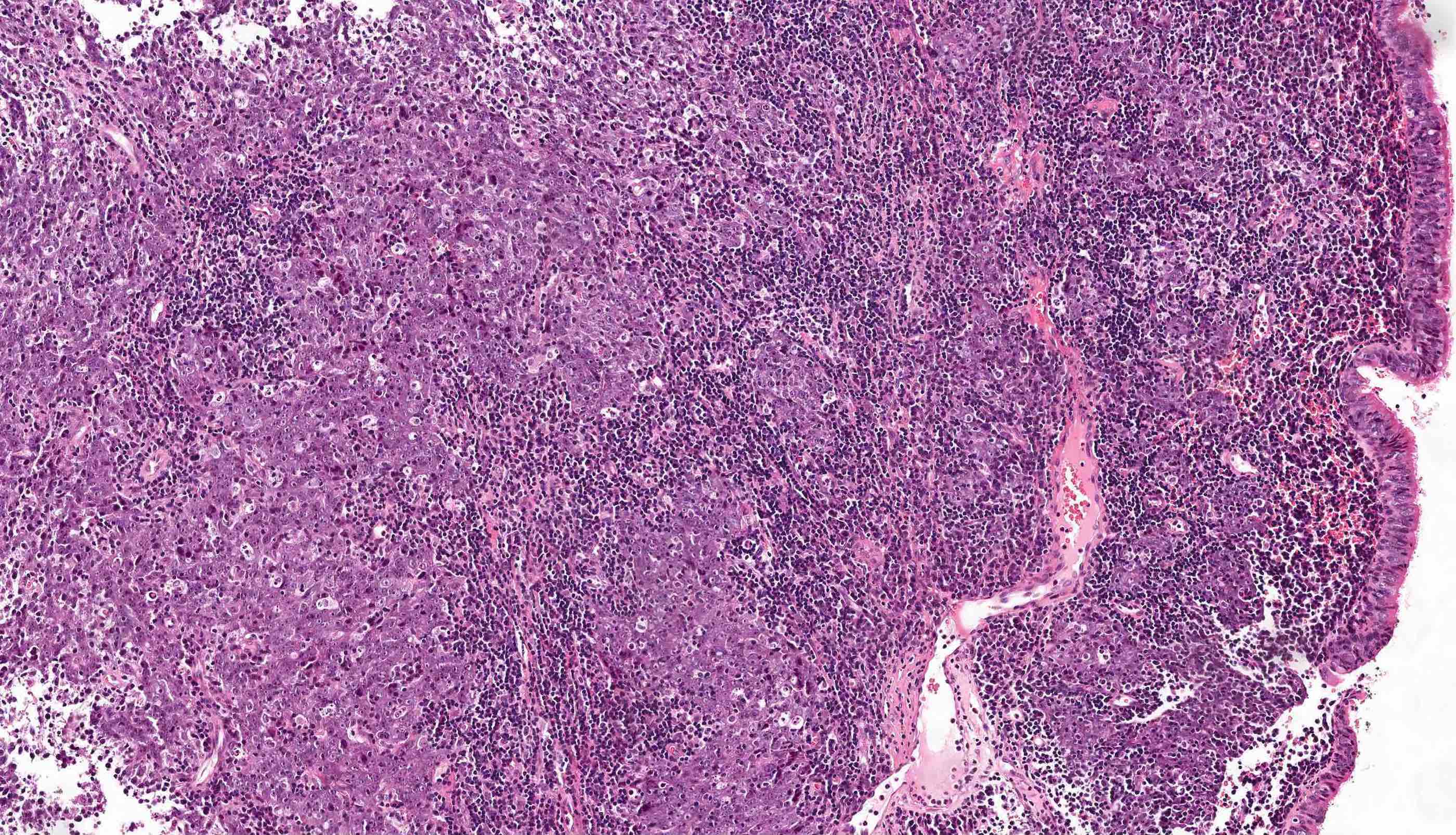
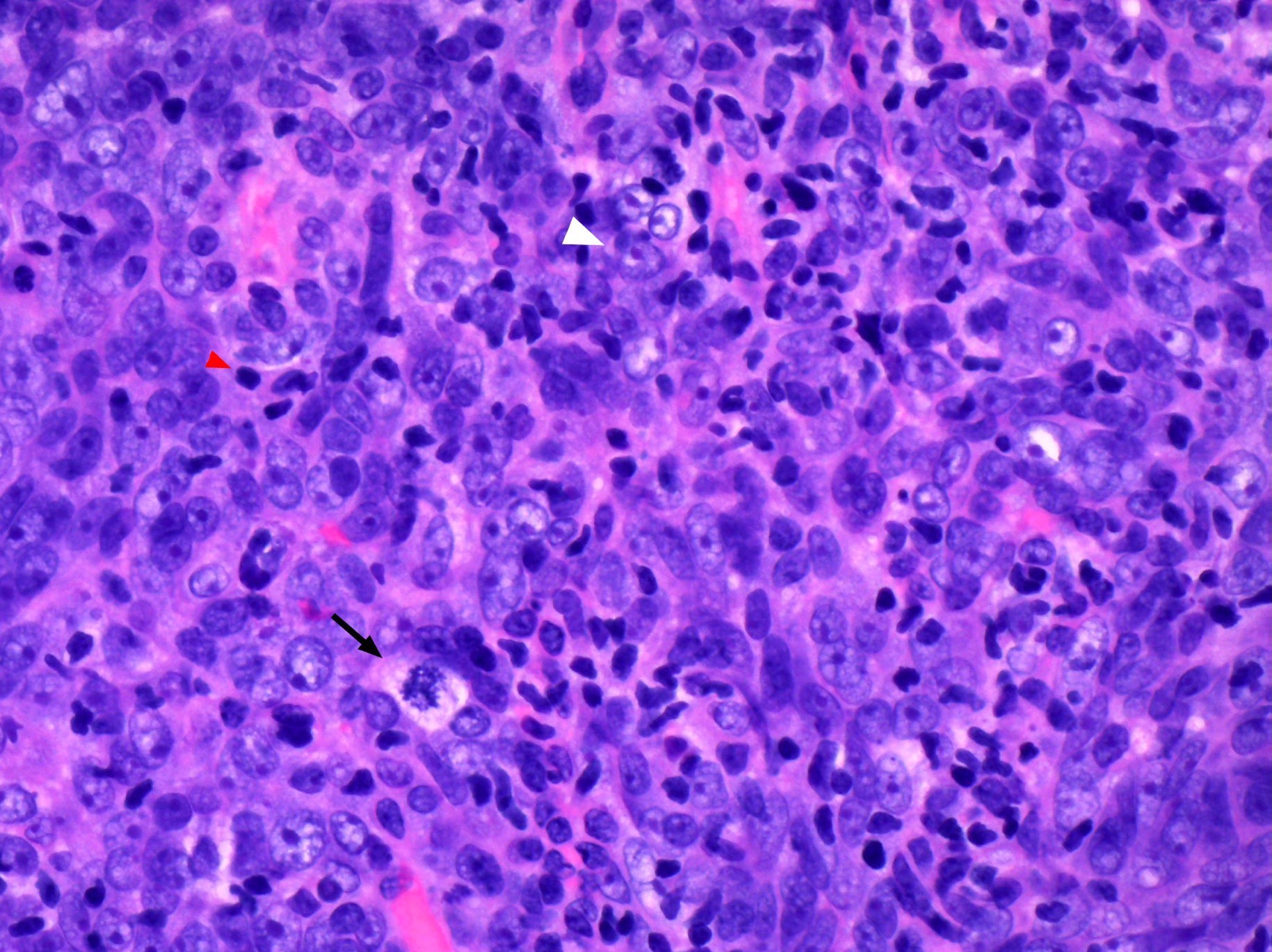
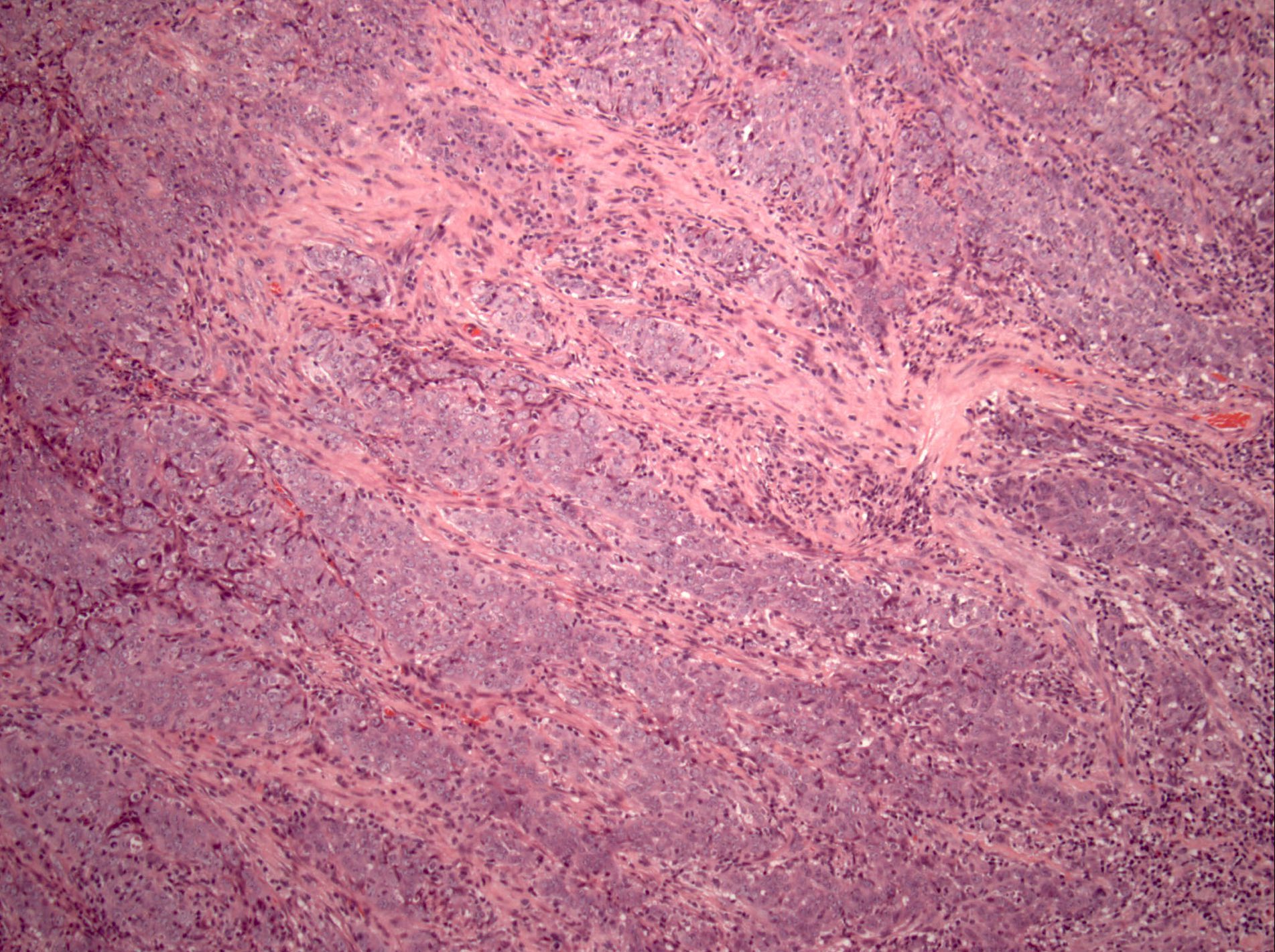
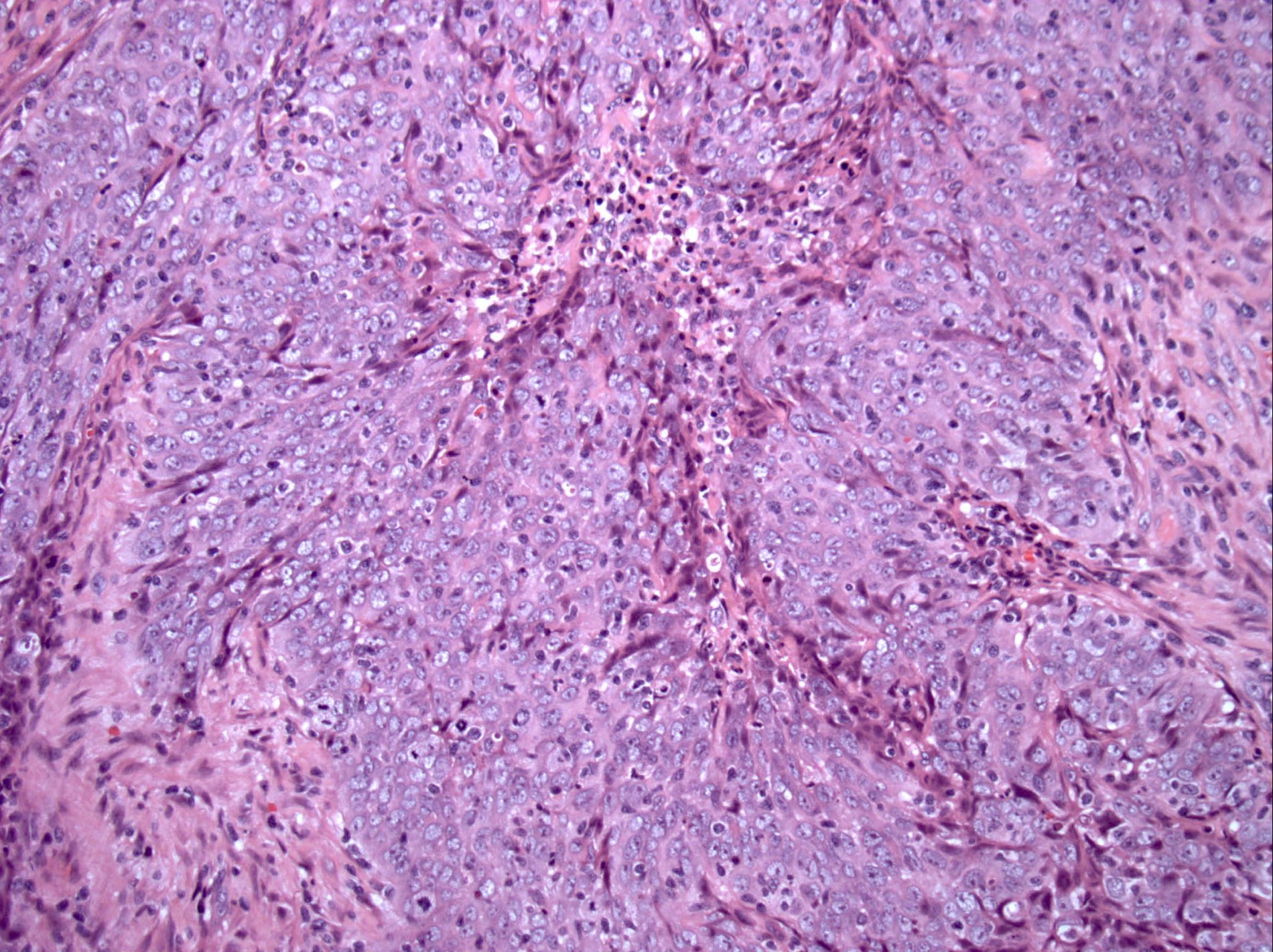
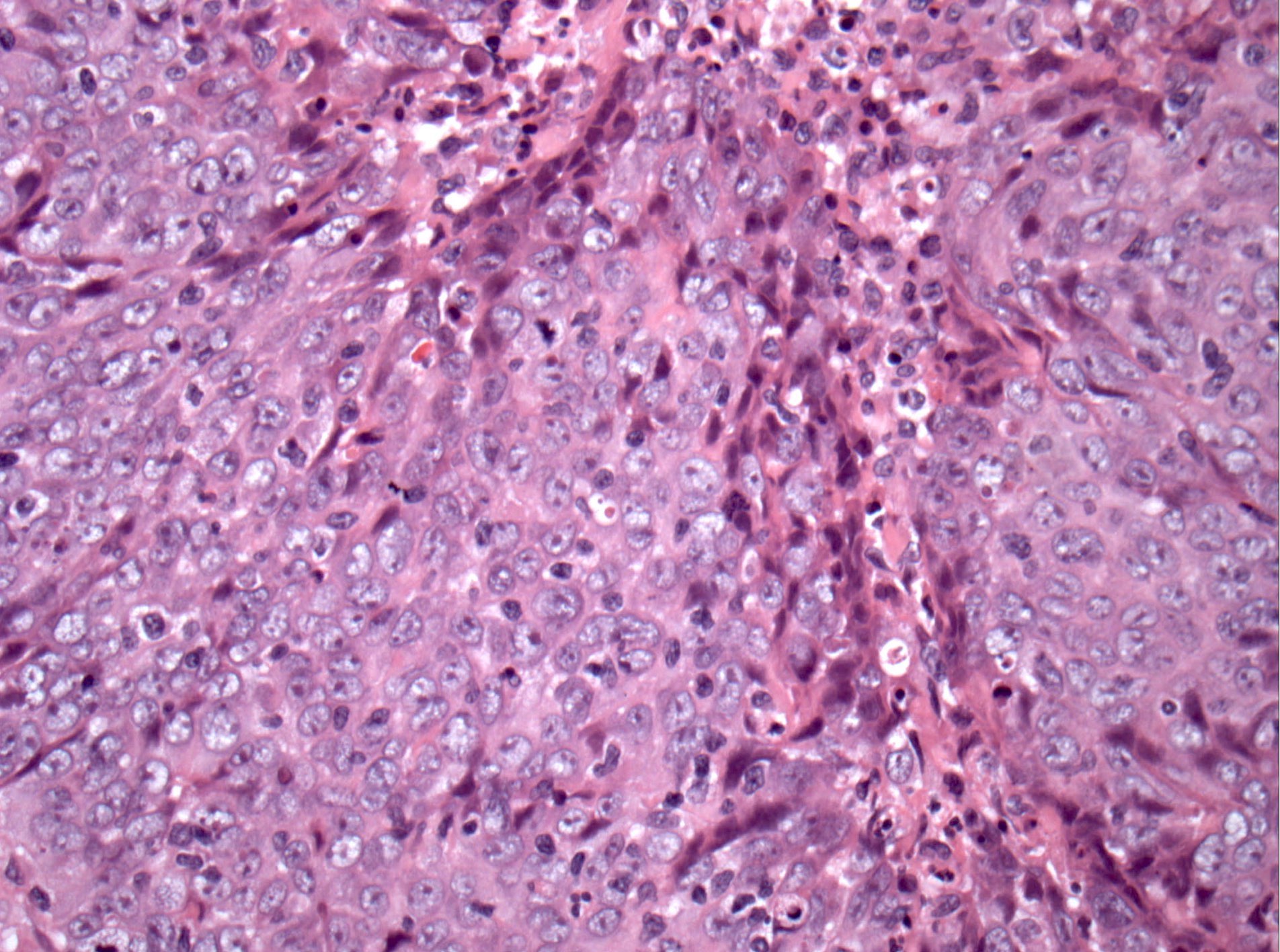
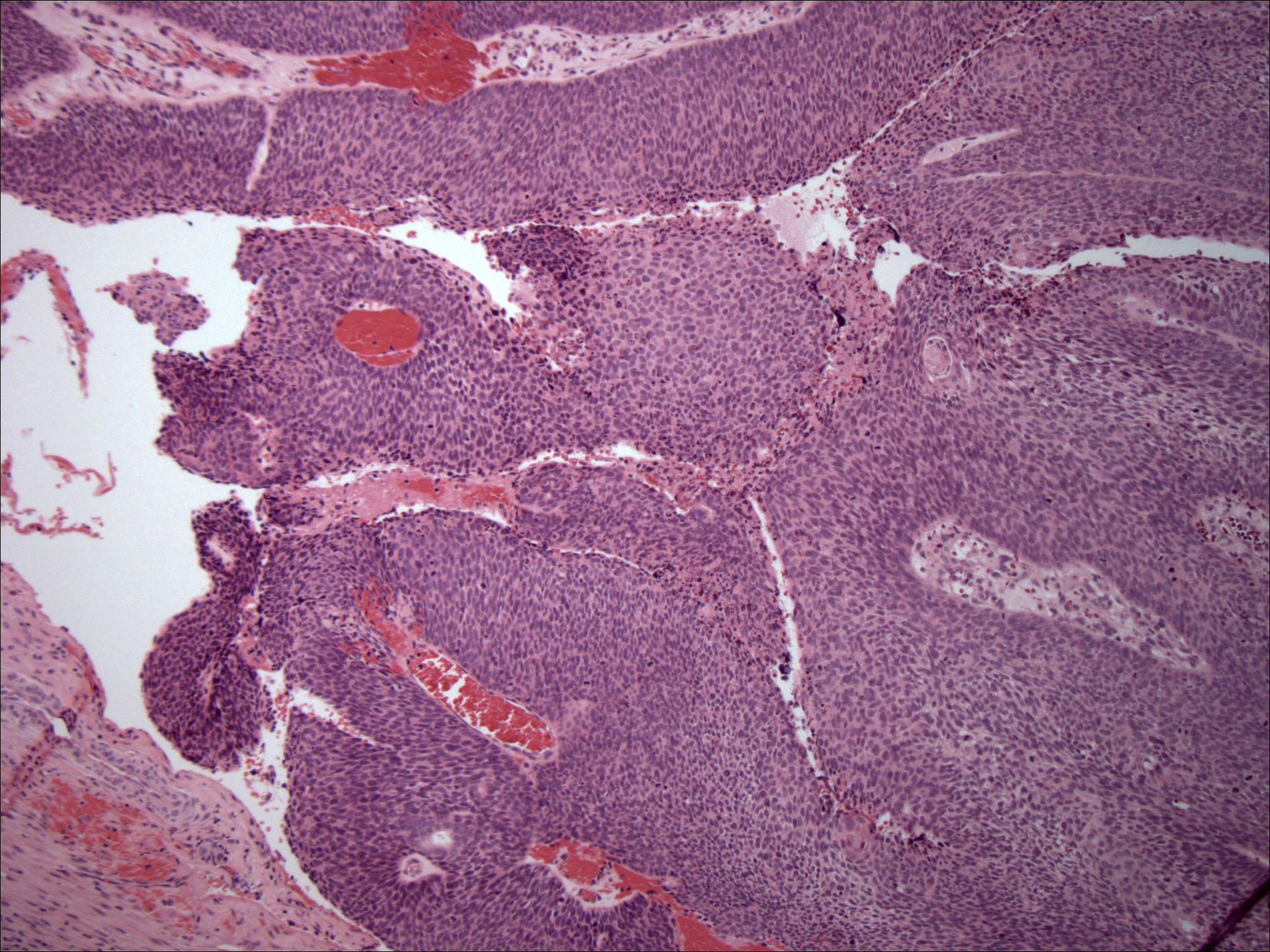
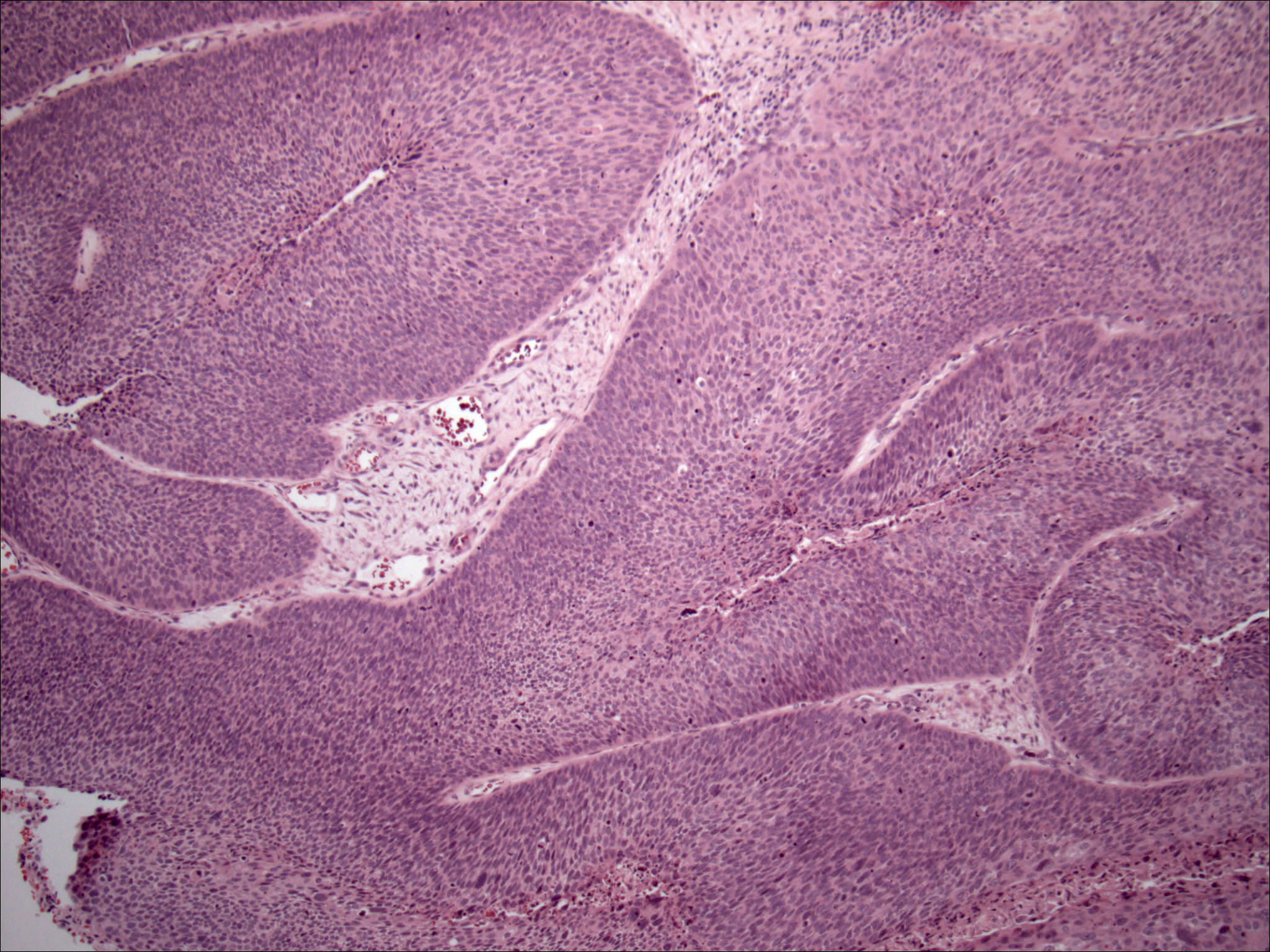
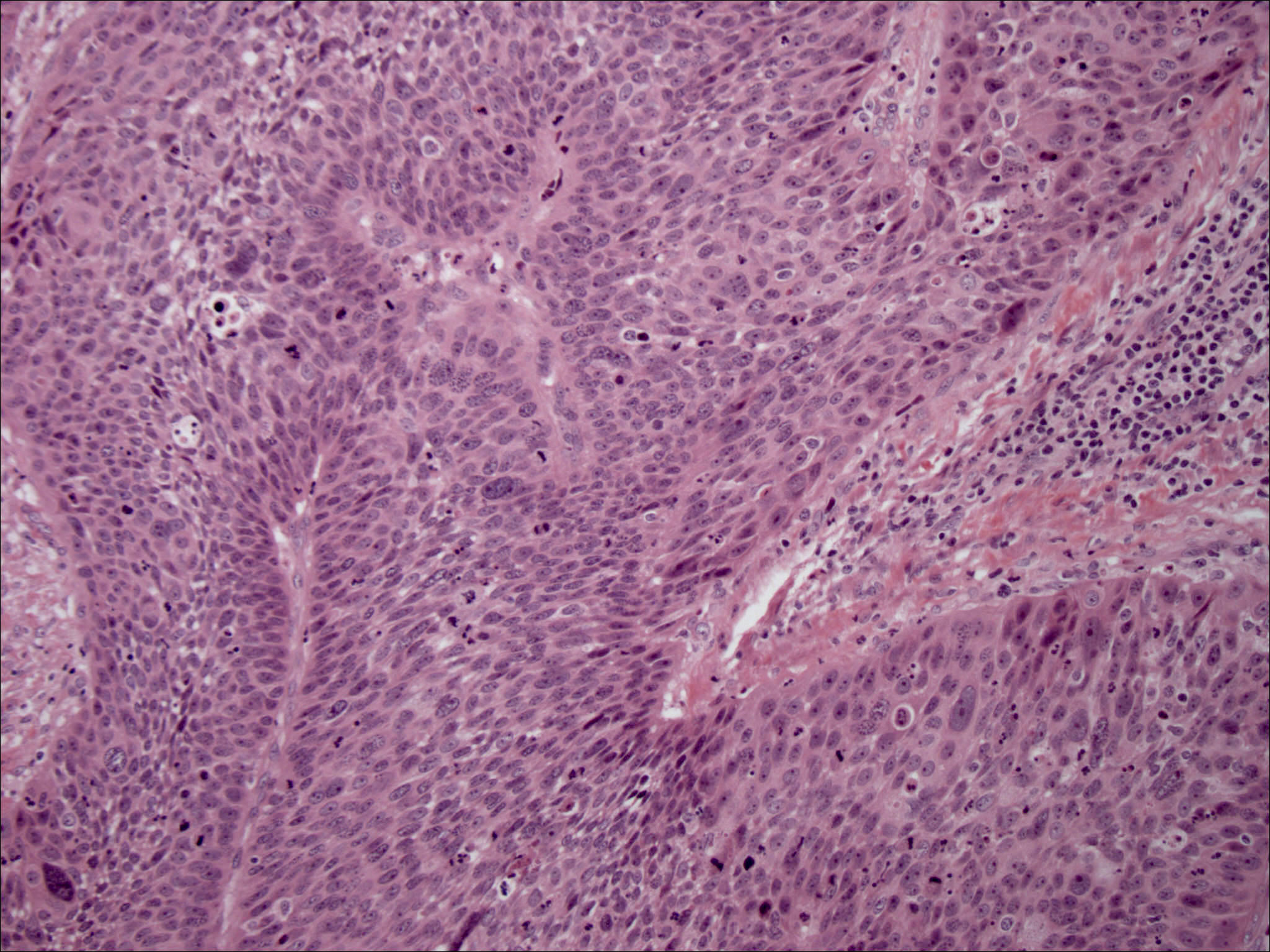
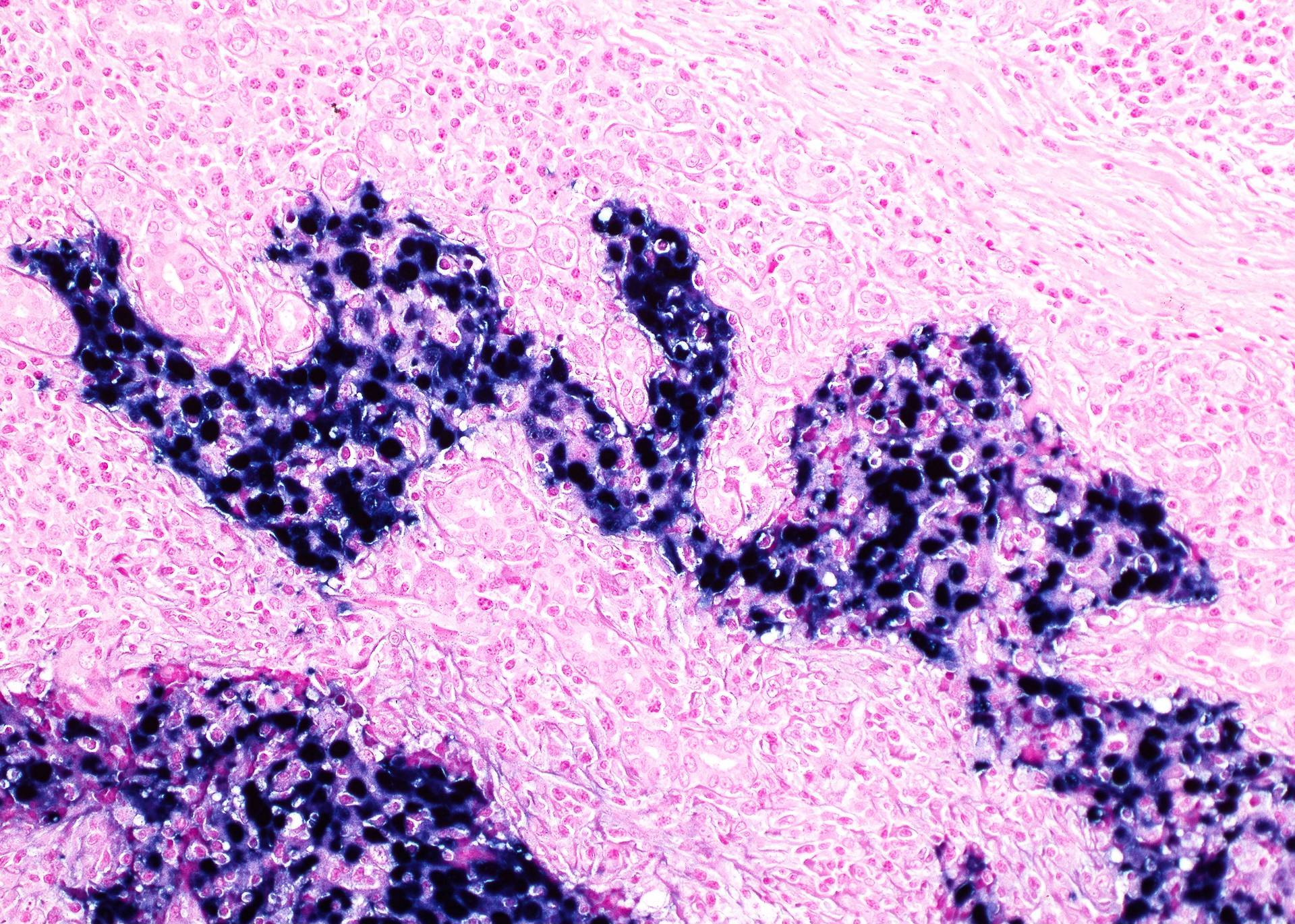
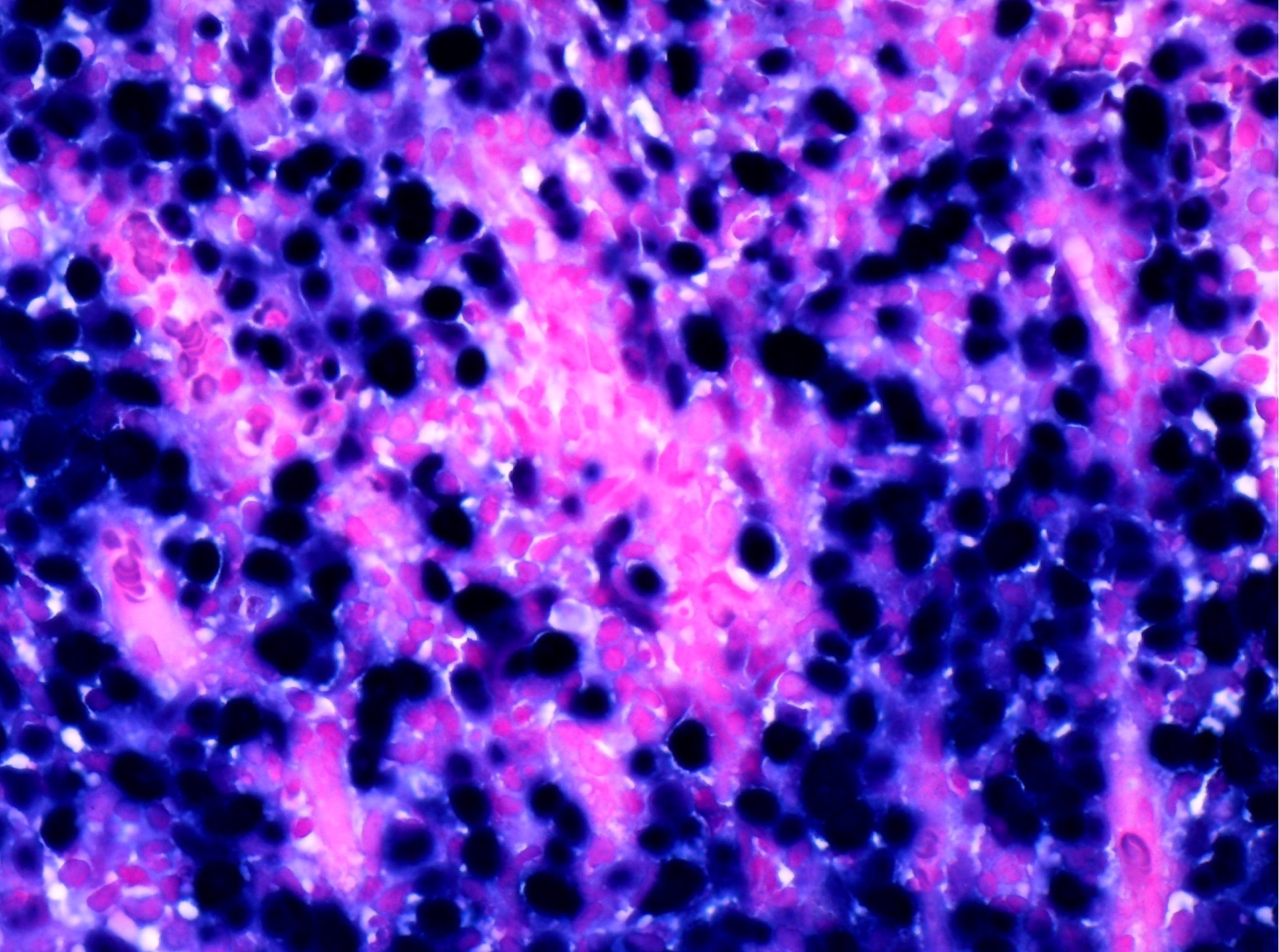
- Nonkeratinizing, undifferentiated subtype
- Either syncytial arrangement of cohesive cells with indistinct cell margins (Regaud pattern) or diffuse cellular infiltrate of noncohesive cells (Schmincke pattern) resembling non-Hodgkin lymphoma (growth patterns have no clinical significance)
- Tumor cells have moderate eosinophilic to amphophilic cytoplasm, round nuclei, prominent eosinophilic nucleoli, vesicular chromatin
- No significant keratinization
- Apoptosis and brisk mitotic activity are invariably present
- Usually (but not always) prominent nonneoplastic lymphoplasmacytic infiltrate accompanying the tumor
- Necrosis is uncommon
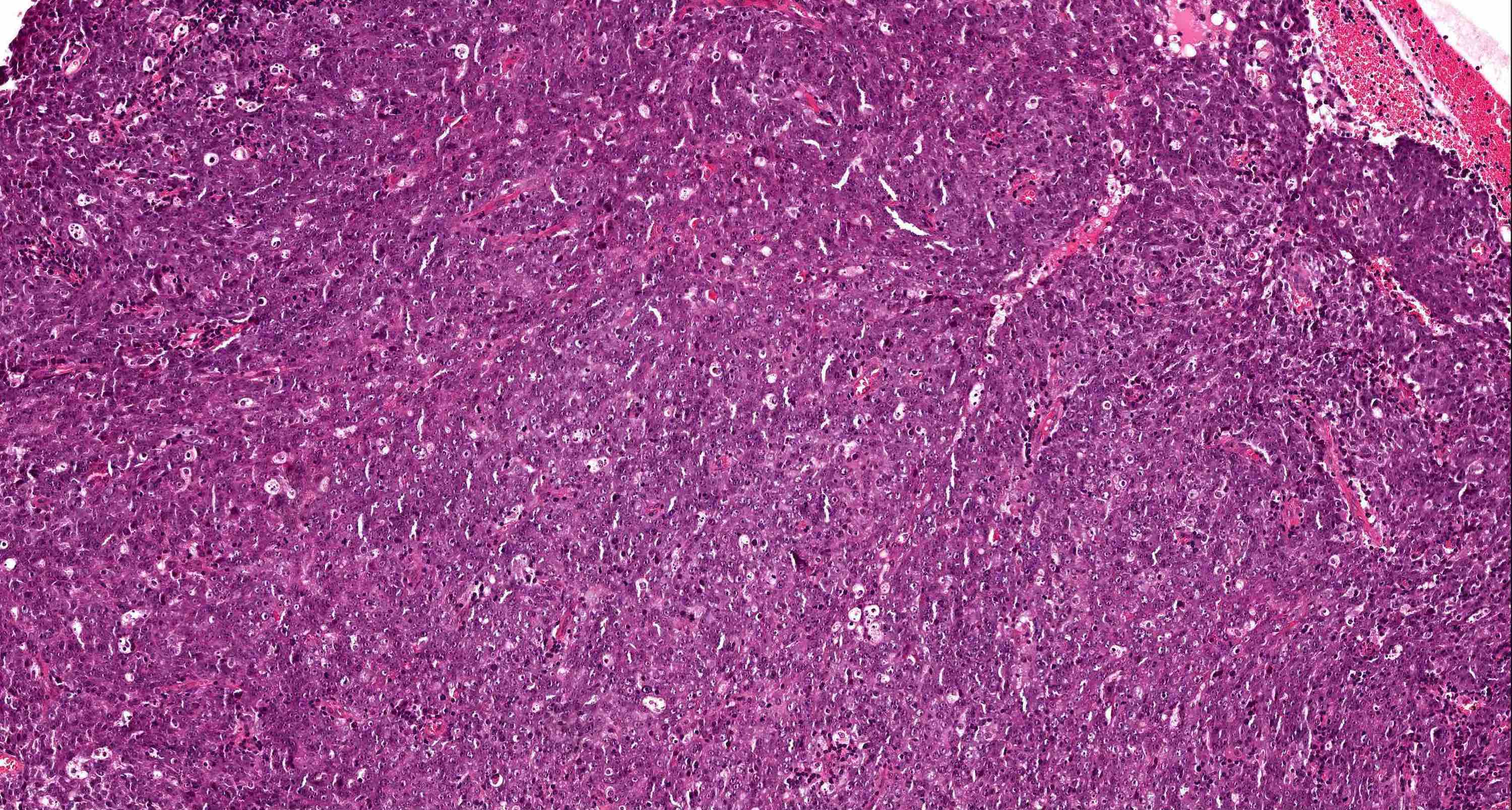
- Nonkeratinizing, differentiated subtype
- Usually interconnecting cords or trabeculae, with little or no keratinization; growth pattern is similar to urothelial carcinoma
- Tumor cells show well defined cell borders with variable intercellular bridges
- Background stroma demonstrates variable lymphoplasmacytic infiltrate
- Usually no desmoplastic response to invading tumor
- Subclassification of nonkeratinizing nasopharyngeal carcinoma into differentiated and undifferentiated subtypes is optional as it is not clinically or prognostically significant; if there is overlapping histology within the same tumor, classify according to the dominant component
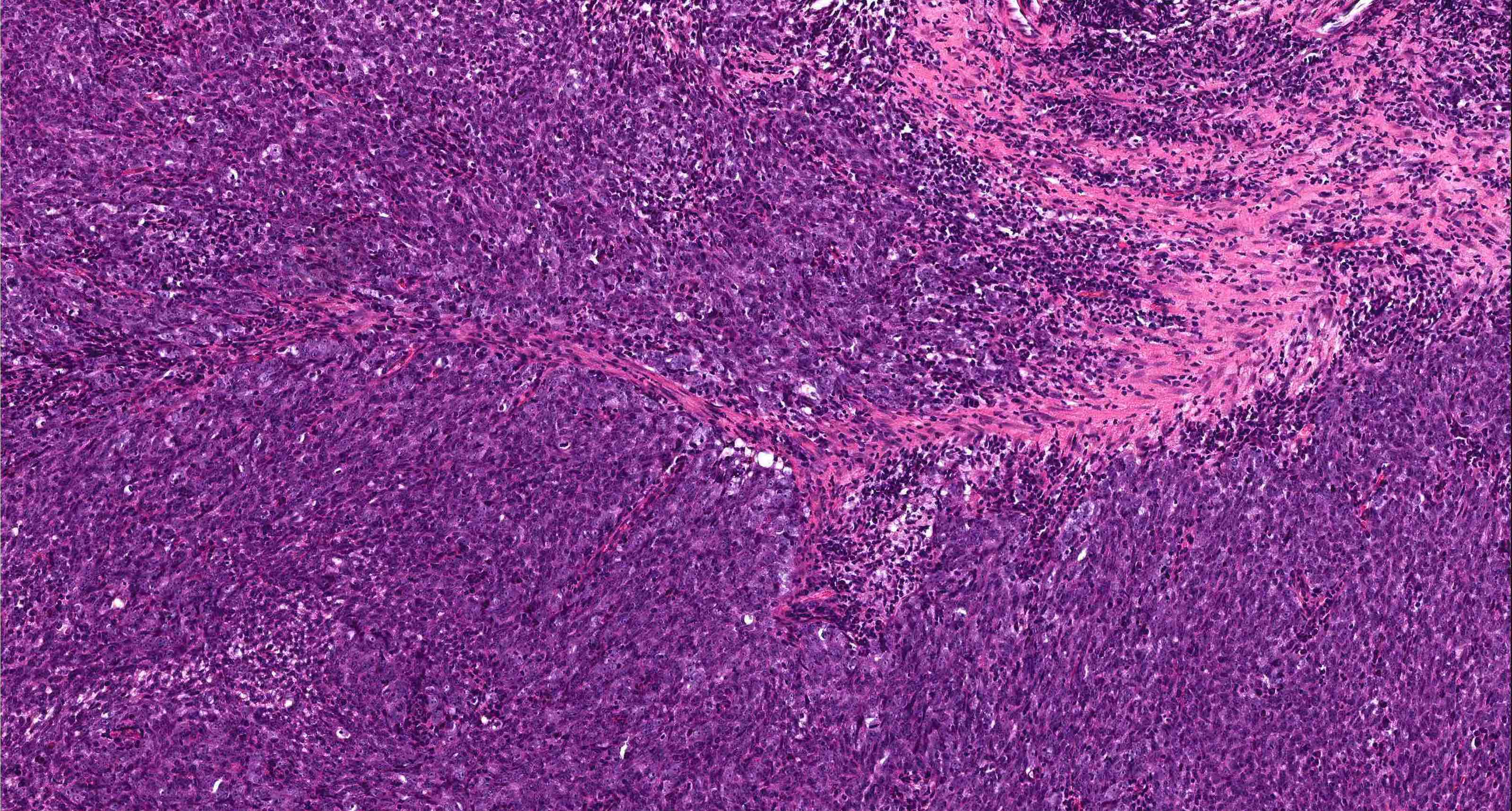
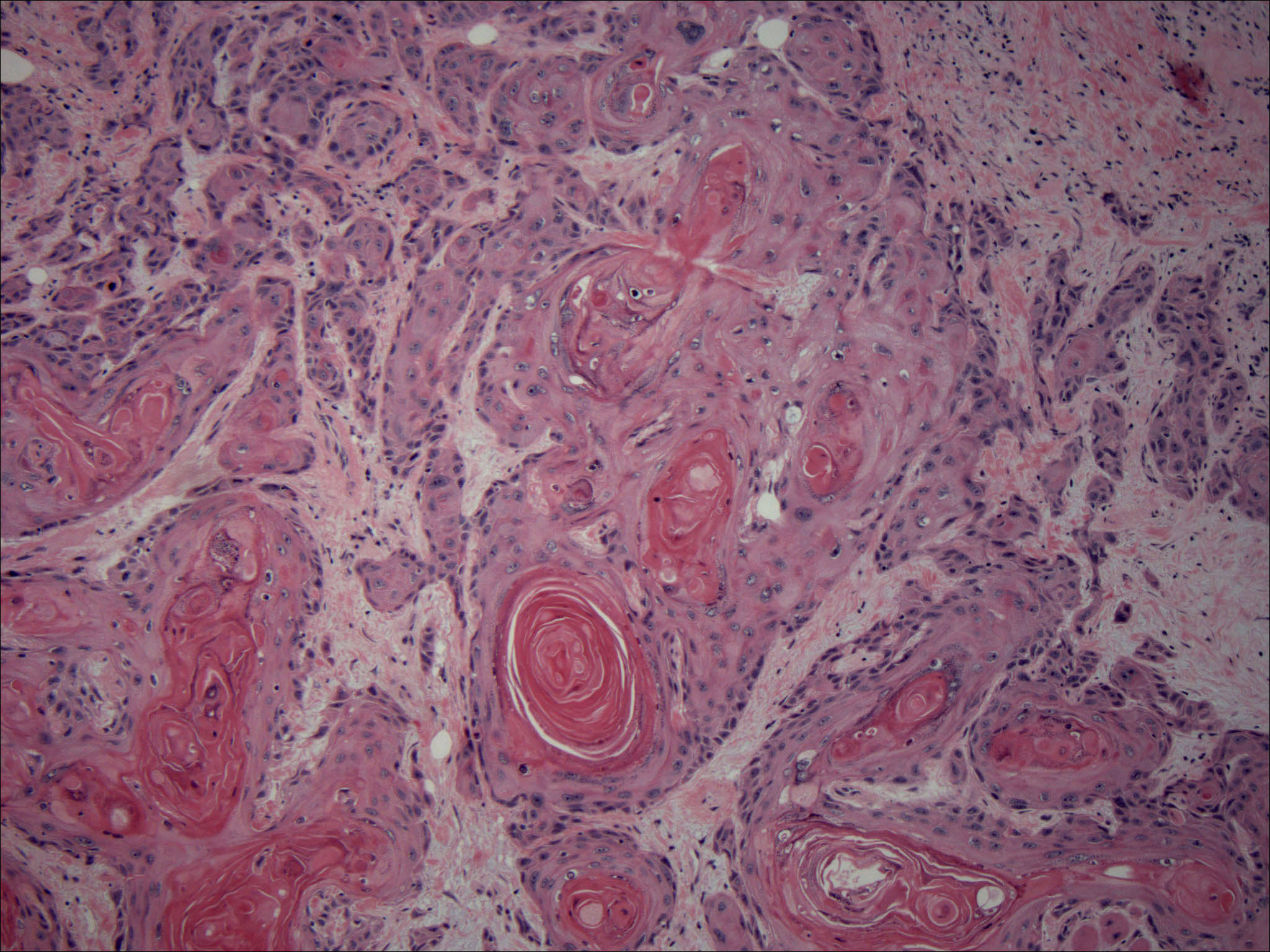
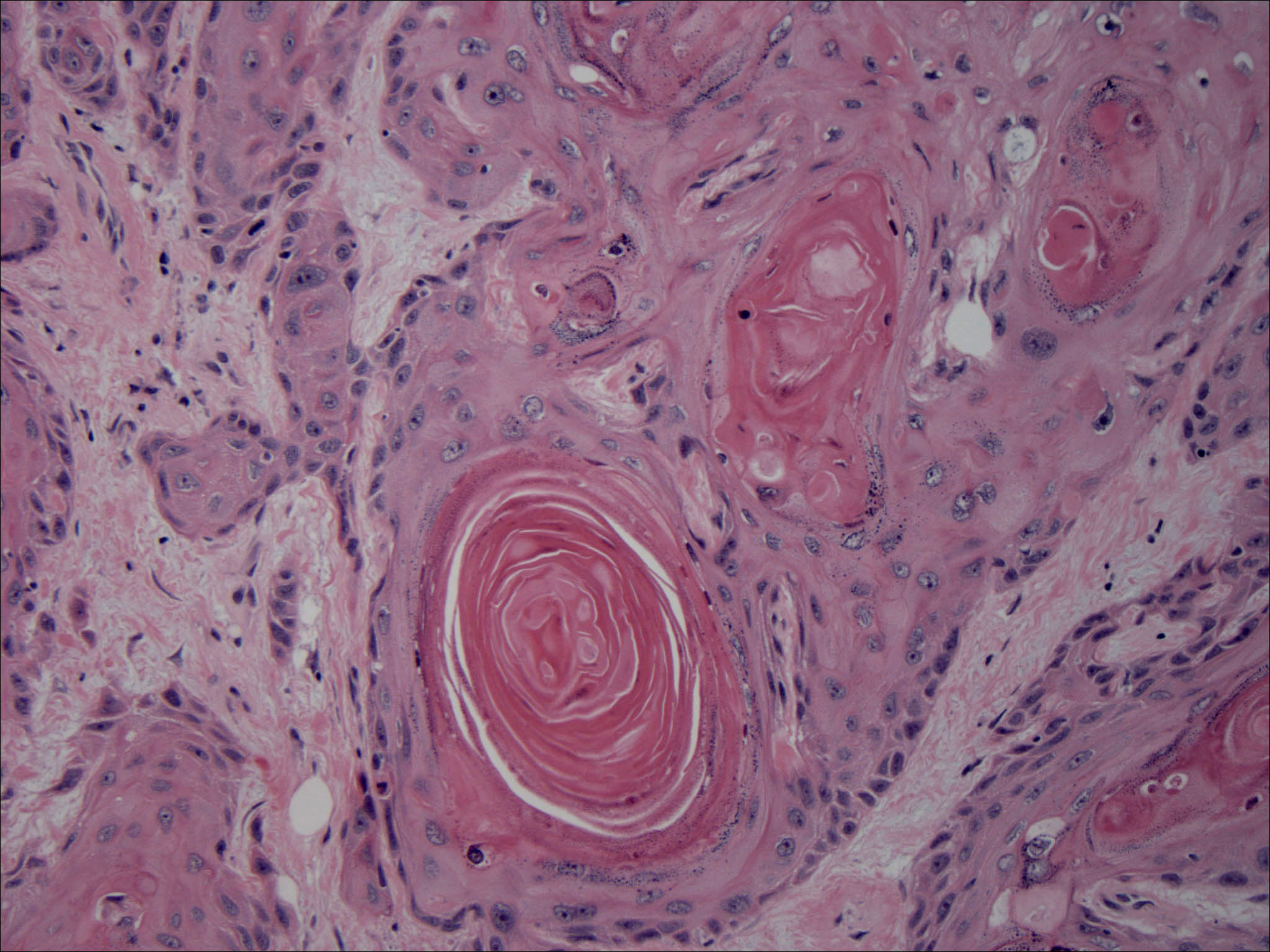
- Keratinizing subtype
- Indistinguishable from keratinizing squamous cell carcinoma of other body sites
- Obvious squamous differentiation as intercellular bridges and keratinization
- Can grade as well differentiated, moderately differentiated or poorly differentiated
- Desmoplastic response common
- Basaloid subtype
- Indistinguishable from basaloid squamous cell carcinoma of other body sites
- Tumor cells have high nuclear / cytoplasmic ratio with scanty cytoplasm, giving the basaloid appearance
- Basaloid tumor nests and sheets, often with peripheral palisading and central comedo type necrosis
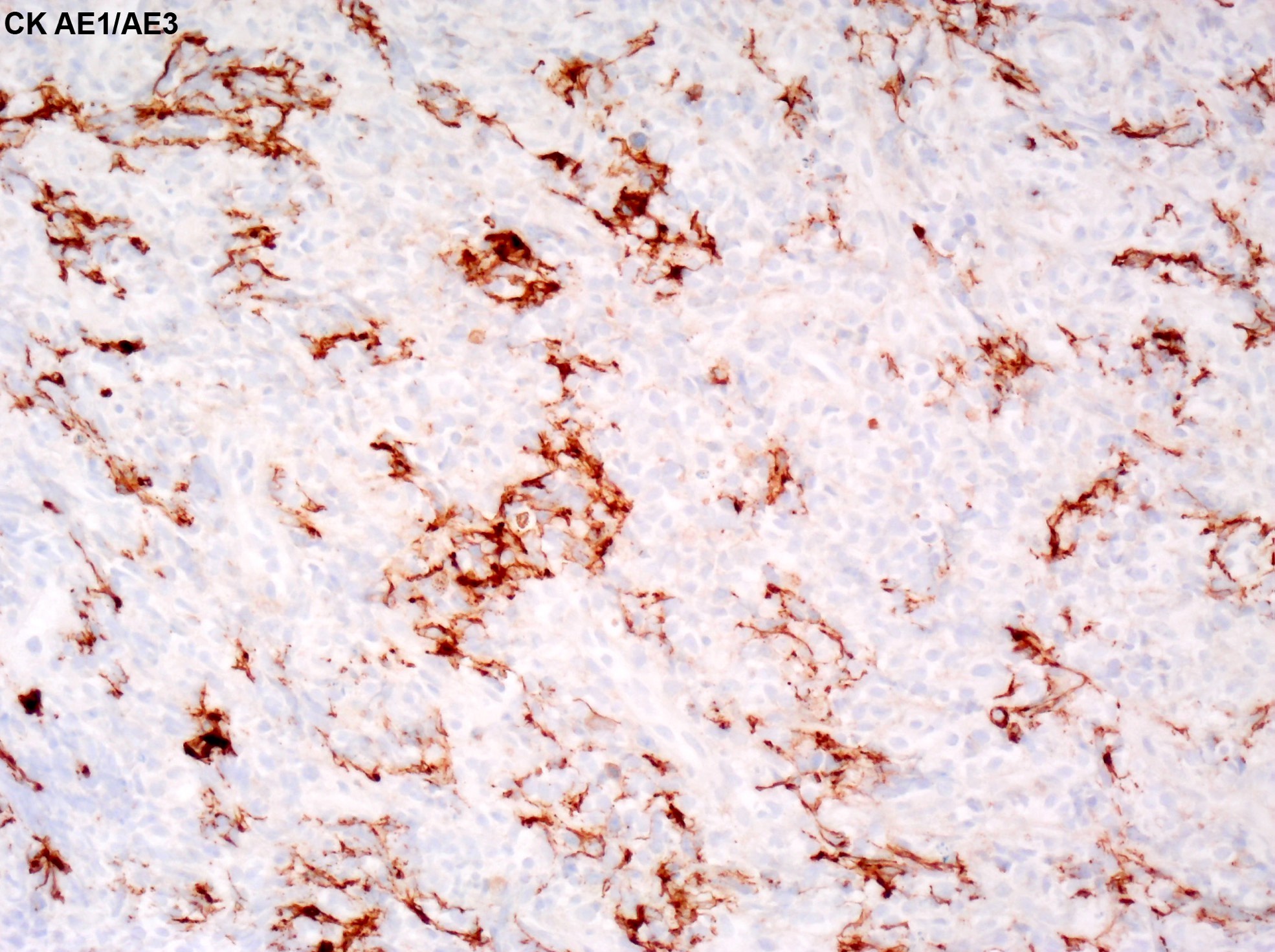
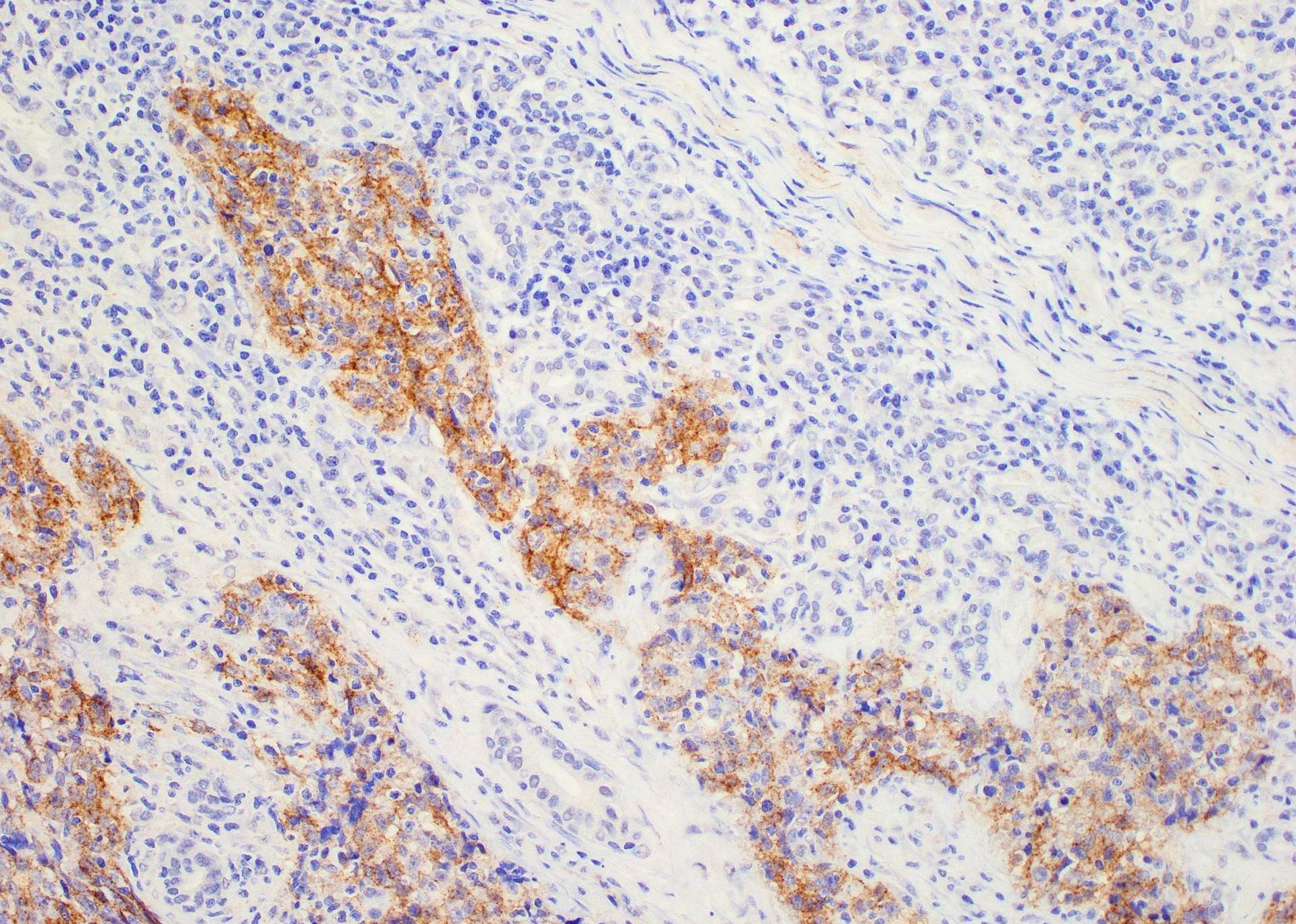
Microscopic (histologic) images
Contributed by Bin Xu, M.D., Ph.D. and Andrey Bychkov, M.D., Ph.D. and Songyang Yuan, M.D., Ph.D.
Nonkeratinizing, undifferentiated subtype
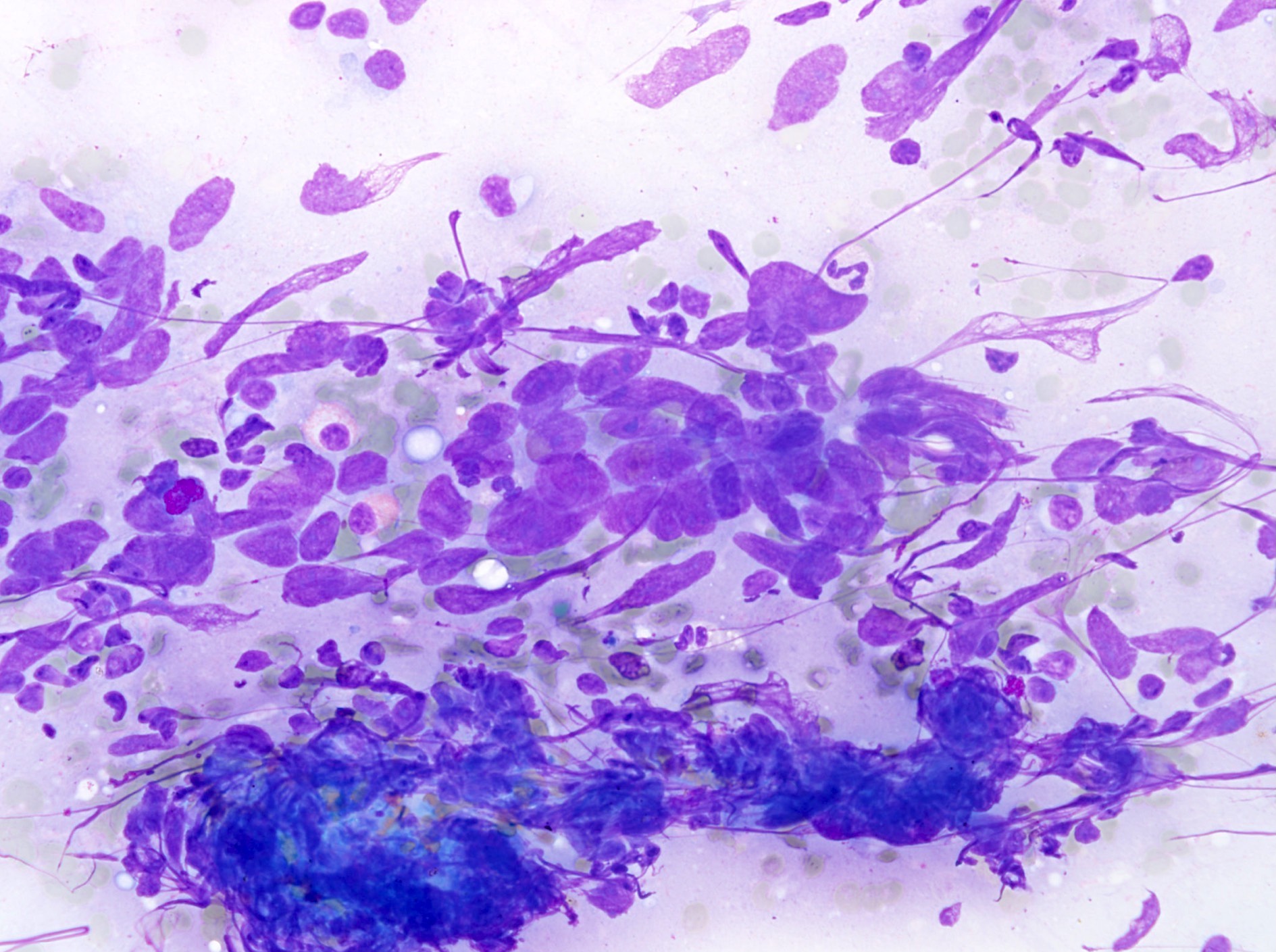
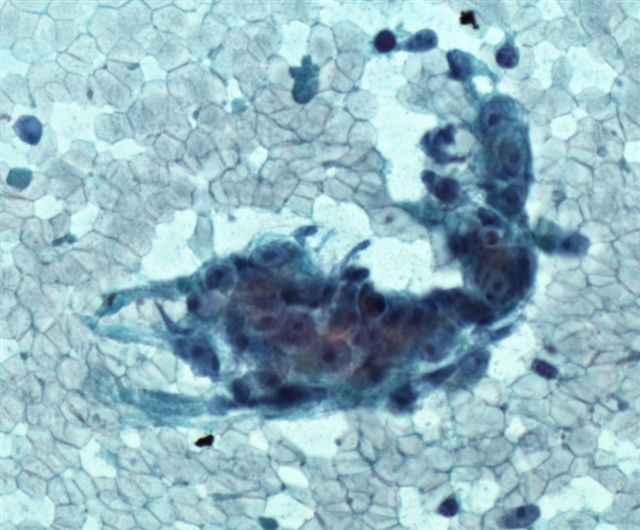
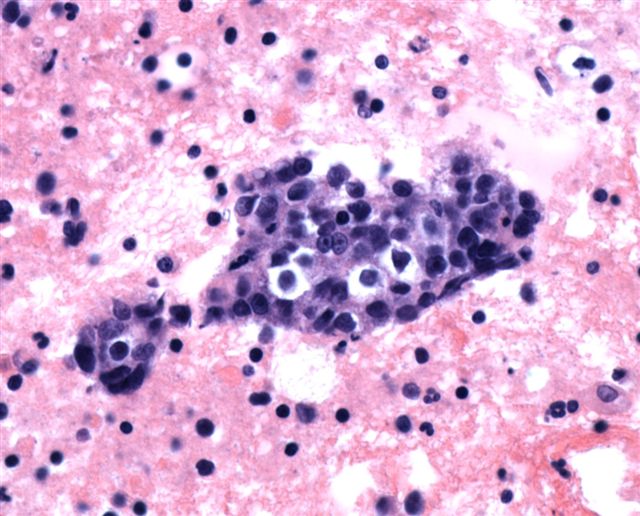
Cytology description
- Nonkeratinizing undifferentiated type shows clusters of tumor cells with indistinct cell border, vesicular nuclei and prominent central nucleoli
- Background lymphocytes and plasma cells are commonly seen
Cytology images
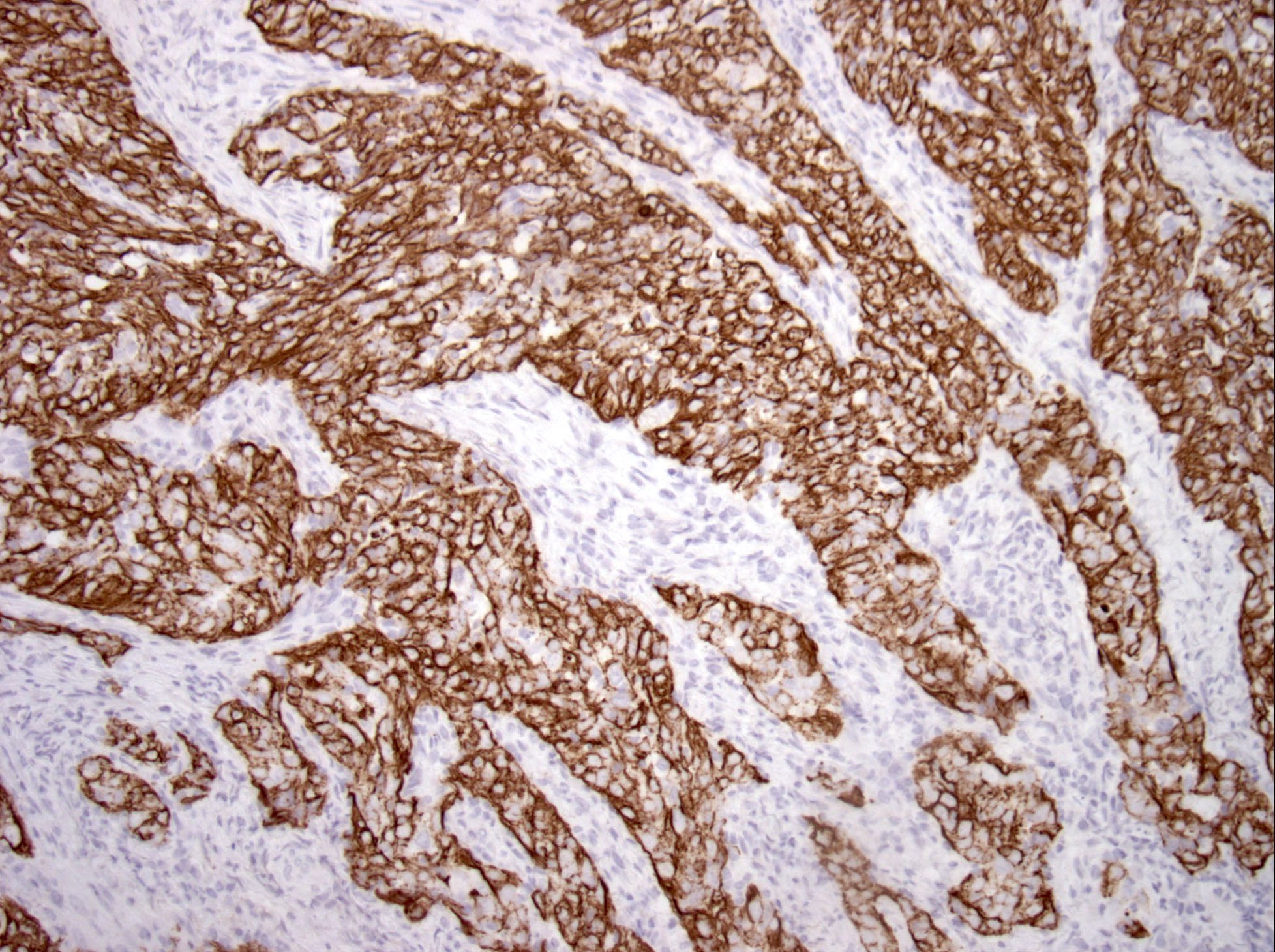
Positive stains
- EBV LMP is less specific and less widely used in North America but is used elsewhere
- Pancytokeratin, high molecular weight CK, p63 and p40 are strongly positive
- Rarely negative for high molecular weight CK and p40
Negative stains
Molecular / cytogenetics description
- Detection of Epstein-Barr virus (EBV) by PCR or ISH (EBER) found in 75 - 100% of cases
Molecular / cytogenetics images
Sample pathology report
- Nasopharynx, biopsy:
- Nasopharyngeal carcinoma, nonkeratinizing, undifferentiated type (see comment)
- Comment: In situ hybridization for Epstein-Barr virus (EBER) is positive in this tumor.
Differential diagnosis
- Diffuse large B cell lymphoma (DLBCL):
- Mucosal malignant melanoma:
- Primary mucosal melanoma of nasopharynx is exceedingly rare, with only a few case reports (J Cancer Res Ther 2014;10:416, J Craniofac Surg 2014;25:e567, J Contemp Brachytherapy 2013;5:157)
- Epithelioid and amelanotic melanoma may share some cytologic similarity; e.g. prominent nucleoli and syncytial sheet-like growth pattern
- Positive for S100, HMB45, MelanA, negative for CK and EBV
- Oropharyngeal nonkeratinizing squamous cell carcinoma:
- Usually nonkeratinizing and shares certain histologic similarities
- Over 85% are p16+ and HPV+ but negative for EBV, compared with nasopharyngeal carcinomas that are commonly related to EBV
- In the rare incidence of HPV related nasopharyngeal carcinoma, radiologic correlation to determine the location of the primary tumor is needed
- Rhabdomyosarcoma:
- Several subtypes of rhabdomyosarcoma, e.g., embryonal rhabdomyosarcoma (including the botryoid variant), alveolar rhabdomyosarcoma, spindle cell rhabdomyosarcoma and pleomorphic rhabdomyosarcoma, have been reported in sinonasal tract / nasopharynx
- Embryonal rhabdomyosarcoma and alveolar rhabdomyosarcoma can demonstrate a primitive small blue round cell morphology that could mimic undifferentiated nasopharyngeal carcinoma
- Positive for myogenic markers (desmin, myoglobin and myogenin), negative for CK and EBV
- Sinonasal undifferentiated carcinoma:
- Arises in nasal cavity and paranasal sinuses only, hyperchromatic tumor cells with coarse chromatin, individual cell necrosis and necrosis of cell nests
- EBER- (Am J Surg Pathol 2002;26:371)
Additional references
Board review style question #1
A recent immigrant from Hong Kong presented with nasal discharge and a nasopharyngeal mass was biopsied. Which of the following statements is true?
- In the United States, the lesion most commonly affects African Americans
- Lesion commonly shows a squamous immunophenotype (i.e. positive for high molecular weight cytokeratin and p40)
- Lesion is most commonly associated with high risk human papillomavirus (HPV)
- Surgery is the standard treatment modality for this lesion
Board review style answer #1
B. Lesion commonly shows a squamous immunophenotype (i.e. positive for high molecular weight cytokeratin and p40)
Comment Here
Reference: Nasopharyngeal carcinoma
Comment Here
Reference: Nasopharyngeal carcinoma
Board review style question #2
Which of the following statements about nasopharyngeal carcinoma is true?
- B cell clonality may be demonstrated in the undifferentiated type of nonkeratinizing nasopharyngeal carcinoma
- Most common subtype of nasopharyngeal carcinoma is the keratinizing type
- Nasopharyngeal carcinoma may be related to EBV or HPV
- Nasopharyngeal carcinoma predominantly affects patients from South America
Board review style answer #2
C. Nasopharyngeal carcinoma may be related to EBV or HPV
Comment Here
Reference: Nasopharyngeal carcinoma
Comment Here
Reference: Nasopharyngeal carcinoma