Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Xu B. Sinonasal papilloma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/nasalsinonasalpapilloma.html. Accessed April 19th, 2024.
Definition / general
- Sinonasal papilloma is a benign epithelial neoplasm of sinonasal tract
- WHO has divided sinonasal papilloma into 3 distinct types (El-Naggar: WHO Classification of Head and Neck Tumours, 4th Edition, 2017):
- Inverted papilloma
- Exophytic papilloma
- Oncocytic papilloma
Essential features
| Comparison of essential features of the 3 types of sinonasal papilloma | |||
| Inverted papilloma | Exophytic papilloma | Oncocytic papilloma | |
| Frequency | Most common | Second most common | Least common |
| Location | Lateral nasal wall / paranasal sinus | Nasal septum | Lateral nasal wall / paranasal sinus |
| Male to female ratio | 2 - 3:1 | 10:1 | 1:1 |
| Most common age of presentation | 5th to 6th decades | 3rd to 5th decades | 5th to 6th decades |
| Association with human papillomavirus (HPV) | High risk HPV Low risk HPV | Low risk HPV | No association |
| Architectural pattern | Endophytic (inverted) | Exophytic (filiform) | Exophytic or endophytic |
| Epithelial lining | Squamous, transitional or respiratory | Squamous, transitional or respiratory | Oncocytic |
| Molecular alterations | EGFR activating mutation | None reported | KRAS mutation |
| Risk of malignant transformation | 5 - 15% | ~0% | 4 - 17% |
Terminology
- Other terminologies that have been used in the literature and previous versions of WHO classification include:
- All types: Schneiderian papilloma and epithelial papilloma
- Exophytic type: transitional cell papilloma, fungiform papilloma, Ringertz papilloma and septal papilloma
- Oncocytic type: cylindrical cell papilloma and columnar cell papilloma
Epidemiology
- Annual incidence is 0.74 - 2.3 per 100,000 population (El-Naggar: WHO Classification of Head and Neck Tumours, 4th Edition, 2017)
- Inverted papilloma is the most common subtype, followed by exophytic papilloma; oncocytic papilloma is the least common
- Inverted and oncocytic papilloma most commonly affect patients in their 5th to 6th decades, while exophytic papilloma occurs in 3rd to 5th decades
- Inverted and exophytic papilloma occur more frequently in males, with a male to female ratio of 2 - 3:1 and 10:1, respectively; oncocytic papilloma affects both genders equally (Head Neck Pathol 2017;11:269)
Sites
- Sinonasal papilloma commonly affects nasal cavity or paranasal sinuses
- Exophytic papilloma is typically located in the nasal septum, while the inverted and oncocytic types predominantly affect lateral nasal wall or paranasal sinuses
- Inverted papilloma may secondarily extend to nonsinonasal sites, e.g. pharynx, ear, cranial cavity
- Sinonasal papilloma is usually unilateral; bilateral involvement is rare
Etiology
- Role of high risk human papillomavirus (HPV) in inverted papilloma remains controversial
- Reported rate of high risk HPV in inverted papilloma and carcinoma ex inverted papilloma ranges from 0 - 100% (World J Otorhinolaryngol Head Neck Surg 2016;3:54, Head Neck Pathol 2017;11:269)
- WHO gives a frequency of 38.5% in inverted papilloma (El-Naggar: WHO Classification of Head and Neck Tumours, 4th Edition, 2017)
- Low risk HPV, especially types 6 and 11, has also been detected in inverted papilloma and is more common than high risk HPV
- Other etiologic factors implicated in inverted papilloma include exposure to welding, organic solvents and smoking (World J Otorhinolaryngol Head Neck Surg 2016;3:54)
- Exophytic papilloma may be related to low risk HPV, especially types 6 and 11
- No significant association between oncocytic papilloma and HPV (Head Neck Pathol 2017;11:269)
Clinical features
- Symptoms are usually nonspecific, including nasal congestion, nasal obstruction, nasal discharge or epistaxis
Diagnosis
- Relies on histology in biopsy or surgical resection
Radiology images
Prognostic factors
- Increased risk of recurrence if involvement of sphenoid sinus, frontal sinus or maxillary sinus walls other than medial or extrasinus extension (Biomed Res Int 2017;2017:9195163)
- Major cause of recurrence is incomplete resection
- Risk of malignant transformation is ~9% in inverted papilloma (range: 5 - 15%) (Eur Arch Otorhinolaryngol 2017;274:2991)
- 4 - 17% of oncocytic papilloma undergo malignant transformation
- Exophytic papilloma is not associated with an increased incidence of carcinoma
Case reports
- 46 year old man with inverted papilloma of the middle ear (Braz J Otorhinolaryngol 2012;78:122)
- 48 year old man and 56 year old man with inverted papilloma of the maxillary sinus (Rom J Morphol Embryol 2016;57:289)
- 60 year old man with inverted papilloma of the lacrimal sac (J Cancer Res Ther 2015;11:238)
- 74 year old woman with inverted papilloma of the temporal bone (BMJ Case Rep 2013;2013:bcr2013201219)
- 82 year old man with oncocytic papilloma of the maxillary sinus mimicking lymphoma (Medicine (Baltimore) 2016;95:e4646)
Treatment
- Complete surgical excision through endoscopic surgery or open radical procedure is the treatment of choice (Clin Otolaryngol 2006;31:499)
- Aim is to completely remove all diseased mucosa; lateral rhinotomy and medial maxillectomy may be required for inverted or oncocytic papilloma
- If treated with local excision only, 50 - 70% may recur, particularly for inverted subtype
Clinical images
Gross description
- Inverted papilloma: pink-tan-gray, soft to moderately firm polypoid growth with convoluted or wrinkled surface
- Exophytic papilloma: usually mushroom shaped and exophytic with papillary appearance
- Oncocytic papilloma: fleshy polypoid growth of variable color
- Generous or complete sampling is advised to search for focus of malignant transformation
Microscopic (histologic) description
Inverted papilloma:
Exophytic papilloma:
Oncocytic papilloma:
Malignant transformation (carcinoma ex sinonasal papilloma):
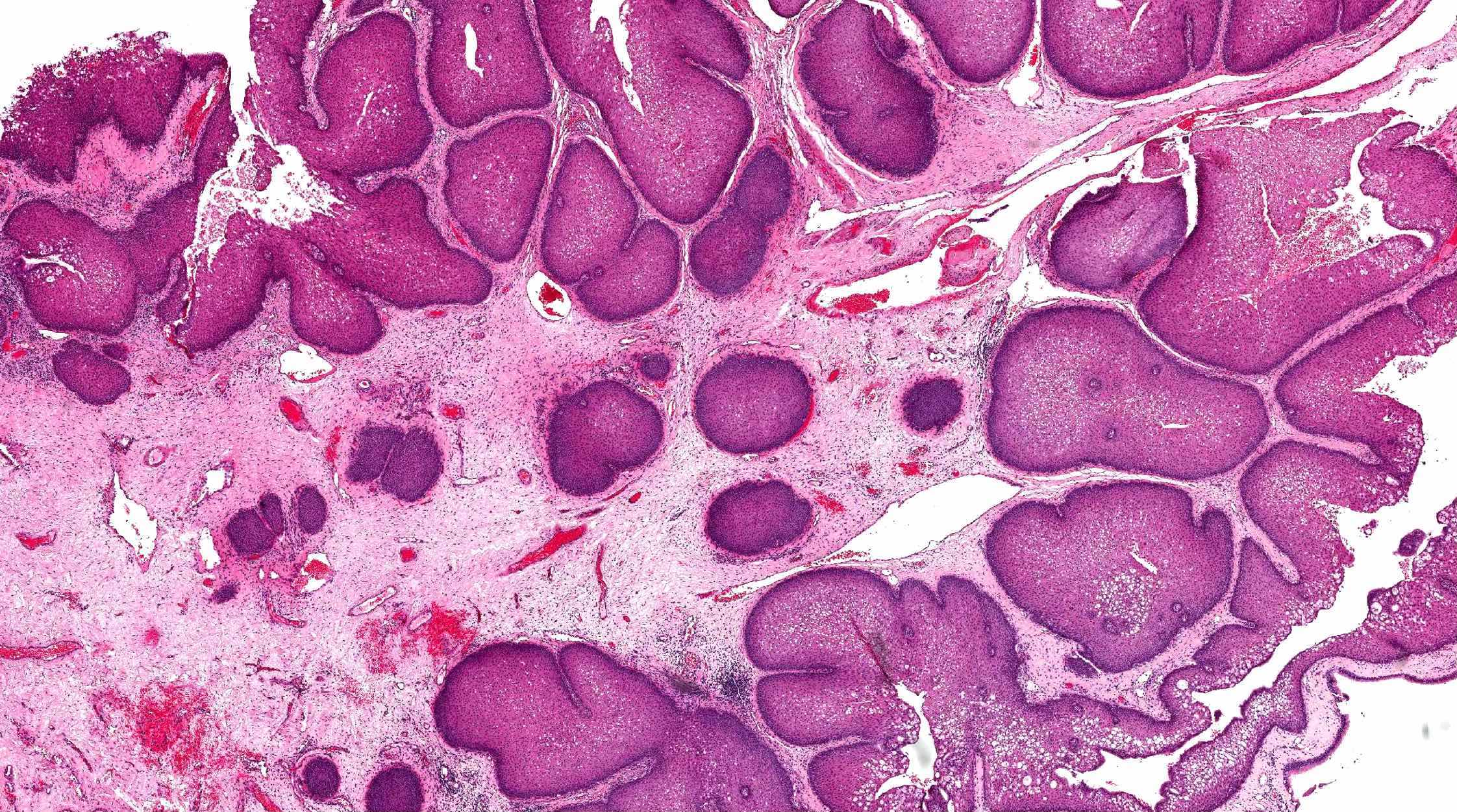
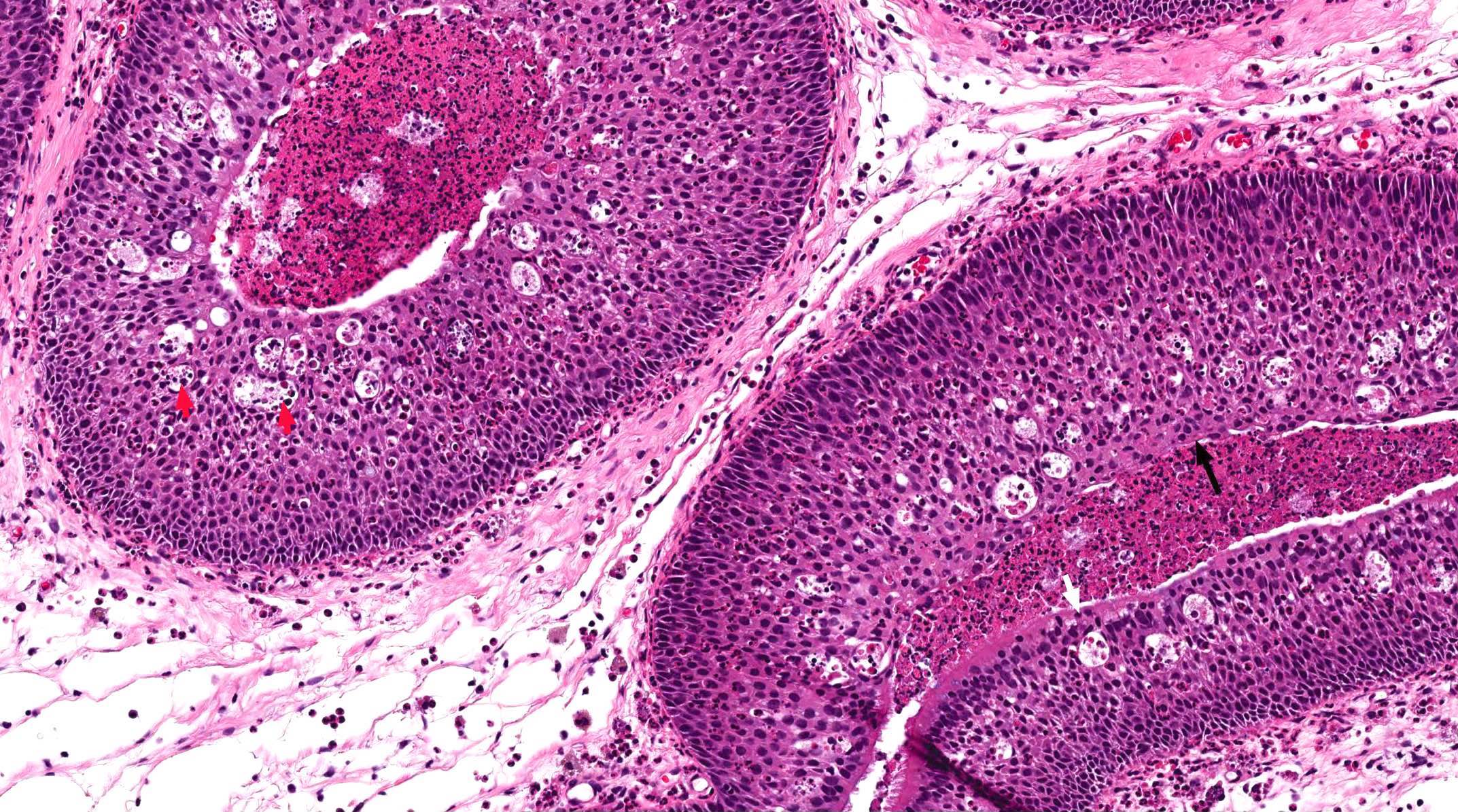
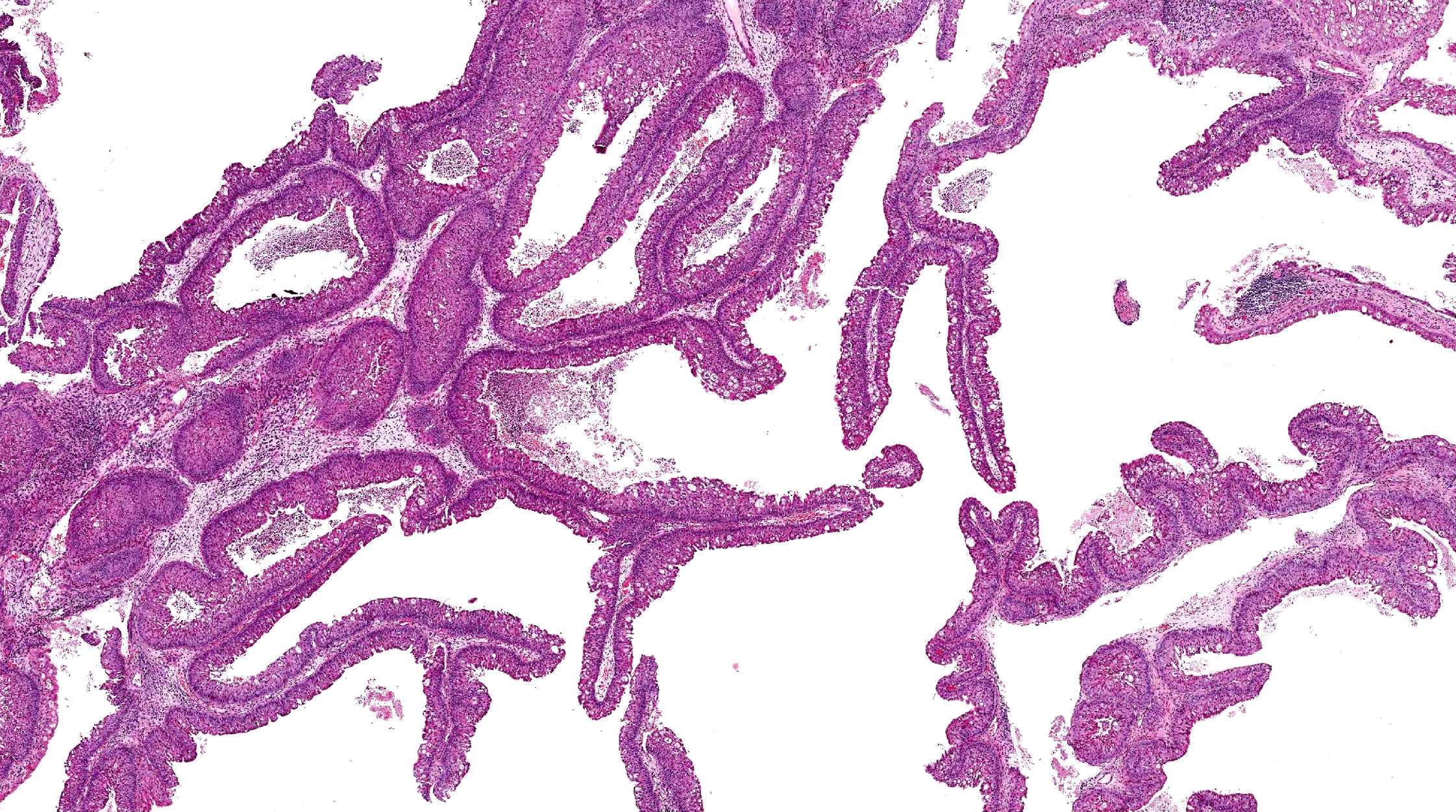
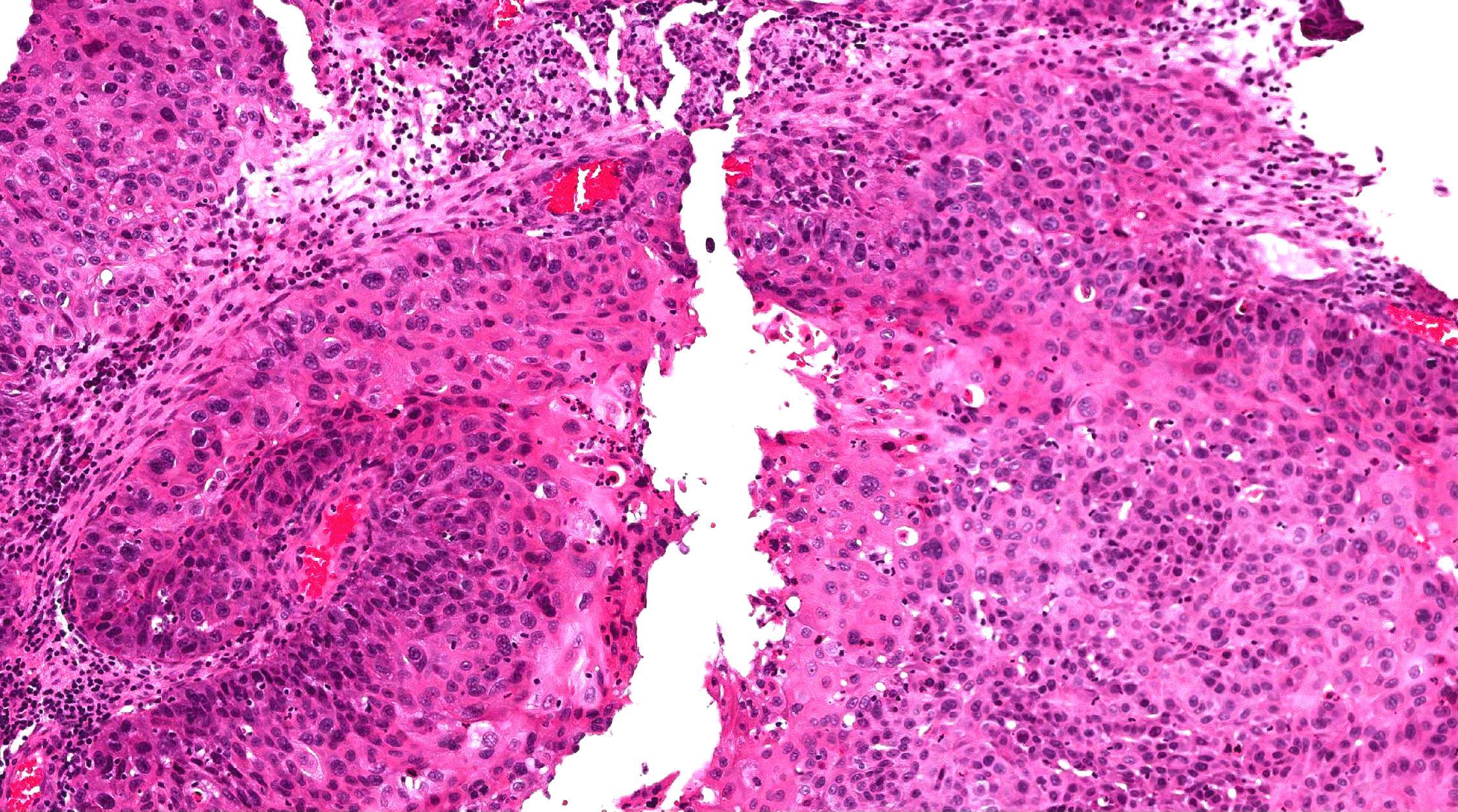
- Architecture: prominent downward endophytic growth of round to elongated interconnected epithelial nests with smooth outer contour
- Epithelium is hyperplastic (5 - 30 cell layers in thickness) and may be of squamous, transitional or respiratory type
- Transmigrating neutrophils and neutrophilic microabscesses may be seen
- Stroma may have edema or chronic inflammation
- Seromucinous gland in the lamina propria is commonly decreased or absent
Exophytic papilloma:
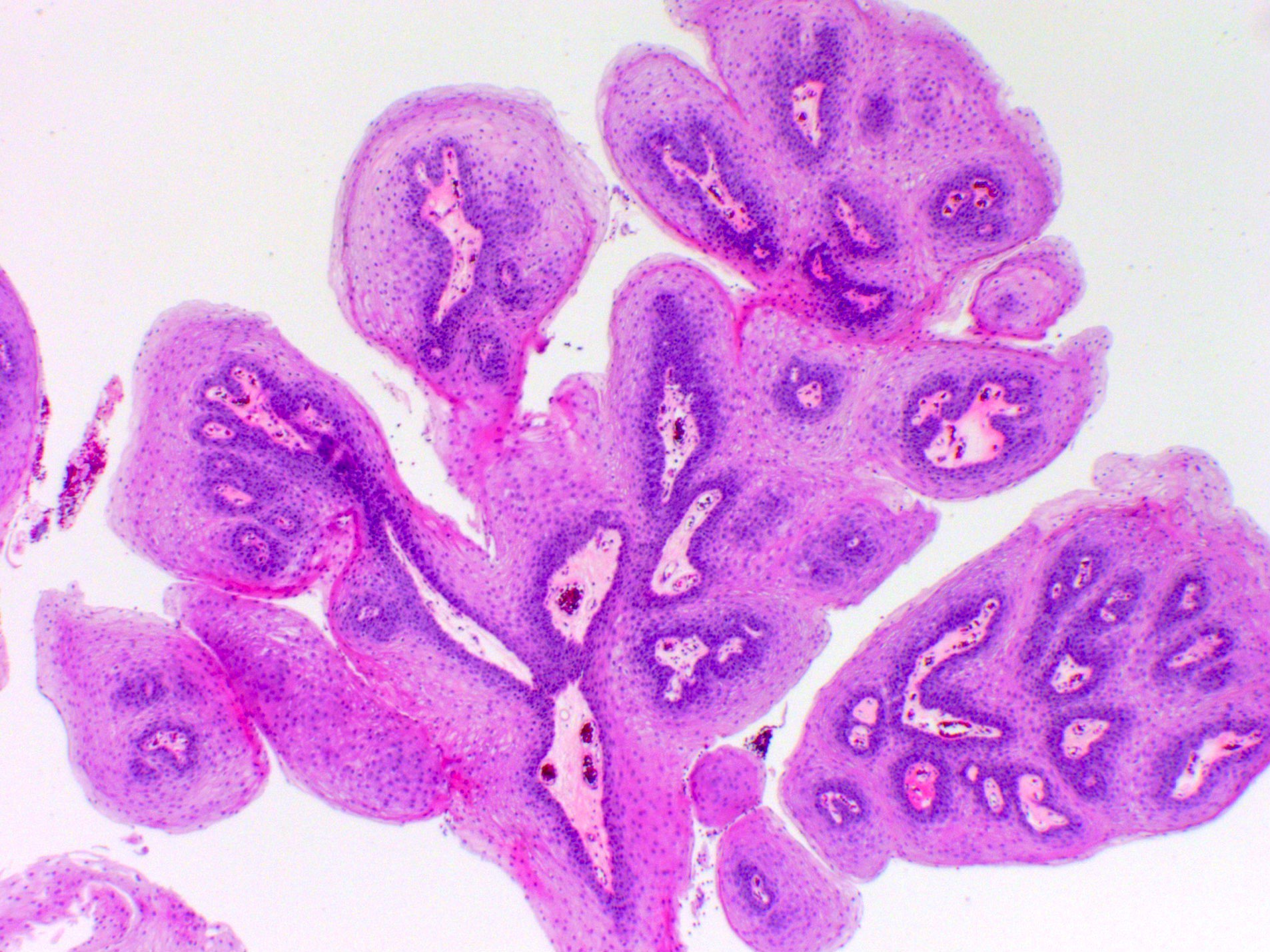
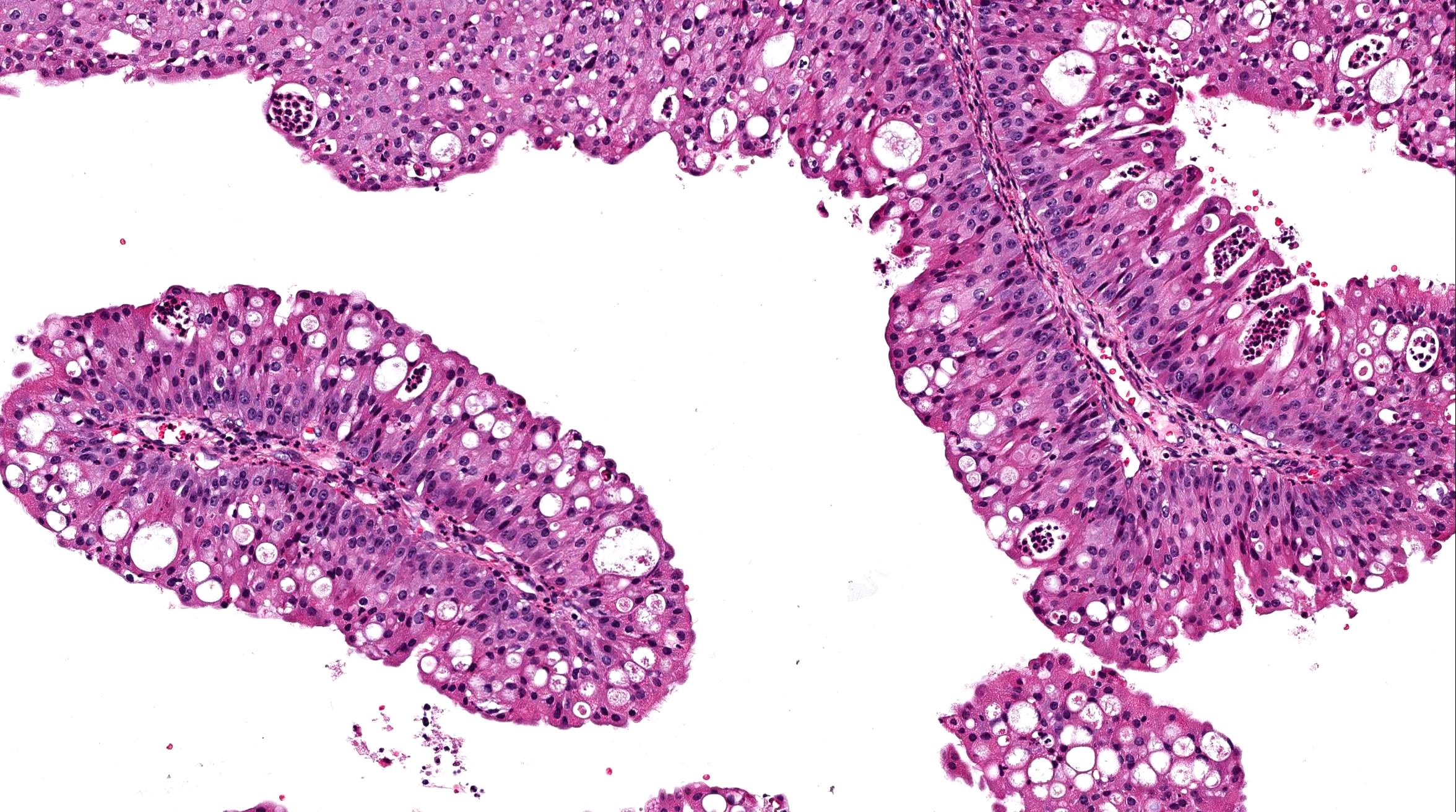
- Architecture: filiform or papillary arrangement with delicate fibrovascular core
- Epithelial lining can be either squamous, respiratory or transitional; it may contain mucus secreting cells and goblet cells
- Variable koilocytosis may be present
- Usually no / scant surface keratinization
- Mitotic figures are absent or limited to the basal layer
- Minimal inflammatory cells
Oncocytic papilloma:
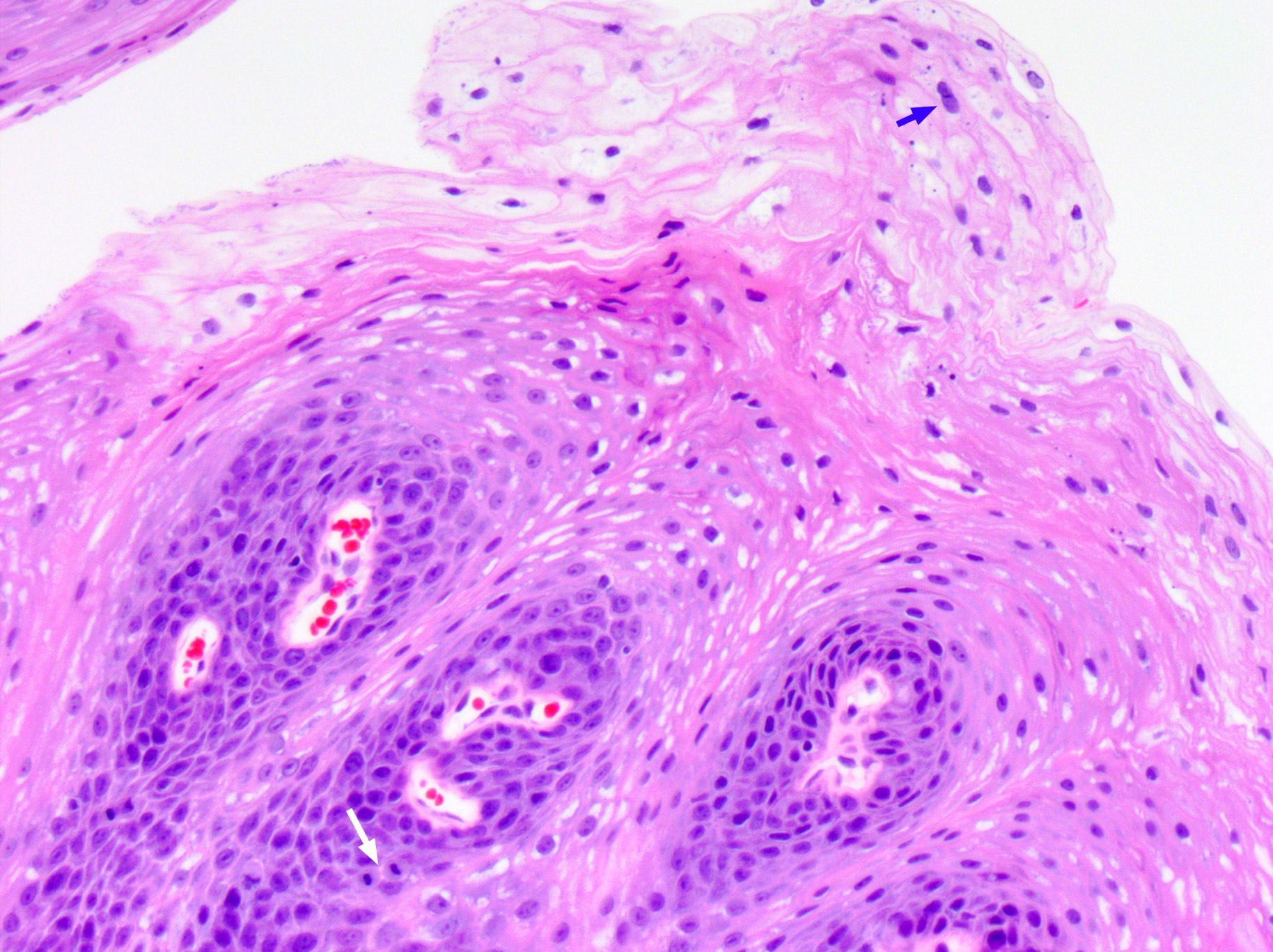
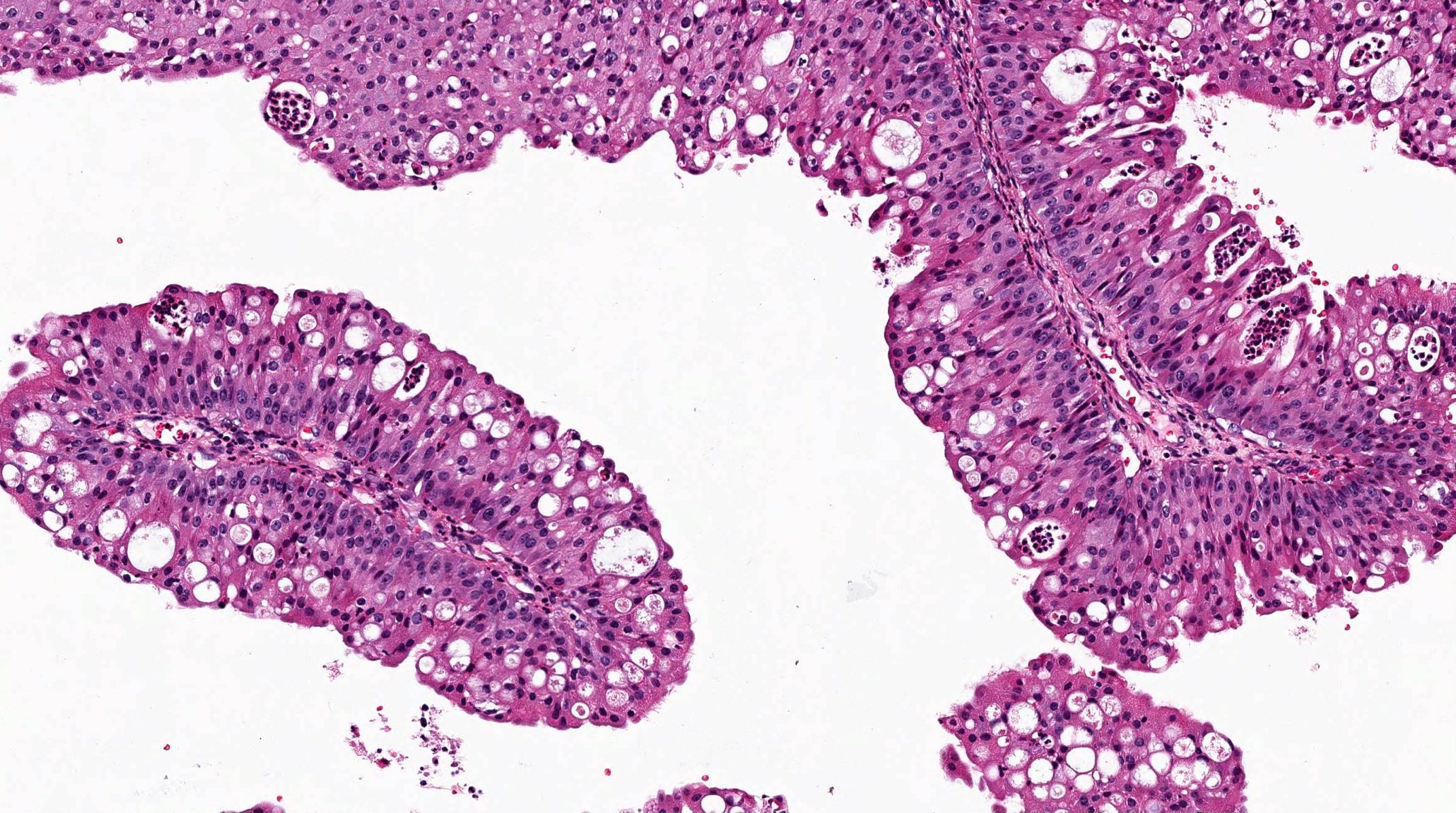
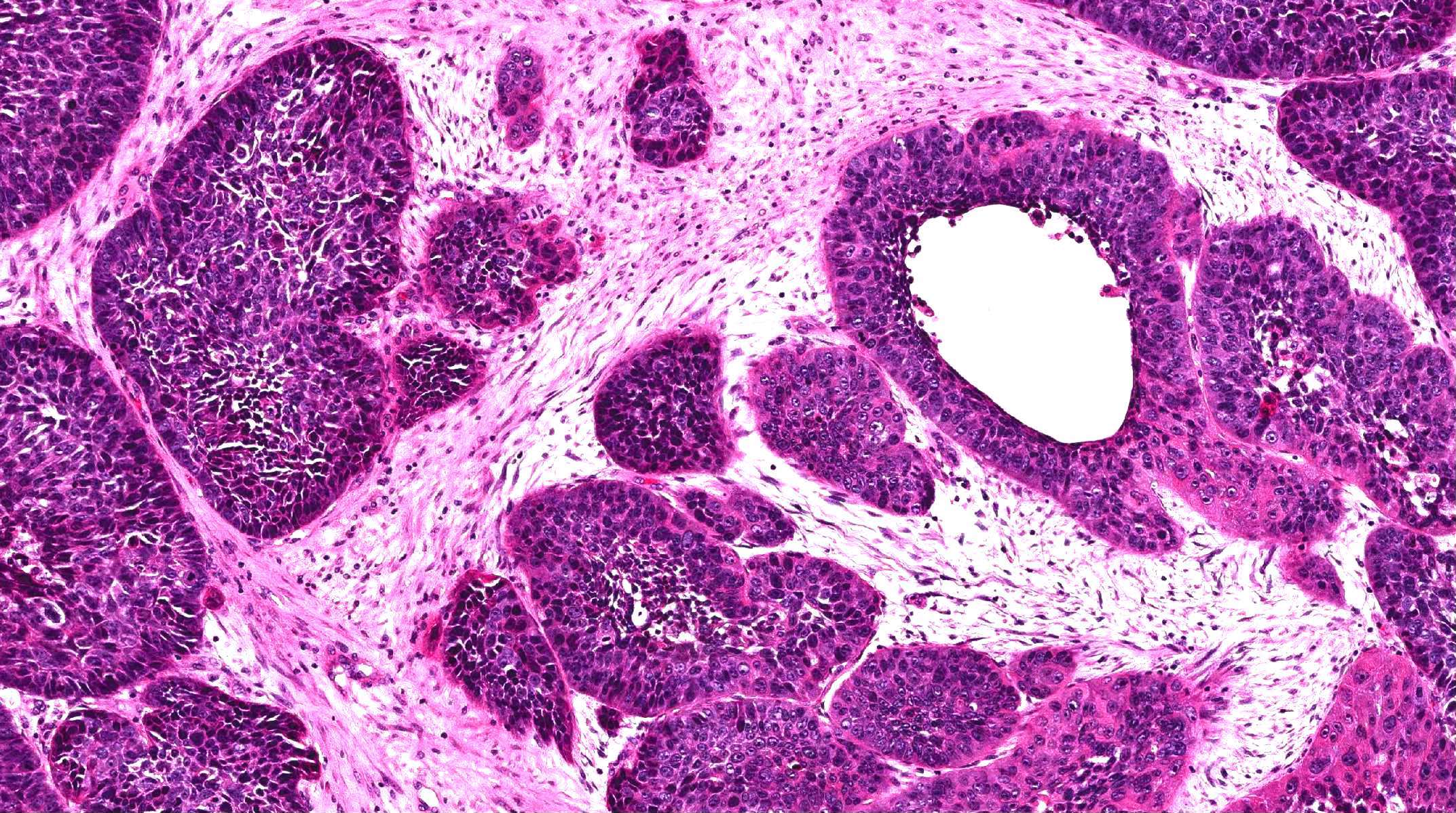
- Architecture: may have endophytic (inverted) or exophytic growth patterns
- Epithelial lining is pseudostratified and columnar with abundant eosinophilic granular cytoplasm and hyperchromatic uniform nuclei
- Intraepithelial mucin filled cysts with neutrophilic microabscesses may be seen
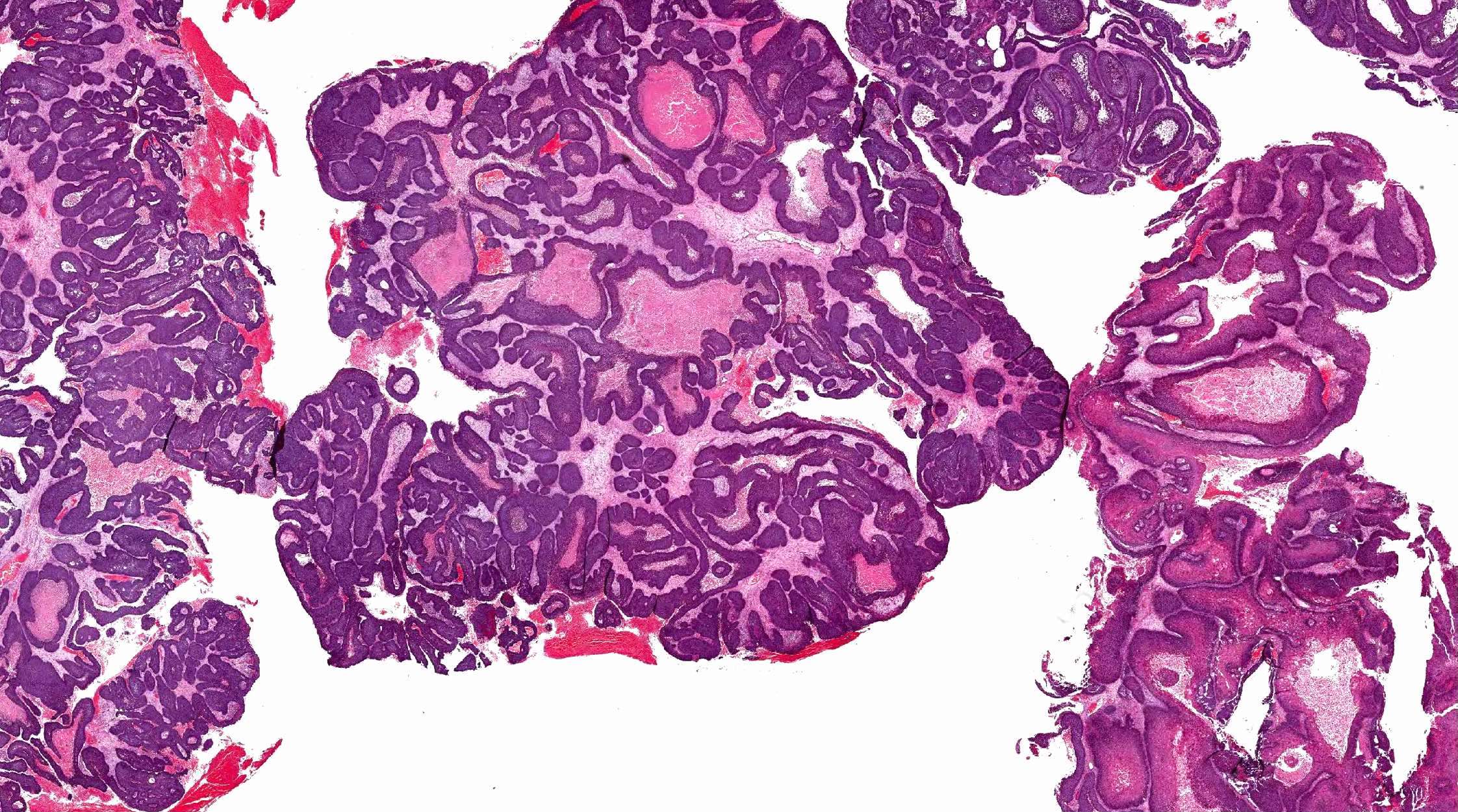
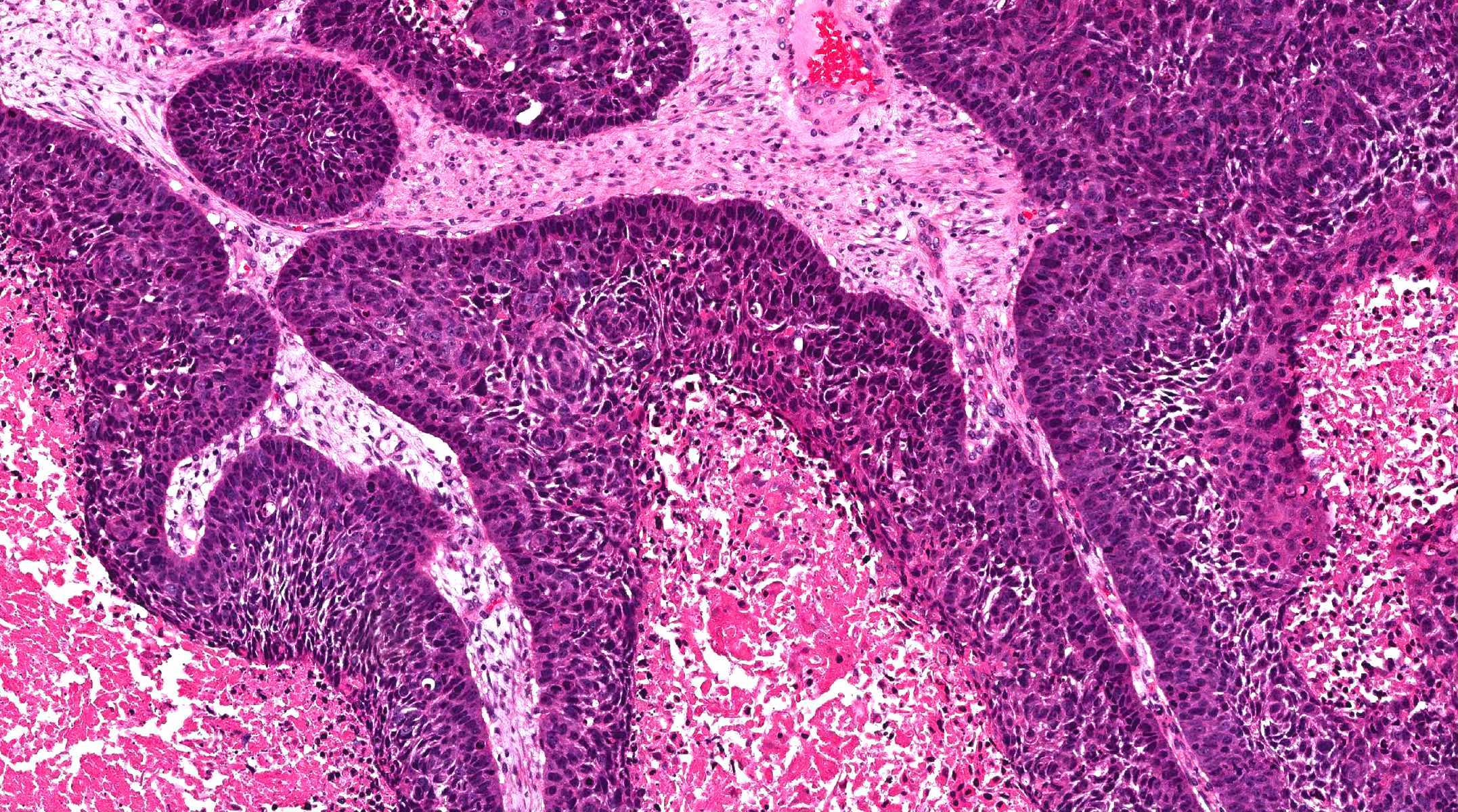
Malignant transformation (carcinoma ex sinonasal papilloma):
- Most common type of carcinoma arising in sinonasal papilloma is squamous cell carcinoma
- Other types of carcinoma that have been reported include verrucous carcinoma, mucoepidermoid carcinoma, small cell carcinoma and sinonasal undifferentiated carcinoma (Head Neck Pathol 2017;11:269)
- Carcinoma is characterized by marked nuclear pleomorphism and hyperchromasia, frequent mitotic figures beyond basal layer including the atypical forms, tumor necrosis and frank invasion with infiltrative irregular nests and desmoplastic stromal reaction
Microscopic (histologic) images
Positive stains
- Cytokeratin AE1 / AE3, CK7, CK5 / 6 (in squamous lining), p40 (in squamous lining)
Molecular / cytogenetics description
- Inverted papilloma may be positive for low risk or high risk HPV by in situ hybridization
- Exophytic papilloma may be positive for low risk HPV by in situ hybridization
- 88% of inverted papilloma and 77% of carcinoma ex inverted papilloma harbor EGFR mutations (Cancer Res 2015;75:2600)
- Most oncocytic papillomas, including those with malignant transformation, have KRAS mutations (J Pathol 2016;239:394)
Sample pathology report
- Maxillary sinus, left; biopsy:
- Sinonasal papilloma, inverted type
Differential diagnosis
- Cutaneous squamous papilloma:
- May involve nasal vestibule and become a differential diagnosis for exophytic papilloma
- May show surface keratinization
- Lacks mucocytes and ciliated respiratory epithelium
- May contain skin adnexa but lacks seromucinous glands
- Nonintestinal type sinonasal adenocarcinoma:
- Has oncocytic cytomorphologic features and is a differential diagnosis for oncocytic papilloma
- Characterized by complex, confluent, back to back glandular proliferation, while oncocytic papilloma has a simple exophytic or endophytic growth pattern without architectural complexity
- High grade tumors may show marked nuclear atypia
- Nonkeratinizing squamous cell carcinoma:
- Infiltrative growth, irregular border, marked nuclear atypia, frequent mitoses, desmoplastic reaction, unequivocal invasion and tumor necrosis
- Respiratory epithelial adenomatoid hamartoma:
- Downward proliferation of respiratory mucosa can mimic inverted papilloma
- Surrounded by a thickened basement membrane
- Absence of hyperplastic changes in the epithelial lining
- Associated with an increase of seromucinous glands
- Rhinosporidiosis:
- Endospores involving the submucosa that may mimic microcysts of oncocytic papilloma
- Endospores are located within stroma rather than epithelium
- Sinonasal inflammatory polyp:
- Has epithelial lining commonly of respiratory type and lacks hyperplastic changes seen in sinonasal papilloma
- Lacks microcysts, transmigrating neutrophils and microabscesses seen in sinonasal papilloma
Additional references
Board review style question #1
Which of the following statements about this sinonasal lesion is false?
- Approximately 30% of cases are associated with high risk human papillomavirus (HPV)
- It affects lateral nasal wall rather than nasal septum
- It affects males and females equally
- It carries approximately 10% risk of malignant transformation
Board review style answer #1
A. This is an oncocytic papilloma. It is not associated with HPV, so "Approximately 30% of cases are associated with high risk human papillomavirus (HPV)" is false.
Comment Here
Reference: Sinonasal papilloma
Comment Here
Reference: Sinonasal papilloma
Board review style question #2
Which of the following statements about sinonasal papilloma is true?
- Both inverted and oncocytic papilloma may show endophytic growth pattern
- Oncocytic sinonasal papilloma has a negligible risk of malignant transformation
- Standard of care for sinonasal papilloma is observation or excision for symptom control
- Subtypes of papilloma that may be related to human papillomavirus (HPV) are oncocytic and exophytic subtypes; inverted papilloma has no significant association with HPV
Board review style answer #2
A. Both inverted and oncocytic papilloma may show endophytic growth pattern
Comment Here
Reference: Sinonasal papilloma
Comment Here
Reference: Sinonasal papilloma