Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Lee N, Ng T. Mucocele. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/oralcavitymucocele.html. Accessed April 25th, 2024.
Definition / general
- Reactive lesion to mucus extravasation that attracts muciphages without any epithelial lining
Essential features
- Mucus extravasation into the surrounding tissue secondary to salivary gland duct trauma
- Pseudocyst with epithelioid macrophages (muciphages) forming the periphery
- Found on oral mucosal sites with minor salivary glands or sublingual gland
- May recur if feeding salivary gland is not also removed
Terminology
- Mucus extravasation phenomenon
- Ranula (if on the floor of mouth arising from the sublingual gland)
- Plunging ranula (if the mucin dissects through the mylohyoid muscle to involve the cervical area)
- Mucus escape reaction
- Not to be confused with salivary duct cyst / salivary retention cyst / mucus retention cyst / mucus duct cyst / sialocyst
ICD coding
- ICD-10: K11.6 - mucocele of salivary gland
Epidemiology
- No gender predilection (J Oral Maxillofac Surg 2011;69:1086)
- Reported in patients of all ages but more common before the third decade due to association with trauma to oral mucosa containing salivary glands (J Oral Maxillofac Surg 2011;69:1086)
Sites
- Lower labial mucosa > floor of the mouth > ventral tongue > buccal mucosa (J Oral Maxillofac Surg 2011;69:1086)
- Superficial mucoceles are most common at the soft palate, retromolar pad and buccal mucosa (J Oral Maxillofac Surg 2011;69:1086)
- Very rare at the upper labial mucosa as it is difficult to traumatize that site; neoplastic minor salivary gland lesions should be considered (J Oral Maxillofac Surg 2011;69:1086)
Pathophysiology
- Local mechanical trauma, such as biting that injures a salivary gland excretory duct (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003;95:467)
- When the duct is severed, mucus escapes into the adjacent tissue (J Oral Maxillofac Surg 2008;66:2050)
- Extravasated mucin attracts macrophages that attempt to phagocytose the foreign material (Acta Histochem 2014;116:40)
- Not associated with primary obstruction of a salivary gland excretory duct, which will lead to mucus retention within a salivary duct cyst (J Oral Maxillofac Surg 2007;65:855)
Etiology
- Trauma to salivary gland excretory duct (Laryngoscope 1988;98:296)
Clinical features
- Dome shaped, sessile nodule measuring a few millimeters to several centimeters (especially ranula) in diameter (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003;95:467)
- Fluctuant to palpation but painless, some may feel firmer (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003;95:467)
- Blue tinge due to the Tyndall effect (J Oral Maxillofac Surg 2008;66:2050)
- Waxes and wanes over time; patient may report “popping” of lesion, may also resolve spontaneously (Laryngoscope 1988;98:296)
- Superficial mucoceles are associated with hyposalivation and lichenoid lesions such as oral lichen planus, lichenoid drug reaction and chronic graft versus host disease (J Oral Maxillofac Surg 2011;69:1086)
Diagnosis
- Based on patient reported history and clinical examination with definitive diagnosis made by histopathologic evaluation under light microscopy
Prognostic factors
- Benign with good prognosis
Case reports
- 11 month old boy with a 3 month history of difficulty suckling and lower labial mucosal nodule (Case Rep Dent 2014;2014:723130)
- 9 year old boy with a nail-biting habit and deep anterior overbite with a recurrent vesicle at the lower labial mucosa (BMJ Case Rep 2016;2016:bcr2016216354)
- 9 year old boy with a history of local trauma resulting in an enlarging left lower lip swelling (J Pharm Bioallied Sci 2015;7:S731)
- 35 year old woman with complicated medical history presenting with an upper labial mucosal nodule (Braz Dent J 2017;28:405)
Treatment
- Excision along with the feeding salivary gland is curative
- Iatrogenic intraoperative damage to neighboring salivary gland parenchyma may contribute to recurrence
- Removal of the sublingual gland with marsupialization of Wharton's duct can reduce the risk of recurrence for large ranulas (J Oral Maxillofac Surg 2008;66:2050)
- Laser ablation, superpotent topical corticosteroids and gamma-linolenic acid have been reported to be effective in isolated case reports for superficial mucoceles (J Oral Maxillofac Surg 2007;65:855)
Gross description
- Nodular mass resembling gelatinous material if removed intact (Acta Histochem 2014;116:40)
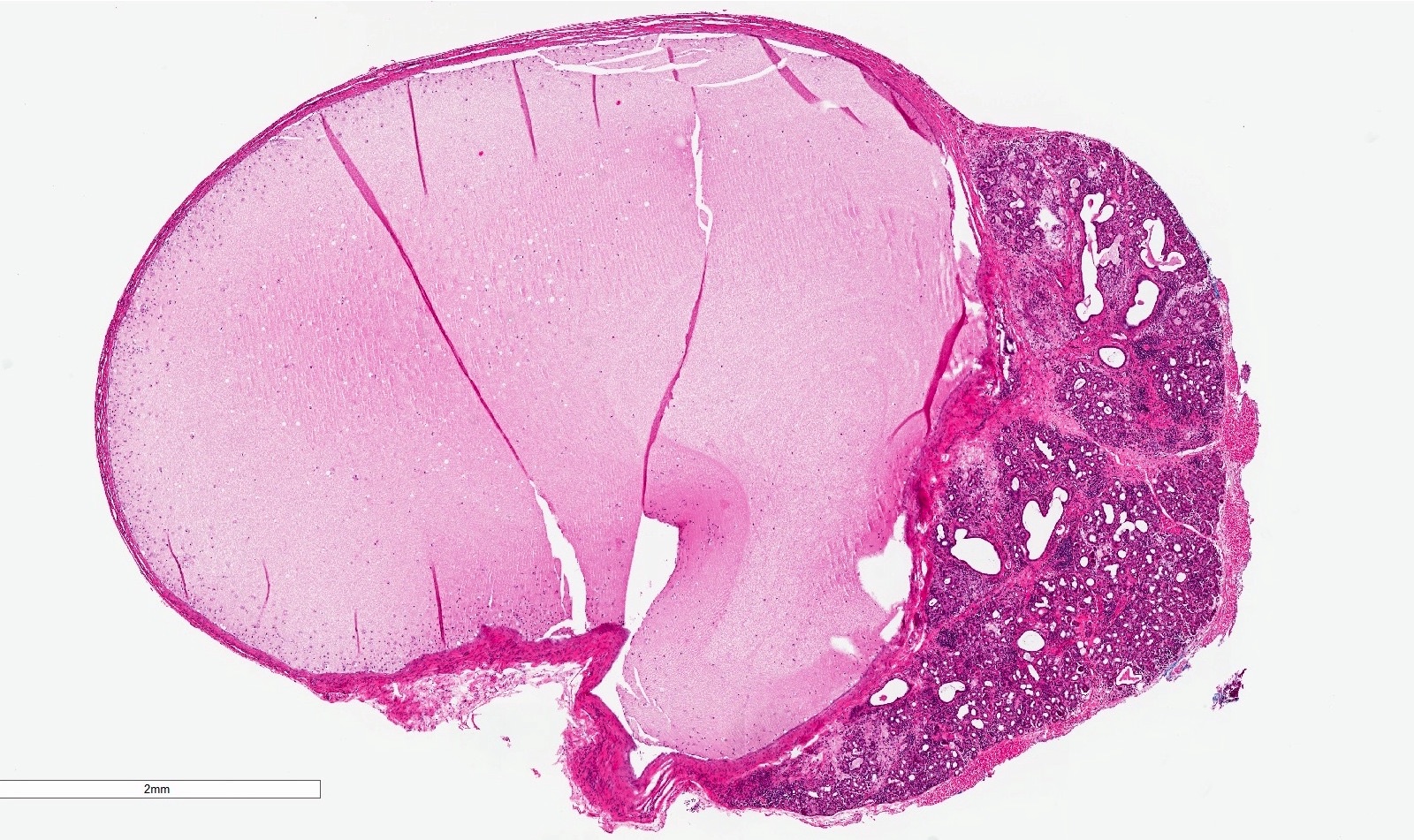
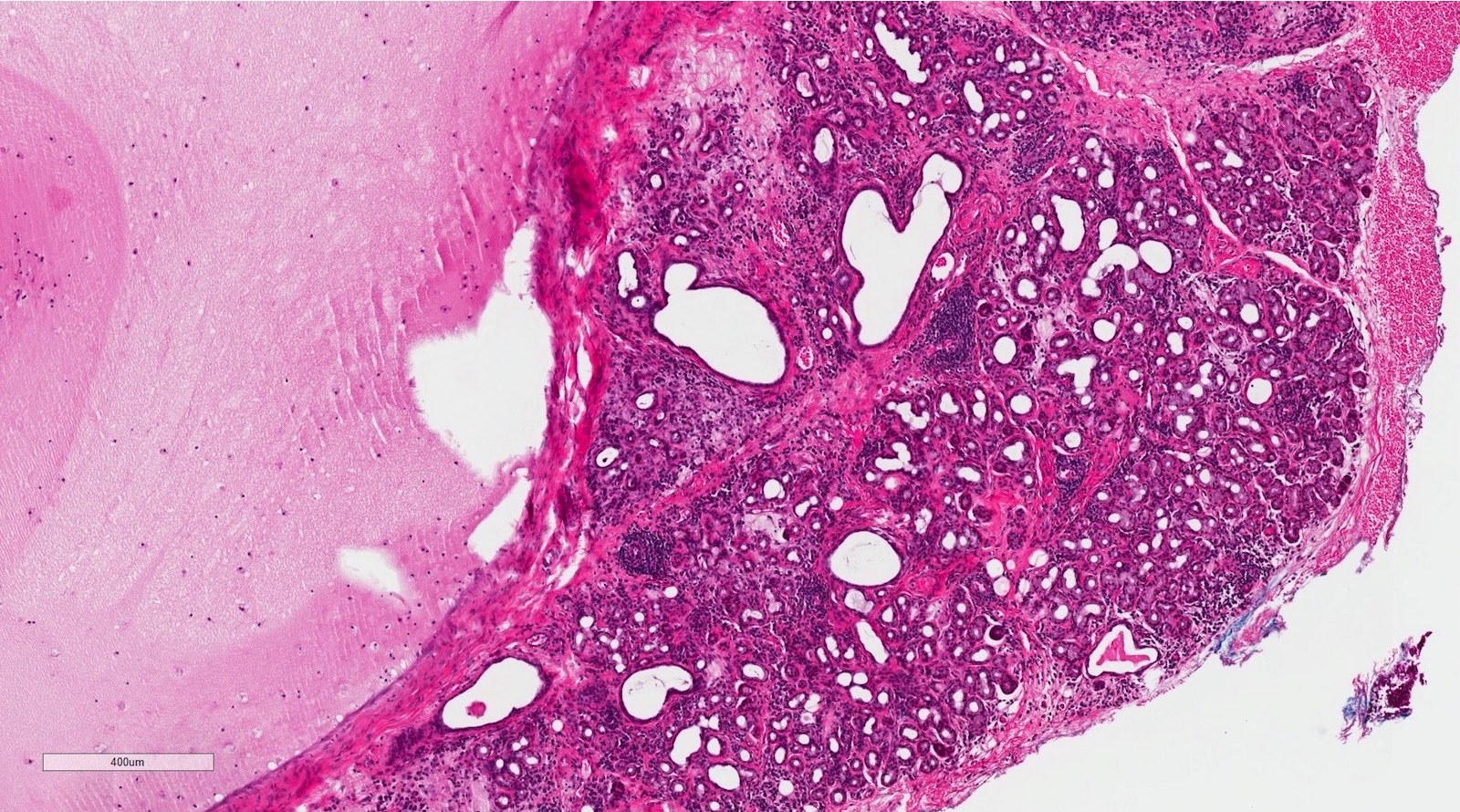
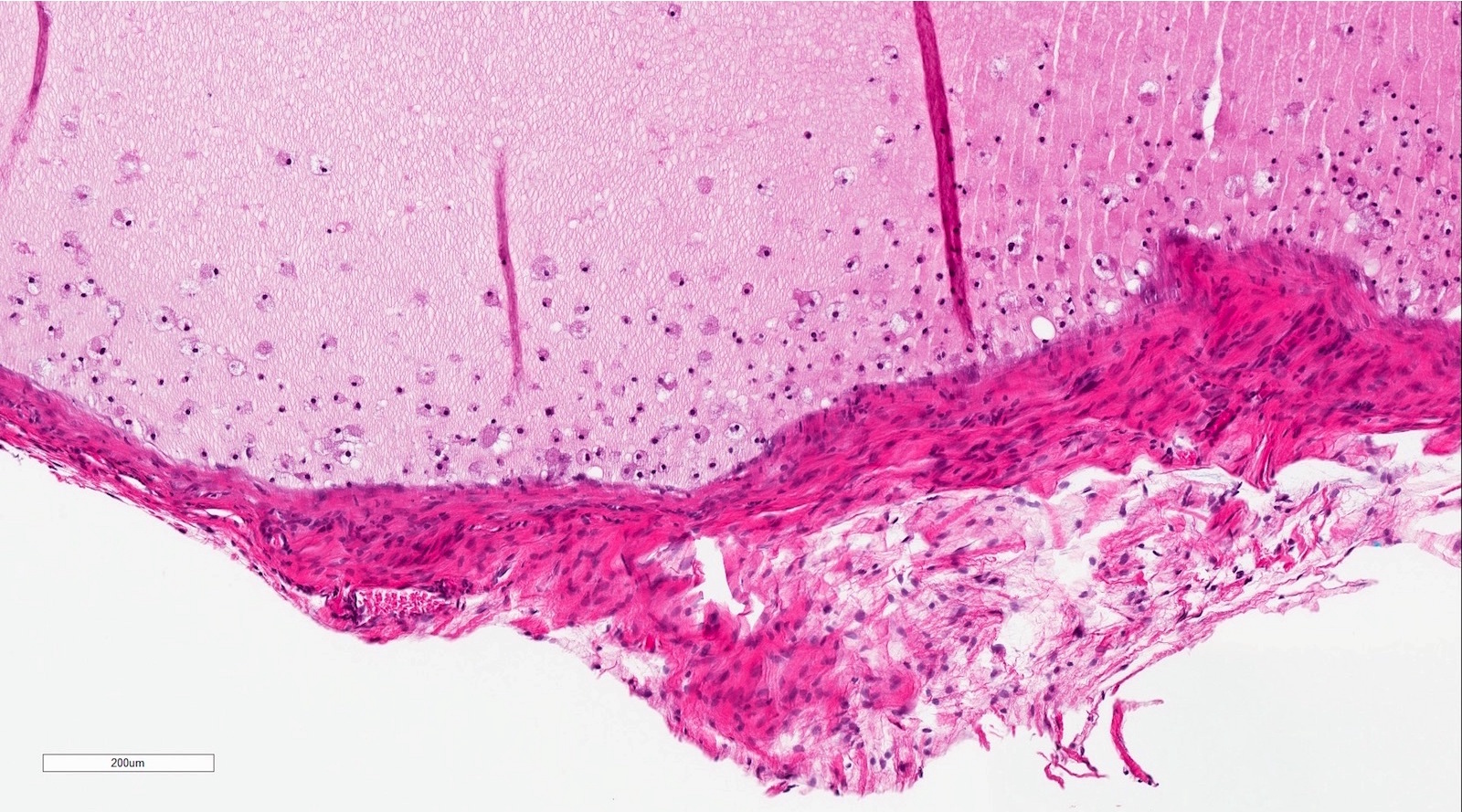
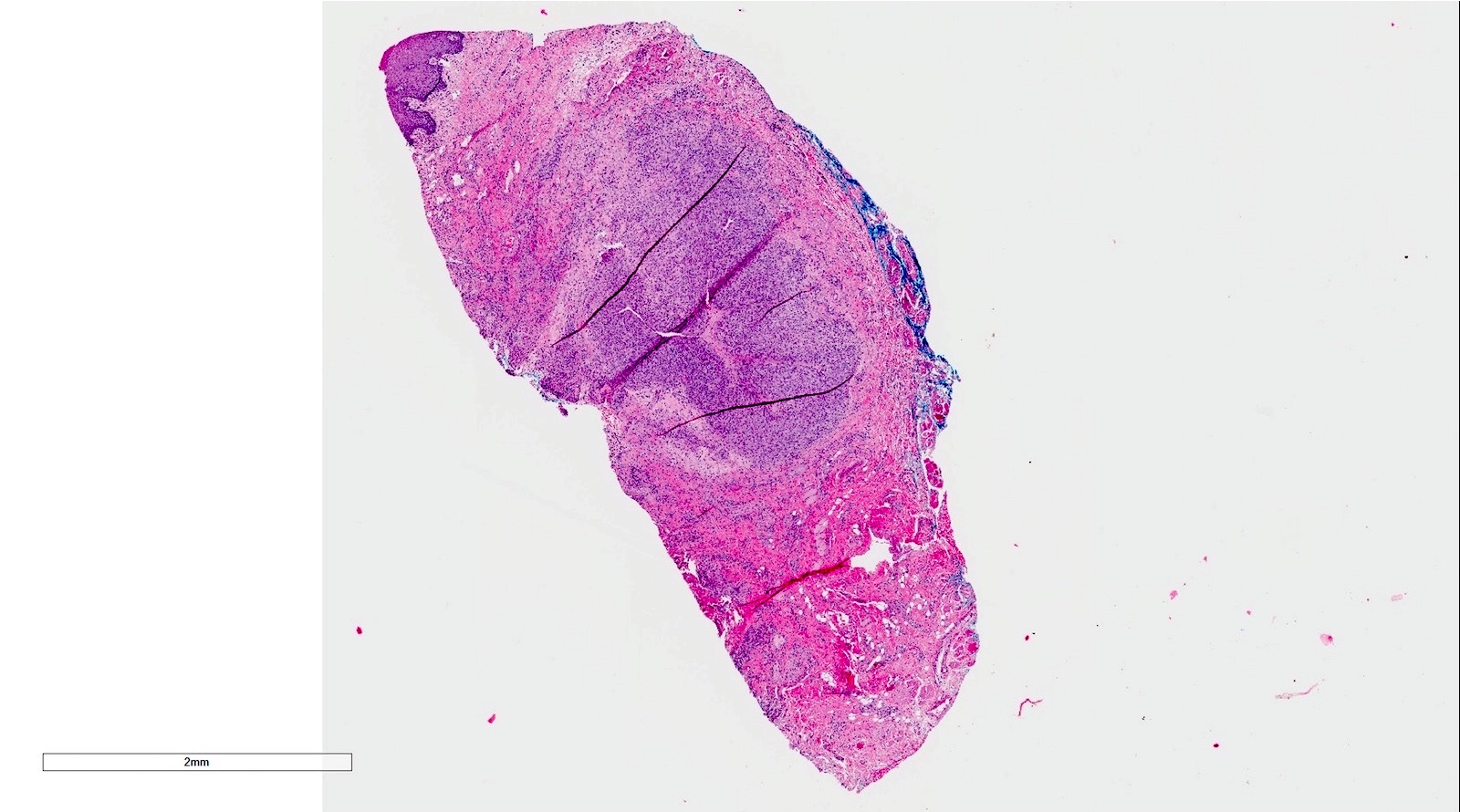
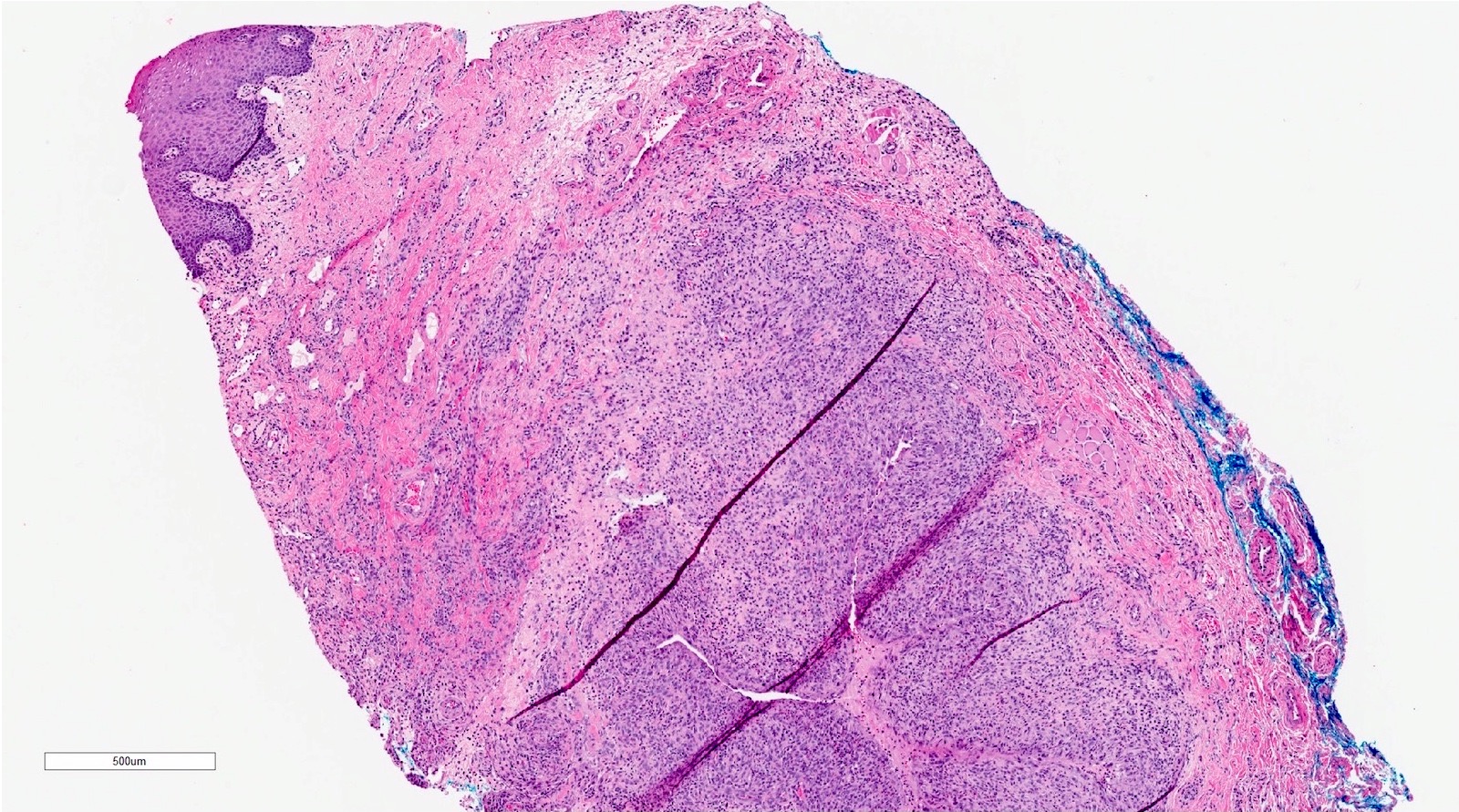
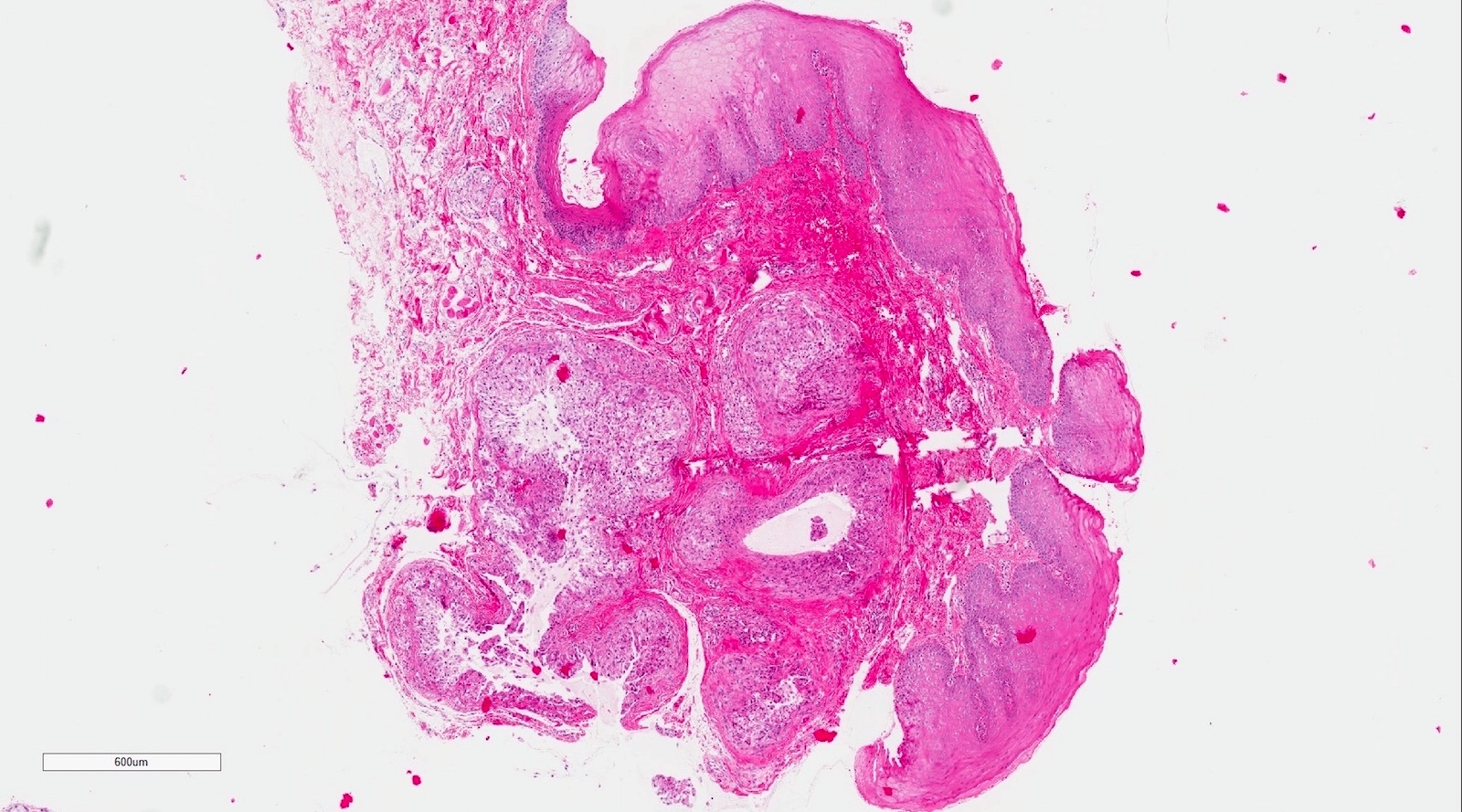
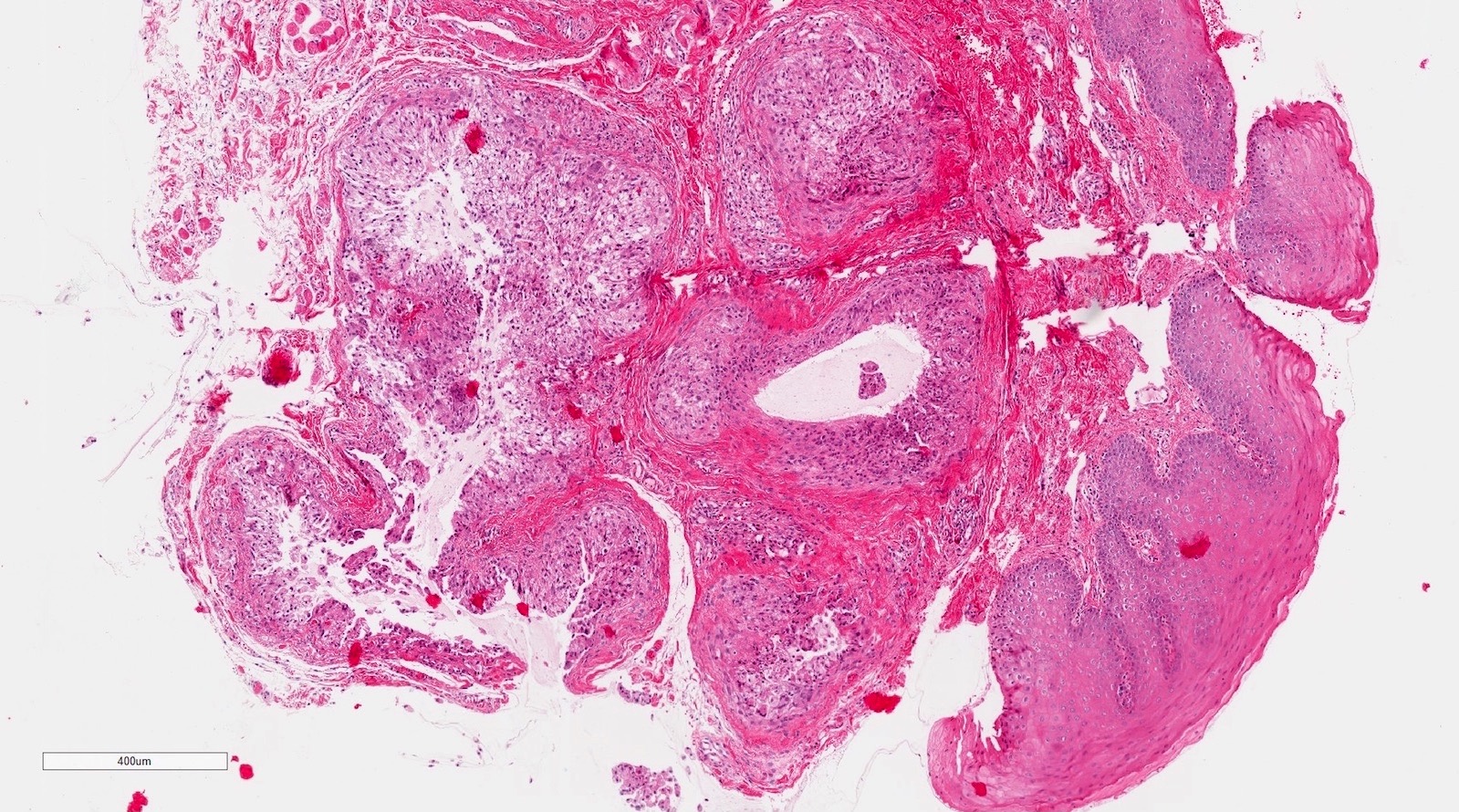
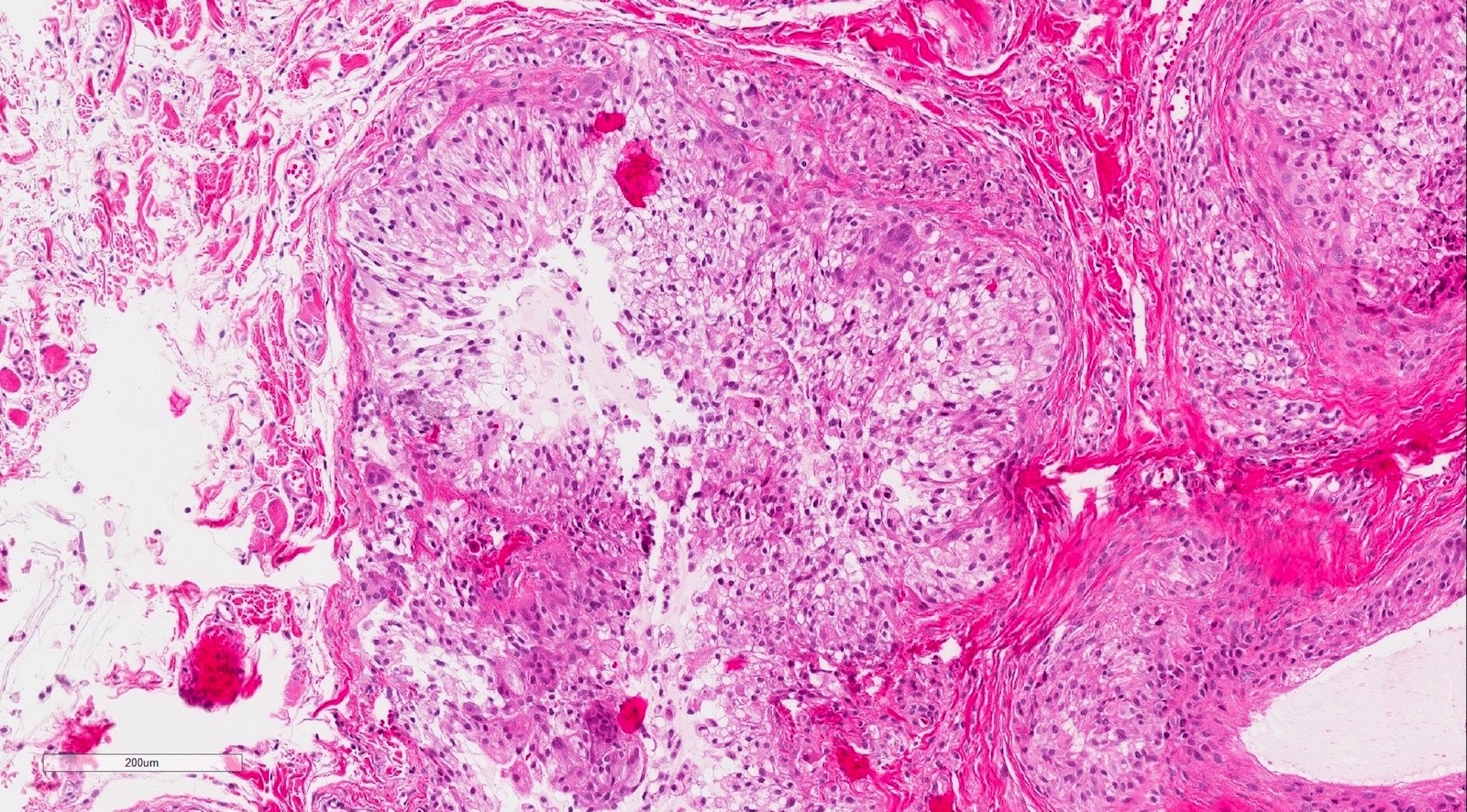
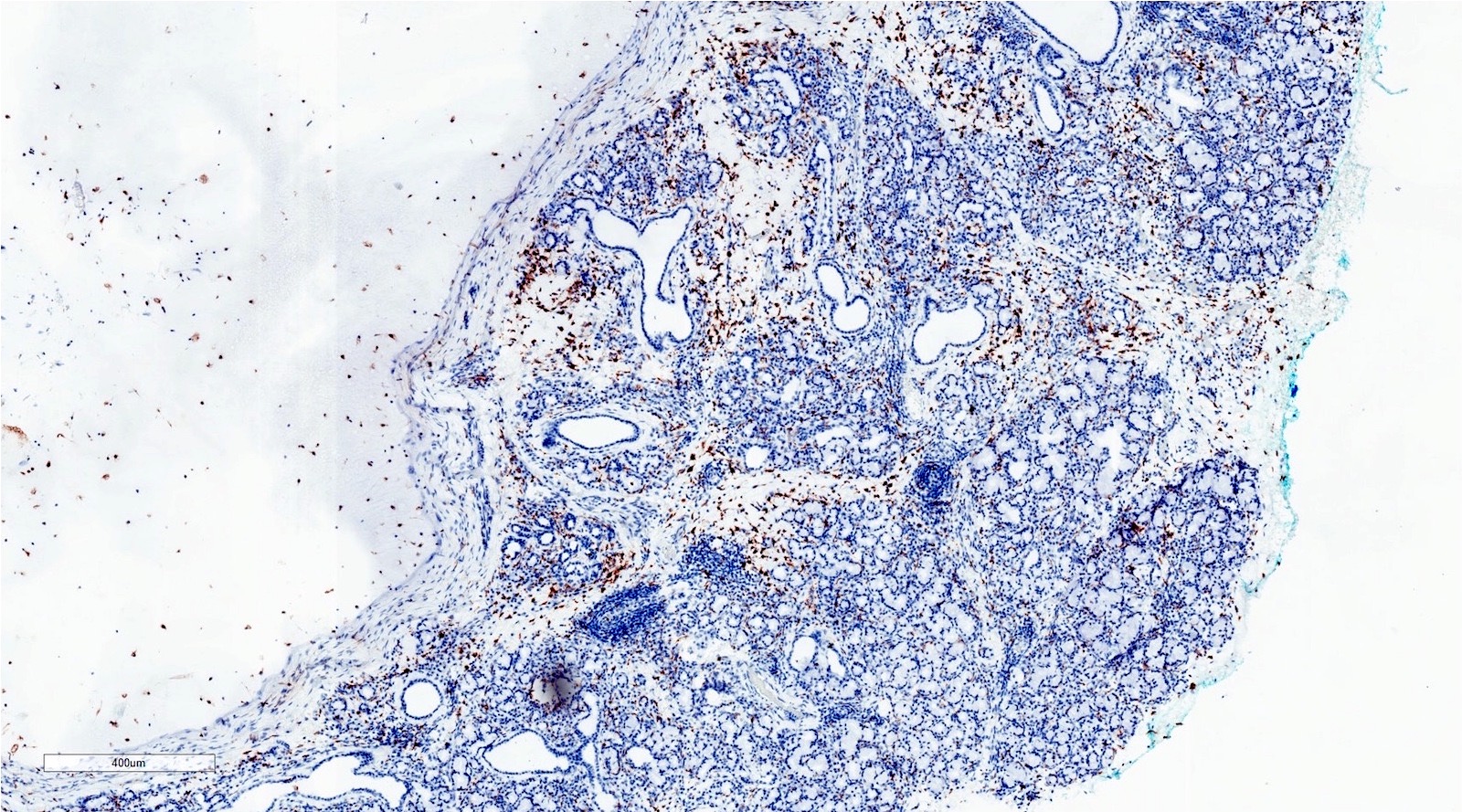
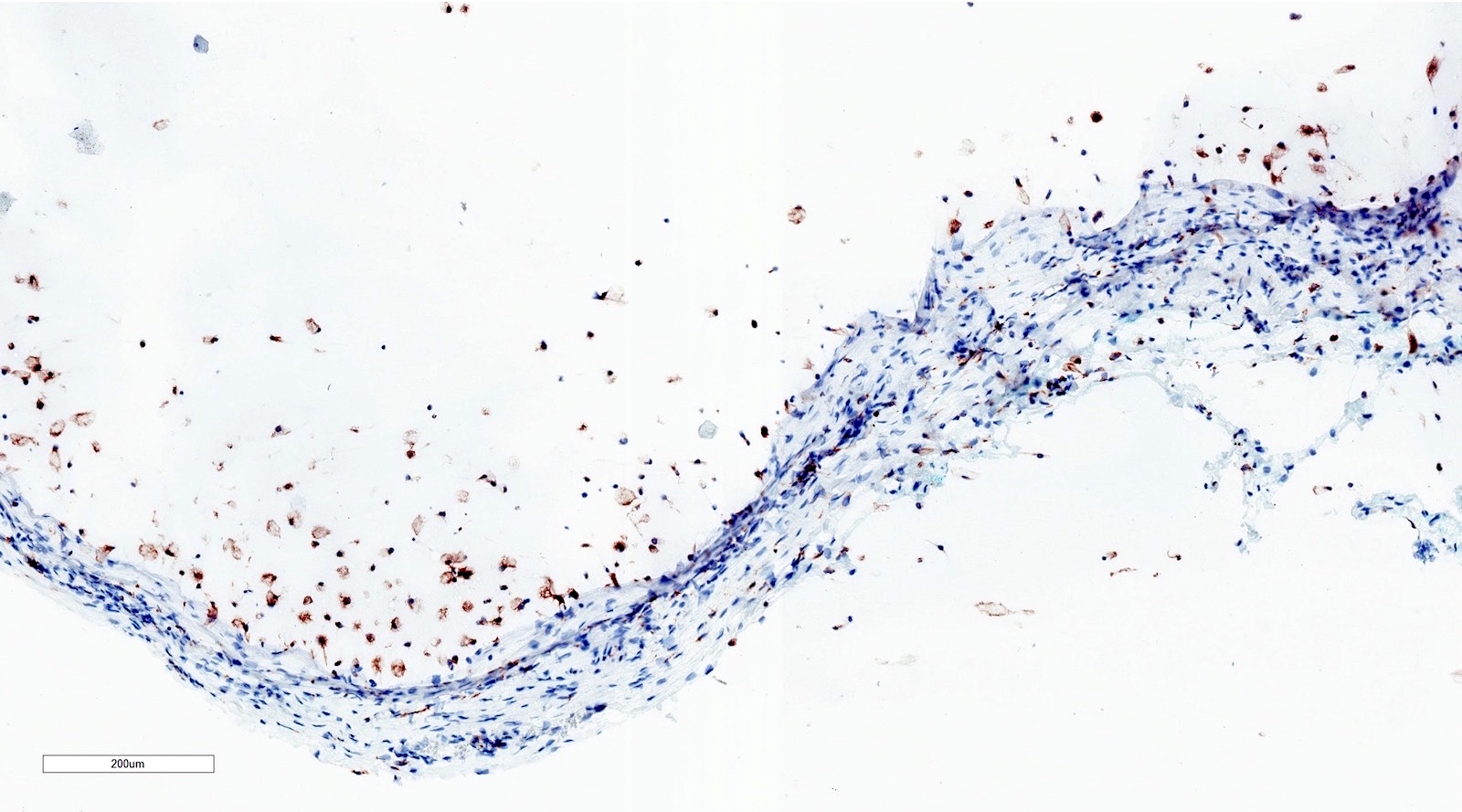
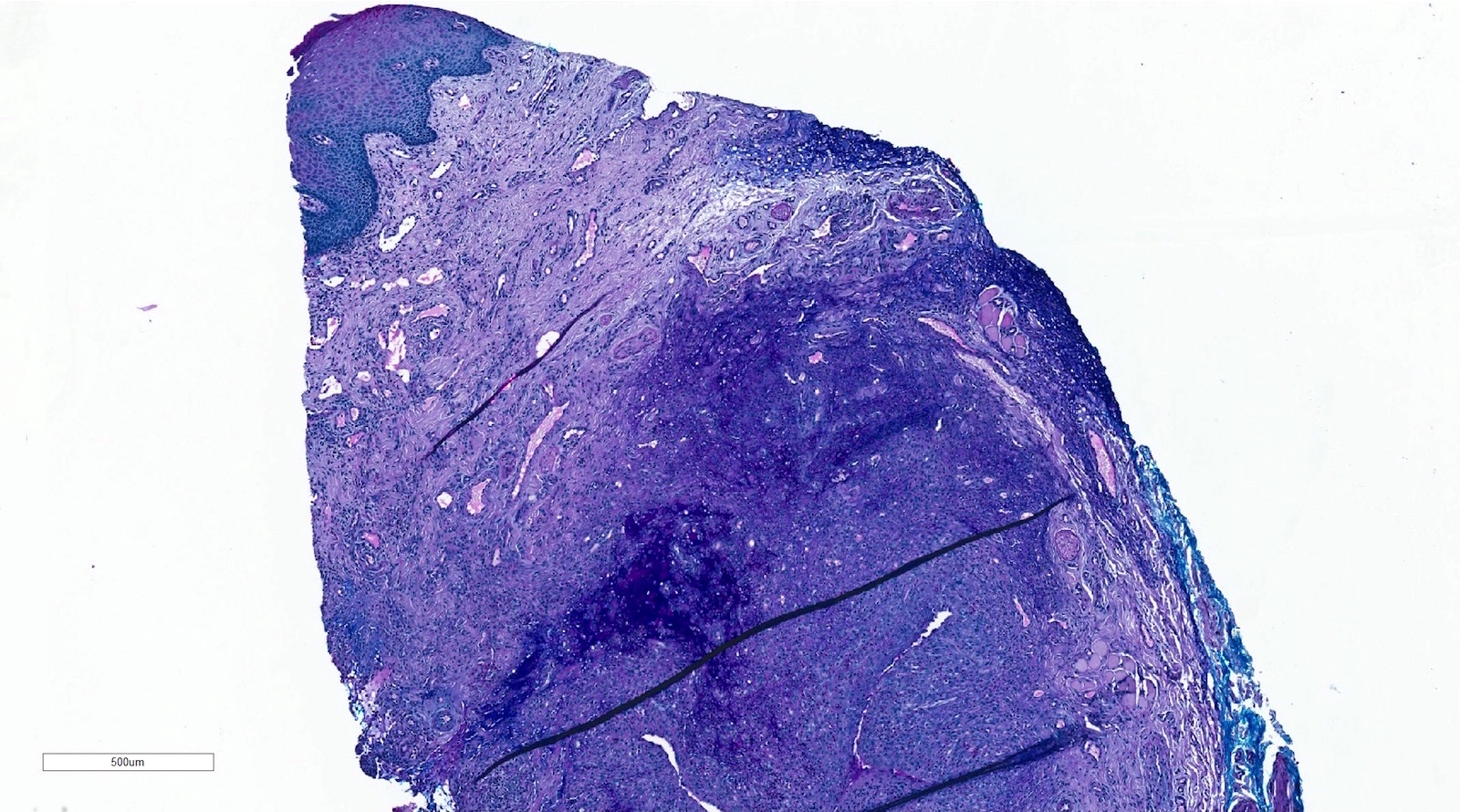
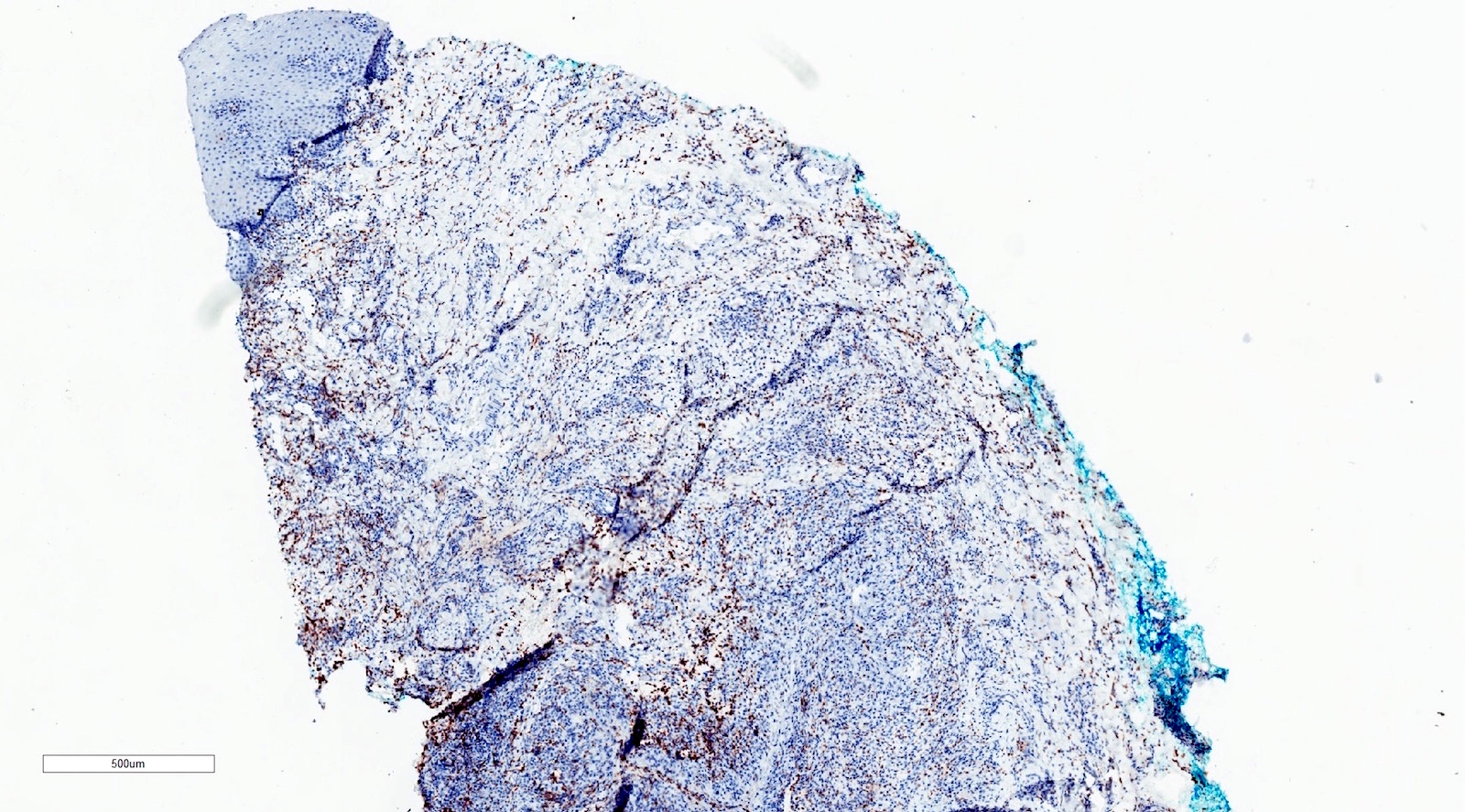
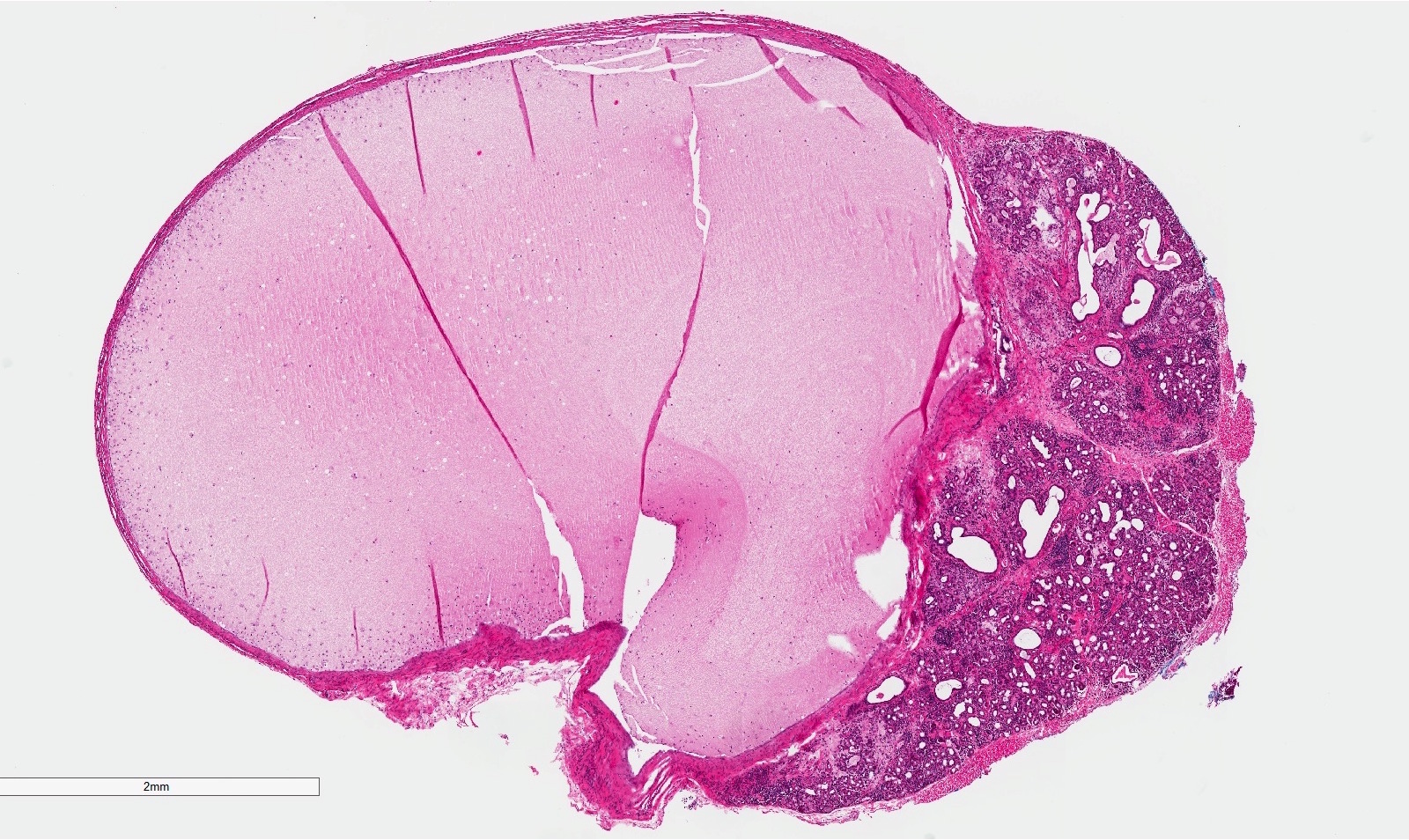
Microscopic (histologic) description
- If removed intact
- Pseudocyst cavity containing mucin, abundant epithelioid foamy histiocytes (muciphages), neutrophils and granulation tissue (Acta Histochem 2014;116:40)
- If removed ruptured
- Fragments of granulation tissue containing epithelioid foamy histiocytes (muciphages) and neutrophils, may see mucinous material (Acta Histochem 2014;116:40)
- Removed salivary gland parenchyma showing obstructive changes
- Acinar atrophy, ductal dilatation with periductal hyalinization, interstitial lymphoplasmacytic infiltrate and interstitial fibrosis at late stage (J Oral Maxillofac Surg 2008;66:2050)
- May see ruptured feeding salivary duct with squamous metaplasia (J Oral Maxillofac Surg 2008;66:2050)
- Long standing lesions organize into fibrosis resembling a fibroepithelial polyp (Acta Histochem 2014;116:40)
- No epithelial cyst lining, may see overlying surface oral mucosa with variable atrophy in superficial mucoceles (J Oral Maxillofac Surg 2011;69:1086)
Microscopic (histologic) images
Positive stains
- Note: stains typically not needed to make the diagnosis
- CD68
- PAS-D
- Mucicarmine
- Alcian blue
Negative stains
Sample pathology report
- Right lower labial mucosa, excision:
- Mucous extravasation phenomenon (mucocele)
- Minor salivary gland parenchyma showing chronic sialoadenitis
Differential diagnosis
- Salivary duct cyst / salivary retention cyst / mucus retention cyst / mucus duct cyst / sialocyst:
- True salivary gland duct epithelial lining that may show an oncocytic bilayer or squamous metaplasia
- Mucoepidermoid carcinoma
- 3 populations of atypical cells (mucous, intermediate, epidermoid) invading the surrounding stroma
- Autoimmune sialadenitis (Sjögren syndrome)
- Minimal obstructive changes such as salivary gland duct dilation and the lymphocytic inflammation is not periductal
- Glandular odontogenic cyst
- True epithelial cystic lining with goblet cells, no extravasated mucin and this lesion is not within the orofacial soft tissues
- Oral focal mucinosis
- No mucin and instead is a well localized non encapsulated collection of myxomatous connective tissue in the stroma
Additional references
Board review style question #1
Board review style answer #1
Board review style question #2
- Among the choices below, what is the most common site to find an oral cavity mucocele?
- Gingiva
- Intrabony, within the maxillary or mandibular bone
- Labial commissure
- Parotid gland
- Upper labial mucosa
Board review style answer #2