Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Forgó E, Longacre TA. High grade serous carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/ovarytumorserouscarcinomahg.html. Accessed April 23rd, 2024.
Definition / general
- Epithelial carcinoma of serous cell lineage with papillary, glandular and solid growth patterns and high grade cytologic atypia
Essential features
- Often bilateral, solid and cystic ovarian masses
- Solid, pseudoendometrioid, transitional cell carcinoma-like (SET) appearance more common in BRCA1 mutations; need to refer to genetic testing
- 3 patterns of aberrant p53 expression correlate with TP53 mutation
- Most important prognostic factor is stage, ~40% overall 5 year survival
Terminology
- High grade serous adenocarcinoma
ICD coding
- ICD-O: 8461/3 - malignant epithelial serous tumors, high grade serous carcinoma
Epidemiology
- Accounts for majority of ovarian carcinoma diagnoses and related deaths
- Affects women disproportionately in western nations
- Increased risk in Caucasian as compared with African American women
- Decreased risk with several menstrual and reproductive factors:
- Parity
- Later age at menarche
- Earlier age of menopause
- Oral contraceptive use
- Increased risk with estrogen only hormonal therapy, combined estrogen and progestin regimens
Sites
- Tubo-ovarian, peritoneum
Pathophysiology
- Hereditary predisposition in 15 - 20% of cases involving BRCA genes (Am J Surg Pathol 2016;40:404):
- BRCA1 germline mutations cause 50% lifetime risk of ovarian cancer at average age of ~50 years
- BRCA2 germline mutations causes lower lifetime risk (10 - 35%) at a later age (average ~55 years)
- Associated with homologous recombination defects
- Hereditary predisposition in 6% of women with Fanconi anemia
- A significant proportion arise in the fallopian tube and spread to the ovaries and peritoneum
Clinical features
- Mean age: 63 years
- Abdominal distension / bloating / pain
- Nausea
- Anorexia / early satiety
- Back pain
- Urinary incontinence
- Advanced disease at presentation in ~80% of cases
Diagnosis
- CT with contrast is the preferred imaging modality
- Diagnosis is by surgical resection and histologic examination of resected tissue - may be associated with serous intraepithelial carcinoma (STIC) in fallopian tube (Histopathology 2014;65:149, Int J Gynecol Pathol 2017;36:230)
Laboratory
- Elevated serum CA-125 level
Radiology description
- Unilocular or multilocular, often bilateral, cystic and solid ovarian masses
- Papillary projections identifiable
- Peritoneal implantations and lymphadenopathy visible
Prognostic factors
- Most important: stage, ~40% overall 5 year survival
- In advanced stage disease, the amount of residual tumor present after staging and debulking is the most important factor
- Low Ki67 proliferation index associated with platinum resistance and decreased survival
- CD3+ or CD8+ tumor infiltrating lymphocytes confer favorable prognosis
Case reports
- 13 year old girl and 69 year old woman with normal sized ovarian carcinoma syndrome (Horm Mol Biol Clin Investig 2018;35:1)
- 22, 35 and 47 year old women with low grade serous neoplasms of the ovary with transformation to high grade carcinomas (Int J Gynecol Pathol 2012;31:423)
- 51 year old woman with high grade serous ovarian cancer 3 years after bilateral salpingectomy (Mol Clin Oncol 2017;6:201)
- 73 year old woman with serous carcinoma of the ovary that metastasized to the tail of the pancreas (Mol Clin Oncol 2016;5:41)
Treatment
- Bilateral salpingo-oophorectomy with hysterectomy, debulking and staging biopsies
- Chemotherapy (neoadjuvant and adjuvant)
- Poly (ADP-ribose) polymerase (PARP) inhibitors with best response in patients with BRCA1 / BRCA2 mutations or other homologous recombination deficiency and platinum sensitivity (Cancer Chemother Pharmacol 2018;81:647, Invest New Drugs 2018;36:828)
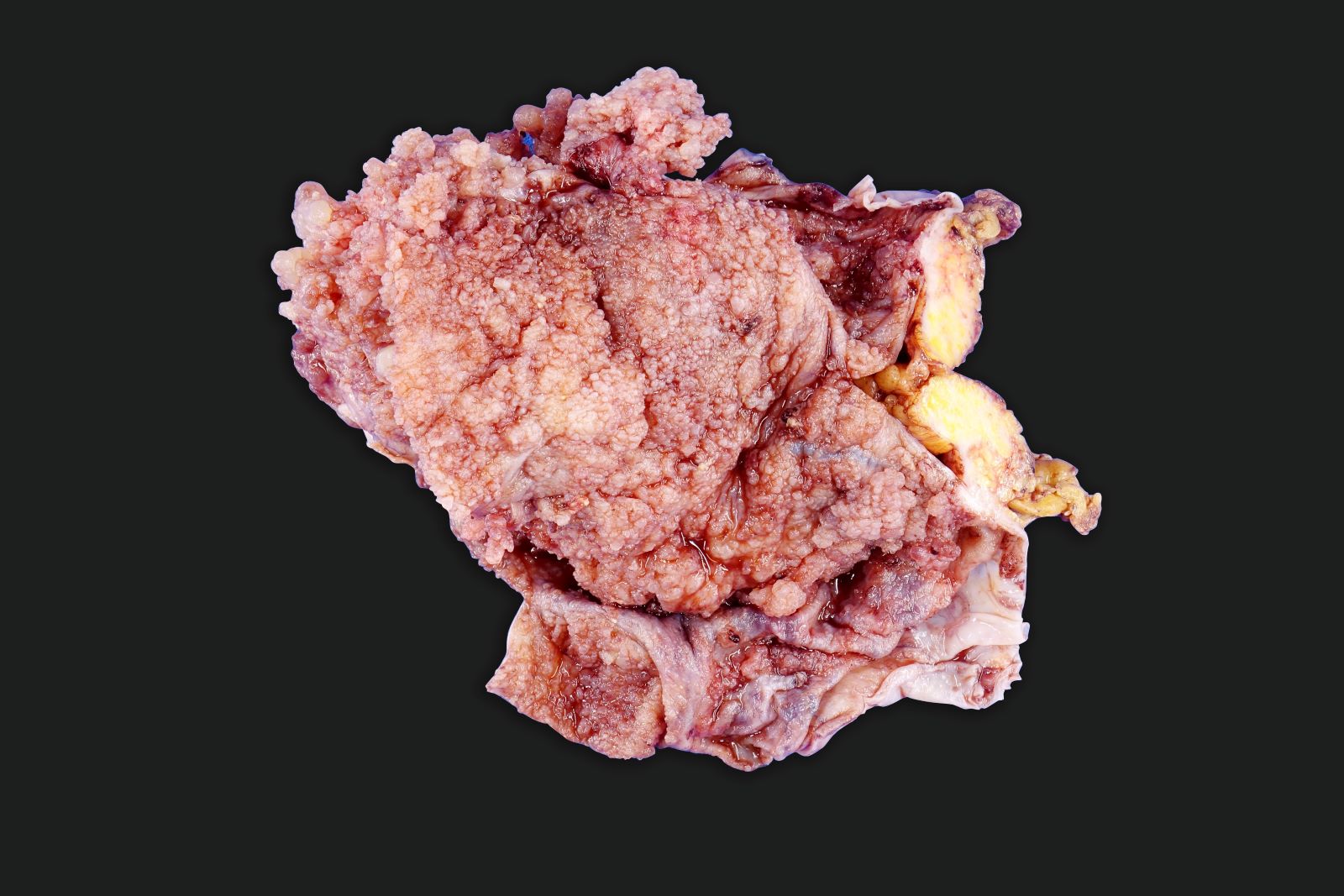
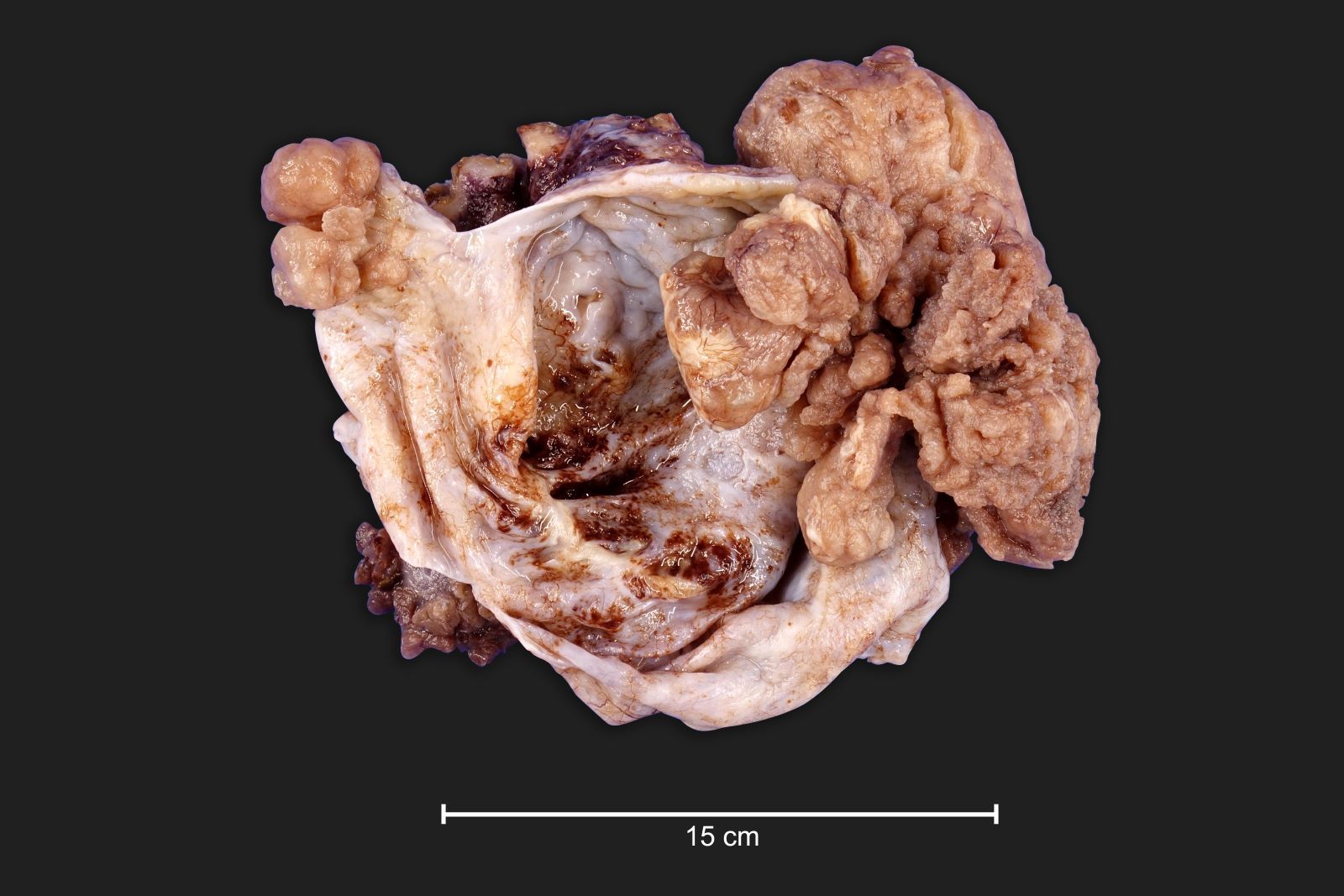
Gross description
- Often bilateral
- Variable in size; often large, ~30% of cases with grossly normal ovary or surface nodules < 1 cm
- Exophytic with solid or papillary growth
- Solid areas tan to white with necrosis and hemorrhage
- Serous / bloody fluid filled cysts
- Fallopian tube can be grossly involved at fimbriated end
Gross images
Frozen section description
- Nuclear pleomorphism (> 3x variation in size)
- Moderate to severe nuclear atypia
- Can have large bizarre forms
- Increased mitotic figures, can be atypical
Frozen section images
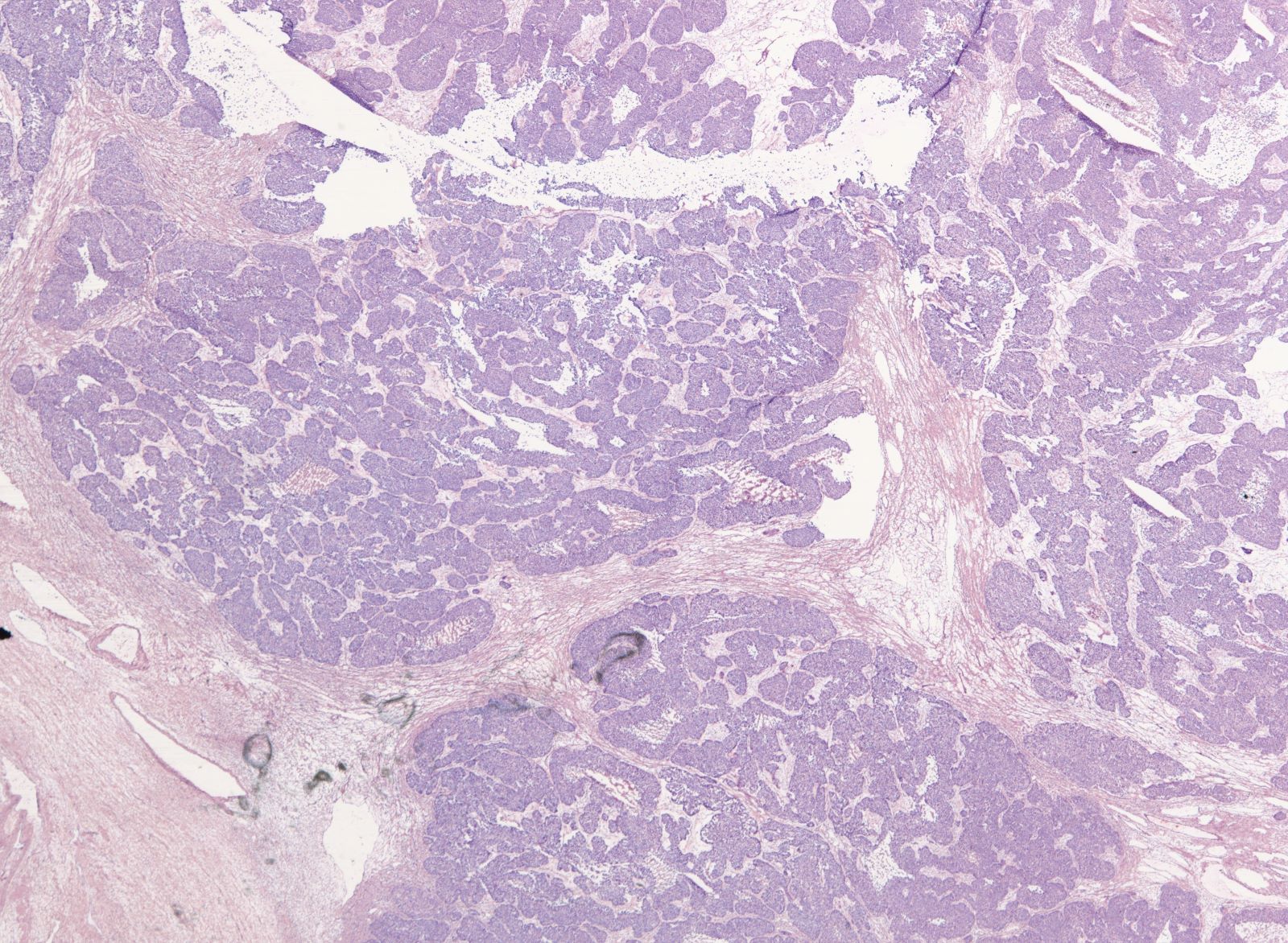
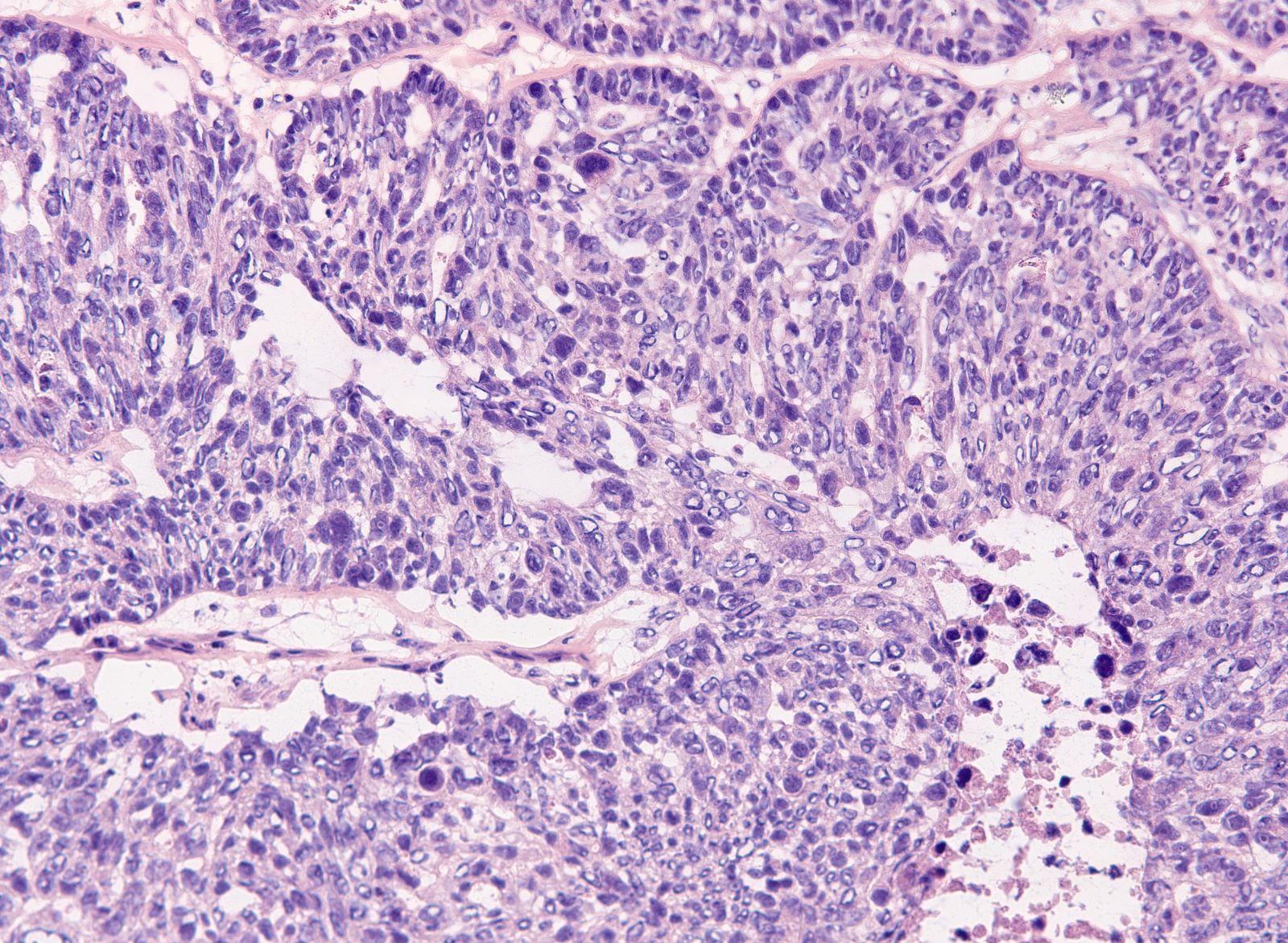
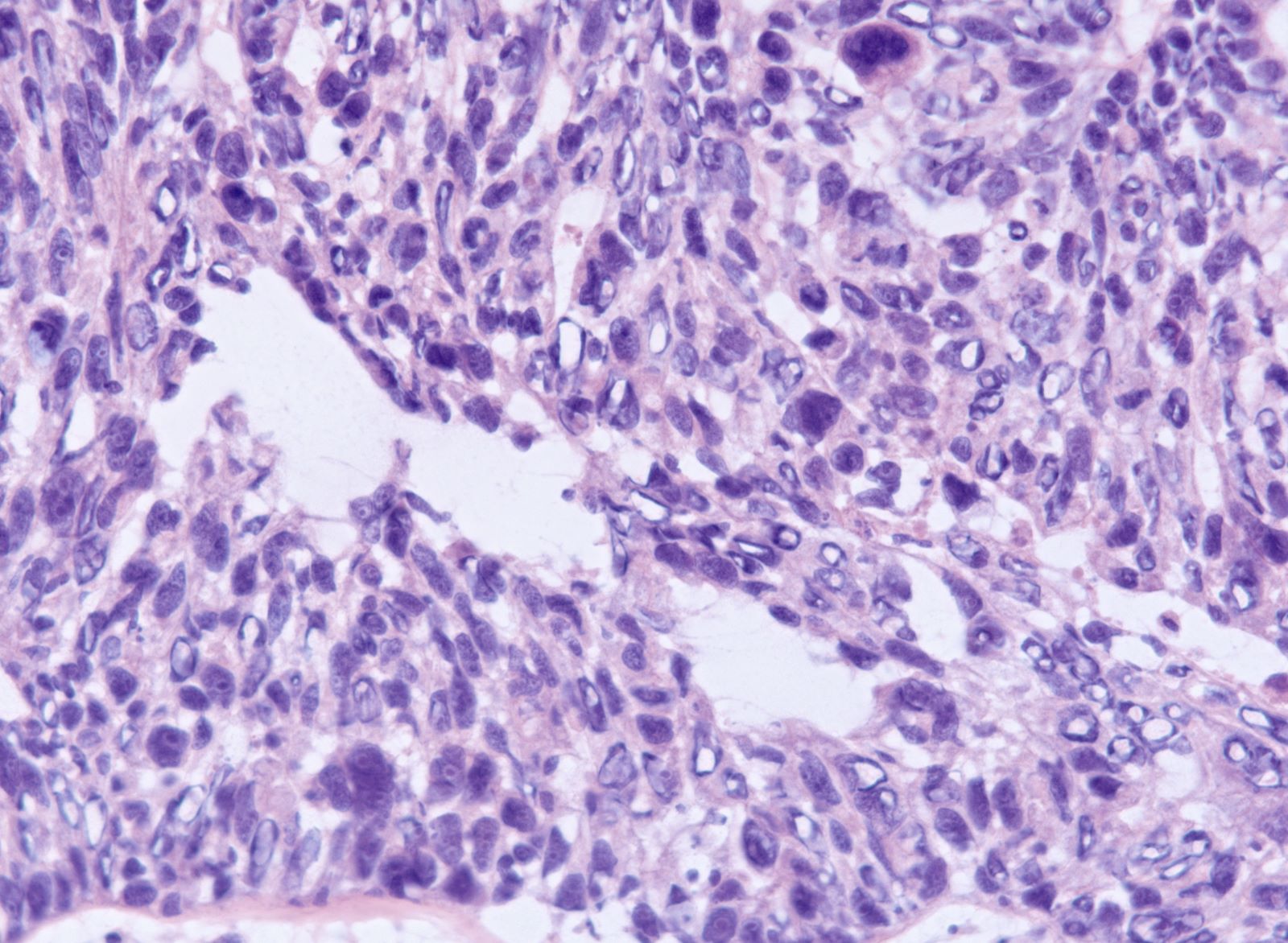
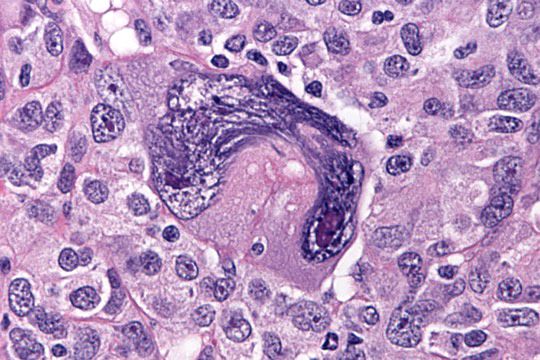
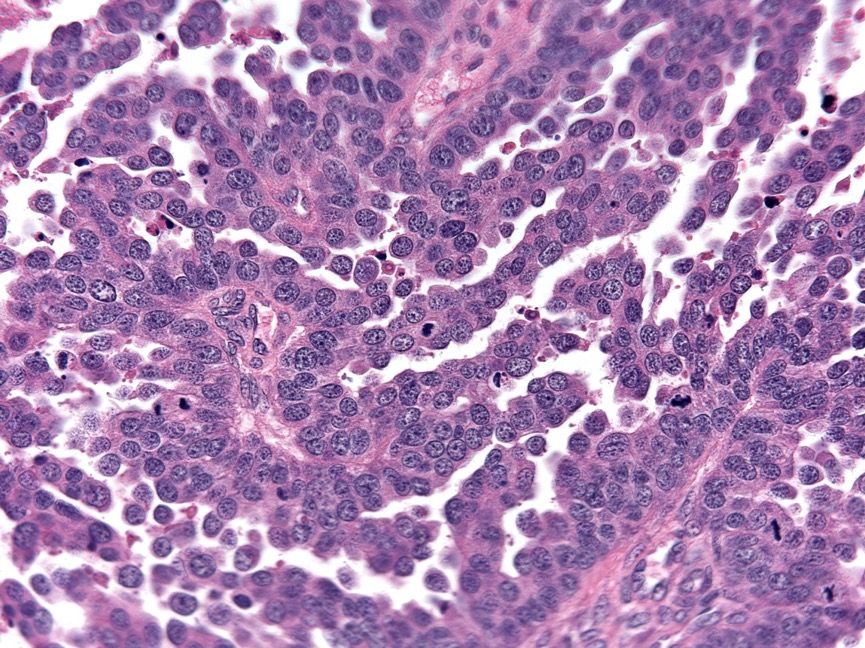
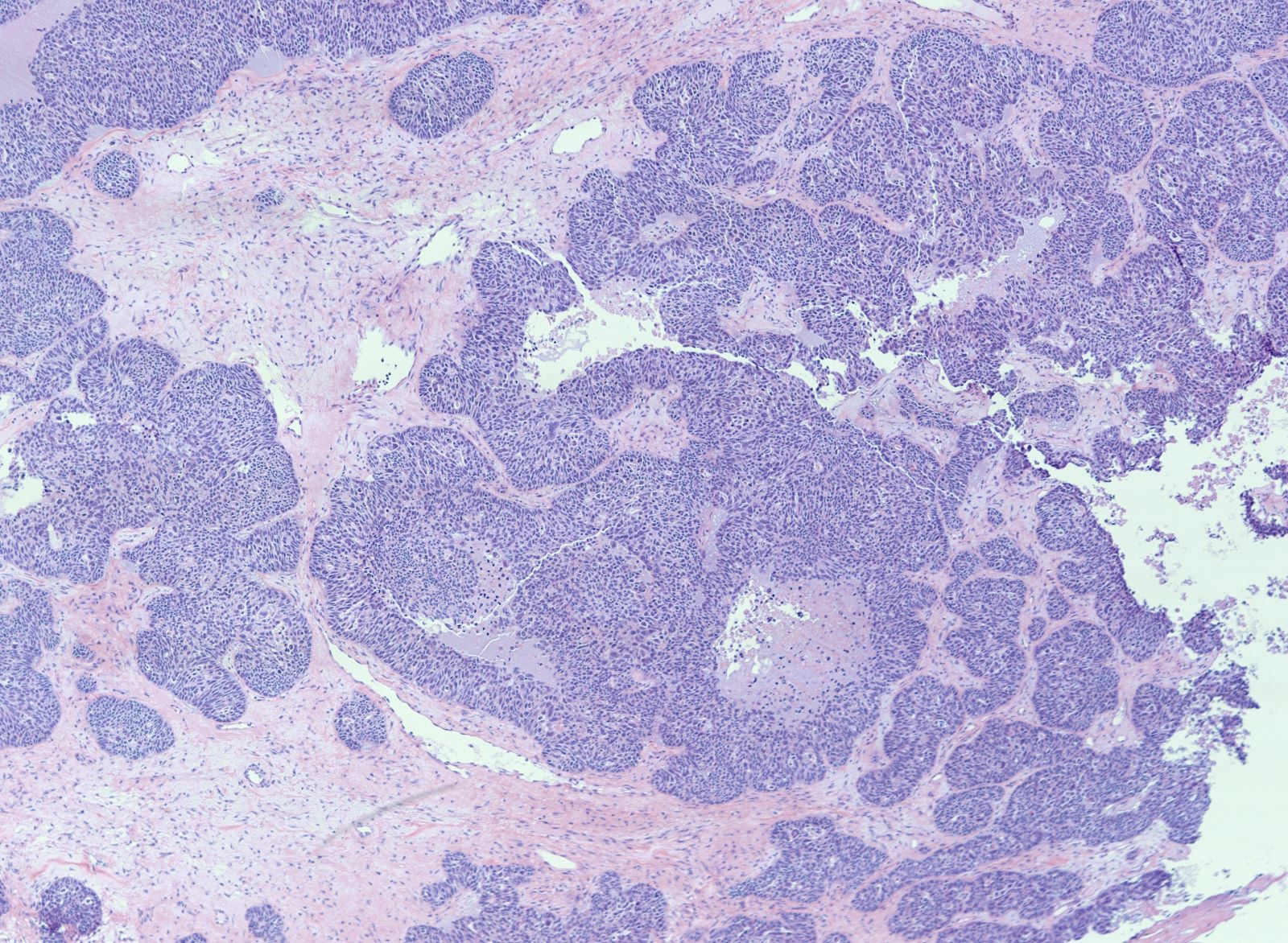
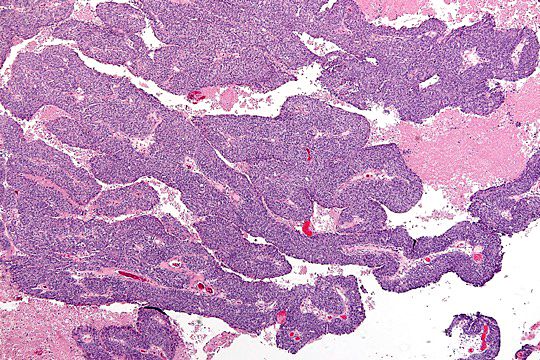
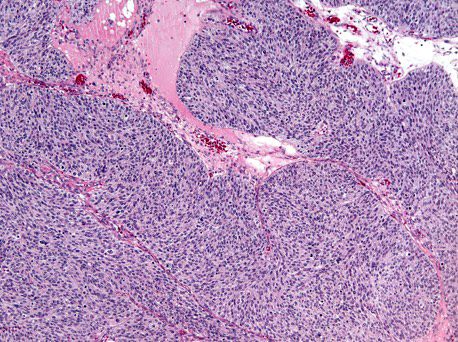
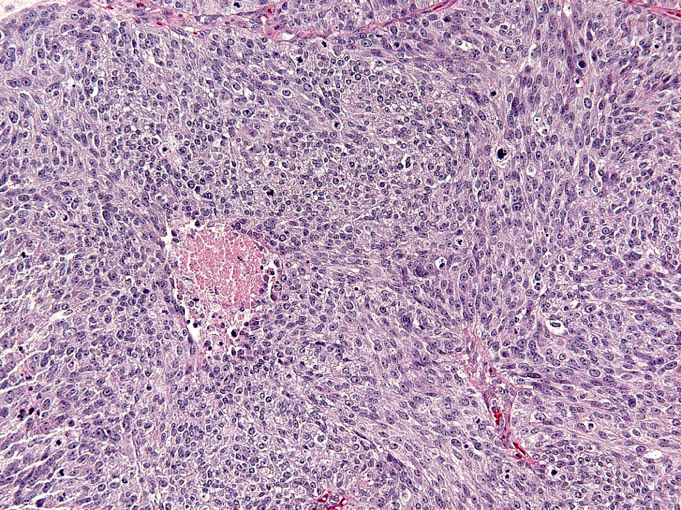
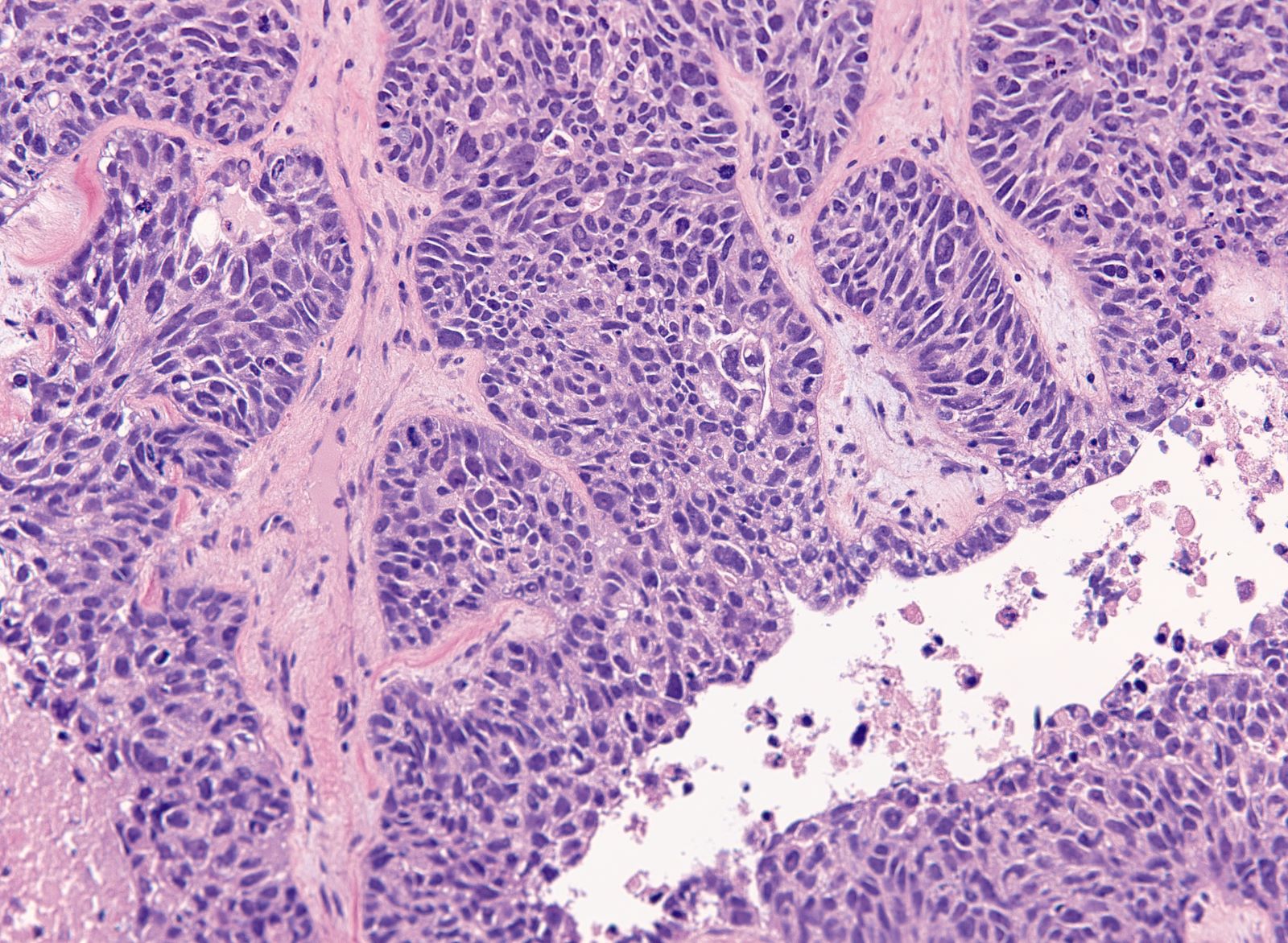
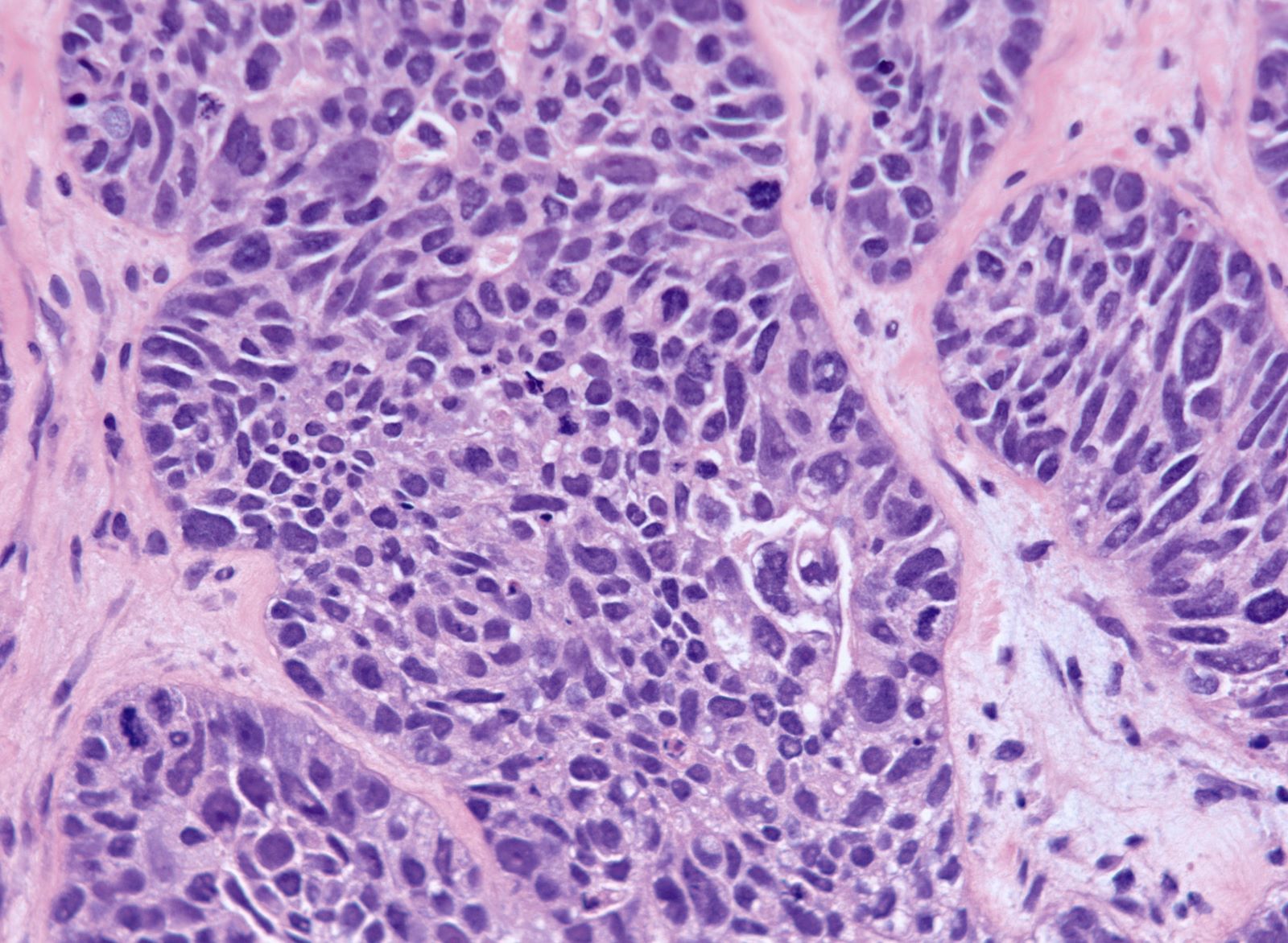
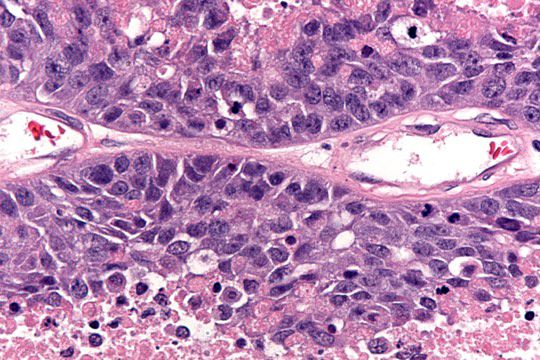
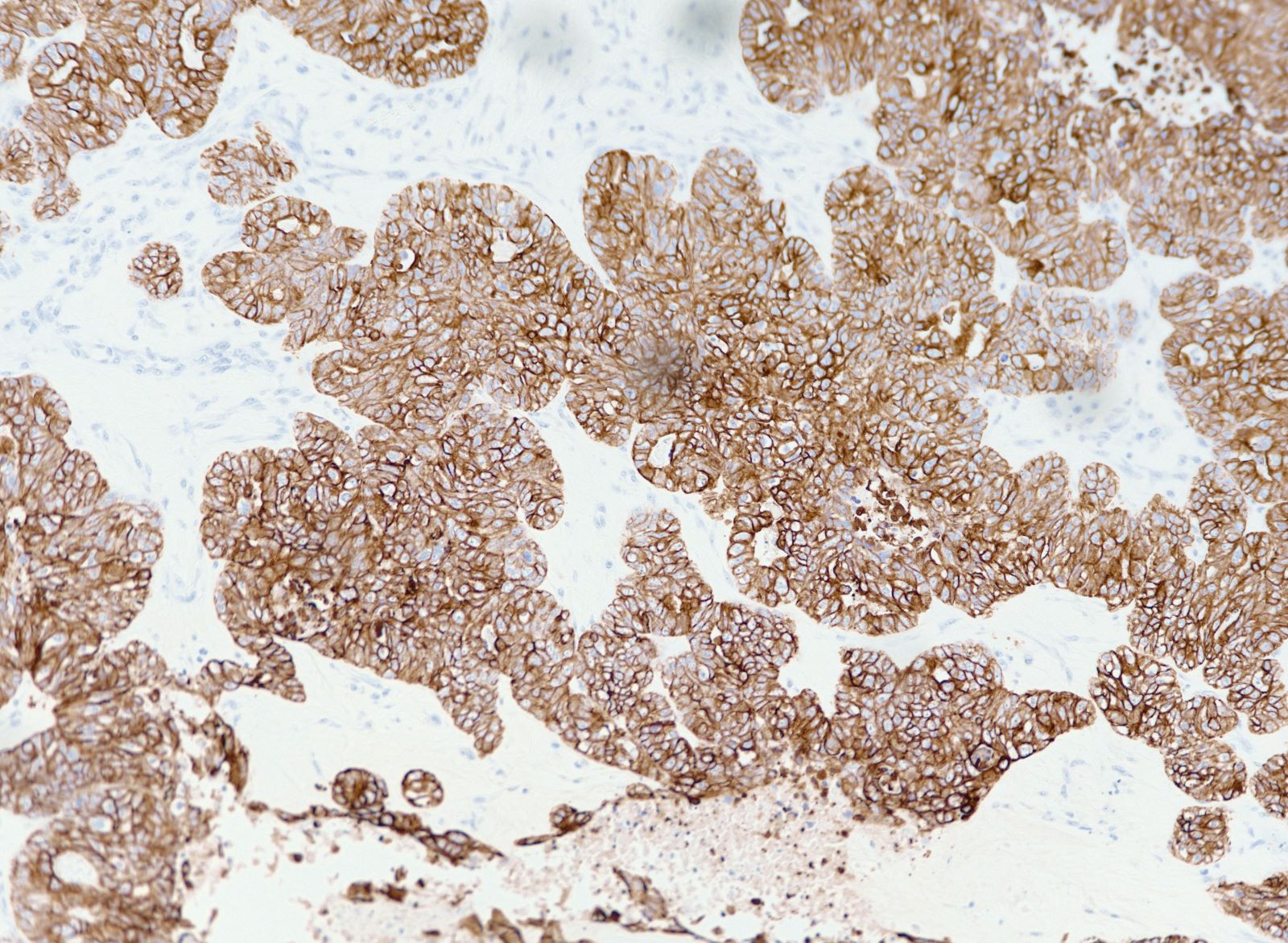
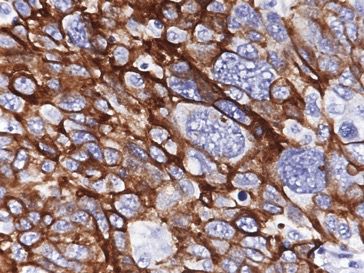
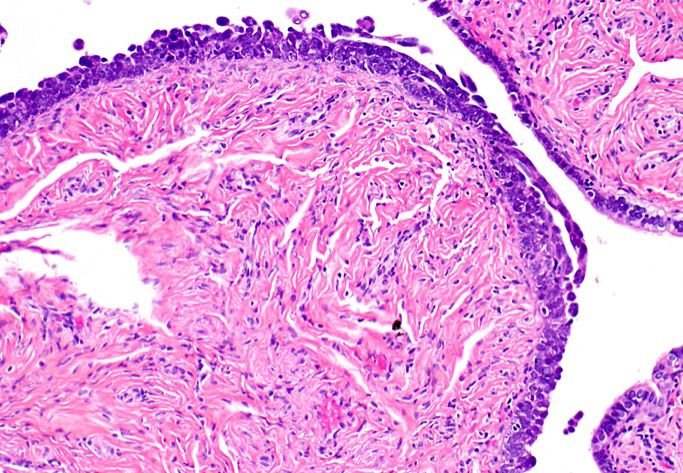
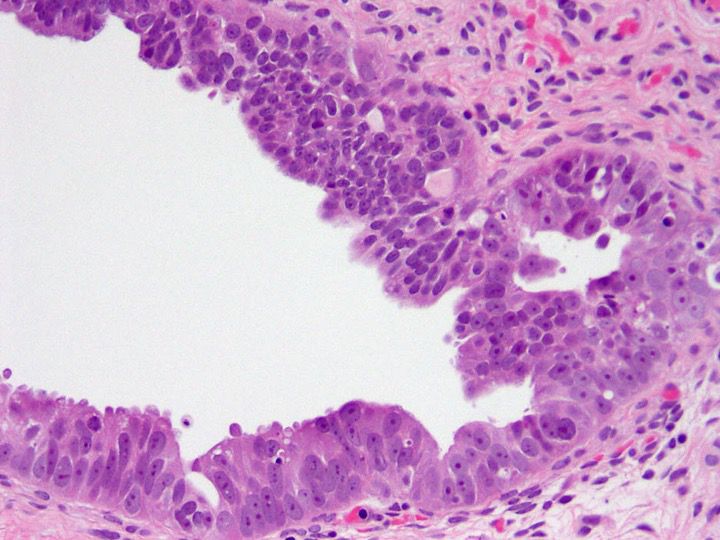
Microscopic (histologic) description
- Solid masses of columnar to cuboidal cells with eosinophilic cytoplasm and slit-like spaces (fusion of papillae)
- Solid, pseudoendometrioid, transitional cell carcinoma-like (SET) appearance (more common in BRCA1 mutations) (Mod Pathol 2012 Apr;25(4):625)
- Hierarchical papillary branching, glandular and cribriform patterns common
- Significant nuclear atypia
- Significant nuclear pleomorphism (> 3x variation in size) with large, bizarre and multinucleated forms (Hum Pathol 2005;36:1049)
- Prominent nucleolus, often large and eosinophilic
- High mitotic index: ≥ 12 mitotic figures per 10 high power fields, often atypical
- Necrosis is frequent
- Can have increased CD3+ or CD8+ tumor infiltrating lymphocytes (more common in BRCA1 mutation)
- Psammoma bodies are variable
- Serous tubal intraepithelial carcinoma (STIC) (90% fimbria, 10% ampulla / isthmus) exhibits similar histologic features; may be bilateral (10 - 20%) and multifocal
- Findings after neoadjuvant chemotherapy: single cells in a background of histiocytic reaction and fibrosis, clear cell change, decrease in mitotic figures, increased psammoma bodies
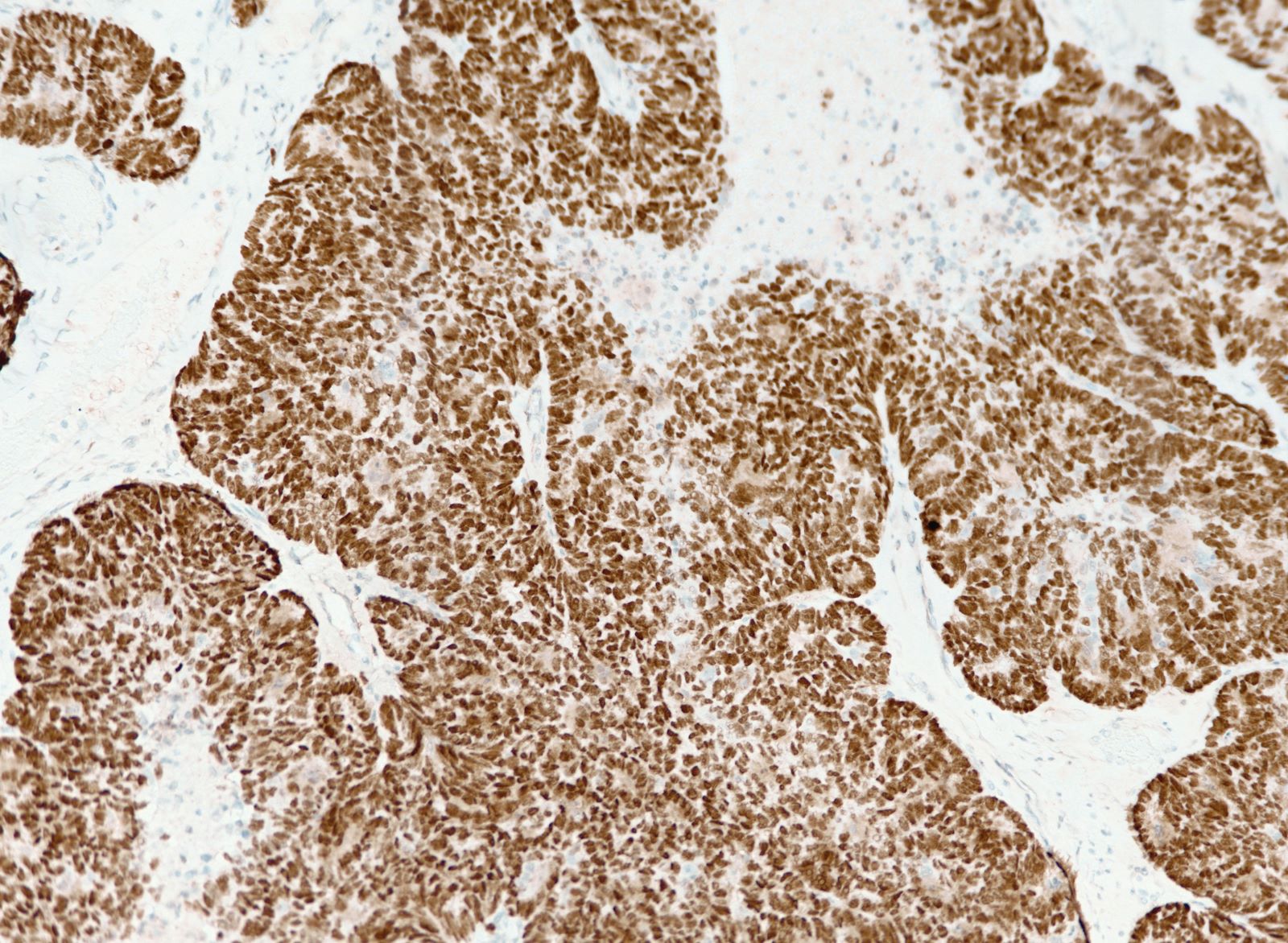
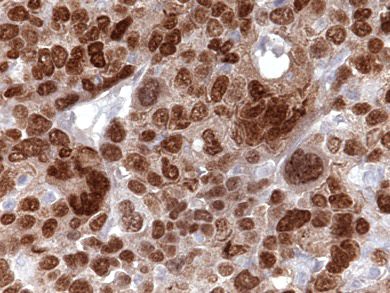
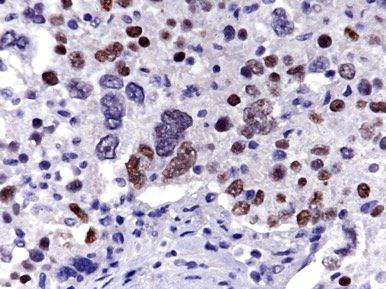
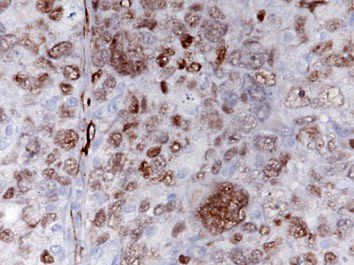
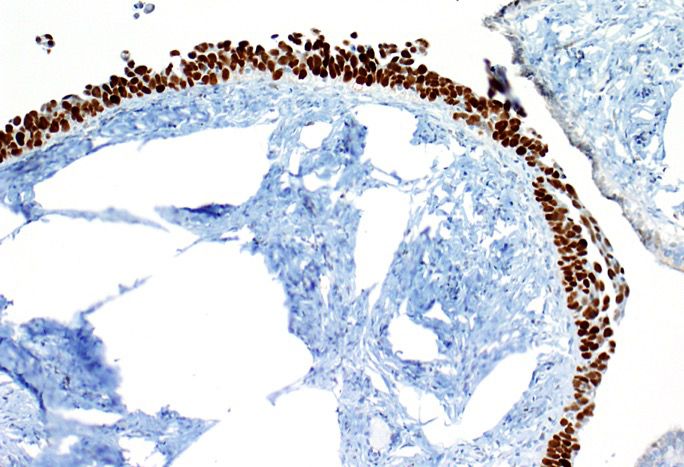
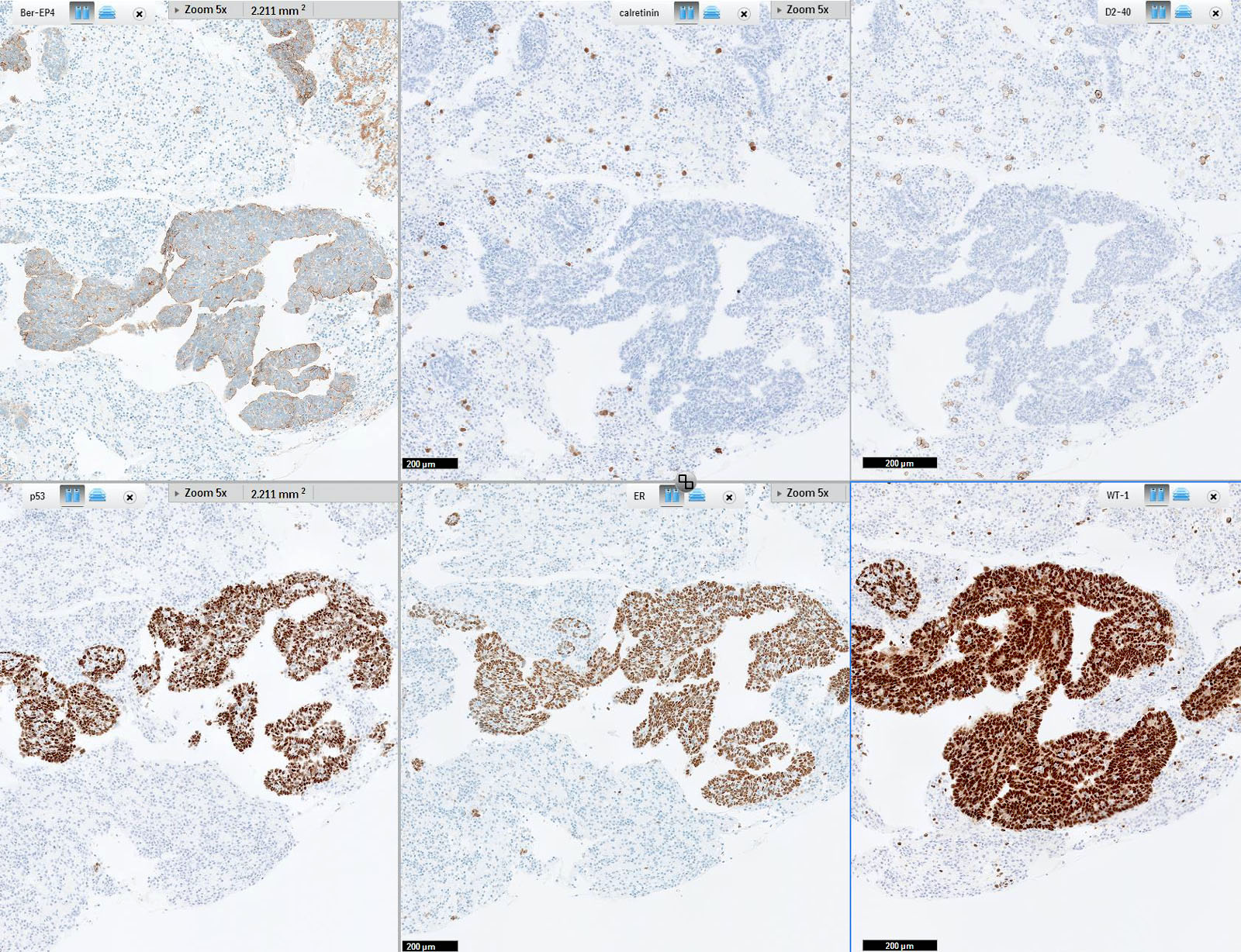
Microscopic (histologic) images
Contributed by Erna Forgó, M.D. and Teri A. Longacre, M.D.
Contributed by Jijgee Munkhdelger, M.D., Ph.D. and Andrey Bychkov, M.D., Ph.D.
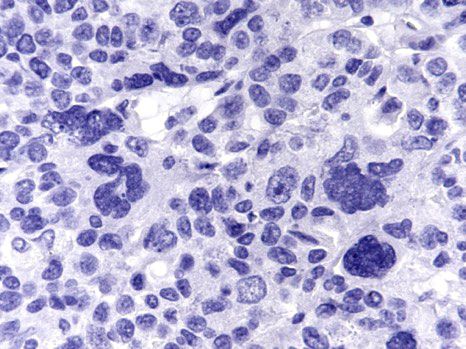
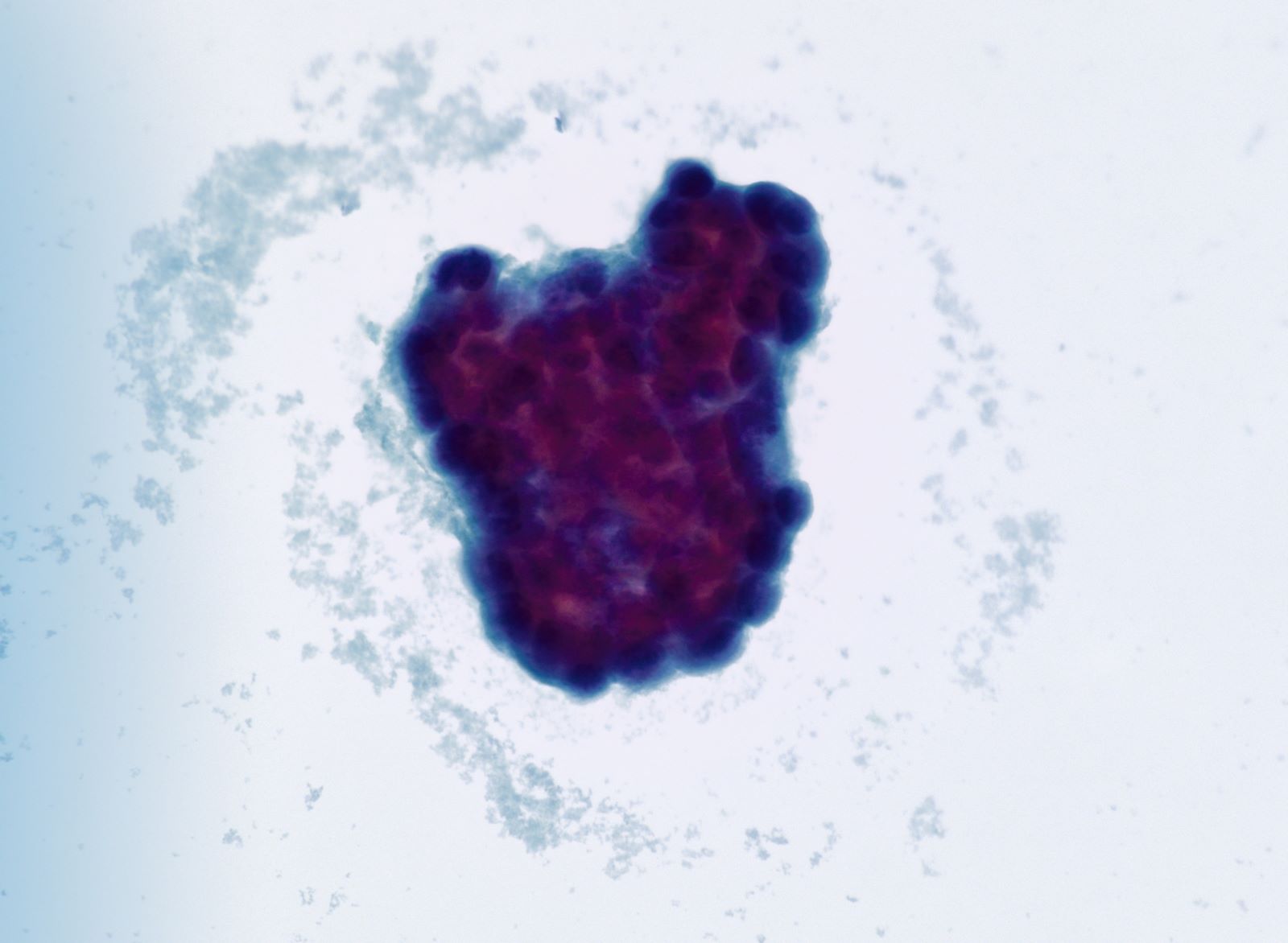
Cytology description
- 3 dimensional clusters or single cells with scant cytoplasm
- Significant nuclear pleomorphism (> 3x variation in size)
- Prominent nucleoli
Cytology images
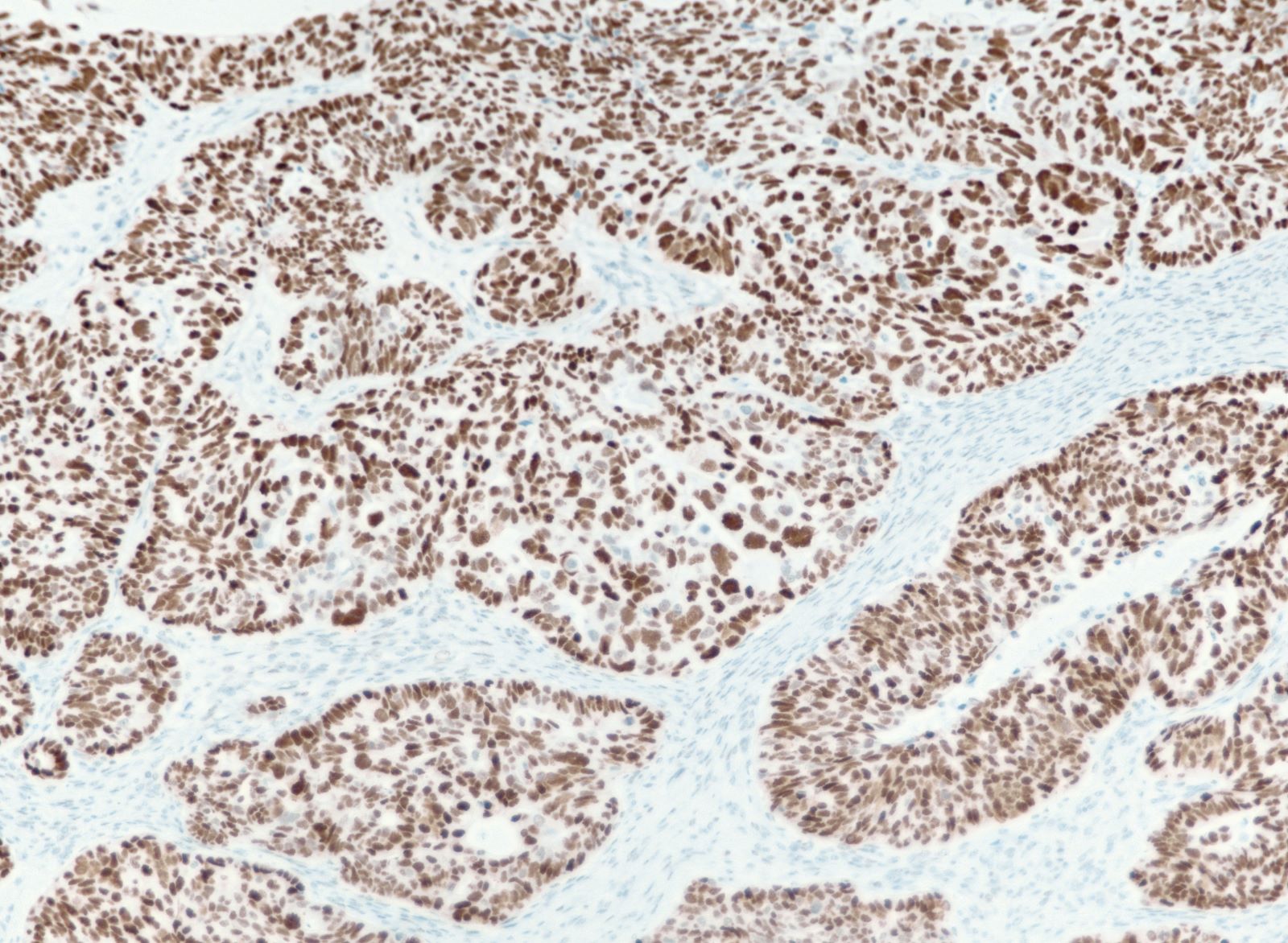
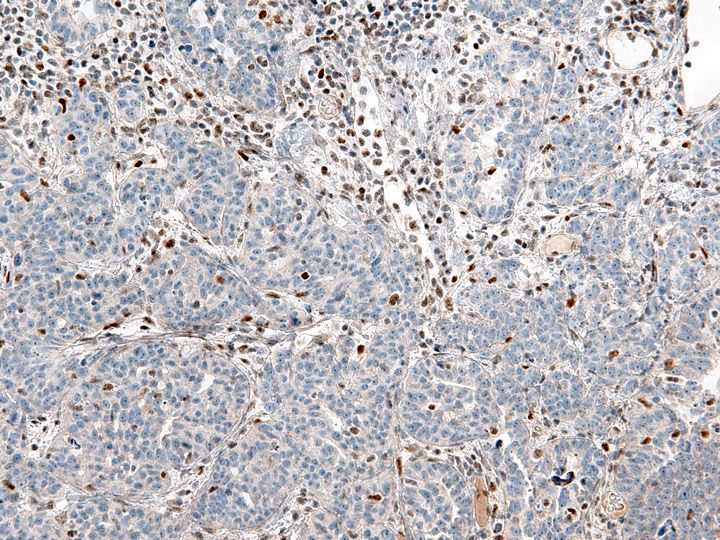
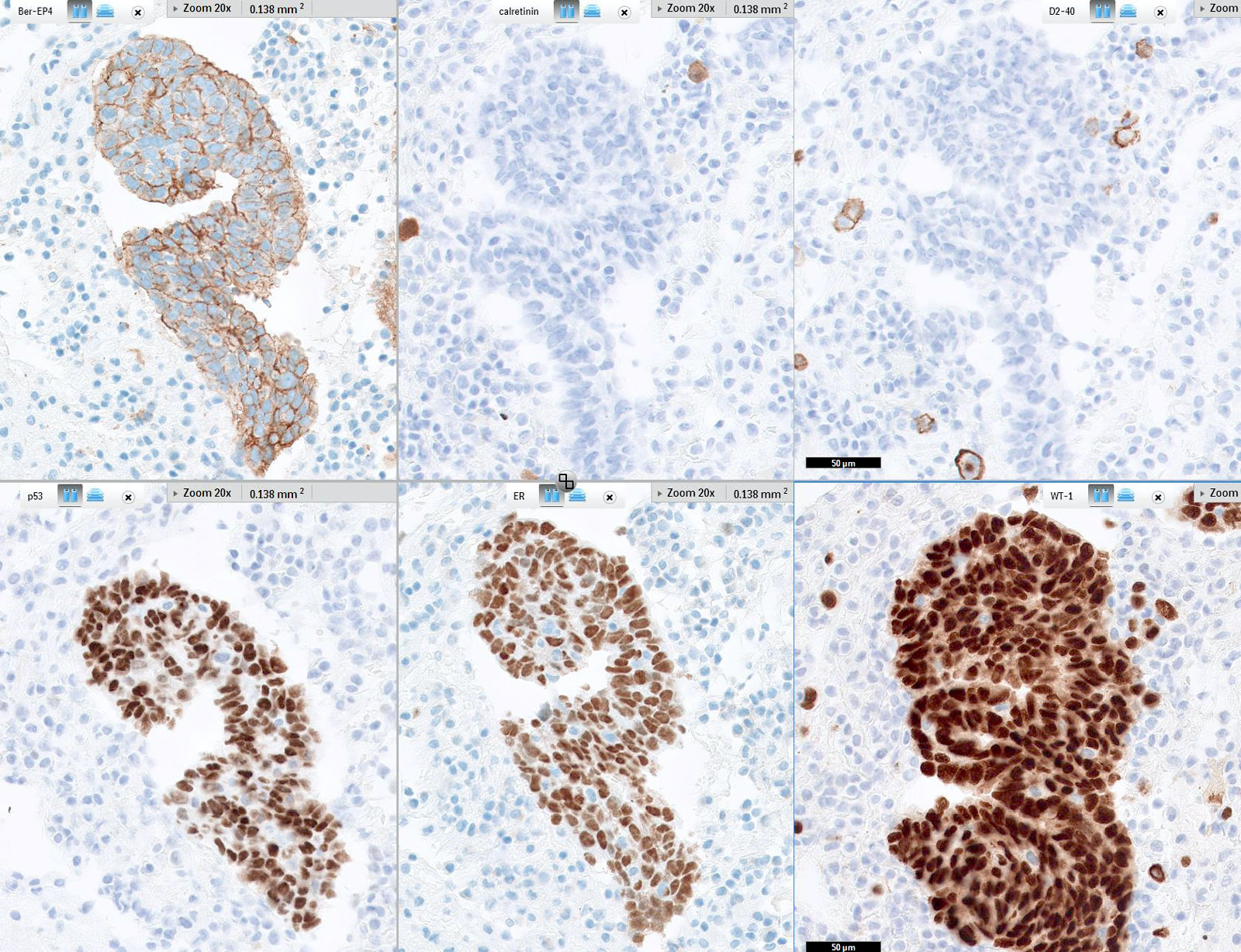
Positive stains
- PAX8, WT1, p16 (~60%), ER (80%), PR (30%), CK7, D2-40 (variable), calretinin (variable, may be focal)
- Aberrant p53 expression that correlates with TP53 mutation, 3 patterns (J Pathol Clin Res 2016;2:247, Int J Gynecol Pathol 2019;38 Suppl 1:S123):
- Overexpression: strong, diffuse nuclear staining in > 80% of cells (missense mutation)
- Null phenotype: complete absence of staining (loss of function mutation)
- Cytoplasmic expression: Cytoplasmic p53 expression with intensity similar to that of internal nuclear controls (loss of function mutation disrupting nuclear localization domain)
- High Ki67 proliferation index (> 75%) (Oncotarget 2016;8:107877)
Molecular / cytogenetics description
- TP53 alterations in nearly all cases
- Germline, somatic or promoter hypermethylation (inactivation) of BRCA1 and BRCA2 in ~50% of cases (Am J Surg Pathol 2016;40:404)
- Prominent DNA copy number changes, including CCN1, MYC, NOTCH3, PIK3CA, AKT oncogenes
Sample pathology report
- Ovary and fallopian tube, right, salpingo-oophorectomy:
- Ovary
- High grade serous carcinoma (see comment and synoptic report)
- Fallopian tube
- Intravascular involvement by high grade serous carcinoma
- Ovary
- Ovary and fallopian tube, left, salpingo-oophorectomy:
- Ovary
- High grade serous carcinoma
- Fallopian tube
- Intravascular involvement by high grade serous carcinoma
- Paratubal cysts
- Ovary
- Comment: We reviewed the frozen sections and confirm the diagnosis rendered. Histologic sections of the right and left adnexa show a high grade neoplasm growing in a solid trabecular pattern that involves both ovaries without capsular disruption. Abundant tumor associated lymphocytes are present. The tumor cells are positive for CK7 and PAX8 with abnormal (overexpression) of p53 but negative for CK20. Estrogen receptor and progesterone receptor expression is negative. These features are best characterized as high grade serous carcinoma which displays a SET (solid, pseudoendometrioid or transitional) pattern. Ovarian carcinomas which show a SET pattern of high grade serous carcinoma may be associated with BRCA gene mutations (somatic or germline).
Differential diagnosis
- Low grade serous carcinoma:
- Minimal nuclear pleomorphism (< 3x variation in size) (Hum Pathol 2005;36:1049)
- Low mitotic index (< 12 mitotic figures per 10 high power fields)
- p53 wild type expression
- p16 negative or patchy positive
- Clear cell carcinoma:
- Undifferentiated carcinoma:
- Metastatic endometrioid serous carcinoma:
- Tumor mass, with or without endometrial intraepithelial carcinoma (precursor lesion) in the endometrium
- Usually WT1 negative or patchy
- Endometrioid adenocarcinoma:
- Malignant mesothelioma:
- Simple papillae lined by 1 cell layer without tufting
- Less severe nuclear atypia
- Low mitotic activity
- D2-40, calretinin positive
- ER negative
Board review style question #1
Board review style answer #1
A. BRCA1. SET (solid, pseudoendometrioid or transitional) pattern has a strong correlation between the presence of BRCA1 mutation and ovarian high grade serous carcinoma phenotype. These tumors also tend to have a higher mitotic index, increased tumor infiltrating lymphocytes and necrosis that can be comedonecrosis or geographic necrosis, when compared with unassociated cases. Recognition of this architectural growth pattern allows for the initiation of appropriate genetic testing and referral into necessary screening programs.
Comment Here
Reference: High grade serous carcinoma
Comment Here
Reference: High grade serous carcinoma
Board review style question #2
Which is the most important prognostic factor for overall survival of ovarian high grade serous carcinoma?
- Grade
- Histologic subtype
- Mitotic index
- Stage
Board review style answer #2
D. Stage. Stage is the most important prognostic factor in ovarian high grade serous carcinoma, with a ~40% overall survival at 5 years. In advanced stage disease, the amount of residual tumor present after staging and debulking is the most important factor for survival. Ovarian, tubal and peritoneal high grade serous carcinomas are staged the same. It has been proposed that ovarian disease in absence of serous intraepithelial carcinoma (STIC) be classified as ovarian in origin, ovarian disease in the presence of STIC be classified as tubal in origin and peritoneal disease in absence of ovarian or tubal involvement be classified as peritoneal in origin.
Comment Here
Reference: High grade serous carcinoma
Comment Here
Reference: High grade serous carcinoma