Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology / etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Case reports | Treatment | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Paolino G, Luchini C. Chronic pancreatitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/pancreaschronic.html. Accessed April 18th, 2024.
Definition / general
- Pancreatic fibroinflammatory syndrome histologically characterized by parenchymal fibrosis, atrophy and duct changes and clinically by pain and symptoms of pancreatic insufficiency (Pancreatology 2020;20:586)
Essential features
- Pancreatic fibroinflammatory disease with fibrosis, loss of acinar tissue and duct changes
- Histology alone is not sufficient; clinical and radiological data are required for diagnosis (Pancreatology 2020;20:586)
Terminology
- Main category: chronic pancreatitis
- Subtypes: alcoholic pancreatitis, obstructive pancreatitis, hereditary pancreatitis, paraduodenal (groove) pancreatitis (PGP)
ICD coding
Epidemiology
- Alcoholic pancreatitis: young to middle aged males (Pathologica 2020;112:197)
- Obstructive pancreatitis: M = F; wide age range (Pathologica 2020;112:197)
- Hereditary pancreatitis: M = F; PRSS1 and CFTR related: very young patients (< 20 years old); SPINK1 associated: adult patients (Nat Genet 1996;14:141, Gastroenterology 1981;81:1143, Nat Genet 2000;25:213)
- Paraduodenal pancreatitis: middle aged males with a history of alcohol abuse and smoking (World J Surg 2009;33:2664)
Sites
- Alcoholic and hereditary chronic pancreatitis affects the whole pancreas
- Obstructive pancreatitis affects the gland distal to the site of obstruction
- Paraduodenal pancreatitis is centered around the minor papilla, in the so called groove area between the common bile duct, the superior margin of the pancreatic head and the duodenal wall (Pathologica 2020;112:197)
Pathophysiology / etiology
- Alcoholic pancreatitis: prolonged alcohol abuse and other cofactors such as smoking (Alcohol Health Res World 1997;21:13)
- Obstructive pancreatitis: obstruction of main or secondary pancreatic ducts due to mass forming lesions or intraductal stones
- Hereditary pancreatitis: germline mutations in the genes serine protease 1 (PRSS1) or serine peptidase inhibitor kazal type 1 (SPINK1); autosomal recessive mutations in cystic fibrosis transmembrane conductance regulator (CFTR)
- Paraduodenal pancreatitis: chronic obstruction of the minor papilla (Pathologica 2020;112:197)
Clinical features
- Severe abdominal pain, often radiated to the interscapular region
- Signs and symptoms of exocrine and endocrine pancreatic dysfunction: steatorrhea, weight loss, bloating, diabetes (J Clin Gastroenterol 2022;56:e1)
- Paraduodenal pancreatitis may be associated with signs and symptoms of duodenal stenosis such as postprandial vomit
- Risk of developing pancreatic ductal adenocarcinoma is increased tenfold in patients with chronic pancreatitis
Diagnosis
- Histology alone is not gold standard; clinical and radiological data are required for a definitive diagnosis of chronic pancreatitis (Pancreatology 2020;20:586)
- Typical clinical picture
- History of alcohol abuse or smoking
- Pancreatic calcifications on CT scans
- Morphological triad of fibrosis, loss of acinar tissue and duct changes
Laboratory
- Lab tests alone are of limited utility in the diagnosis of chronic pancreatitis
- Low plasma amylase levels, particularly in advanced cases (Alcohol Health Res World 1997;21:13)
Radiology description
- Ultrasound: diffuse hyperechogenicity
- CT: parenchymal atrophy, duct dilation, presence of calcification and pseudocysts
- Paraduodenal pancreatitis may mimic cystic lesions or malignancy and may be associated with the so called double duct sign, due to dilation of the main pancreatic duct and the common bile duct (Alcohol Health Res World 1997;21:13)
Case reports
- 34 year old man with a mass forming chronic pancreatitis mimicking a cystic neoplasm (World J Gastroenterol 2018;24:297)
- 39 year old woman with hereditary pancreatitis who developed a pancreatic anaplastic carcinoma (Am J Case Rep 2021;22:e928993)
- 51 year old woman with paraduodenal pancreatitis mimicking undifferentiated carcinoma with osteoclastic giant cells (UCOCGC) (Cytopathology 2015;26:122)
- 57 year old man with chronic pancreatitis with ductal stones in the pancreatic head, successfully treated by surgery (J Surg Case Rep 2020;2020:rjaa352)
Treatment
- Therapeutic strategies are mostly supportive
- Paraduodenal pancreatitis may require pancreaticoduodenectomy
- Mass forming / symptomatic cases may be amenable to surgical resection
- Reference: Dis Mon 2021;67:101225
Gross description
- Whitish parenchyma with extensive fibrosis, dilated ducts and calculi
- Fibrotic parenchyma retains a lobulated appearance
- In advanced stages, a reduction in the volume of the pancreatic gland may occur
- Parenchymal and intraductal calcification are typical and often grossly appreciable
- Pseudocysts are more common in alcoholic pancreatitis, whereas obstructive pancreatitis shows retention cysts (Pathologica 2020;112:197)
- Paraduodenal pancreatitis may show cystic change near the minor ampulla and trabeculated fibrosis centered around the duodenal wall (Semin Diagn Pathol 2004;21:247)
Gross images
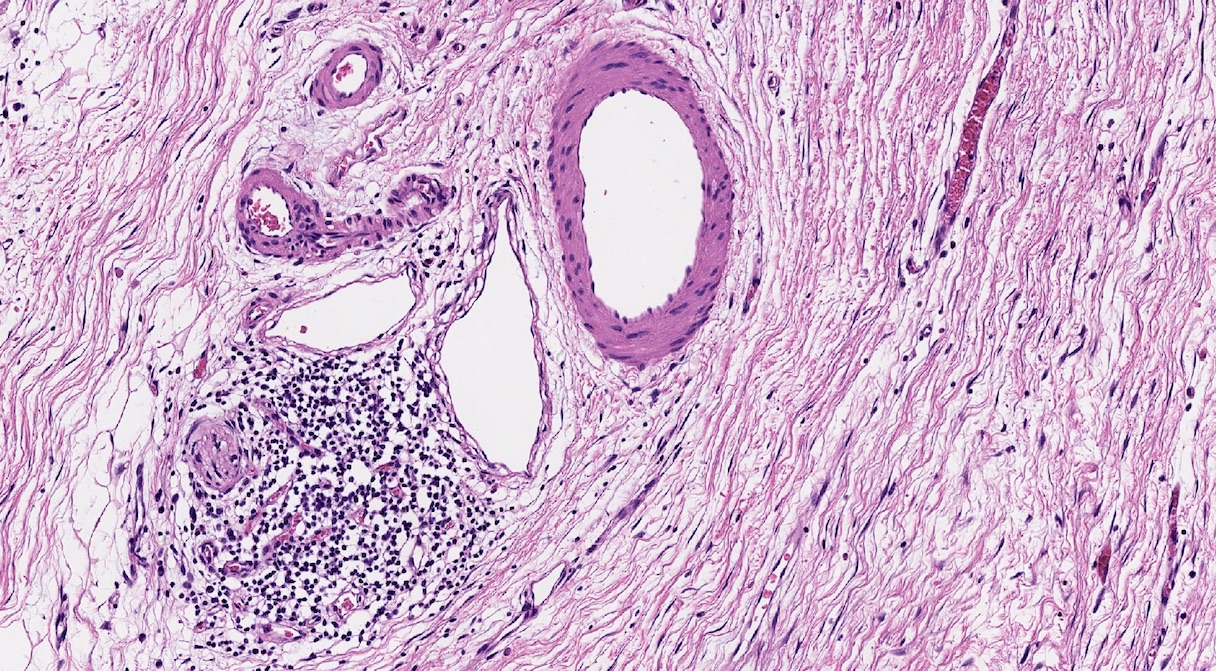
Frozen section description
- Frozen sections may show extensive fibrosis of the parenchyma and architectural distortion of pancreatic ducts
- To identify invasive carcinoma on frozen sections with chronic pancreatitis, look for ruptured glands, high grade dysplasia, mitoses, perineural invasion, naked gland in peripancreatic adipose tissue
- References: Arch Pathol Lab Med 2005;129:1610, Arch Pathol Lab Med 2022;146:84
Frozen section images
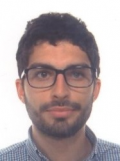
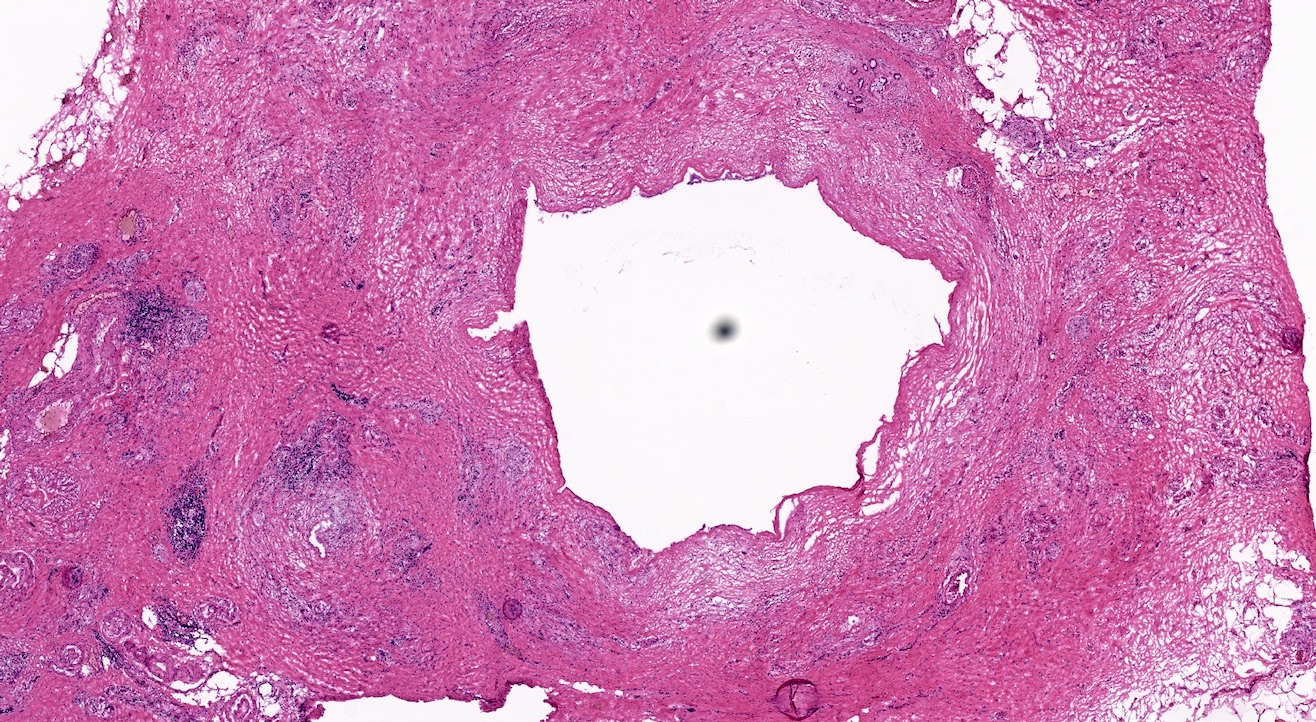
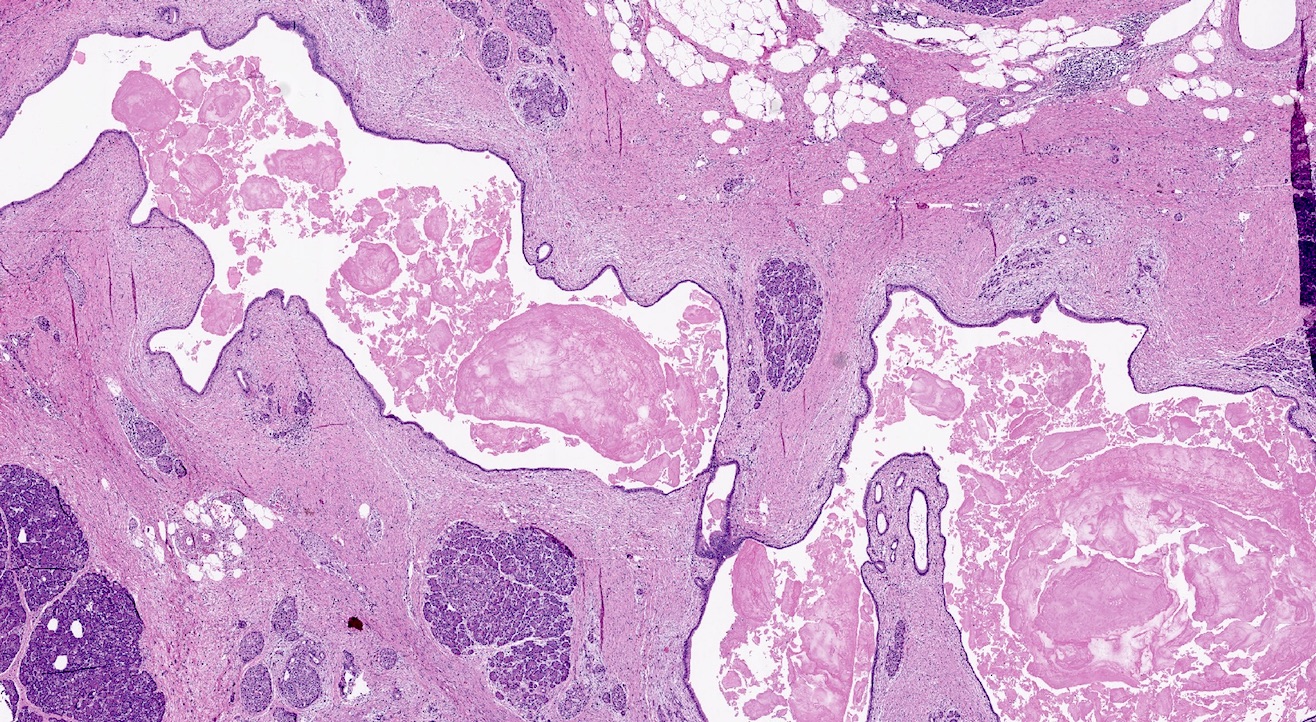
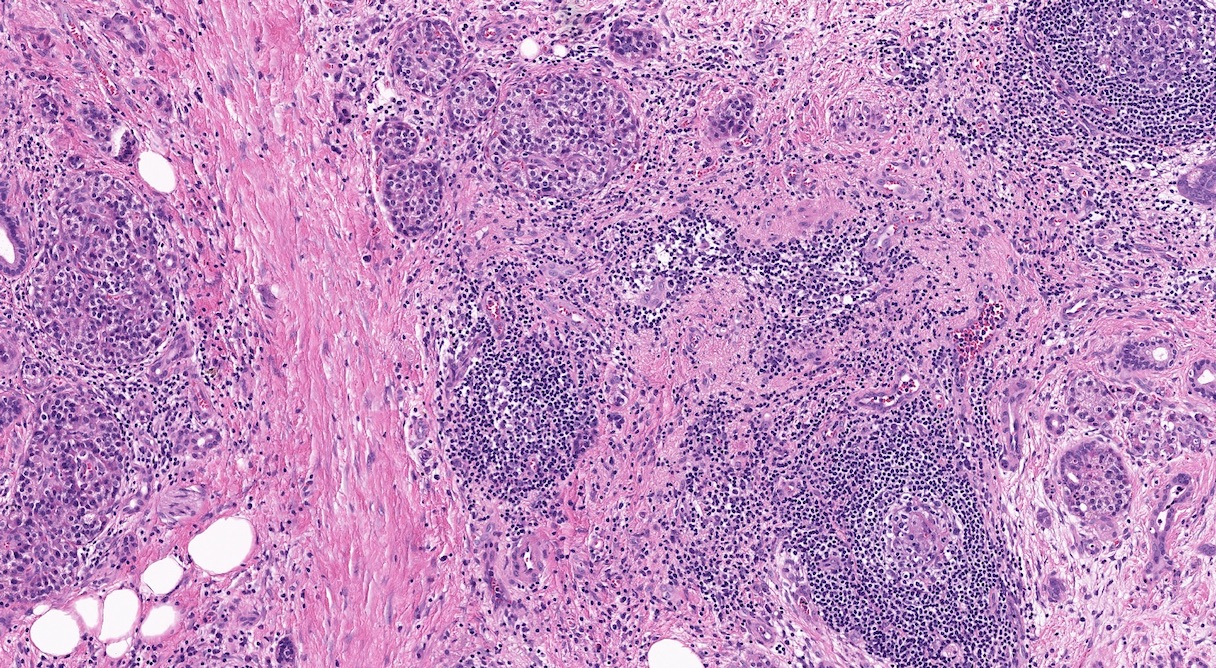
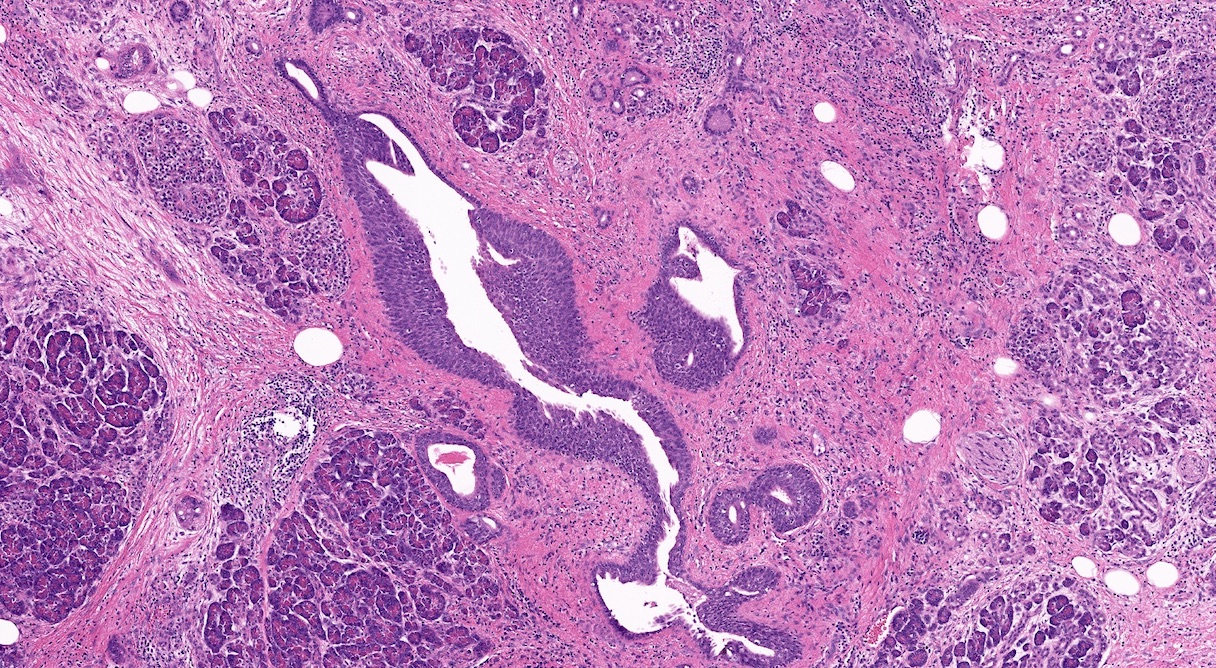
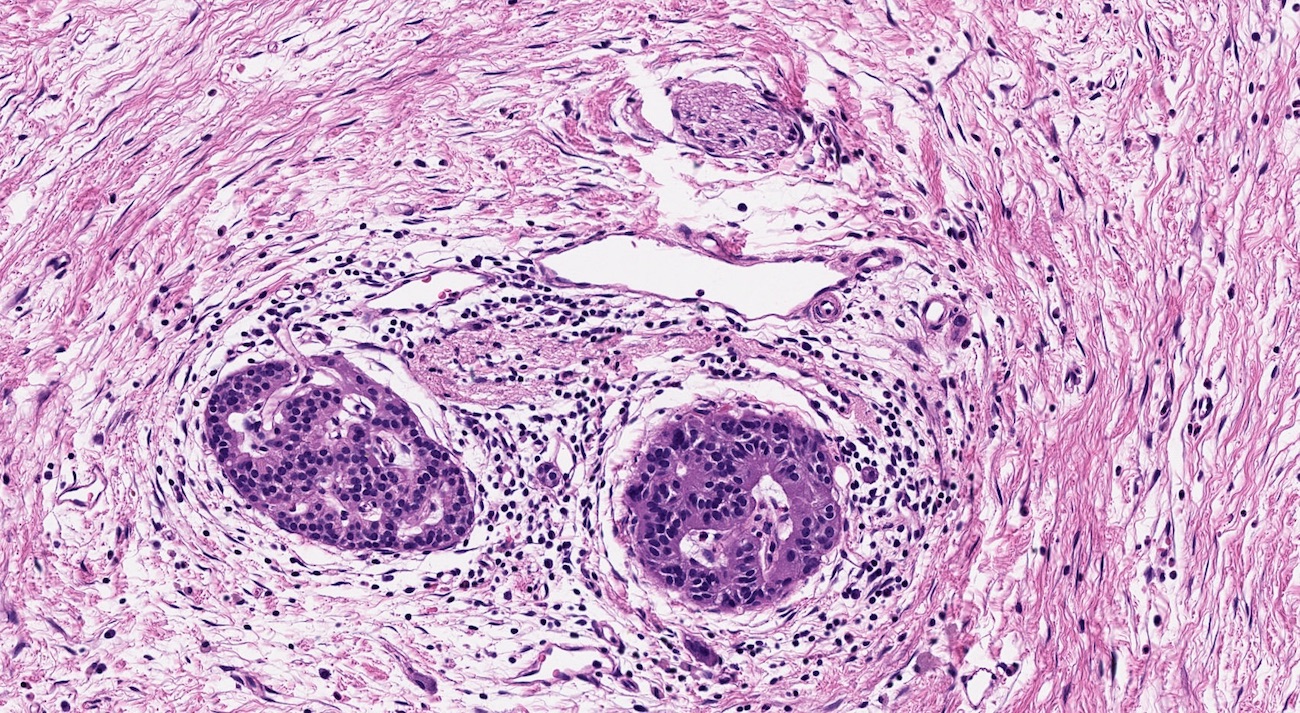
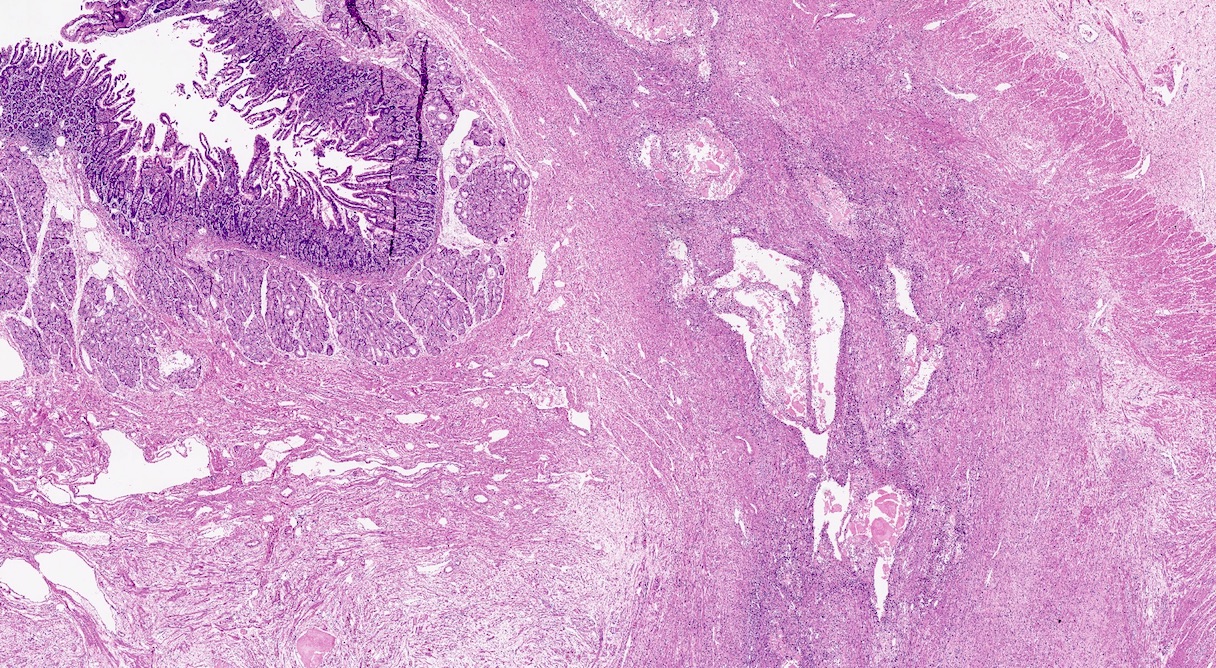
Microscopic (histologic) description
- Triad of cardinal features: fibrosis, loss of acinar tissue, duct changes (Pancreatology 2020;20:586)
- No universally accepted and reproducible grading system (Pancreatology 2020;20:586)
- No unique morphologic features to distinguish different etiologies of nonautoimmune chronic pancreatitis
- Fibrosis is initially perilobular; during disease progression, it involves the pancreatic lobular units, eventually replacing the acinar parenchyma (so called intralobular fibrosis)
- Acinar tissue may be replaced by fibrosis or fatty tissue; the latter process (lipomatous atrophy) is more frequently seen in hereditary pancreatitis (Pathologica 2020;112:197)
- Loss of acinar tissue predates that of pancreatic islets, which are often seen isolated in fibrosis or fatty tissue in advanced cases
- Ductal changes include distortion of ductal profiles, ectasia, presence of intraluminal concretions of amorphous material (so called protein plugs), squamous metaplasia, intraductal calcification
- Foci of low and high grade pancreatic intraepithelial neoplasia (PanIN) may be encountered
- Foci of periductal chronic inflammation and fat necrosis represent a common finding
- Pseudocysts lined by granulation tissue are common in alcoholic chronic pancreatitis
- Paraduodenal pancreatitis shows Brunner gland hyperplasia, myofibroblastic proliferation in the duodenal wall, cysts lined by cuboidal ductal epithelium, which may be replaced by granulation tissue; multinucleated giant cells may be found (Cytopathology 2015;26:122)
Microscopic (histologic) images
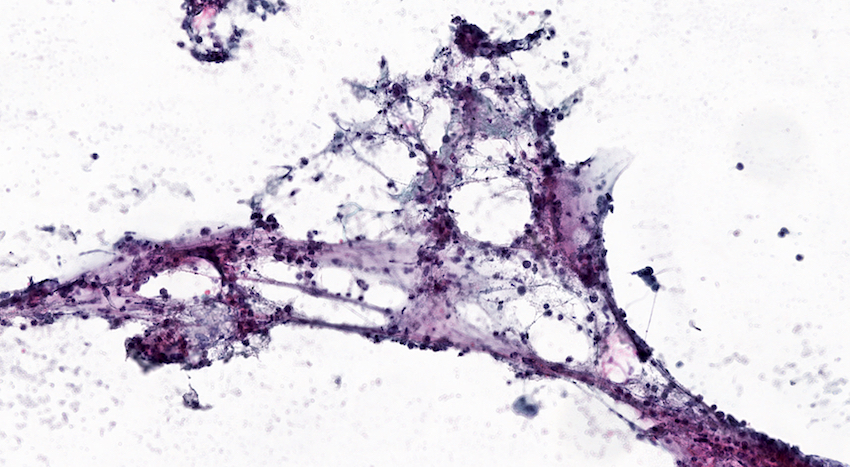
Cytology description
- Clusters of acinar cells with mild atypia and no atypical mitotic figures
- Chronic inflammatory elements: lymphocytes, macrophages
- Clusters of activated fibroblasts may be found
- Proteinaceous material may be present
- Neutrophils may be present in case of associated acute inflammation
- Multinucleated giant cells may be present in paraduodenal pancreatitis (Cytopathology 2015;26:122)
Cytology images
Positive stains
- Ductal epithelium is positive for keratins CK7 and CK19
- Nuclear expression of SMAD4 is retained
- Reference: World J Gastrointest Surg 2021;13:406
Negative stains
- Staining for p53 does not show a mutated pattern of expression
Molecular / cytogenetics description
- Most common mutations in PRSS1 related hereditary pancreatitis are R122H, R122C, N29I and A16V (Am J Physiol Gastrointest Liver Physiol 2014;306:G466)
- SPINK1 related pancreatitis is associated with the presence of high risk SPINK1 N34S haplotype (PLoS One 2008;3:e2003)
Sample pathology report
- Duodenum and pancreatic head, pancreaticoduodenectomy:
- Pancreatic head with diffuse fibrous replacement of acinar tissue, foci of chronic inflammation, pseudocysts lined by granulation tissue, duct ectasia with protein plugs and squamous metaplasia of the lining epithelium (see comment)
- No evidence of infiltrating carcinoma
- 12 lymph nodes and duodenal margins with no significant pathologic change
- Comment: Histologic picture is consistent with chronic pancreatitis.
Differential diagnosis
- Pancreatic ductal adenocarcinoma:
- Ruptured glands, gland in peripancreatic adipose tissue without pancreatic islets, mitotic figures, perineural and vascular invasions are useful tips in the differential diagnosis
- Immunohistochemistry for p53 and SMAD4 may be of aid in the differential diagnosis between chronic pancreatitis and foci of ductal adenocarcinoma
- Autoimmune pancreatitis type 1:
- Chronic inflammation centered around ducts and venules
- Presence of ≥ 10 IgG4 positive plasma cells/high power field (HPF), although a widely accepted and standardized threshold is still lacking
- Integration of clinical, laboratory and radiological data is required for differential diagnosis
- Autoimmune pancreatitis type 2:
- Granulocytic epithelial lesions (GEL) with formation of neutrophil microabscesses within the duct lumen
- Integration of clinical, laboratory and radiological data is required for differential diagnosis
Additional references
Board review style question #1
What are the cardinal features of chronic pancreatitis?
- Fat necrosis, chronic inflammation and loss of Langerhans islets
- Fibrosis, loss of acinar tissue and duct changes
- Giant cell granulomas, perineural inflammation and plasma cell infiltrate
- Intraductal proliferative lesions, lipomatous atrophy and perivenulitis
- Necrosis, granulocytic epithelial lesions and pseudocysts
Board review style answer #1
Board review style question #2
Is there a reproducible grading system for chronic pancreatitis?
- No, there is no universally accepted grading system
- Yes, grading is based on the degree of acinar tissue loss
- Yes, grading is based on the entity of fibrosis
- Yes, grading is based on the presence of pseudocysts
- Yes, grading is based on the severity of chronic inflammation
Board review style answer #2
A. No, there is no universally accepted grading system. However, classification as mild, moderate or severe may be applied.
Comment Here
Reference: Chronic pancreatitis
Comment Here
Reference: Chronic pancreatitis