Table of Contents
Definition / general | Procedure | Sections to obtain | Tips | Gross description | Gross images | Gross template samples | Additional references | Board review style question #1 | Board review style answer #1Cite this page: Sahin Ozkan H, Basturk O. Grossing. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/pancreasgrossing.html. Accessed April 18th, 2024.
Definition / general
- This topic describes how to gross specimens obtained from pancreaticoduodenectomy, distal pancreatectomy and total pancreatectomy procedures
- Essential clinical history: none
Procedure
Pancreaticoduodenectomy (Whipple) specimens:
Distal pancreatectomy specimens:
Total pancreatectomy specimens:
- Orientation and external examination
- Specimen consists of pancreatic head and duodenum and occasionally distal stomach and gallbladder
- Examine the specimen freshly
- Measure the overall specimen and each organ / structure
- Identify the trapezoid:
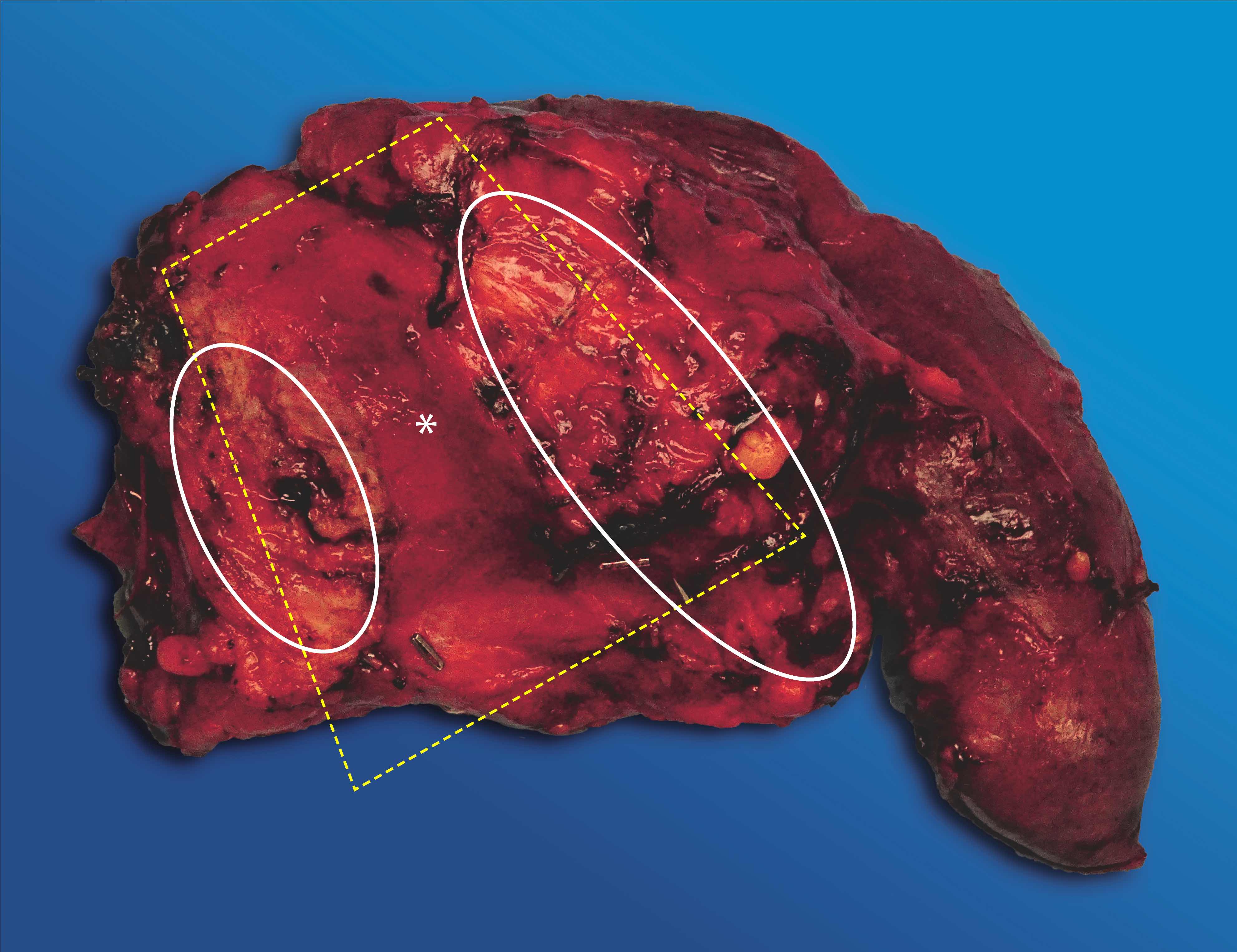
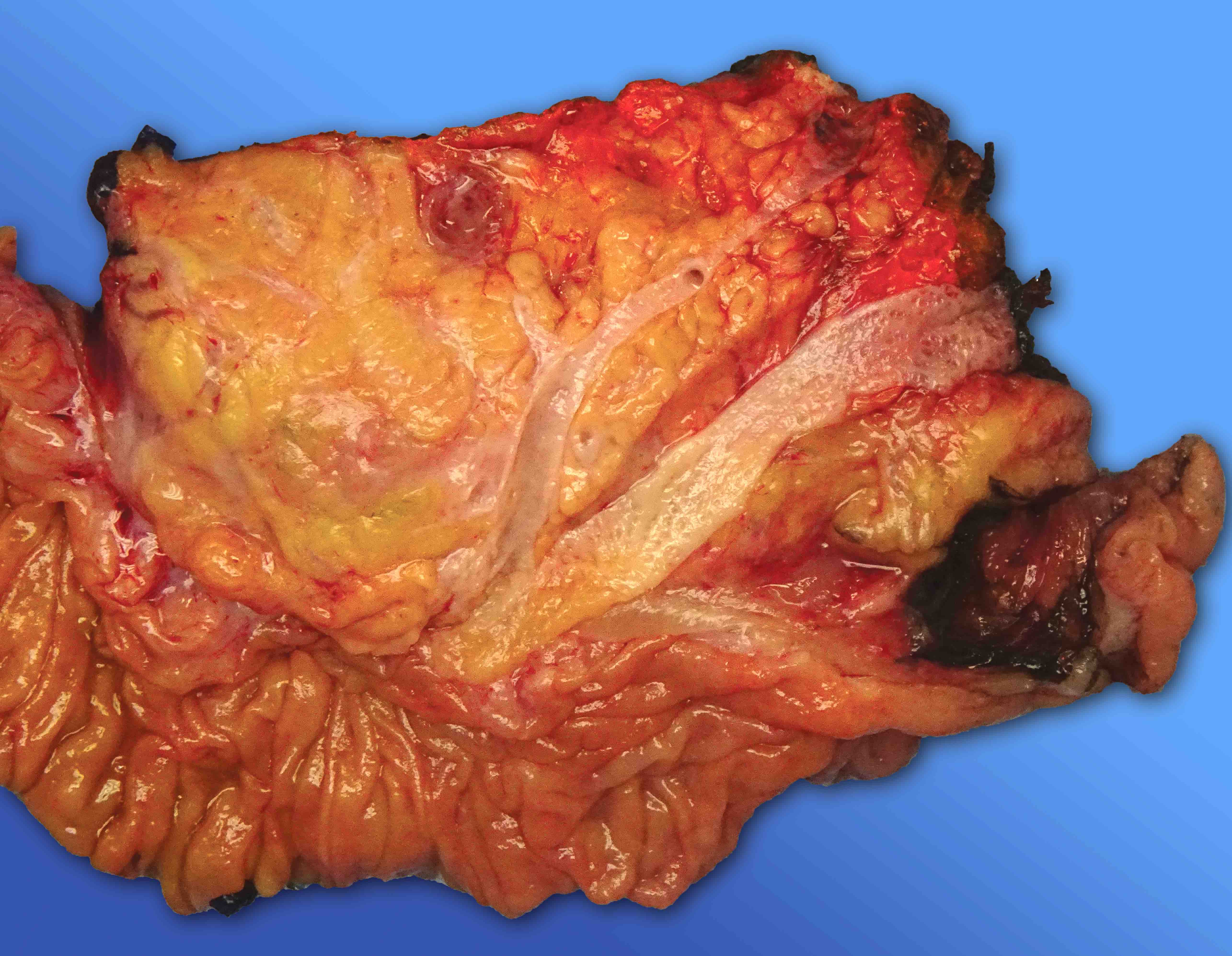
- There is a trapezoid shaped area in the posteromedian aspect of the pancreatic head (Am J Surg Pathol 2014;38:480)
- The center of the trapezoid is a concave, smooth and shiny surfaced firm area, on which the superior mesenteric vein / portal vein and superior mesenteric artery lie
- This area is referred to as the vascular groove or vascular bed (see figure 1)
- Identify and ink the important structures and margins:
- Trapezoid is formed by the pancreatic neck margin on the left, the uncinate margin on the right and the common bile duct (CBD) on the top (see figure 1)
- Pancreatic duct (PD) is in the upper half of the pancreatic neck margin towards the vascular groove
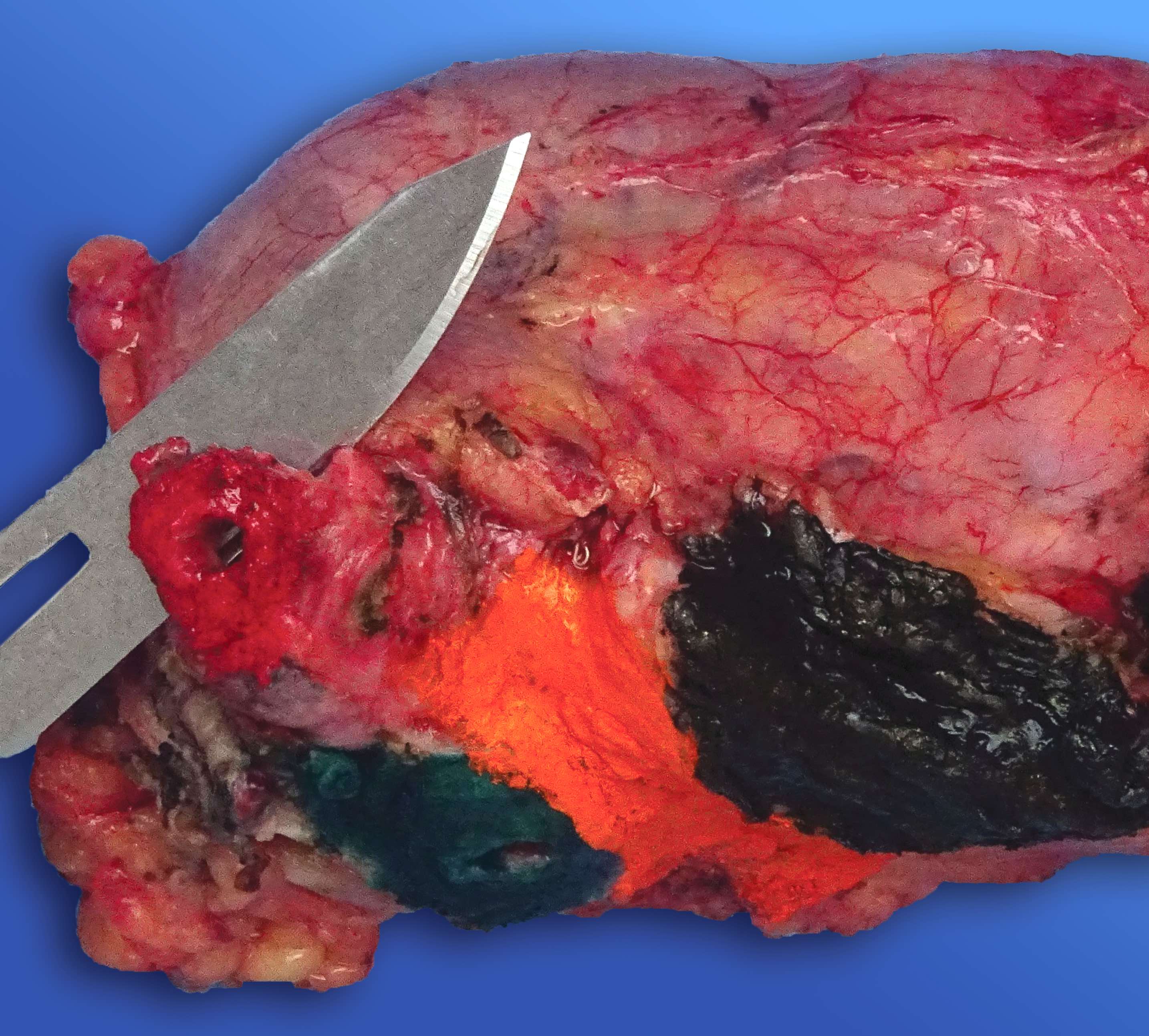
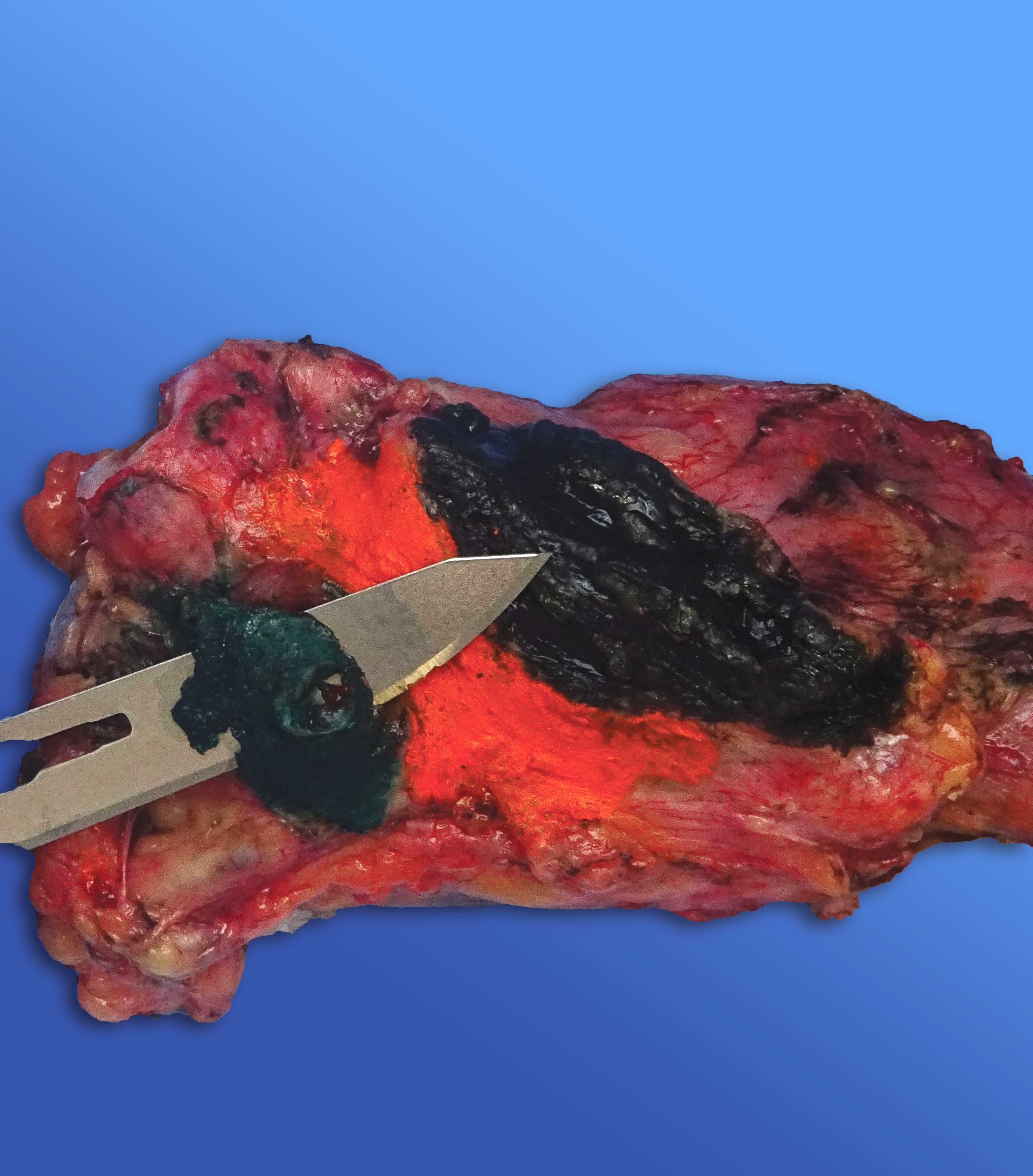
- Ink the pancreatic neck margin, uncinate margin and common bile duct margin with different colors (e.g., green, black and red, respectively) (see figure 2)
- Although it is not a surgical margin, ink the vascular groove area (e.g., orange) as well, after checking if it includes a portion of the portal vein (Am J Surg Pathol 2014;38:480)
- Check if a portion of the portal vein is present in the vascular groove area: if present, ink the superior and inferior margins using different colors
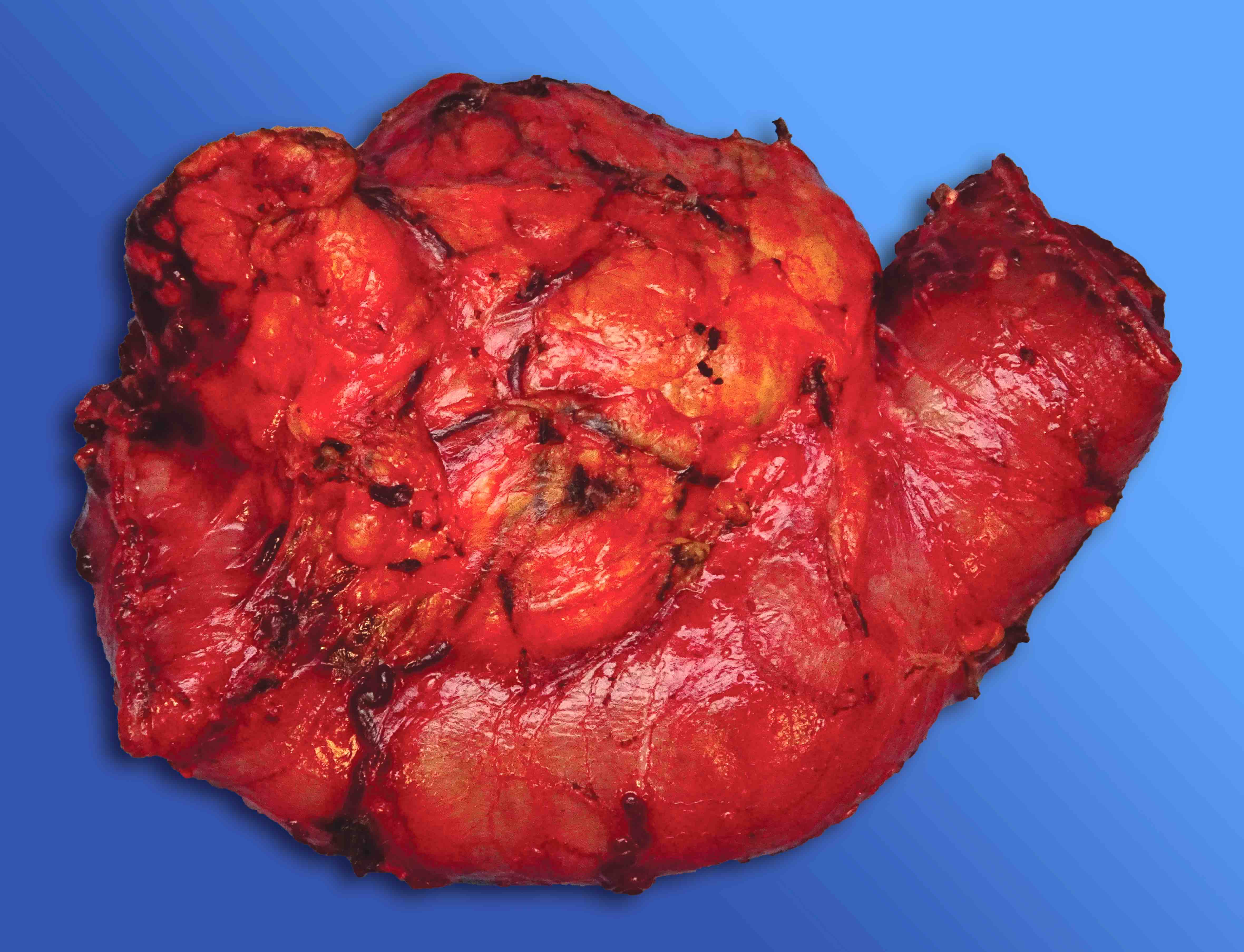
- Identify and ink the anterior and posterior free peritoneal surfaces:
- Anterior free surface is convex shaped and contains abundant fat tissue
- Pancreatic head - duodenum transition is abrupt and easily identifiable on this surface (see figure 3)
- However, the posterior free surface is flat and shiny in appearance while the pancreatic head - duodenum transition in this area is smoother and barely identifiable (see figure 4)
- If not sutured or stapled, the common bile duct margin can be seen readily on this aspect
- Although they are not surgical margins, it is encouraged to ink the anterior and posterior free surfaces in different colors (e.g., blue for anterior, black for posterior) (Am J Surg Pathol 2014;38:480)
- Removing the margins
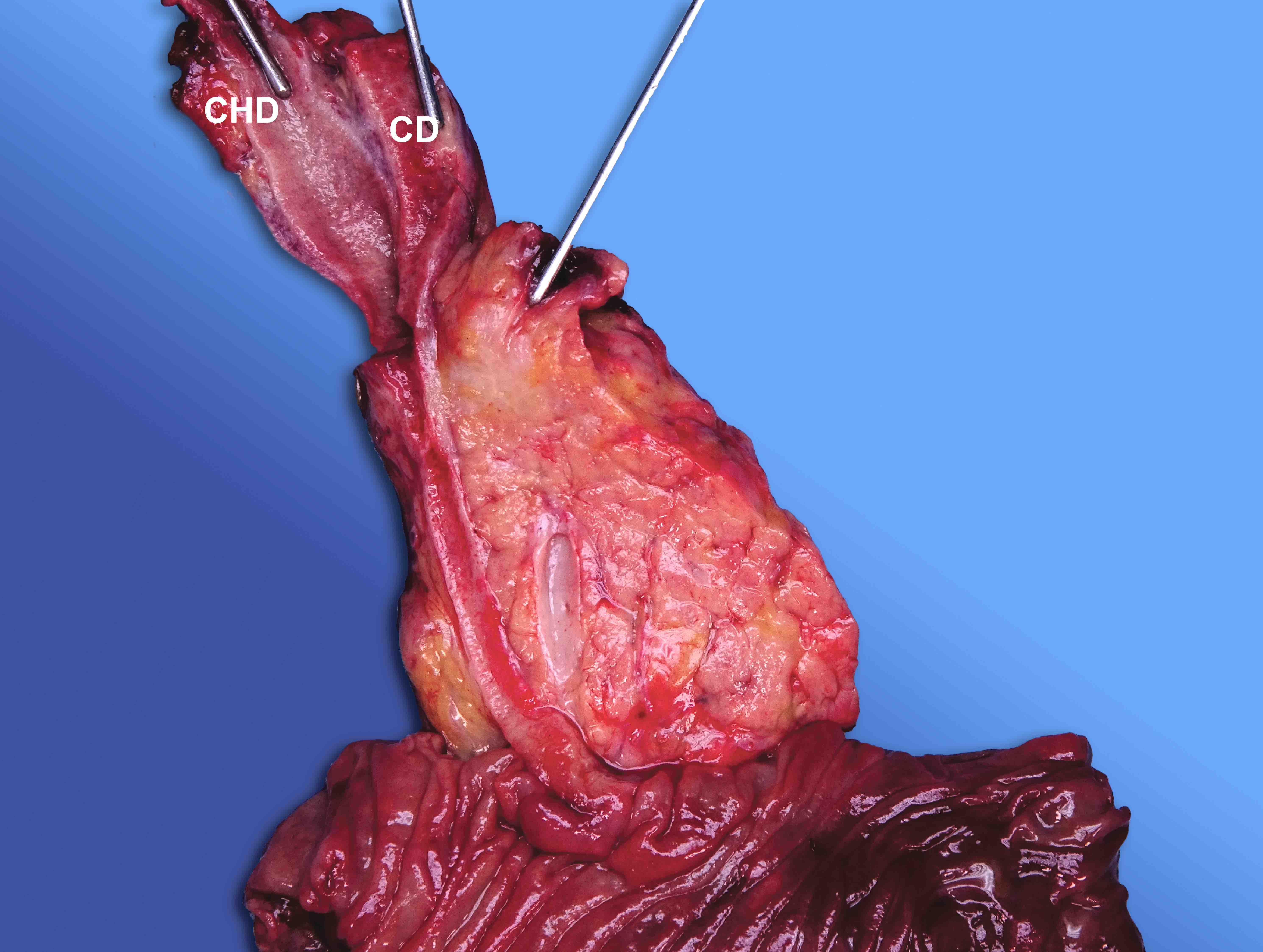
- Bile duct margin:
- Shave and submit enface (see figure 5) (Am J Surg Pathol 2014;38:480)
- Bile duct margin corresponds to the CBD margin in most of the specimens
- However, if gallbladder is attached to the specimen, it corresponds to common hepatic duct (CHD) margin
- If the specimen includes cystic duct (CD) without attached gallbladder, it corresponds to both CHD and CD margins
- Pancreatic neck margin (including PD): shave and submit enface (see figure 6) (Am J Surg Pathol 2014;38:480)
- Uncinate (retroperitoneal or posteroinferior or superior mesenteric artery) margin:
- This margin is formed by blunt dissection of the pancreatic head from the retroperitoneal soft tissues in the posterior inferior aspect of the uncinate process, rather than a surgical cut
- Shave and submit entirely as 3 - 4 mm thick bread loaf sections in 2 or 3 cassettes (see figure 7) (Am J Surg Pathol 2014;38:480)
- Portal vein margins (if present): superior and inferior margins of the vein can be shaved and submitted enface or can be submitted as a part of the main perpendicular sections of the vessel wall
- Vascular groove (vascular bed or superior mesenteric / portal vein bed) surface:
- Submitting 1 perpendicular section that shows the area closest to the tumor is enough for most of the cases
- However, shaving and submitting bread loaf sections just like the uncinate margin is another option
- Proximal (stomach / duodenum) and distal (duodenum) margins: submit 1 shaved section from each margin
- Bile duct margin:
- Opening the duodenum and examining intraduodenal aspect
- Open through the antipancreatic (antiampullary) border (Am J Surg Pathol 2014;38:480)
- Inspect the ampullary region to identify and describe any lesions (e.g., intra / periampullary localization; mass forming, papillary or mucinous features, etc.)
- Inspect the minor (accessory) ampulla, if present:
- It is located ~2 cm anterior and superior to the main ampulla and looks like a small bump / nodule / polyp (see figure 8)
- In some cases, the PD might open into minor ampulla (Am J Surg Pathol 2014;38:480)
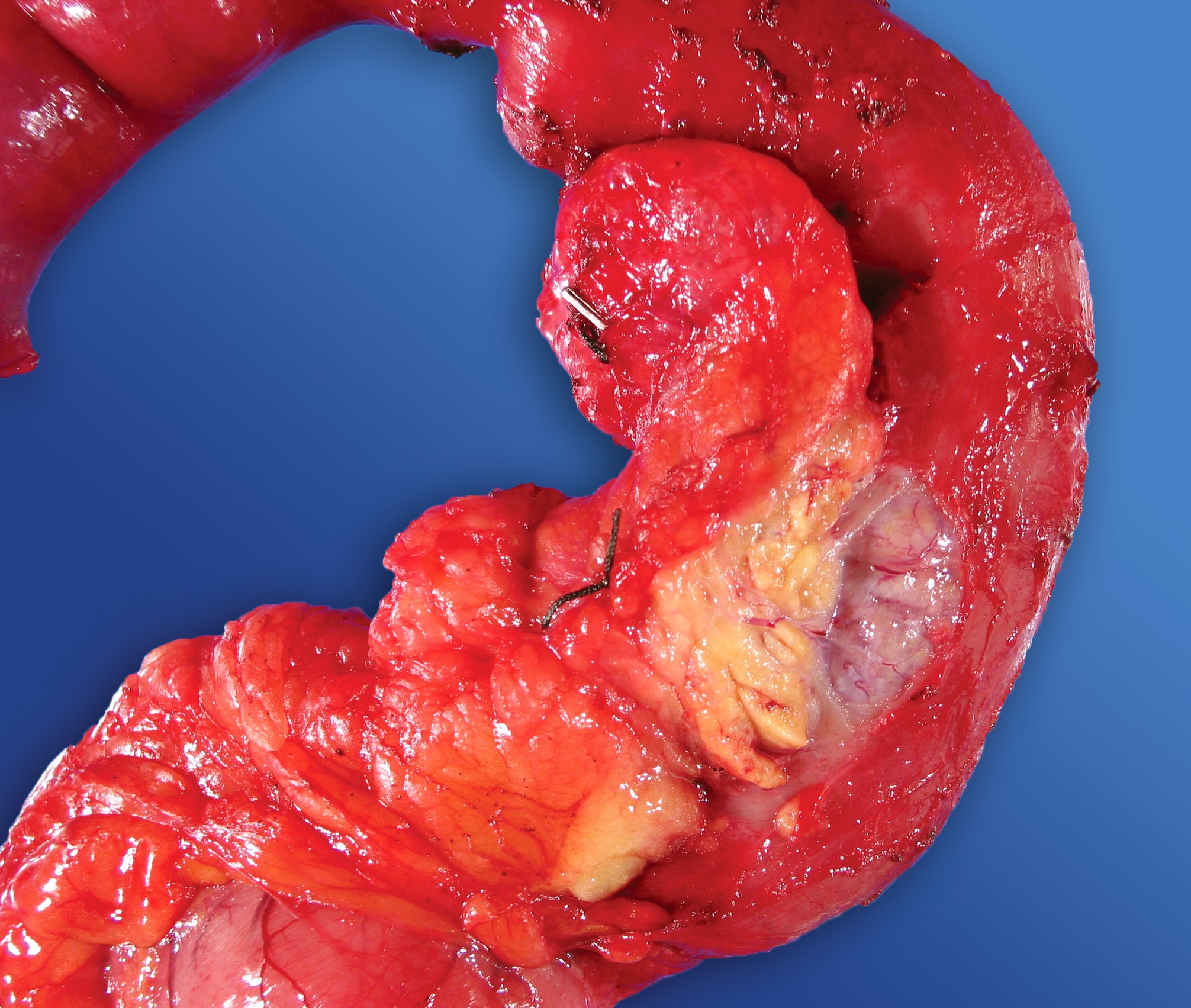
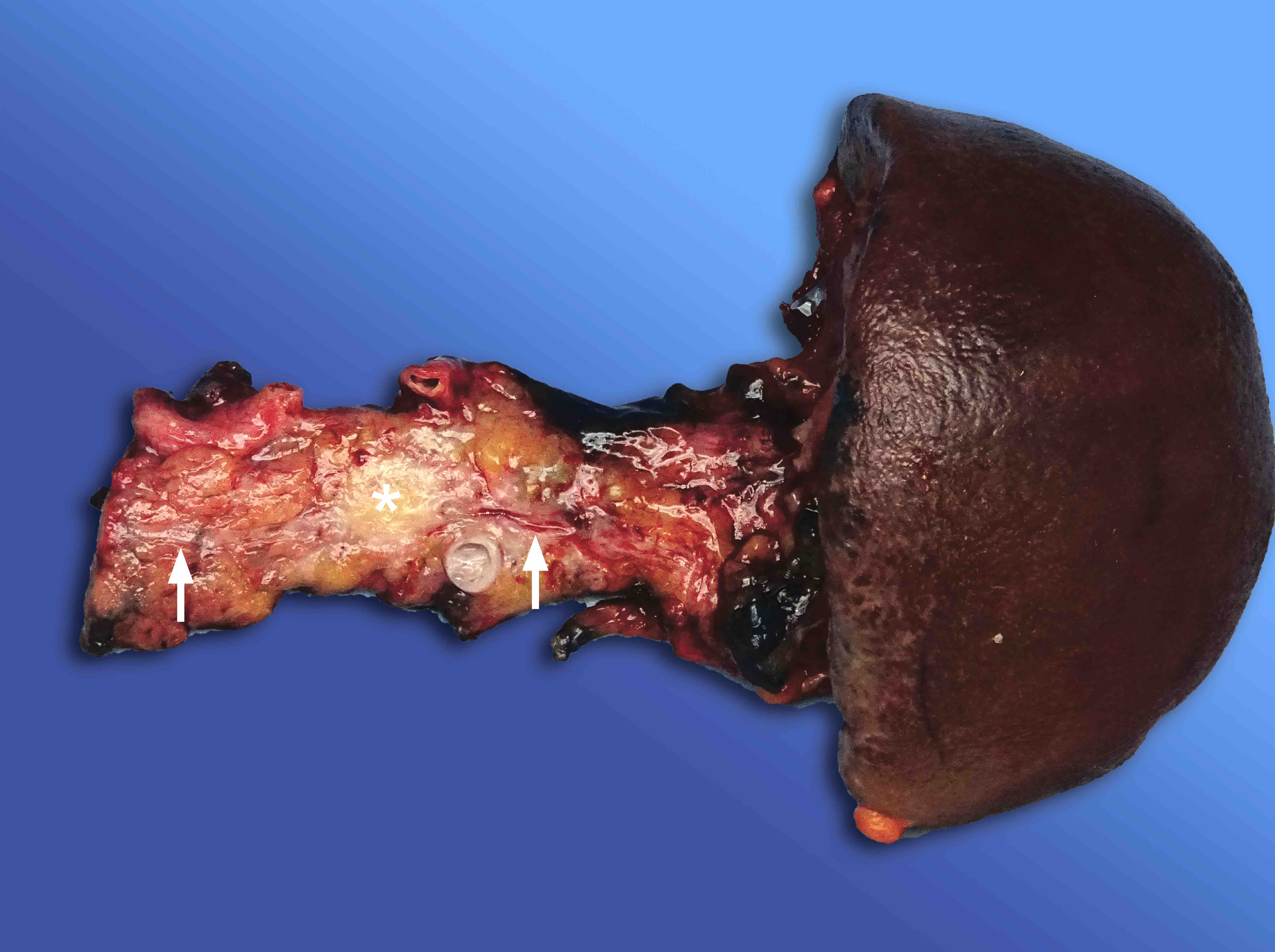
- Bivalving and sectioning
- Although there are several approaches in sectioning the pancreatic head, bivalving is the most commonly used method as it allows for assessment of the relation of tumor with both the CBD and PD and for proper evaluation and documentation of ampullary tumors (Am J Surg Pathol 2014;38:480)
- Bivalve the pancreatic head by placing the probes in the CBD and PD to the ampulla; probe the CBD all the way to the ampulla and the PD at least as far as it can be traced
- Start sectioning using a long knife (e.g., 6 inches)
- Knife needs to be angled as if cutting the probes themselves (see figure 9)
- Carefully examine and re-angle after each stroke (Am J Surg Pathol 2014;38:480)
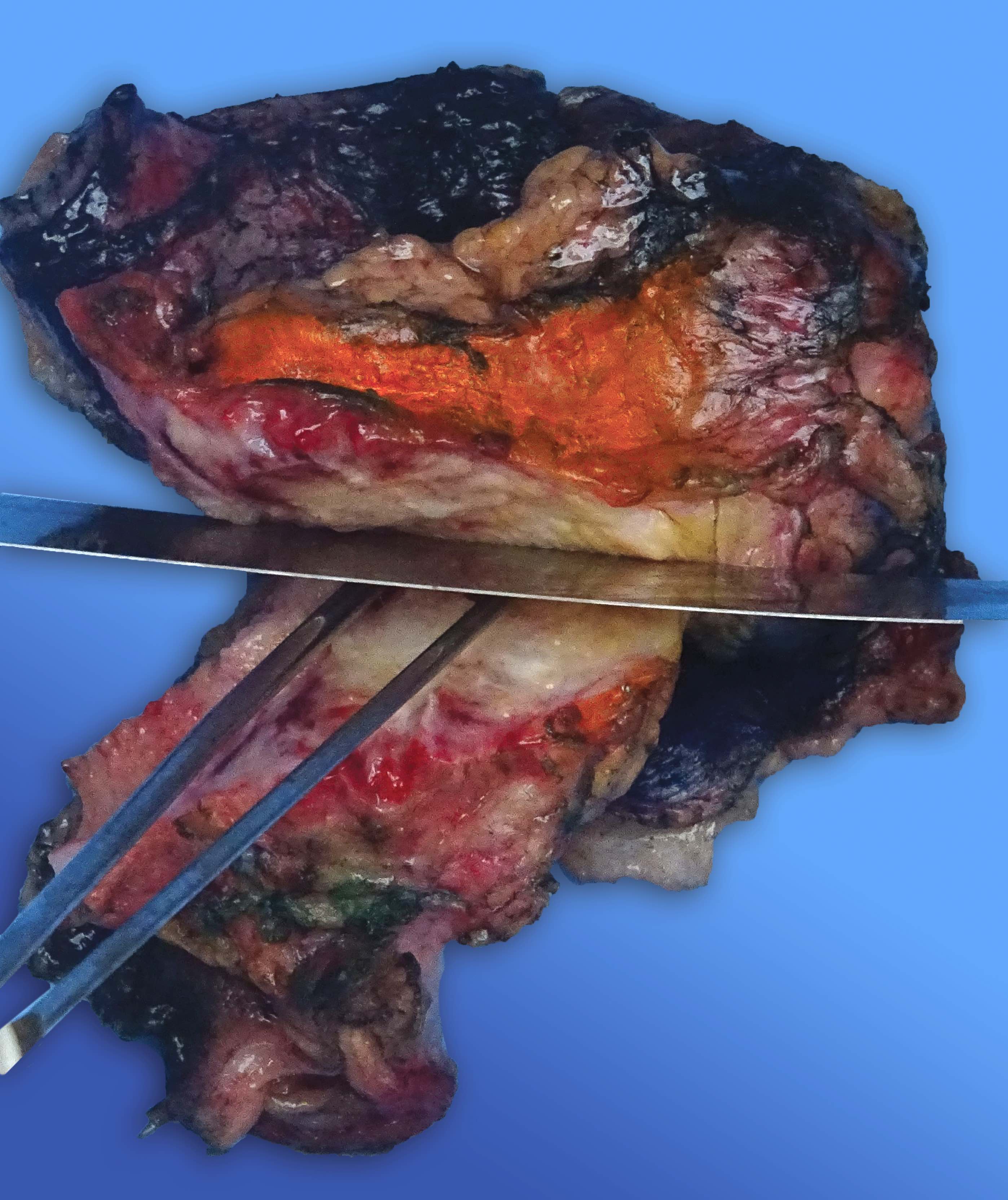
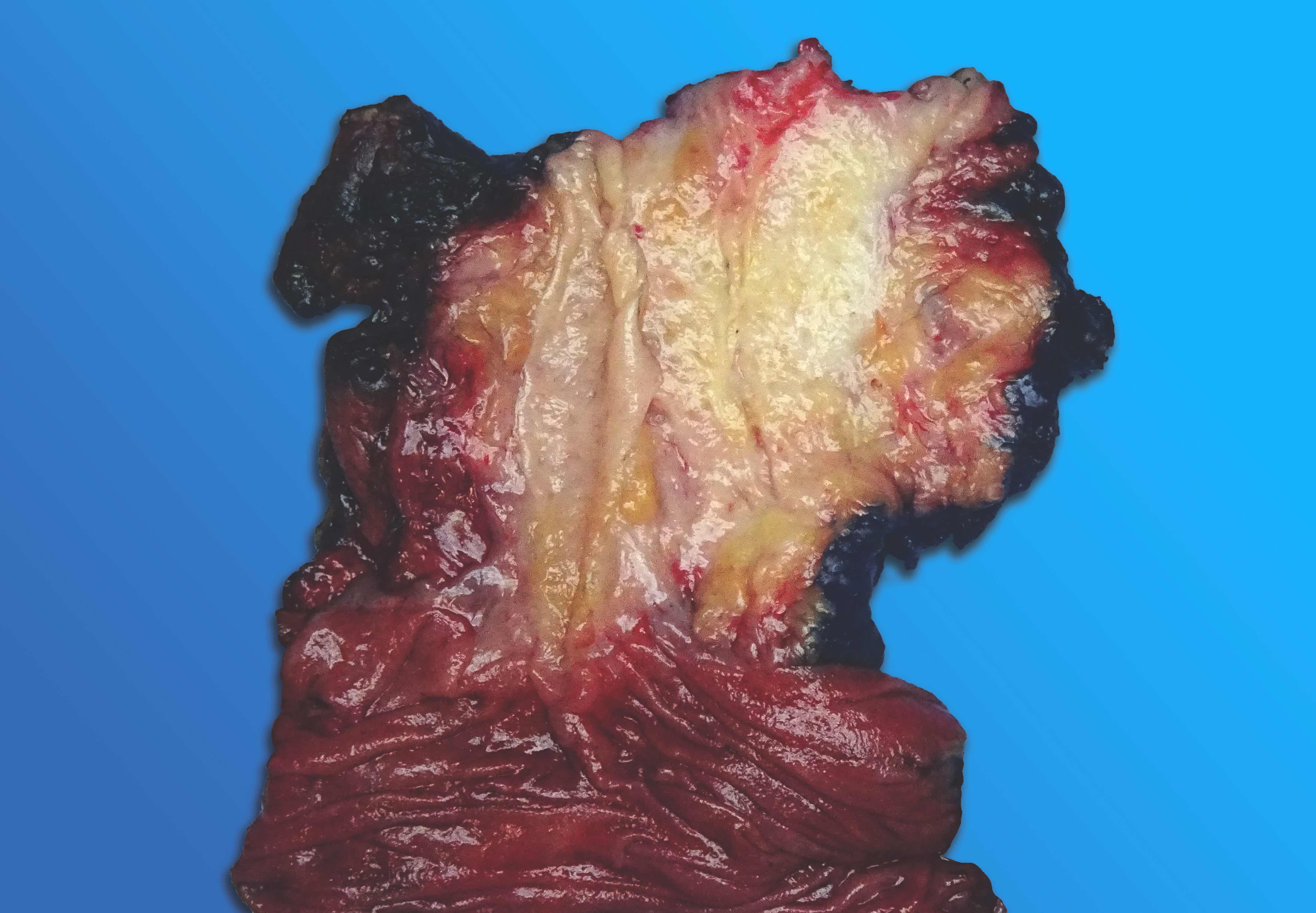
- Finally, the pancreatic head should be separated into anterior and posterior halves (see figure 10)
- Identifying the tumor(s)
- Inspect and describe the following features of the tumor(s): localization, size (measurements), characteristics (e.g., color, solid / cystic, necrotic / hemorrhagic / papillary areas, soft / firm, well circumscribed / ill defined), association with / distance from the CBD, PD, ampulla, margins and surfaces
- Harvest fresh tumor samples for the tumor bank as needed
- Identifying variant anatomies (i.e., low union)
- Normal (most common) insertion of the CD into the CHD is at least 5 mm above the pancreatic parenchyma border
- Other levels of insertion (i.e., within the 5 mm of pancreatic parenchyma border or even intrapancreatic) are considered as low union, which have been shown to play a significant role in pancreatobiliary and periampullary carcinogenesis (HPB (Oxford) 2020;22:1675)
- Therefore, when present, it should be documented (see figure 11)
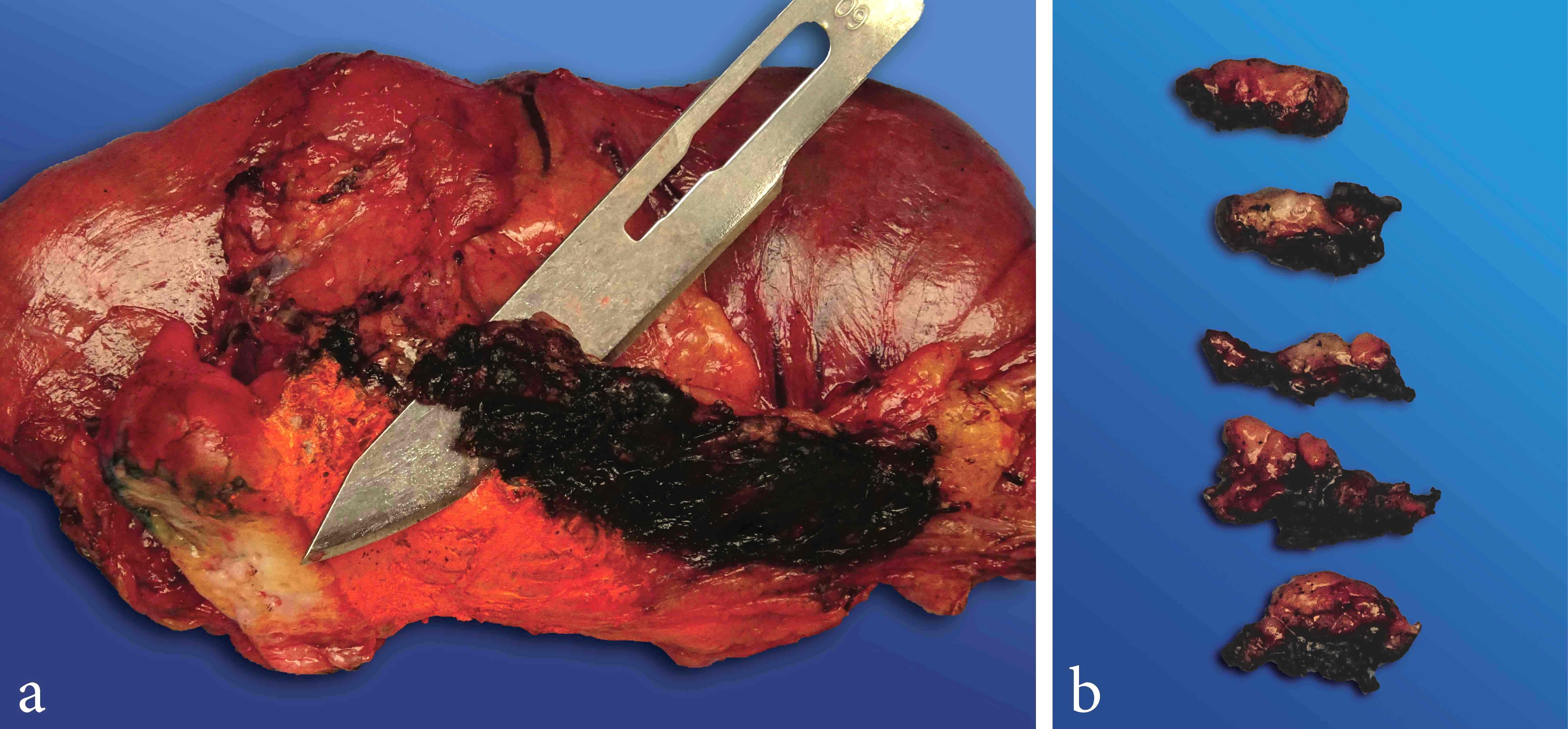
- Lymph node dissection
- Peripancreatic lymph nodes are separated into 8 regions as peri-CBD, anterior pancreatic, anterior pancreatoduodenal, superior pancreatic, inferior pancreatic, posterior pancreatic, posterior pancreatoduodenal and uncinate margin lymph nodes; however, these regions currently do not play any role in pN staging
- Shave off all peripancreatic soft tissues using the orange peeling method (see figures 12 and 13) including the priorly inked anterior and posterior free surfaces (Am J Surg Pathol 2014;38:480, Mod Pathol 2009;22:107)
- Submit entirely in subsequent cassettes
- Make a note of sectioned lymph nodes to prevent overcounting
- Dissect and submit perigastric and periduodenal lymph nodes using conventional methods
- Fixation and harvesting
- Let the specimen be properly fixed in formalin for 24 - 48 hours
- After fixation, submit at least 1 section per centimeter of the tumor for solid tumors
- Increase the number of the sections or even submit it entirely if the tumor was treated (Am J Surg Pathol 2022;46:754)
- Unless there is a grossly visible invasion, cystic / intraductal tumors should be submitted entirely to rule out invasion (Ann Surg 2016;263:162)
- Include proper sections to show any association between the tumor and important structures (i.e., ampulla, CBD, PD, vascular bed, duodenum, etc.)
- Include nontumoral tissue sections from the pancreas and the adjacent organs
- Taking gross images
- Always take several images of the specimen in both fresh (before and after inking, bivalving and sectioning) and fixed states
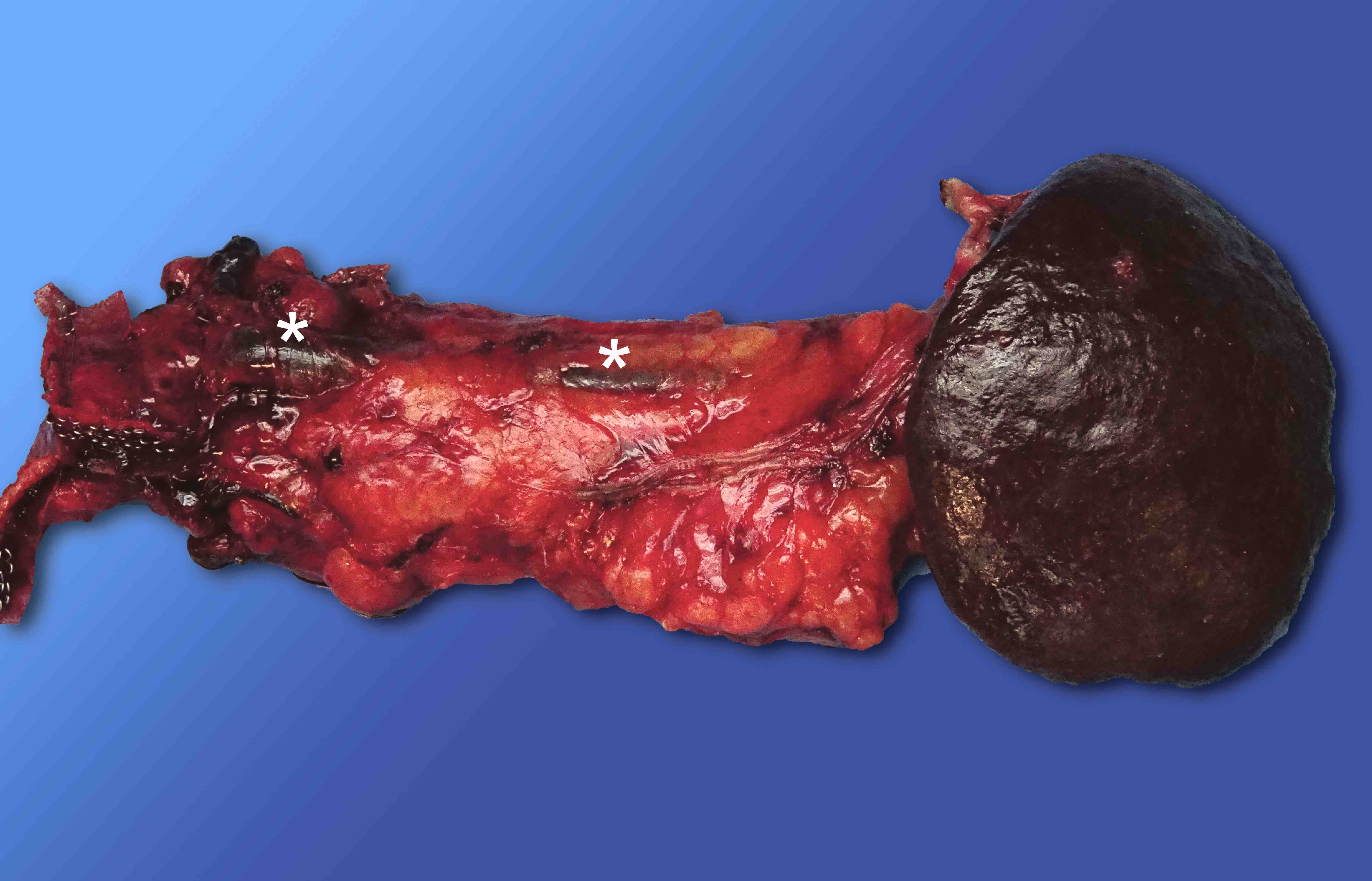
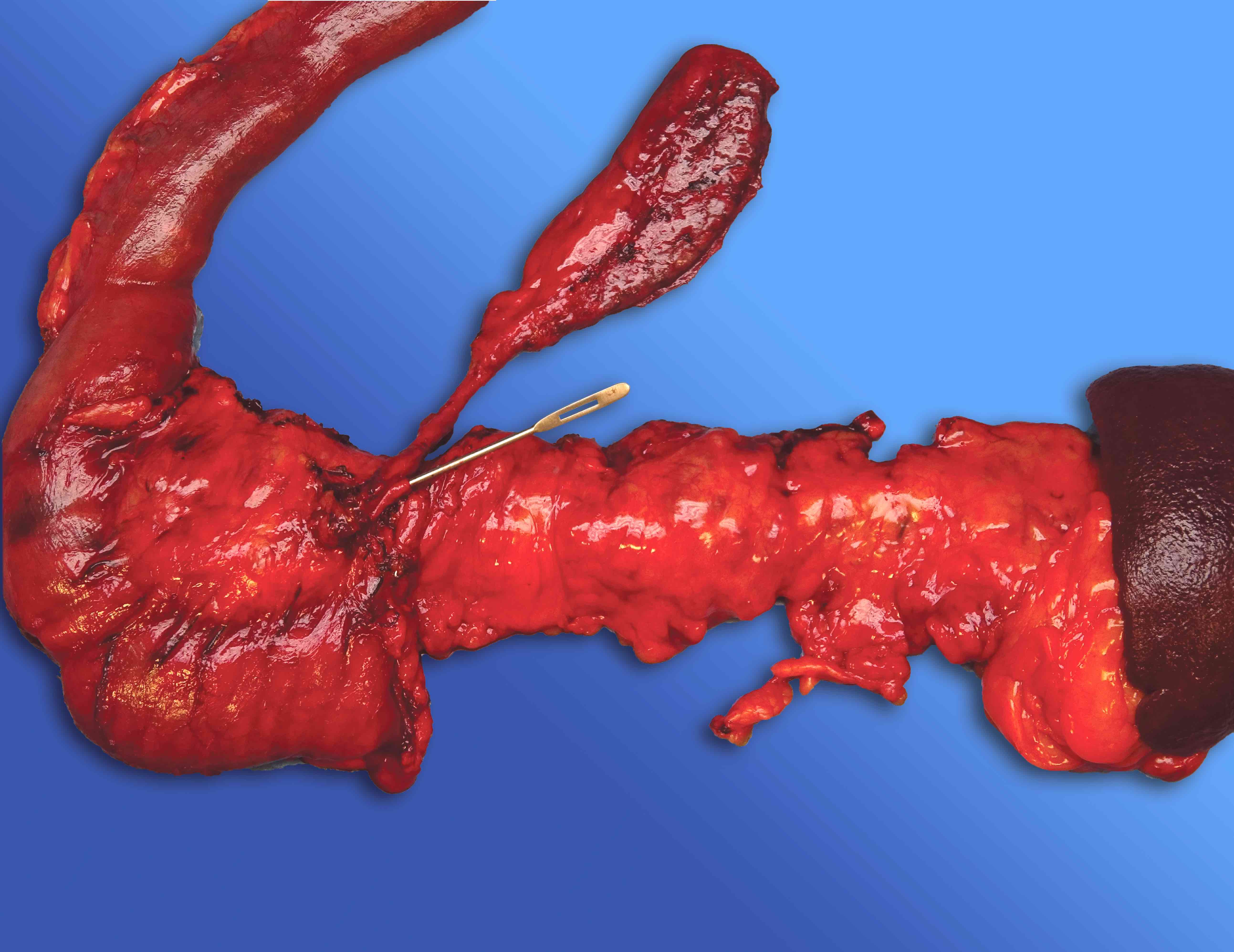
Distal pancreatectomy specimens:
- Orientation, external examination and removing the margin
- Specimen consists of body and tail of the pancreas with or without spleen attached
- Freshly examine the specimen
- Measure the overall specimen and each organ / structure
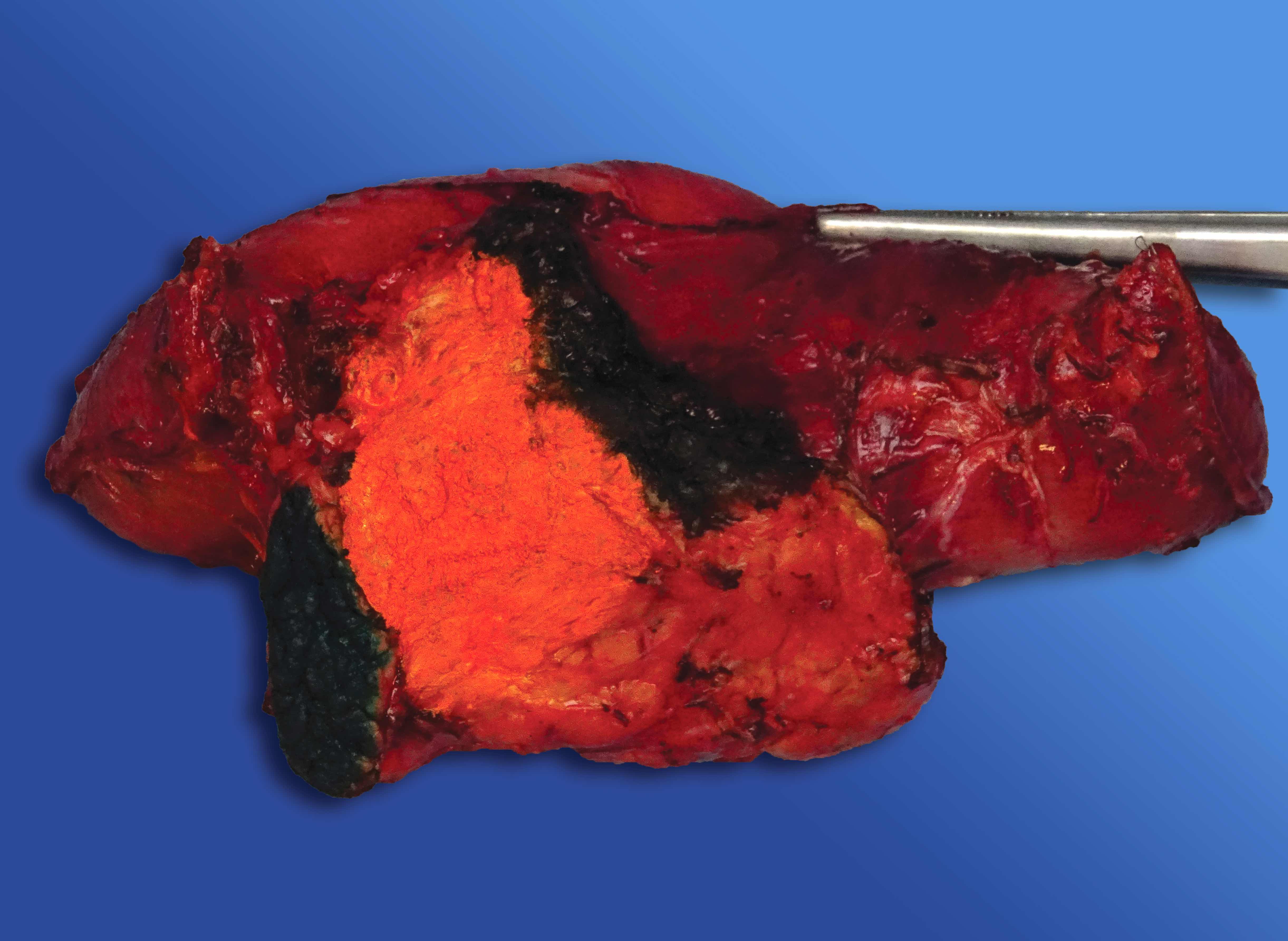
- Identify splenic artery on the superior and splenic vein on the posterior surface of the pancreas (see figures 14 and 15)
- Ink anterior and posterior surfaces in different colors (e.g., blue for anterior, black for posterior)
- Identify, ink and remove the pancreatic parenchymal (duct) margin; shave and submit enface
- Sectioning
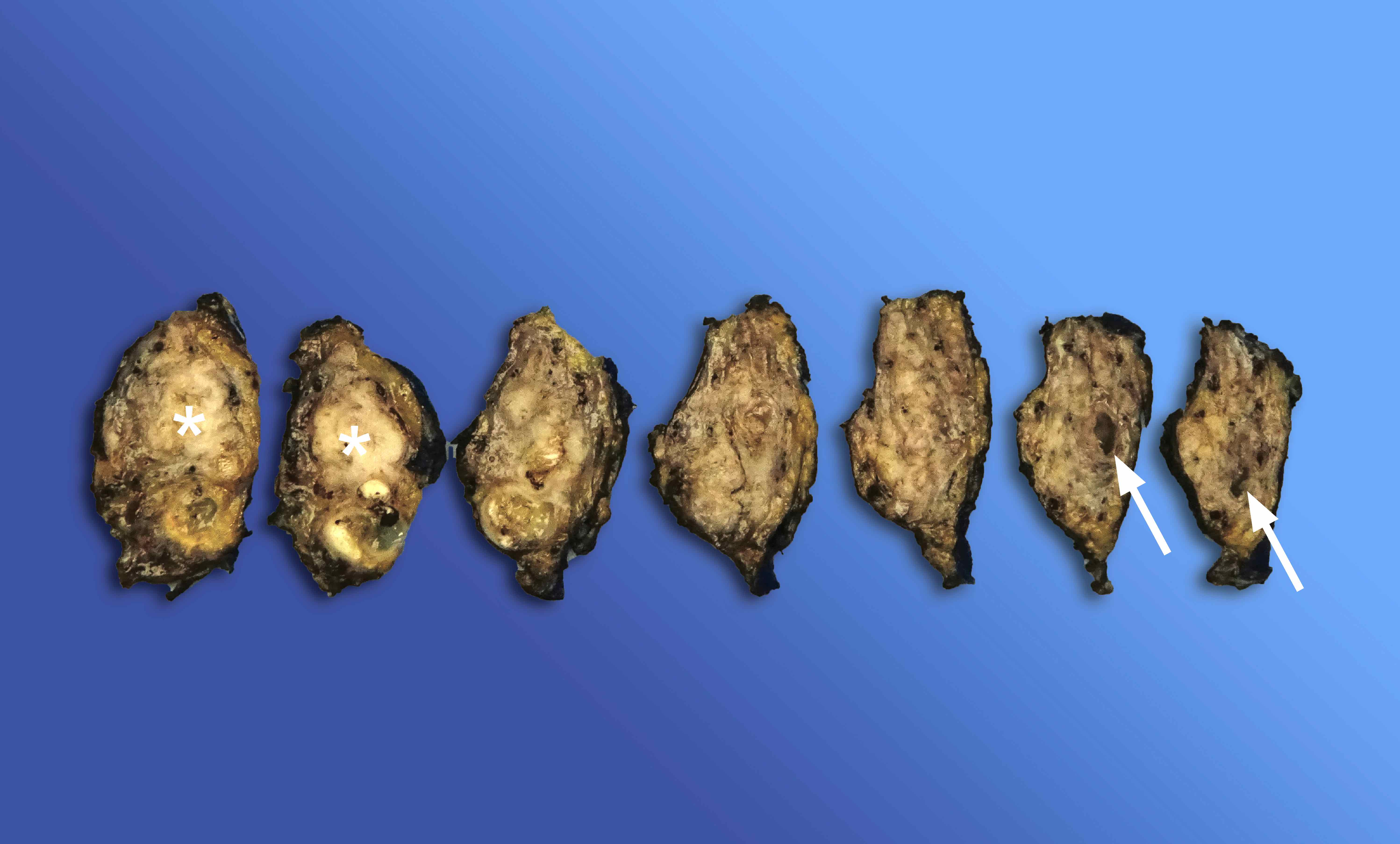
- One approach is serial sectioning of the entire pancreas and spleen at 0.5 - 1 cm intervals starting from the proximal edge of the pancreas (see figure 16)
- Alternatively, entire pancreas and spleen can be bivalved and sectioned with the guidance of a probe placed in the PD, starting from the proximal edge of the pancreas (see figure 17)
- Then, perpendicular (to the surfaces) sections are submitted from each half
- Identifying the tumor(s)
- Inspect and describe the following features of the tumor(s): localization, size (measurements), characteristics (e.g., color, solid / cystic, necrotic / hemorrhagic / papillary areas, soft / firm, well circumscribed / ill defined), association with / distance from the PD, pancreatic parenchymal margin, anterior and posterior surfaces and spleen
- Harvest fresh tumor samples for the tumor bank as needed
- Lymph node dissection
- Dissect the peripancreatic and splenic hilar lymph nodes using conventional methods
- Fixation and harvesting
- Let the specimen be properly fixed in formalin for 24 - 48 hours
- After fixation, submit at least 1 section per centimeter of the tumor for solid tumors
- Increase the number of the sections or even submit it entirely if the tumor was treated (Am J Surg Pathol 2022;46:754)
- Unless there is a grossly visible invasion, cystic / intraductal tumors should be submitted entirely to rule out invasion (Ann Surg 2016;263:162)
- Include proper sections to show any association between the tumor and important structures (i.e., PD, spleen, splenic hilum, etc.)
- Include nontumoral tissue sections from the pancreas and the spleen
- Taking gross images
- Always take several images of the specimen in both fresh (before and after inking, bivalving and sectioning) and fixed states
Total pancreatectomy specimens:
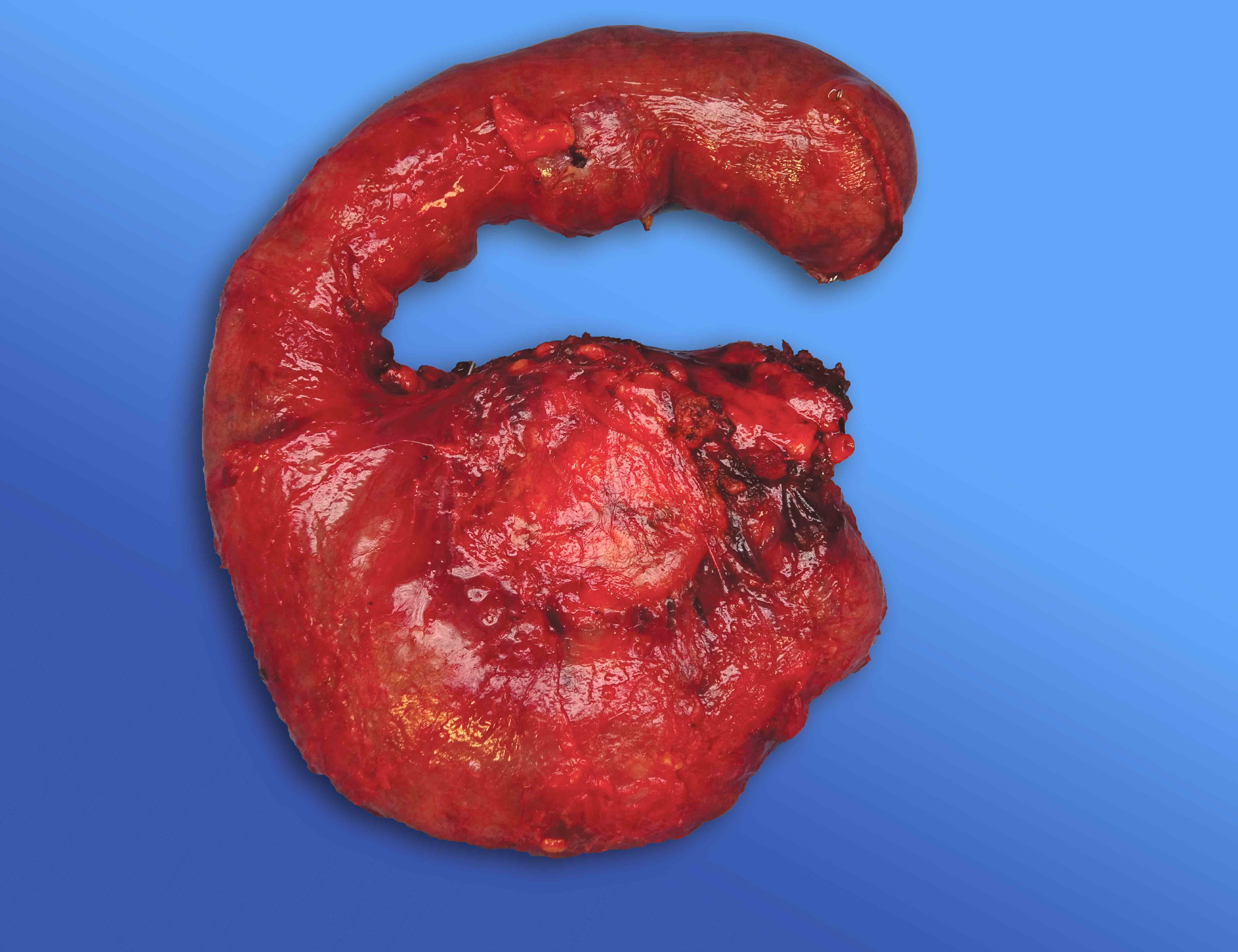
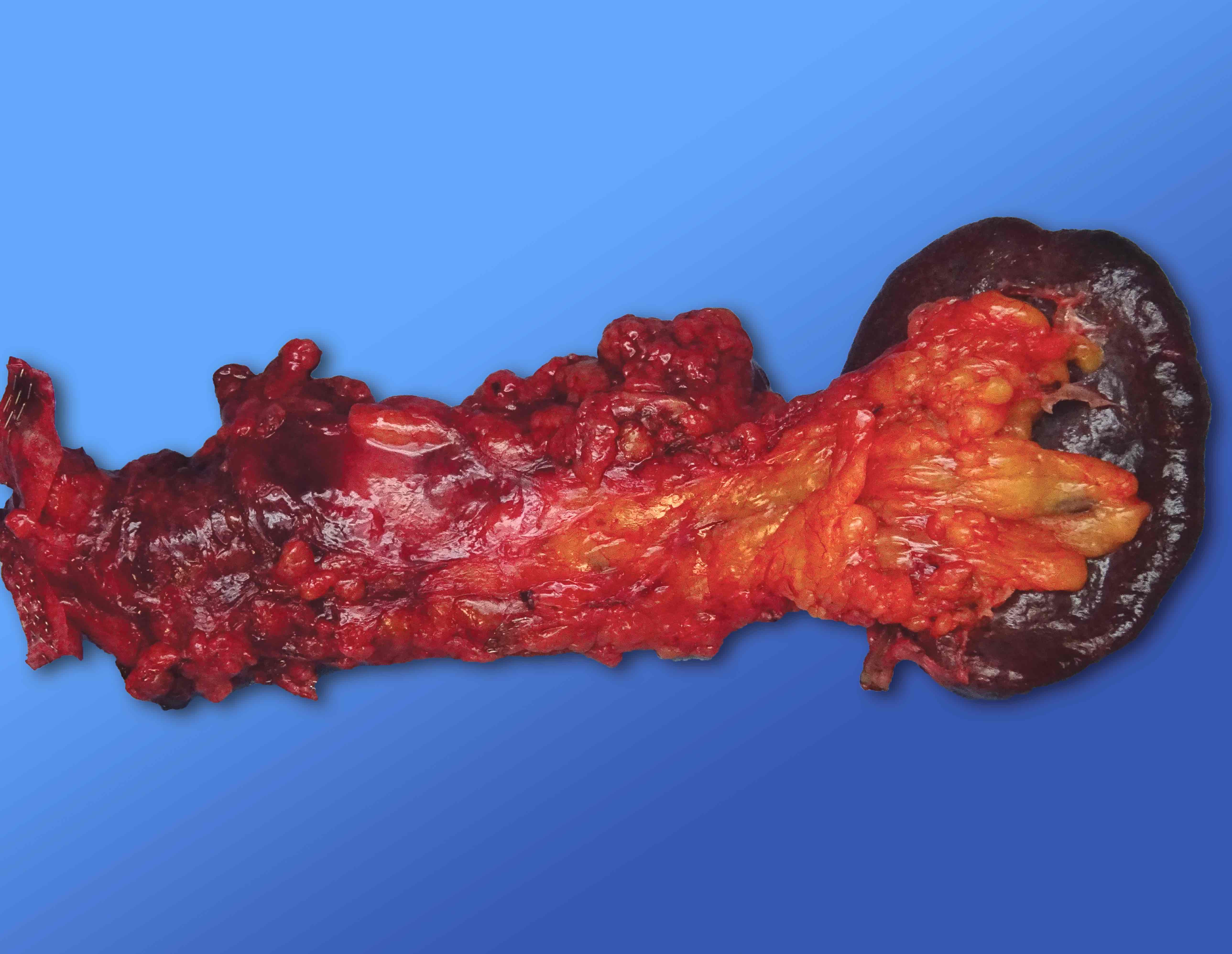
- Specimen consists of pancreatic head, neck, body and tail, in addition to duodenum, spleen and occasionally distal stomach and gallbladder (see figure 18)
- Follow the steps for pancreaticoduodenectomy and distal pancreatectomy for the appropriate portions of the specimen (see above)
Sections to obtain
- Tumor:
- Submit representative tumor sections for a total of 1 cassette per 1 cm of the largest tumor dimension; increase the number as needed (e.g., if the tumor is cystic / intraductal, if the patient had neoadjuvant therapy, etc.) (Am J Surg Pathol 2022;46:754, Ann Surg 2016;263:162)
- Include proper sections to show any association between the tumor and adjacent structures
- Margins: submit the proper margins for pancreaticoduodenectomy, distal pancreatectomy and total pancreatomy specimens as described above
- Lymph nodes: submit all dissected lymph nodes (and the entire peripancreatic soft tissue for pancreaticoduodenectomy specimens) properly (Am J Surg Pathol 2014;38:480)
- Nontumoral adjacent organs: submit uninvolved tissue sections from the pancreas and adjacent organs in 1 cassette for each organ
Tips
- Distinguishing CBD and PD:
- Probing the PD:
- If the PD orifice is not easily identified in the pancreatic neck margin, squishing the pancreatic head and looking for the pancreatic fluid coming from the PD might be useful
- However it needs to be done carefully, as the pancreatic fluid can only be seen in the first few attempts
- In some cases, probing of the PD is problematic, especially in the distal part, because of its narrow and kinked nature in contrast to the CBD which is always probe-patent
- One option is retroprobing the PD from the ampulla
- If it does not work, another option is to probe the PD as far as it can be traced and past that point using the guidance of the CBD alone
- If the PD orifice is not easily identified in the pancreatic neck margin, squishing the pancreatic head and looking for the pancreatic fluid coming from the PD might be useful
- Cystic tumors:
- Examine the nature of cystic fluid (e.g., mucinous, clear, hemorrhagic, etc.)
- Assess the association of the cyst with main / branch pancreatic ducts
- Pay attention to the solid / granular / papillary / nodular areas of the cyst, if any, since they have value in evaluating the invasion
- Ampullary tumors:
- Ampullary carcinoma is defined by the bulk of the tumor (> 75%) being located in the ampulla
- Classification of ampullary carcinomas (i.e., intra-ampullary, ampullary ductal, periampullary duodenal and ampullary, NOS) depends on a proper gross examination (Am J Surg Pathol 2012;36:1592)
- Sections should be taken perpendicularly to make measurement of the invasion depth possible; they should also include the ampulla, pancreas, periampullary duodenum and periampullary soft tissues
- Nonampullary duodenal tumors:
- By definition, the epicenter of a nonampullary duodenal carcinoma is entirely located in the duodenum and the ampulla is uninvolved
- Distal CBD tumors:
- Distal CBD carcinoma is defined by whether the bulk of the tumor is located circumferentially around the CBD or if an associated precursor intraductal neoplasm is identified in the CBD (Mod Pathol 2016;29:1358, J Gastrointest Surg 2016;20:953)
- Taking gross images of the specimen in both fresh and fixed states is helpful for microscopic examination and reporting
Gross description
- Pancreatic ductal adenocarcinoma (PDAC):
- Ill defined solid mass with irregular / infiltrating borders, gray-white-tan greenish in color, firm and scirrhous in consistency (Am J Surg Pathol 2014;38:480)
- Necrosis or cystic degeneration may be present
- Pancreatic neuroendocrine carcinoma (NEC):
- Ill defined or vaguely nodular solid mass with relatively irregular / infiltrating borders, tan-white-brown-red or yellowish in color, usually fleshier than PDAC
- Necrosis and hemorrhage are often easily identified (Am J Surg Pathol 2014;38:437)
- Pancreatic neuroendocrine tumor (PanNET):
- Well circumscribed solid mass with pushing borders, gray-tan pinkish in color, soft and fleshy in consistency (Endocr Pathol 2014;25:65)
- Cystic degeneration or accompanying fibrosis, calcification and ossification may be present
- Acinar cell carcinoma (ACC):
- Well circumscribed and sometimes encapsulated, solid, bulky mass, gray-tan pinkish reddish in color, fleshy in consistency (Semin Diagn Pathol 2016;33:307)
- Solid pseudopapillary tumor (SPN):
- Well circumscribed and encapsulated mass, which reveals solid and cystic areas, tan-brown pinkish in color, fleshy and friable in consistency
- Hemorrhage and necrosis are observed in most cases (Arch Pathol Lab Med 2009;133:423)
- Intraductal papillary mucinous neoplasm (IPMN):
- Cystic mass in the main or branch pancreatic ducts, may reveal mucin or papillary structures (Am J Surg Pathol 2014;38:480, Semin Diagn Pathol 2014;31:452)
- Intraductal oncocytic papillary neoplasm (IOPN):
- Multilocular or unilocular cystic mass in the main pancreatic duct with friable papillary / nodular projections (Mod Pathol 2016;29:1058, Am J Surg Pathol 2019;43:656)
- Intraductal tubulopapillary neoplasm (ITPN):
- Multinodular / polypoid / solid mass in the main pancreatic duct, without a very distinct cyst formation and papillary projections (Semin Diagn Pathol 2014;31:452, Mod Pathol 2017;30:1760)
- Mucinous cystic neoplasm (MCN):
- Well circumscribed and large cystic mass without any association with ductal system, may reveal papillary / trabecular / nodular / solid areas (Arch Pathol Lab Med 2009;133:423, J Gastrointest Surg 2008;12:401)
- Serous cystadenoma (SCA):
- Well circumscribed and multicystic (sponge-like) tumor, usually with a central scar and without any association with ductal system (Am J Surg Pathol 2015;39:1597, Semin Diagn Pathol 2014;31:475)
- Rare cases may reveal oligocystic or even solid appearance
Gross template samples
- Pancreaticoduodenectomy (Whipple) specimens:
- The specimen is received (fresh), labeled as pancreatoduodenectomy and consists of pancreatic head, duodenum and (other organs). The pancreas measures ( ) x ( ) x ( ) cm, the duodenum measures ( ) cm in length and ( ) cm in circumference, (other organs) measures ( ) cm. External surface of the pancreas is ( ). The pancreatic neck / duct margin is inked (green), the bile duct margin is inked (red), the uncinate margin is inked (black), the vascular groove is inked (orange), posterior surface of the pancreas is inked (black) and anterior surface of the pancreas is inked (blue). The bile duct and pancreatic neck / duct margins are shaved and submitted enface. The uncinate margin is shaved, serially sectioned and entirely submitted.
- Proximal and distal margins of the duodenum are submitted. Duodenum is opened through the antipancreatic border. Ampulla reveals ( ). The bile duct and pancreatic duct are probed.
- Bivalving of the pancreas reveals that the pancreatic duct is ( ) cm in length with a luminal circumference of ( ) cm, the bile duct is ( ) cm in length with a luminal circumference of ( ) cm. Cystic duct is present / absent in the specimen. If cystic duct is present, it is ( ) cm in length, with a luminal circumference of ( ) cm and it adjoins the common hepatic duct at ( ). There is a ( ) x ( ) x ( ) cm solid / cystic mass, ( ) in color, with a firm / soft / fleshy cut surface, ill defined / well circumscribed borders, located at the ( ). The tumor is in association with ( ). ( ) are involved by the tumor. The tumor is in ( ) cm distance from the ( ). Representative sections of the tumor submitted. Ampulla is submitted. Entire peripancreatic soft tissues and dissected periduodenal lymph nodes are submitted. The remaining pancreatic cut surface reveals ( ) / unremarkable. The remaining duodenal mucosal surface reveals ( ) / unremarkable. Other organs on the specimen reveal ( ) / unremarkable. Representative sections of the remaining pancreas and adjacent organs are submitted.
- Distal pancreatectomy specimens:
- The specimen is received (fresh), labeled as distal pancreatectomy and splenectomy, and consists of distal pancreas and spleen. The distal pancreas measures ( ) x ( ) x ( ) cm. Spleen is () gr and measures ( ) x ( ) x ( ) cm. The pancreatic parenchymal margin is shaved and submitted enface. The anterior surface of the pancreas is inked (blue) and the posterior surface is inked (black). Serially sectioning (or bivalving) of the specimen reveals a ( ) x ( ) x ( ) cm solid / cystic mass, ( ) in color, with a firm / soft / fleshy cut surface, ill defined / well circumscribed borders, located at the ( ). The tumor is in association with ( ). ( ) are involved by the tumor. The tumor is in ( ) cm distance from the ( ). Representative sections of the tumor submitted. Peripancreatic and perihilar lymph nodes are dissected and submitted. The remaining pancreatic cut surface reveals ( ) / unremarkable. Sections of the spleen reveal ( ) / unremarkable. Representative sections of the remaining pancreas and spleen are submitted.
- Total pancreatectomy specimens:
- See the gross template samples for pancreaticoduodenectomy and distal pancreatectomy specimens
Additional references
Board review style question #1
Gross examination of a pancreaticoduodenectomy (Whipple) specimen reveals a white-tan colored, firm, solid mass with ill defined borders, located in the pancreatic head. Which of the following would be included in the initial differential diagnosis?
- Acinar cell carcinoma
- Pancreatic ductal adenocarcinoma
- Solid pseudopapillary tumor
- Well differentiated pancreatic neuroendocrine tumor, grade 1
- Well differentiated pancreatic neuroendocrine tumor, grade 3
Board review style answer #1