Table of Contents
Definition / general | Essential features | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Case reports | Treatment | Peripheral smear description | Peripheral smear images | Molecular / cytogenetics description | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Wheeler E, Putnam NE. Babesia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/parasitologybabesia.html. Accessed April 24th, 2024.
Definition / general
- Babesia spp. are protozoan parasites that infect red blood cells
- Taxonomy:
- Phylum: Apicomplexa
- Order: Piroplasmida
- Family: Babesiidae
Essential features
- Babesiosis is caused by Babesia spp., transmitted via tick bites (most commonly, Ixodes) (Pathogens 2021;10:1447)
- Infection of erythrocytes leads to hemolytic anemia and cytokine production causing fever, jaundice, hepatosplenomegaly and, in severe cases, multiorgan failure (Pathogens 2022;11:399)
- Diagnosis is made upon seeing multiple infected red cells with extracellular ring forms on blood smear
- Classical blood smear finding is a tetrad of intracellular ring forms (Maltese cross) with extracellular ring forms
- Mild infections resolve spontaneously
- Moderate and severe manifestations may require treatment (moderate: atovaquone and azithromycin; severe: clindamycin, quinine, exchange transfusion)
Epidemiology
- More than 70 species exist worldwide but most cases of babesiosis in the United States are due to B. microti
- In Europe, B. divergens is associated with more serious clinical syndrome (Pathogens 2021;10:1165)
- In the Northeastern U.S., Ixodes scapularis, commonly known as deer tick or black legged tick, is the main species of tick that transmits B. microti (Pathogens 2021;10:1447)
- Splenectomy, HIV infection, immunosuppression and advanced age increase the likelihood of severe infection (Pathogens 2022;11:399)
- Humans are incidental hosts; natural hosts include small rodents (voles, field mice, etc.) (Pathogens 2021;10:1447)
- Other modes of transmission include transfusion, organ transplantation and transplacental (Pathogens 2022;11:399)
- Co-infection with Anaplasma and Borrelia can occur, as both diseases are vectored by Ixodes scapularis (Pathogens 2021;10:1447)
Sites
- Parasite found in the blood
Pathophysiology
- Babesia parasites are maintained in animal tick cycles, where ticks have transovarian and stage to stage transmission (Trop Parasitol 2015;5:94)
- Cycle of human infection (Pathogens 2021;10:1447):
- A Babesia infected tick will inject sporozoites via saliva into the bloodstream in the form of pyriform bodies
- Trophozoites infect erythrocytes and asexually reproduce via binary fission
- Erythrocyte lysis releases merozoites that infect other erythrocytes or are taken up by feeding ticks
- Lysis of red cells leads to a cascade of inflammatory responses resulting in fever, malaise with more severe disease (i.e., disseminated intravascular coagulation [DIC], renal failure, shock) in patients with splenectomy, immunosuppression and advanced age (Pathogens 2022;11:399)
Clinical features
- Symptoms include fever without periodicity, malaise, headache, chills, fatigue, weakness
- Signs include hemolytic anemia, hepatosplenomegaly
Diagnosis
- Diagnosis is made on thick and thin blood smear with Giemsa stain (gold standard)
- When parasitemia is low and in cases of screening (particularly for blood products), serological assays and antigen capture assays can be performed (Pathogens 2022;11:399)
- During acute disease, polymerase chain reaction (PCR) may be used for diagnosis in the form of organism specific Babesia spp. PCR or as part of larger tick borne disease PCR panels that include anaplasmosis, ehrlichiosis and babesiosis
Case reports
- 37 year old man in Singapore who acquired Babesia microti infection in the U.S. (Emerg Infect Dis 2020;26:826)
- 66 year old man in the South Bronx presenting with febrile illness (Clin Pract Cases Emerg Med 2018;2:61)
- 70 year old woman presenting with asplenic sepsis (Turk J Haematol 2019;36:284)
- 81 year old man from upstate New York with fevers, malaise, vague abdominal pain and confusion (Proc (Bayl Univ Med Cent) 2020;34:97)
Treatment
- Mild: resolves spontaneously
- Moderate: combination atovaquone and azithromycin
- Severe: can be treated with clindamycin, quinine, sometimes exchange transfusion
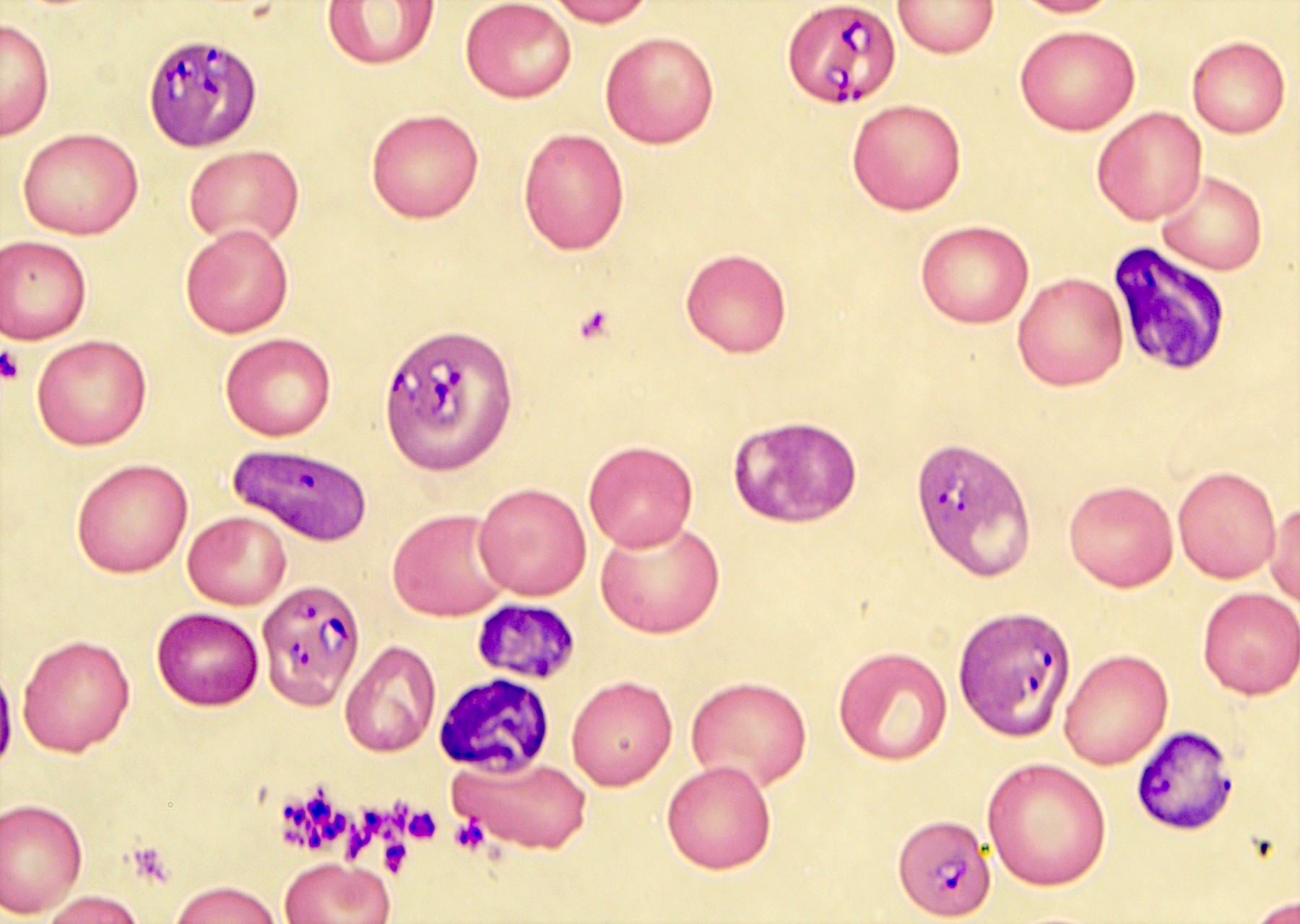
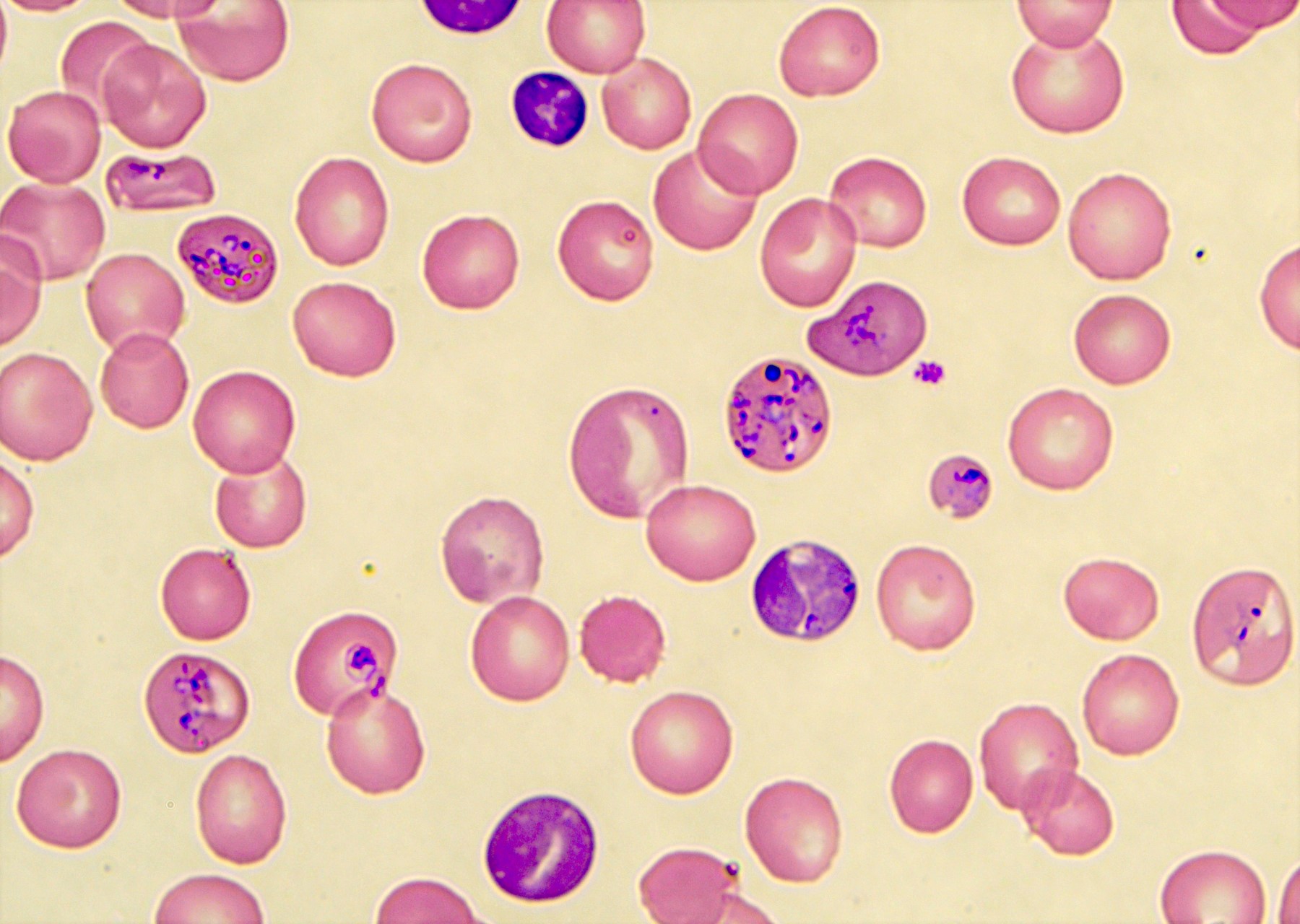
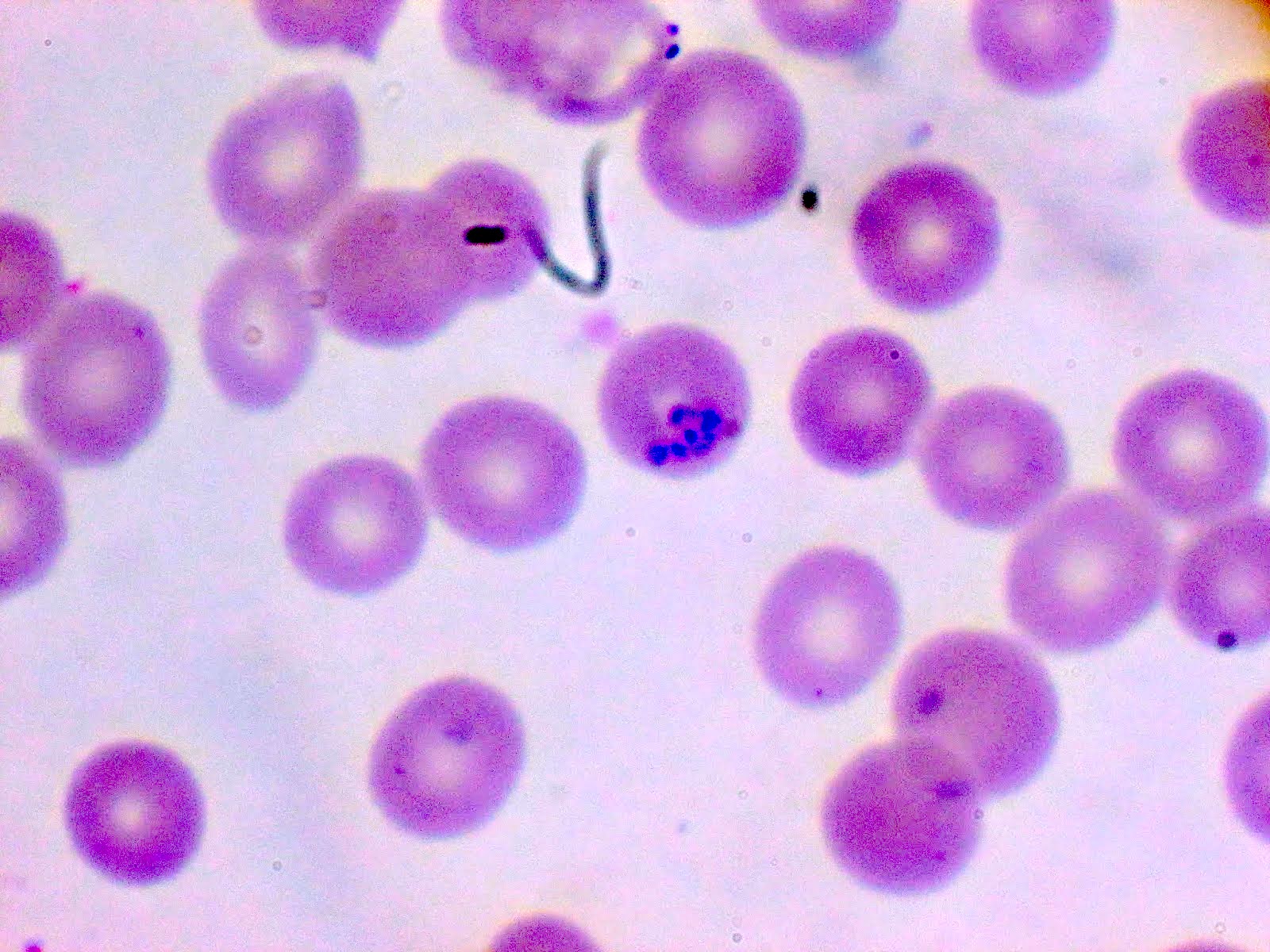
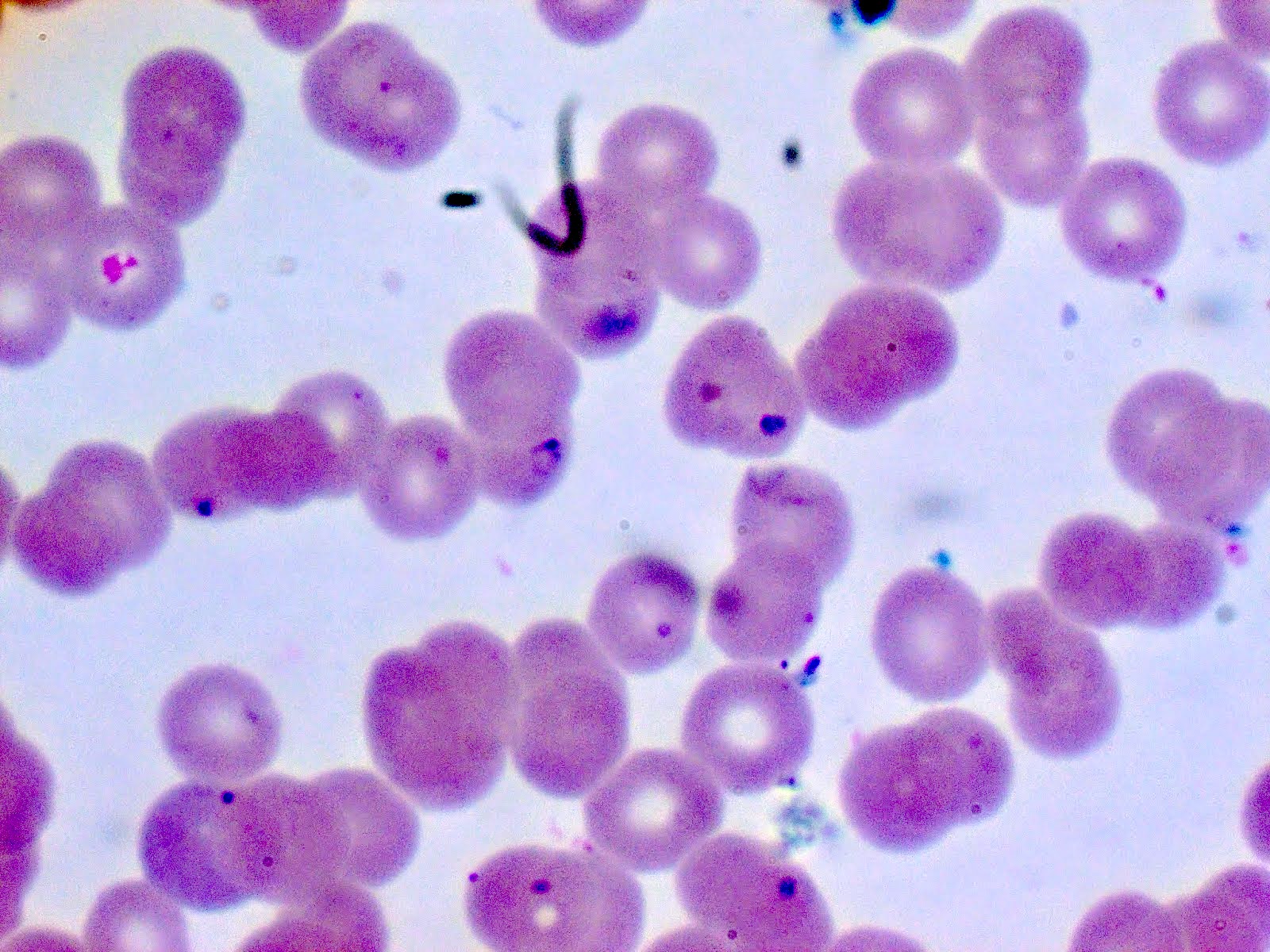
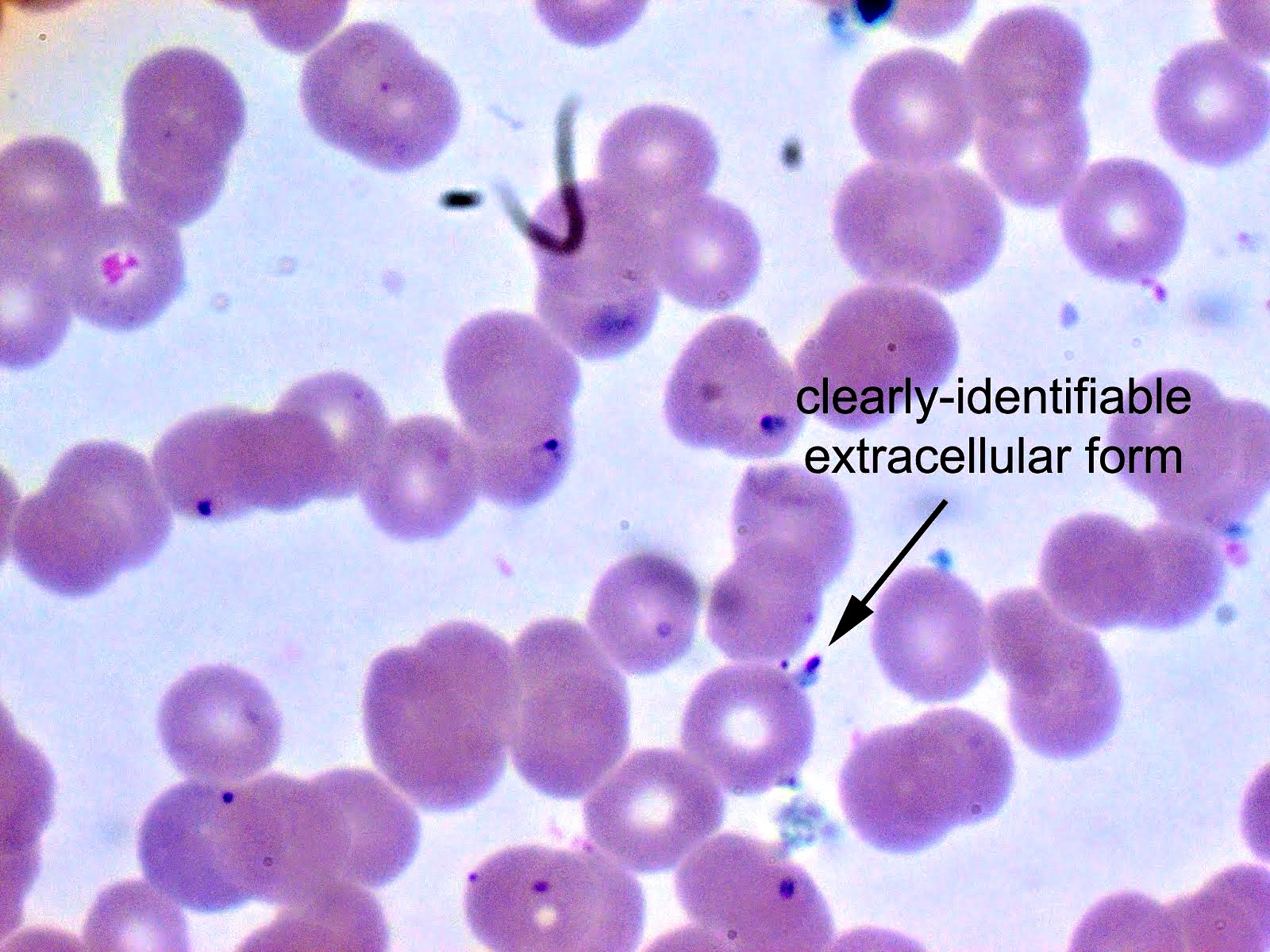
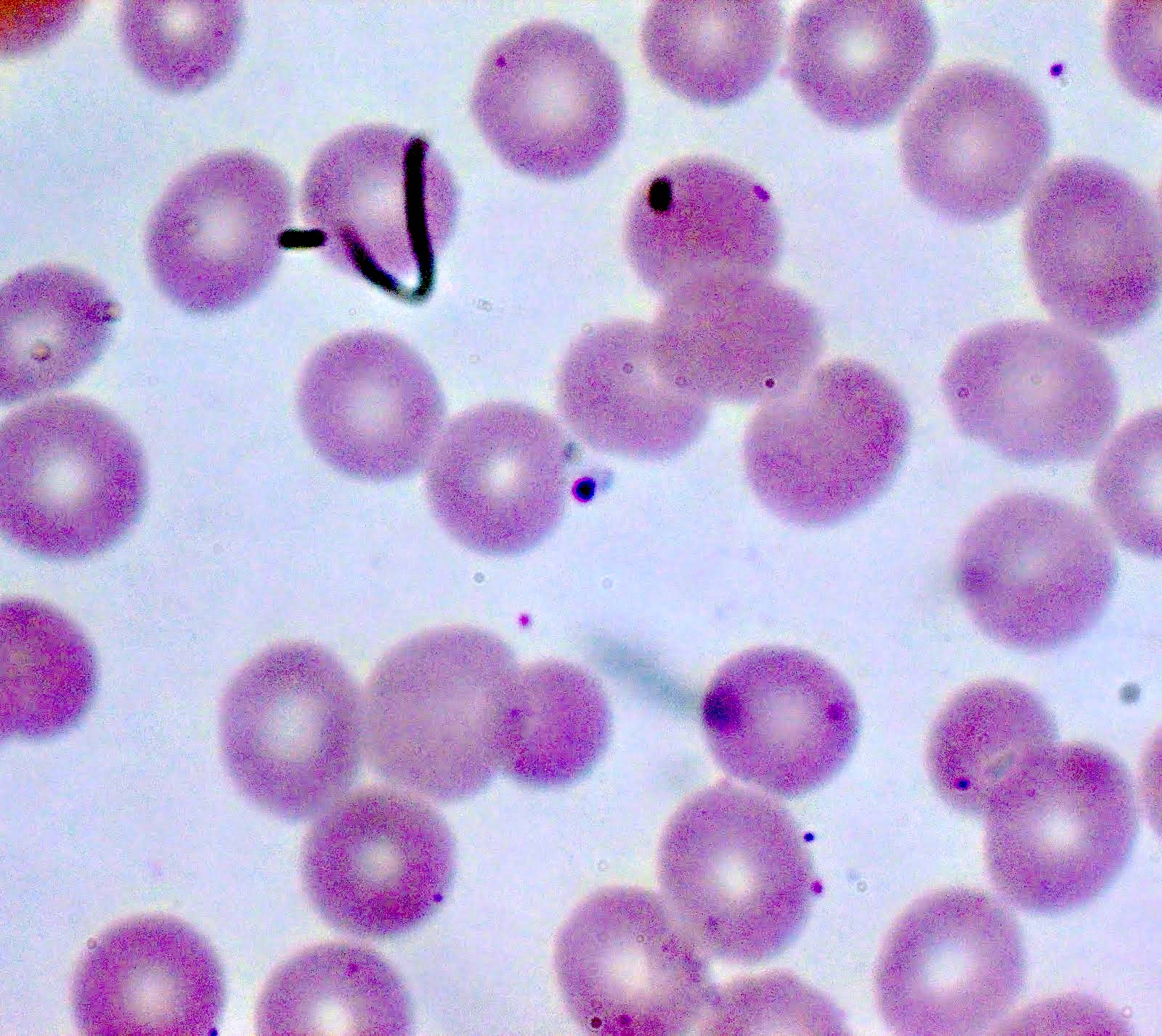
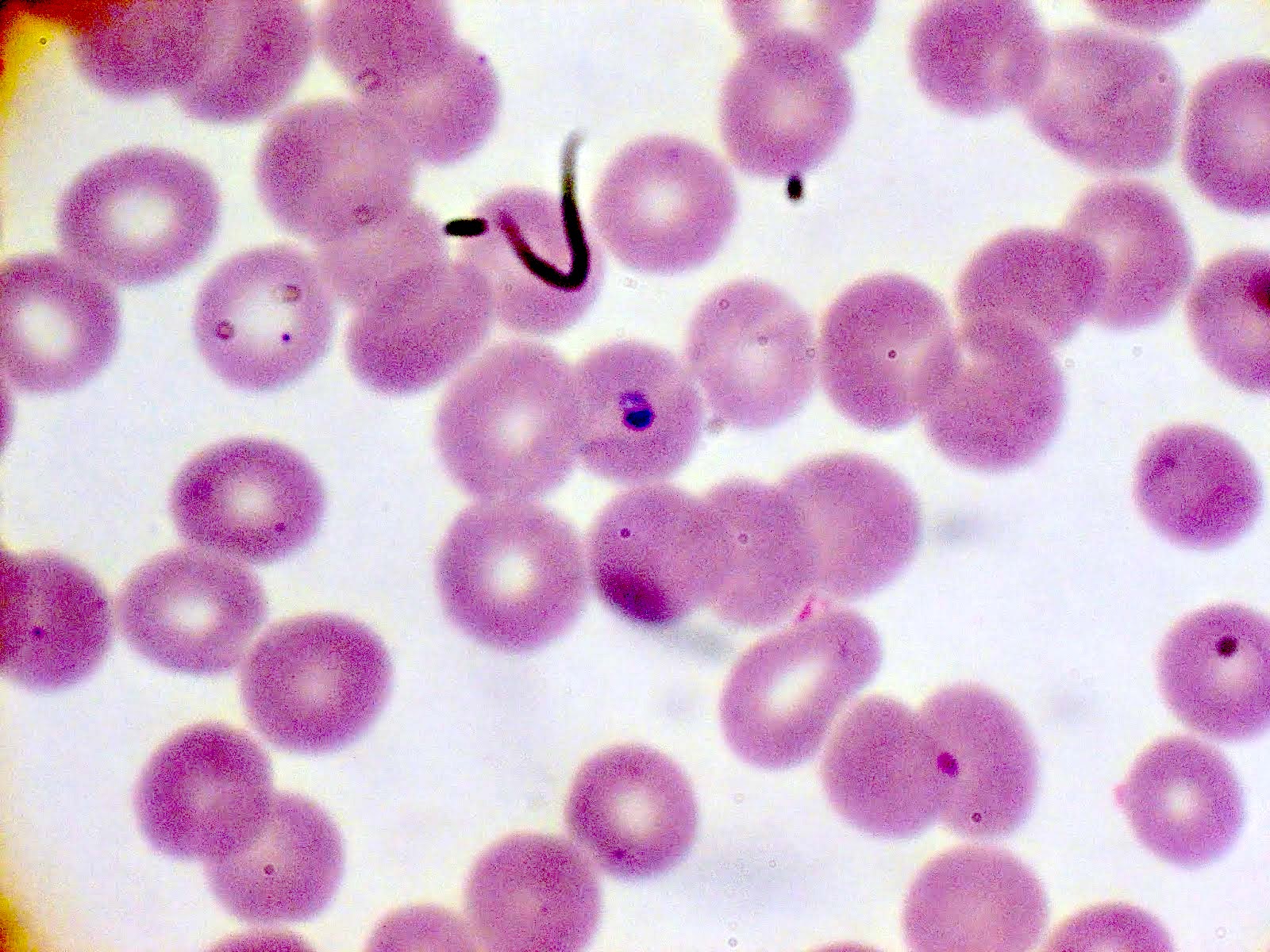
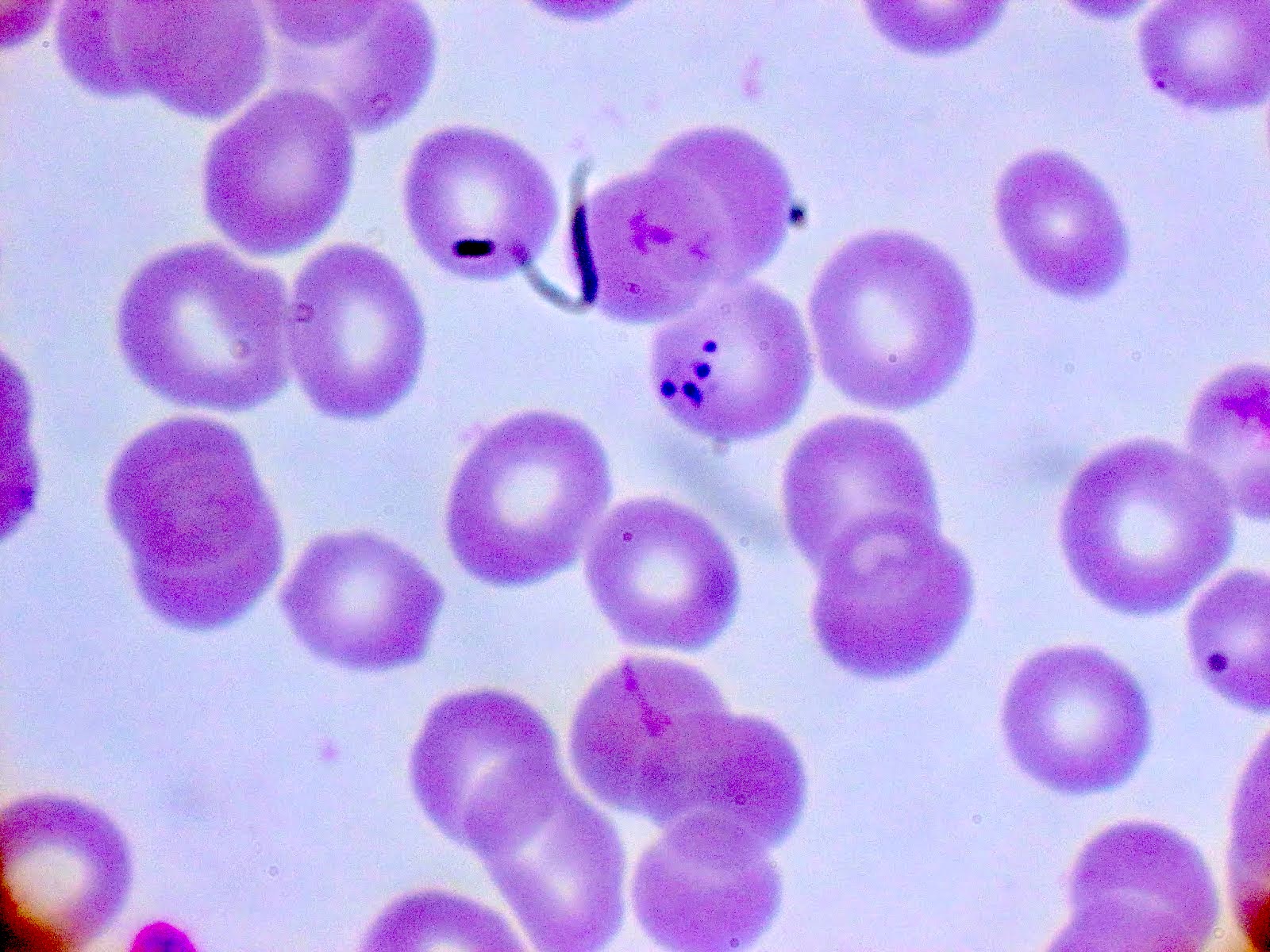
Peripheral smear description
- Thick smear Giemsa stain:
- Red / purple chromatin dot with pale blue cytoplasm forming a ring
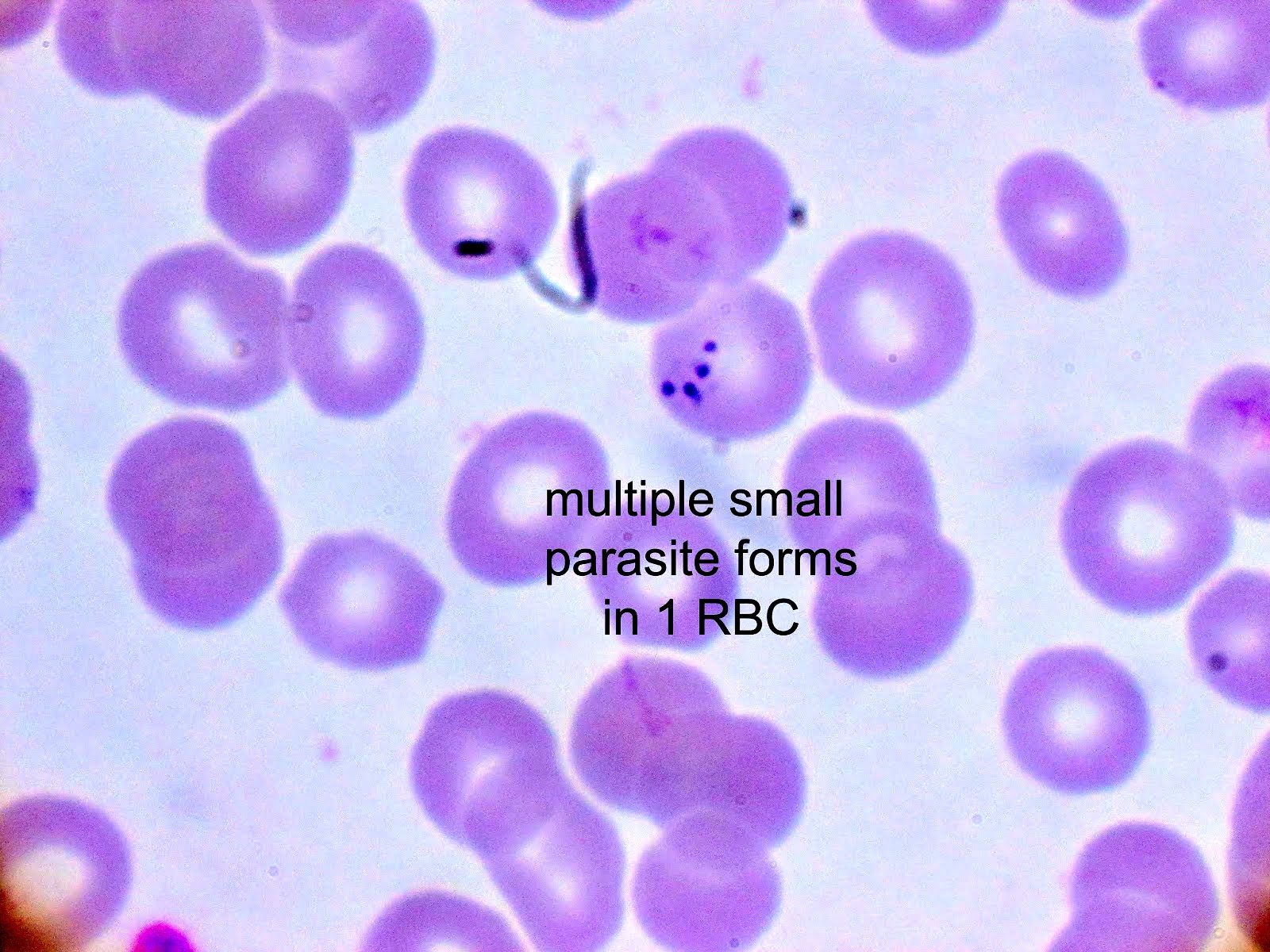
- Thin smear Giemsa stain (Pathogens 2022;11:399):
- Intracellular and extracellular ring forms
- Usually multiple forms within each infected red cell
- Maltese cross = classical finding of tetrad of intracellular ring forms
Peripheral smear images
Molecular / cytogenetics description
- PCR tests for Babesia DNA exist and can be used in cases of low parasitemia and blood product screening
Differential diagnosis
- Plasmodium falciparum (Pathogens 2021;10:1165):
- Up to 2 intracellular ring forms
- No extracellular ring forms
- Can see banana shaped gametocytes
- Clinical history of travel to endemic area
- May exhibit periodicity in fever
- Other Plasmodium spp. (Pathogens 2021;10:1165):
- Red cells with normally 1 ring form, occasionally 2
- Will commonly see other forms: schizonts, gametocytes, etc.
- No extracellular ring forms
- Clinical history of travel to endemic area
- May exhibit periodicity in fever
- If there has been a known Ixodes tick exposure and general symptoms of fever and malaise, differential diagnoses should include the following (Trends Parasitol 2018;34:295):
- Lyme disease:
- No visible parasites on blood smear
- Serology and PCR studies positive for Borrelia burgdorferi, a spirochete bacterium
- Commonly co-infects with Babesia
- Tick borne relapsing fever:
- No visible parasites on blood smear
- Serology and PCR studies positive for Borrelia miyamotoi
- Anaplasmosis:
- No visible intraerythrocytic or extracellular trophozoites
- May have morula observed in granulocytes
- Serology and PCR studies positive for Anaplasma phagocytophilum, a tick borne bacterium
- Ehrlichiosis:
- No visible intraerythrocytic or extracellular trophozoites
- May have morula observed in monocytes or granulocytes
- Serology and PCR studies positive for Ehrlichia spp.
- Powassan virus disease:
- No visible parasites on blood smear
- Laboratory diagnosis by testing serum or cerebrospinal fluid for virus specific antibodies
- Lyme disease:
Board review style question #1
Board review style answer #1
A. It causes more severe disease in asplenic patients. Babesiosis is less severe in those with an intact spleen, as the diseased red cells can be removed. The primary treatment of babesiosis is with atovaquone and amoxicillin. Babesiosis can co-infect with Lyme disease, Anaplasma and other tick borne diseases. Babesia is endemic to U.S. (most characteristically Mid-Atlantic to Northeastern U.S.) and Europe, not to sub-Saharan Africa (unlike Plasmodium spp.).
Comment Here
Reference: Babesia
Comment Here
Reference: Babesia
Board review style question #2
The clinical microbiology lab received a blood specimen from a 10 year old boy presenting with fever, malaise and chills. Significant history includes recent camping trip to Connecticut. Seen on thin smear are intraerythrocytic and extraerythrocytic ring forms and some red cells with up to 6 ring forms. What is the most likely diagnosis?
- Babesia microti
- Borrelia burgdorferi
- Plasmodium falciparum
- Plasmodium malariae
Board review style answer #2
A. Babesia microti. Babesia spp. are characterized by multiple intracellular ring forms and extracellular forms on blood smear. Babesiosis is common in the Northeastern U.S. due to prevalence of Ixodes (deer) tick. Without travel to malaria endemic regions, Plasmodium can be eliminated as a potential diagnosis. While the Ixodes scapularis tick can also vector Borrelia burgdorferi, the causative agent of Lyme disease, B. burgdorferi is a spirochete that is unlikely to be observed on blood smears.
Comment Here
Reference: Babesia
Comment Here
Reference: Babesia