Table of Contents
Definition / general | Terminology | Epidemiology | Pathophysiology / etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Life cycle | Prognostic factors | Mixed infections | Case reports | Treatment | Clinical images | Peripheral smear images | Differential diagnosis | Additional referencesCite this page: Fadel H. Plasmodium non-falciparum. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/parasitologymalariapvivax.html. Accessed April 25th, 2024.
Definition / general
- 4 species of plasmodia causing human malaria are Plasmodium vivax, Plasmodium falciparum, Plasmodium malariae and Plasmodium ovale
- P. vivax infections occur in both tropical and temperate zones, between 45° N and 40° S (WHO: Malaria [Accessed 10 January 2018])
Terminology
- Malaria (from the Italian mal aria, meaning bad air) is an acute and sometimes chronic infection of the bloodstream characterized clinically by fever, anemia and splenomegaly and is caused by apicomplexan parasites of the genus Plasmodium
Epidemiology
- P. vivax and P. ovale are the least frequent of malaria species; most cases arise in Western Africa, India, South America
- P. malariae occurs worldwide but with a lower incidence than P. falciparum or P. vivax
- Disease generally occurs between 45°N and 40°S (WHO: World Malaria Report 2014 [Accessed 9 January 2018])
- Plasmodium knowlesi usually causes malaria in monkeys (Lancet 2004;363:1017, Trends Parasitol 2008;24:406, Emerg Infect Dis 2008;14:1434)
Pathophysiology / etiology
- Spread exclusively by female anopheline mosquitoes
- Fever paroxysm occurs over 6 - 10 hours and is initiated by the synchronous rupture of erythrocytes with the release of new infectious blood stage forms known as merozoites
- Transfusion induced malaria may occur when blood donors have subclinical malaria and may prove fatal for the recipient
- Similarly, congenital malaria may occur in infants born to mothers from endemic areas; the infant acquires the infection at birth due to rupture of placental blood vessels with maternal fetal transfusion
- Neither transfusion nor congenital malaria is expected to relapse because exoerythrocytic schizogony does not occur
- Persons who lack certain Duffy blood group determinants are protected against P. vivax infection
- P. malariae can be maintained at low infection rates because it can remain in a human host for an extended period of time and still remain infectious to mosquitoes
Clinical features
- Defining clinical features of a malarial attack or paroxysm consist of, in order, shaking chills, fever (up to 40° C or higher) and generalized diaphoresis, followed by resolution of fever
- In the early stages of the disease, febrile episodes occur irregularly but eventually become more synchronous, assuming the usual tertian (P. vivax, P. falciparum and P. ovale) or quartan (P. malariae) periodicity
- Patients with malaria may develop anemia and may have other manifestations, including diarrhea, abdominal pain, headache and muscle aches and pains
- Patients with P. vivax or P. ovale infection may have relapses after many months or years
- Persons with P. falciparum and P. malariae infection may have symptom free periods but suffer from sporadic recrudescences owing to persisting low grade parasitemia
- Involvement of the brain is known as cerebral malaria, in which the patient becomes disoriented, progressing to delirium, coma and often death
- P. malariae causes a chronic infection that can last a lifetime; usually considered to have a low morbidity rate (Wikipedia: Plasmodium malariae [Accessed 9 January 2018])
Diagnosis
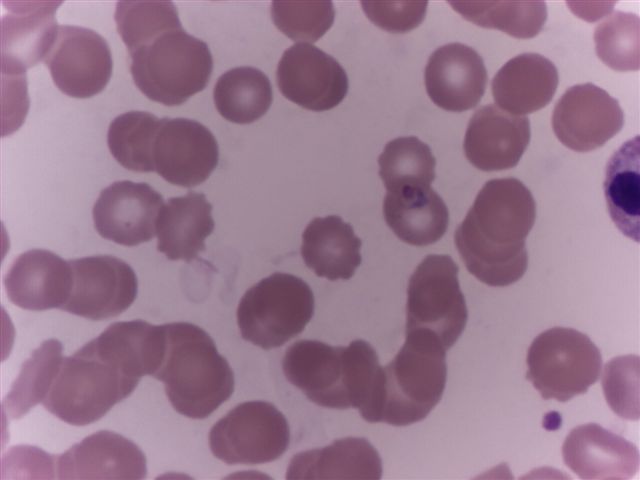
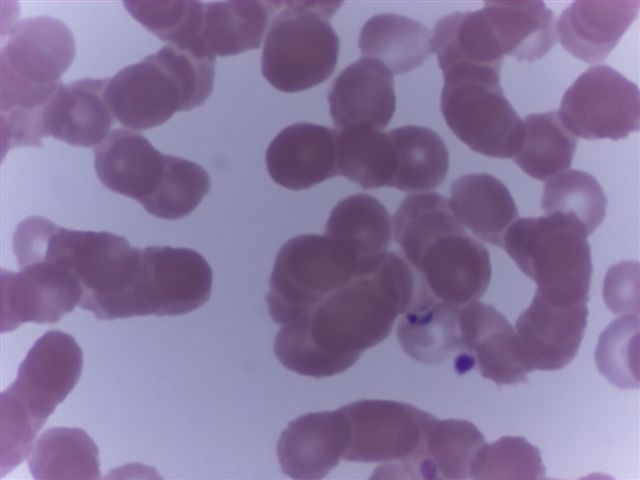
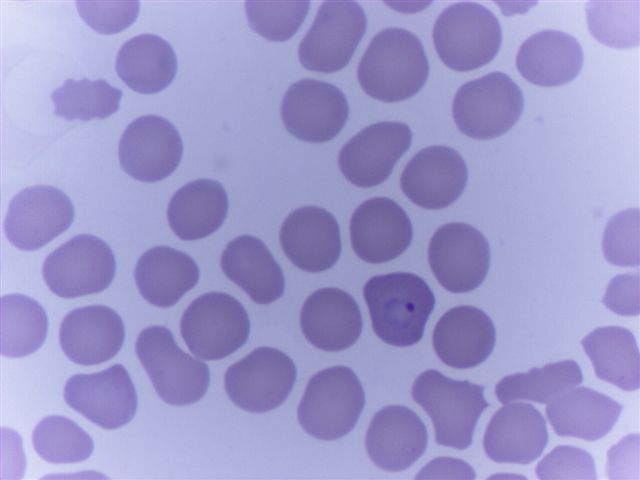
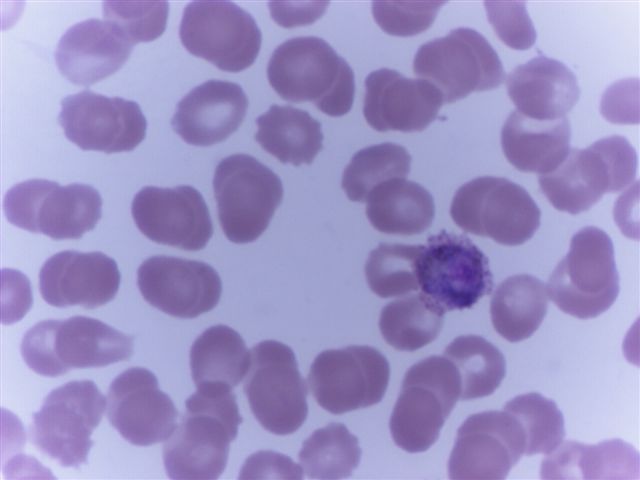
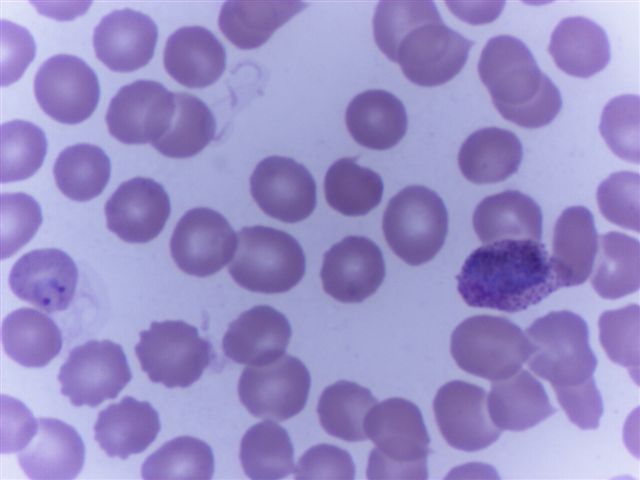
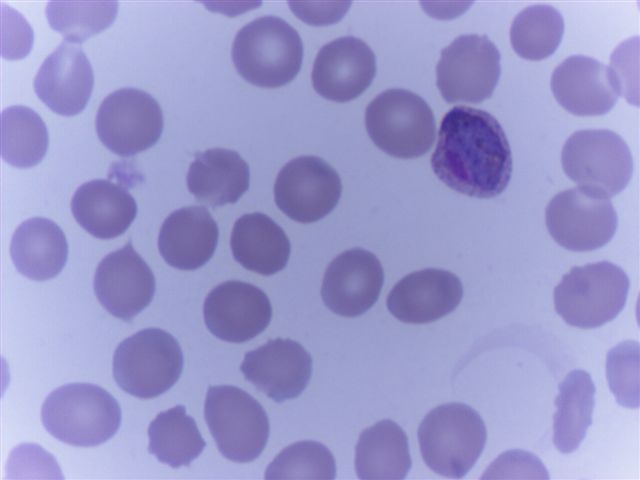
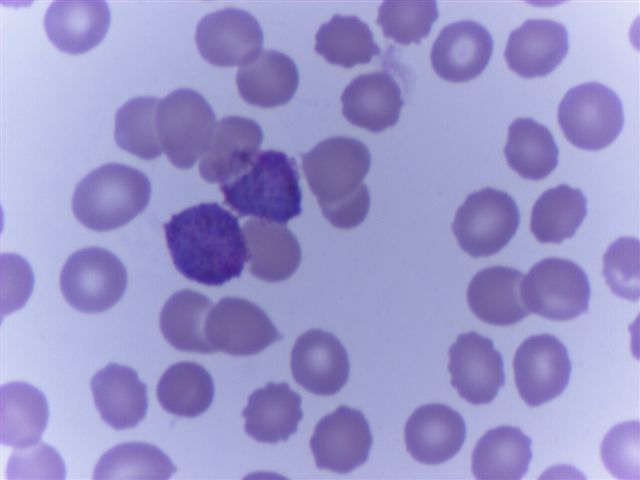
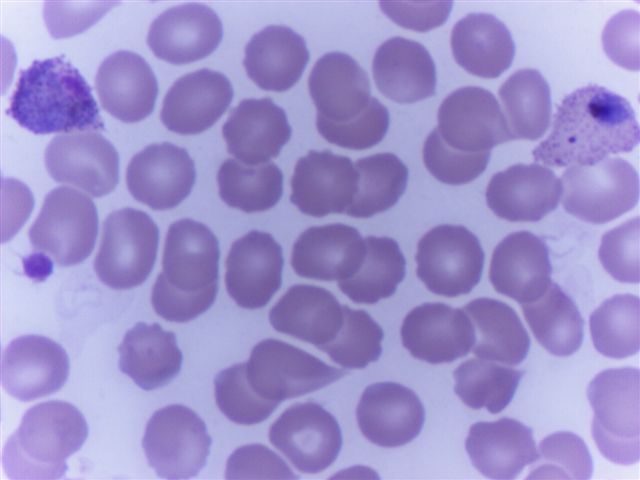
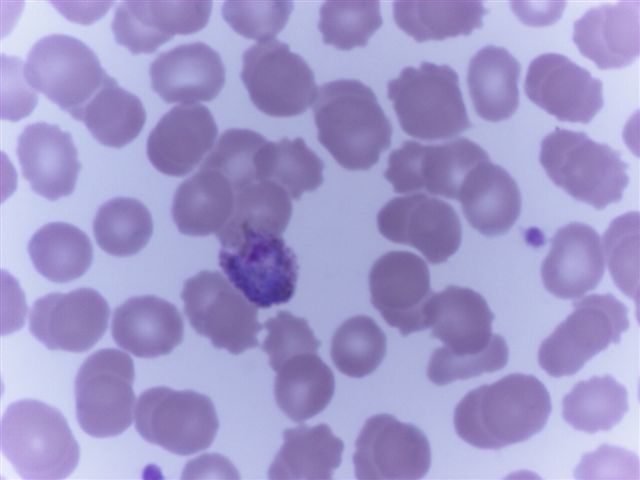
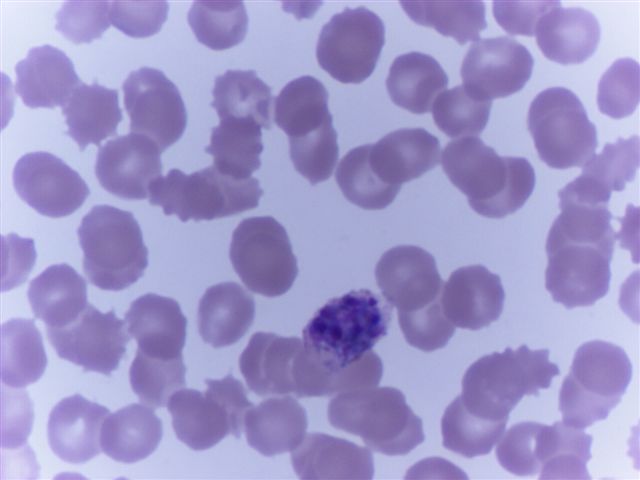
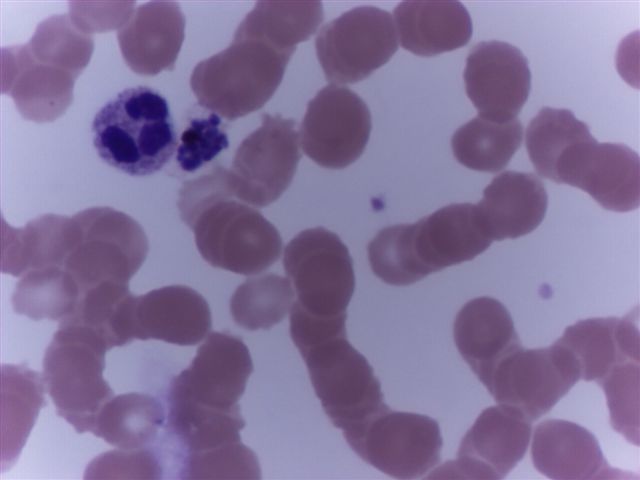
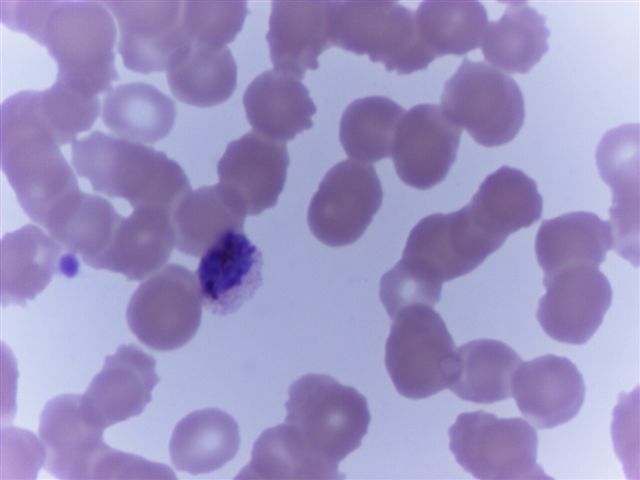
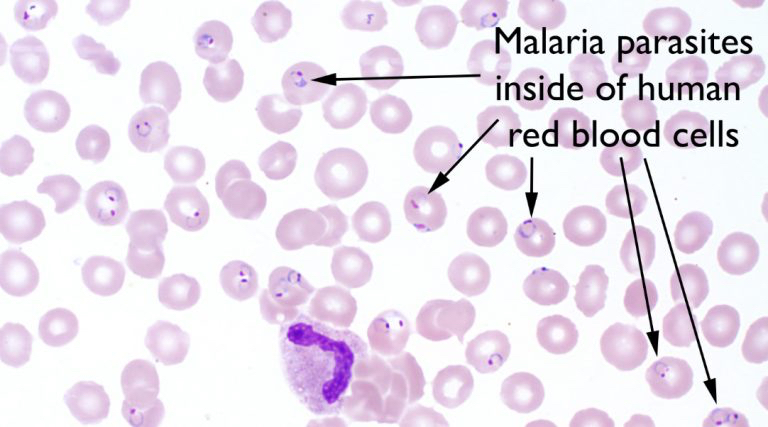
- Growing trophozoites of P. vivax have irregular shapes and are termed ameboid
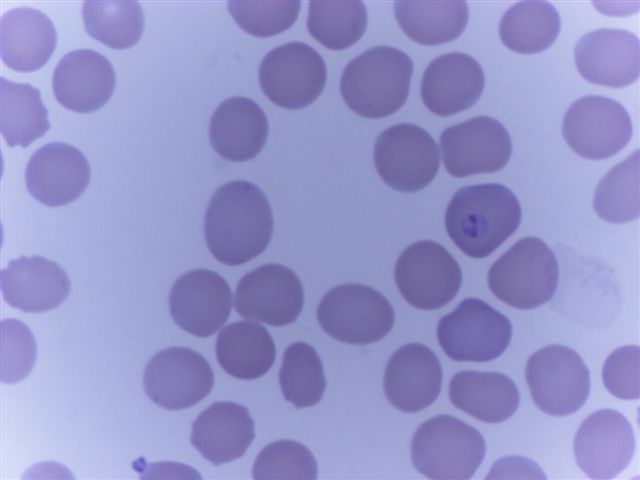
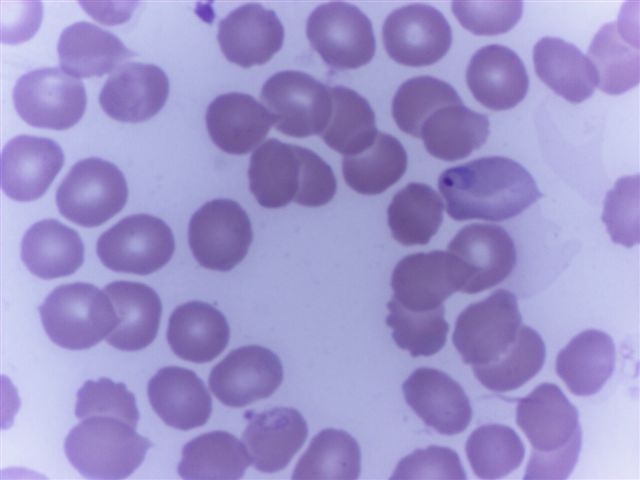
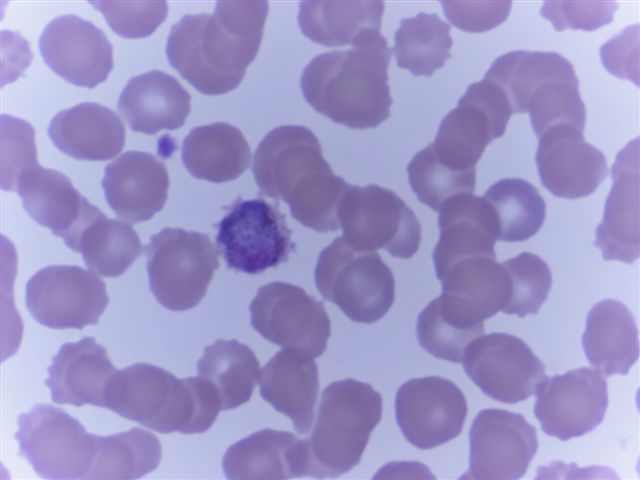
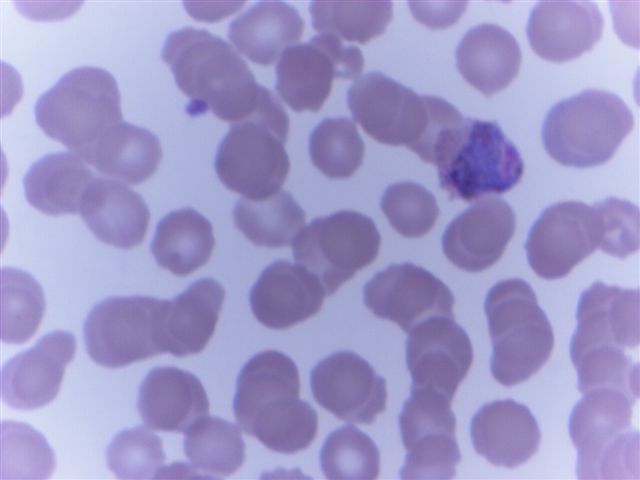
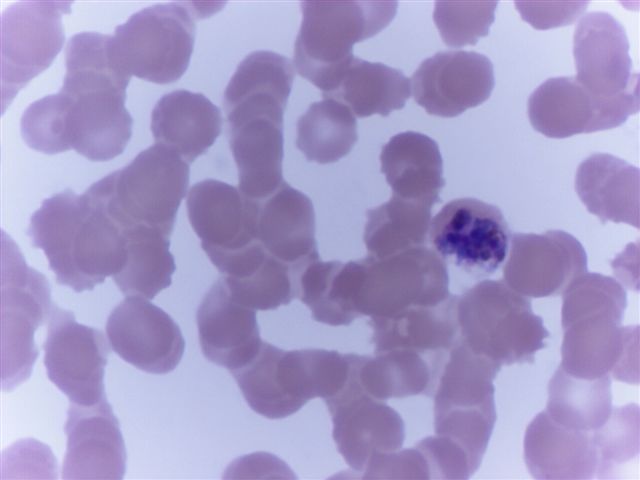
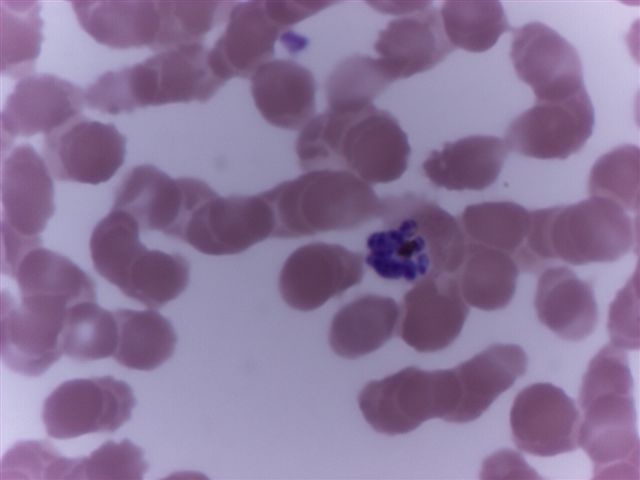
- Identification of malarial parasites on thin blood films requires a systematic approach
- 3 major factors should be considered: appearance of infected erythrocytes, appearance of parasites and stages found
- P. vivax and P. ovale parasites primarily infect young erythrocytes, whereas P. malariae infects older erythrocytes and P. falciparum infects erythrocytes of all ages
- Appearance of RBC and size:
- P. malariae: normal
- P. ovale: enlarged; maximum size may be 1.25 - 1.5 times normal red blood cell diameter; ~20% or more of infected red blood cells are oval or fimbriated (border has irregular projections)
- P. vivax: enlarged; maximum size (attained with mature trophozoites and schizonts); may be up to 2 times normal erythrocyte diameter
- Schüffner stippling:
- P. malariae: Ziemann dots rarely seen; Schüffner stippling is not seen in P. malariae or P. falciparum infections
- P. ovale: with all stages except early ring forms
- P. vivax: Maurer dots (comma shaped spots, dark blue by Giemsa staining, on RBC surface) are seen with all stages except early ring forms
- Parasite cytoplasm:
- P. malariae: rounded, compact trophozoites with dense cytoplasm; band form trophozoites occasionally seen
- P. ovale: rounded, compact trophozoites; occasionally slightly ameboid; growing trophozoites have large chromatin mass
- P. vivax: irregular, ameboid in trophozoites, has a spread out appearance
- Appearance of parasite pigment:
- P. malariae: dark brown, coarse, conspicuous
- P. ovale: dark brown and conspicuous
- P. vivax: golden brown, inconspicuous
- Number of merozoites:
- P. malariae: 6 - 12; average is 8; rosette schizonts are occasionally seen
- P. ovale: 6 - 14; average is 8
- P. vivax: 12 - 24; average is 16
- Stages found in circulating blood:
- P. malariae: all stages; wide variety of stages usually not seen; relatively few rings or gametocytes generally present
- P. ovale: all stages
- P. vivax: all stages; wide range of stages may be seen on any given film
Laboratory
- Laboratory evaluation relies on timely examination of thick and thin blood films to demonstrate the intraerythrocytic parasites
- More advanced laboratory methods, including acridine orange staining and detection of parasite specific DNA
Life cycle
- Morphologic stages seen in erythrocytes include trophozoites (growing forms), schizonts (dividing forms) and gametocytes (sexual forms)
- Malarial parasites undergo a sexual phase (sporogony) in Anopheles mosquitoes that produces infectious sporozoites and an asexual stage (schizogony) in humans that produces schizonts and merozoites
- In the bloodstream, some merozoites eventually differentiate into gametocytes (gametogony), which when ingested by female anopheline mosquitoes, mature into male microgametes and female macrogametes
- Fusion of a microgamete and a macrogamete results in the formation of the motile ookinete, which migrates to the outside of the mosquito stomach wall and forms an oocyst
- Within the oocyst, numerous spindle shaped sporozoites are formed
- Mature oocyst ruptures into the body cavity, releasing sporozoites, which then migrate through the tissues to the salivary glands, from which they are injected into the vertebrate host as the mosquito feeds
- Time required for development in the mosquito ranges from 8 - 21 days
- Sporozoites injected into the vertebrate host reach the hepatic parenchymal cells within minutes and initiate the proliferative phase known as exoerythrocytic schizogony
- Release of merozoites from ruptured hepatic schizonts initiates the bloodstream infection or erythrocytic schizogony and eventually the clinical symptoms of malaria
- P. vivax and P. ovale differ from P. falciparum and P. malariae in that true disease relapses of the former species may occur weeks to months following subsidence of previous attacks; this occurs due to renewed exoerythrocytic and eventually erythrocytic schizogony from latent hepatic sporozoites, which are known as hypnozoites
- Recurrence of disease due to P. falciparum or P. malariae, called recrudescences, arise from increased numbers of persisting blood stage forms to clinically detectable levels, not from persisting liver stage forms
- Liver cells are infected only by sporozoites from the mosquito; thus, transfusion acquired P. vivax or P. ovale infection does not relapse
- Merozoites released from infected hepatocytes subsequently infect erythrocytes
- Following amplification of parasites in the bloodstream for a period of time and the development of synchrony in their appearance, clinical attacks of malaria occur
- P. falciparum infects erythrocytes of all ages; P. vivax and P. ovale parasites primarily infect young erythrocytes; P. malariae infects older erythrocytes
- Species causing infection in 1987 were P. vivax (44%), P. falciparum (43%), P. malariae (4%), P. ovale (3%) and undetermined (6%)
Prognostic factors
- Persons who lack certain Duffy blood group determinants are protected against P. vivax infection
- Glucose-6-phosphate dehydrogenase (G6PD) deficiency has been associated with protection from malaria but evidence is less striking than with these other genetic abnormalities
Mixed infections
- ~5% of infections are mixed but diagnosis requires definite evidence of 2 separate populations of parasites
- Most common mixed infections are P. falciparum and P. vivax
- Finding gametocytes of P. falciparum in a person obviously infected with P. vivax is diagnostic
Case reports
- 24 year old woman with Plasmodium ovale malaria imported from West Africa (Korean J Parasitol 2013;51:213)
- 27 year old woman with fever, shivering and myalgia for 3 months (Asian Pac J Trop Biomed 2014;4:S56)
- 30 year old woman with frontal lobe infarct in Plasmodium vivax infection (Neurol India 2014;62:67)
- 35 year old man with first case of Plasmodium knowlesi infection in a Japanese traveller (Malar J 2013;12:128)
- 39 year old woman with first case of Plasmodium cynomolgi infection (from monkeys to mosquitos) (Malar J 2014;13:68)
- 39 year old man with Plasmodium ovale wallikeri infection (Korean J Parasitol 2013;51:557)
- 42 year old man with severe P. ovale infection (Malar J 2014;13:85)
- 59 year old woman with transfusion transmitted Plasmodium malariae (Malar J 2013;12:439)
Treatment
- Chloroquine (or hydroxychloroquine) remains the treatment of choice for all P. vivax and P. ovale infections, except in Indonesia's Irian Jaya (Western New Guinea) region and the geographically contiguous Papua New Guinea, where chloroquine resistance is common (up to 20% resistance) (Curr Opin Infect Dis 2009;22:430)
- Chloroquine resistance is an increasing problem in other parts of the world, such as Korea and India
- When chloroquine resistance is common or when chloroquine is contraindicated, then artesunate is the drug of choice, except in the U.S., where it is not approved for use
- No widespread evidence of chloroquine resistance in P. malariae and P. knowlesi species; therefore, chloroquine (or hydroxychloroquine) may still be used for both of these infections
- In addition, any regimens for chloroquine resistant malaria may be used for P. malariae and P. knowlesi infections
Peripheral smear images
Contributed by Monica E. De Baca, M.D. and Bobbi Pritt, M.D.
Images hosted on other servers:
Differential diagnosis
- Differential diagnosis for P. malariae and P. vivax:
- African trypanosomiasis
- Amebiasis and amebic liver abscess
- Bacteremia
- Brucellosis
- Viral illness
- Differential diagnosis for P. ovale:
- Endocarditis, bacterial
- Gastroenteritis
- Pharyngitis
- Plague
- Pneumococcal bacteremia