Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Sanchez DF, Cubilla AL. Penile intraepithelial neoplasia (PeIN). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/penscrotumPeIN.html. Accessed April 17th, 2024.
Definition / general
- Intraepithelial neoplastic proliferation with variable degree of dysplasia, keratinization and nuclear atypia
- Penile intraepithelial neoplasia (PeIN) is classified as HPV related / dependent or HPV unrelated / independent, similar to invasive carcinomas (Am J Pathol 2001;159:1211, Semin Diagn Pathol 2015;32:198)
- Considered a precursor of penile invasive carcinoma
Essential features
- Classified as HPV related / dependent or HPV unrelated / independent
- May occur in any of the penile mucosal epithelial areas, most commonly in the glans and foreskin
- Differentiated PeIN is related to lichen sclerosus
- HPV16 is the most frequent genotype associated with PeIN
Terminology
- Synonyms are as follows: erythroplasia of Queyrat, Bowen disease, carcinoma in situ (CIS), squamous intraepithelial lesion, dysplasia (mild, moderate and severe) and bowenoid papulosis
- PeIN is the recommended nomenclature for penile precancerous lesions (Epstein: Tumors of the Prostate Gland, Seminal Vesicles, and Scrotum, 2020, Eur Urol 2016;70:93)
- PeIN refers to squamous lesions and excludes Paget disease, urothelial carcinoma in situ and malignant melanoma in situ
- Some authors stratify PeIN into grades I, II and III (Int J Urol 2019;26:353)
ICD coding
Epidemiology
- There is geographic variation in the presentation of PeIN (Hum Pathol 2012;43:190)
- Differentiated PeIN is more commonly diagnosed in countries with a high frequency of penile cancer
- HPV related PeIN is more common in countries with a low frequency of penile cancer
- In countries with a high frequency of invasive penile carcinomas (2 - 5 cases/100,000), PeIN is rarely diagnosed as a solitary lesion (Hum Pathol 2012;43:190)
- In countries in which invasive penile carcinomas are rare (≤ 1 case/100,000), PeIN is the most common penile neoplasia at clinical diagnosis
- PeIN affects patients younger than those with invasive cancers (Hum Pathol 2012;43:1020)
- Mean age is ~58 years old
- HPV related PeIN preferentially affects younger patients
- Predisposing factors: HIV / immunosuppression, lack of or delayed circumcision, inflammatory / irritative conditions (balanitis, buried penis, phimosis) (Mod Pathol 2022;35:1101)
Sites
- PeIN is most commonly found in the glans and foreskin (Histopathology 2011;58:925, Int J Urol 2019;26:353)
- Differentiated PeIN, non-HPV related, preferentially involves the foreskin inner mucosal epithelium
- ~33% of cases with PeIN are multicentric, especially the HPV related types
- PeIN may occur in the skin of the shaft of the penis
Etiology
- Undifferentiated: high risk HPV
- Differentiated: lichen sclerosus
Clinical features
- Lesions can be subclassified according to morphological features and HPV genotypes present (Am J Surg Pathol 2017;41:820)
- Non-HPV related PeIN / differentiated
- Represented by differentiated PeIN
- Squamous or simplex PeIN are synonyms
- Putative precursors of non-HPV related keratinizing squamous cell invasive carcinomas, the majority of penile cancers
- Most cases in association with invasive carcinoma and rarely as a solitary lesion
- Difficult to diagnose and underrecognized by pathologists due to only subtle histologic changes
- Foreskin is a preferential site but the glans is also involved
- Frequently associated with lichen sclerosus
- HPV related PeIN / undifferentiated
- Subclassified in basaloid, warty and warty basaloid subtypes (Epstein: Tumors of the Prostate Gland, Seminal Vesicles, and Scrotum, 2020, Eur Urol 2016;70:93)
- Bowen disease, CIS, high grade PeIN are synonyms
- In young males with multicentric lesions, it has been referred to as bowenoid papulosis (Cancer 1978;42:1890)
- More frequently multicentric than differentiated PeIN
- Putative precursors of HPV related basaloid and condylomatous (warty) invasive carcinomas or mixtures, ~33% of penile cancers (Am J Surg Pathol 2017;41:820)
- Straightforward diagnosis and well recognized by pathologists
- Glans is a preferential site but the foreskin, coronal sulcus and shaft may also be involved
- HPV16, 6 and 11 are the most commonly found genotypes (Lancet Oncol 2019;20:145, Int J Surg Pathol 2020;28:265)
- HIV positive patients are more susceptible to develop HPV related PeIN (AIDS 2006;20:1201)
- Mixed PeIN
- Coexisting non-HPV and HPV related PeIN in the same specimen
- Rarely found as solitary lesions
- Multicentric lesions may be in collision, next to each other or in separate foci
- Pathological features and HPV composition are similar in PeIN and invasive carcinomas (Int J Surg Pathol 2020;28:265)
- HPV is usually negative in differentiated PeIN and the corresponding invasive non-HPV related squamous cell carcinoma
- HPV is usually positive in PeIN and the corresponding invasive basaloid or warty invasive carcinoma
- Morphological similarity and HPV genotype composition indicate a causal relation of PeIN and corresponding invasive carcinoma
Diagnosis
- Dermatoscopy
- Biopsy
- Excision
Prognostic factors
- Frequent recurrence (48%) (Mod Pathol 2022;35:1101)
- Low rate of progression to invasive carcinoma (2%) (Mod Pathol 2022;35:1101)
Case reports
- 51 year old man with pruritic lesions on the penis, scrotum, pubis and gluteal region (JAAD Case Rep 2017;3:542)
- 68 year old man presented with phimosis (Open Access Maced J Med Sci 2017;6:61)
- 79 year old man with penile lesion involving the distal urethra (SAGE Open Med Case Rep 2020;8:2050313X20918985)
Treatment
- Local excision (Mohs surgery, glans resurfacing, glansectomy) is the most frequent approach (BJU Int 2022;129:752, Semin Diagn Pathol 2015;32:232)
- Laser therapy is associated with higher complication and recurrence rate (BJU Int 2022;129:752, Eur Urol Focus 2021 May 11 [Epub ahead of print])
- Topical agents (5-fluorouracil, imiquimod 5%)
- Local destructive methods (photodynamic therapy, cryotherapy, curettage and electrocautery)
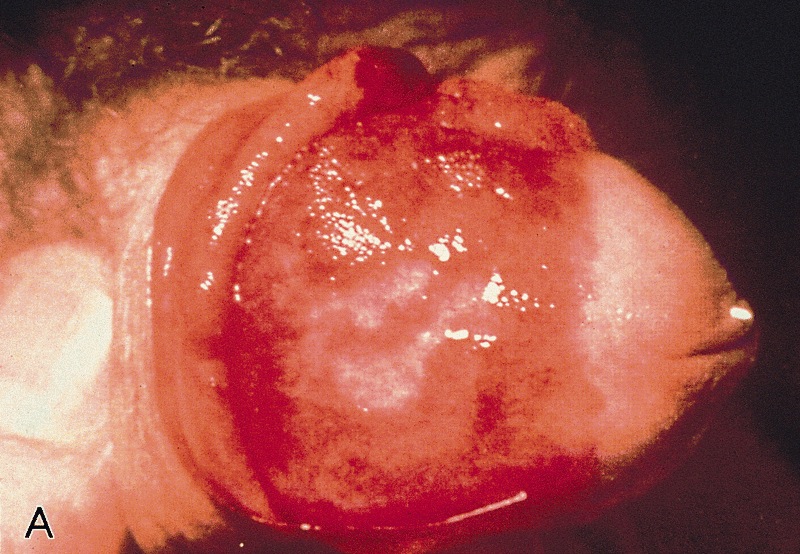
Clinical images
Gross description
- Non-HPV related PeIN / differentiated
- Solitary white or pink macule, plaque or slightly elevated geographical lesion
- Affects the foreskin and glans and rarely the shaft
- HPV related PeIN
- Lesions are flat or slightly elevated or papular, velvety, erythematous, dark brown or black
- Warty PeINs are granular or villous
- Borders are irregular or sharply delineated
- References: Epstein: Tumors of the Prostate Gland, Seminal Vesicles, Penis, and Scrotum, 2020, Eur Urol 2016;70:93
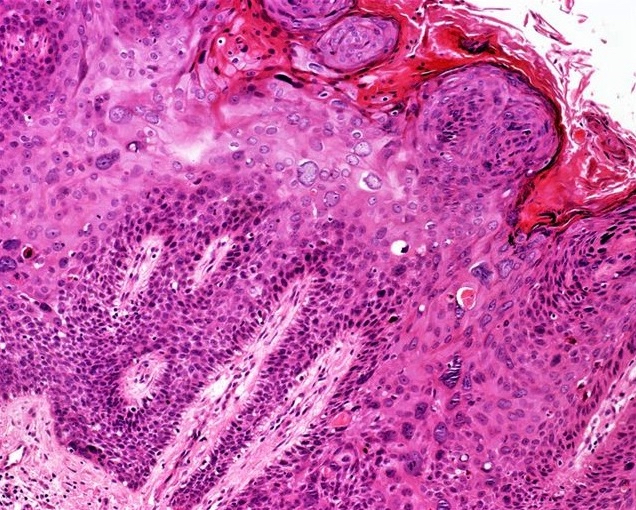
Microscopic (histologic) description
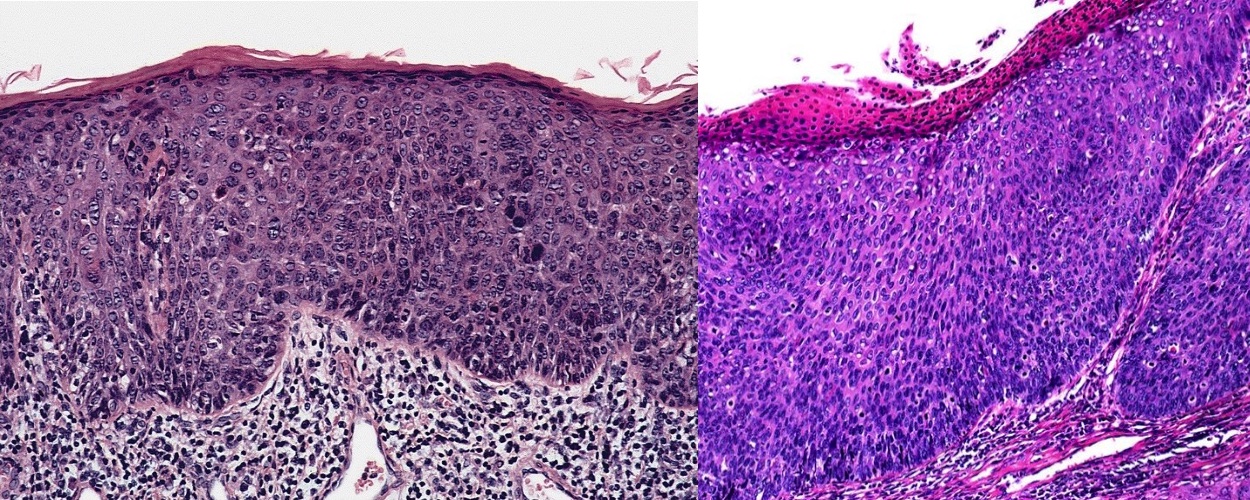
- Non-HPV related PeIN / differentiated
- Common features are hyperkeratosis, parakeratosis, hypergranulosis, acanthosis, elongation of rete ridges, abnormal squamous maturation and squamous cell atypia
- Prominent intercellular edematous bridges and intraepithelial keratinization
- Some histological heterogeneity: hyperplasia-like, classic and pleomorphic features
- Most common or classic feature is a keratinized maturing lesion with obvious atypical cells involving 2 or 3 basal epithelial layers
- Less common are the hyperplasia-like features, with acanthotic thickening of the epithelium and subtle basal cell atypia
- In the pleomorphic variant, there are anaplastic cells involving most of the epithelial thickness but with evident maturation or cellular keratinization
- Grading system if used can classify as follows: hyperplasia-like as grade 1, classic as grade 2, pleomorphic as grade 3
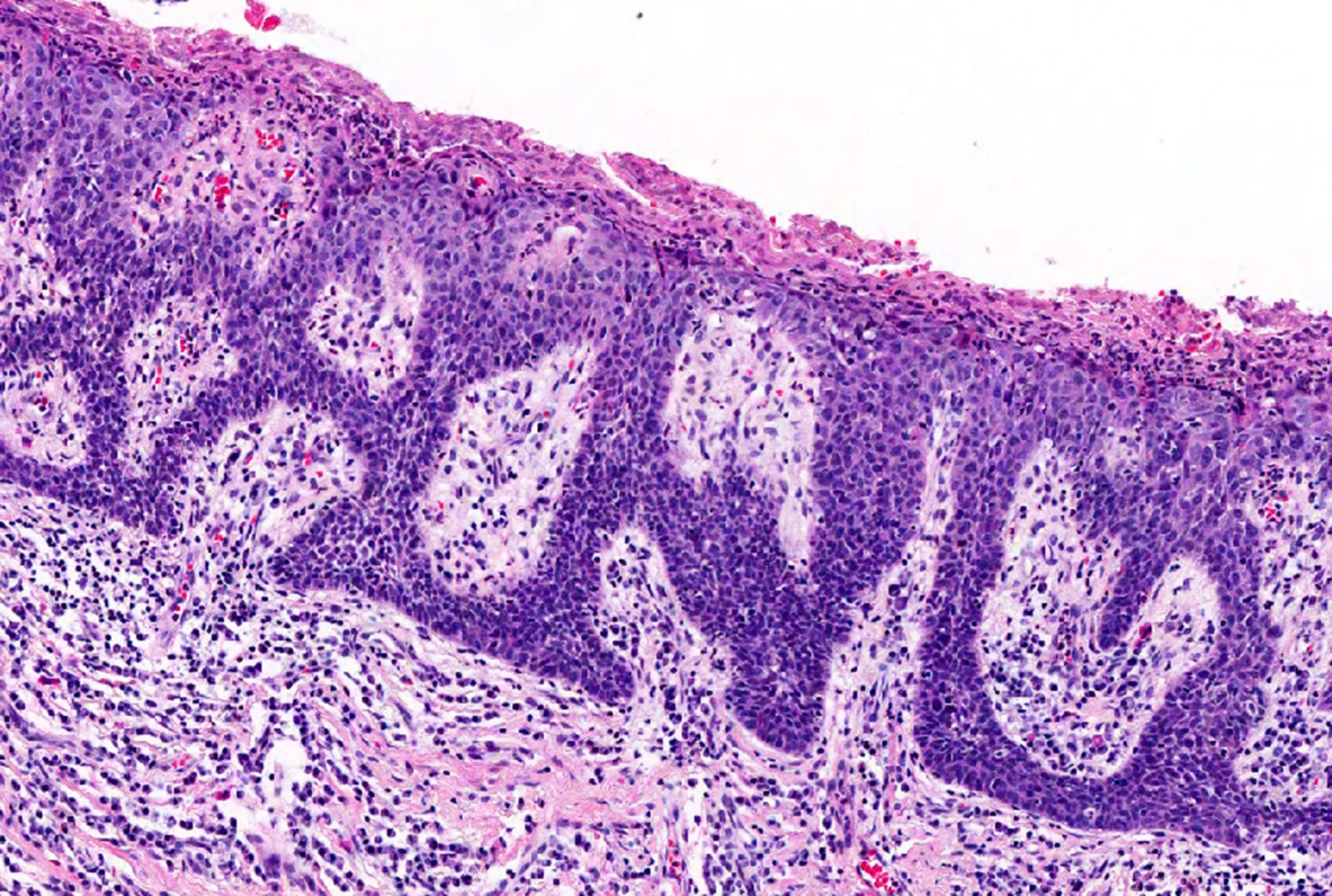
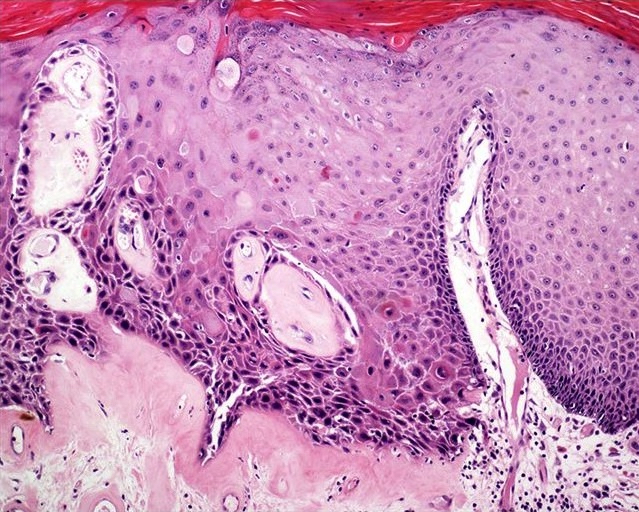
- Basaloid PeIN
- Most frequent subtype
- Uni or multicentric
- Usually, flat lesions with a broad or undulating base
- Occasionally, papillary lesions simulating urothelial tumors
- Monotonous uniform small anaplastic basaloid cell population
- Replace the full epithelial thickness
- Superficial hyper and parakeratosis often with some koilocytes is typical
- Rarely, cells are larger, spindly or pleomorphic
- High nuclear cytoplasmic ratio
- Numerous mitoses may be noted
- Starry sky pattern is not uncommon
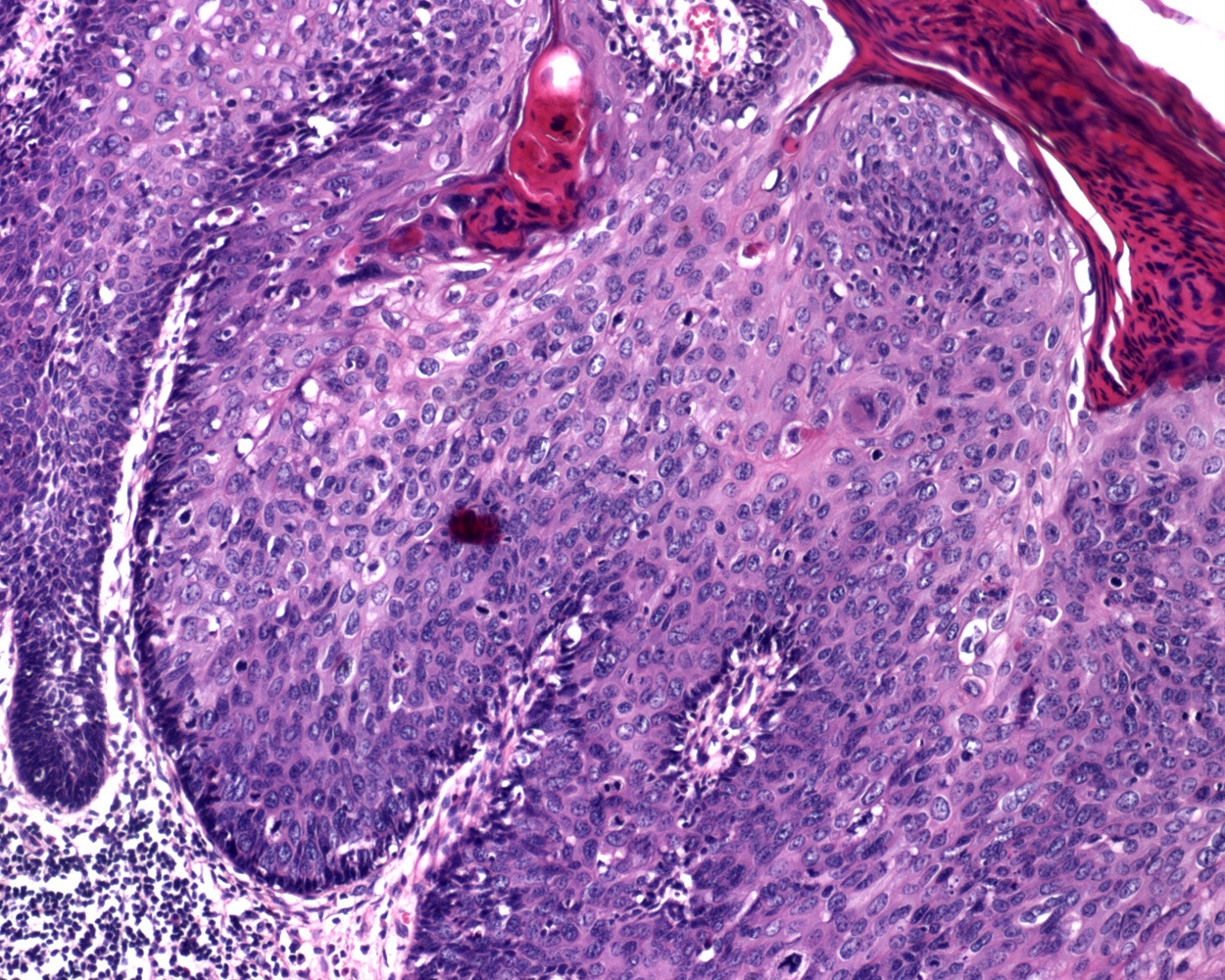
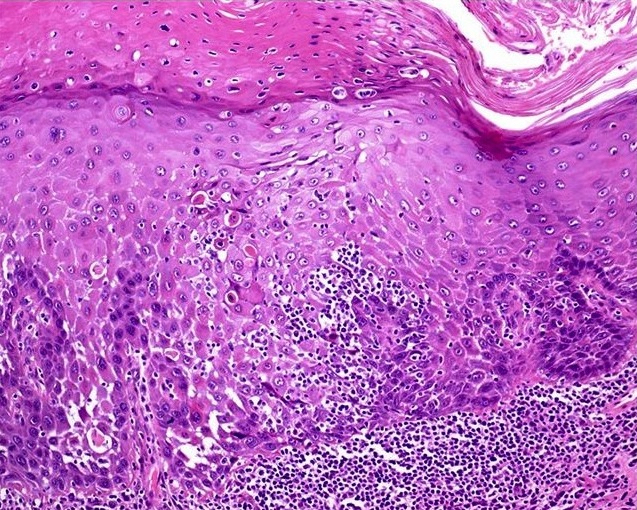
- Warty PeIN
- Presentation as a solitary lesion is unusual (Am J Surg Pathol 2017;41:820)
- Most commonly, it is part of a multicentric lesion
- Associated with invasive warty or basaloid carcinomas
- Squamous maturing lesion
- Striking micropapillary spiking features
- Surface shows hyper and parakeratosis
- Hallmark is atypical superficial or deep pleomorphic koilocytosis
- Multinucleation, nuclei with irregular contours, perinuclear halo and dyskeratosis are common
- Warty basaloid PeIN
- Warty cells and basaloid cells in about equal proportions
- Unifocal or multicentric lesions
- May be associated with invasive basaloid or warty carcinomas
- Hyper and parakeratosis, papillary or spiking features at the upper half
- Upper half is composed of clear warty-like cells
- Lower half is composed of small, anaplastic basaloid type cells
Microscopic (histologic) images
Contributed by Alcides Chaux, M.D. and Antonio Cubilla, M.D.
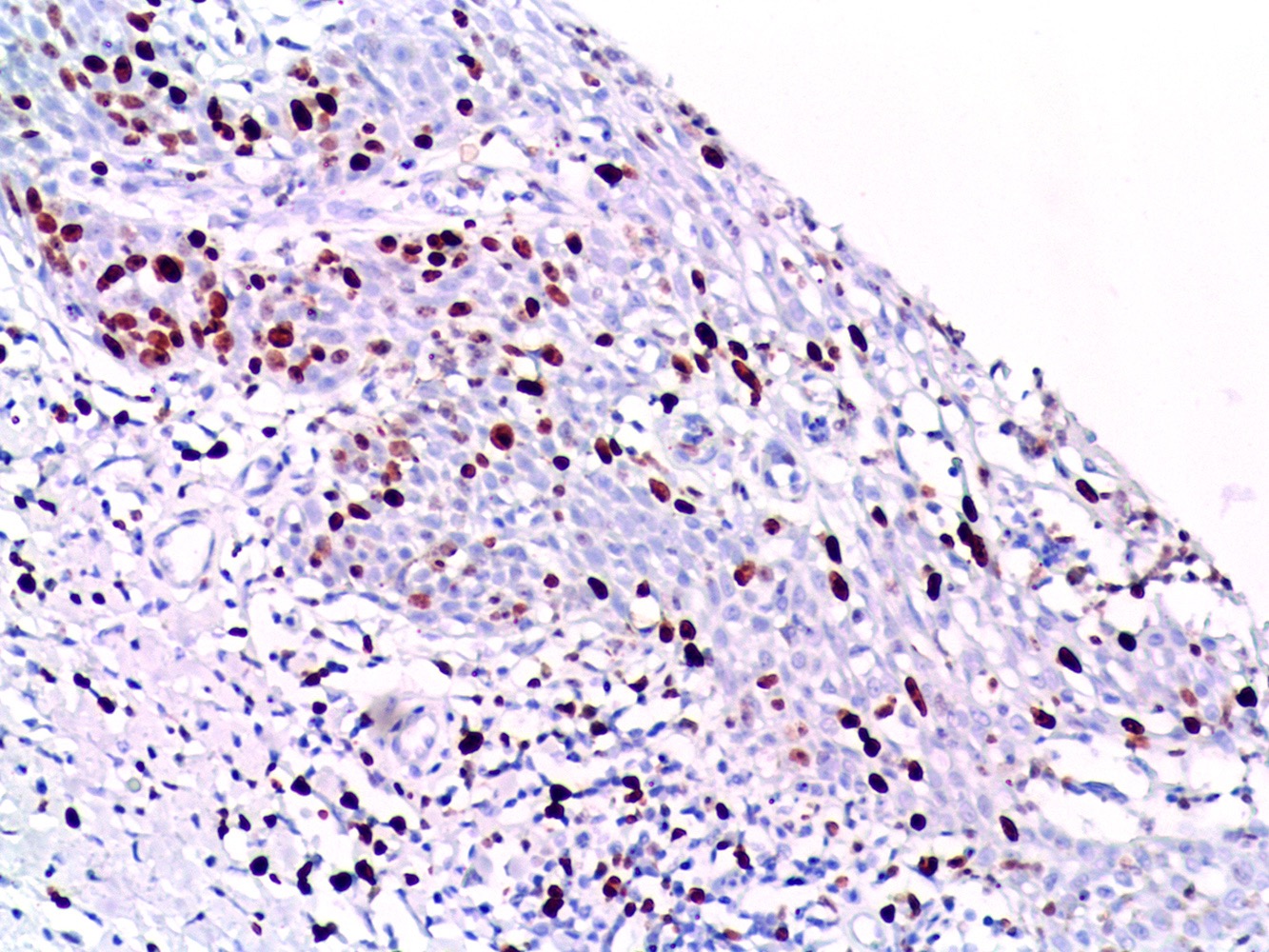
Positive stains
- Non-HPV related PeIN / differentiated
- HPV related PeIN / undifferentiated
- Ki67: positive in most cells, full thickness
- p16: 99% positive, en bloc for basaloid PeIN and ≤ 50% of epithelial thickness in warty basaloid and warty PeIN (Am J Surg Pathol 2010;34:385, Mod Pathol 2022;35:1101)
Negative stains
- Non-HPV related PeIN / differentiated
Molecular / cytogenetics description
- HPV detection by PCR or ISH is negative in differentiated PeIN
- High risk HPV is detected in most HPV related PeIN
- HPV16 found in 67% of basaloid PeIN (Am J Surg Pathol 2017;41:820)
- Low risk HPV is present in 16% of warty PeIN (Am J Surg Pathol 2017;41:820)
- More variable HPV genotypic composition in warty PeIN
Sample pathology report
- Penis, glans, biopsy:
- HPV related basaloid penile intraepithelial neoplasia (PeIN) (see comment)
- Comment: Lateral margins are involved by PeIN. High risk HPV ISH positive. p16 immunostaining is positive en bloc.
Differential diagnosis
- Non-HPV related / differentiated PeIN:
- Squamous hyperplasia:
- Condyloma acuminatum, flat type:
- HPV related PeIN (versus pleomorphic differentiated PeIN):
- HPV related PeIN:
- Urothelial carcinoma in situ (versus basaloid PeIN):
- p16 negative
- Condyloma acuminatum with atypical features (versus warty PeIN) (Int J Surg Pathol 2020;28:265):
- p16 negative
- May harbor low or high risk HPV
- Squamous cell carcinoma warty and basaloid types (versus warty and basaloid PeIN)
- Urothelial carcinoma in situ (versus basaloid PeIN):
Board review style question #1
A 55 year old man undergoes excision of a 1 cm, slow growing, erythematous plaque on the glans penis. At microscopy, the epithelium showed full thickness dysplasia, pleomorphic cells and mitoses. A representative photomicrograph is shown above. p16 immunostaining was strongly positive and Ki67 was positive in all cell layers. Which of the following statements is true regarding the depicted tumor?
- Differentiated PeIN hyperplasia-like is the diagnosis
- Distinguishing this lesion from squamous hyperplasia is difficult
- HPV16 is the most frequent genotype identified in the lesion
- It is the precursor of the most frequent invasive penile carcinoma subtype
- This neoplasia is usually related to lichen sclerosus
Board review style answer #1
C. HPV16 is the most frequent genotype identified in the lesion. This is HPV related PeIN. 67% of basaloid PeIN are positive for HPV16 genotype.
Comment Here
Reference: Penile intraepithelial neoplasia
Comment Here
Reference: Penile intraepithelial neoplasia
Board review style question #2
A 78 year old man undergoes excision of a 1 cm whitish plaque on the foreskin. At microscopy, the epithelium showed full thickness dysplasia, pleomorphic cells with ample cytoplasm and mitoses. Which of the following steps is needed for a final diagnosis?
- CD4 / CD8 for evaluating lichen sclerosus
- HMB45 immunostaining
- Ki67 for differentiating warty from basaloid PeIN
- In situ hybridization for high risk HPV
- p53 for ruling out squamous hyperplasia
Board review style answer #2
D. In situ hybridization for high risk HPV. In situ hybridization for high risk HPV is needed to confirm HPV related basaloid PeIN versus non-HPV related differentiated PeIN with pleomorphic features.
Comment Here
Reference: Penile intraepithelial neoplasia
Comment Here
Reference: Penile intraepithelial neoplasia