Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Sanchez DF, Cubilla AL. Lichen sclerosus (balanitis xerotica obliterans). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/penscrotumbxo.html. Accessed April 20th, 2024.
Definition / general
- Chronic inflammatory mucocutaneous condition (J Eur Acad Dermatol Venereol 2018;32:91)
- Male equivalent of lichen sclerosus et atrophicus of vulva
Essential features
- Chronic inflammatory and sclerotic benign condition
- Clinical diagnosis is usually straightforward
- Middle aged men
- Unknown etiology
- Associated with penile intraepithelial neoplasia (PeIN) and penile carcinomas
Terminology
- Also called lichen sclerosus et atrophicus
- Balanitis: inflammation of glans, from Greek ("acorn")
- Xerotica: unable to determine origin of term but used by Stuhmer in 1928 (see also Arch Dermatol Syph 1941;44:547)
ICD coding
Epidemiology
- Middle aged men
- Frequency (J Urol 2011;185:522):
- Overall: 1.4/100,000
- Asian: 0.9/100,000
- African American: 1.4/100,000
- Other: 1.7/100,000
- White: 2.1/100,000
- Reported in young boys (Ann R Coll Surg Engl 2007;89:62, Pediatr Surg Int 2018;34:1245)
- Common cause of phimosis (Histopathology 2011;58:925)
Sites
- Inner foreskin, coronal sulcus and glans mucosae
- Urethra may be affected
- Rarely extends to the shaft
Pathophysiology
- Unknown at this time
Etiology
- Chronic inflammation (BJU Int 2011;108:14)
- Autoimmune association remains elusive (Acta Derm Venereol 2013;93:238)
- HPV, Borrelia burgdorferi, EBV and were reported as concurrent (Int J Dermatol 2018;57:139, Arch Dermatol 2008;144:591)
Clinical features
- Most common cause of pathological phimosis in boys
- Narrowing of urethral meatus and paraphimosis
- Associated with low grade keratinizing squamous cell carcinoma (non-HPV variants: squamous cell, NOS, pseudohyperplastic, verrucous and papillary, in glans and foreskin) (Am J Surg Pathol 2003;27:1448, Int J Surg Pathol 2004;12:351)
- Rarely found in basaloid or warty invasive carcinoma
- The majority are associated with differentiated PeIN versus HPV related PeIN
- Atypical lichen sclerosus, with epithelial dysplastic changes (low grade or high grade, are currently classified as differentiated PeIN) (Moch: WHO Classification of Tumours of the Urinary System and Male Genital Organs, 4th Edition, 2016)
- There is a sequential spatial distribution of lichen sclerosus with precancerous and invasive carcinoma suggesting it is a precancerous condition (Int J Surg Pathol 2019;27:477)
Diagnosis
- Peniscopy: grayish white plaques in foreskin, coronal sulcus or glans
- Biopsy all suspected cases (J Urol 2007;178:2268)
Prognostic factors
- Local anatomy alterations if untreated (Br J Dermatol 2018;178:839)
- Meatal stenosis
- Urethral strictures
- Concealed buried penis
- Sexual dysfunction
- More than half of patients responds to local therapy (J Eur Acad Dermatol Venereol 2012;26:730)
- Up to 25% of surgical treated require further interventions (J Eur Acad Dermatol Venereol 2012;26:730)
- p53, CDKN2A alterations suggest progression to neoplasia (Int J Biol Sci 2019;15:1429)
Case reports
- 45 year old man with lichen sclerosus and granuloma annulare in his foreskin (Rom J Morphol Embryol 2015;56:1179)
- 56 year old man with urethral squamous cell carcinoma and long history of genital lichen sclerosus (Am J Mens Health 2018;12:493)
- 70 year old man with lichen sclerosus, nevus elasticus and neoplastic progression (JAAD Case Rep 2015;1:163)
- 76 year old man with lichen sclerosus associated nevus on glans mimicking melanoma (JAAD Case Rep 2020;6:323)
Treatment
- Local corticosteroids
- Imiquimod
- PUVA (Psoralen and UltraViolet A) therapy
- Biopsy all cases of possible BXO (J Urol 2007;178:2268)
- Circumcision is indicated for preputial lesions (J Eur Acad Dermatol Venereol 2012;26:730)
Clinical images
Gross description
- Grayish, bluish to white irregular geographic foci of atrophy
- Erosion, ulceration and raised pearly white areas
- In advanced cases, inner preputial folds may disappear due to replacement of elastic fibers by fibrous tissue (Am J Clin Dermatol 2013;14:27)
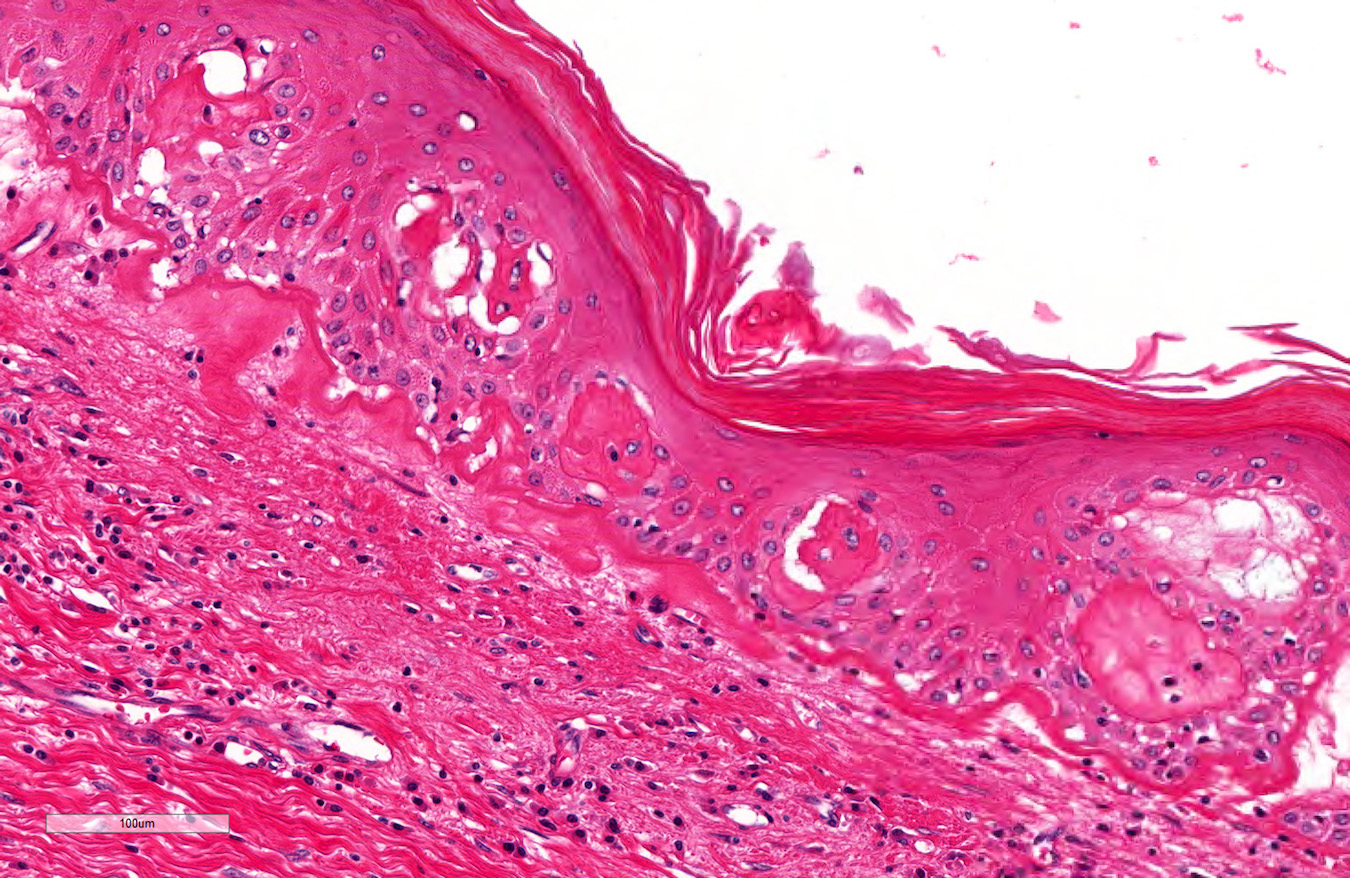
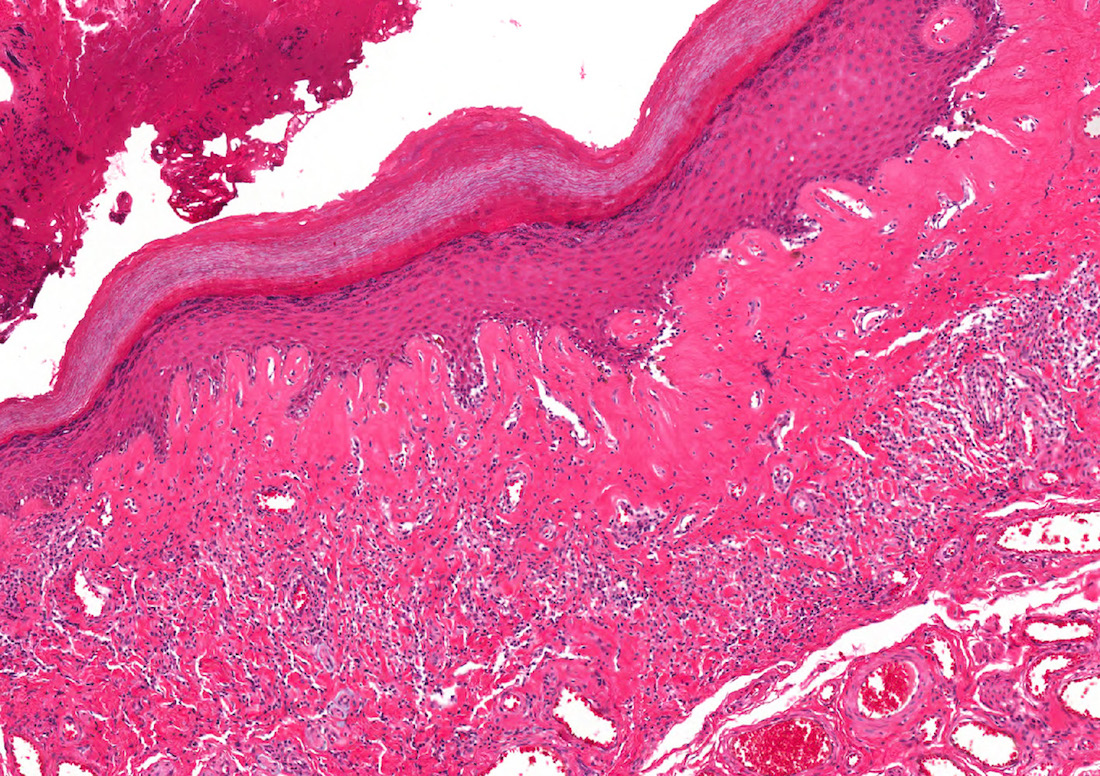
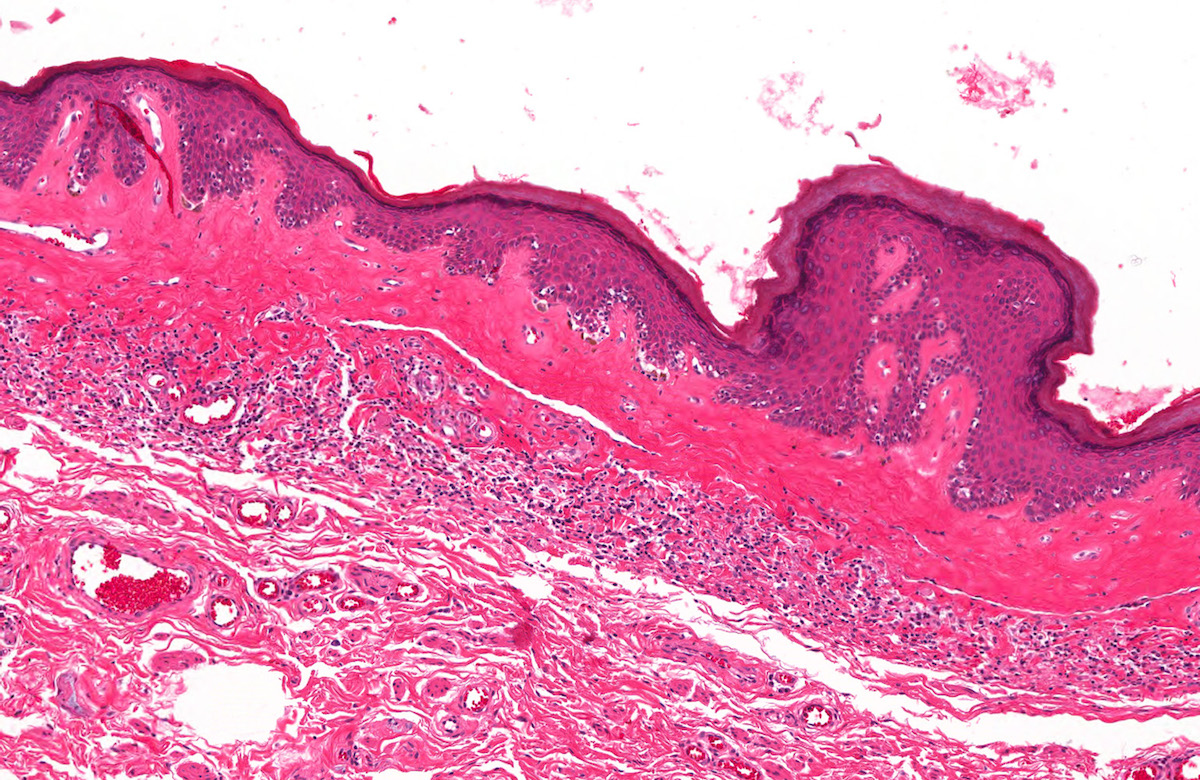
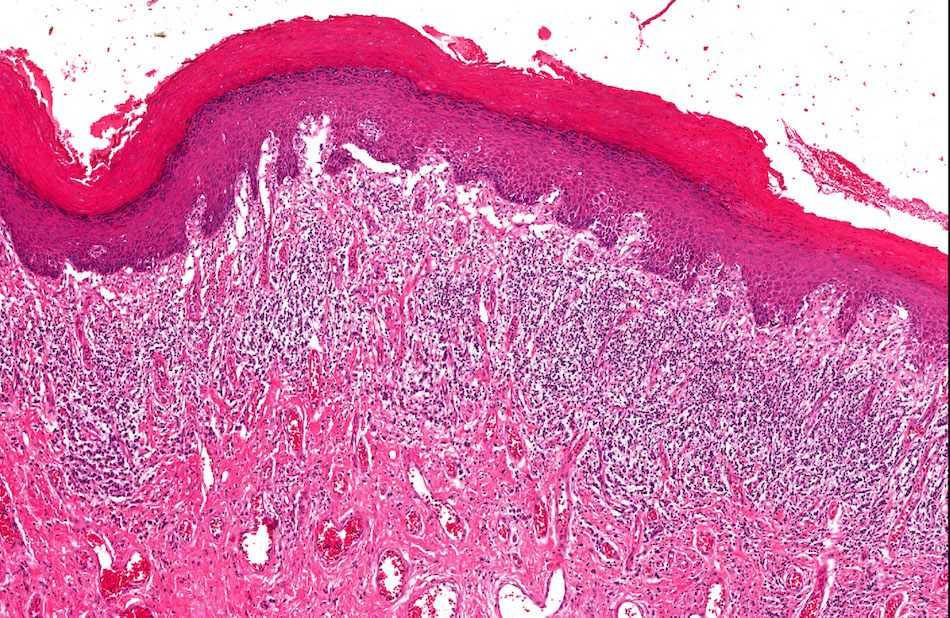
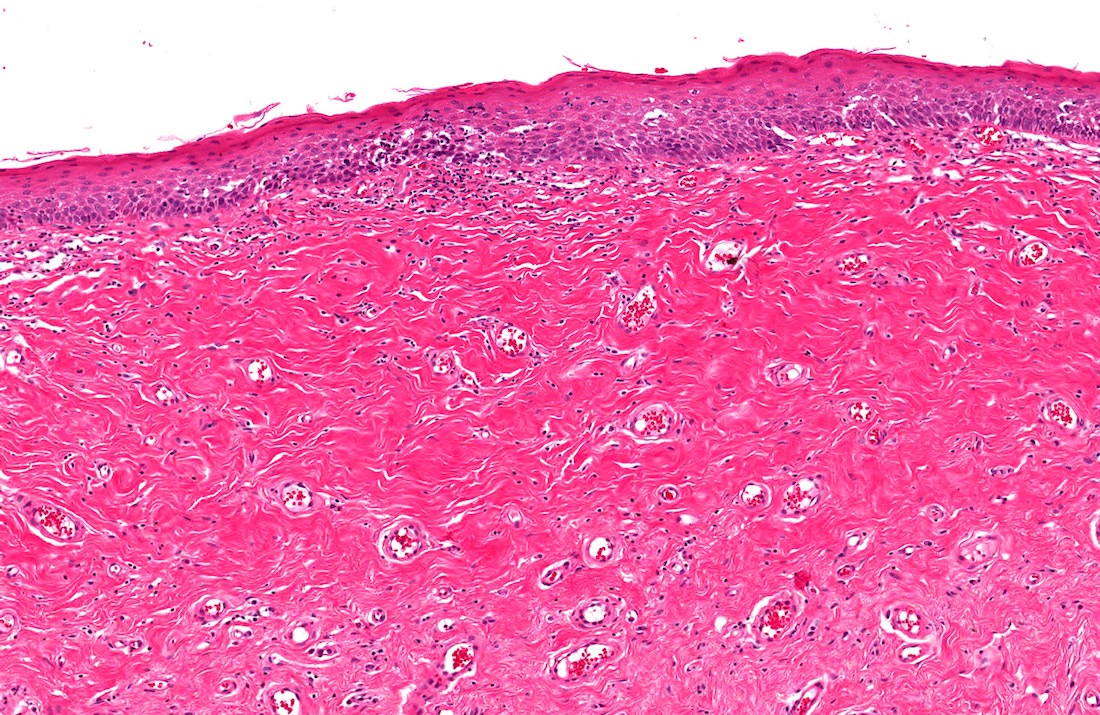
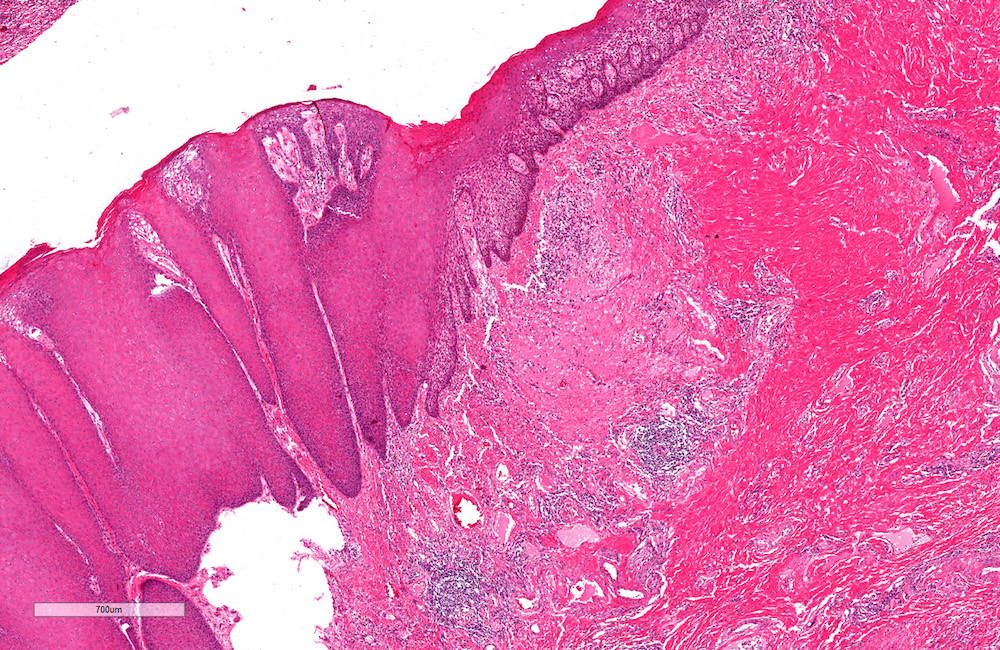
Microscopic (histologic) description
- Topographical evaluation from surface epithelia to deep penile layers (dartos in foreskin and corpus spongiosum in glans) is recommended as follows (Int J Surg Pathol 2020;28:468)
- Squamous epithelium:
- Normal, atrophic or hyperplastic, the latter most common, with more than 10 cell epithelial layers
- Hyperkeratosis associated with hyperplasia
- Vacuolar degeneration of basal layer, landmark lesions in all types of lichen
- Tissue separation at the basal layer, which indices late epithelial ulceration
- Lamina propria:
- Thickening and loss of structures
- Edema, hypervascularity and typically sclerosis
- Distinctive sclerotic patterns
- At the surface: perivascular, globular or linear sclerosis
- Diffuse sclerosis in deeper lamina propria tissues
- Presence of a sclerotic globule is sufficient for diagnosis
- Sclerotic changes spares corpus spongiosum of glans and foreskin dartos
- Lymphocytic infiltration:
- Landmark lesion with variable presentation
- At the interface of epithelium and lamina propria
- Distant from basal layer deep in lamina propria
- Lymphocytes are the basis for subtyping
- Lichenoid: lymphocytes at the basal layer
- Band-like or classic: lymphocyte in deep lamina propria
- Lymphocytic depletion: only few lymphocytes present
- Depletion of lymphocytes is typical of cancer associated lichen sclerosis
- During progression sclerosis increases; fully developed lesions are characterized by:
- Epithelial thinning and ulceration
- Wide hyalinized band in the upper dermis
- Lymphocytic infiltrate below the hyalinized band
- Penile intraepidermal neoplasia and/or carcinoma can be associated
Microscopic (histologic) images
Contributed by Diego F. Sanchez, M.D. and Antonio L. Cubilla, M.D.
Positive stains
- Immunohistochemistry is not needed for diagnosis but can suggest progression to neoplastic lesions
- p53: 40% of cases adjacent to cancer showed positive parabasal cells in other organs (Br J Cancer 2003;89:2249)
- Ki67: positive in basal epithelial cells (J Urol 2013;190:399)
- MCM3 (mini chromosome maintenance 3 protein): positivity in long standing lichen sclerosus and correlates with Ki67 expression (J Urol 2013;190:399)
- CD3, CD4, CD8: T cells marker are positive in the lymphocytic infiltrate (Histopathology 2006;48:730)
Molecular / cytogenetics description
- Some reports regarding RNA expression are (Int J Biol Sci 2019;15:1429):
- Upregulation of miR-155, TNF, IL6, galectin 7, collagen (type I, III, V), p53
- Downregulation of FOXO3, CDKN1B, IL10 and endothelial ECM1
- CDKN2A and p53 epigenomic modifications
Videos
Lichen sclerosus et atrophicus
Sample pathology report
- Foreskin, circumcision:
- Lichen sclerosus (see comment)
- Comment: Epithelial hyperplasia and hyperkeratosis was noted. Scarce lymphocytic infiltrate was seen in the lamina propria and between sclerotic tissue suggesting lymphocytic depleted variant. This subtype has been reported associated with preneoplastic lesions and carcinoma which were not observed in this specimen.
Differential diagnosis
- Lichen planus:
- Dense lymphoid infiltrate is the hallmark
- Absence of hyalinization / sclerosis
- This later can be difficult to differentiate with early lichen sclerosus
- Zoon balanitis:
- Plasma cell balanitis
- Usually absence of granular and cornified layers
- Very rare
Additional references
Board review style question #1
- A 30 year old man went to the urologist complaining about difficulty with coitus. He has a history of untreated phimosis from childhood. At the clinical examination, a buried penis is found. Circumcision is performed and the following image shows the findings. What is your diagnosis?
- Acute postitis
- Amyloidosis
- Lichen planus
- Lichen sclerosus
- Zoon balanitis
Board review style answer #1
D. Lichen sclerosus. Atrophic epithelium, dense hyalinized fibrotic tissue replacing lamina propria and subjacent lymphocytic inflammatory infiltrate.
Comment Here
Reference: Lichen sclerosus (balanitis xerotica obliterans)
Comment Here
Reference: Lichen sclerosus (balanitis xerotica obliterans)
Board review style question #2
- Regarding lichen sclerosus, which of the following is correct?
- Circumcision is always curative
- HPV is the most common etiology
- Immunohistochemistry is needed for accurate diagnosis
- It is associated with neoplastic lesions
- Only seen in anogenital area
Board review style answer #2
D. It is associated with neoplastic lesions. Although it is a benign chronic inflammatory condition, this lesion is associated with non-HPV related PeIN and carcinomas.
Comment Here
Reference: Lichen sclerosus (balanitis xerotica obliterans)
Comment Here
Reference: Lichen sclerosus (balanitis xerotica obliterans)