Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Chapel DB, Husain AN. Well differentiated papillary mesothelial tumor (peritoneum). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/peritoneumwelldiffpapillarymeso.html. Accessed April 23rd, 2024.
Definition / general
- Well differentiated papillary mesothelioma (WDPM) is a neoplastic mesothelial proliferation of low malignant potential, which predominantly involves the peritoneum of young women
Essential features
- Most cases diagnosed incidentally during surgery for an unrelated indication
- Composed of branching papillae lined by a single layer of bland cuboidal mesothelial cells
- Invasion of underlying pre-existing tissues (e.g. fat, muscle, ovarian stroma) precludes the diagnosis (→ diagnosis of malignant mesothelioma)
- BAP1 loss and CDKN2A (p16) homozygous deletion preclude the diagnosis (→ diagnosis of malignant mesothelioma)
Terminology
- Localized mesothelioma (confusing terminology; use not recommended) (Am J Surg Pathol 1995;19:1124)
ICD coding
- ICD-10: D19.9 - Benign neoplasm of mesothelial tissue, unspecified
Epidemiology
- F:M = ~5:1
- Median age at diagnosis: ~40 years (range 7 - 75)
Sites
- Peritoneum is most commonly affected site
- Rare cases involve the pleura or tunica vaginalis (Hum Pathol 2019;92:48, Am J Surg Pathol 2004;28:534)
- Cases in the pleura or tunica vaginalis more evenly distributed between men and women
- Pleural cases diagnosed at older age (median ~60 years)
- Pleural cases have higher rate of asbestos exposure (~50%)
Pathophysiology
- Molecularly distinct from epithelioid malignant peritoneal mesothelioma (Cancers (Basel) 2020;12:E1568)
Etiology
- Asbestos exposure reported in only ~1% (causality not established)
Clinical features
- Most cases (> 90%) incidentally identified during abdominal surgery for an unrelated cause
- Rare florid cases (< 10%) present with abdominal pain, weight loss or ascites
Diagnosis
- Tissue sampling followed by microscopic evaluation
Radiology description
- In patients with florid or symptomatic disease, computed tomography (CT) may show ascites or thickening of the bowel wall or mesentery
Prognostic factors
- Most cases follow a benign clinical course
- Recurrence rate in morphologically classical cases is low (< 5%)
- Recurrence rate reportedly higher in cases with invasive foci in papillary cores and with higher disease burden (Am J Surg Pathol 2014;38:990, Eur J Surg Oncol 2019;45:371)
- Fatal outcomes rare
- Progression to malignant peritoneal mesothelioma is exceptionally rare (< 5%) and causality is unclear (may occur years to decades later)
Case reports
- 28 year old woman with a large peritoneal tumor, presenting with ascites (J Lab Physicians 2018;10:248)
- 48 year old man with a tumor in an inguinal hernia (Indian J Pathol Microbiol 2012;55:546)
Treatment
- Observation
- Surgical cytoreduction and hyperthermic intraperitoneal chemotherapy performed in some cases with diffuse, symptomatic or recurrent disease (Ann Surg Oncol 2019;26:852)
- Randomized clinical trials not available
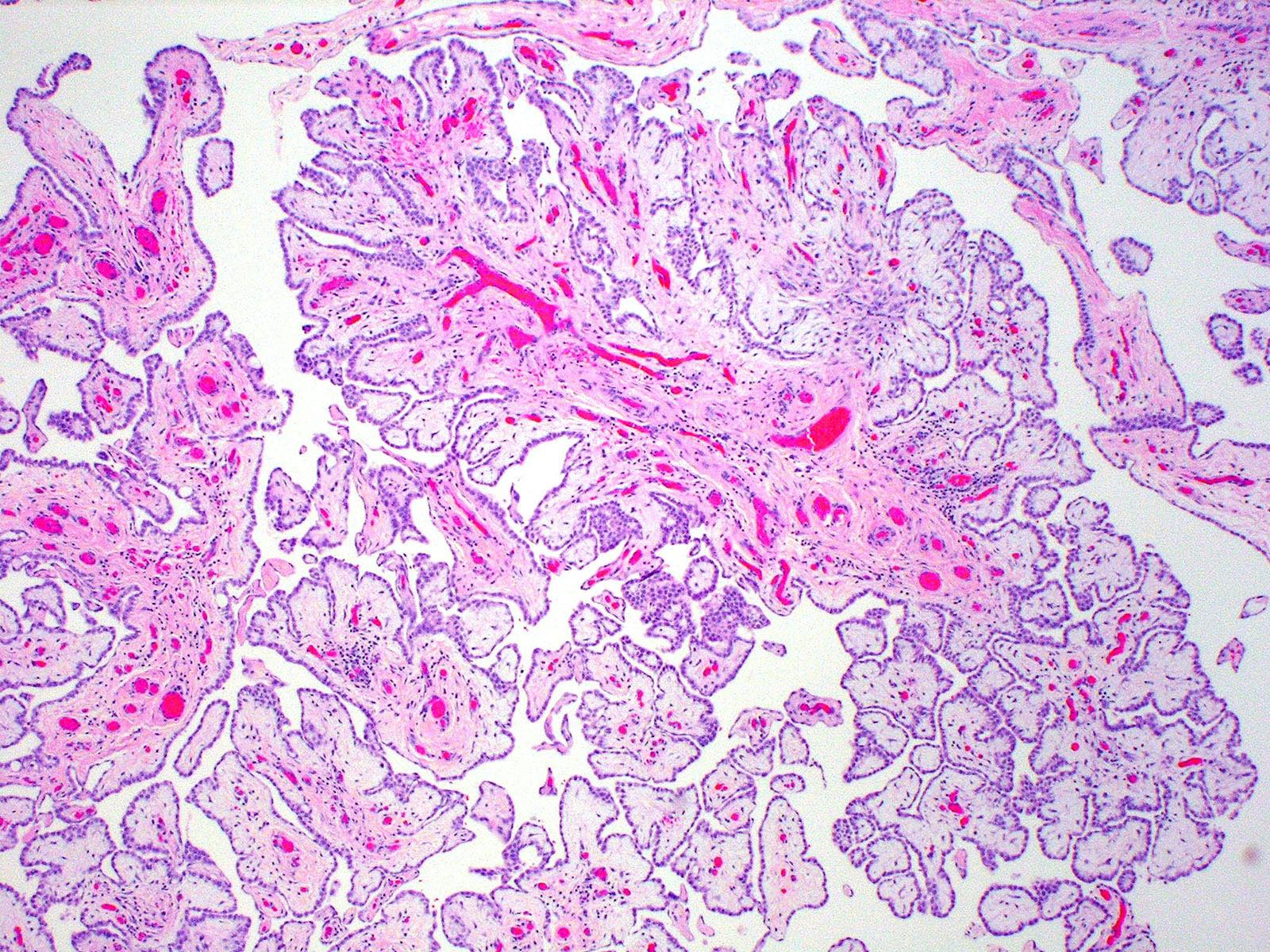
Gross description
- Discrete nodular implants
- Papillary fronds macroscopically evident in some (but not all) cases
- Individual implants usually 0.2 - 2.0 cm but may be up to several centimeters (Am J Surg Pathol 2012;36:117)
- Approximately 50% of cases are unifocal and 50% are multifocal (Ann Diagn Pathol 2019;38:43)
- Ovarian or fallopian tube surface involved in a minority of cases
Gross images
Frozen section description
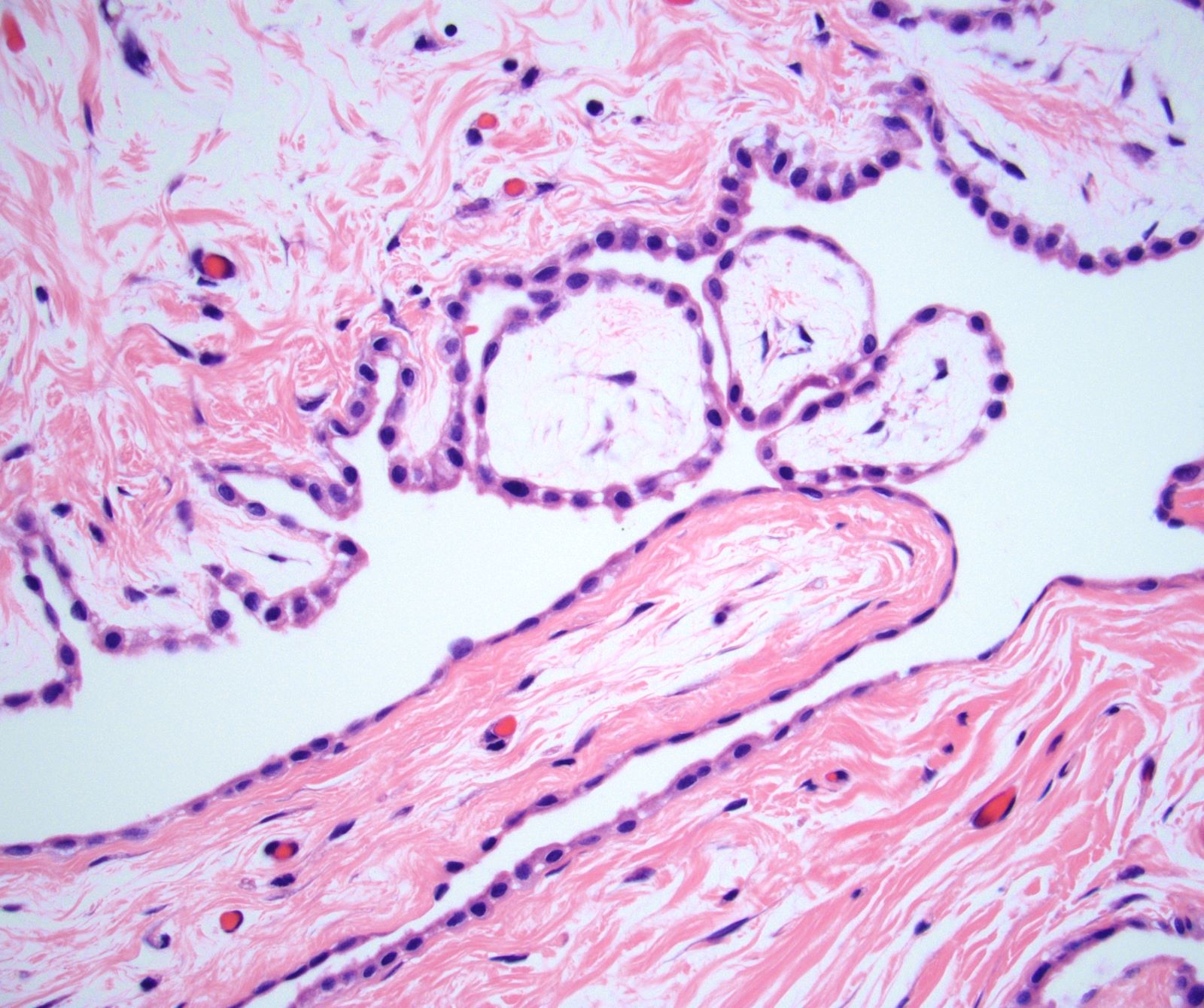
- Papillary architecture (Am J Surg Pathol 2012;36:117)
- Single nonstratified layer of low cuboidal cells with bland cytomorphology
- No solid growth
- No invasion of underlying tissues
- Correlate with surgical findings, re: extent of peritoneal involvement
Frozen section images
- See Virtual slides
Microscopic (histologic) description
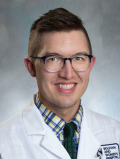
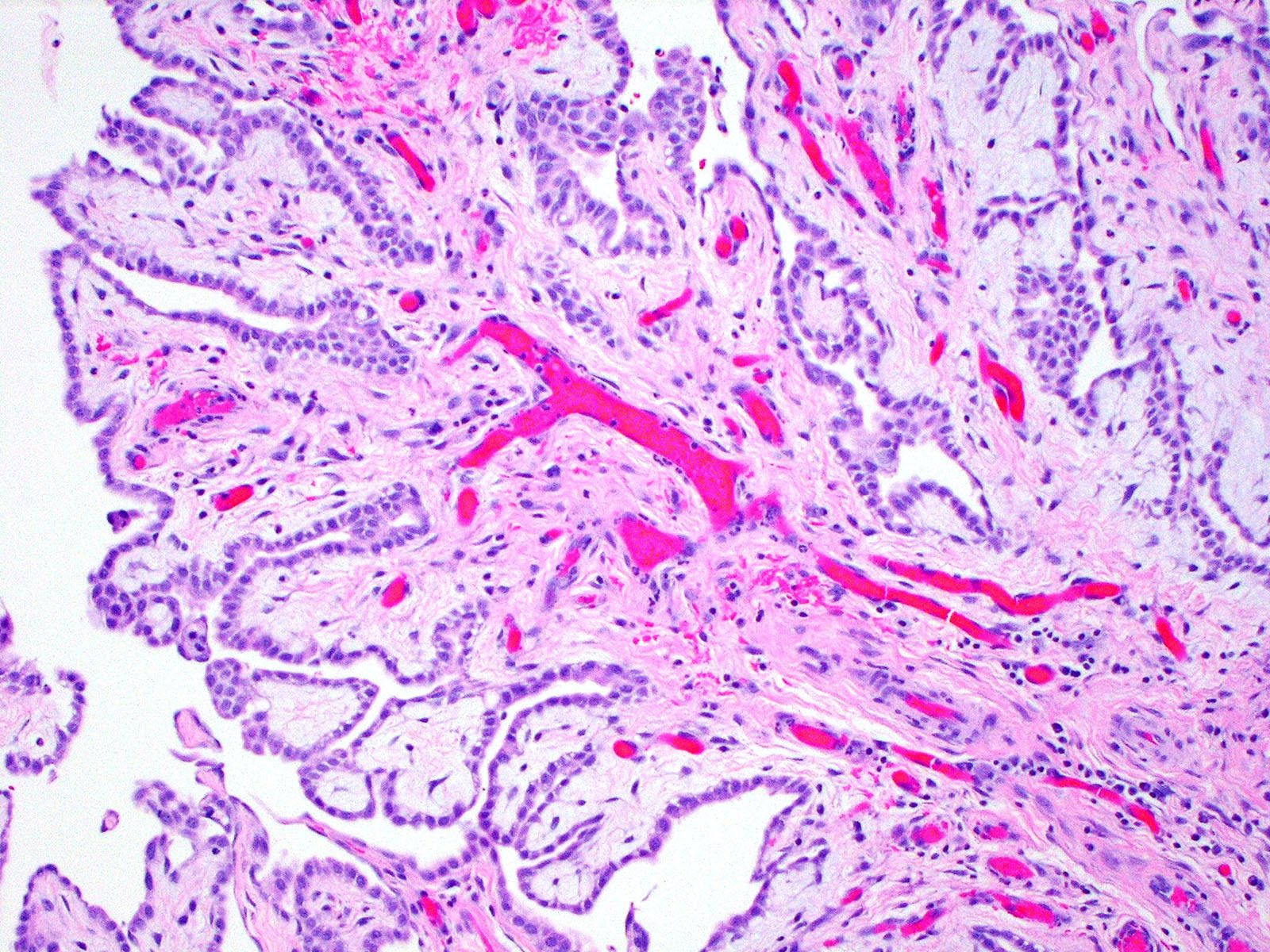
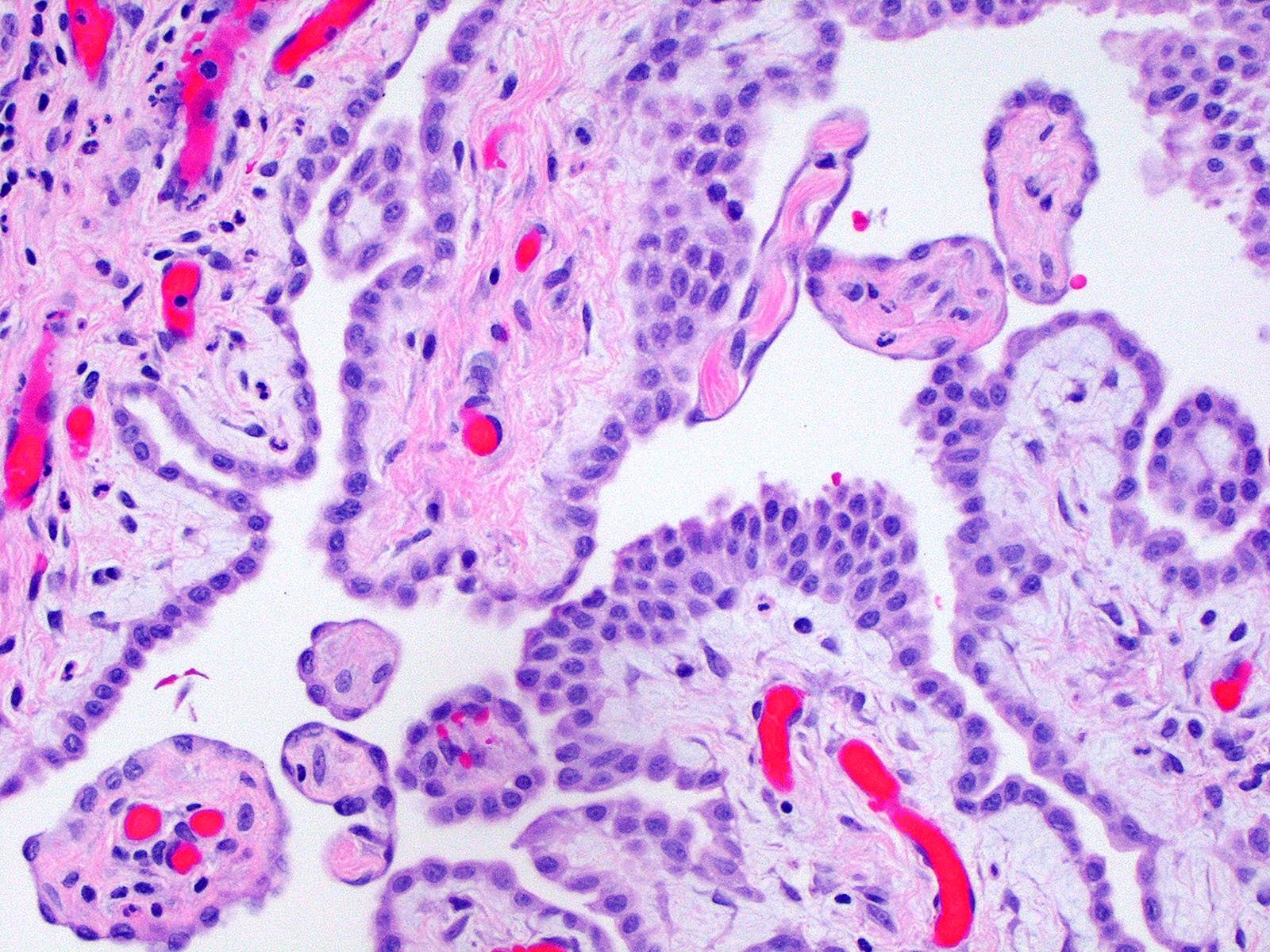
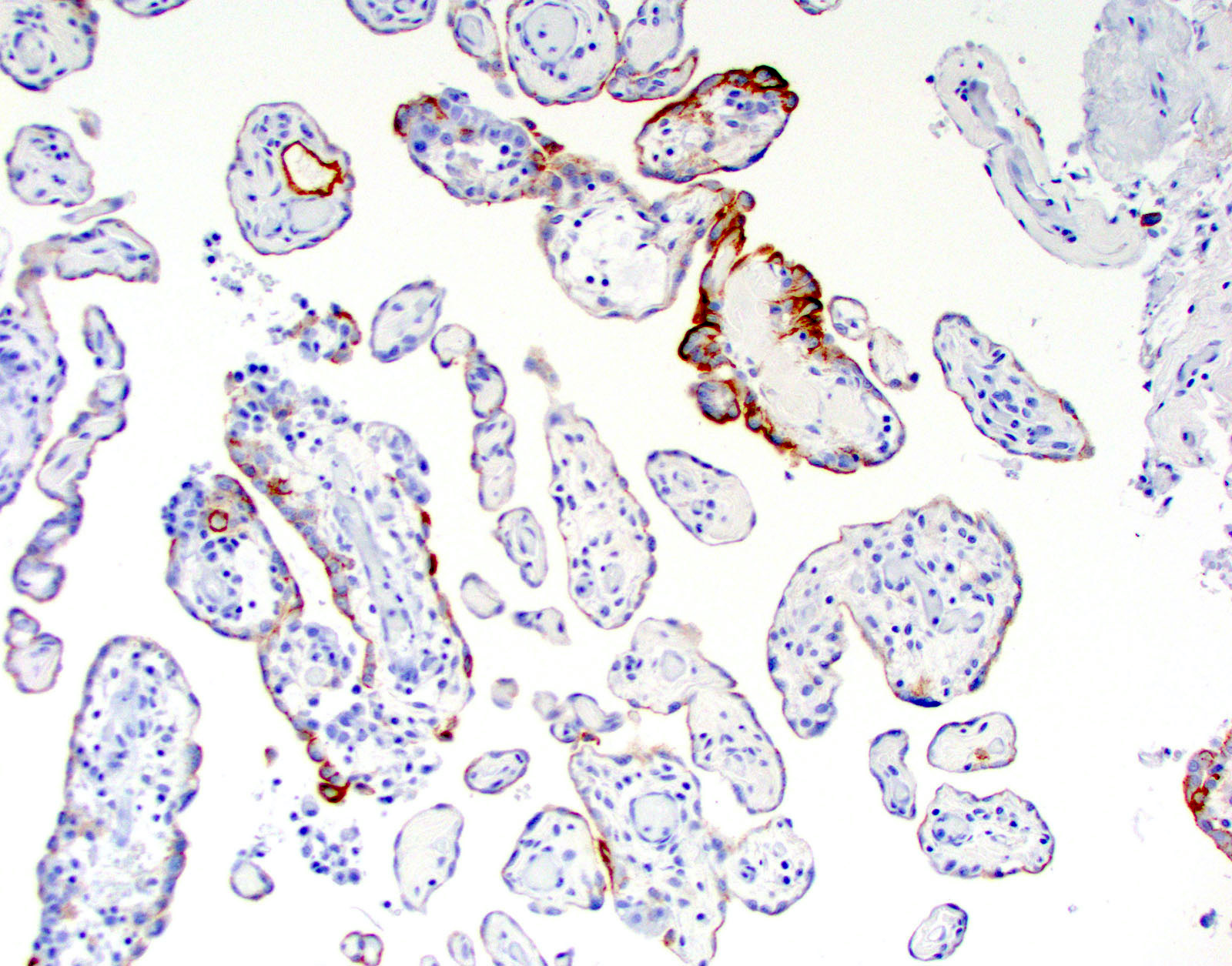
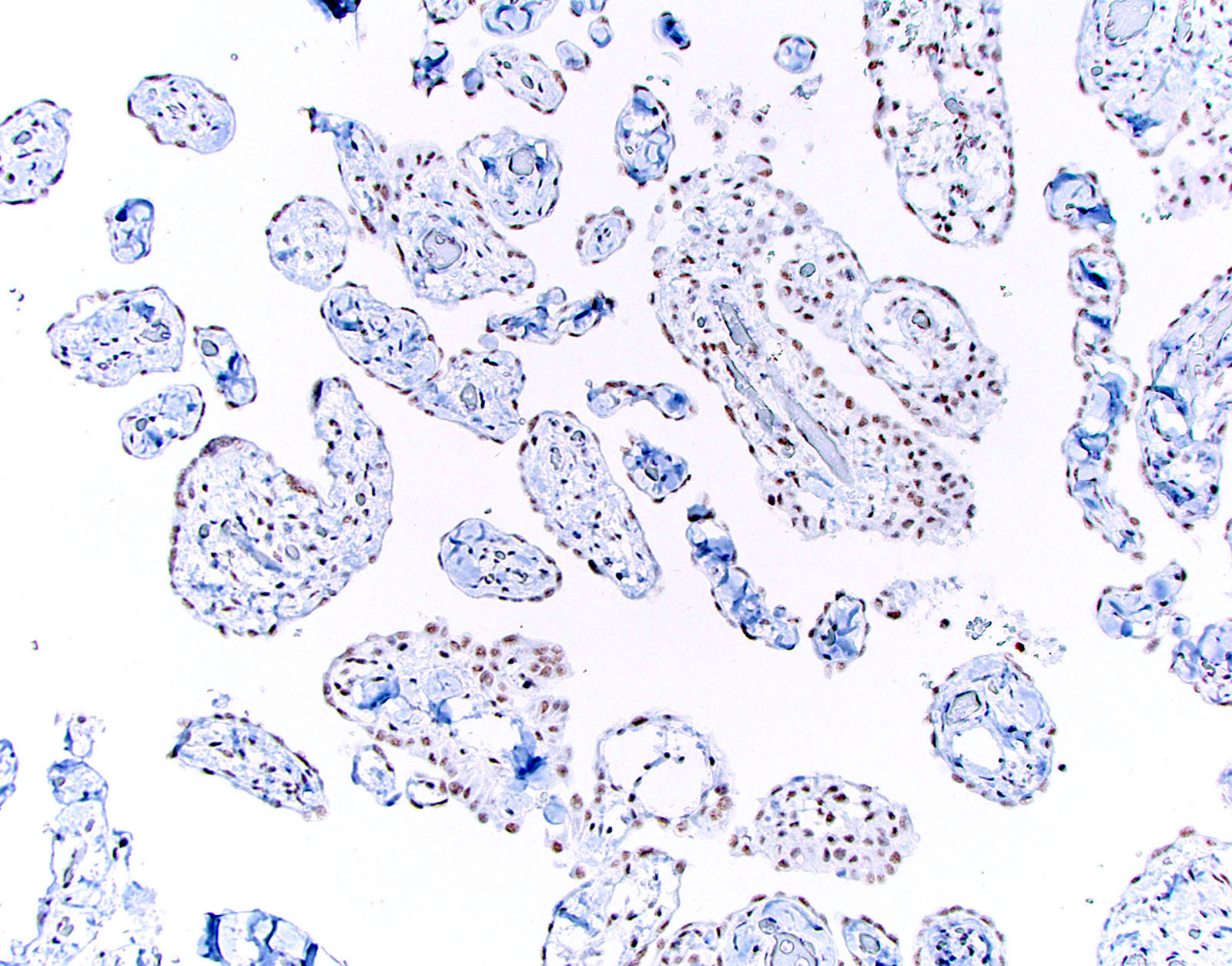
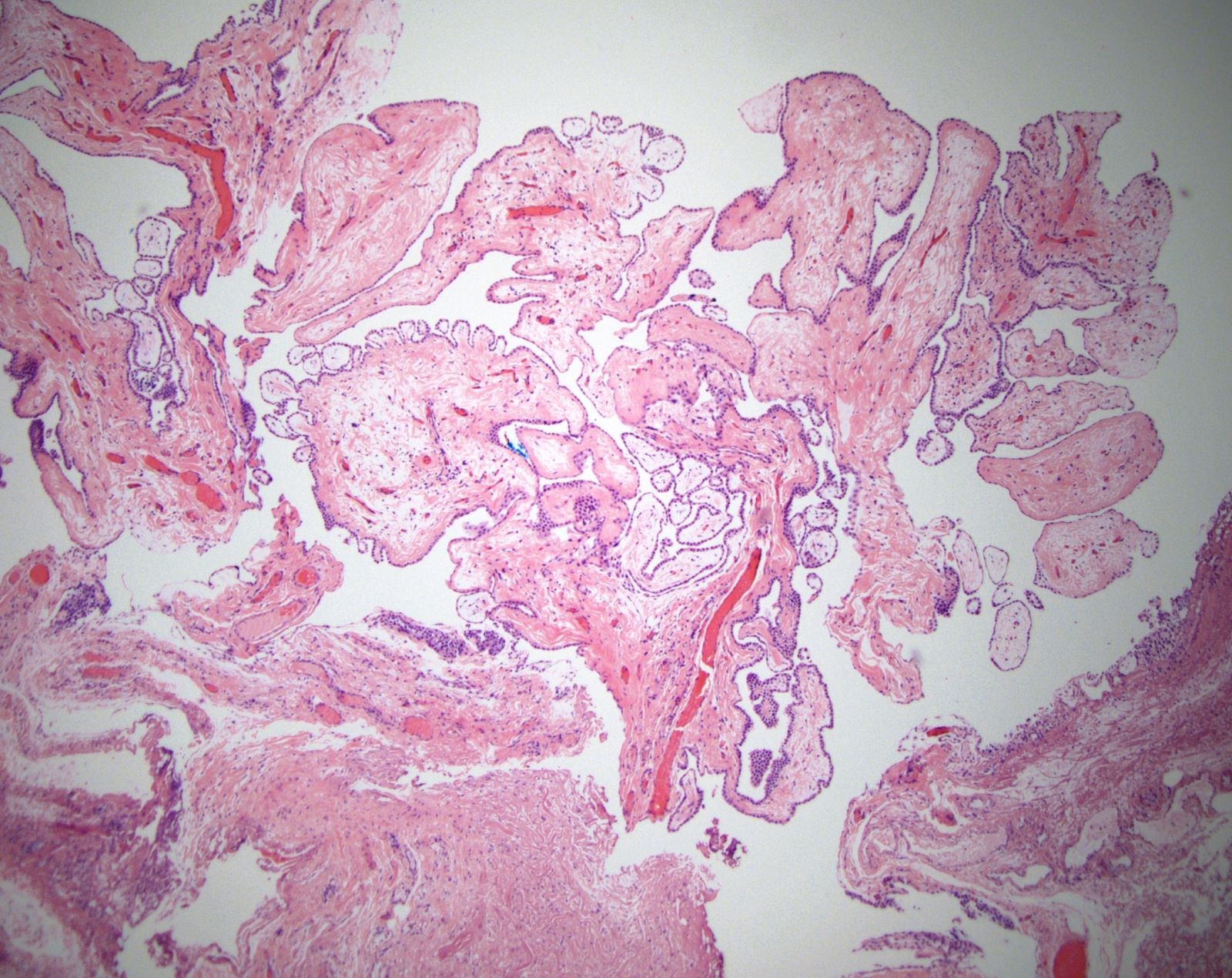
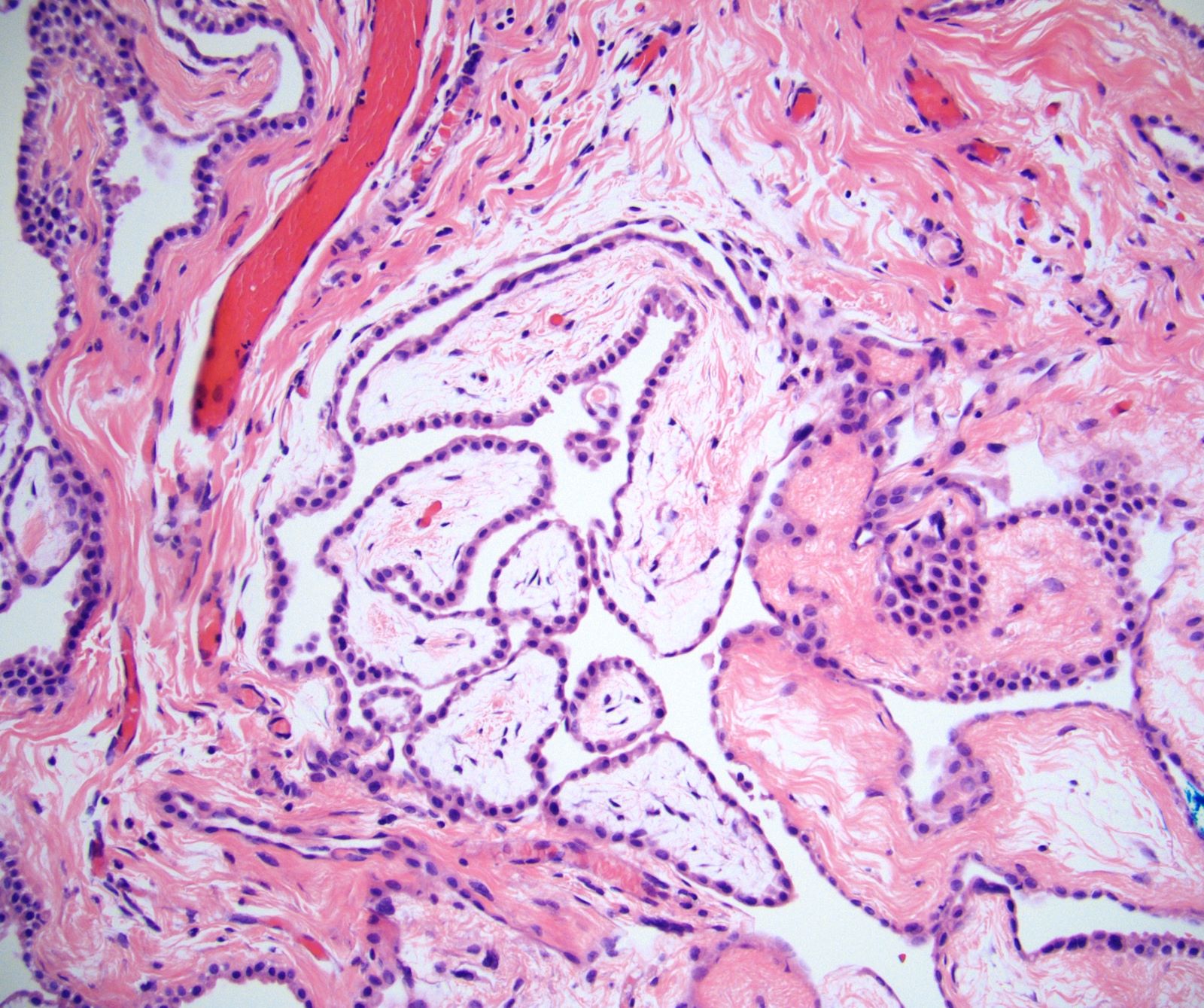
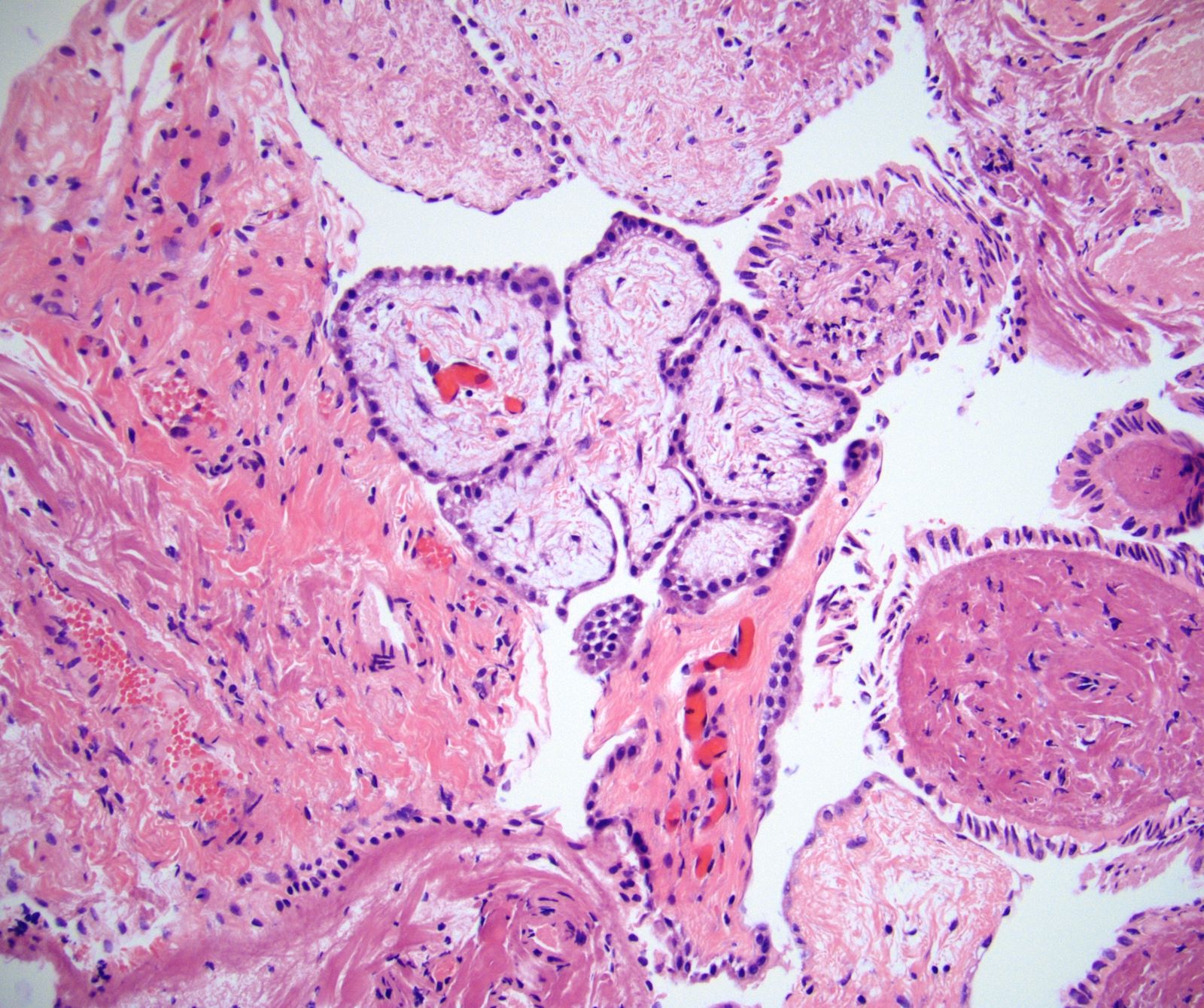
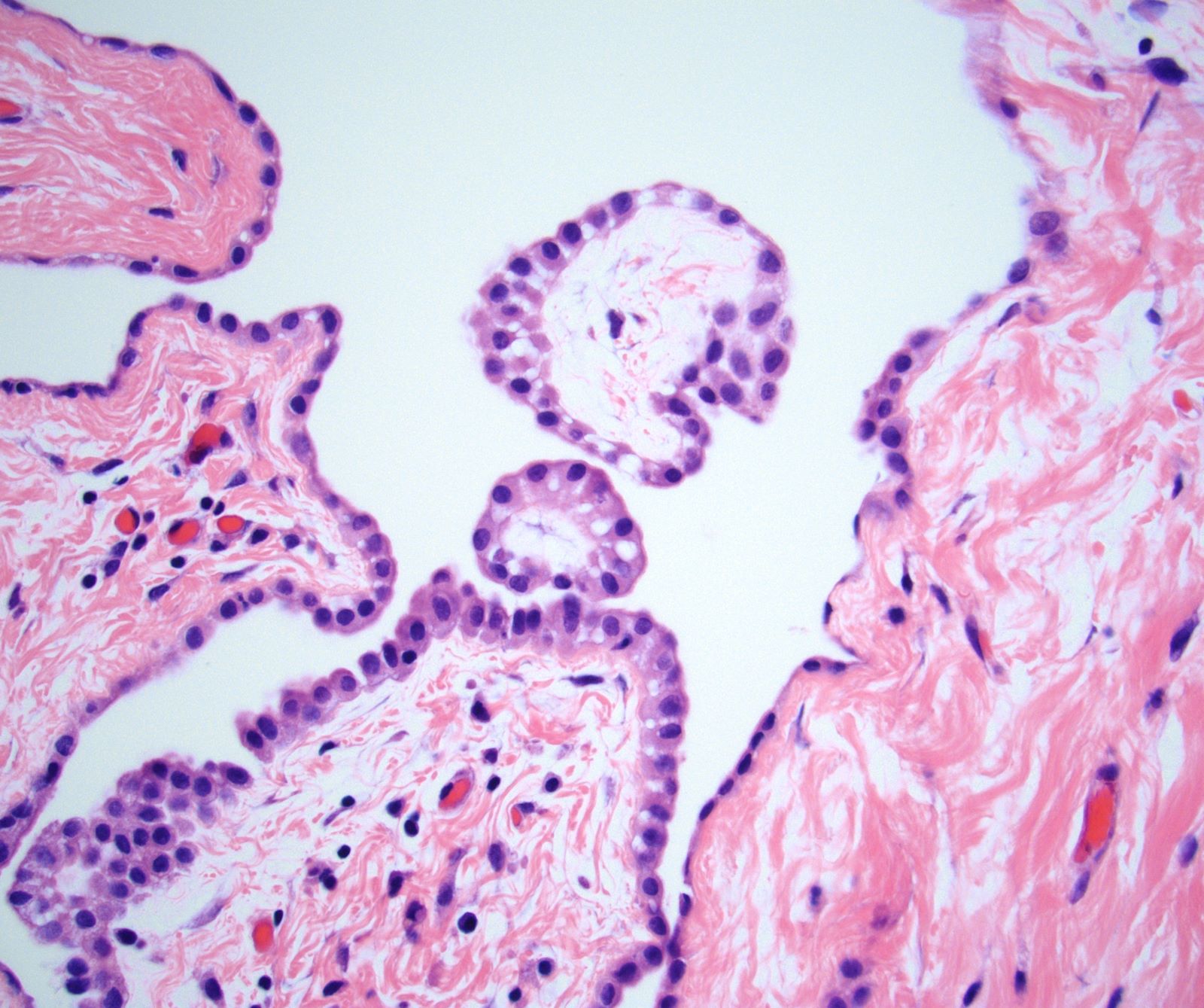
- Branching plump papillae lined by a single layer of bland cuboidal cells (Am J Surg Pathol 2012;36:117, Ann Diagn Pathol 2019;38:43, Histopathology 2013;62:805)
- Minimal cytologic atypia; single small nucleoli may be present
- Mitoses usually absent (or at most 1 mitosis per 10 high power fields)
- Papillary cores may show myxoid change, edema, psammomatous calcifications, fibrosis, foamy macrophages or chronic inflammation
- Invasion of underlying pre-existing tissues is absent
- Unusual patterns
- Some cases associated with a discrete adenomatoid tumor or multicystic mesothelioma (no apparent effect on prognosis)
- Invasive foci composed of tubules, single cells, small solid nests or cords within papillary cores (see Prognostic factors)
Microscopic (histologic) images
Virtual slides
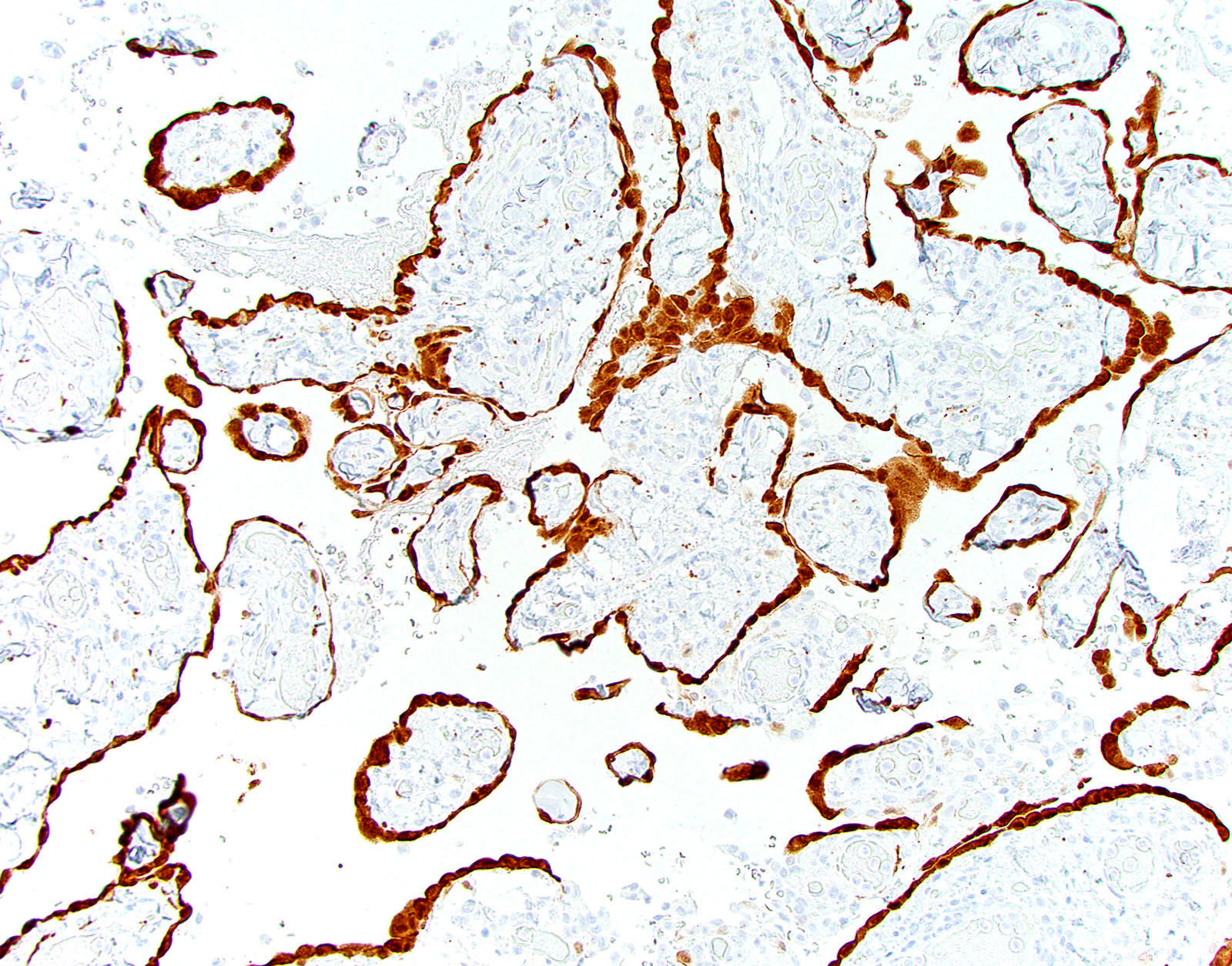
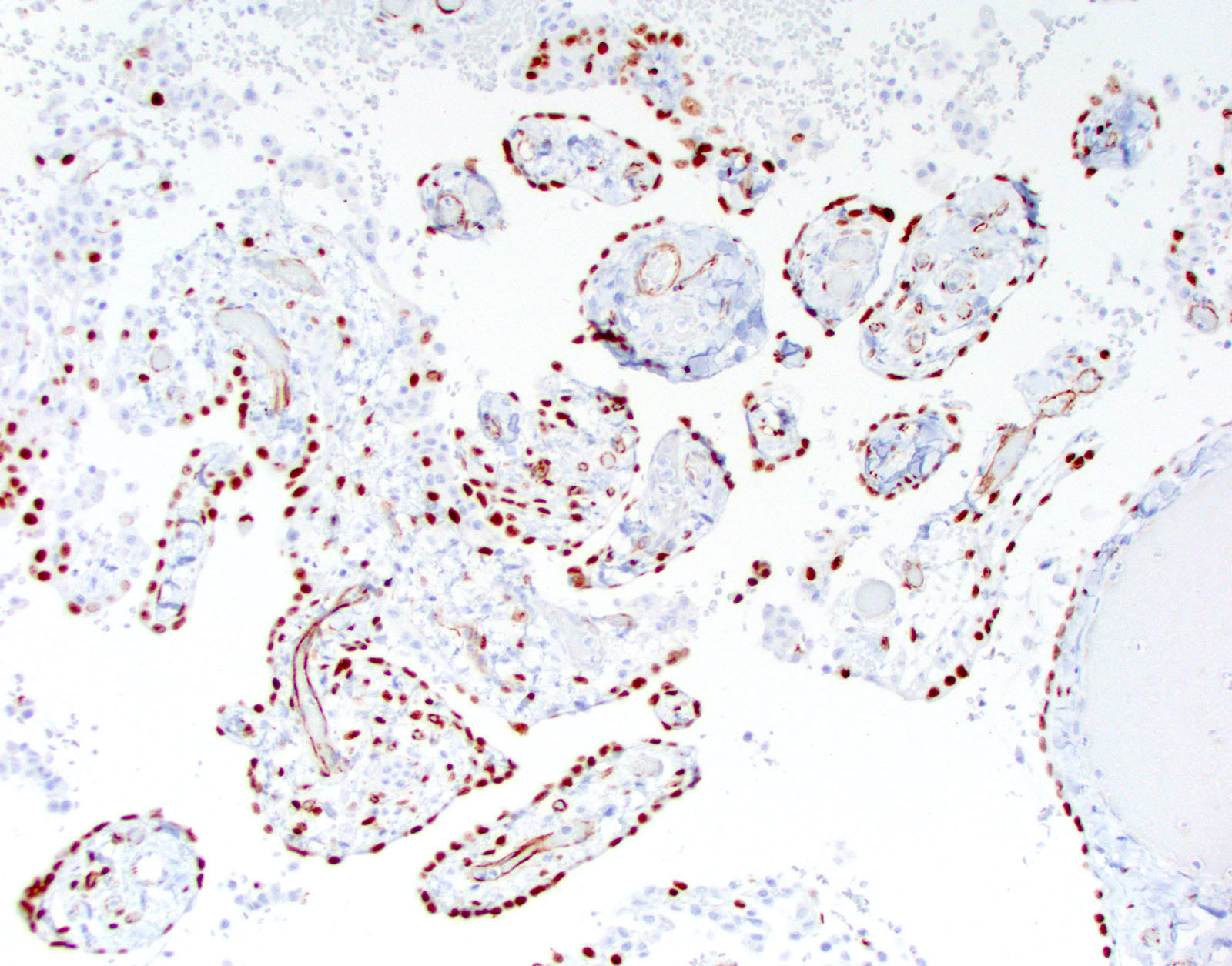
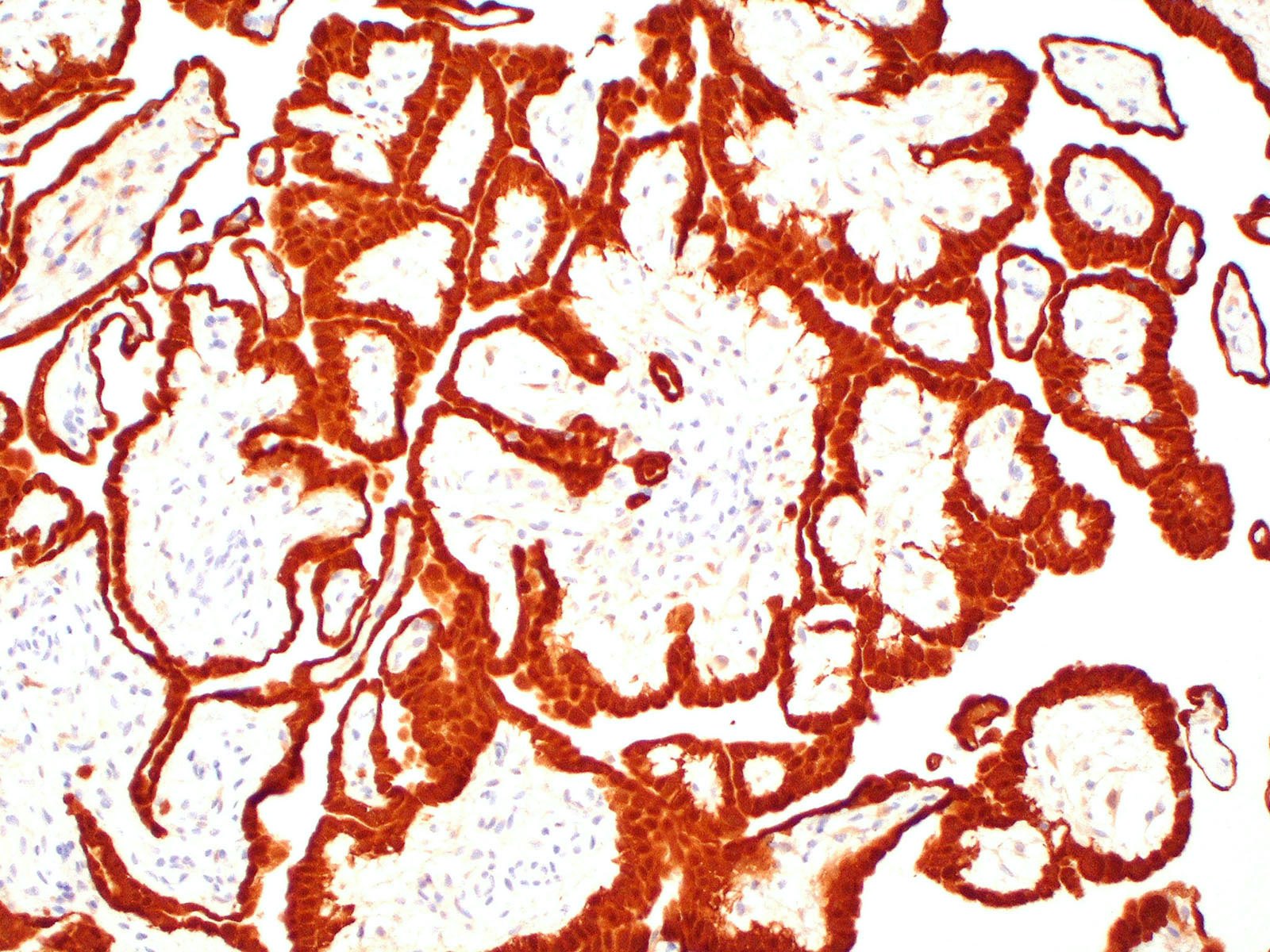
Positive stains
- Broad spectrum cytokeratin (100%)
- Calretinin (virtually 100%) (cytoplasmic + nuclear staining is most specific)
- WT1 (virtually 100%)
- D2-40 (virtually 100%)
- Cytokeratin 5/6 (~90%)
- PAX8 (60 - 95% show at least partial staining) (Hum Pathol 2018;72:160, Ann Diagn Pathol 2019;38:43)
- Ki67 < 5%
- BAP1 retained in virtually all cases (loss strongly suggests malignant mesothelioma with WDPM-like features) (Hum Pathol 2018;79:168)
Negative stains
Electron microscopy description
- Mesothelial cells lining papillary cores show (Am J Surg Pathol 2001;25:1304):
- Long slender microvilli (length to diameter ratio > 10)
- Abundant mitochondria and rough endoplasmic reticulum
- Well formed desmosomes
Molecular / cytogenetics description
- All cases appear to harbor mutation in TRAF7 or CDC42 (Mod Pathol 2019;32:88)
- TRAF7 mutations also found in adenomatoid tumors, suggesting biologic connection
- BAP1 mutation or deletion exceptionally rare
- Lack homozygous CDKN2A (p16) deletion
- Abnormal karyotypes seen in a subset (Am J Surg Pathol 2014;38:990)
Sample pathology report
- Peritoneal nodule, biopsy:
- Well differentiated papillary mesothelioma (0.6 cm) (see comment)
- Comment: Microscopic examination shows branching papillae lined by bland cuboidal mesothelial cells. No mitoses are seen. These morphologic features are consistent with well differentiated papillary mesothelioma. Small unifocal lesions are generally regarded as benign, although recurrences are reported in rare cases. Clinical correlation is advised with appropriate follow up to exclude regrowth or recurrence.
- Peritoneal lesion, excision:
- Well differentiated papillary mesothelioma (2.0 cm) with invasive foci (see comment)
- Comment: Microscopic examination reveals a bland mesothelial lesion with features of well differentiated papillary mesothelioma, including branching papillae lined by a single layer of bland cuboidal mesothelial cells. However, the papillary cores are infiltrated in few foci by nests and cords of bland mesothelial cells. There is no invasion of the underlying peritoneal fibroadipose tissue. Such lesions have been termed "well differentiated papillary mesothelioma with invasive foci" and there is evidence suggesting that such lesions have a higher rate of recurrence compared with banal well differentiated papillary mesothelioma. Clinical and radiographic correlation is advised with appropriate follow up to exclude recurrence.
Differential diagnosis
- Diffuse malignant peritoneal mesothelioma:
- Diffuse involvement of the peritoneum
- Infiltration of underlying pre-existing tissue is typical
- At least moderate cytologic atypia in most cases
- Increased mitotic activity (> 1 mitosis per 10 high power fields is typical)
- Solid architecture may be present
- BAP1 loss frequent (~70%)
- May contain WDPM-like foci so thorough sampling is necessary
- Localized malignant peritoneal mesothelioma:
- Exceptionally rare diagnosis
- Localized disease (resembling WDPM)
- Complex papillary or solid architecture, identical to that seen in diffuse malignant peritoneal mesothelioma
- At least moderate cytologic atypia in most cases
- Increased mitotic activity (> 1 mitosis per 10 high power fields is typical)
- May contain WDPM-like foci so thorough sampling is necessary
- Reactive mesothelial hyperplasia:
- History of surgery, inflammatory disease or cardiovascular disease
- Reactive or inflammatory changes also seen in adjacent flat serosa
- Serous borderline tumor:
Additional references
Board review style question #1
The unifocal lesion depicted in the photomicrograph was discovered incidentally during an exploratory laparoscopy in a 38 year old woman with endometriosis. It measured 0.6 cm on gross examination. On immunohistochemical stains, lesional cells were positive for calretinin (shown above) but negative for MOC31. Which of the following is true about the depicted entity?
- Immunohistochemical loss of BAP1 is seen in ~70% of cases
- Men are more frequently affected than women
- Most cases are causally linked to asbestos exposure
- Most cases of this entity result in patient death within 10 years
- WT1 expression is seen in virtually 100% of cases
Board review style answer #1
E. WT1 expression is seen in virtually 100% of cases. This is a well differentiated papillary mesothelioma.
Comment Here
Reference: Well differentiated papillary mesothelioma
Comment Here
Reference: Well differentiated papillary mesothelioma
Board review style question #2
Which of the following molecular alterations is most frequently seen in well differentiated papillary mesothelioma of the peritoneum?
- BAP1 missense mutation
- CDKN2A homozygous deletion
- NF2 homozygous deletion
- TP53 missense mutation
- TRAF7 mutation
Board review style answer #2