Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Mendoza R, Lanjewar S, Gupta R. Epithelioid trophoblastic tumor. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/placentaETT.html. Accessed April 25th, 2024.
Definition / general
- Epithelioid trophoblastic tumor (ETT) is a very rare gestational trophoblastic tumor derived from neoplastic chorionic type intermediate trophoblasts
Essential features
- Histologic features include nodular and expansile growth pattern of nests and cords of relatively uniform tumor cells with distinct cell borders, moderate eosinophilic to clear cytoplasm and associated extracellular eosinophilic, hyaline-like material
- Presence of decidualized stromal cells in the periphery is a useful diagnostic clue
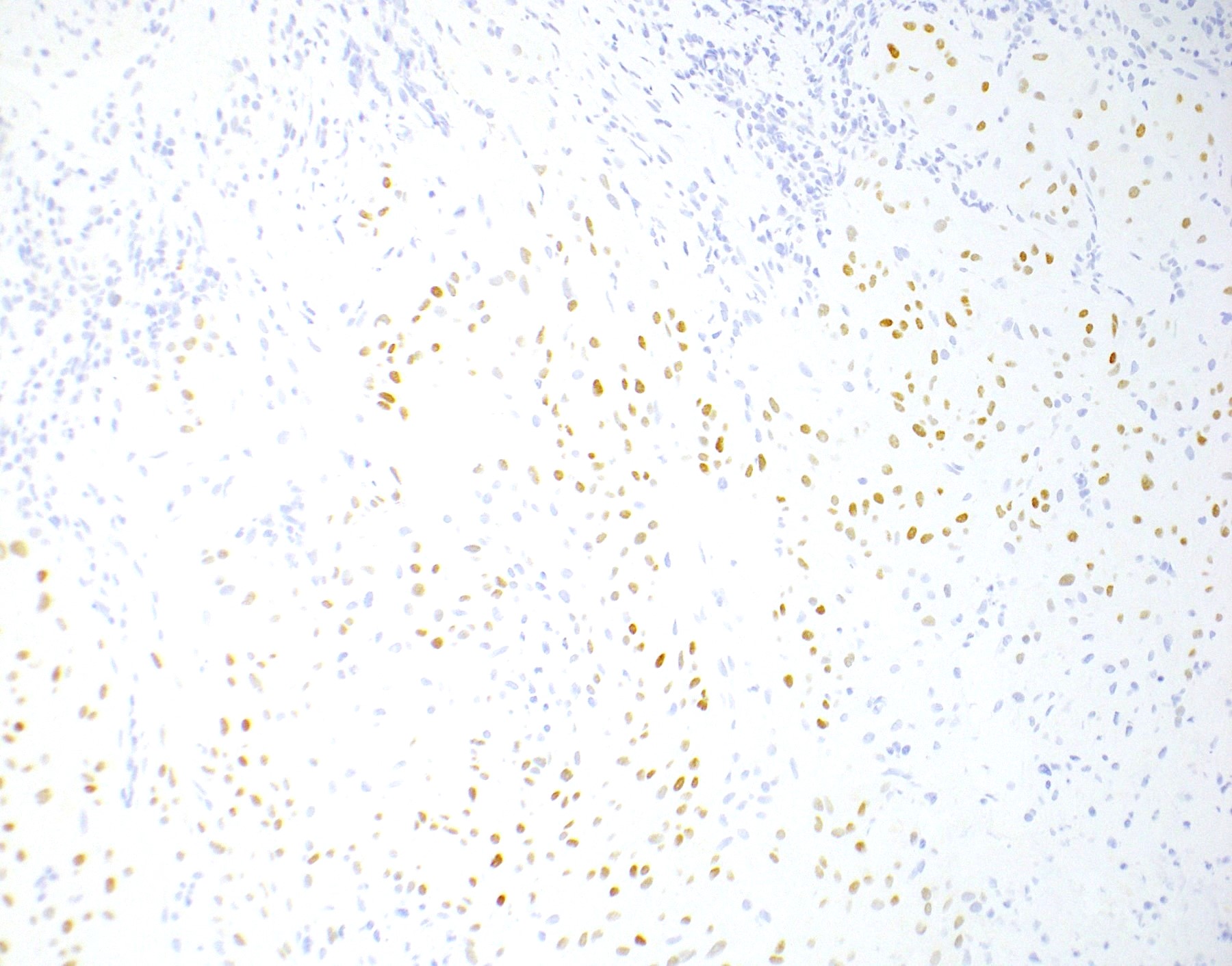
- Diffuse immunohistochemical expression of p63 with essentially negative human placental lactogen (HPL) can help differentiate from placental site trophoblastic tumor
ICD coding
Epidemiology
- Usually occurs in women of 15 - 48 years of age (mean, 36.1 years) (Am J Surg Pathol 1998;22:1393, Mod Pathol 2006;19:75)
- May also be observed in premenopausal and postmenopausal women (Int J Gynecol Cancer 2003;13:551, Int J Gynecol Pathol 2020;39:8)
- 1 - 2% of gestational trophoblastic neoplasms (Am J Obstet Gynecol 2011;204:11)
Sites
- Uterus: 50% of cases arise from uterine cervix or lower uterine segment (Am J Surg Pathol 1998;22:1393, Mod Pathol 2006;19:75)
- Rarely can arise in extrauterine locations: vagina, fallopian tube, ovary and pelvic peritoneum (Pathology 2003;35:136, Indian J Pathol Microbiol 2008;51:242, Int J Gynecol Cancer 2008;18:843)
- Distant metastasis in 25% of patients: lungs (most common) liver, gallbladder, kidney, pancreas and spine (Am J Surg Pathol 2009;33:1809, Gynecol Oncol 2008;108:452, Spine (Phila Pa 1976) 2010;35:E1072, Int J Gynecol Pathol 2000;19:381, Int J Gynecol Cancer 2013;23:1334)
Etiology
- This tumor arises from malignant transformation of intermediate trophoblastic cells of chorionic laeve (Arch Pathol Lab Med 2019;143:65, Am J Surg Pathol 1998;22:1393)
- Epithelioid trophoblastic tumor is most commonly associated with antecedent term pregnancy in 67% of cases but can also follow spontaneous abortions (16%) and hydatidiform moles (16%) (Am J Surg Pathol 1998;22:1393, Am J Surg Pathol 2004;28:405)
Clinical features
- Vaginal bleeding or menometrorrhagia is the most common symptom but amenorrhea can also occur (Mod Pathol 2006;19:75)
- Latency ranges from 2 months to 15 years, with an average of 6.2 years; median interval of 32 months (Mod Pathol 2006;19:75, Int J Gynecol Cancer 2003;13:551)
Diagnosis
- Imaging
- Clinical laboratory
- Histopathologic diagnosis on biopsy or resection specimen
Laboratory
- Mild to moderate elevation of serum hCG of < 2500 mIU/mL is detectable in 80% of cases (Mod Pathol 2006;19:75, J Reprod Med 2008;53:465)
Radiology description
- On ultrasound, it may appear as lobulated, echolucent or echogenic mass with intratumoral, scattered, branching vascularity and turbulent blood flow on color flow Doppler (Ultrasound Obstet Gynecol 2010;36:249)
- Metastatic lesions may appear as mildly enhancing nodules on CT scan with clear boundaries and less uniform echoes (J Med Case Rep 2020;14:178)
- MRI shows heterogeneously enhancing tumor with moderate hypointense signal on T1
Radiology images
Prognostic factors
- Metastasis is seen in 25% of patients (Am J Surg Pathol 1998;22:1393)
- Survival rate of 87 - 90% (Am J Surg Pathol 1998;22:1393, Am J Surg Pathol 2009;33:1809)
- Poor prognosis is associated with:
- FIGO stage IV disease (Int J Gynecol Cancer 2013;23:1334)
- Interval between antecedent pregnancy and diagnosis of > 4 years or > 120 months (Gynecol Oncol 2015;137:456, J Cancer 2019;10:11)
- Beta hCG levels > 1000 IU/L (J Cancer 2019;10:11)
- Mitotic count more than 5 per 10 high power fields (Obstet Gynecol Sci 2017;60:124)
Case reports
- 31 year old gravida 1 para 0 woman with lung mass and low level serum hCG elevation 2 years after early pregnancy loss (Medicine (Baltimore) 2019;98:e14010)
- 36 year old gravida 5 para 3 woman with mass in Cesarean scar defect (Gynecol Oncol Rep 2021;36:100715)
- 36 year old gravida 1 para 1 woman with thickened endometrium and uterine cavity mass in hysteroscopy (Transl Cancer Res 2020;9:2037)
- 40 year old gravida 4 para 2 woman with keratoacanthoma-like nodules as first presentation of widely metastatic disease (Dermatol Online J 2019;25:13030)
- 44 year old gravida 1 para 1 woman with vaginal bleeding and lower abdominal pain 12 years after last pregnancy (Clin Pract 2021;11:631)
Treatment
- Surgical resection is the definitive treatment
- Multi agent chemotherapy after surgery in metastatic disease (J Cancer 2019;10:11):
- FAEV (5-fluorouracil, actinomycin-D, etoposide and vincristine)
- EMA / CO (etoposide, methotrexate, actinomycin-D / cyclophosphamide and vincristine)
- EMA / EP (etoposide, methotrexate, actinomycin-D / etoposide and cisplatin)
- Recent benefit seen with administration of PD-1 / PDL1 immune checkpoint inhibitors (i.e., pembrolizumab) (Gynecol Oncol Rep 2021;37:100819)
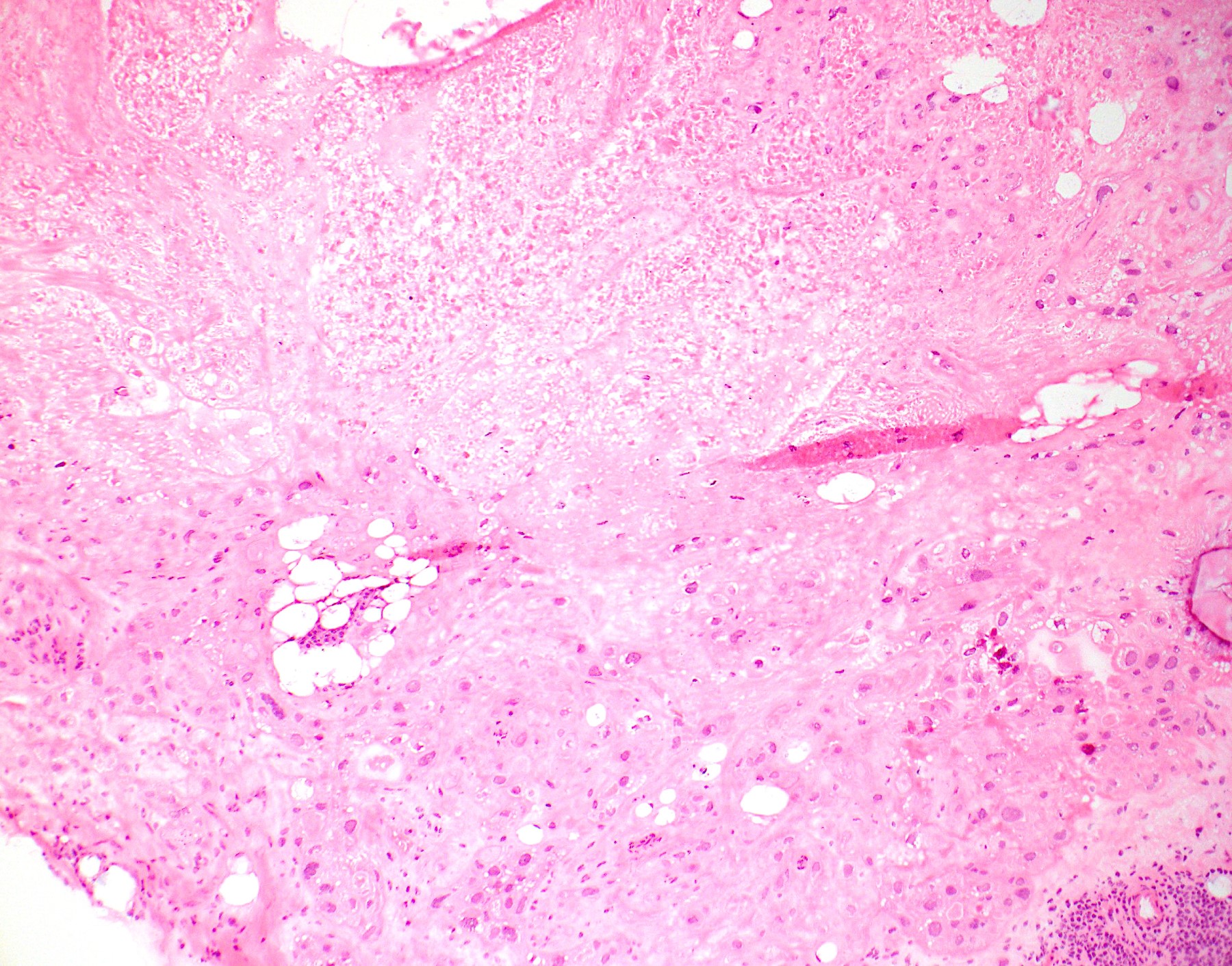
Gross description
- Tumor presents as an expansile mass with white yellowish fleshy, solid appearance on cut surface and invades the underlying stroma
- Necrosis and hemorrhage may also be present
- Ulceration and fistula formation is common
Gross images
Frozen section description
- Nests and cords of epithelioid cells with eosinophilic to clear cytoplasm, distinct cell borders, moderate cytologic atypia and frequent mitosis; set in a hyaline matrix
- Associated with geographic necrosis, apoptotic cells, focal calcifications and scattered decidualized stromal cells in the periphery
- May be mistaken for squamous cell carcinoma
Frozen section images
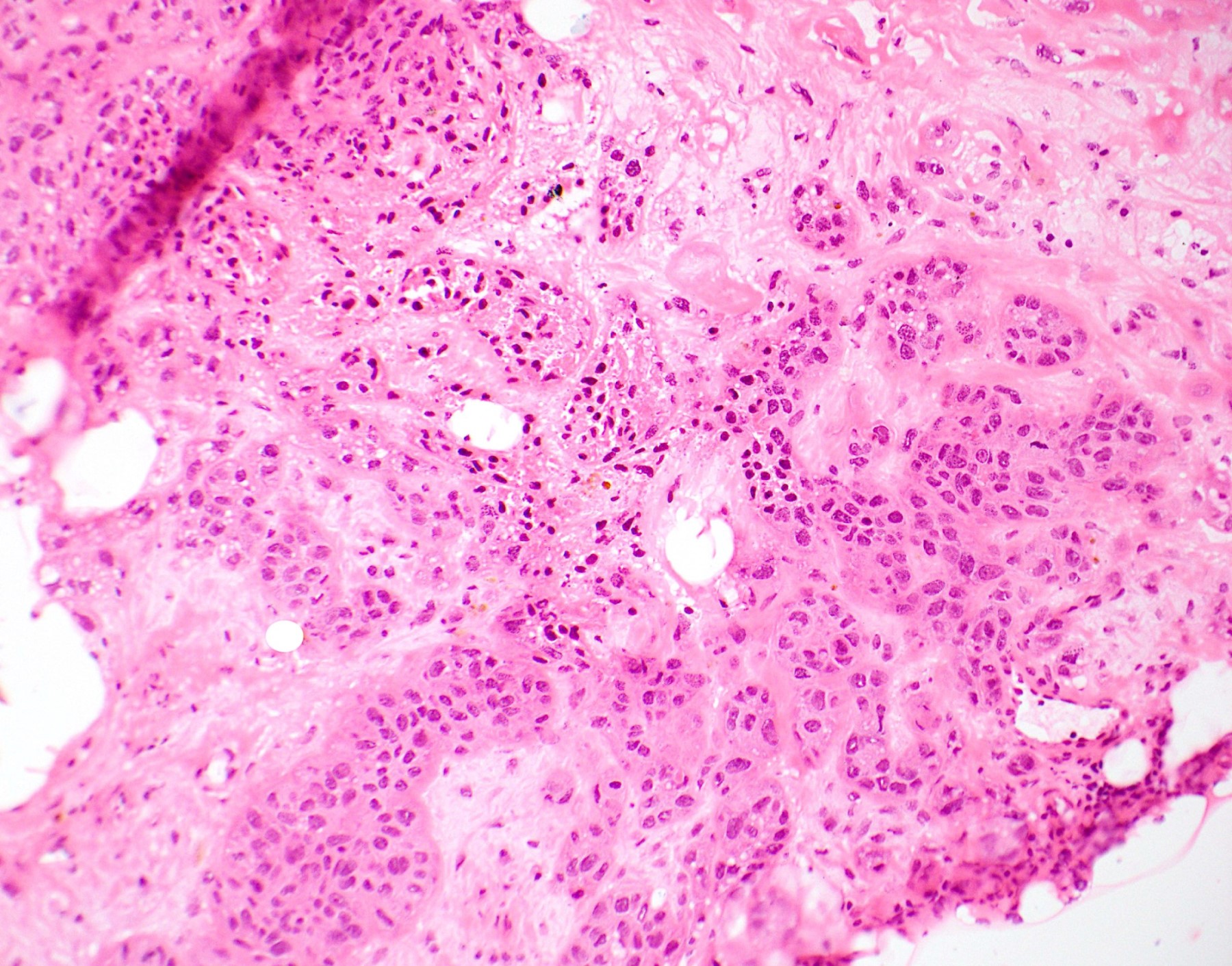
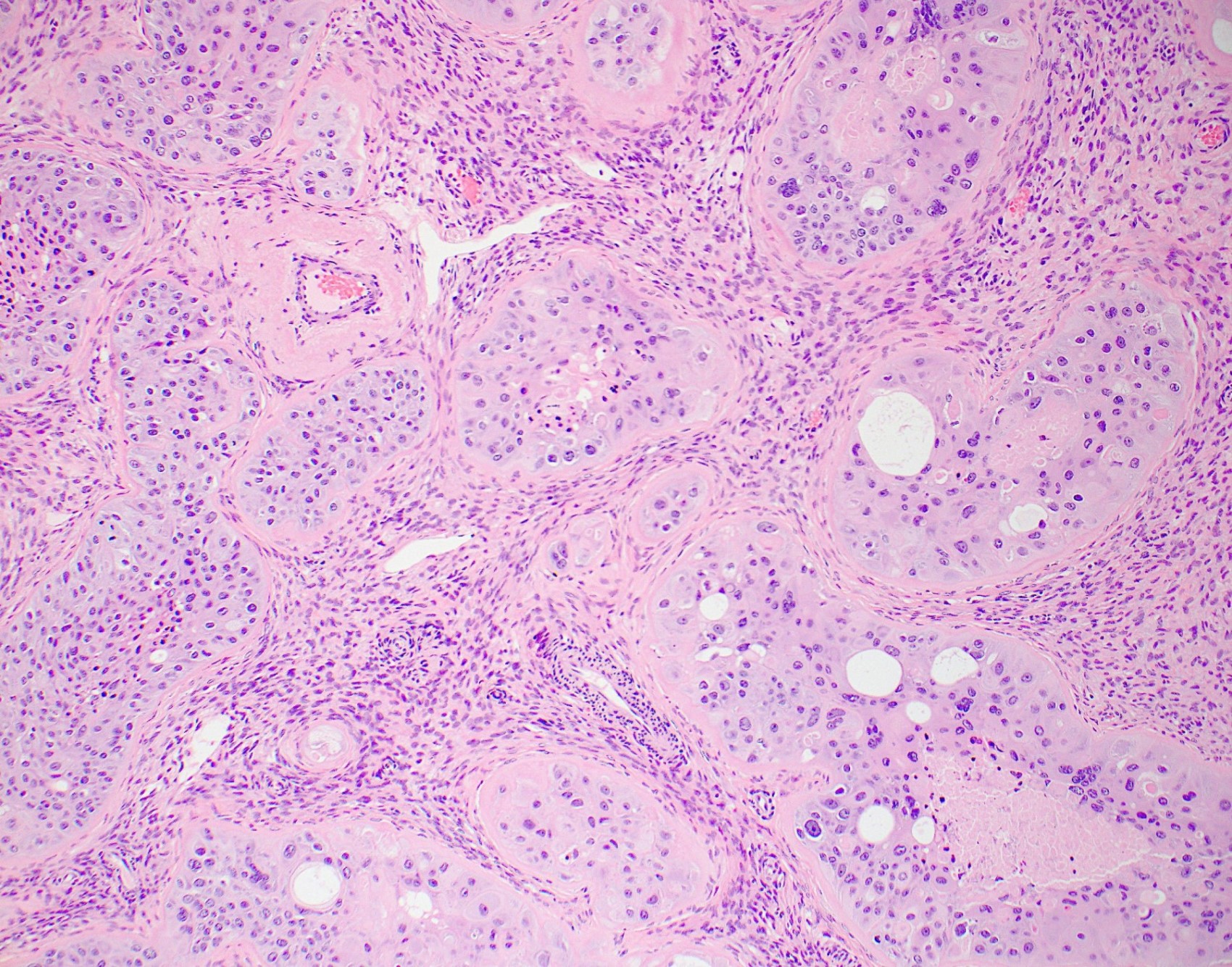
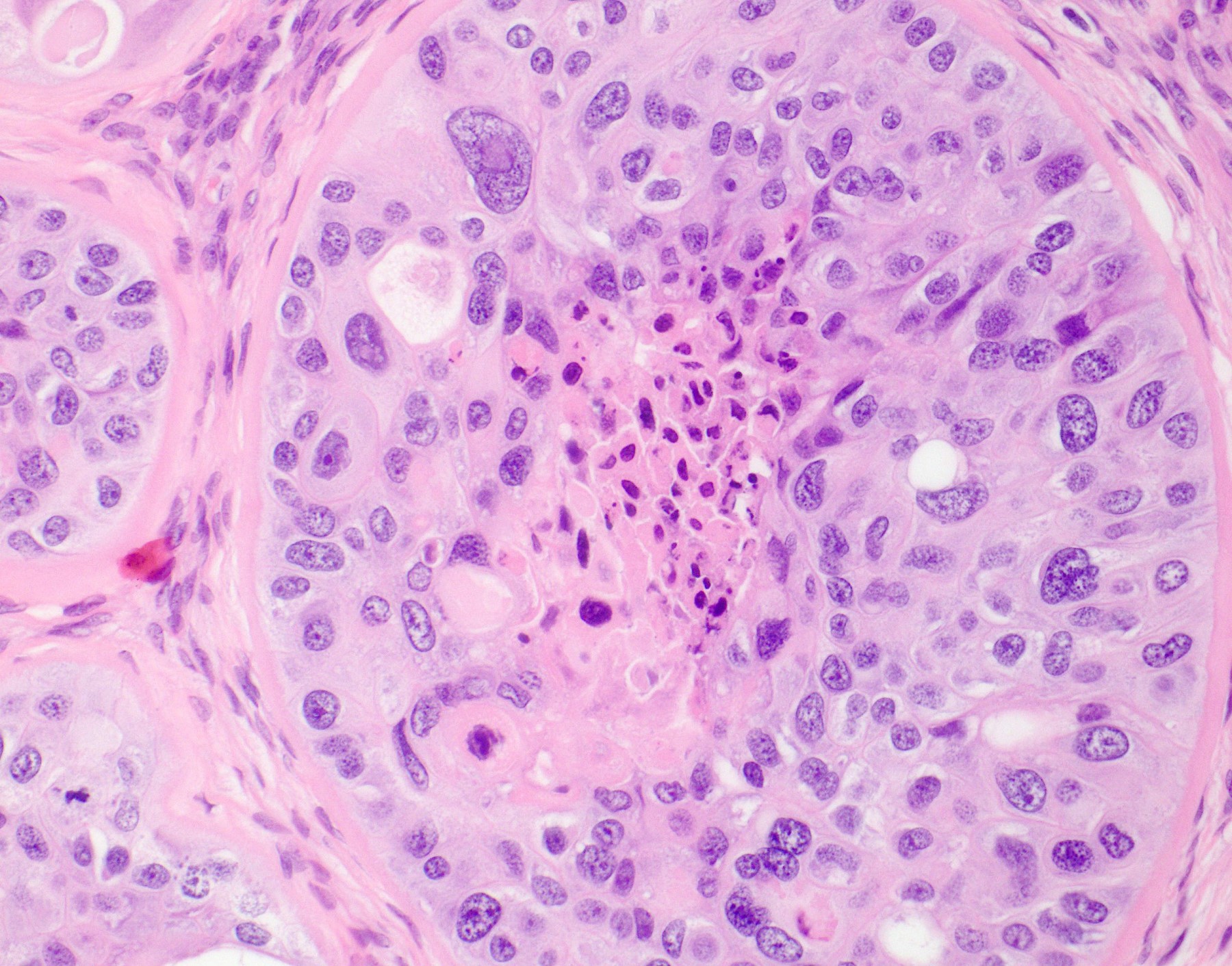
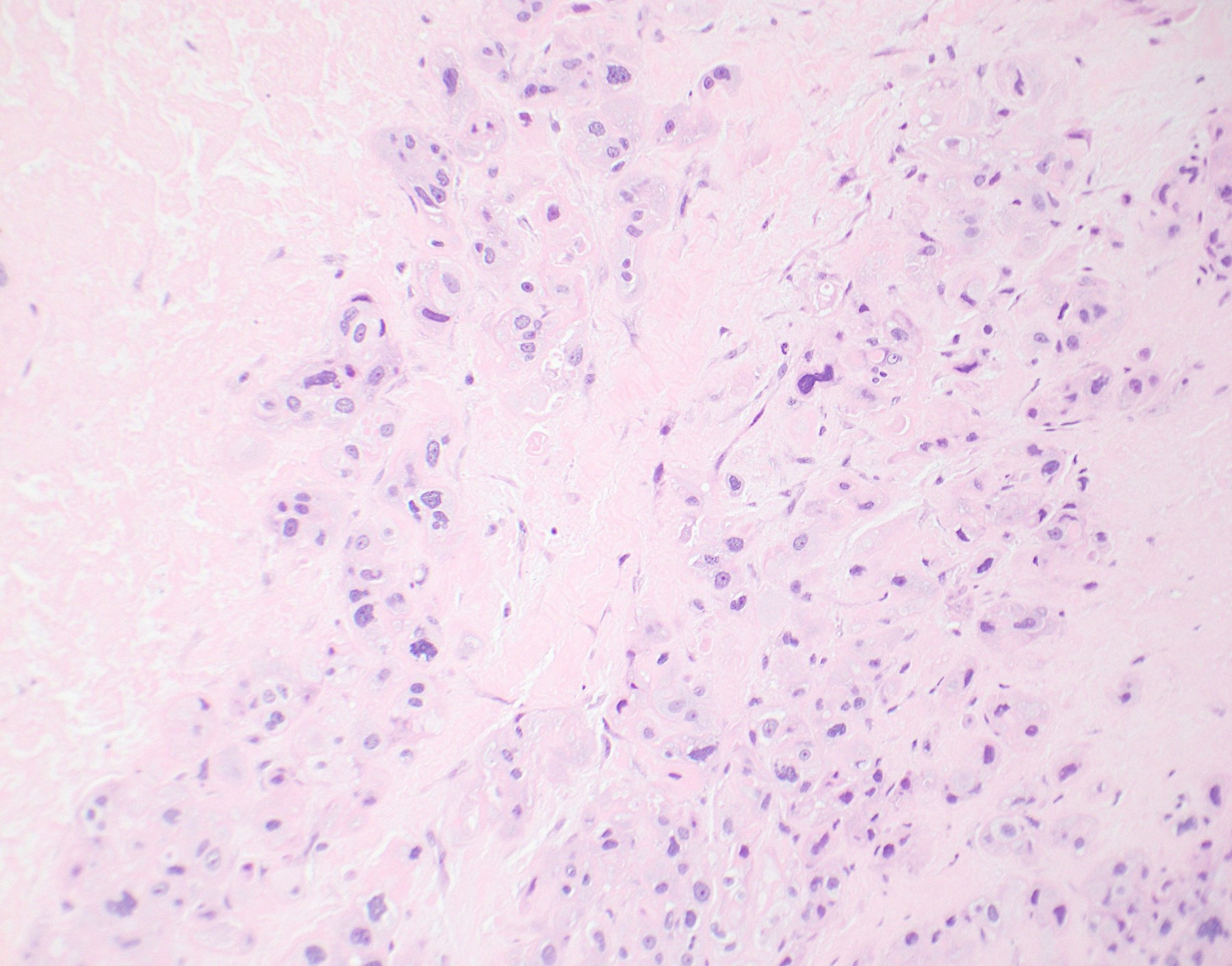
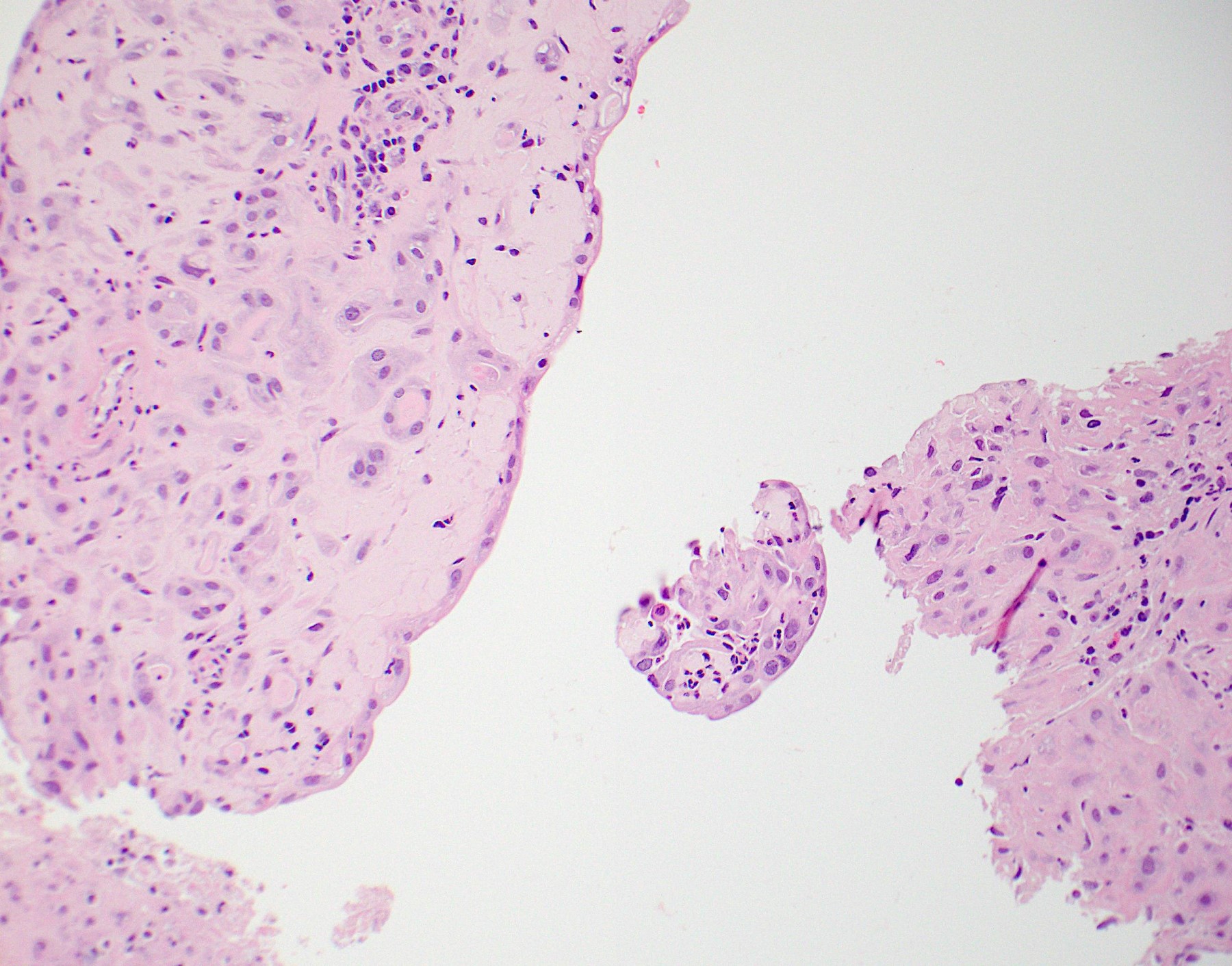
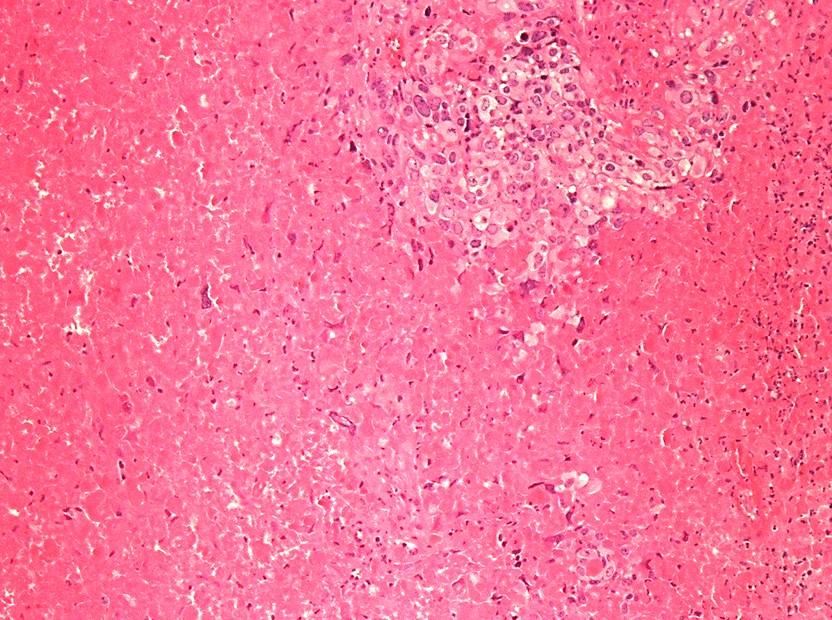
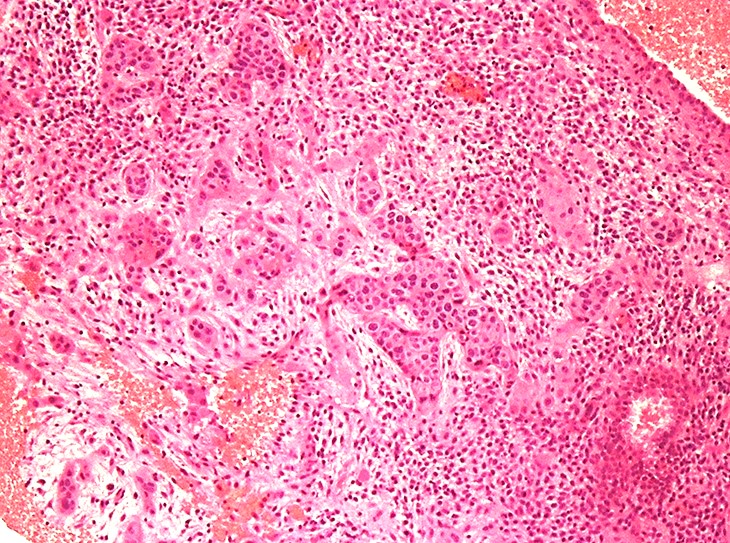
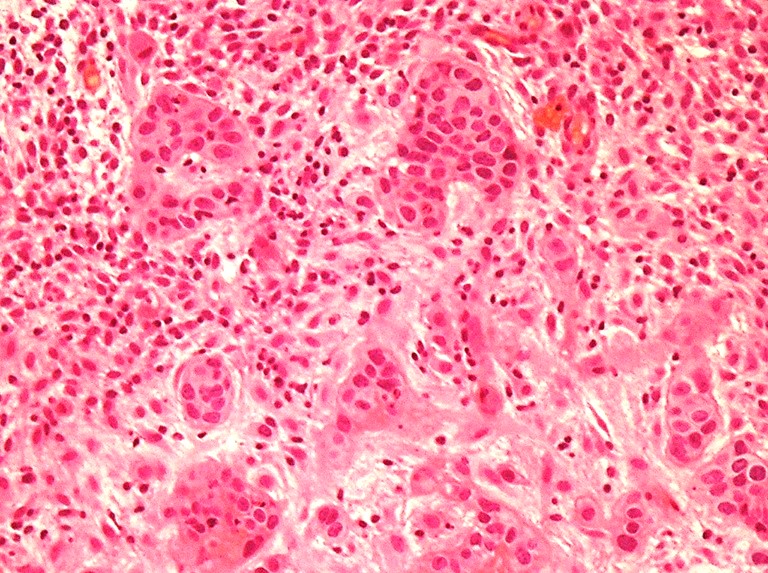
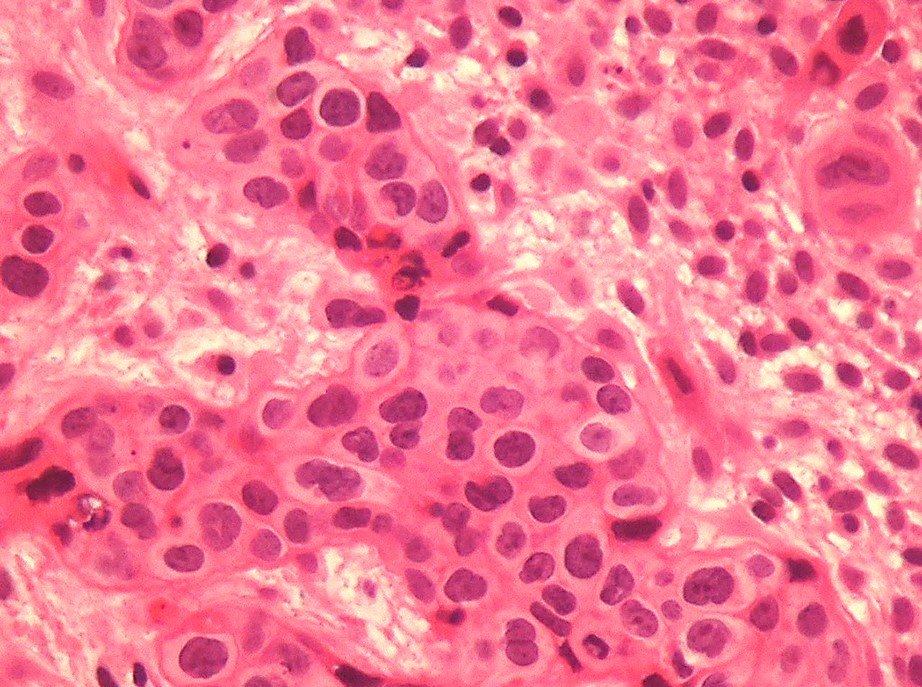
Microscopic (histologic) description
- Tumor shows nodular, expansile growth of relatively uniform, medium sized tumor cells arranged in nests, cords or large sheets
- Tumor cells have a moderate amount of finely granular, eosinophilic to clear cytoplasm with distinct cell membrane and round nuclei with small nucleoli
- Moderate nuclear atypia is seen in most of the tumors
- Well circumscribed tumor border is characteristic; however, focal infiltrative peripheral areas are not uncommon
- Occasional syncytiotrophoblastic cells may be present; unless they represent a substantial population, they do not warrant a diagnosis of choriocarcinoma
- Extensive or geographic necrosis is often present
- Eosinophilic hyaline-like material is characteristically present in the center of some tumor nests, simulating keratin formation
- The mitotic count ranges from 0 - 9 per 10 high power fields but as high as 48 per 10 high power fields has been observed
- Focal areas of placental site nodule, placental site trophoblastic tumor and choriocarcinoma can rarely be identified within the tumor
- Unique histologic features:
- Scattered decidualized benign stromal cells may be present at the tumor periphery
- Calcification is common
- ETT tumor cells frequently colonize the mucosal surface or glandular epithelium of the cervix and endometrium and can simulate high grade squamous intraepithelial lesion or squamous epithelium
- Reference: Am J Surg Pathol 1998;22:1393, Arch Pathol Lab Med 2019;143:65
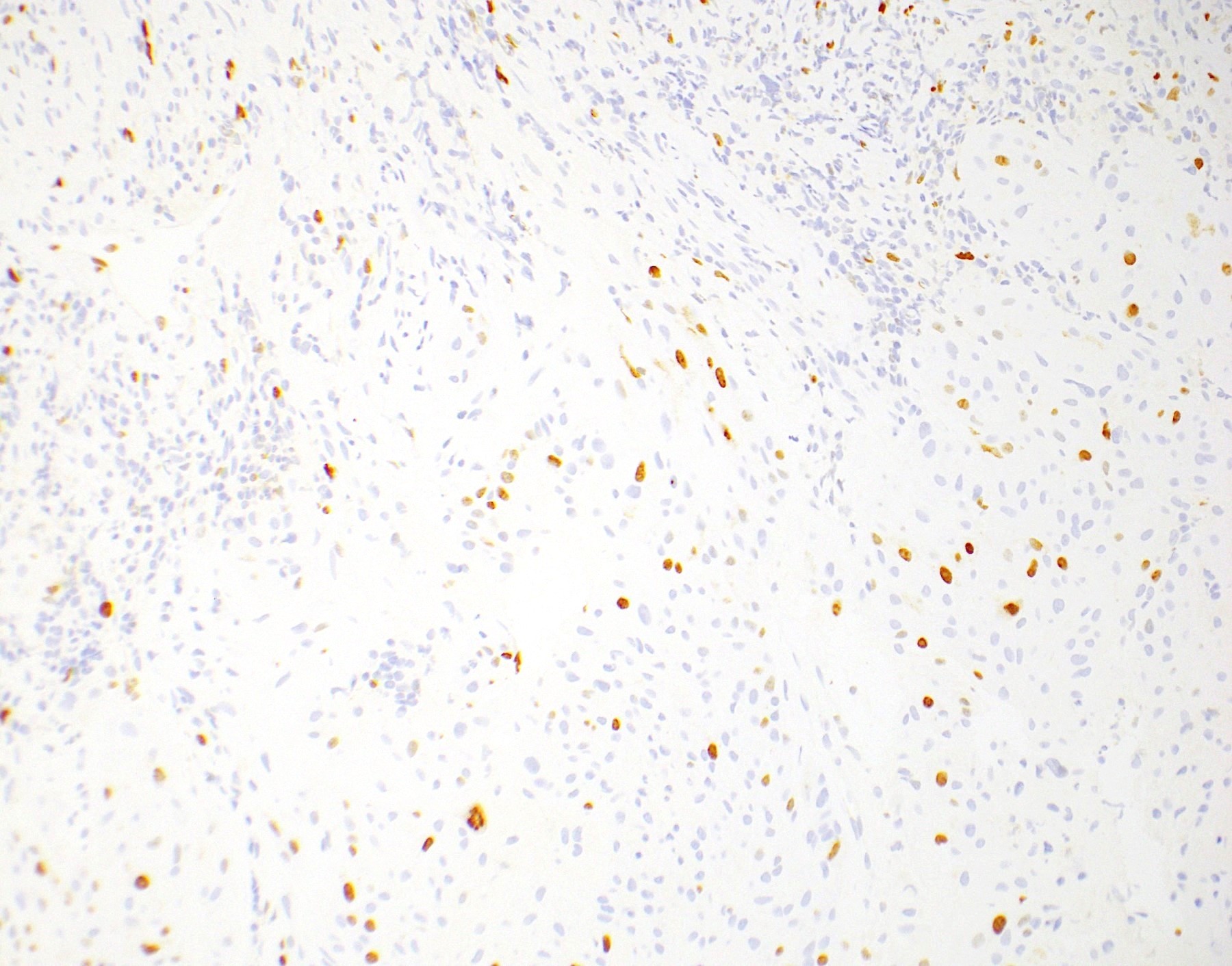
Microscopic (histologic) images
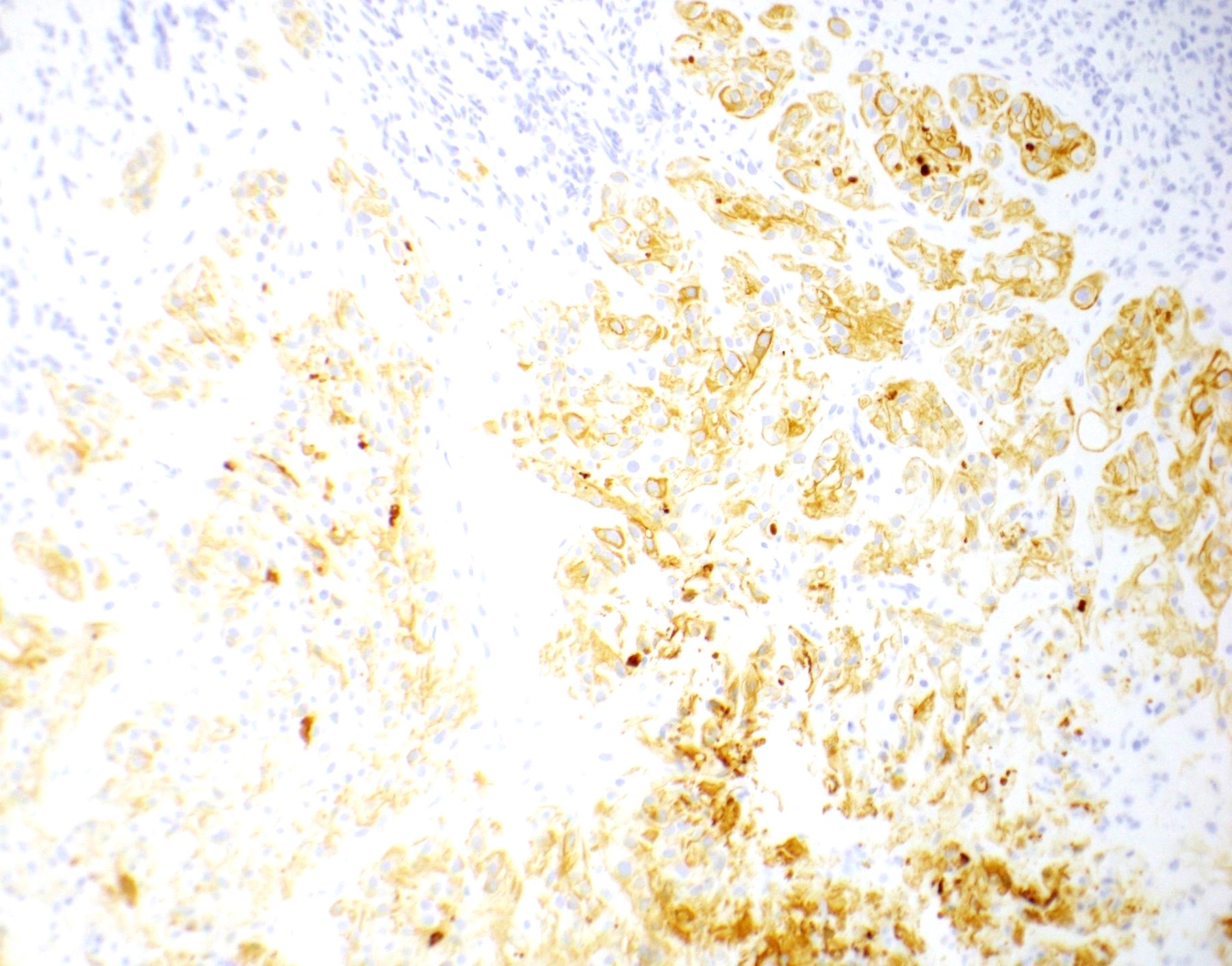
Positive stains
- p63 (Am J Surg Pathol 2004;28:1177)
- HLA-G
- HSD3B1
- Inhibin-alpha
- Cyclin E
- GATA3
- CD10
- EMA
- CK (CK7, CK18, CAM 5.2, AE1 / AE3)
- Ki67 labeling index > 10% (mean: 18%, range: 10 - 25%)
- Reference: Am J Surg Pathol 1998;22:1393
Negative stains
- hCG (Am J Surg Pathol 2004;28:1177, Am J Surg Pathol 1998;22:1393)
- PLAP (rare cells may be positive) (Am J Surg Pathol 1998;22:1393)
- HPL (rare cells may be positive) (Ann Diagn Pathol 2007;11:228, Am J Surg Pathol 1998;22:1393)
- MEL-CAM (rare cells may be positive) (Ann Diagn Pathol 2007;11:228, Am J Surg Pathol 1998;22:1393)
- ER / PR (Am J Surg Pathol 1998;22:1393)
Molecular / cytogenetics description
- LPCAT1::TERT fusion and TERT upregulation (PLoS One 2021;16:e0250518)
- Short tandem repeat multiplex PCR assay shows paternal alleles, confirming trophoblastic origin (Mod Pathol 2009;22:232)
Sample pathology report
- Uterus and cervix; hysterectomy:
- Epithelioid trophoblastic tumor (3.6 cm) involving the lower uterine segment and upper endocervix (see comment)
- Comment: The partially necrotic tumor shows expansile growth of epithelioid tumor cells with eosinophilic to clear cytoplasm, distinct cell membranes and moderate nuclear atypia. Mitotic activity is moderately increased (up to 6 per 10 high power fields). Scattered decidualized stroma is present in the periphery. The tumor invades 1.2 cm into a 1.8 cm thick myometrium and extends 1.1 cm into a 2.3 cm thick cervix. Immunohistochemical stains show the tumor is positive for AE1 / AE3, p63, HLA-G, inhibin and cyclin E, with increased Ki67 proliferation index (20%) and negative for HPL, hCG, ER and PR. The overall findings support the above diagnosis.
Differential diagnosis
- Cervical squamous cell carcinoma:
- Definitive squamous intraepithelial lesion, true keratin formation, cell bridges, not associated with decidualized stromal cells at the periphery
- hCG is not increased
- Negative for trophoblastic differentiation markers
- Endometrioid carcinoma:
- Placental site nodule (PSN):
- Single to multiple, well circumscribed nodules usually < 5 mm in size
- Mitotic activity is very low (Ki67 proliferation index < 8%)
- Atypical placental site nodule:
- Larger size of the nodule than PSN (> 5 to 10 mm), increased cellularity, marked nuclear atypia, moderately increased mitotic activity and Ki67 proliferation index between 8% and 10%
- May have cyclin E expression
- Placental site trophoblastic tumor:
- Choriocarcinoma:
Additional references
Board review style question #1
A 35 year old gravida 2 para 1 woman presents with vaginal bleeding. On ultrasound, a 2.5 cm fungating lower uterine mass / upper endocervical is identified. The findings from the biopsy specimen are shown in the images above. The immunohistochemical stains show positive expression for p63, HLA-G and inhibin and negative expression for HPL, PLAP, hCG and p16. What is the most likely diagnosis?
- Choriocarcinoma
- Epithelioid trophoblastic tumor
- Placental site trophoblastic tumor
- Squamous cell carcinoma of the cervix
Board review style answer #1
Board review style question #2
Which of the following immunohistochemical stains can help differentiate placental site trophoblastic tumor from epithelioid trophoblastic tumor?
- CD10
- hCG
- HSD3B1
- p63
Board review style answer #2