Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Mendoza R, Lanjewar S, Gupta R. Placental site trophoblastic tumor. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/placentaPSTT.html. Accessed April 17th, 2024.
Definition / general
- Placental site trophoblastic tumor (PSTT), a rare gestational trophoblastic disease (0.25 - 5% of all trophoblastic tumors), is a neoplastic proliferation of intermediate trophoblasts at placental implantation site (Hum Pathol 1991;22:847)
Essential features
- Consists of aggregates or sheets of large, polyhedral to round, predominantly mononucleated cells composed of implantation site intermediate trophoblastic cells
- Characteristic vascular invasion is often present, in which the tumor cells replace the wall of myometrial vessels
- Tumor cells are positive for HPL, CD146 and HSD3B1 but only focally positive for hCG and negative for PLAP; Ki67 index is < 30%
- Serum beta hCG levels are low (< 1,000 mIU/mL)
Terminology
- Atypical choriocarcinoma, syncytioma, chorioepitheliosis, trophoblastic pseudotumor
ICD coding
- ICD-O: 9104/1 - placental site trophoblastic tumor
- ICD-11: 2C75.0 & XH1RM5 - malignant trophoblastic neoplasm of placenta and placental site trophoblastic tumor
Epidemiology
- Patients are usually in the reproductive age group (mean: 31 years; range: 20 to 63 years)
Sites
- Uterus (corpus, lower uterine segment)
- Rarely, fallopian tubes and ovaries (Int J Gynecol Pathol 2003;22:362)
Pathophysiology
- Has been thought to develop as a result of neoplastic transformation of cytotrophoblastic cells; the transformed cells assume the differentiation toward implantation site intermediate trophoblast (Lancet Oncol 2007;8:642)
- Duplication of paternal X chromosome is considered to cause abnormal genetic overdosing and plays a role in trophoblastic proliferation; 85% of PSTT have had a female antecedent gestation (Lab Invest 2000;80:965)
Etiology
- Unknown
Clinical features
- Patients can present with either amenorrhea or abnormal bleeding, often accompanied by uterine enlargement (Gynecol Oncol 2005;99:603, Gynecol Oncol 2006;100:511)
- When uterine enlargement ceases, the diagnosis of a missed abortion is sometimes made
- Rarely, PSTT is associated with virilization, nephrotic syndrome and erythrocytosis (Obstet Gynecol 1992;79:846, Hum Pathol 1985;16:35, Clin Nephrol Case Stud 2018;6:27)
- 66% of cases follow a full term pregnancy, with a median latency of 12 - 18 months (ranging from a few months to 20 years) (Gynecol Oncol 2006;100:511, Gynecol Oncol 1999;73:216)
- Occasionally occurs following spontaneous abortions and hydatidiform moles (10 - 50% of cases) (Gynecol Oncol 2004;92:708, J Reprod Med 2002;47:460, Histopathology 1982;6:211)
- At presentation, > 80% of cases are International Federation of Gynecology and Obstetrics (FIGO) stage 1 (Gynecol Oncol 2006;100:511)
- Recurrence or metastasis occurs in 25 - 30% of patients (Gynecol Oncol 2001;82:415, J Reprod Med 2002;47:460)
- Mortality rate is 6.5 - 27% (Gynecol Oncol 2019;153:684)
Diagnosis
- Biopsy or hysterectomy specimen
Laboratory
- Serum levels of beta hCG are generally low (< 1,000 mIU/mL)
- Mild to moderate elevation of serum hCG (5 - 26,000 mIU/mL, average: 680 mIU/mL) is detectable in 80% of cases (Gynecol Oncol 2006;100:511, Gynecol Oncol 2001;82:415, Gynecol Oncol 2005;99:603, J Reprod Med 2002;47:460)
Radiology description
- On ultrasonography, a solid mass within the endometrial cavity or in the myometrium may be identified, with more or less prominent blood vessels on color Doppler imaging; in certain cases, ultrasound may reveal an enlarged uterus with a heterogeneous echotexture, echogenic foci and cystic areas of hemorrhage
- On MRI, a frequent observation is the distortion of the junctional zone caused by a myometrial or endometrial mass, which is typically isointense to normal myometrium on T1 weighted images and isointense to slightly hyperintense to the myometrium on T2 weighted images; a diffusely heterogeneous pattern of the uterus with loss of zonal anatomy is also observed
- Reference: J Radiol Case Rep 2015;9:14
Prognostic factors
- Poor prognostic factors include
- Tumor cells with clear cytoplasm, deep myometrial invasion, large tumor size, necrosis and high mitotic count (> 2.5 mitoses/mm², equating to > 5 mitoses/10 high power fields of 0.5 mm in diameter and 0.2 mm² in area) (Gynecol Oncol 2006;100:511)
- Advanced stage, ≥ 48 months since antecedent pregnancy, age > 40 years and the presence of tumor cells with clear cytoplasm are independent predictors of a worse prognosis (Gynecol Oncol 2006;100:511)
Case reports
- 28 year old Chinese woman presenting with thrombotic microangiopathy (Medicine (Baltimore) 2018;97:e12698)
- 32 year old woman presenting with amenorrhea after a normal childbirth and who subsequently developed nephrotic syndrome (Clin Nephrol Case Stud 2018;6:27)
- 37 year old Caucasian woman with paraneoplastic nodular regenerative liver hyperplasia associated with PSTT (Gynecol Oncol Rep 2019;29:16)
- Successful treatment of 13 cases of PSTT (Gynecol Oncol Rep 2020;32:100548)
Treatment
- Simple hysterectomy is curative in most cases (Br J Cancer 2000;82:1186)
- Combination chemotherapy usually results in a high response rate and long term remission even in patients with recurrent or metastatic PSTT but only a few patients achieve a complete response (J Clin Diagn Res 2014;8:OD12, Gynecol Oncol Rep 2017;21:86, Front Oncol 2019;9:937)
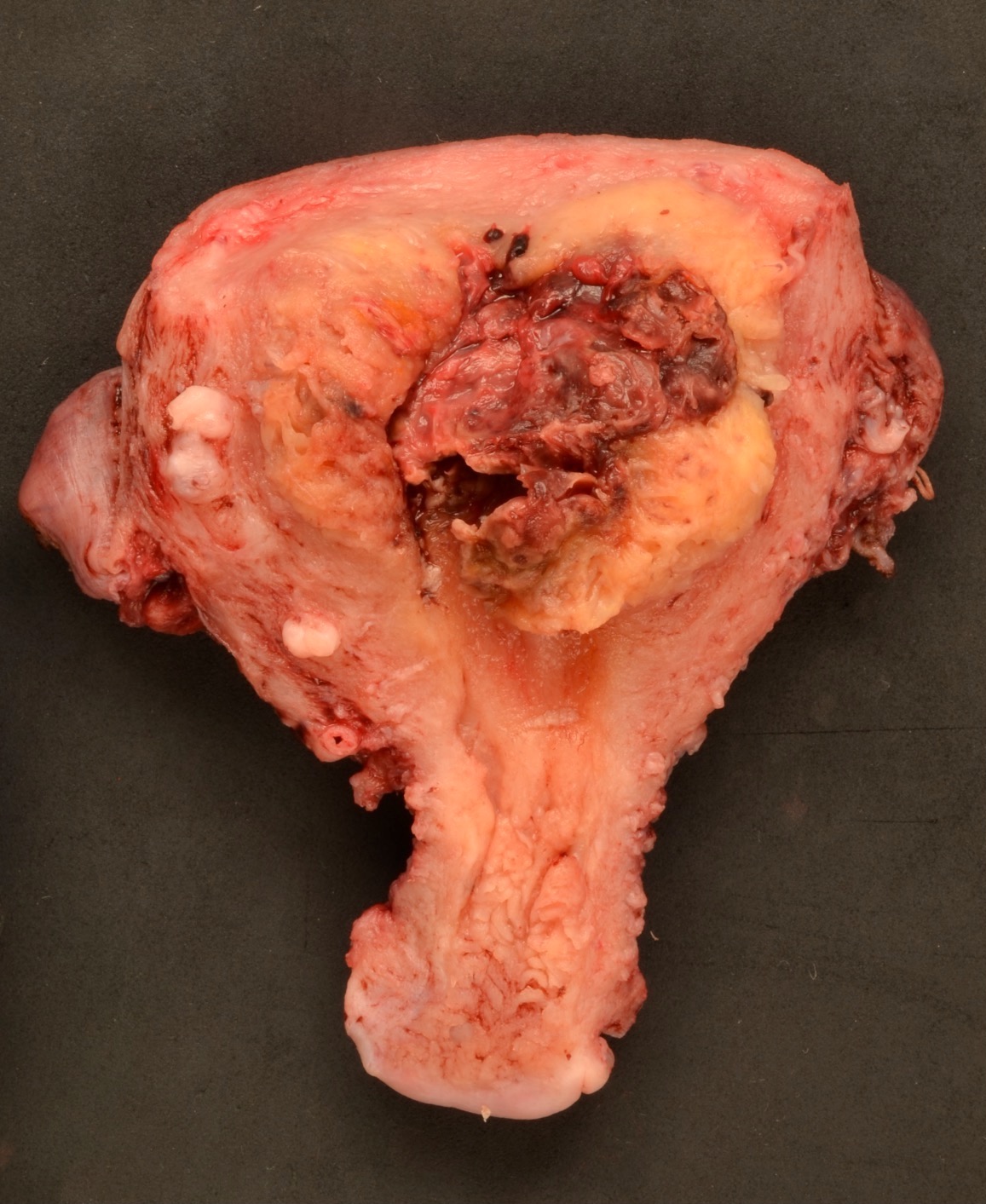
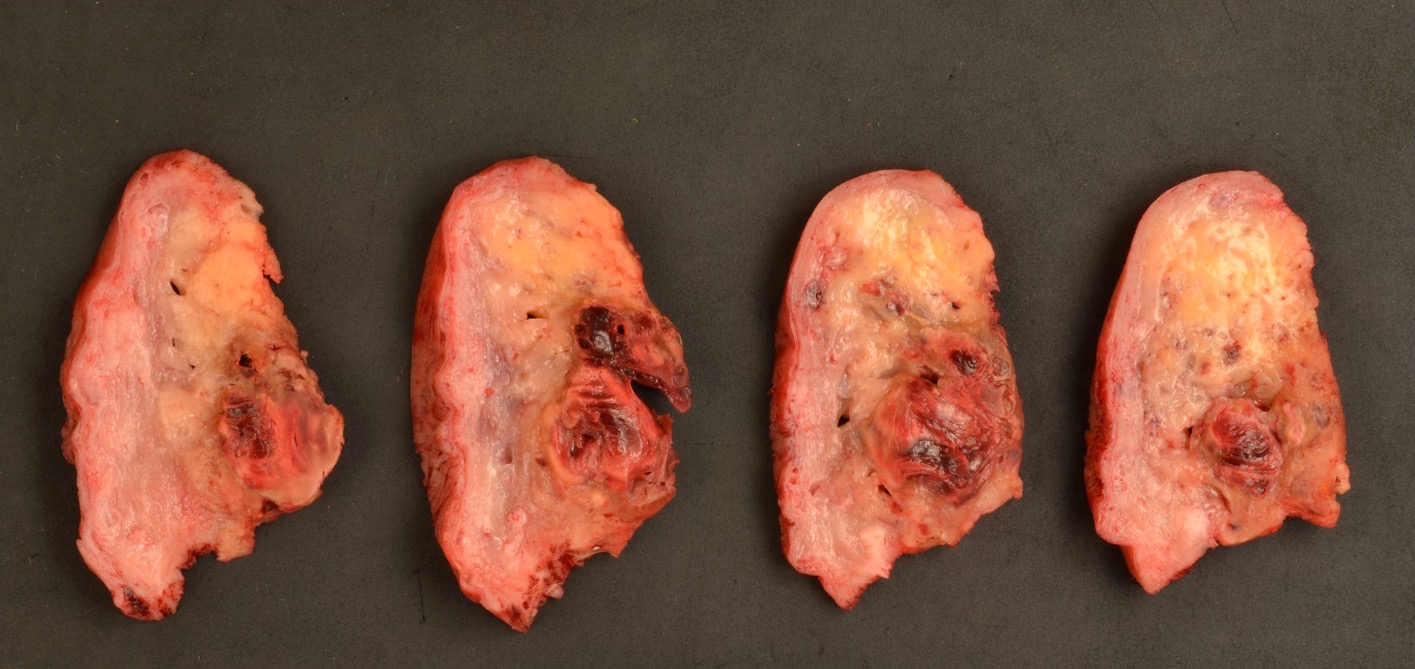
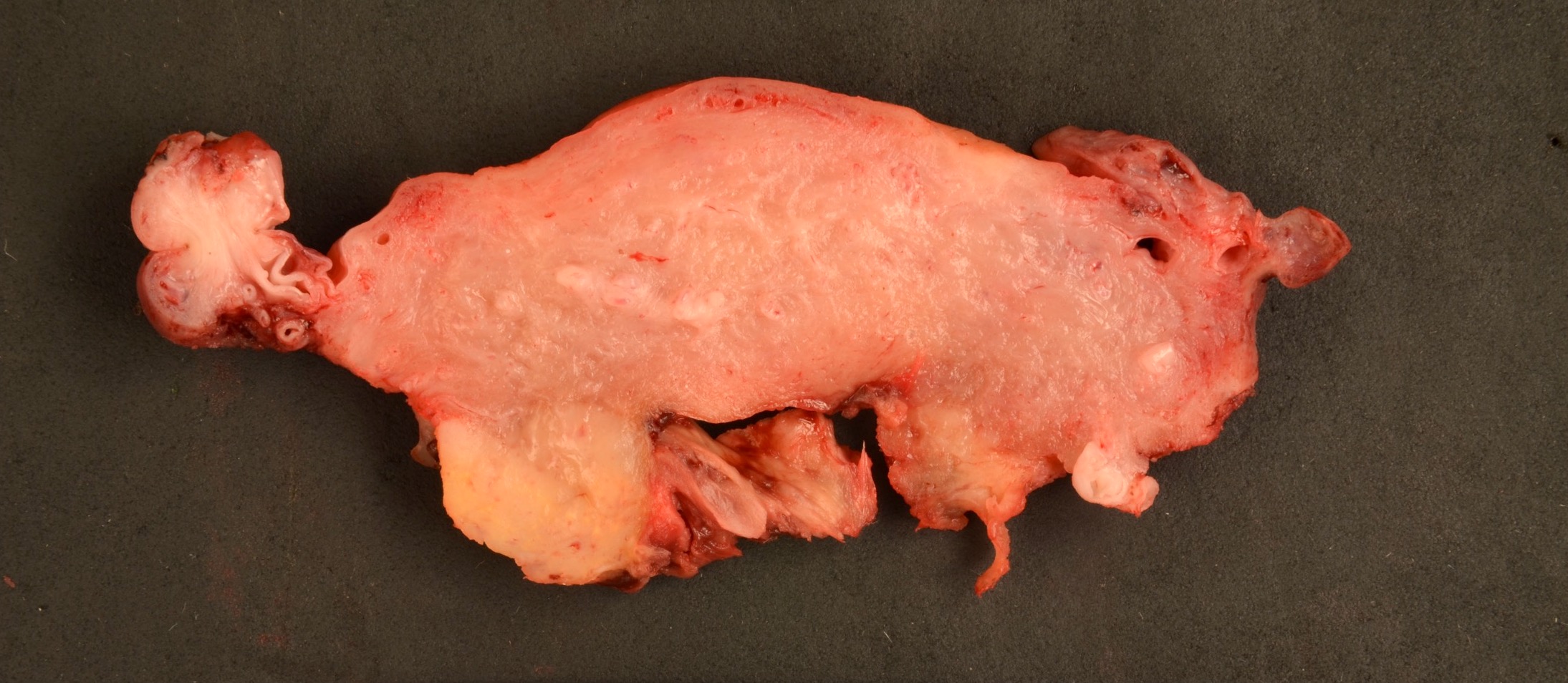
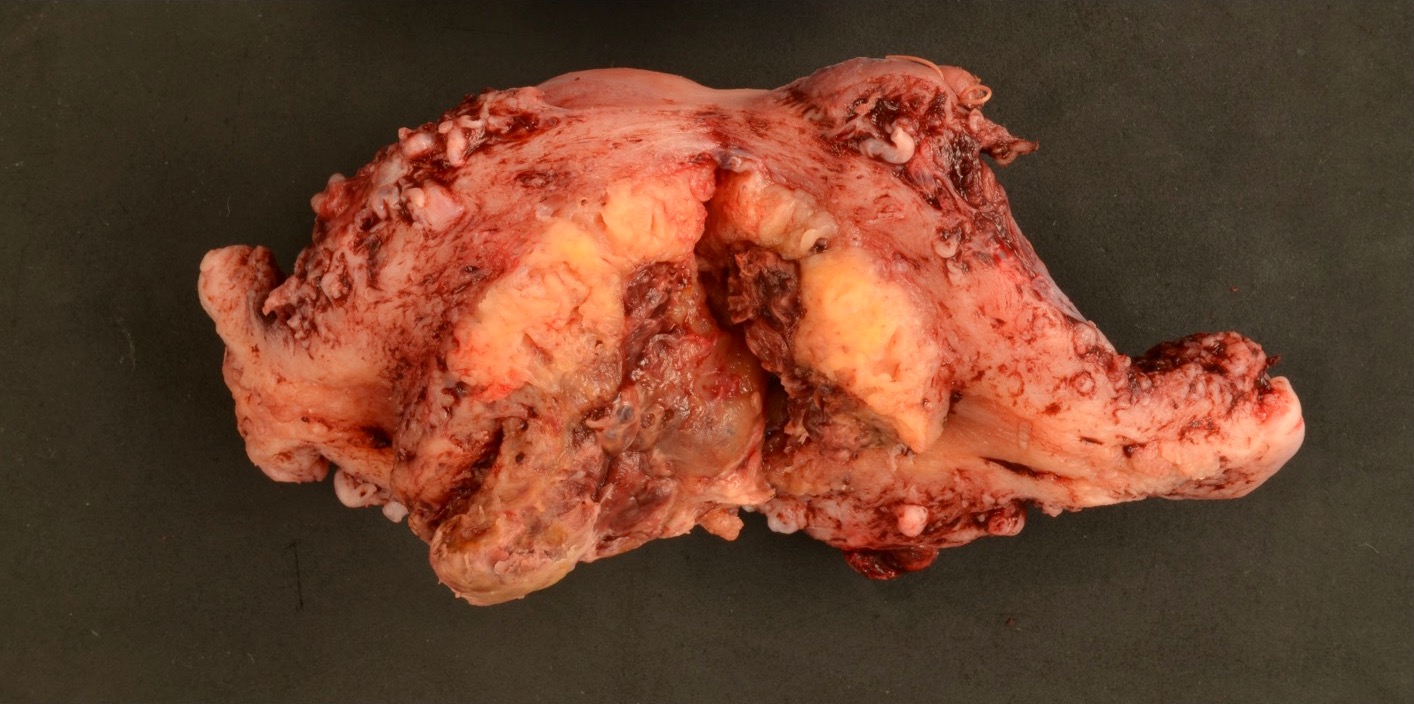
Gross description
- Well circumscribed, nodular mass up to 10 cm
- Can be polypoid, projecting into the uterine cavity or may predominantly involve the myometrium
- Sectioned surface is usually solid, fleshy and white-tan to light yellow, containing only focal areas of hemorrhage or necrosis, if present
- Deep myometrial invasion is seen in 50% of cases (Gynecol Oncol 2006;100:511)
- Invasion frequently extends to the uterine serosa (10%) and in rare instances, to the adnexal structures, including broad ligament (Gynecol Oncol 2006;100:511)
- Reference: Kurman: Blaustein's Pathology of the Female Genital Tract, 7th Edition, 2019
Gross images
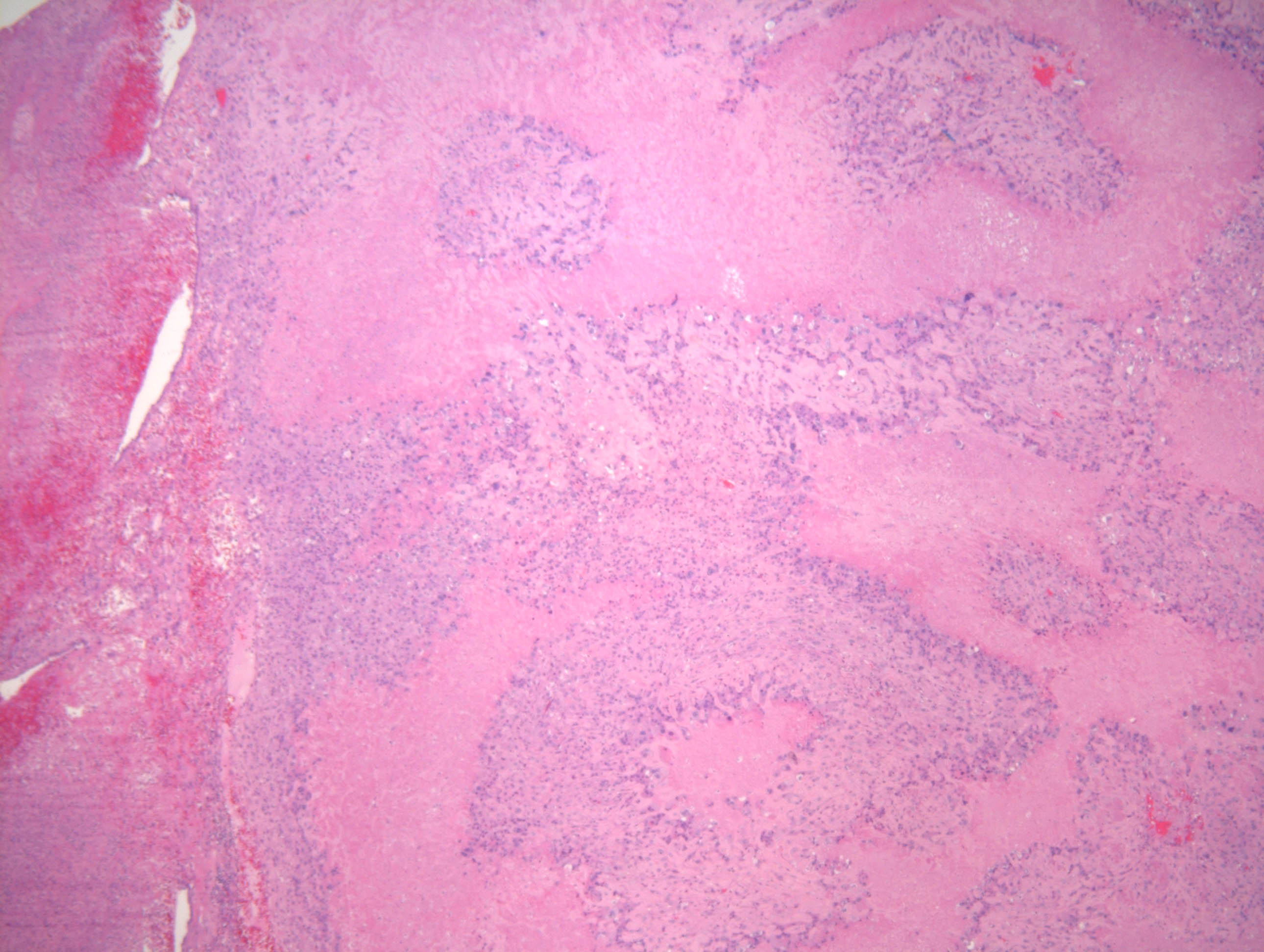
Microscopic (histologic) description
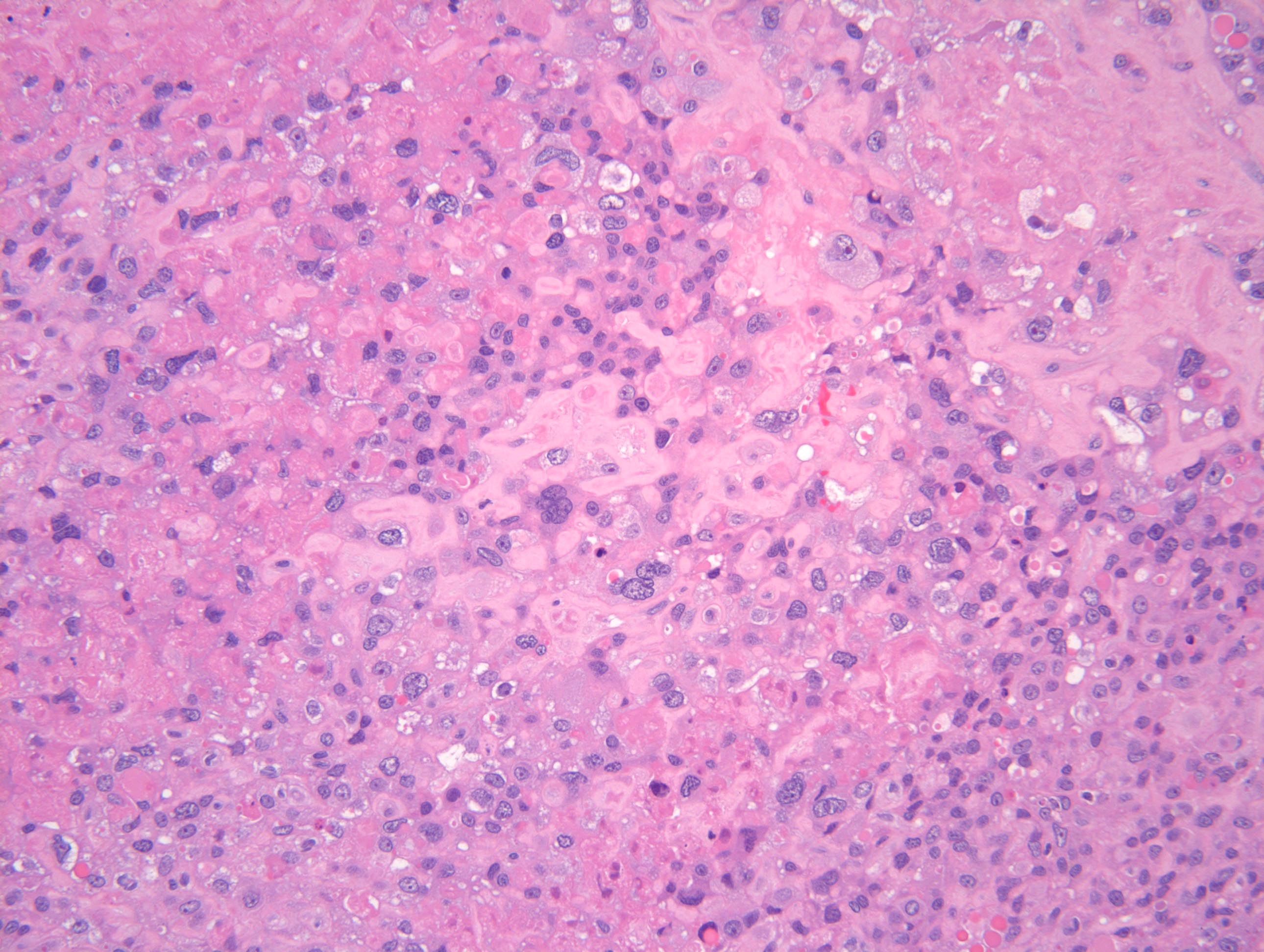
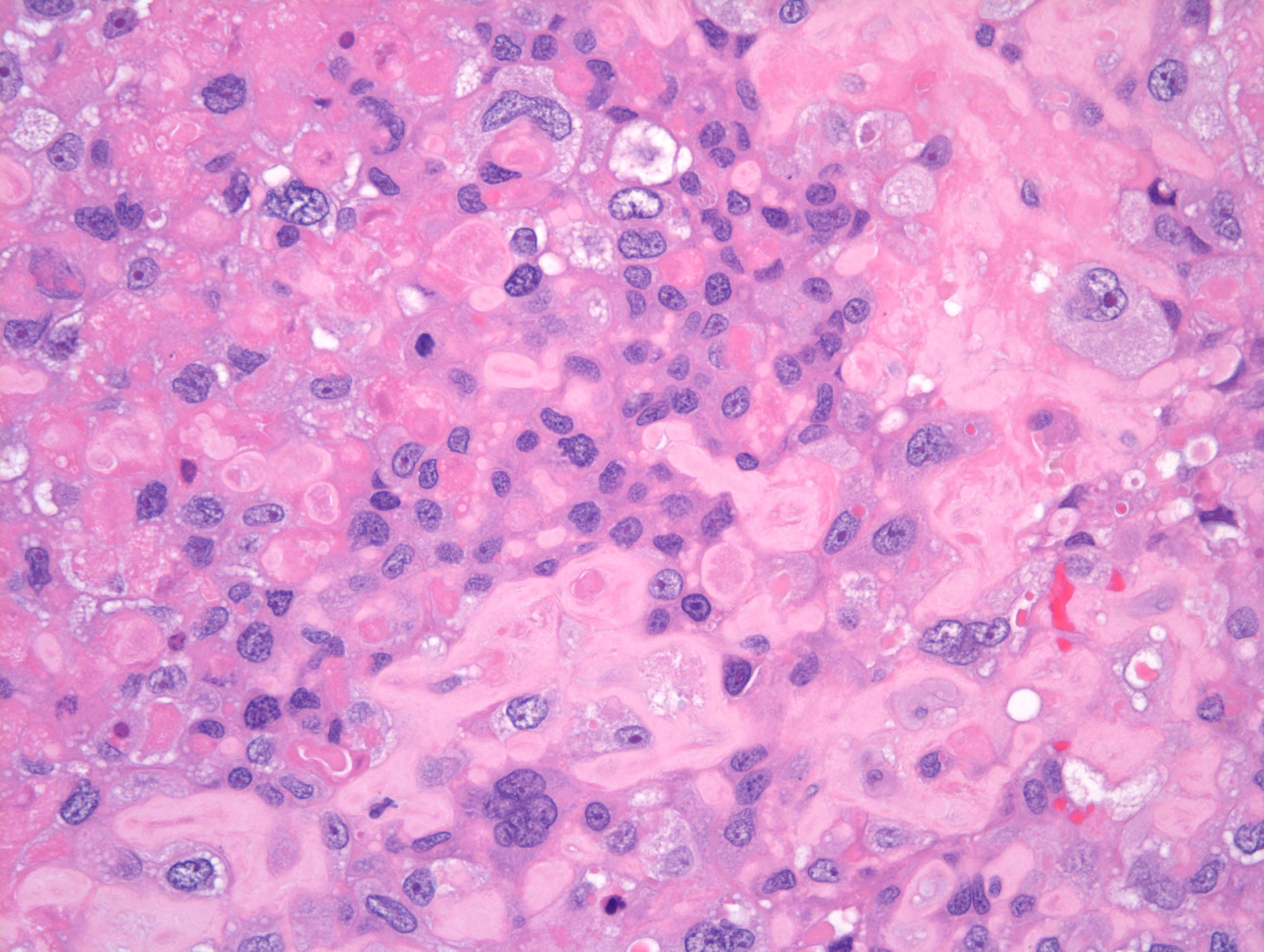
- Infiltrative growth pattern consisting of aggregates or sheets of large, polyhedral to round, predominantly mononucleated cells composed of implantation site intermediate trophoblastic cells
- Scattered multinucleated implantation site trophoblastic cells are common
- Tumor cells often aggregate into confluent sheets; however, at the periphery the trophoblast cells invade singly or in cords and nests, characteristically infiltrating the myometrium by separating individual muscle fibers and groups of fibers
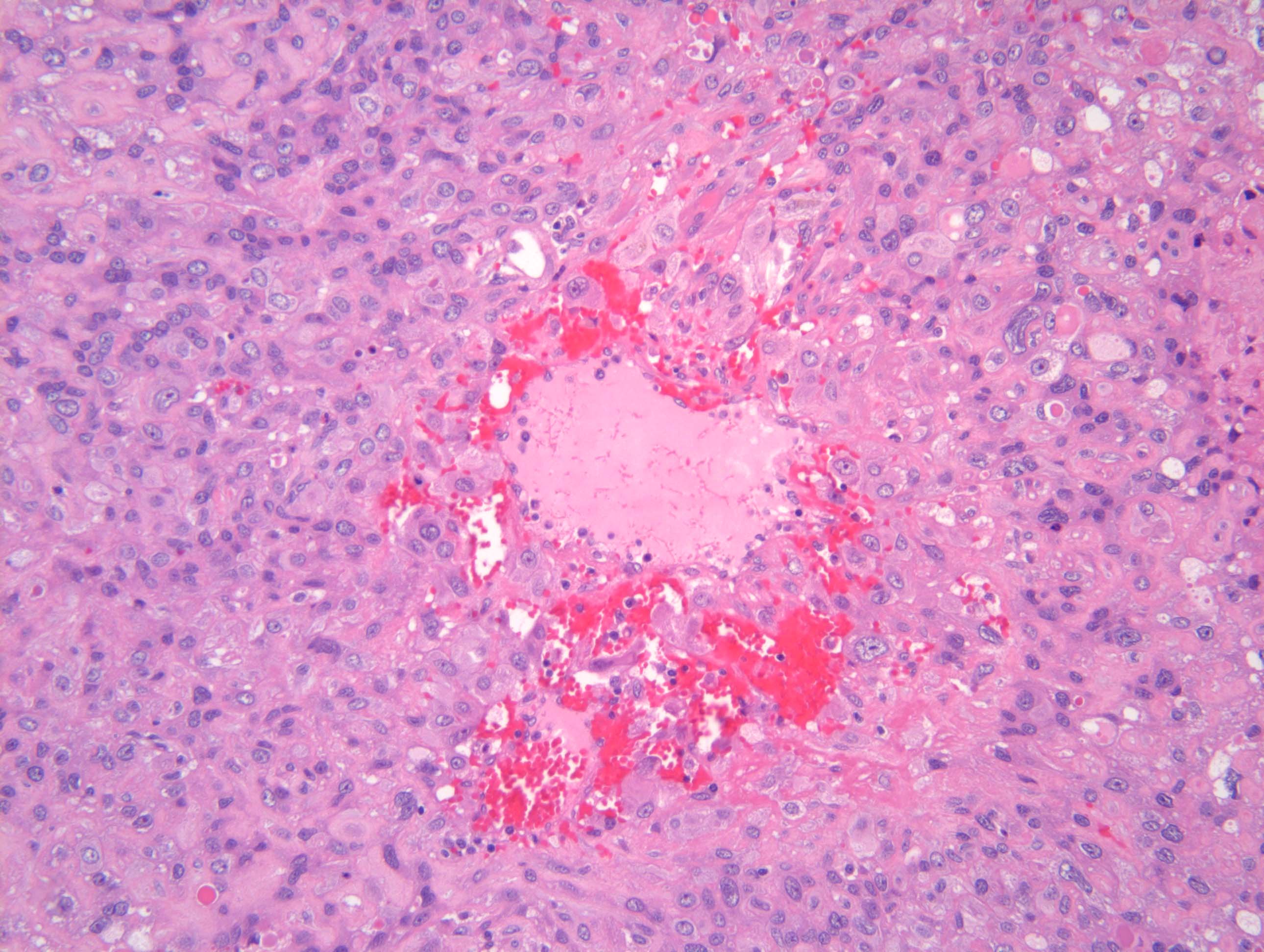
- Vascular invasion is often present, in which the tumor cells replace the wall of myometrial vessels; these transformed blood vessels are unique among all human solid tumors and are diagnostic for PSTT
- Cytologically, the cells have an abundant amphophilic (and occasionally eosinophilic or clear) cytoplasm; nuclei are pleomorphic and nuclear atypia is generally pronounced, with frequent, large, convoluted nuclei and marked hyperchromasia
- Most tumors have a low mitotic count, with 1 - 2 mitoses/mm² (equating to 2 - 4 mitoses/10 high power fields of 0.5 mm in diameter and 0.2 mm² in area) (Gynecol Oncol 2006;100:511, Int J Gynecol Pathol 2001;20:31, Clin Obstet Gynecol 1984;27:248)
- Decidua or an Arias-Stella reaction may be present in the adjacent, uninvolved endometrium; villi are almost never identified
- Necrosis may be present
- Reference: Kurman: Blaustein's Pathology of the Female Genital Tract, 7th Edition, 2019
Microscopic (histologic) images
Positive stains
- HPL (Ann Diagn Pathol 2007;11:228)
- Cytokeratin
- MUC4
- HSD3B1
- HLA-G
- MEL-CAM (CD146)
- CD10
- GATA3 (Am J Surg Pathol 2015;39:101)
- PDL1 (Int J Gynecol Pathol 2017;36:146)
- Ki67 is expressed in 8 - 20% of cells (Ann Diagn Pathol 2007;11:228, Int J Gynecol Pathol 2001;20:31)
Negative stains
- p63 (Ann Diagn Pathol 2007;11:228)
- hCG (focally positive)
- Inhibin (focally positive)
- PLAP
- Reference: Zhonghua Bing Li Xue Za Zhi 1998 Aug;27:294
Molecular / cytogenetics description
- Presence of paternally derived X chromosome and absence of Y chromosome (Mod Pathol 2007;20:1055)
Sample pathology report
- Uterus, cervix, total hysterectomy:
- Placental site trophoblastic tumor (see comment)
- Comment: The tumor is a polypoid, nodular mass infiltrating into the myometrium. It is composed mostly of mononucleated eosinophilic polygonal cells with admixed multinucleated cells, morphologically similar to intermediate trophoblastic cells. The tumor cells infiltrate in between the myometrial fibers and invades the myometrial vessel walls. Areas of tumor necrosis are identified comprising about 20% of the specimen. Mitotic activity is 1 - 2/mm² and the Ki67 index is approximately 15%. The tumor cells stain positively with HPL, MUC4 and CD146, focally positive for hCG and AE1 / AE3 and were negative for p63, p16, HMB45, S100, SMA and inhibin.
Differential diagnosis
- Exaggerated placental site (EPS):
- Exuberant infiltration of implantation site intermediate trophoblastic
- Microscopic, lacks mitotic activity (Ki67 ~0%) and composed of intermediate trophoblastic cells separated by masses of hyaline
- Usually admixed with decidua and chorionic villi and contains large numbers of multinucleated trophoblastic cells
- Epithelioid trophoblastic tumor (ETT):
- Choriocarcinoma:
- Squamous cell carcinoma (SCC) of the cervix:
- Poorly differentiated carcinoma:
- May show glandular differentiation and some variant epithelial differentiation (squamous, tubal)
- Epithelioid smooth muscle tumors:
- Metastatic melanoma:
Additional references
Board review style question #1
A 31 year old woman, gravida 2, para 1, presents with profuse vaginal bleeding. Prior to this, the patient had amenorrhea for about 12 weeks with uterine enlargment. Ultrasound reveals a 10 - 12 week enlarged uterus with a 4 cm polypoid endomyometrial mass. There was no intrauterine pregnancy. Serum beta hCG is < 1,000 mIU/mL. On H&E sections of the endometrial sample, the tumor shows an infiltrative growth pattern consisting of aggregates or sheets of large, polyhedral to round, predominantly mononucleated cells (representative section is shown above). Vascular invasion is present, replacing the wall of myometrial vessels. The proliferation index (Ki67) is < 30%. What is the most likely diagnosis?
- Choriocarcinoma
- Epithelioid trophoblastic tumor
- Placental site nodule
- Placental site trophoblastic tumor
Board review style answer #1
Board review style question #2
Characteristic histological features helpful in differentiating placental site trophoblastic tumor from most other neoplasms are
- Ability to replace and re-epithelialize the endocervical / endometrial surface epithelium
- Invasion and replacement of myometrial vessel walls
- Presence of distinct neoplastic components (triphasic tumor)
- Presence of extensive geographic necrosis and expression of p63
Board review style answer #2
B. Invasion and replacement of myometrial vessel walls
Comment Here
Reference: Placental site trophoblastic tumor
Comment Here
Reference: Placental site trophoblastic tumor