Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Kowalski PJ. Umbilical vasculitis and funisitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/placentaacutefunisitis.html. Accessed April 24th, 2024.
Definition / general
- Inflammation of the umbilical vessels (vasculitis) and cord substance (funisitis) occurs in response to many injuries and constitutes the fetal inflammatory response
Essential features
- Umbilical vasculitis and funisitis represent a fetal response to injury
- Vasculitis and funisitis are often microscopic findings but when the inflammatory response is severe, gross findings may also be evident
- Microorganisms are often causative, although vasculitis and funisitis can be seen in a wide range of injury
- Chorioamnionitis or meconium exposure are often associated conditions
Terminology
- Specific diagnoses can define the location and extent of the general inflammatory process
- Vasculitis: a general term defining inflammation of an umbilical vessel
- Funisitis: inflammation within the cord substance / Wharton jelly
- Arteritis: inflammation involving an umbilical artery
- Phlebitis: inflammation involving the umbilical vein
- Peripheral funisitis: inflammation located at the radial periphery or external surface of the umbilical cord and may be the primary observed histologic pattern
- Necrotizing funisitis: established or longstanding infections demonstrating tissue necrosis, abundant inflammation and accumulation of cellular debris throughout the umbilical cord
ICD coding
Epidemiology
- Patients with documented microorganisms (e.g. herpes simplex virus, group B Streptococcus, Candida albicans, Treponema pallidum)
- Patients with preterm labor, chorioamnionitis or meconium exposure
Sites
- Progressive inflammatory infiltration that involves umbilical vein, umbilical arteries or umbilical cord substance (Wharton jelly)
Pathophysiology
- Microorganisms gain access to the placenta or umbilical cord by ascension from the endocervical canal, by the maternal blood stream or by direct inoculation (such as from a diagnostic procedure)
- Cytokines (IL8, interferon gamma, complement components, leukotriene B4) are released by endothelium, mast cells and macrophages in response, creating a chemoattractant chemical gradient for neutrophils
- Chemical gradient may be augmented by certain peptides released by microorganisms
- Activated neutrophils marginate against the vascular endothelium and transmigrate through the vascular wall into the connective tissue of Wharton jelly (for general funisitis and all forms of vasculitis)
- Eventual precipitation of immune complexes (for necrotizing funisitis) as microbiologic antigens elicit a maternal antibody response through the transplacental passage of antibodies
- Reference: Kumar: Robbins & Cotran - Pathologic Basis of Disease, 10th Edition, 2020
Etiology
- Bacteria associated with intrauterine infection (group B Streptococcus, Escherichia coli, Fusobacterium or Bacteriodes species, Listeria monocytogenes)
- Fungi (Candida species)
- Less common causes include Actinomyces species, herpes simplex virus and Treponema pallidum (a classic causative agent of necrotizing funisitis)
- Reference: Am J Obstet Gynecol 2015;213:S29
Clinical features
- Typically seen in association with chorioamnionitis (maternal inflammatory response, including fever, tachycardia, leukocytosis or foul smelling amniotic fluid)
- Minimal / mild inflammation (particularly mild phlebitis of the umbilical vein) can be associated with only meconium exposure
Diagnosis
- Presence of any neutrophilic infiltrate involving the umbilical vein, umbilical arteries, cord substance (Wharton jelly) or peripheral umbilical cord
- Qualifying the location and degree of inflammation is encouraged over the generic use of the term funisitis, historically used to inadequately describe the presence of any inflammation in any location
Laboratory
- Positive documentation of intrapartum infection or maternal infectious status may be useful in some cases
Radiology description
- Inflammation induced calcifications within Wharton jelly can be distributed to resemble a spiral barber's pole on maternal radiographs in some cases of necrotizing funisitis
Prognostic factors
- Linked to increased incidence of interventional deliveries, low Apgar scores, clinical sepsis and admission to neonatal intensive care units (Virchows Arch 2016;468:503)
Case reports
- 24 year old woman with abnormal fetal heart rate pattern presenting as congenital syphilis (ISRN Obstet Gynecol 2011;2011:320246)
- 37 year old woman with stillbirth due to Listeria monocytogenes (Autops Case Rep 2018;8:e2018051)
- 41 year old woman with Candida funisitis / chorioamnionitis and stillbirth (Case Rep Womens Health 2020;27:e00239)
- 4 cases with necrotizing funisitis and herpes simplex infection (Hum Pathol 1994;25:715)
Gross description
- External surface of an involved umbilical cord is usually unremarkable
- Peripheral funisitis may be seen as multiple small, white or yellow plaques on the surface of the umbilical cord (often associated with Candida infection)
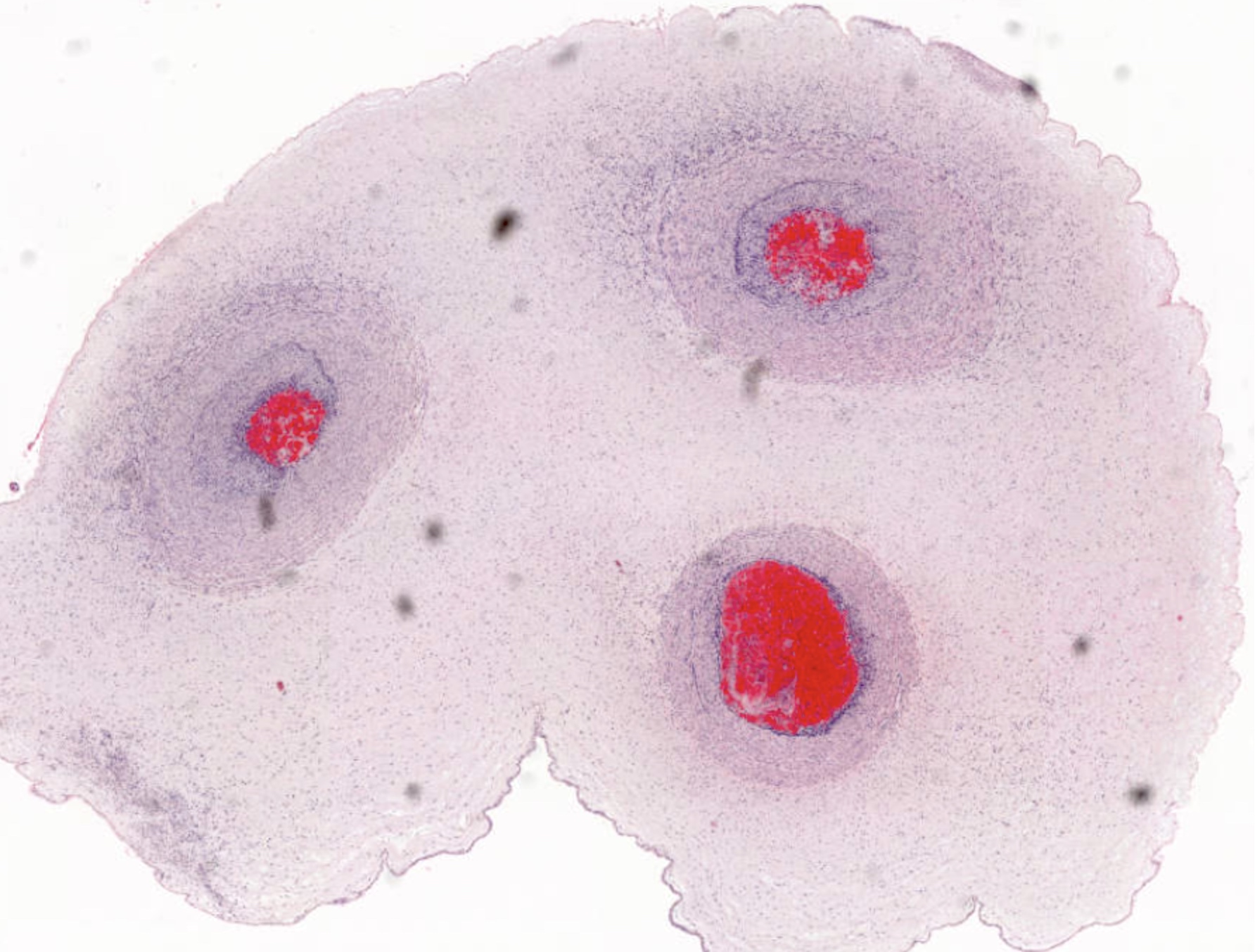
- Necrotizing funisitis on cut surface may appear as concentric perivascular rings resembling Ouchterlony immunodiffusion plates
- Necrotizing funisitis may become calcified and appear chalky white or as a white linear spiral (barber's pole configuration)
- Reference: Beargen: Manual of Pathology of the Human Placenta, 2nd Edition, 2011
Gross images
Microscopic (histologic) description
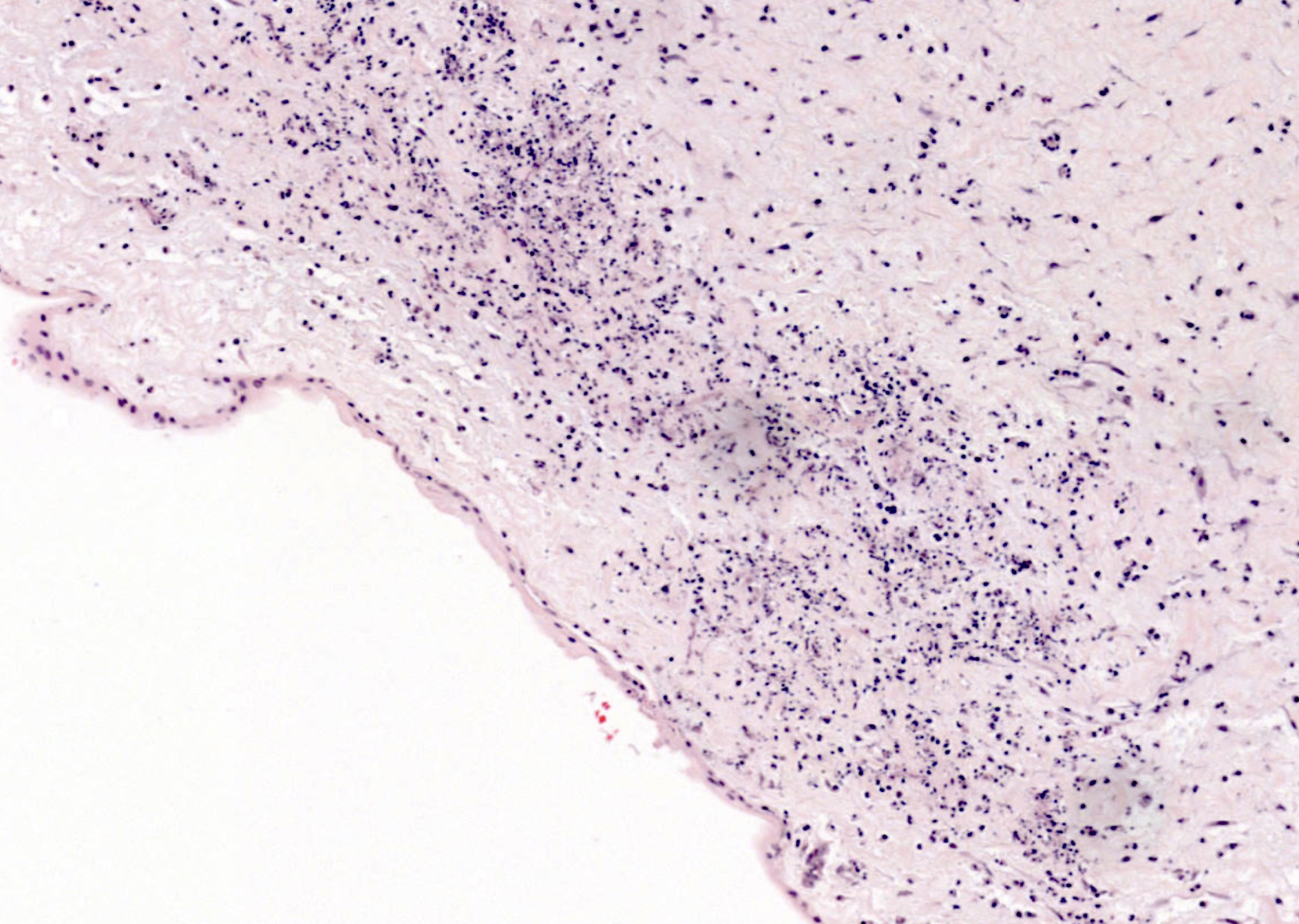
- Umbilical phlebitis is the presence of neutrophils in the wall of umbilical vein (stage 1: early; most common histologic finding)
- Umbilical arteritis is the presence of neutrophils in the wall of 1 or both umbilical arteries (stage 2: intermediate)
- Necrotizing funisitis typically shows 3 vessel panvasculitis, with degenerating neutrophilic and cellular debris present in the cord substance, sometimes arranged as concentric arcs (or waves) of necrosis (stage 3: late)
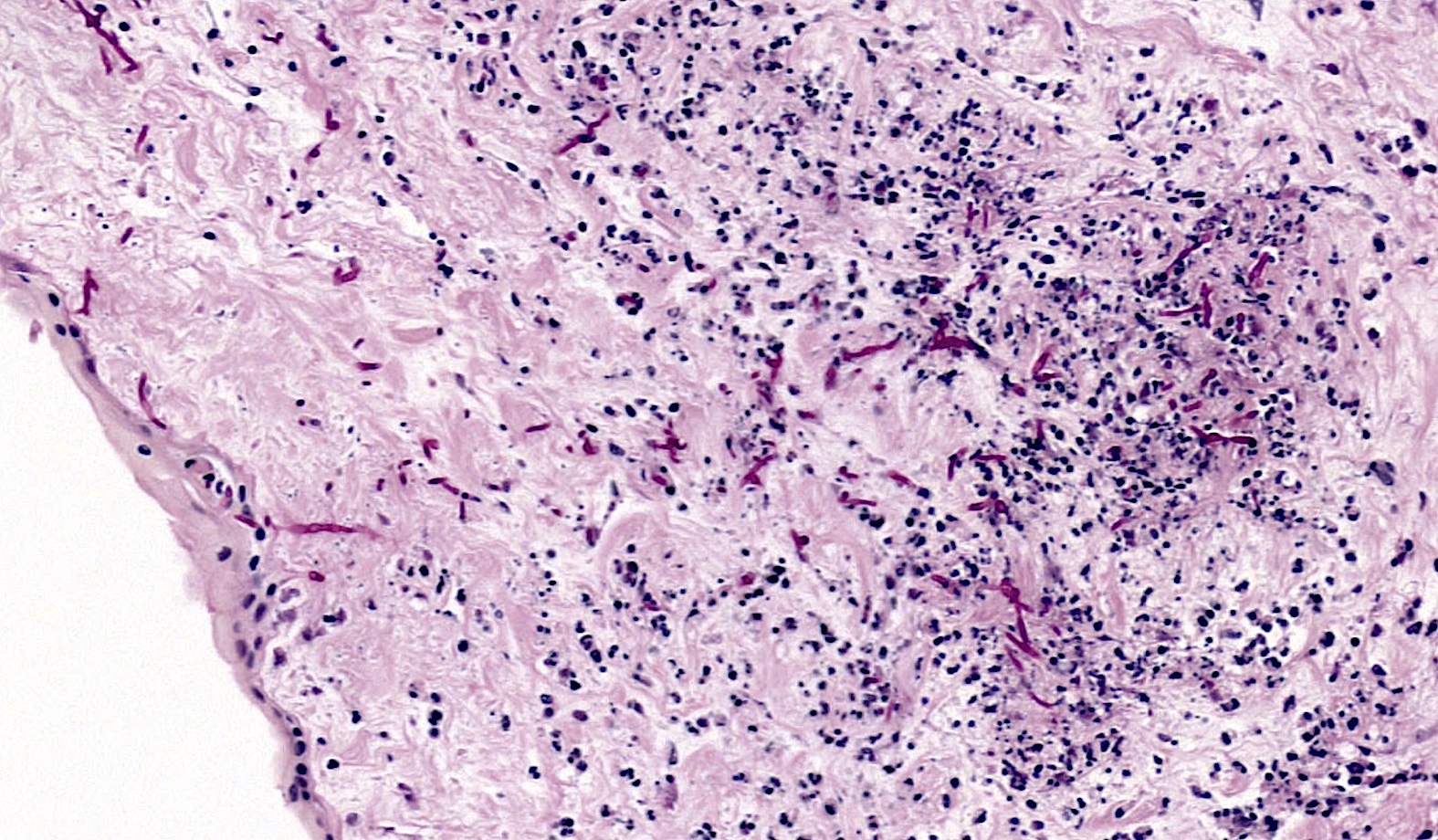
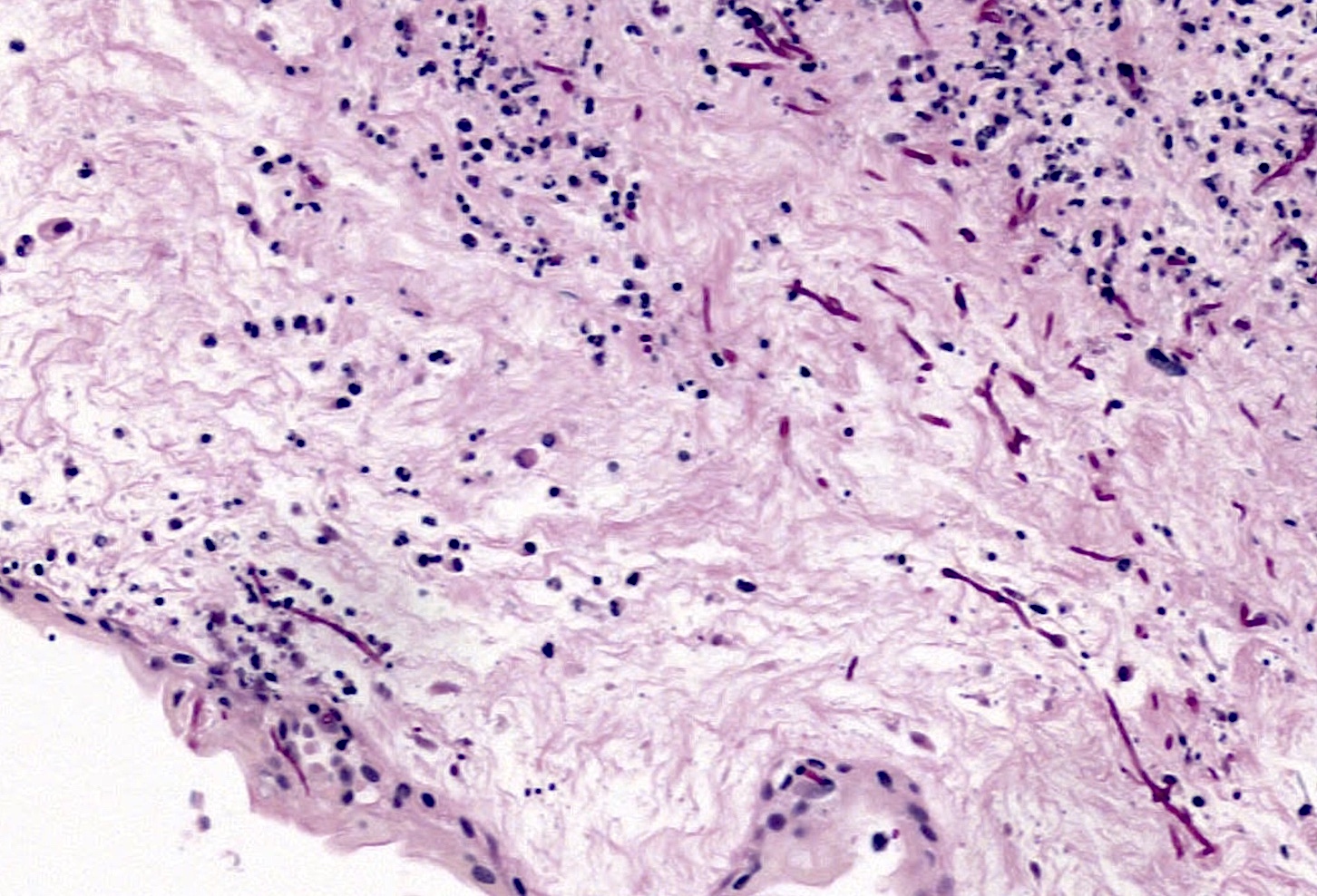
- Peripheral funisitis displays epithelial necrosis and multiple microabscesses involving the periphery of the umbilical cord (and often Candida species can be documented)
- Evidence of meconium exposure may be observed, possibly with meconium induced myocyte necrosis
- Calcification of the immune complexes or cellular debris can be partially or entirely encircling the vessels, particularly with necrotizing funisitis
- Reference: Kraus: Placental Pathology (AFIP Atlas of Nontumor Pathology), 1st Edition, 2005
Microscopic (histologic) images
Positive stains
- GMS / PAS: fungal etiologies, such as Candida species
- Brown-Brenn Gram stain: for bacteria
- Warthin-Starry or Steiner silver stains: spirochetes / syphilis
- Treponema immunohistochemistry: syphilis
- HSV immunohistochemistry: herpes
Sample pathology report
- Placenta, third trimester, spontaneous passage:
- Umbilical cord with panvasculitis, diffuse acute funisitis and peripheral microabscesses (see comment)
- Comment: Colonization with organisms morphologically compatible with Candida species, confirmed by PAS special stain.
Differential diagnosis
- Acute chorioamnionitis:
- Often shows both panvasculitis and funisitis (stage 3)
- Inflammation appears centered around vessels
- Foul smelling specimens, with green tinged and slimy membranes
- Intrauterine fetal demise:
- Vasculitis and funisitis of any degree or distribution possible
- General breakdown and inflammation of delicate membranes
Additional references
Board review style question #1
A 32 year old with no prenatal care presents with premature rupture of membranes and delivers an infant at approximately 31 weeks with Apgars of 5 and 6 at 1 and 5 minutes. At delivery, a maternal fever of 101.5 °F and foul smelling amniotic fluid are identified. The placental surface and fetal membranes are green tinged and opaque. The umbilical cord reveals the features seen in the submitted image (PAS stain). Which of the following gross features would most likely be found on careful macroscopic examination of the umbilical cord?
- Excessive twisting
- Excessively long length
- Peripheral white plaque(s)
- True knot(s)
- Umbilical vein thrombosis
Board review style answer #1
C. Peripheral white plaque(s). While often no macroscopic lesions are seen in cases of mild-moderate umbilical vasculitis or funisitis, gross findings are evident in some circumstances. A common gross finding with funisitis is the presence of peripheral white, creamy or yellowish plaques / lesions, which are often due to infection by Candida species (which is present in the above image). Additionally, white concentric rings may be appreciated around umbilical vessels. This finding is usually associated with necrotizing funisitis and represents the accumulation of dying cells, cellular debris and associated immune complexes that aggregate as arcs around vessels (analogous to the precipitin arcs seen in an Ouchterlony immunodiffusion assay).
Comment Here
Reference: Umbilical vasculitis and funisitis
Comment Here
Reference: Umbilical vasculitis and funisitis
Board review style question #2
A 19 year old G1P0 delivers a healthy term infant with post due dates (40.5 weeks) and Apgars of 9 and 9 at 1 and 5 minutes. Meconium fluid is identified at delivery. Which of the following is the most likely histologic finding in the umbilical cord?
- Arteritis involving one or both umbilical arteries
- Concentric calcifications around umbilical vessels
- Necrotizing funisitis
- Phlebitis involving the umbilical vein
- 3 vessel vasculitis (panvasculitis)
Board review style answer #2
D. Phlebitis involving the umbilical vein. Mild phlebitis (inflammation specifically of the umbilical vein) is a relatively common finding with meconium in the amniotic fluid. Presumably, this is due to the early / developing fetal response toward an injurious agent (meconium).
Comment Here
Reference: Umbilical vasculitis and funisitis
Comment Here
Reference: Umbilical vasculitis and funisitis