Table of Contents
Definition / general | Procedure | Sections to obtain | Tips | Gross description | Gross images | Sample gross description report | Diagrams / tables | Additional references | Board review style question #1 | Board review style answer #1Cite this page: Khan W, Ravishankar S. Grossing. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/placentagrossing.html. Accessed April 20th, 2024.
Definition / general
- This topic describes how to gross specimens obtained from placental deliveries
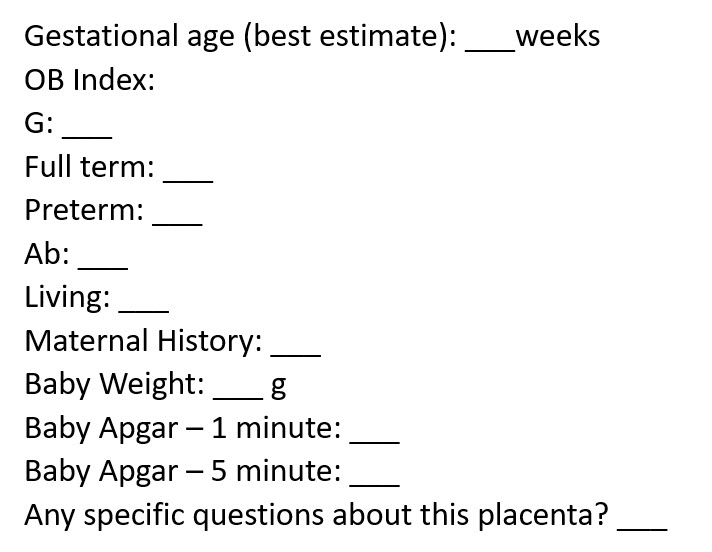
- Essential clinical history:
- Placenta should always be grossed with knowledge and context of the clinical history
- To improve efficiency, institutions may create a specific requisition sheet for placentas that contains this information
- EMR systems are able to automatically populate the requisition from the patient’s chart, limiting the burden on both the clinician / nursing staff and pathologist
- Gestational age at delivery
- Maternal information: gravida (G) and para (P) status
- Maternal history: presence of pregnancy related complications (pre-eclampsia, gestational hypertension, gestational diabetes, intrauterine growth restriction [IUGR], etc.) and prepregnancy disorders (chronic hypertension, pregestational diabetes, obesity, group B streptococci [GBS] status, etc.)
- Clinical presentation and perinatal / labor course:
- Examples: premature rupture of membranes (PROM), vaginal bleeding, maternal fever / clinical chorioamnionitis, nonreassuring fetal heart tracing, meconium stained fluid, etc.
- Neonatal weight
- Neonatal Apgar scores
- Any additional findings or specific questions that the clinical team has about the placenta
- Placental examination in the fresh state is highly preferable to formalin fixed specimens; however, not all institutions may be able to accommodate this preference
- Note that placentas can stay in refrigeration for a relatively long period of time (1 week or more) without significant degradation of histology
- See the Amsterdam consensus statement paper for additional information on placental grossing and sampling (Arch Pathol Lab Med 2016;140:698)
Procedure
- Singleton placentas:
- Remove the placenta from the container, including any detached segments of umbilical cord or blood clots that may be included
- Wipe off excess blood and orient yourself to the major anatomic structures: the fetal surface, maternal surface, cord and membranes
- Umbilical cord:
- Measure the length of the umbilical cord
- If there are detached segments of cord, measure each segment and provide an aggregate / total measurement
- Long cords are > 70 cm
- Measure the average diameter of the umbilical cord
- Note any areas of stricture or thinning
- Inspect the cord insertion and measure the distance to the closest margin
- Abnormal cord insertions include peripheral (< 3.0 cm), marginal (< 0.5 cm), velamentous and furcate
- Note the presence of any amniotic webs and whether they are tight or loose
- Note the degree of coiling
- Hypercoiled: greater than 3 - 4 coils/10 cm
- Hypocoiled: less than 0 - 1 coils/10 cm
- Identify the number of vessels: 2 versus 3
- May need to look at multiple cross sections to determine, correlate with ultrasound imaging reports, if available
- Inspect the entire length of the cord and describe any abnormalities
- Hematomas, cysts / masses, rupture / defects, thrombi, surface nodules or plaques (classic finding in Candida funisitis), true knots
- Note that false knots are clinically insignificant and do not need to be described
- Remove the cord from the placenta at the insertion site
- Measure the length of the umbilical cord
- Extraplacental membranes:
- Assess completeness of membranes
- Locate the membrane rupture site and measure distance from the closest placental edge
- Evaluate the color and opacity of the membranes
- Normal: translucent
- Green stained: meconium
- Brown stained: hemosiderin
- Opaque: chorioamnionitis
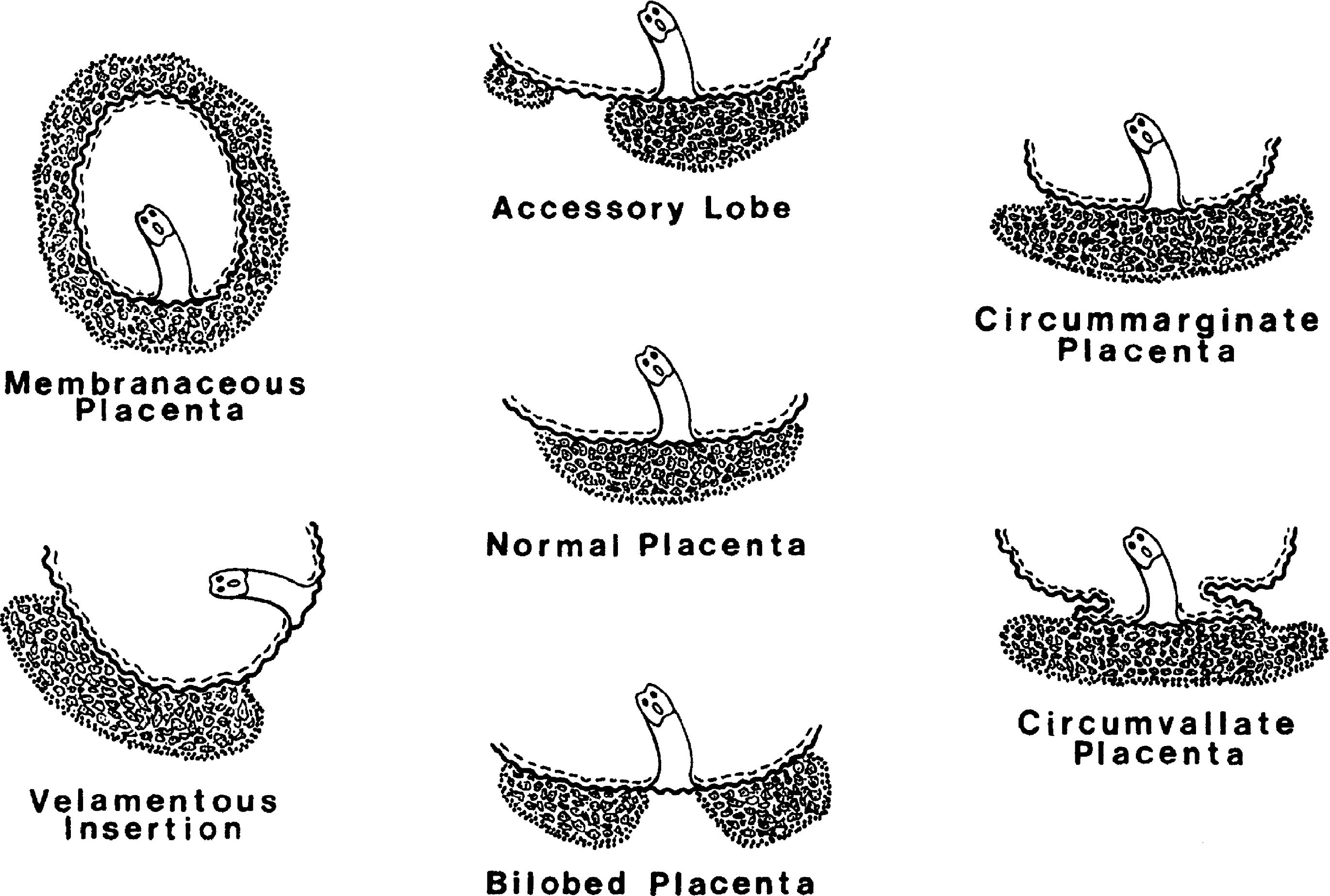
- Assess the membrane insertion into the placental disc
- Marginal (normal), circummarginate, circumvallate
- If velamentous insertion, assess the intactness of the membranous vessels and describe any areas of disruption
- After taking membrane rolls, remove the membranes from the placenta
- Placental disc:
- Measure the placenta in 3 dimensions
- Weigh the placenta (most reference tables use the trimmed weight [i.e., the weight of the placenta after removal of the cord and membranes])
- Assess the shape of the disc
- Discoid, bilobed, multilobate, accessory lobes
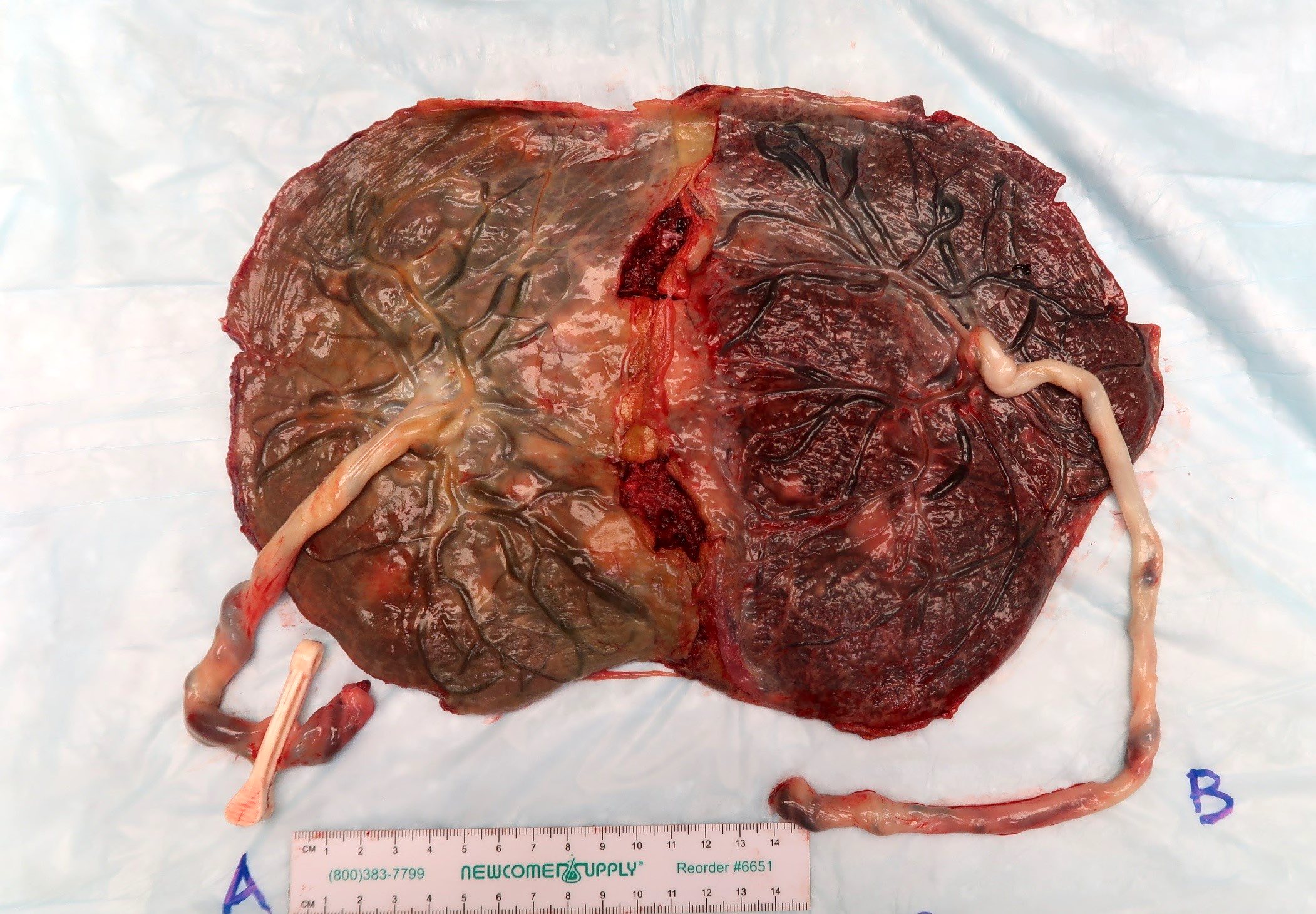
- Measure the size of any accessory lobes (may be multiple) and note their distance from the main placental disc and whether the connecting membranous vessels are intact
- Assess the fetal surface
- Color, opacity, subamniotic hemorrhage
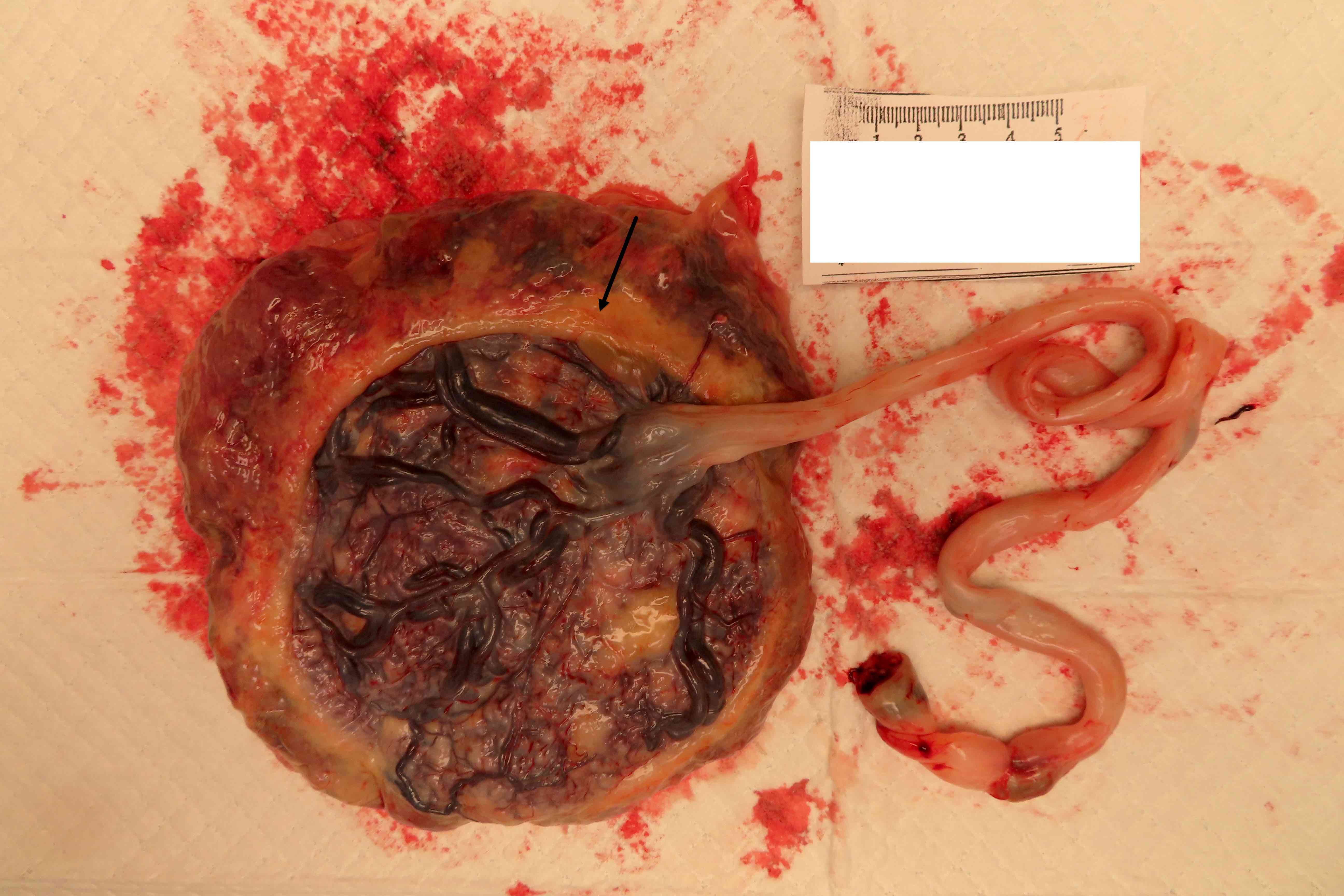
- Presence of squamous metaplasia (small white nodules that do not rub off; clinically insignificant), amnion nodosum (small white-yellow nodules that do rub off; clinically significant, associated with oligohydramnios)
- Note any nodules, masses or cysts
- Examine the fetal vessels for thrombi or disruption (particularly in abnormal cord insertions)
- Note the amount of subchorionic fibrin deposition (optional)
- Subchorionic fibrin is normal and does not necessarily need to be described or sampled unless extensive
- Assess the maternal surface
- Determine if the maternal surface is complete; are all cotyledons present?
- Disrupted but appears complete; there is disruption of the surface but no missing tissue
- Disrupted, possibly incomplete; there is disruption of the surface with missing tissue
- In these cases, ink the junction of the intact and disrupted maternal surface and take additional sections of the junction (Mod Pathol 2020;33:2382)
- Fragmented: there are portions of the placenta that are entirely detached from the main disc
- Retroplacental blood clots:
- Central or marginal?
- Compression of underlying villous parenchyma
- Firm lesions in underlying villous parenchyma
- Areas of atrophy / thinning of the placental parenchyma
- Palpate the entire placenta for firm areas; let your fingers do the walking
- Serially section the placenta at 5 mm intervals
- Assess the color of the villous parenchyma
- Normal: dark red
- Pale: may represent areas of avascular villi
- Examine the cut surfaces carefully for lesions
- Color, consistency, size in 3 dimensions, location relative to the fetal and maternal surface and placental margin
- Single versus multiple lesions
- Percentage of villous tissue with lesions involved
- Determine if the maternal surface is complete; are all cotyledons present?
- Multiple gestation placentas:
- Dichorionic twins:
- Separate with no dividing membrane: gross as 2 separate singletons
- Separate with a dividing membrane: evaluate the dividing membrane as described below, then gross as 2 separate singletons
- Fused with a dividing membrane: evaluate the dividing membrane as described below, then pull the 2 placentas apart and gross as 2 separate singletons
- Monochorionic twins:
- Gross as a single placenta as described below
- Umbilical cord:
- Determine if the cords are oriented with regard to which corresponds to twin A versus twin B (often done with cord clamps)
- If the cords are not oriented, assign a random orientation for placenta A versus placenta B and maintain that orientation throughout the gross description and section code
- Extraplacental membranes:
- Monochorionic monoamniotic: no dividing membrane
- Monochorionic diamniotic: dividing membrane consists of 2 layers of amnion, should be thin and translucent
- Dichorionic diamniotic: dividing membrane consists of 2 layers of amnion and 2 fused chorions
- If a dividing membrane is present, take a membrane roll of it
- Placental disc:
- Monochorionic twins:
- Evaluate the percentage of vascular territory belonging to each twin
- Keep in mind that the dividing membrane does not necessarily correspond to the vascular division
- Can have clinically significant vascular anastomoses, which should be documented if possible
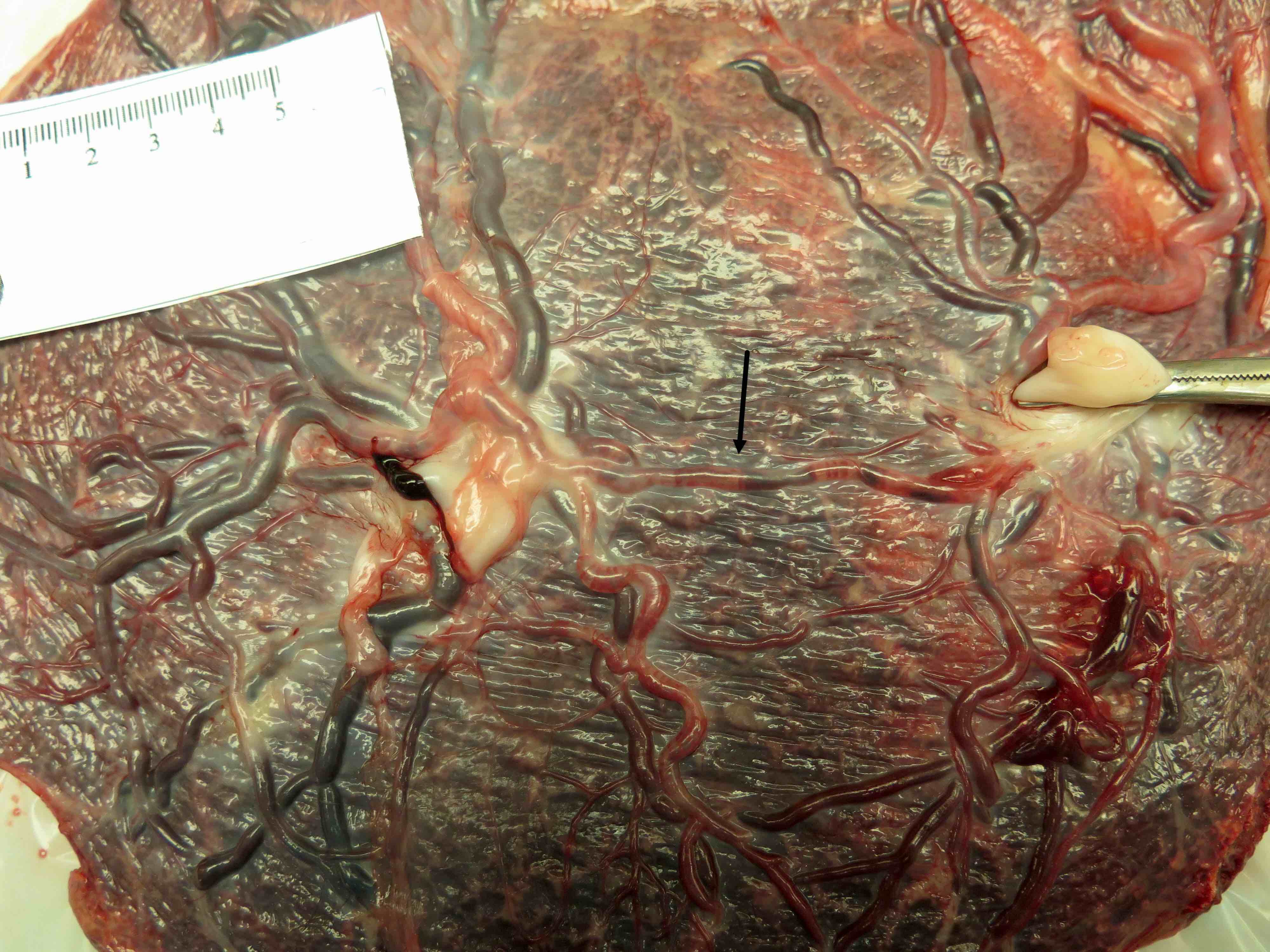
- Inspect the fetal surface carefully for surface anastomoses between the 2 twins
- Arteries pass over veins
- Can have artery to artery, artery to vein or vein to vein anastomoses
- Perform injection studies to evaluate for deep anastomoses (Pediatr Dev Pathol 2013;16:237)
- Various techniques have been described, including ink, milk and air
- Inject an artery / vein on 1 placenta and trace any flow that crosses into the vascular territory of the other placenta
- Evaluate the percentage of vascular territory belonging to each twin
- Dichorionic twins:
- Process as 2 separate singleton placentas
- Monochorionic twins:
- Dichorionic twins:
Sections to obtain
- Singleton placentas:
- Umbilical cord (1 block with 2 cross sections): 1 from the proximal one - third of the cord and 1 from the distal one - third of the cord
- Additional sections of any lesions as needed
- Membrane rolls (1 block with 2 cross sections):
- Remove a sliver of the marginal placental parenchyma at the site of membrane attachment
- Be sure to include the area of circummarginate or circumvallate membrane attachment in your section, if present
- Grasp the sliver of parenchyma in smooth forceps and wrap the membranes around the forceps with the amnion on the outside
- Cut a cross section of the roll to submit for histology
- Create 2 separate membrane rolls, each with a single cross section submitted
- Cord insertion site (1 block)
- 1 full thickness section of the placental parenchyma at or adjacent to (if velamentous insertion) the cord insertion site
- Placental parenchyma (2 blocks)
- Full thickness sections of representative random placental parenchyma, taken from the central two - thirds of the placental disc
- Do not sample the margin of the placenta unless it is to demonstrate a lesion
- Full thickness sections of representative random placental parenchyma, taken from the central two - thirds of the placental disc
- Abnormalities / lesions
- 1 representative section of each type of lesion should be submitted; if multiple grossly identical lesions are identified, it is only necessary to submit 1 of them for histologic examination
- Lesions that should be submitted include: infarcts, thrombi, masses, pale areas of parenchyma
- Lesions that do not need to be submitted include: areas of atrophy, accessory lobes, subchorionic fibrin (unless extensive)
- If the placenta is disrupted, possibly incomplete or fragmented, submit an additional block with at least 3 perpendicular cross sections of the basal plate only (not full thickness), adjacent to the area of disruption
- The purpose of this block is to look for myometrial fibers that may be adherent to the basal plate
- 1 representative section of each type of lesion should be submitted; if multiple grossly identical lesions are identified, it is only necessary to submit 1 of them for histologic examination
- Umbilical cord (1 block with 2 cross sections): 1 from the proximal one - third of the cord and 1 from the distal one - third of the cord
- Multiple gestation placentas:
- Same as singleton placentas, with the addition of the dividing membrane roll, which should be submitted as its own separate block
- References: Placenta 2003;24:116, APMIS 2018;126:544
Tips
- While placentas should be grossed fresh, sections may be difficult to cut to the appropriate thickness to allow for adequate fixation and processing
- Place the membrane rolls and the sections of placental parenchyma in a cup of formalin and allow to fix for 1 - 2 hours before trimming, taking and submitting the final sections
- If the placenta is too thick to fit a full thickness section in 1 cassette, submit 2 cassettes with the fetal surface (cord insertion site and 1 random section) and 1 with the maternal surface
- If the completeness of the maternal surface is questionable, it is helpful to take a photograph for review at a later date, if needed
- Photographing the fetal surface in monochorionic twin placentas can be helpful for subsequent evaluation for surface anastomoses; remember to wipe the blood off the surface before photographing
Gross description
- Acute chorioamnionitis: opaque membranes or fetal surface with slight yellow discoloration
- Candida funisitis: tan-white to tan-yellow plaques on the surface of the umbilical cord
- Amnion nodosum: white-yellow or yellow-green nodules on the fetal surface, measuring up to X cm
- Chorangioma: tan-red to tan-yellow well circumscribed nodule / mass, measuring XX cm, located at the cord insertion site / X cm from the margin
- Chronic abruption: brown stained membranes, marginal retroplacental hematoma, circumvallate membrane insertion
- Infarct / perivillous fibrin plaque: tan-white or tan-yellow firm lesion, measuring XX cm and located X cm from the margin
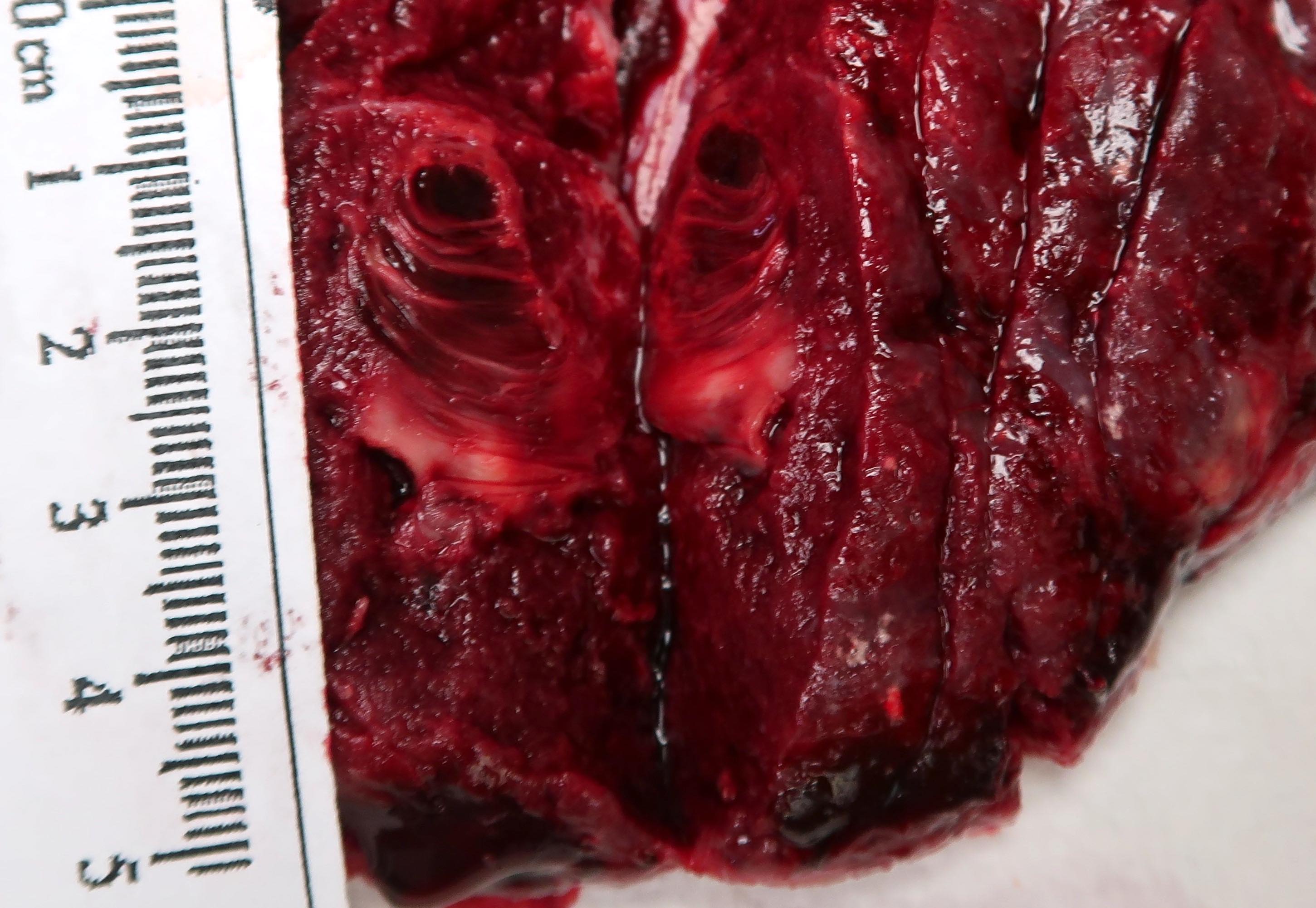
- Intervillous thrombus: dark red lamellated lesion, measuring XX cm and located X cm from the margin
- Massive perivillous fibrin deposition / maternal floor infarction: firm areas distributed throughout the placental parenchyma / along the basal plate, involving approximately X% of the placental parenchyma
- Meconium staining: green stained membranes, umbilical cord or fetal surface
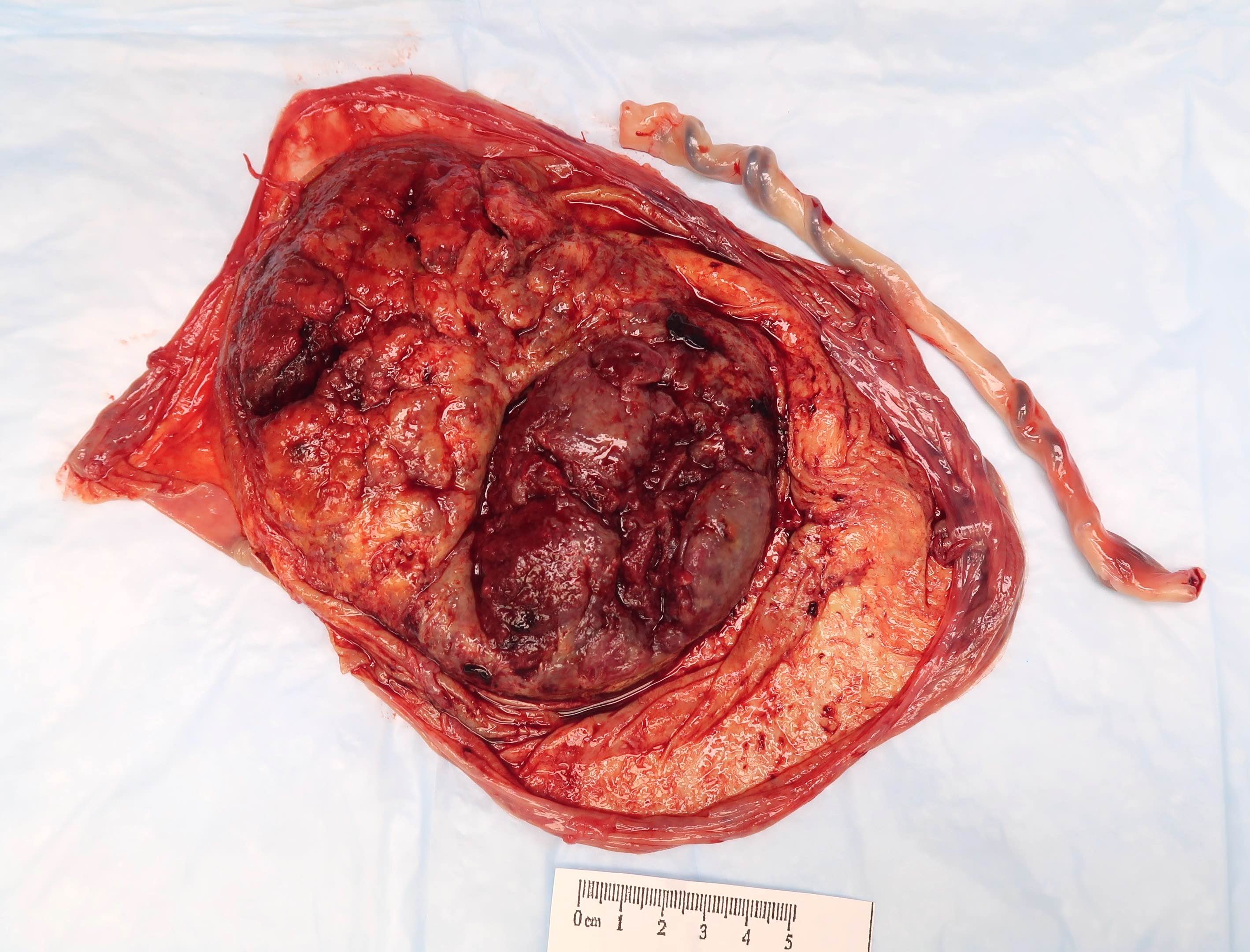
- Retroplacental hematoma: maternal surface with central / marginal dark red blood clot, with or without indentation of the overlying placental parenchyma
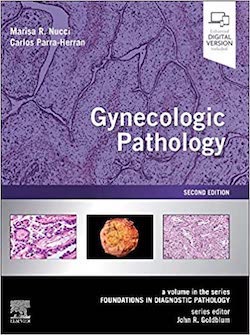
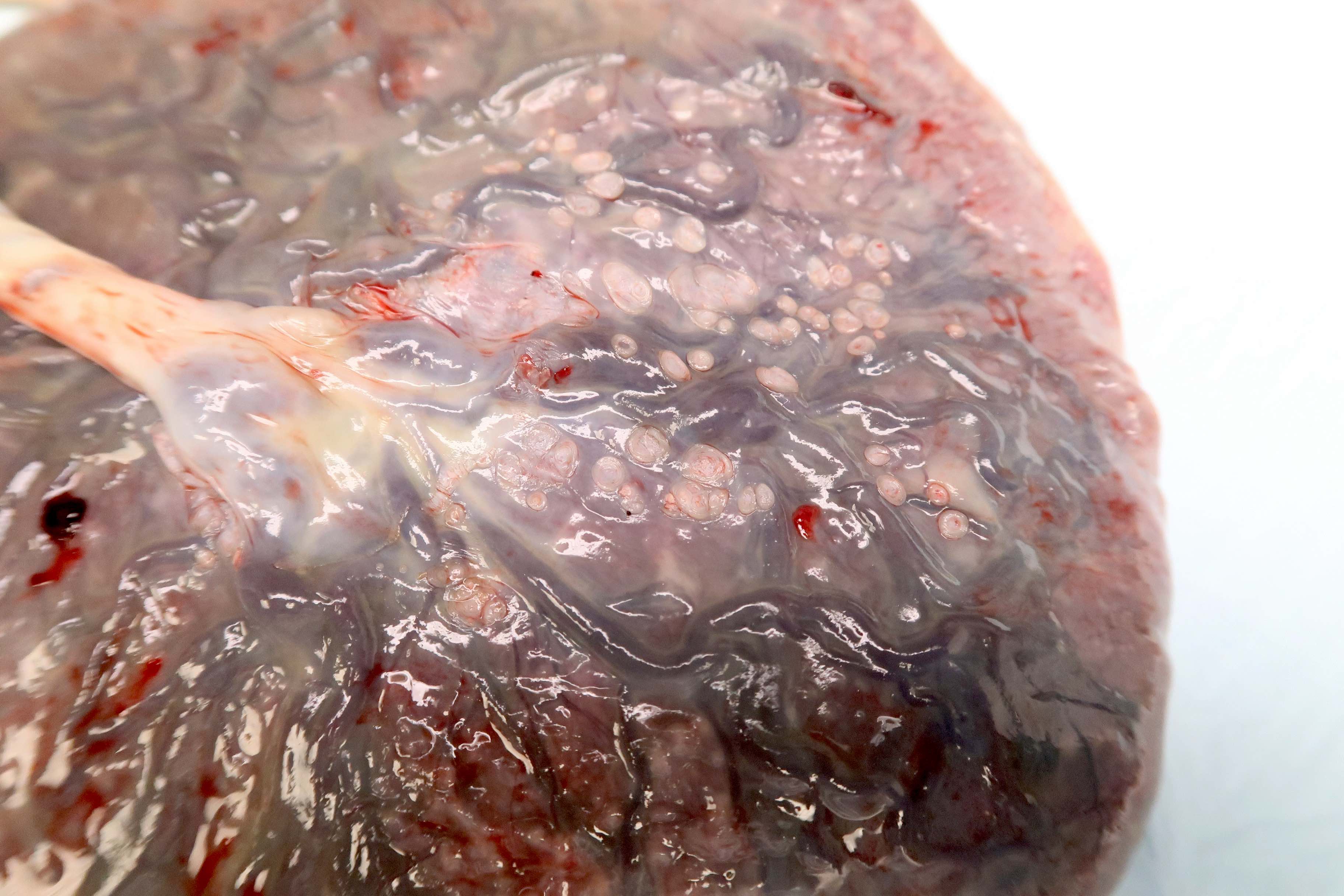
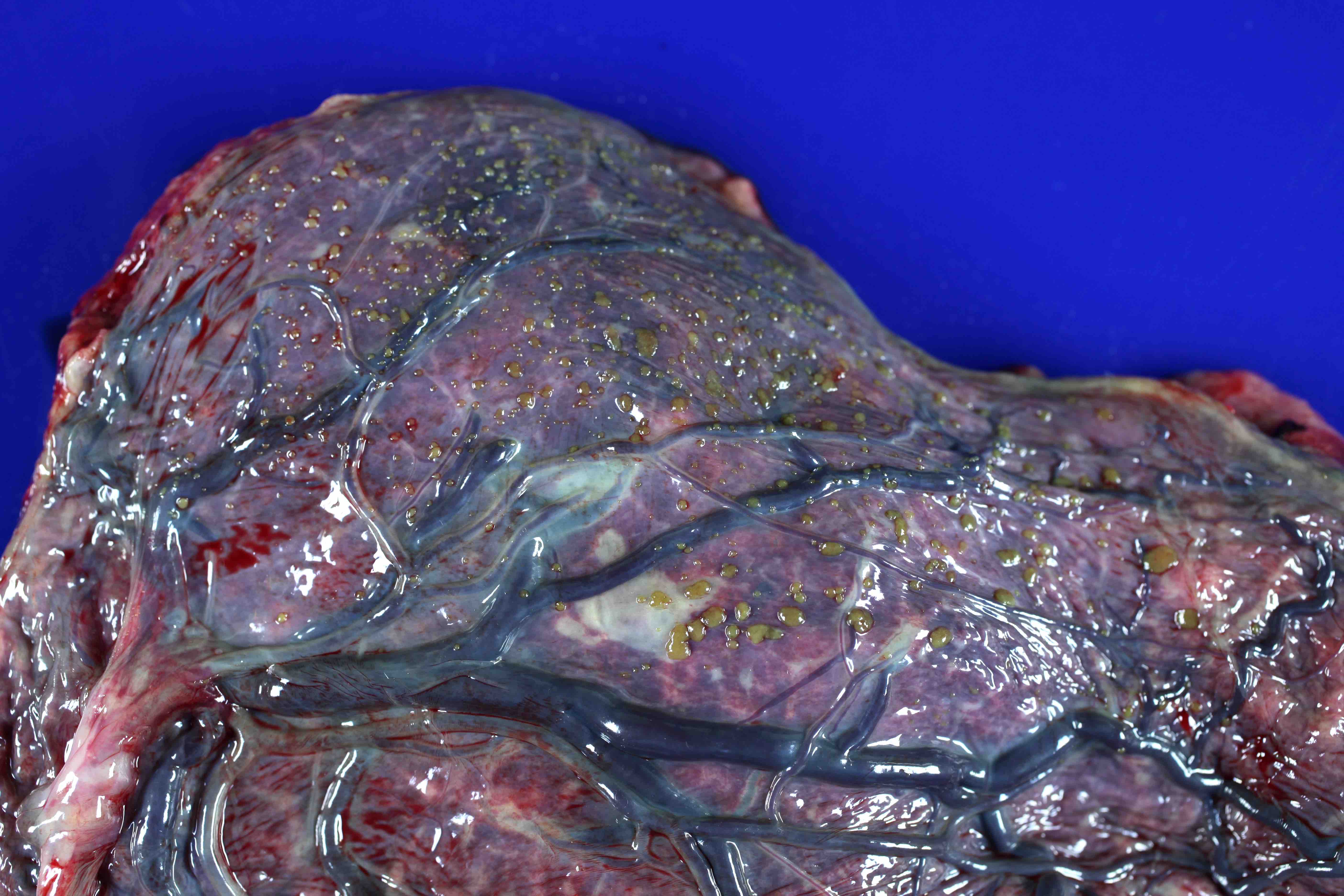
Gross images
Contributed by Sanjita Ravishankar, M.D.
Sample gross description report
- Received fresh, labeled with the patient’s name and hospital number, is a placenta. The placental membranes are translucent and complete. The membrane insertion is marginal. The point of membrane rupture is 4.0 cm from the nearest margin. The umbilical cord is pale yellow, 40 cm in total length and inserts in the placenta, 5.0 cm from the margin. There are up to 2 coils per 10 cm. On cut section, the cord has 3 vessels and measures 1.0 x 1.4 cm. The placenta is discoid, 17 x 15 x 2.5 cm and weighs 420 g without cord or membranes. The fetal surface is blue-red and translucent. The maternal surface is complete. The cut surface is dark red and spongy. No gross abnormalities are noted. Representative sections are submitted in 5 cassettes.
- Summary of cassettes:
- A1: umbilical cord sections
- A2: membrane rolls
- A3: placental parenchyma, umbilical cord insertion site
- A4 - A5: placental parenchyma
Diagrams / tables
Additional references
Board review style question #1
Which of the following statements is true regarding appropriate gross handling of the placental finding depicted above?
- Clinically insignificant and does not need to be described
- Does not occur more than once in the same placenta
- Should be sampled as part of routine sections
- Status of the connecting vessels and distance from the main disc are important to describe
Board review style answer #1
D. Status of the connecting vessels and distance from the main disc are important to describe
Comment Here
Reference: Placenta - Grossing
Comment Here
Reference: Placenta - Grossing