Table of Contents
Definition / general | Essential features | ICD coding | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Gross description and processing | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Iczkowski KA. Biopsy. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/prostatecore.html. Accessed April 19th, 2024.
Definition / general
- Biopsies may be taken in several formats
- Systematic approach may involve sextant (6) samples from selected regions of prostate by a spring loaded 18 gauge biopsy
- Currently, up to 18 samples are taken; more for mapping biopsies (J Urol 2019;202:264)
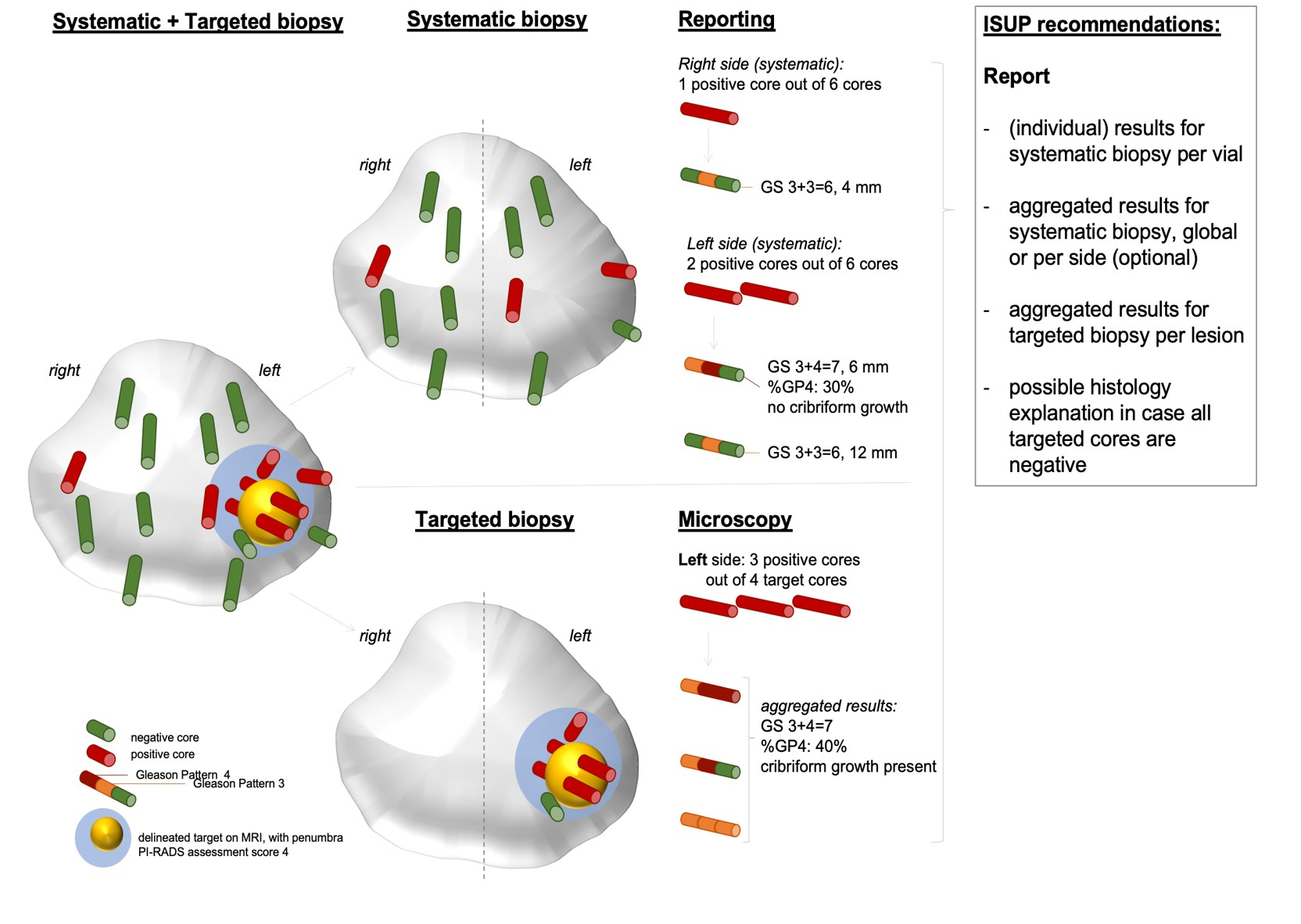
- Region of interest (ROI) biopsies at a multiparametric MRI targeted lesion carry greater sensitivity for cancer detection and prognosis (Hum Pathol 2018;76:68)
- Sampling may be region of interest only, systematic only or combined
Essential features
- 4 strongest features for cancer diagnosis: an infiltrative (rather than clustered) pattern of acini, nuclear enlargement, prominent nucleoli and loss of basal cells
- 2019 International Society of Urological Pathology (ISUP) biopsy reporting requirements:
- Report the percentage Gleason pattern 4 for all Gleason score 7
- Intraductal carcinoma presence should be mentioned and it should be graded when in the presence of invasive cancer and not graded when an isolated finding
- Cribriform carcinoma presence / absence in Gleason 4 cancer should be specified
- For systematic biopsies, Gleason score (ISUP grade group) should be reported per individual site, whereas for an MRI targeted biopsy, a global (aggregate) score should be reported for each region of interest
- Note: the presence of intraductal carcinoma should be noted
- Isolated (pure) intraductal carcinoma should not be graded (consensus recommendation by ISUP and GUPS)
- In the presence of invasive carcinoma, incorporation of the intraductal carcinoma component in the Gleason score remains debatable and requires further studies (see pros and cons on reporting IDCP with coexisting invasive carcinoma in a recent review (Histopathology 2021;78:231, Pathology 2020;52:192, Histopathology 2021;78:342)
ICD coding
- ICD-9:
- ICD-10:
- ICD-11: 2C82.Z - malignant neoplasms of prostate, unspecified
- As of 2014, Medicaid has limited the number of biopsy sites to 9 for full 88305 reimbursement so some practices are capping the number of biopsies at 9
Clinical features
- 25% of tumor bearing specimens contain only a small focus of carcinoma
- Transperineal biopsies are alternative approach to transrectal biopsies
- Gleason score in biopsy correlates with that of prostatectomy (same: 58%, variable 1 unit: 92%)
- Tumor seeding of needle tract is a rare complication of perineal needle biopsy; more likely with poorly differentiated carcinomas and less common with transrectal biopsy (BJU Int 2015;115:698)
- Findings at 12 core transrectal ultrasound guided prostate needle biopsy plus preoperative PSA predict advanced local disease at prostatectomy (Am J Clin Pathol 2012;137:739)
Diagnosis
- Common cancer features are nucleomegaly (96%), infiltrative growth pattern (88%), intraluminal secretions (78%), prominent nucleoli (64%), associated high grade prostatic intraepithelial neoplasia (PIN) (40%), amphophilic cytoplasm (36%), hyperchromatic nuclei (30%), intraluminal crystalloids (22%)
- Uncommon features are perineural invasion (2%), collagenous micronodules (2%), mitotic figures (2%) (Mod Pathol 1998;11:543)
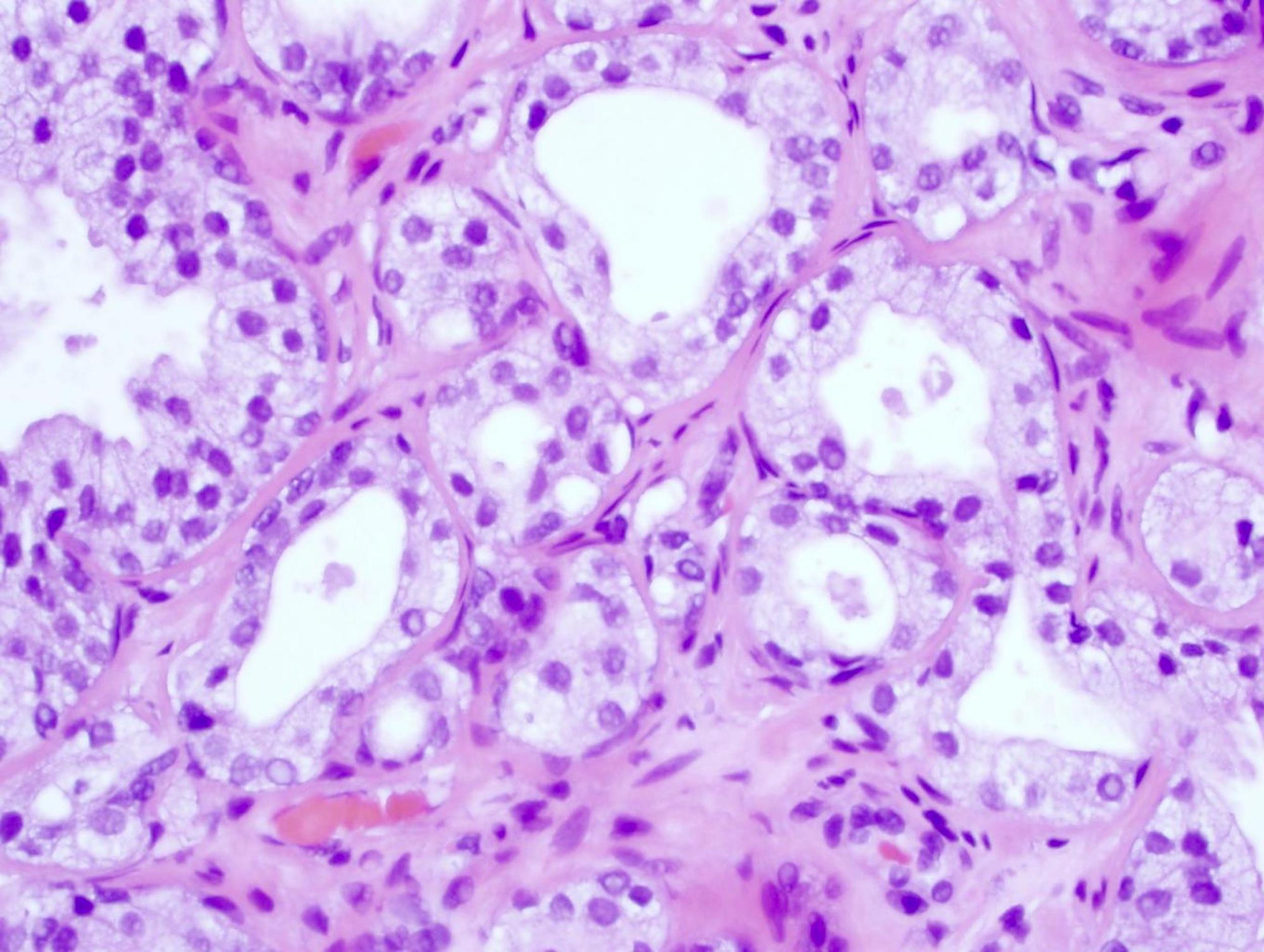
- Glomerulations are rounded tufts of cancer cells within glands reminiscent of renal glomeruli;
- Glomerulations are present in 5% of radical prostatectomy specimens (5 - 20% of each tumor) and 3% of needle biopsies with cancer (5 - 10% of each cancer)
- They are not observed in benign lesions (Hum Pathol 1998;29:543)
- Glomerulations are rounded tufts of cancer cells within glands reminiscent of renal glomeruli;
- Photo essay of general principles (Ann Diagn Pathol 2014;18:301)
- Minimal cancer on biopsy is defined as < 1 mm but there is usually pathologically significant tumor at prostatectomy
- Collagenous micronodules are nodular masses of paucicellular, eosinophilic, fibrillar stroma that impinge on acinar lumens (Arch Pathol Lab Med 1995;119:444)
- Reporting of prostate cancer for each specimen part includes the fraction of biopsy cores or fragments that are involved by cancer and either the percent of each involved core on the slide or the length in millimeters of each involved core on the slide (Am J Surg Pathol 2020:44:e87)
- For example: prostatic adenocarcinoma, Gleason 3+4 (score = 7) within 20% and 40% of 2 out of 3 core fragments, tumor lengths 3 mm and 5 mm
- Perineural invasion and extraprostatic extension should be mentioned in the line diagnosis if present
- If absent throughout the tumor, a comment at the conclusion of the line diagnoses should mention the absence of these findings
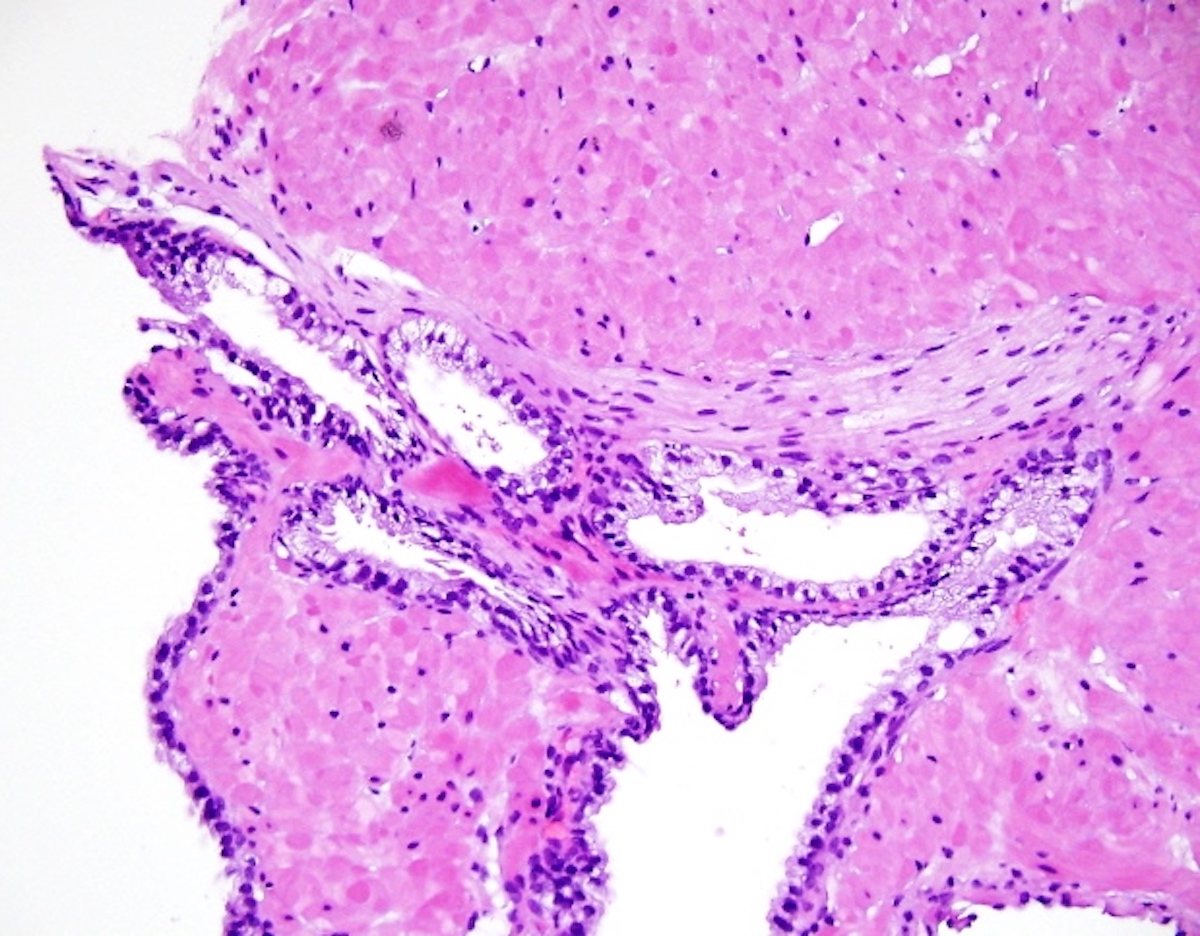
- Caution should be taken with perineural invasion, as perineural impingement by benign acini can mimic invasion by cancer (see Figure 2 below)
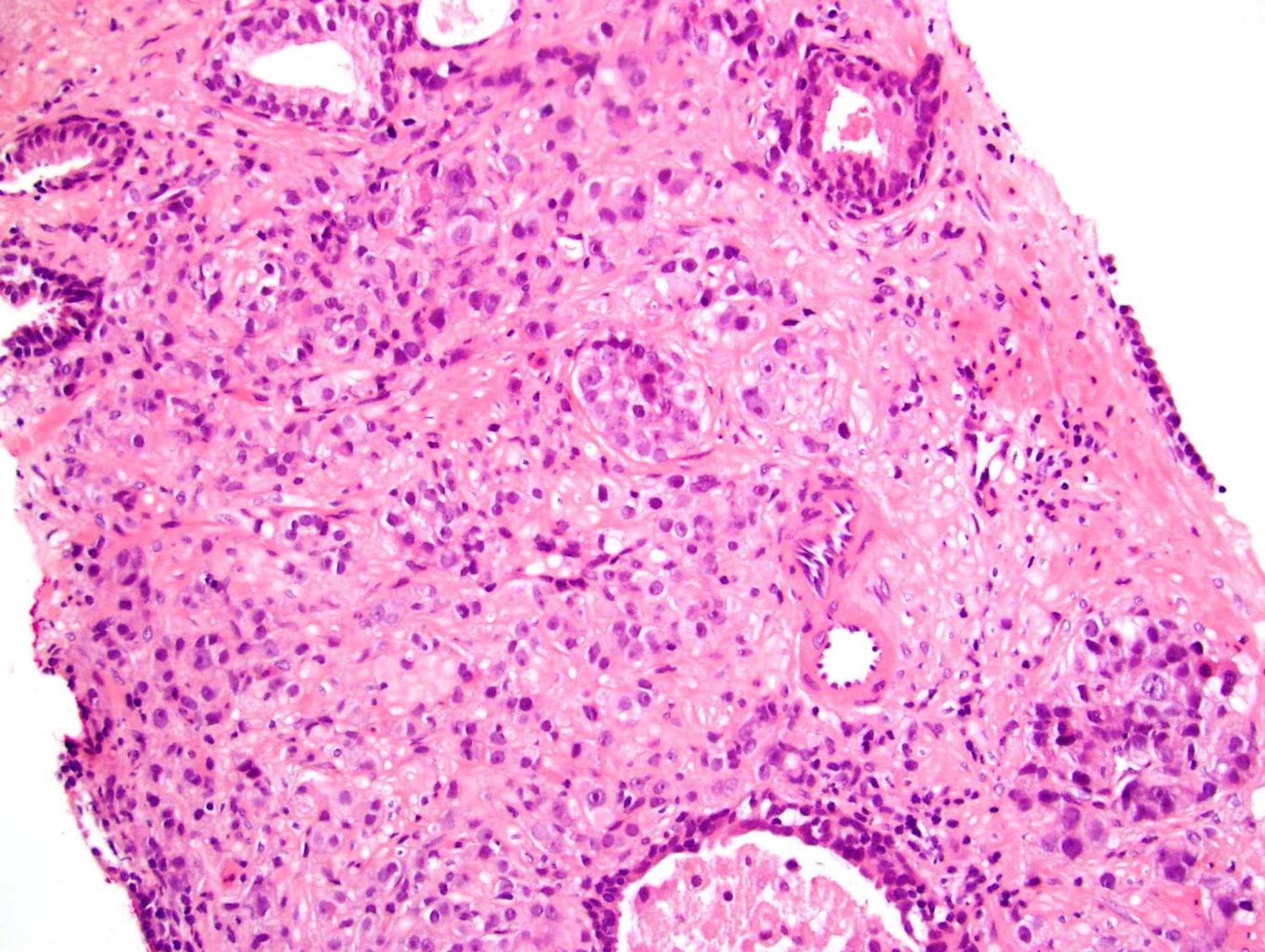
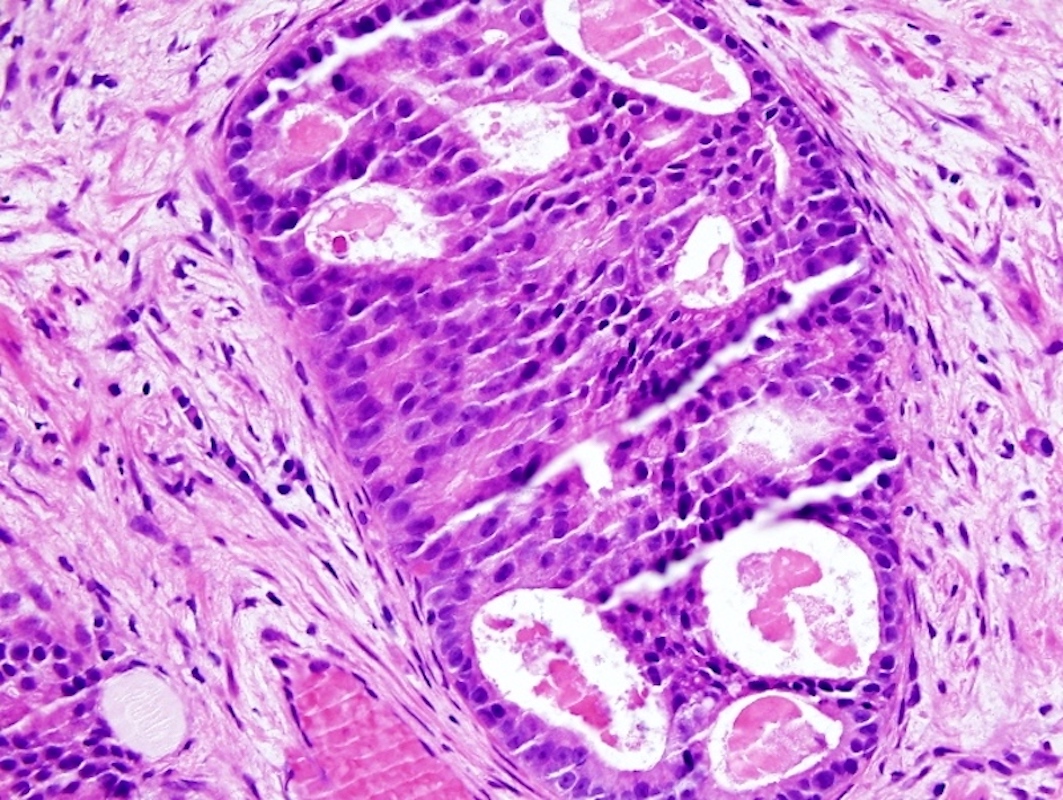
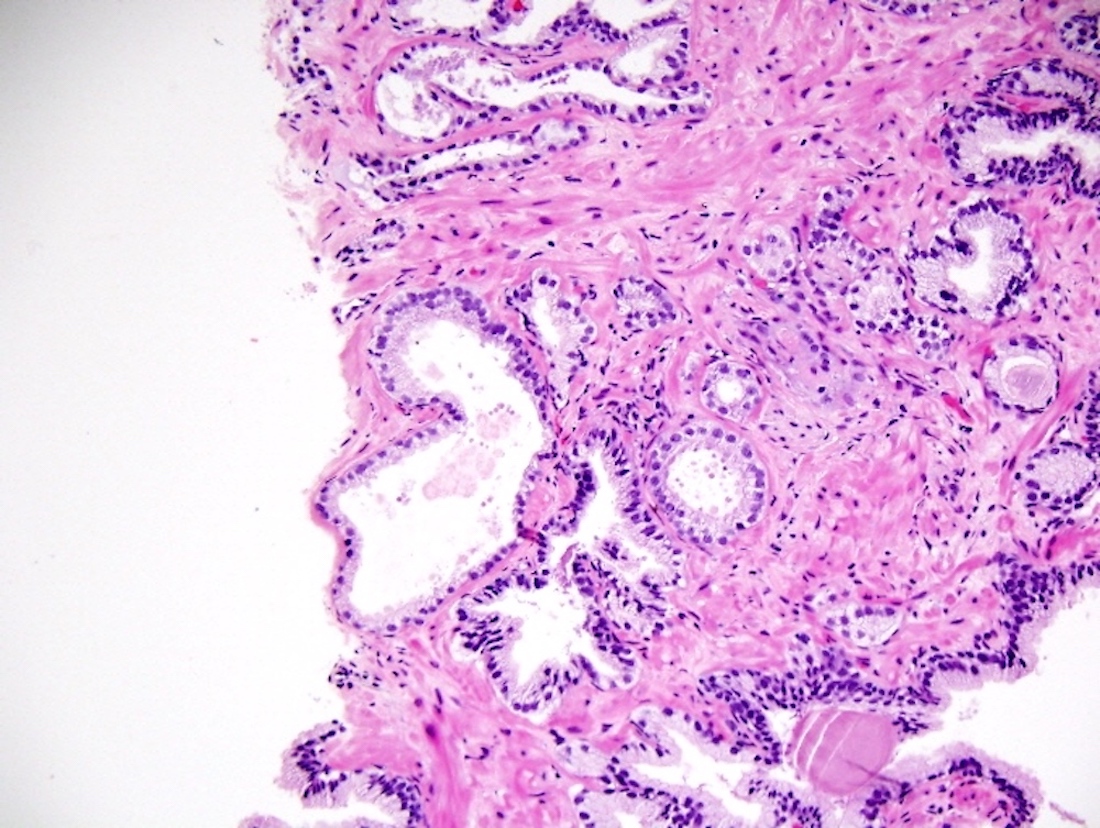
- Intraductal prostate carcinoma (IDC) should be recognized
- An uncommon finding in biopsies, intraductal prostate carcinoma consists of a cribriform to solid, large, often dilated gland space, bounded by basal cells, that contains cells with marked nuclear enlargement and atypia which exceeds the atypia in high grade prostatic intraepithelial neoplasia (see Figure 6 below)
- Intraductal prostate carcinoma has characteristic genetic alterations (Mod Pathol 2013;26:587)
- Intraductal prostate carcinoma almost always occurs with invasive carcinoma and the invasive component is almost always high grade
- Intraductal prostate carcinoma must be mentioned, whether isolated or associated with invasive carcinoma
- ISUP and GUPS disagree on whether intraductal prostate carcinoma should be graded into the invasive cancer or not counted for grading (Am J Surg Pathol 2020:44:e87, Arch Pathol Lab Med 2021;145:461)
- This may infrequently alter overall grade; intraductal prostate carcinoma is not graded when an isolated finding (Histopathology 2020;77:503)
- Intraobserver agreement, even among expert urologic pathologists, is only mediocre and certain findings interfere with consensus, although immunostains may help (Ann Diagn Pathol 2014;18:333)
- ISUP and GUPS disagree on whether intraductal prostate carcinoma should be graded into the invasive cancer or not counted for grading (Am J Surg Pathol 2020:44:e87, Arch Pathol Lab Med 2021;145:461)
- Targeted biopsy reporting is different
- Aggregated findings of all cores sampled per region of interest (ROI) should be reported
- If the targeted cores are negative, the nonneoplastic findings (particularly inflammation) should be reported to explain the radiologic false positive abnormality (see Diagram 1 above) (Hum Pathol 2018;76:68)
- Adequacy: biopsy is unsatisfactory if no prostatic glands or stroma are found; stroma only may indicate a stromal hyperplastic nodule and is satisfactory
- Use of second opinion:
- Second opinion of core biopsies from outside institutions is beneficial before radical prostatectomy is performed (Am J Surg Pathol 1996;20:851, Int J Clin Exp Pathol 2011;4:468)
- Standard practice at NCI designated comprehensive cancer centers
- Second opinion produces Gleason scores on biopsy that are significantly more predictive of radical prostatectomy findings than the outside diagnoses
- More errors occur with Gleason score 6, which tends to underestimate the prostatectomy Gleason score (Am J Surg Pathol 1997;21:566)
- Pure Gleason 3 cancer may be managed by watchful waiting, thus second opinions are particularly called for to help discriminate the threshold between Gleason 3+3 (grade group 1) and Gleason 3+4 (grade group 2)
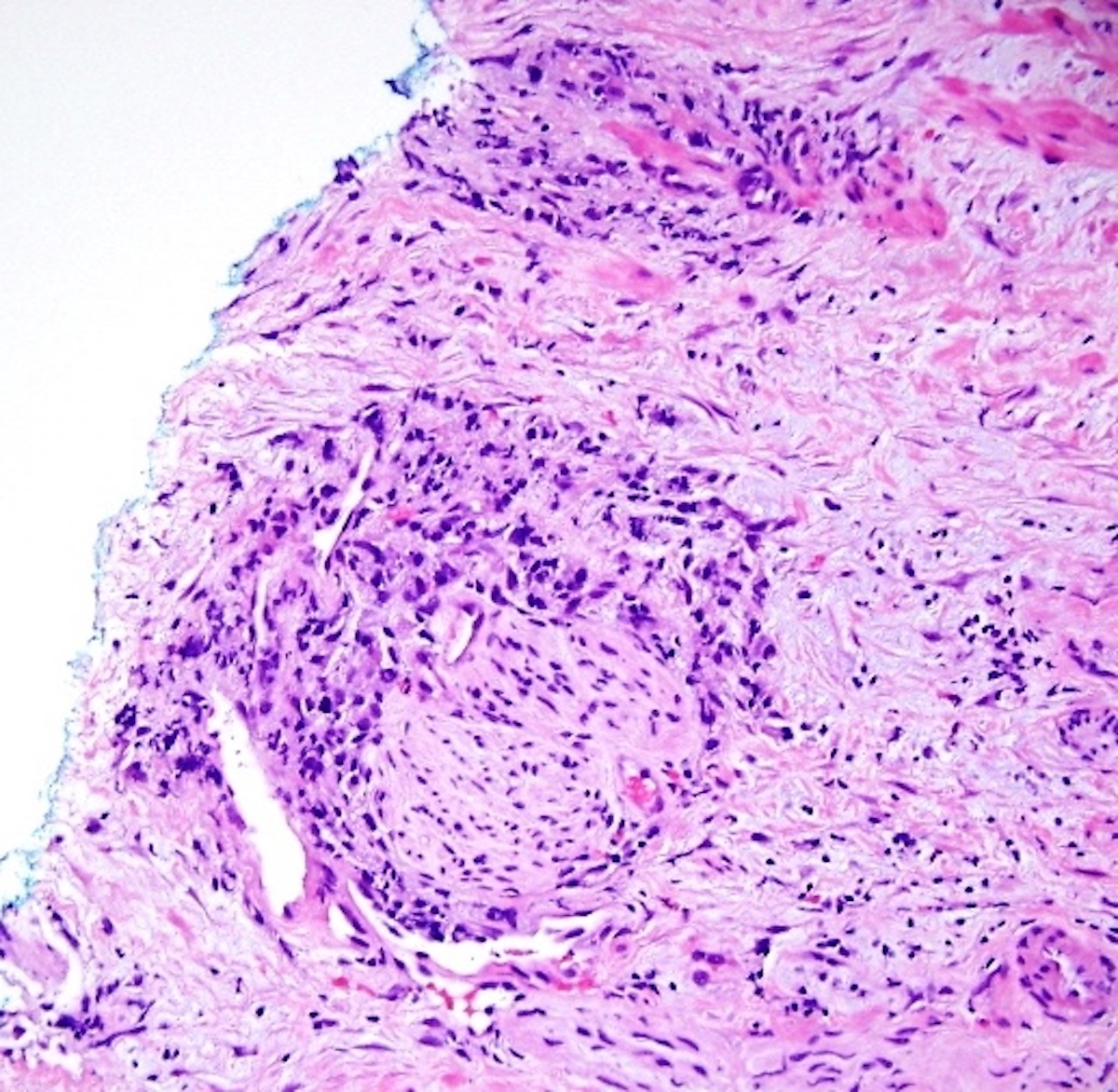
- Most important finding missed by outside pathologists is extraprostatic extension (EPE), which elevates the tumor stage from T2 to T3a (see Figure 3 below)
- In a cohort of 65 cases, 11 patients had EPE
- In 5 of those 11 patients, the outside pathologists failed to comment on the presence of the EPE (Int J Clin Exp Pathol 2011;4:468)
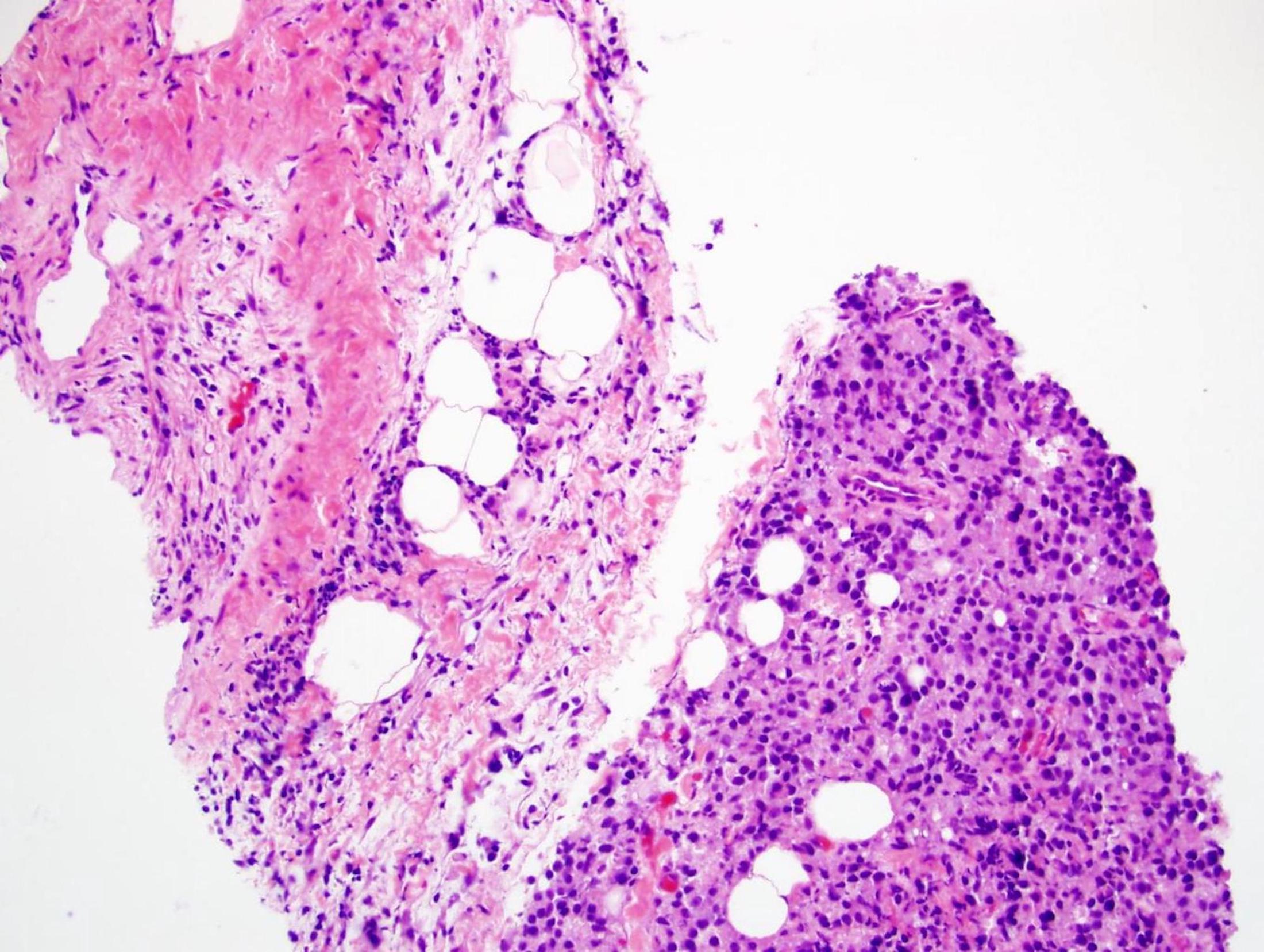
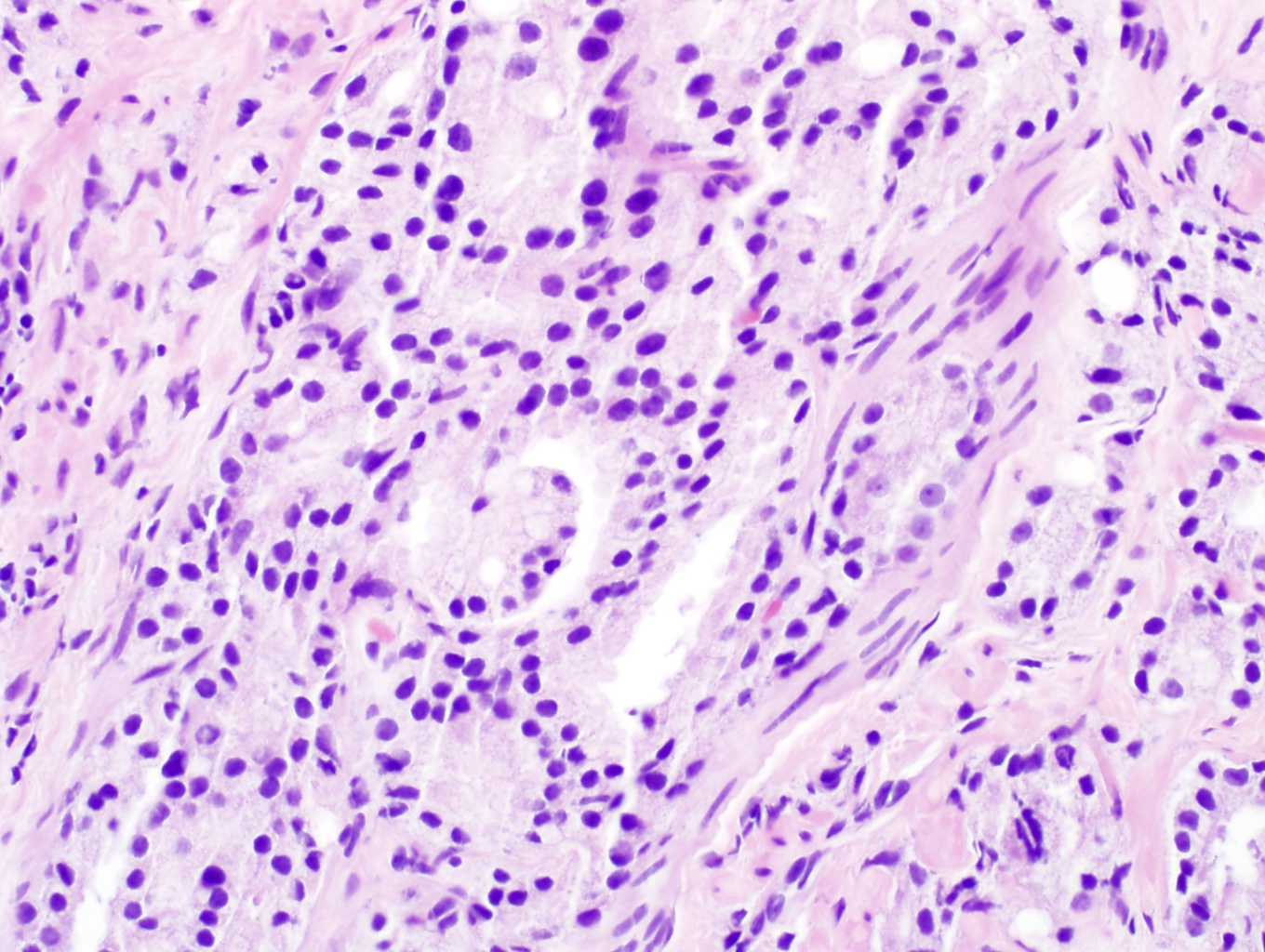
- Another finding that is easily missed yet sometimes overcalled is grade 5 prostate cancer (see Figure 4 below) (Urology 2012;79:178)
- If there are single cells or clusters of cells without even the tiniest lumen formation, a component of Gleason grade 5 cancer should be diagnosed
- It often forms a secondary part of the Gleason score; that is, 3+5 or 4+5
- Gleason grade 5 cancer, however, may itself mimic inflammatory cells (see Figure 5 below)
- Second opinion of core biopsies from outside institutions is beneficial before radical prostatectomy is performed (Am J Surg Pathol 1996;20:851, Int J Clin Exp Pathol 2011;4:468)
Laboratory
- Serum prostate specific antigen is often elevated above 4 ng/mL
- Some urologists use 2.5 ng/mL as a more sensitive but less specific threshold for biopsy (Urol Int 2010;84:141)
Prognostic factors
- In order to facilitate prognosis, certain reporting standards are endorsed by CAP Cancer Protocols and both USCAP urologic pathology societies:
- Each separately submitted vial gets its own line diagnosis
- Fraction of cores per specimen involved by cancer should be stated; recommended to report the either the percentage or the length (millimeters) of each individual core involved by cancer since these strongly predict prostatectomy findings (Am J Surg Pathol 2005;29:1228)
- Many laboratories and pathologists report both the percentage and the length
- For example: prostatic adenocarcinoma, Gleason 3+4 (score of 7) involving 20% and 30% of 2 out of 2 cores, tumor lengths 3 mm and 4 mm
- Many laboratories and pathologists report both the percentage and the length
- Reporting the percent of Gleason 4 cancer is now required in Gleason 3+4 or 4+3 cancer (grade groups 2 or 3) (Am J Surg Pathol 2020:44:e87)
- Although it is not necessary when the highest score in any specimen part is Gleason 8 - 10 (grade groups 4 or 5) (Arch Pathol Lab Med 2021;145:461)
- Reporting the presence or absence of cribriform pattern is also required whenever Gleason 4 cancer is diagnosed, because of its adverse prognostic impact (Adv Anat Pathol 2018;25:31)
- Reporting other patterns of Gleason 4 is optional
- Whether perineural invasion and extraprostatic extension are present or absent can be stated as a comment at the end of the list of line diagnoses
- Sextant approach has a false negative rate up to 25% due to sampling error (Mol Urol 2000;4:93)
Case reports
- 42 - 78 year old men with rectal adenocarcinoma (Hum Pathol 2007;38:1836)
- 46 - 75 year old men with solitary fibrous tumor on needle biopsy and transurethral resection of the prostate (Am J Surg Pathol 2007:31:870)
- 51 - 87 year old men with urothelial carcinoma diagnosed on prostate needle biopsy (Am J Surg Pathol 2001;25:794)
- 58 - 93 year old men with primary mucin producing urothelial type adenocarcinoma of prostate (Am J Surg Pathol 2007:31:1323)
- 65 year old man with prostatic sarcoidosis and PSA elevated to 7.2 ng/mL (J Urol 2013;190:711)
- 67 year old man with squamous cell carcinoma of the prostate (Case Reports in Clin Pathol 2016;3:60)
- 76 year old man with renal-like clear cell carcinoma, positive for CD10 and PSA (In Vivo 2020;34:2751)
- 16 prostate needle biopsies with distorted benign rectal glands that mimic prostate cancer (Am J Surg Pathol 2006;30:866)
Treatment
- Nonsurgical approaches include radiotherapy with hormone ablation and cryotherapy
- Alternative is surgery which nowadays is usually robotic radical prostatectomy
Gross description and processing
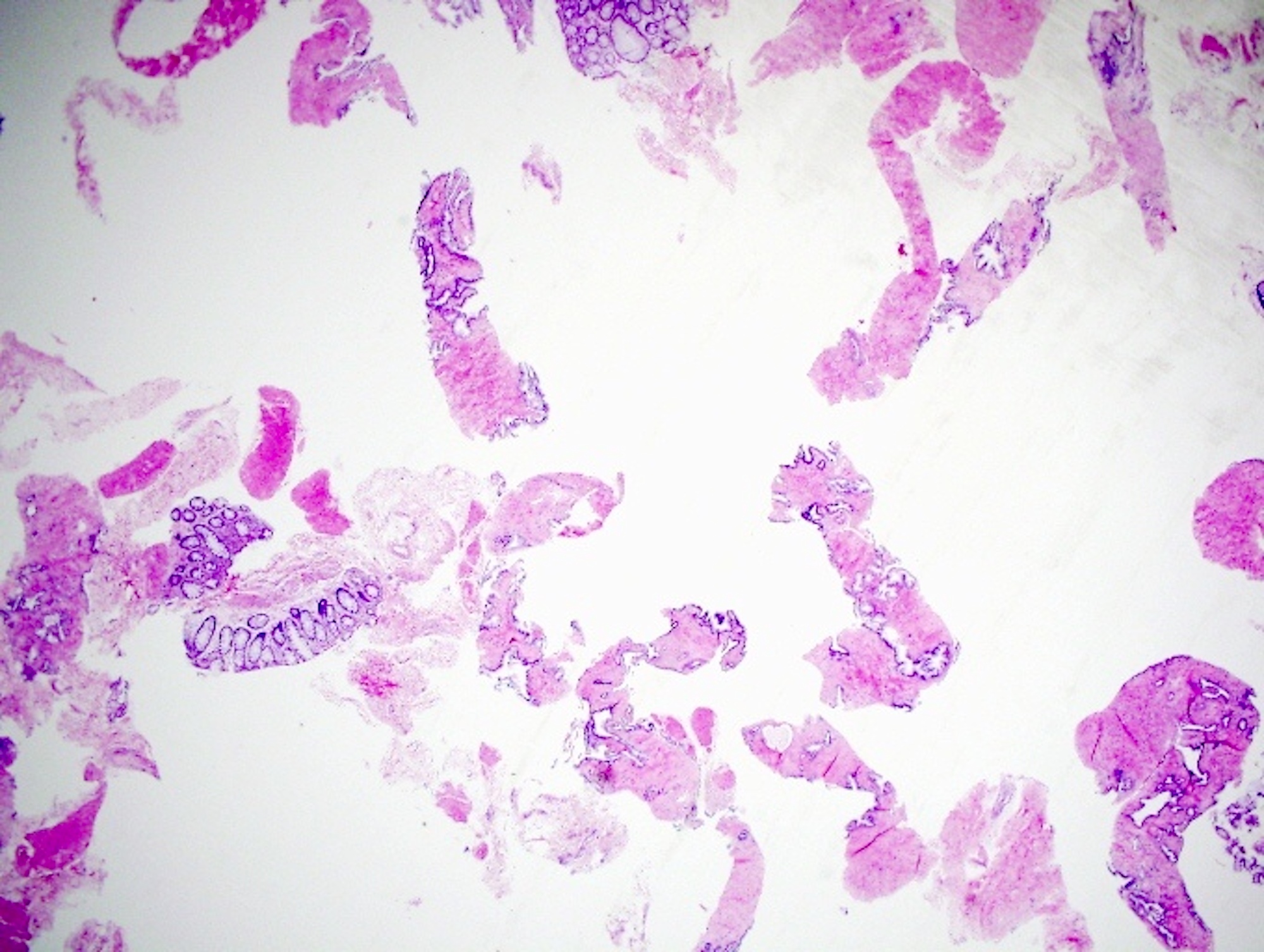
- Method of gross submission of prostate biopsies is crucial
- Most laboratories submit up to 2 cores (a core being defined as ≥ 1 cm length) per cassette, regardless of the number of cores per vial
- If a vial contains a dozen cores or core fragments, submission of all the material in 1 cassette leads to almost uninterpretable slides because of specimen crossing over and fragmentation (see Figure 1 below) (Ann Diagn Pathol 2014;18:301)
- Having no more than 2 full cores per cassette minimizes the tissue that falls out of the plane of section
- However, some laboratories are able to submit 3 cores (from 3 different vials) in 1 cassette using differential inking to indicate sites of the cores
- Great care must be taken with this approach but the diagnostic yield is comparable to 1 specimen per cassette (Ann Diagn Pathol 2013;17:357)
- Advantages are reducing the number of slides for the pathologist to look at and reducing processing costs and storage space
- 3 levels are recommended for maximal detection of cancer (Arch Pathol Lab Med 1998;122:833, Am J Clin Pathol 1997;107:26, Am J Surg Pathol 1999;23:257)
- 5 levels may be cut with levels 2 and 4 unstained, reserved for stains such as investigation of atypical small acinar proliferation (ASAP), suspicious for but not diagnostic of malignancy; 1, 3 and 5 are used for hematoxylin eosin (Am J Clin Pathol 1998;109:416)
- Average of 23% of total length of a core is missed by a single histologic level
- Pre-embedding cores using stretch method may yield more tumor / core, more cores with tumor, more cases with tumor, fewer atypical small acinar diagnoses, fewer cases with ≤ 3 mm of Gleason 6 or less cancer (Hum Pathol 2000;31:1102)
Frozen section description
- Frozen section is not recommended for prostate biopsy
Microscopic (histologic) description
- Features suggestive of malignancy in a core are (malignant versus benign specimens) (Arch Pathol Lab Med 2002;126:554):
- Prominent nucleoli (94% versus 25%)
- Marginated nucleoli (88% versus 7%)
- Multiple nucleoli (64% versus 0%)
- Blue tinged mucinous secretions (52% versus 0%)
- Intraluminal crystalloids (41% versus 1%)
- Intraluminal amorphous eosinophilic material (87% versus 2%)
- Collagenous micronodules (2% versus 0%)
- Glomerulations (15% versus 0%)
- Perineural invasion (22% versus 0%)
- Retraction clefting (39% versus 7%)
- Invasion of fat (1% versus 0%)
Microscopic (histologic) images
Virtual slides
Cytology description
- Frozen section is not recommended for prostate biopsy
Positive stains
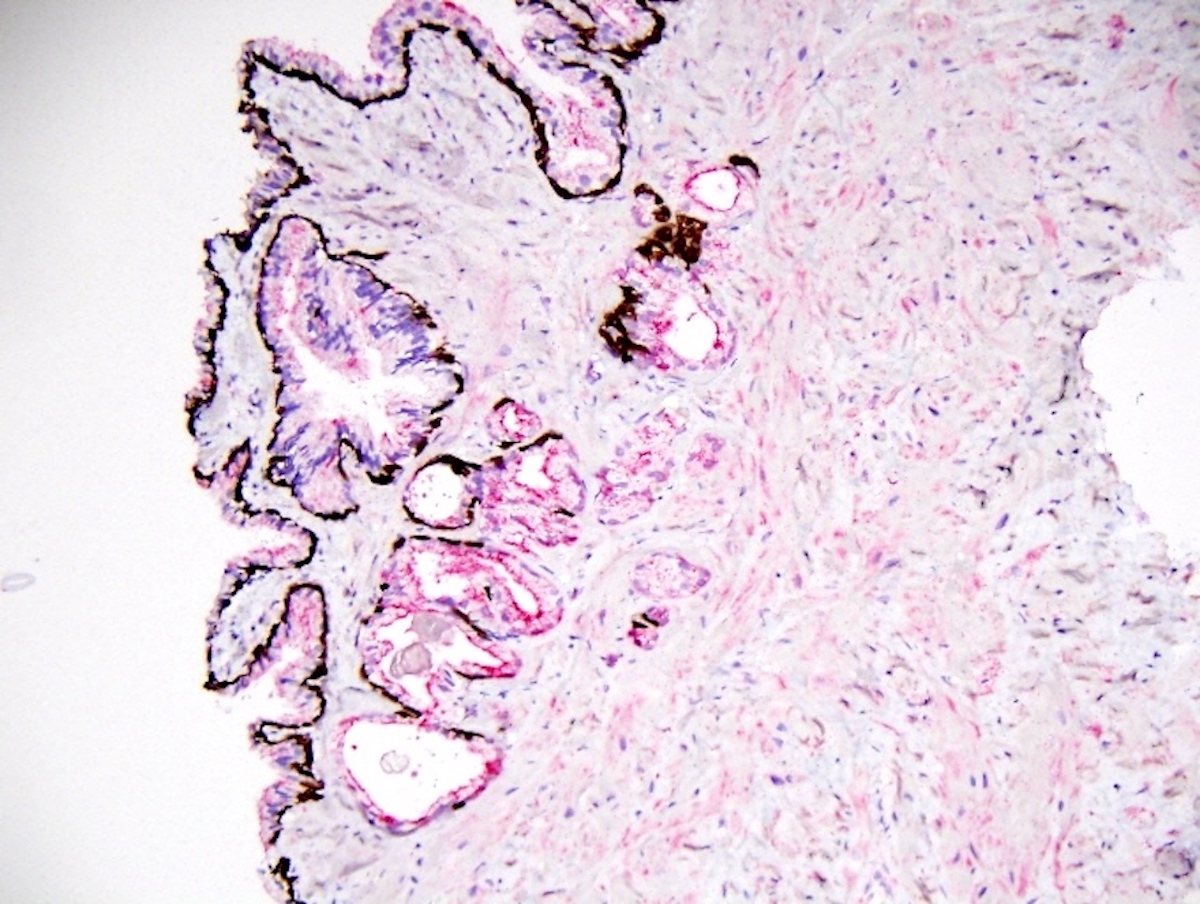
- Immunostains should be reserved for equivocal cases where hematoxylin eosin is inconclusive (Int Urol Nephrol 2010;42:325)
- Or to distinguish intraductal from invasive cancer (Am J Surg Pathol 2020:44:e87, Arch Pathol Lab Med 2021;145:461)
- Sensitive and specific for prostate carcinoma on needle biopsies but not all suspicious / atypical small acinar proliferation (ASAP) cases can be resolved by immunostain cocktail (see Figures 7 and 8 above)
- Can also destain / restain needle biopsies and put original sections on coated slides (Hum Pathol 2000;31:1155)
- Prostatic intraepithelial neoplasia (PIN) cocktail with P504S (red) and 34ΒE12 + p63 (brown) is widely used to diagnose limited prostatic adenocarcinoma (Am J Surg Pathol 2002;26:1169, Am J Surg Pathol 2003;27:365)
- Caveat: P504S stains some hyperplastic nodules and benign glands adjacent to transition zone carcinomas (Hum Pathol 2003;34:228)
- P504S / p63 can be used as a single color cocktail to distinguish prostatic cancer involvement in seminal vesicles versus cancer mimickers because of the architectural complexity of the seminal vesicles and ejaculatory ducts (Arch Pathol Lab Med 2010;134:983)
Negative stains
- High molecular weight cytokeratin 34ΒE12 and p63 are lacking in adenocarcinoma since basal cells are absent
- Positive staining can identify benign mimickers of cancer including benign crowded glands, adenosis and atrophy and occasionally discriminate high grade PIN versus cancer
- Negative high molecular weight keratin 34ΒE12 is diagnostic of adenocarcinoma only if there is a high (90%) H&E suspicion of carcinoma, one must also see staining of obviously benign glands as internal control (Am J Surg Pathol 2002;26:1151)
- Negative or very light staining with P504S in suspicious foci does not necessarily indicate a benign diagnosis (Am J Surg Pathol 2002;26:1169)
Molecular / cytogenetics description
- FISH for PTEN loss is a precise test for this adverse finding but immunostaining is usually done first
Sample pathology report
- Give Gleason sum, the grade group, percentages of cores, fraction of cores and tumor lengths; if primary and secondary Gleason are different and the highest Gleason sum = 7, give the % of secondary
- Prostate, left apex, biopsy:
- Prostatic adenocarcinoma, Gleason 3+3 (score = 6, grade group 1) within 80% and 90% of 2 out of 3 cores; tumor lengths 4 mm and 6 mm
- Perineural invasion is present
- Benign fibromuscular stroma only (1 core)
- Prostate, left mid, biopsy:
- Prostatic adenocarcinoma, Gleason 3+4 (score = 7, grade group 2) within 80%, 90%, 90% and 100% of 4 out of 5 cores; tumor lengths 4 mm, 6 mm, 6 and 10 mm
- 30% of tumor is Gleason 4, not cribriform
- Perineural invasion is present
- Benign fibromuscular stroma only (3 cores)
- Prostate, left base, biopsy:
- Benign prostatic tissue. Mild atrophy. Mild chronic inflammation. Et cetera.
- Comment (end of report): Tumor shows no extraprostatic extension.
Differential diagnosis
- Atrophy:
- Most common mimic of cancer
- Histologic similarity (small acini) but not cytologic similarity (lack of cellular atypia)
- High grade PIN (Am J Clin Pathol 2000;114:896):
- Conversely, mimics cancer by having cytologic similarity (cellular atypia) but not histologic similarity (larger gland space and retained basal cells)
- Atypical adenomatous hyperplasia:
- Another small acinar cancer mimic: clustered, not infiltrative like cancer
- See Figure 9 above, also called adenosis
Board review style question #1
Board review style answer #1
A. Corpora amylacea. Corpora amylacea are usually a mark of benign acini. Cancer findings that are more common include prominent nucleoli and infiltrative growth. Less common but very specific for cancer are glomerulations and mitotic figures.
Comment Here
Reference: Prostate gland & seminal vesicles - Biopsy
Comment Here
Reference: Prostate gland & seminal vesicles - Biopsy
Board review style question #2
Required findings to report based on current consensus include
- Global (case level) grading
- Glomeruloid pattern
- Percentage of grade 4 cancer if the Gleason score is 7
- Percentage of grade 4 cancer if the Gleason score is 8 - 10
Board review style answer #2
C. Percentage of grade 4 cancer if the Gleason score is 7. This is a reporting requirement. Within 3+4 cancer (grade group 2), it matters greatly whether the 4 is 1% or 49%. If the cancer is 4+4=8 or if Gleason 5 is present in any specimen part, then stating percentage of Gleason 4 is optional for the remaining parts.
Global (case level) grading is optional according to current recommendations; however, if multiple cores are from a single radiologically targeted site / region of interest, a global grade should be assigned to all those cores. The glomeruloid pattern, although specific for cancer, is not necessary to report but the presence or absence of cribriform pattern is since it carries a special prognostic impact.
Comment Here
Reference: Prostate gland & seminal vesicles - Biopsy
Global (case level) grading is optional according to current recommendations; however, if multiple cores are from a single radiologically targeted site / region of interest, a global grade should be assigned to all those cores. The glomeruloid pattern, although specific for cancer, is not necessary to report but the presence or absence of cribriform pattern is since it carries a special prognostic impact.
Comment Here
Reference: Prostate gland & seminal vesicles - Biopsy