Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Jin Z, Falzarano SM. Benign prostatic hyperplasia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/prostatenodhyper.html. Accessed April 30th, 2024.
Definition / general
- Benign nodular enlargement of the prostate gland
- Histopathologically, hyperplasia (nonneoplastic new growth) of stromal and glandular components
Essential features
- Benign nodular lesion with proliferation of stromal and glandular components
- Predominantly located in the transition zone of the prostate
- Diagnosis of benign prostatic hyperplasia (BPH) should not be used on routine prostate biopsies (Hum Pathol 2002;33:796)
Terminology
- Benign prostatic hypertrophy (misnomer)
- Nodular hyperplasia
ICD coding
Epidemiology
- 50% prevalence in men between 51 - 60 years (J Urol 1984;132:474)
- Increasing incidence with increasing age (J Urol 1984;132:474)
Sites
- Transition (periurethral) zone of the prostate (Invest Urol 1978;15:340)
Pathophysiology
- Proliferation of both stromal and epithelial cells, leading to new glandular budding and branching, with formation of nodules
- Central role of sex steroids (5αdihydrotestosterone, estrogens) and growth factors (fibroblast growth factor, transforming growth factor beta) (Nat Rev Urol 2011;8:29)
Etiology
- Exact etiology unknown
- Multiple theories, including embryonic reawakening, stem cell proliferation and hormonal imbalances (Nat Rev Urol 2011;8:29)
Clinical features
- Increased bladder outlet resistance
- Lower urinary tract symptoms (LUTS), including:
- Obstructive symptoms (hesitancy, intermittent stream and straining)
- Urinary bladder irritation symptoms (frequency, urgency and urge incontinence)
- Urinary retention (whether acute or chronic)
- Severity assessed through self administered questionnaire (Am Fam Physician 2014;90:769)
Diagnosis
- Clinical history
- Physical examination (including digital rectal exam, assessment of bladder distention, motor and sensory deficits of the lower extremities and perineum and decreased anal sphincter tone to identify neurogenic bladder)
- Urinalysis
- Serum prostate specific antigen (PSA) measurement not recommended routinely (Annu Rev Med 2016;67:137)
- Other studies, depending on symptoms (Am Fam Physician 2014;90:769)
Laboratory
- Urinalysis may reveal hematuria, proteinuria or evidence of urinary tract infection
- Prostate specific antigen (PSA) may be elevated (Curr Opin Urol 2000;10:3)
Radiology description
- Imaging typically not specific for benign prostatic hyperplasia
- Often performed to rule out other causes of lower urinary tract symptoms
- Hypoechogenic nodules or variable echogenicity on ultrasound
- Nodules ranging from hypointense to hyperintense on MRI T2 weighted images, depending on stroma / gland ratio (Diagn Interv Radiol 2016;22:215)
- 7 subtypes of benign prostatic hyperplasia on MRI based on location of the hyperplasia (Diagn Interv Radiol 2016;22:215)
Prognostic factors
- Not a precursor or risk factor for prostate cancer (Practitioner 2012;256:13, Am J Epidemiol 2011;173:1419)
- Side effects of medications may increase with increasing age (Ther Adv Urol 2020;12:1756287220929486)
- Immediate and long term complications of surgical treatment are relatively rare (Annu Rev Med 2016;67:137)
- Risk of recurrence varies with type of treatment (Annu Rev Med 2016;67:137)
Case reports
- 17 year old boy with acute urinary retention due to benign prostatic hyperplasia (J Pediatr Urol 2016;12:267.e1)
- 61 year old man with spontaneous prostatic hematoma in a case of benign prostatic hyperplasia (BMJ Case Rep 2019;12:e228787)
- 71 year old man with primary prostate intravascular large B cell lymphoma presenting as prostatic hyperplasia (Medicine (Baltimore) 2019;98:e18384)
- 78 year old man with giant benign prostatic hyperplasia (Urol Case Rep 2019;28:101051)
Treatment
- Watchful waiting for patients with mild symptoms or moderate to severe symptoms with minimal impairment in quality of life (Annu Rev Med 2016;67:137)
- Medical treatment based on alpha blockers (nonselective; alpha-1A selective), 5-alpha-reductase inhibitors, phosphodiesterase type 5 inhibitors and combination products (Am Fam Physician 2014;90:769, Front Pharmacol 2020;11:658, Ther Adv Urol 2020;12:1756287220929486)
- Surgical treatment, including ablative (such as transurethral resection, simple prostatectomy, transurethral laser vaporization, ablation, enucleation) and other procedures (such as transurethral incision, prostatic urethral lift device) reserved for patients who either have failed medical management or have complications (Curr Urol Rep 2020;21:32, BJU Int 2020;126:317, Am Fam Physician 2014;90:769)
Gross description
- Variably sized nodules with a gray to yellow color and a granular appearance bulge above the cut surface of a prostate section
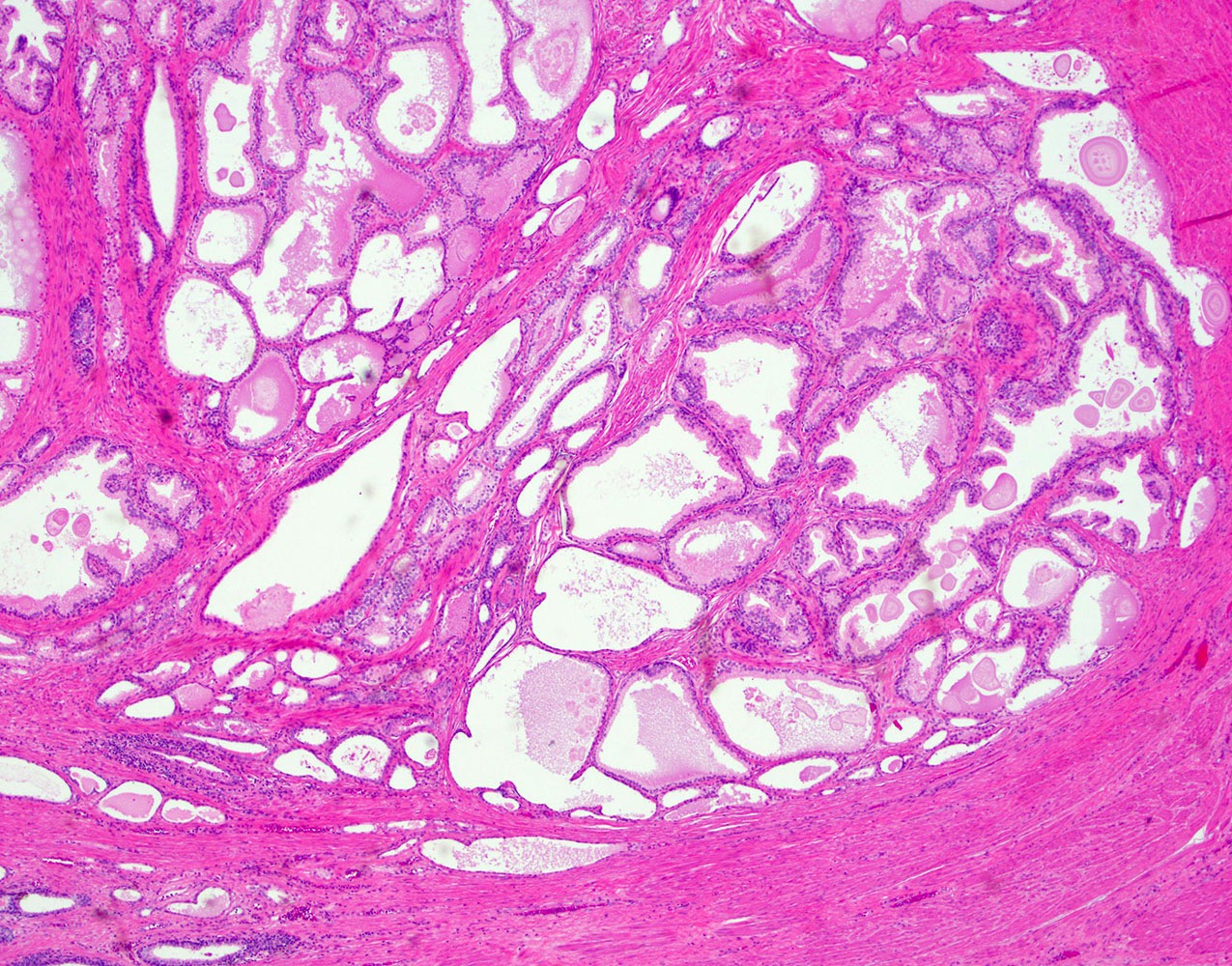
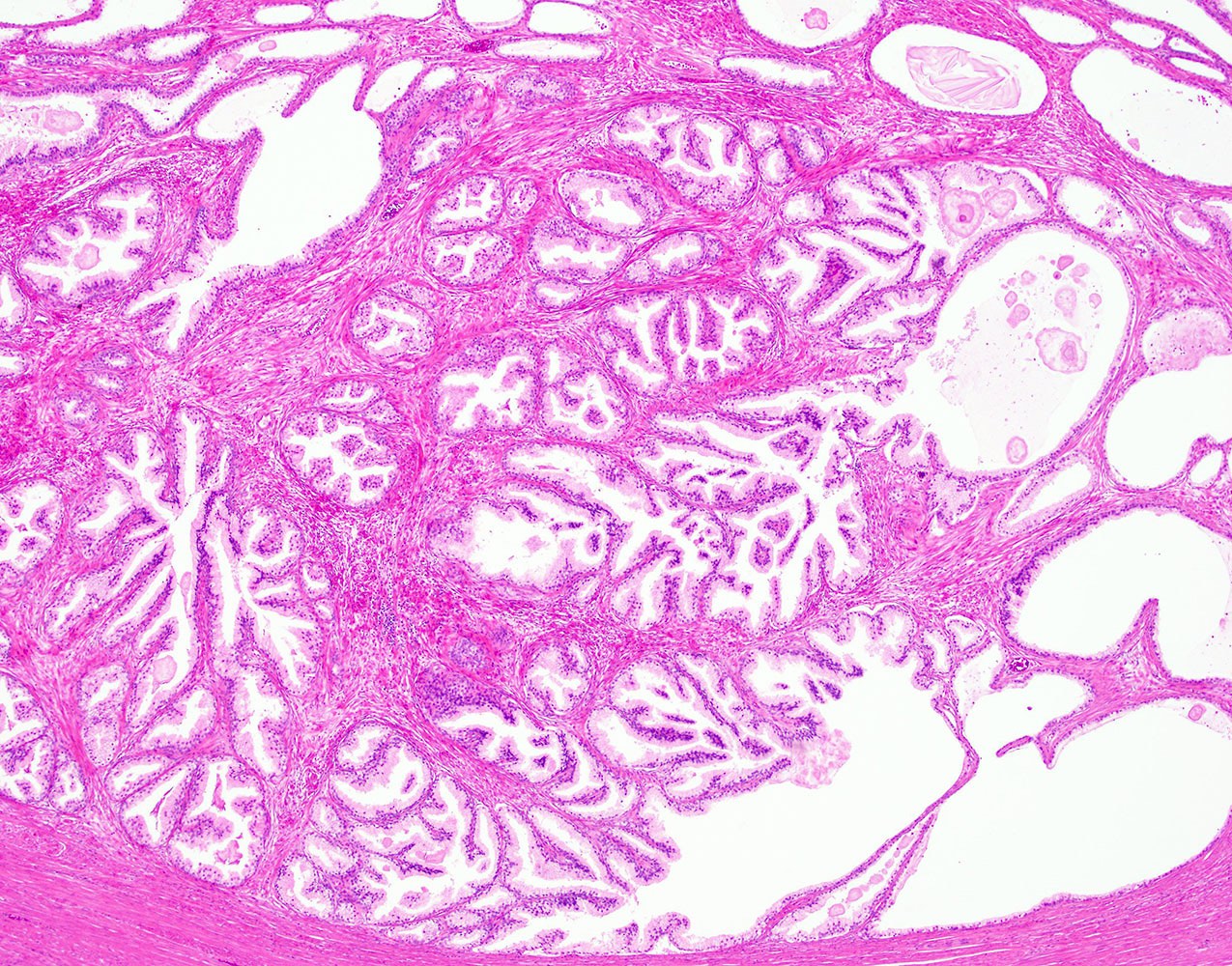
Microscopic (histologic) description
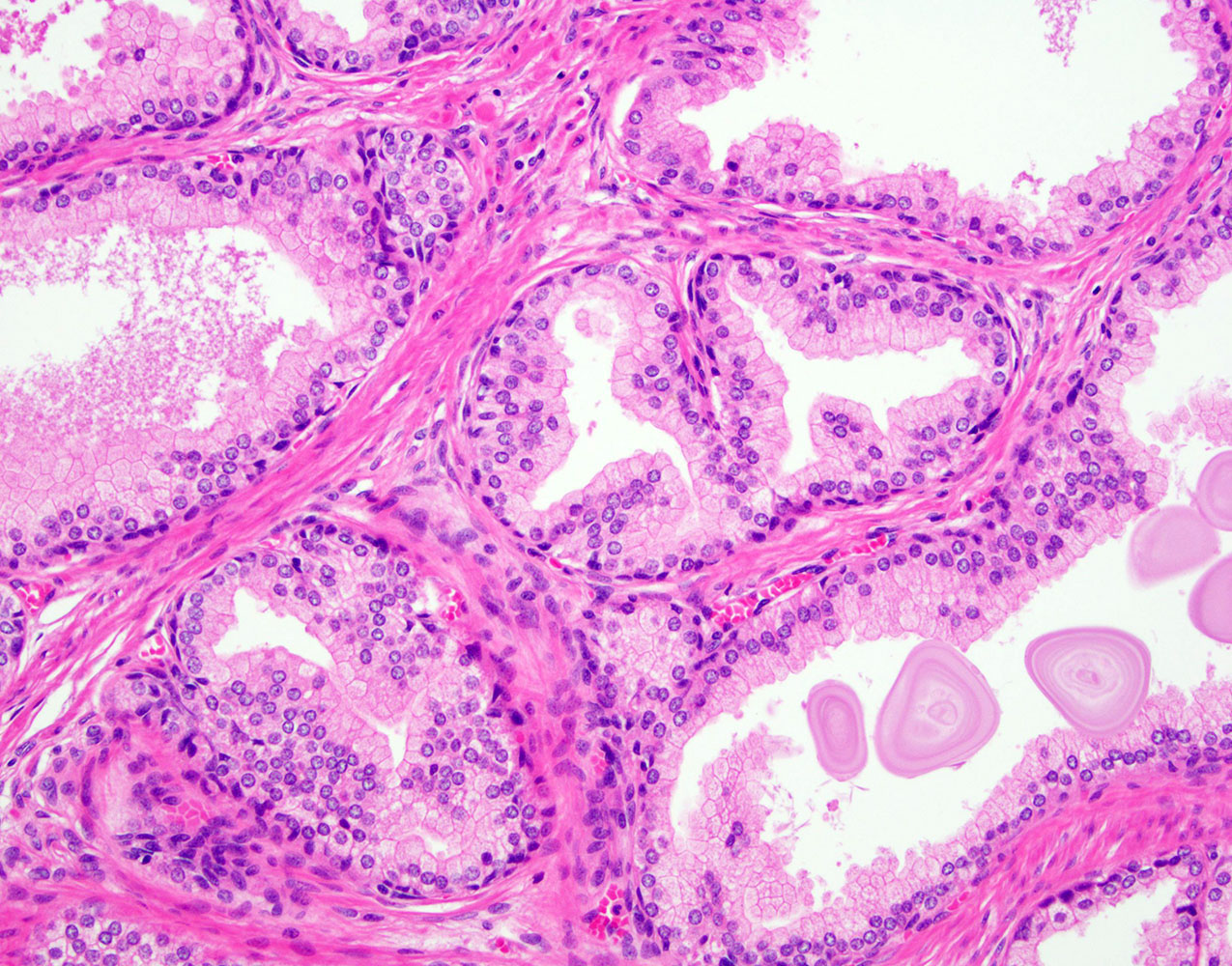
- Epithelial hyperplasia is characterized by nodular lesions composed of variably sized glandular structures lined by basal and secretory cells
- Glandular dilatation with papillary infoldings and cysts, often containing corpora amylacea, sometimes calcifications
- Epithelial lining ranging from flat to columnar, with pink pale cytoplasm, regular, centrally located nuclei and inconspicuous nucleoli
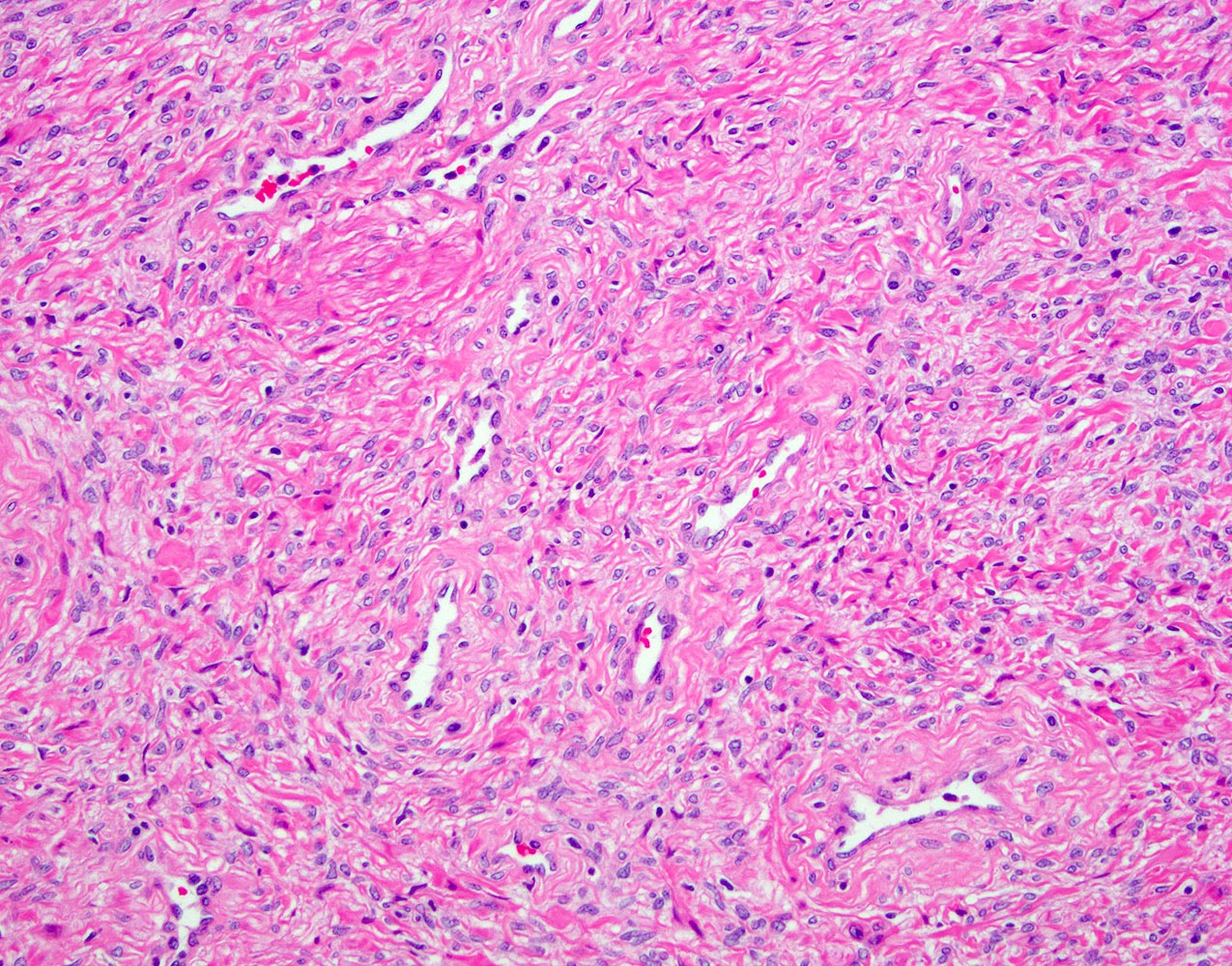
- Stromal nodules are composed of bland spindle cells with round to ovoid nuclei with open chromatin
- Thick walled small capillary vessels can be seen on cross sections
- Ischemic changes / infarcts can be seen within the nodules
- Morphologic variants include:
- Clear cell cribriform hyperplasia
- Basal cell hyperplasia
- Adenosis / atypical adenomatous hyperplasia
- Leiomyomatous nodules
- Fibroadenomatous
- Phyllodes type hyperplasia
- Reference: Am J Surg Pathol 1988;12:619
Microscopic (histologic) images
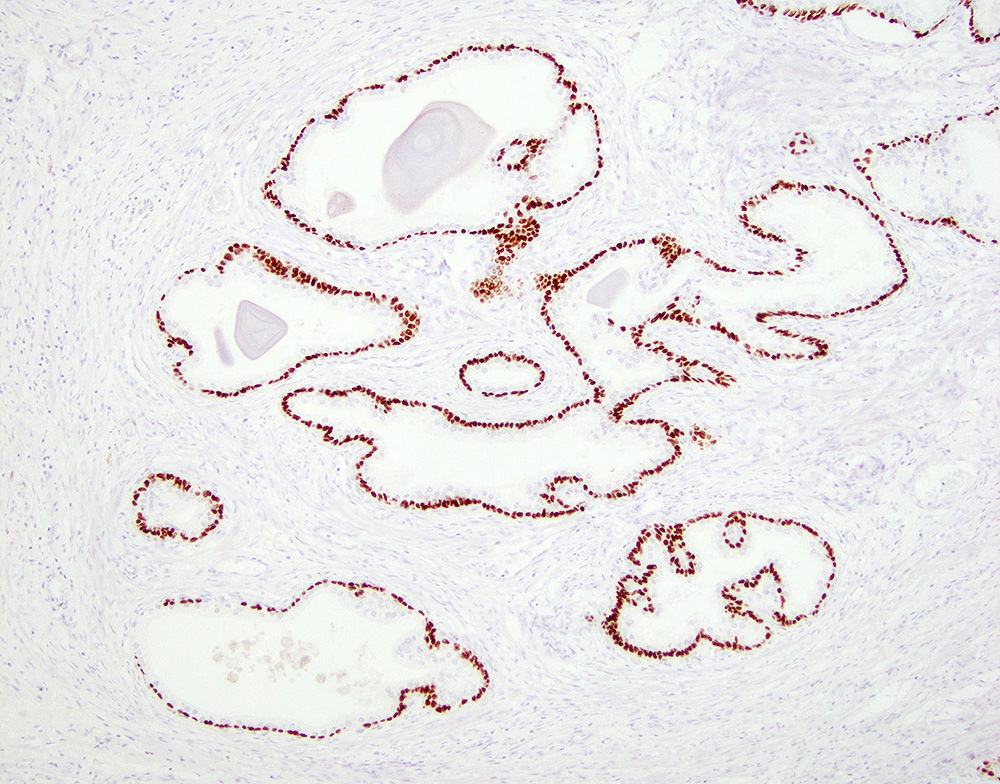
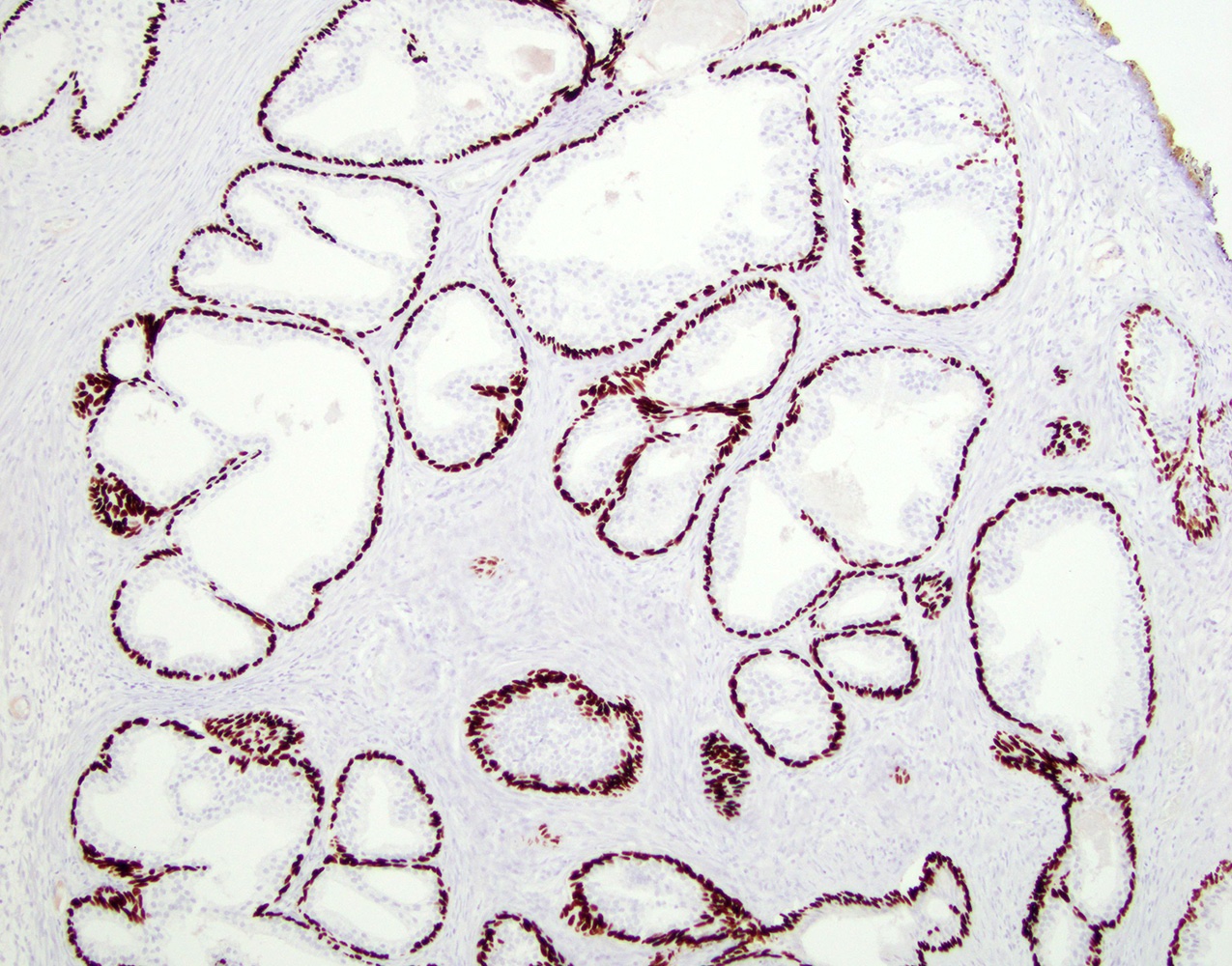
Positive stains
- Immunostains typically not needed
- Basal cells
- High molecular weight cytokeratin (e.g. 34 beta E12, CK5/6, CK14)
- p63
- Secretory (luminal) cells
- Stromal cells
- CD34, smooth muscle actin (SMA)
- Desmin variable
- Reference: Am J Surg Pathol 1988;12:619
Sample pathology report
- Prostate chips, transurethral resection:
- Benign prostatic hyperplasia
- Prostate tissue, transurethral laser enucleation:
- Benign prostatic tissue with stromal and glandular hyperplasia (58 grams)
Differential diagnosis
- Prostatic adenocarcinoma (e.g. pseudohyperplastic type):
- Specialized stromal tumors (Am J Surg Pathol 2006;30:694)
- Stromal tumor of uncertain malignant potential (STUMP):
- Higher degree of cellularity
- Lacks numerous thick walled small blood vessels
- Stromal sarcoma:
- Significant cytologic atypia, increased mitotic activity, necrosis
- Stromal tumor of uncertain malignant potential (STUMP):
- Other mesenchymal tumors
- Leiomyosarcoma:
- Significant cytologic atypia, increased mitotic activity, necrosis (Cancer 1995;76:1422)
- Solitary fibrous tumor:
- Patternless growth of uniform spindled cells with bland nuclei in background ropy collagen, staghorn hemangiopericytomatous vessels
- STAT6 positive (strong diffuse) (Hum Pathol 2016;54:184)
- Gastrointestinal stromal tumor (GIST):
- CD117 positive
- May involve prostate secondarily from rectum (Am J Surg Pathol 2006;30:1389)
- Leiomyosarcoma:
Additional references
Board review style question #1
The above image is from an open suprapubic prostatectomy specimen. Which of the following is true about the disease?
- Increasing incidence with increasing age
- It is considered a precursor to prostate adenocarcinoma
- It is more frequent in the peripheral zone of the prostatic gland
- Medical therapy has no role in the management of the disease
- Surgical treatment is contraindicated
Board review style answer #1
A. Increasing incidence with increasing age. The image shows benign prostatic hyperplasia.
Comment Here
Reference: Benign prostatic hyperplasia
Comment Here
Reference: Benign prostatic hyperplasia
Board review style question #2
Board review style answer #2