Prostate gland & seminal vesicles
General
Staging
Last author update: 8 February 2023
Last staff update: 31 May 2023
Copyright: 2003-2024, PathologyOutlines.com, Inc.
PubMed Search:
Prostate AJCC staging
Page views in 2023: 12,420
Page views in 2024 to date: 4,580
Cite this page: Zynger D. Staging. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/prostatestaging.html. Accessed April 18th, 2024.
Definition / general
- All prostate carcinomas are covered by this staging system
- These topics are not covered: sarcoma, urothelial carcinoma (refer to male urethra staging for carcinoma of the prostatic urethra)
Essential features
- AJCC 7th edition staging was sunset on December 31, 2017; as of January 1, 2018, use of the 8th edition is mandatory
ICD coding
- ICD-O-3: C61.9 - prostate gland
Primary tumor (pT)
- pT2: organ confined
- pT3a: extraprostatic extension or microscopic invasion of bladder neck
- pT3b: seminal vesicle muscle invasion
- pT4: fixed tumor or invasion of structures such as external sphincter, rectum, bladder, levator muscles or pelvic wall
Notes:
- There is no pT1 classification
- Note that cT1 is a part of clinical classification for clinically inapparent, nonpalpable tumor detected in specimens other than a prostatectomy such as a TURP or prostate biopsy with clinically inapparent, nonpalpable, incidental tumor in 5% or less of tissue defined as cT1a, clinically inapparent, nonpalpable, incidental tumor in > 5% defined as cT1b and clinically inapparent, nonpalpable tumor in a prostate needle biopsy defined as cT1c
- Extraprostatic extension: usually this is dichotomized as focal (< 1 high power field in 1 - 2 slides) versus nonfocal / established (> 1 high power field in 1 - 2 slides)
- Microscopic invasion of bladder neck: presence of tumor in thick muscle usually with no adjacent nonneoplastic glands
- Seminal vesicle invasion: invasion of the extraprostatic seminal vesicle muscular wall
Regional lymph nodes (pN)
- pNX: cannot be assessed
- pN0: no regional lymph node metastasis
- pN1: regional lymph node metastasis
Notes:
- Regional lymph nodes include periprostatic, pelvic, hypogastric, obturator, internal iliac, external iliac, sacral
Prefixes
- y: preoperative radiotherapy or chemotherapy
- r: recurrent tumor stage
Histologic grade group (G)
| Grade group
| Gleason score
| Gleason pattern
|
| 1
| ≤ 6
| ≤ 3+3
|
| 2
| 7
| 3+4
|
| 3
| 7
| 4+3
|
| 4
| 8
| 4+4, 3+5, 5+3
|
| 5
| 9 - 10
| 4+5, 5+4, 5+5
|
AJCC prognostic stage groups (utilizing pT categorization)
| Stage group I: | pT2 | N0 | M0 | PSA < 10 | Grade group 1 | Gleason score ≤ 3+3=6
|
| Stage group IIA: | pT2 | N0 | M0 | PSA ≥ 10 - < 20 | Grade group 1 | Gleason score ≤ 3+3=6
|
| Stage group IIB: | pT2 | N0 | M0 | PSA < 20 | Grade group 2 | Gleason score 3+4=7
|
| Stage group IIC: | pT2 | N0 | M0 | PSA < 20 | Grade group 3 - 4 | Gleason score 4+3=7, 4+4=7, 3+5=8, 5+3=8
|
| Stage group IIIA: | pT2 | N0 | M0 | PSA ≥ 20 | Grade group 1 - 4 | Gleason score ≤ 6 - 8
|
| Stage group IIIB: | pT3 - 4 | N0 | M0 | Any PSA | Grade group 1 - 4 | Gleason score ≤ 6 - 8
|
| Stage group IIIC: | pT2 - 4 | N0 | M0 | Any PSA | Grade group 5 | Gleason score 9 - 10
|
| Stage group IVA: | pT2 - 4 | N1 | M0 | Any PSA | Any grade group | Any Gleason score
|
| Stage group IVB: | pT2 - 4 | N0 - 1 | M1 | Any PSA | Any grade group | Any Gleason score
|
Registry data collection variables
- Pretreatment serum PSA
- Grade group
- Gleason score
- Gleason patterns
- Tertiary Gleason pattern on prostatectomy
- Number of cores examined
- Number of cores positive
- Needle core biopsies positive one on side, both sides or beyond prostate
- Metastatic sites
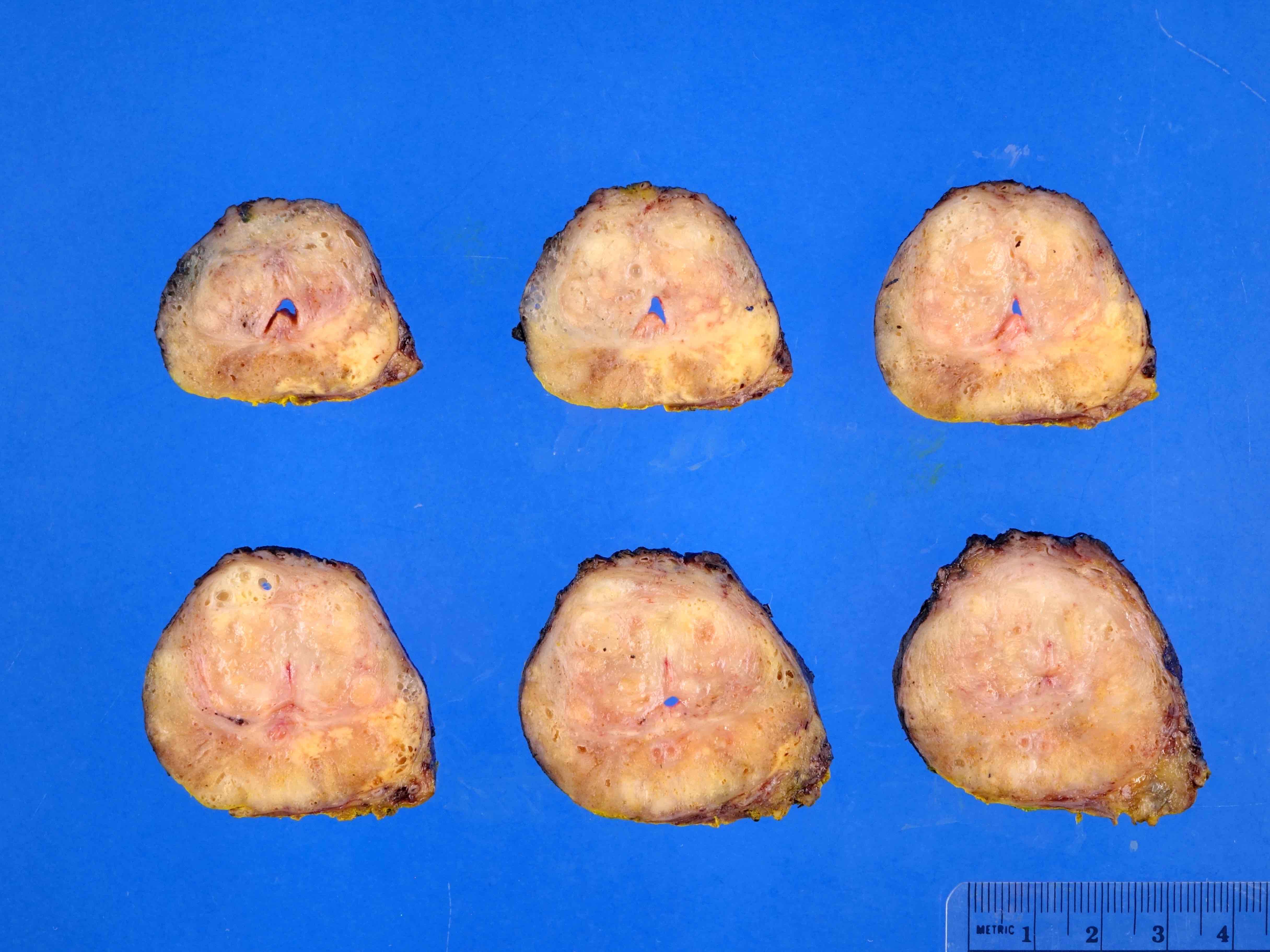
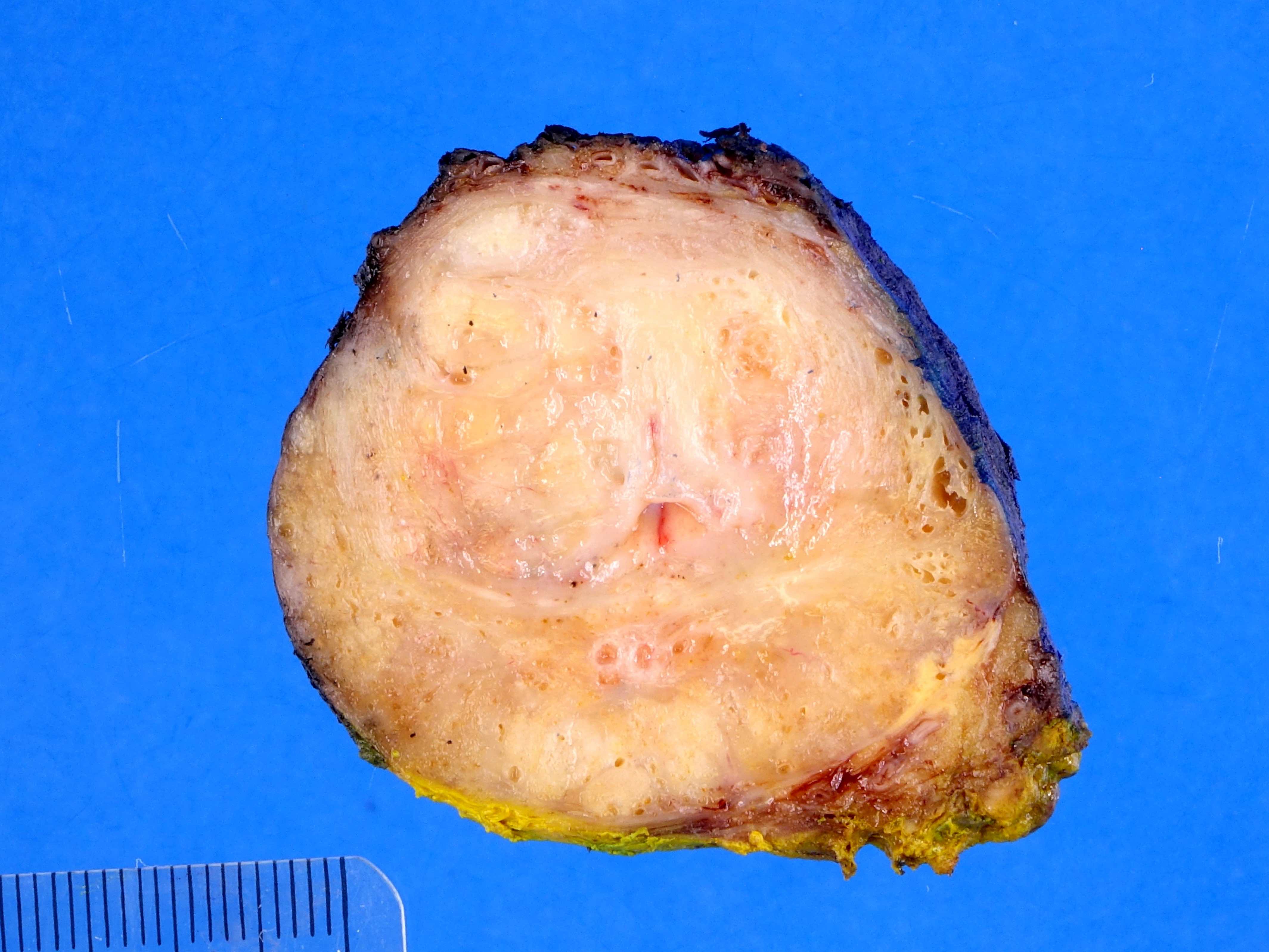
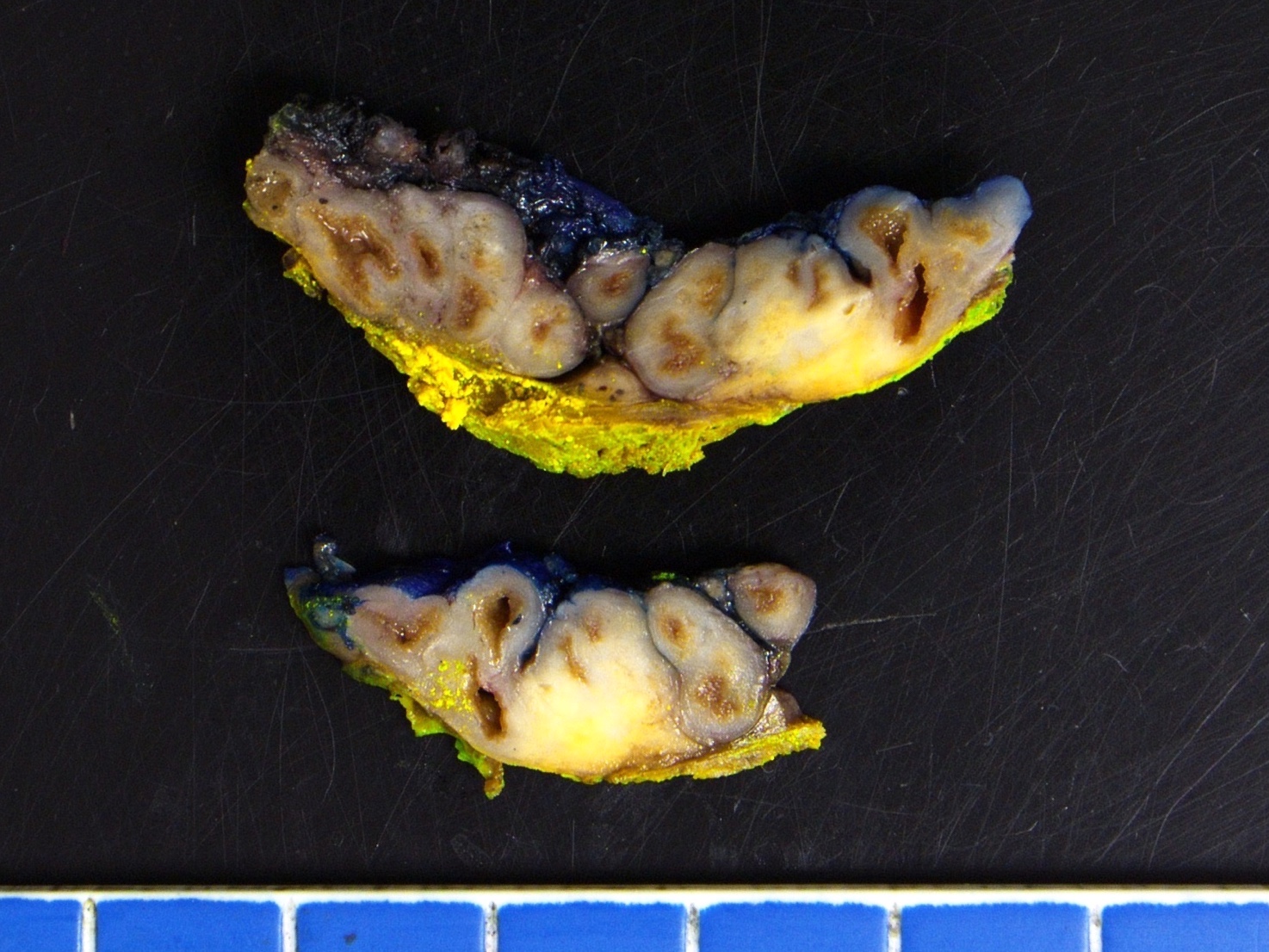
Gross images
Contributed by Debra L. Zynger, M.D.
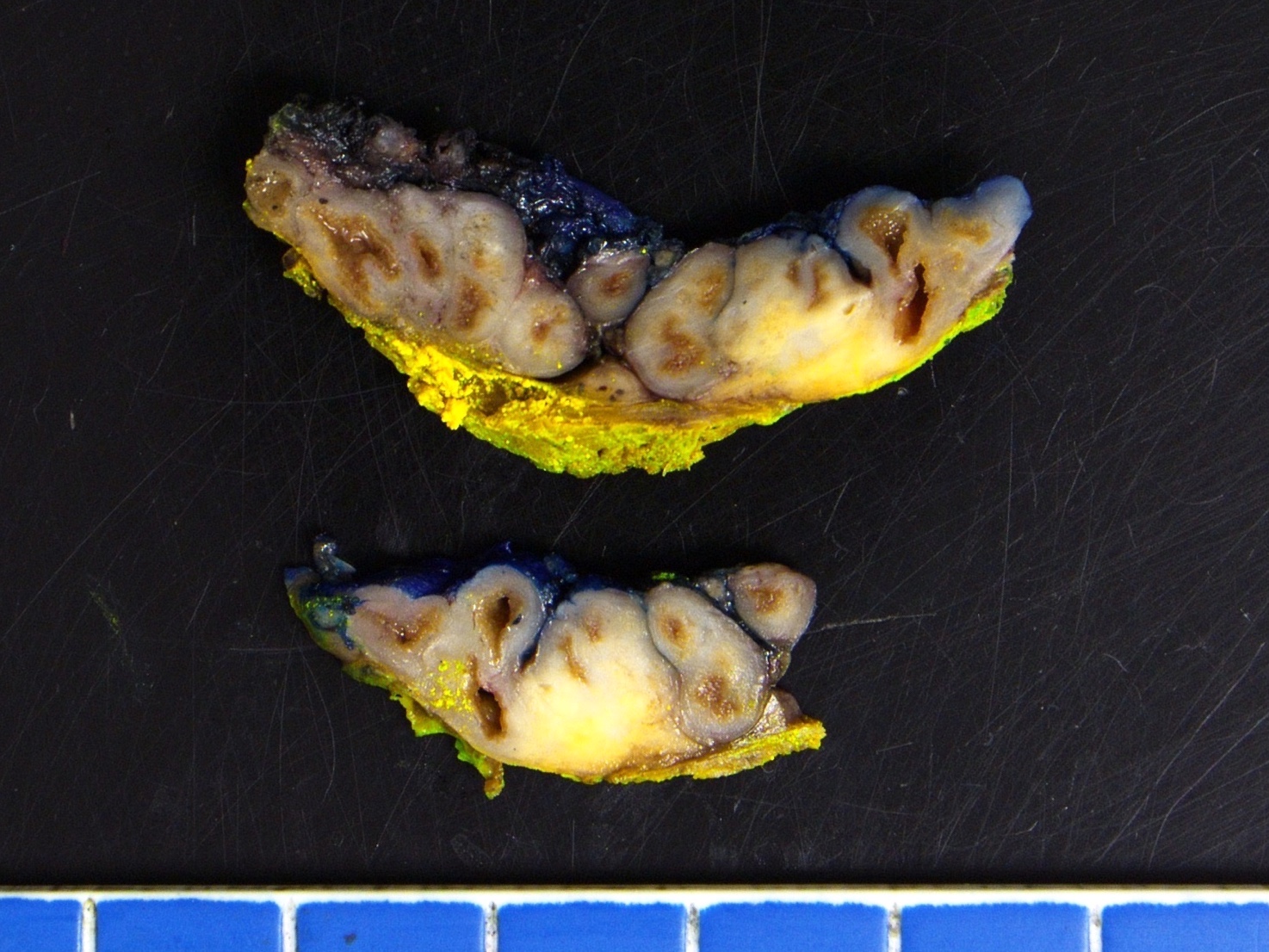

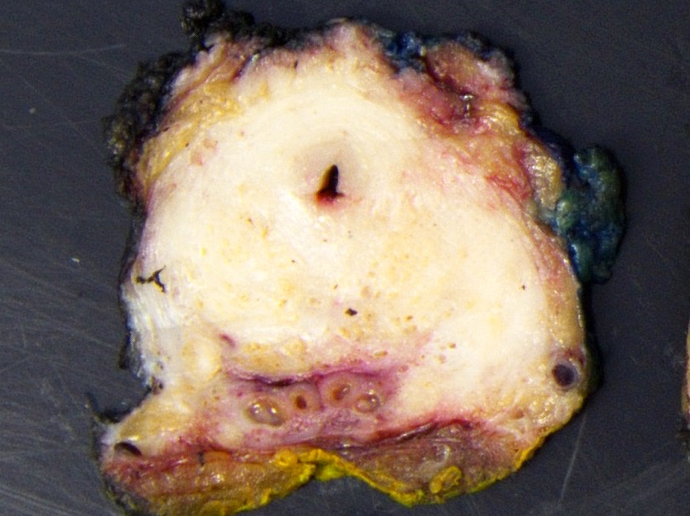
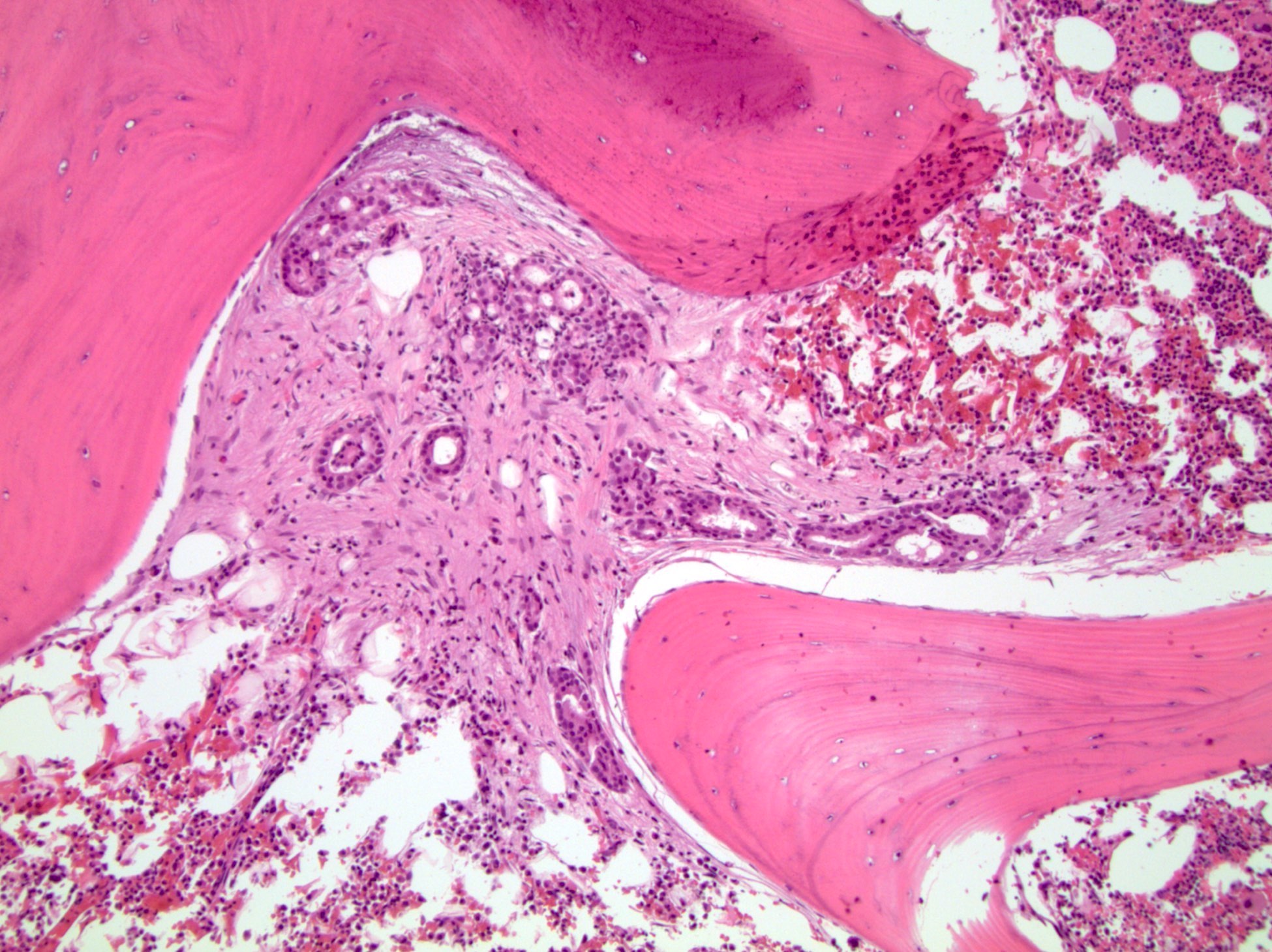
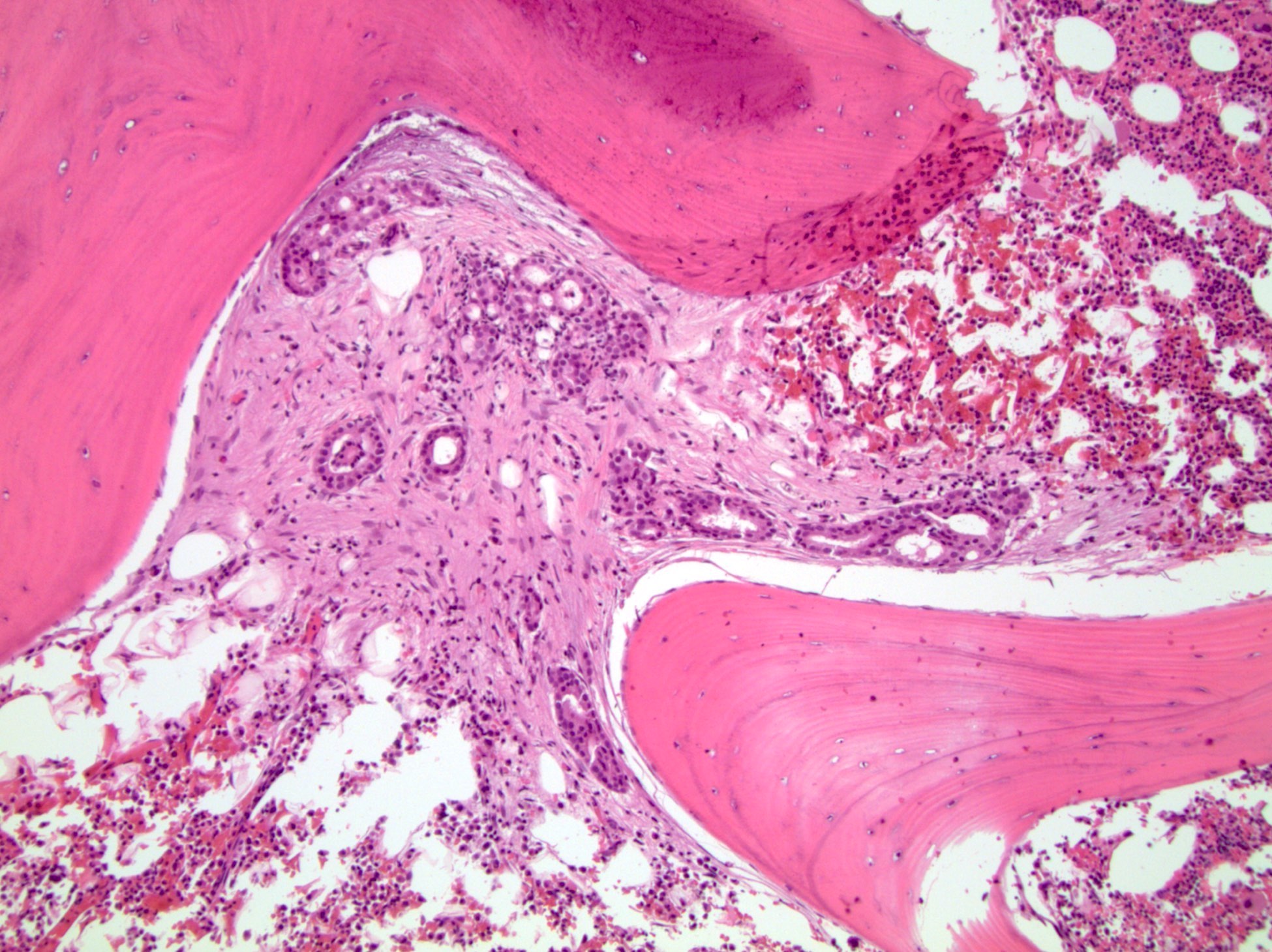
Seminal vesicle invasion (pT3b)
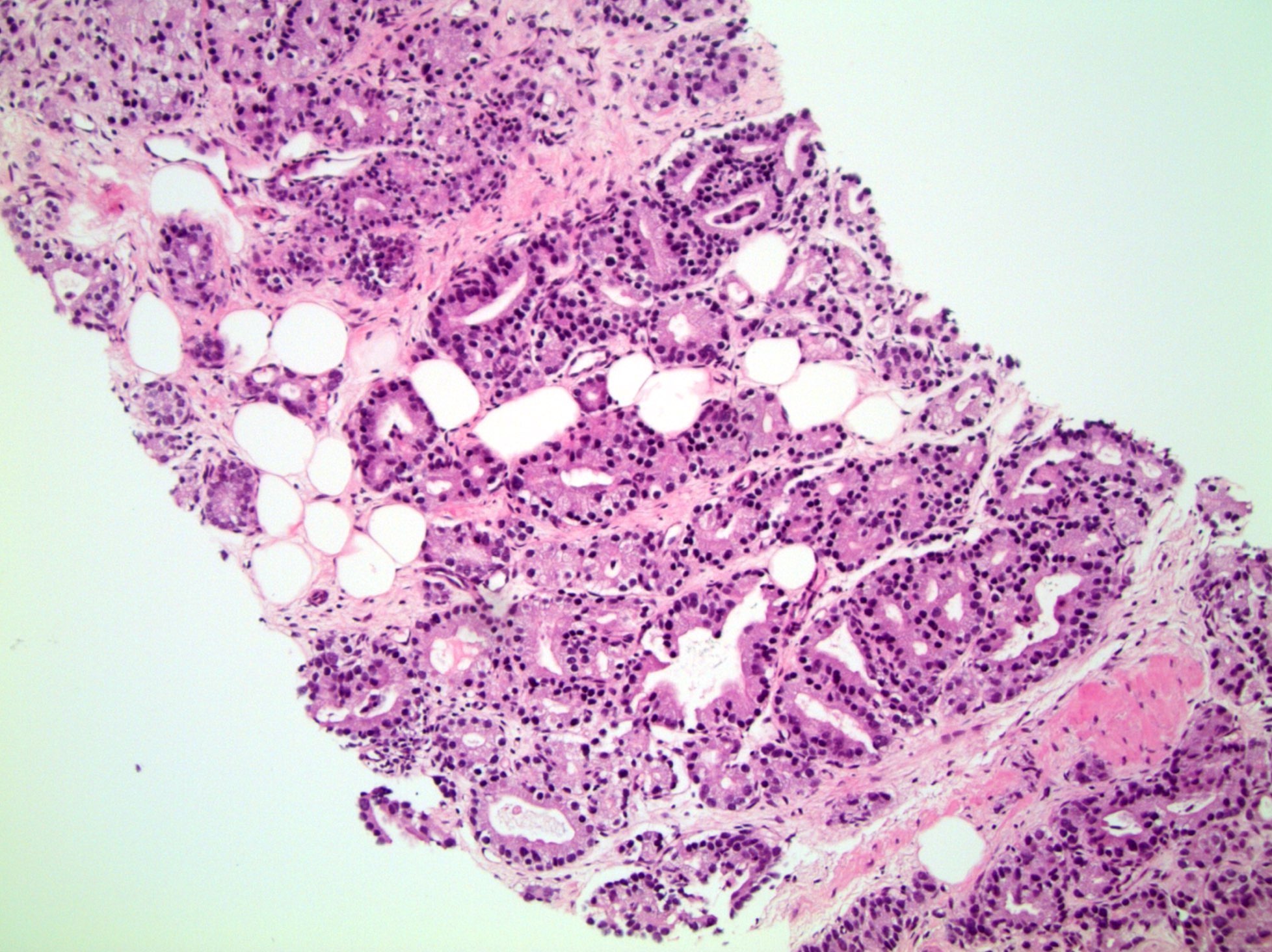
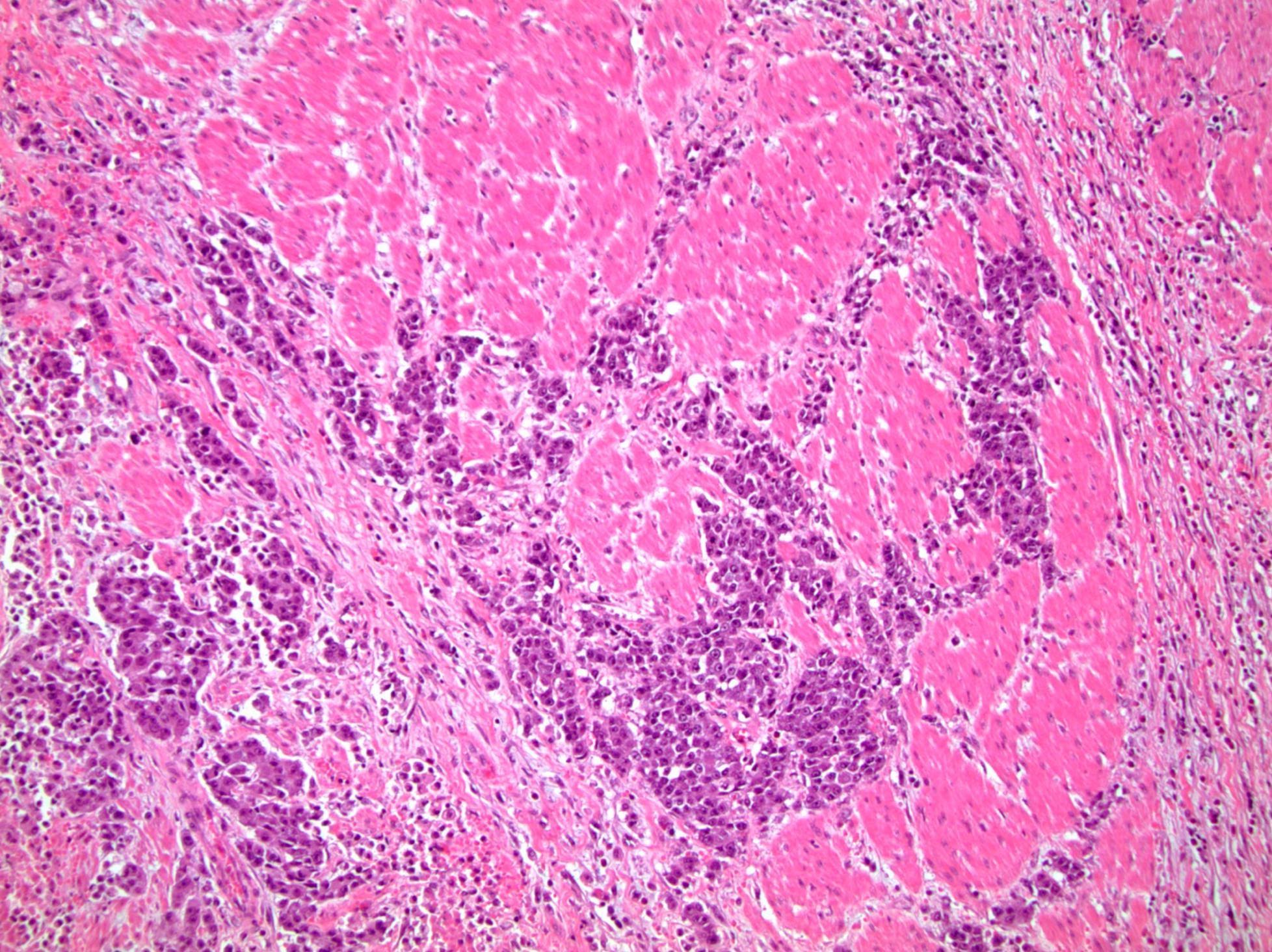
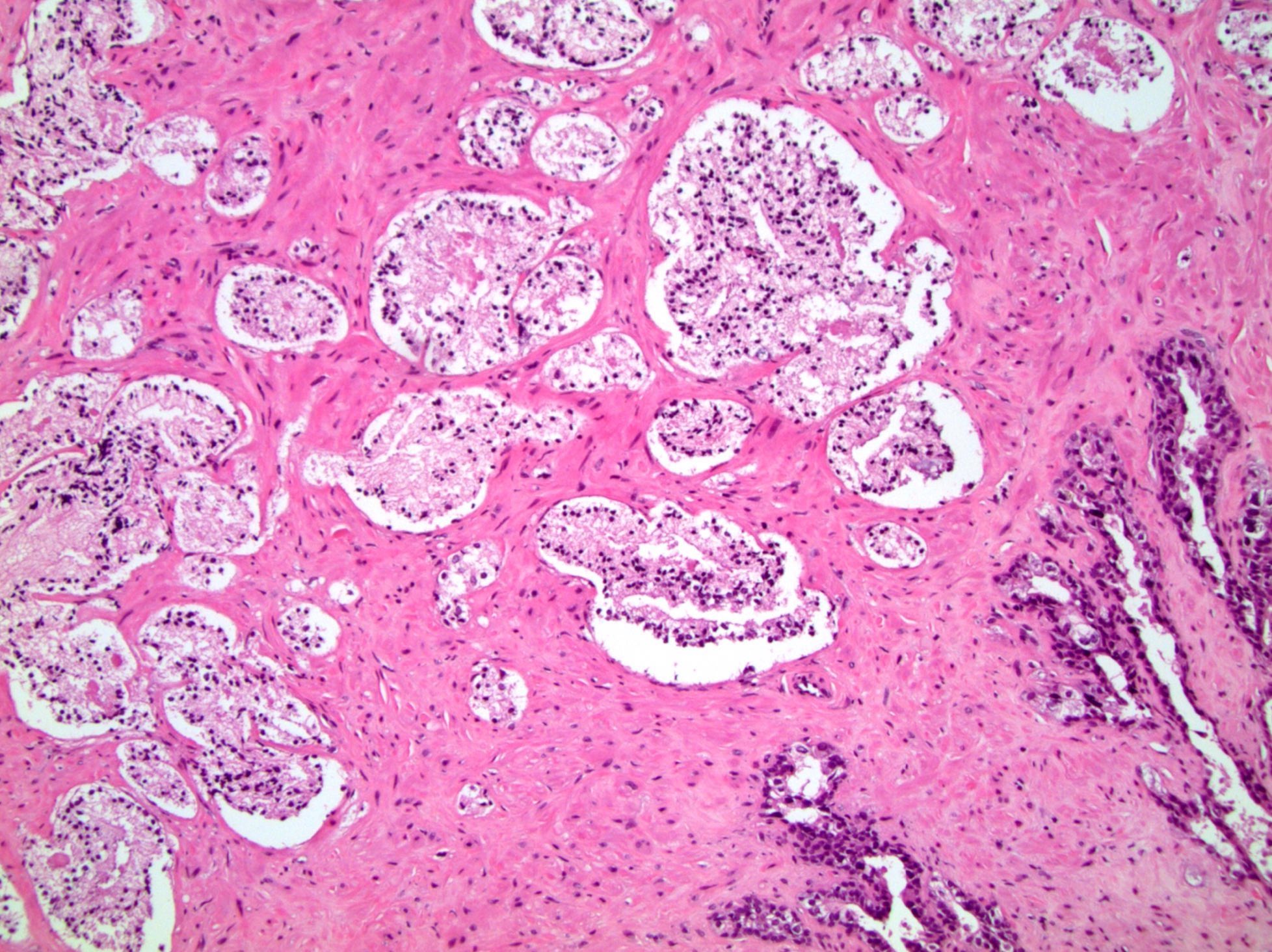
Microscopic (histologic) images
Contributed by Debra L. Zynger, M.D.
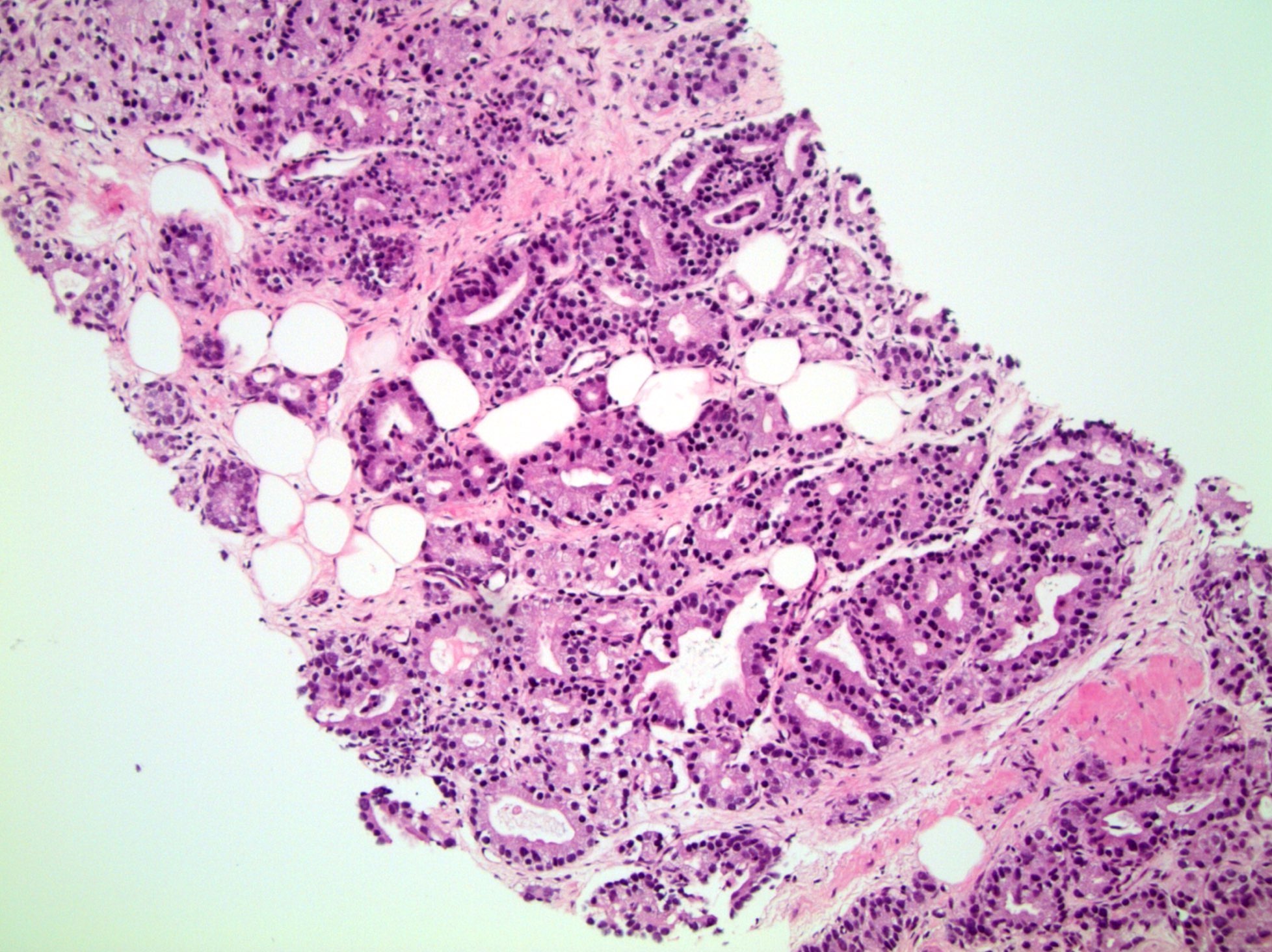
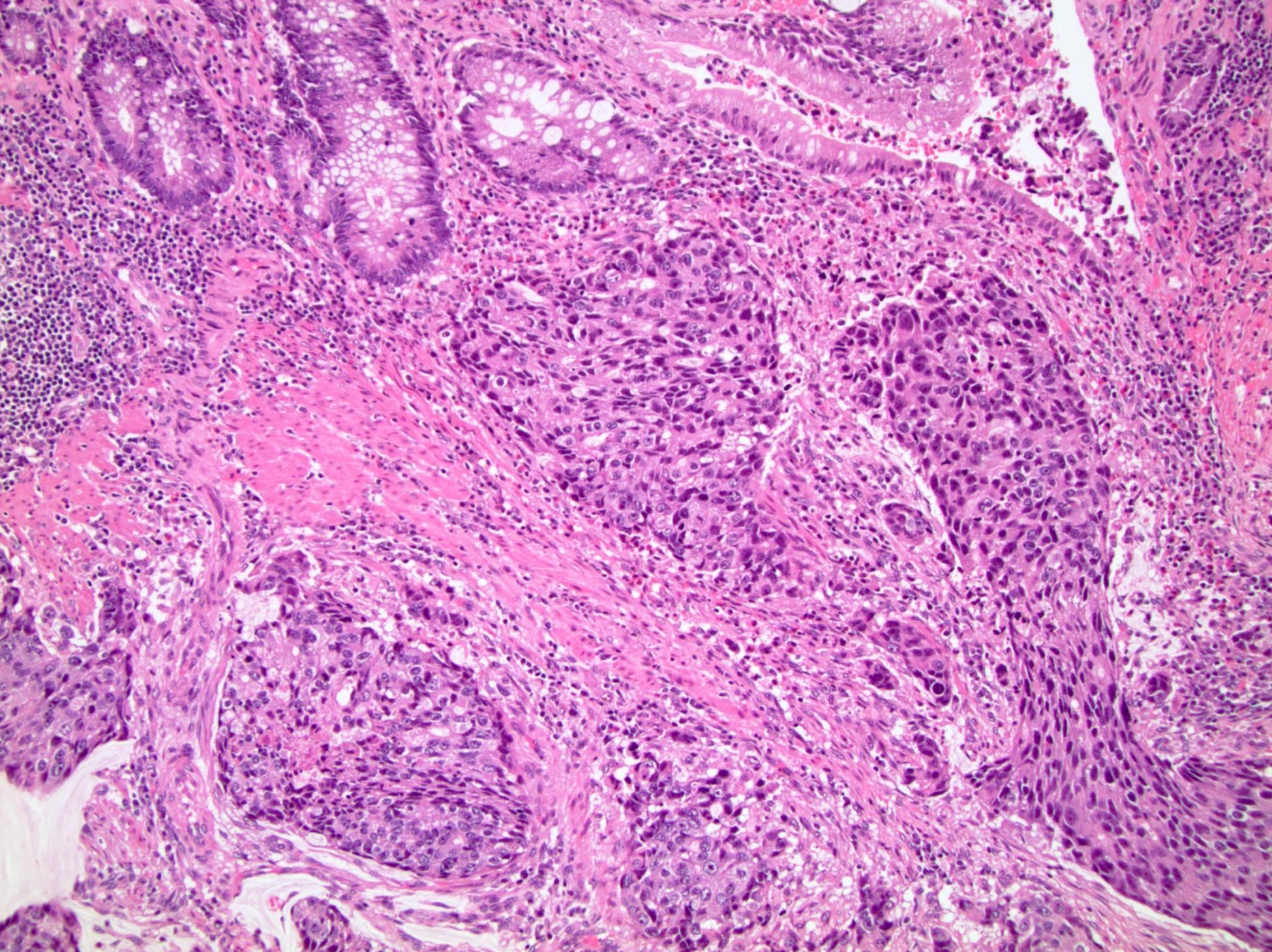
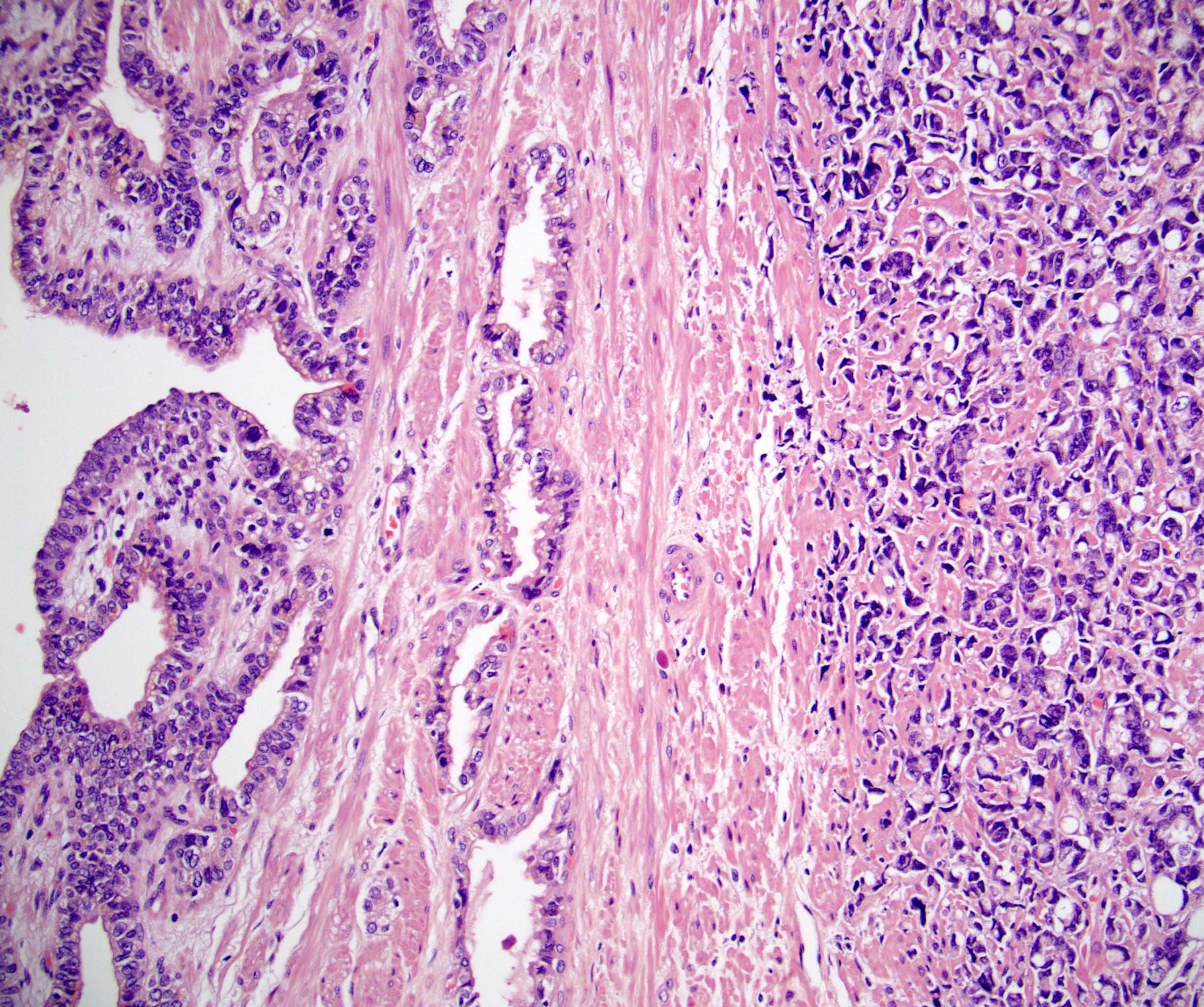
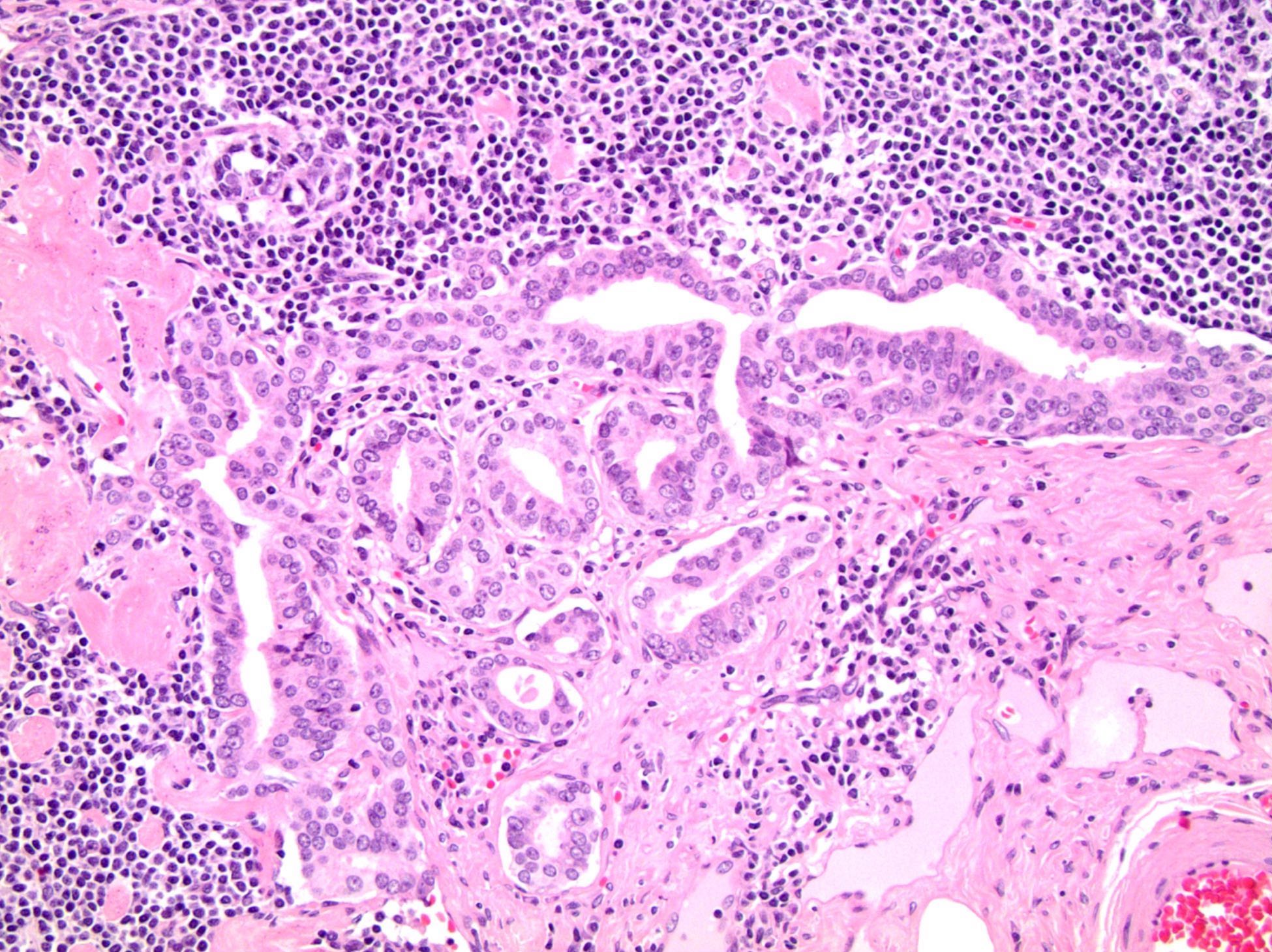
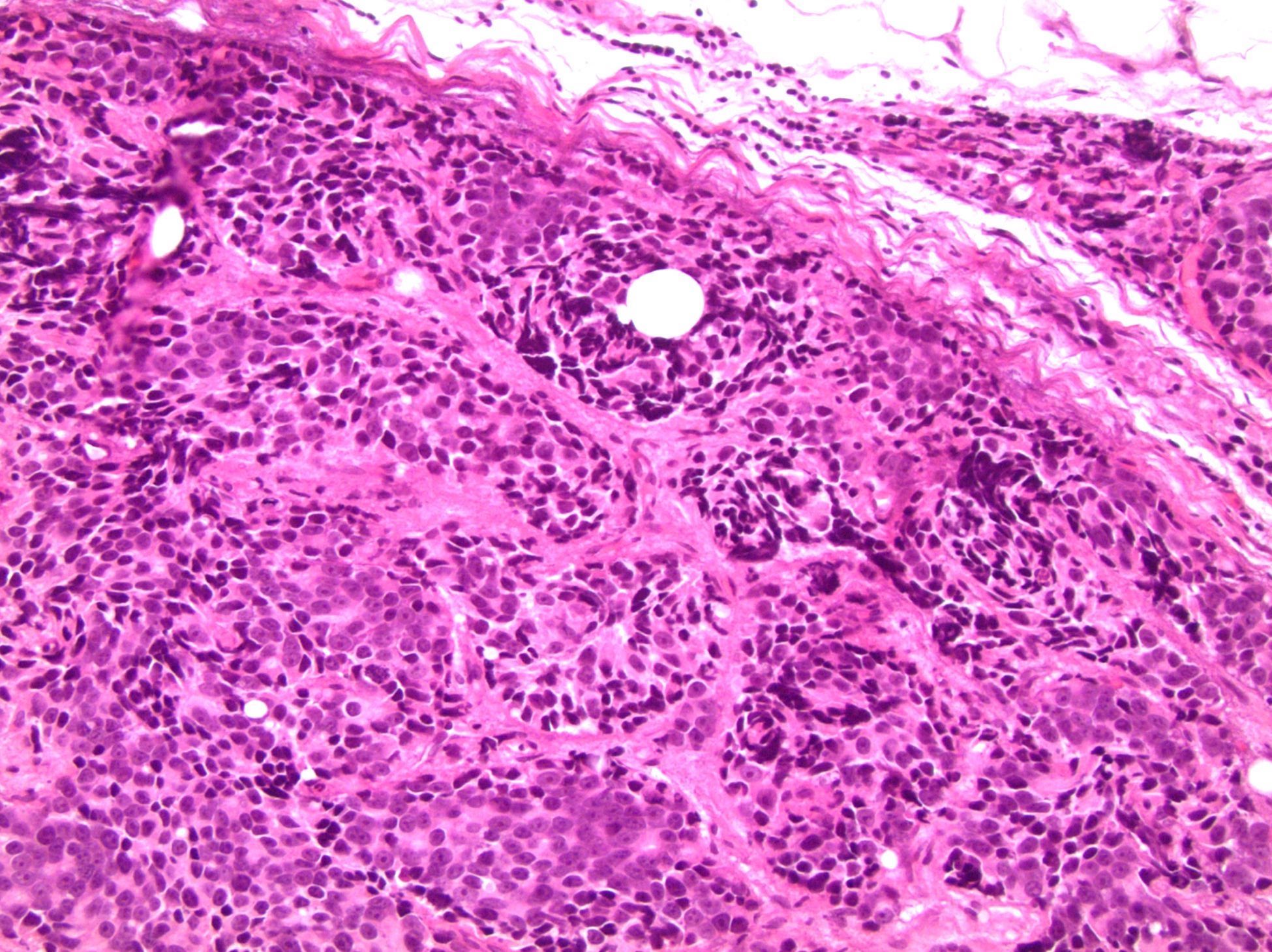
Extraprostatic extension (pT3a)
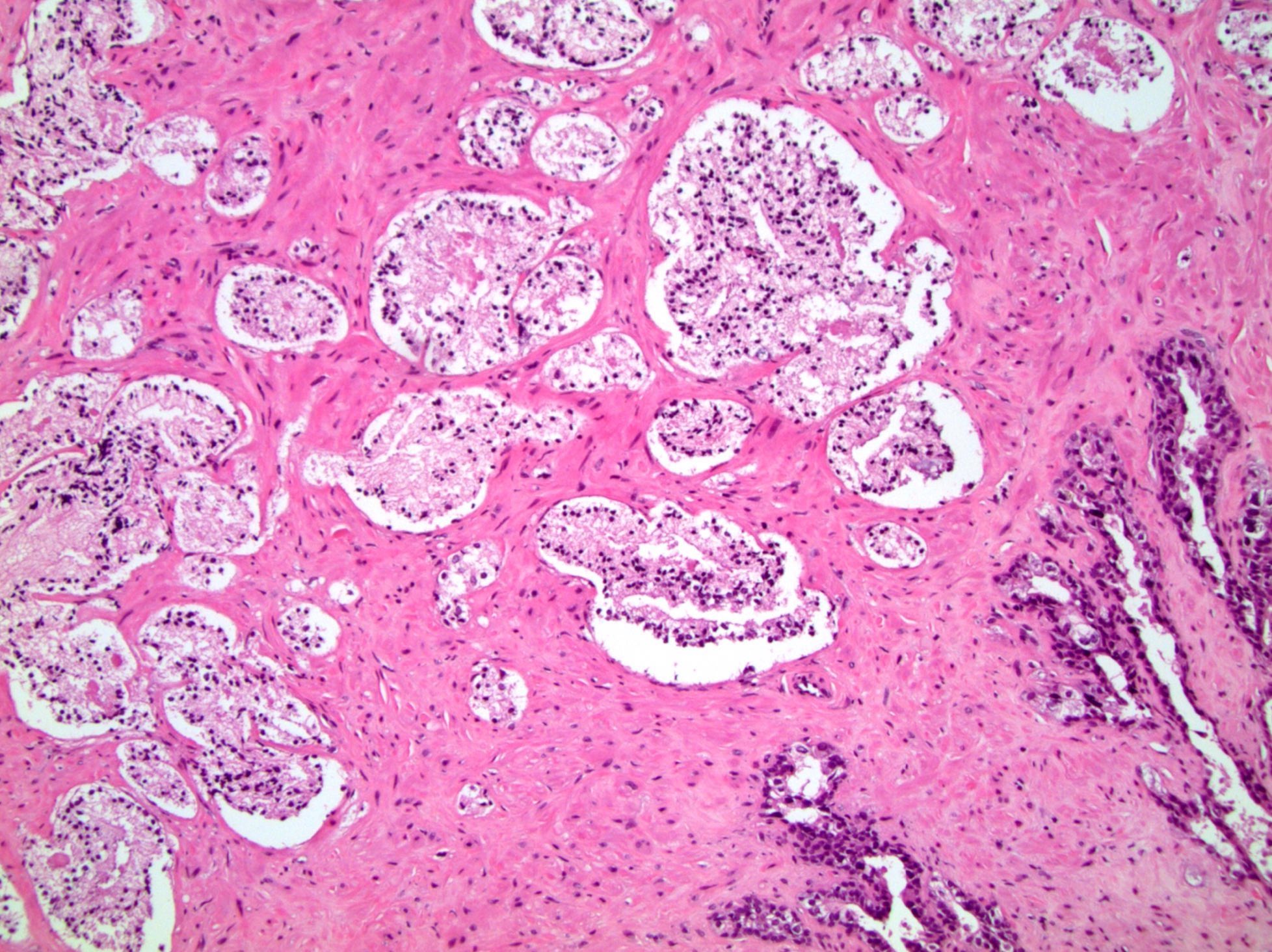
Bladder neck invasion (pT3a)

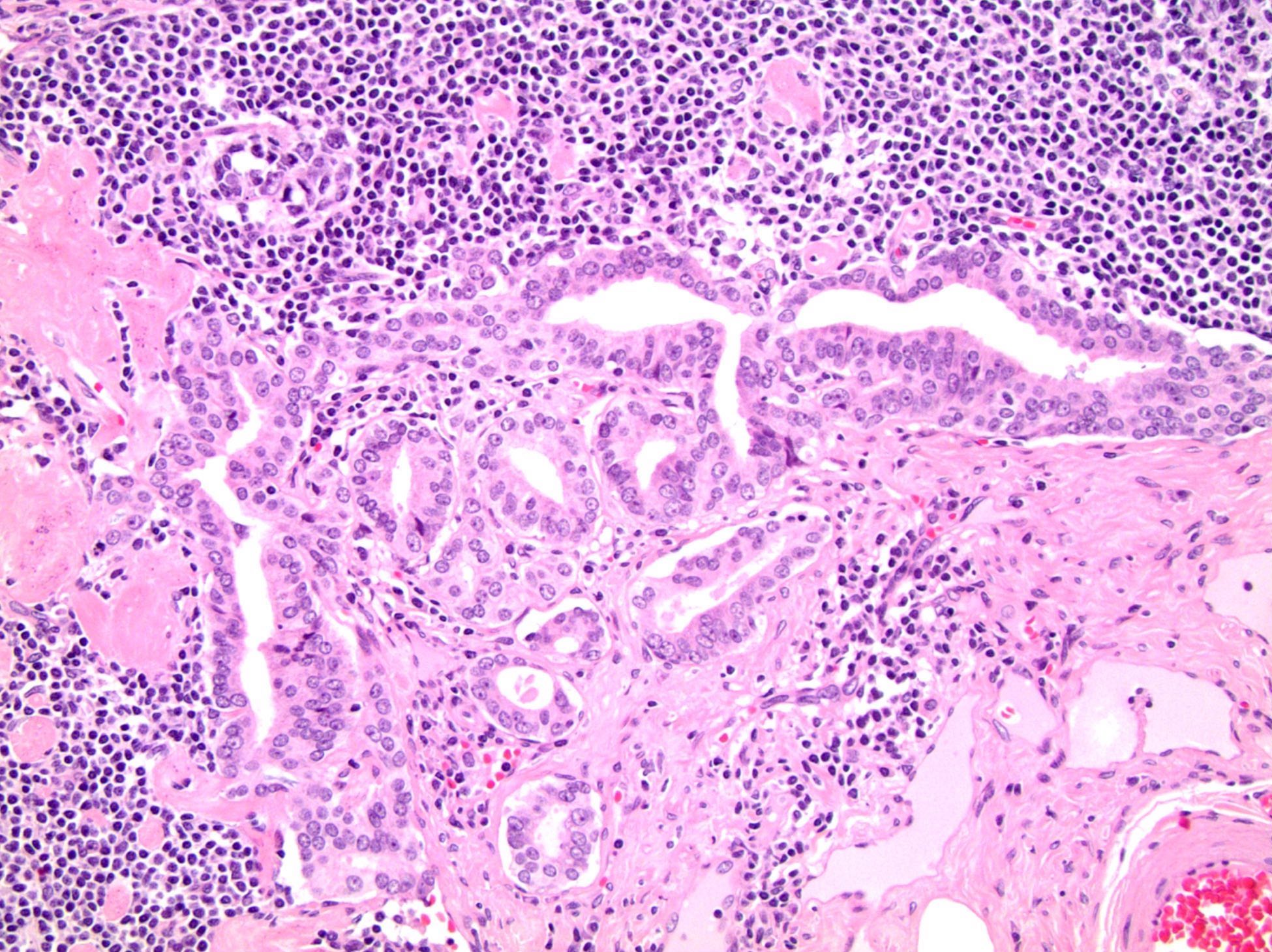
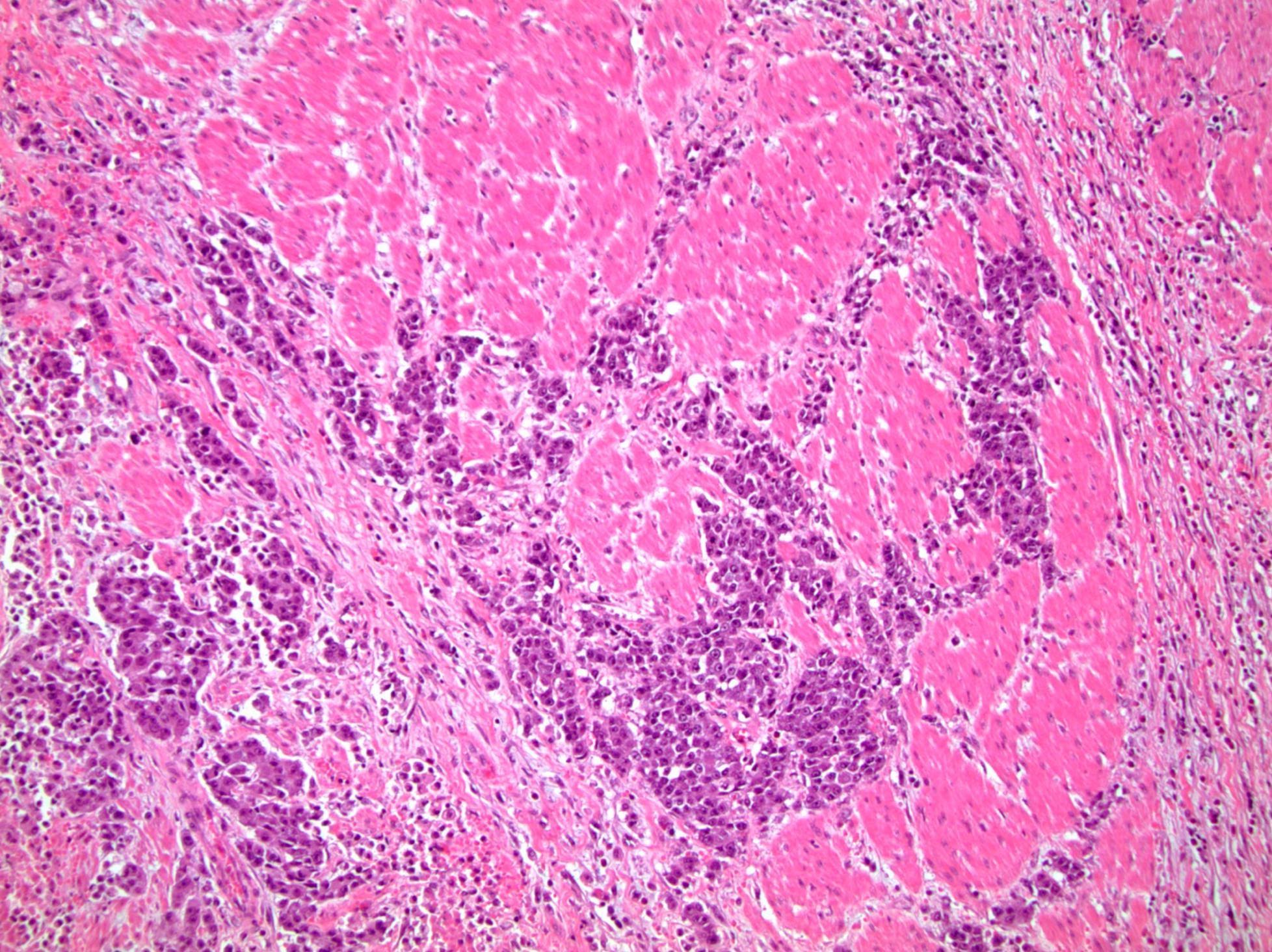
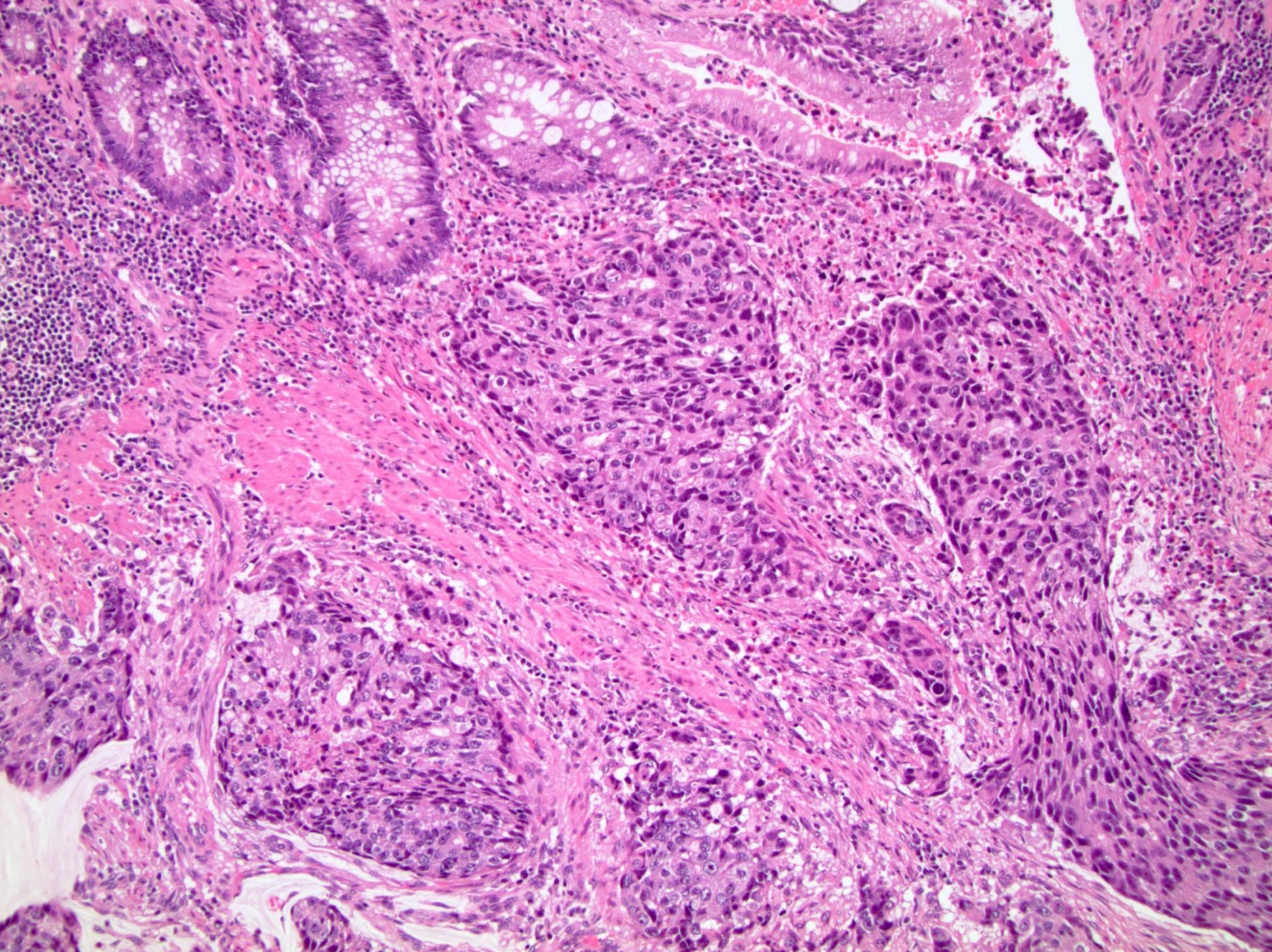
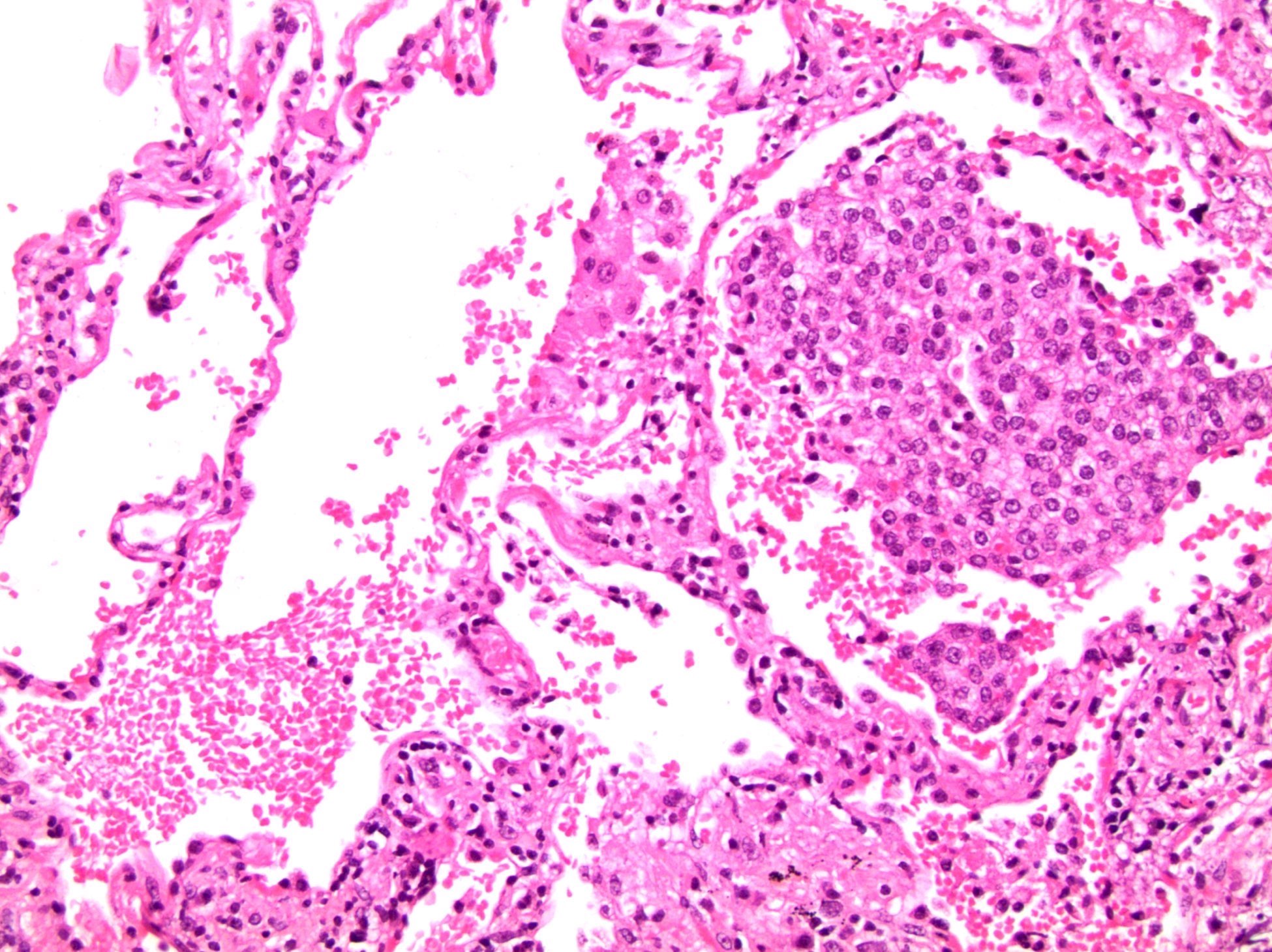
Seminal vesicle invasion (pT3b)
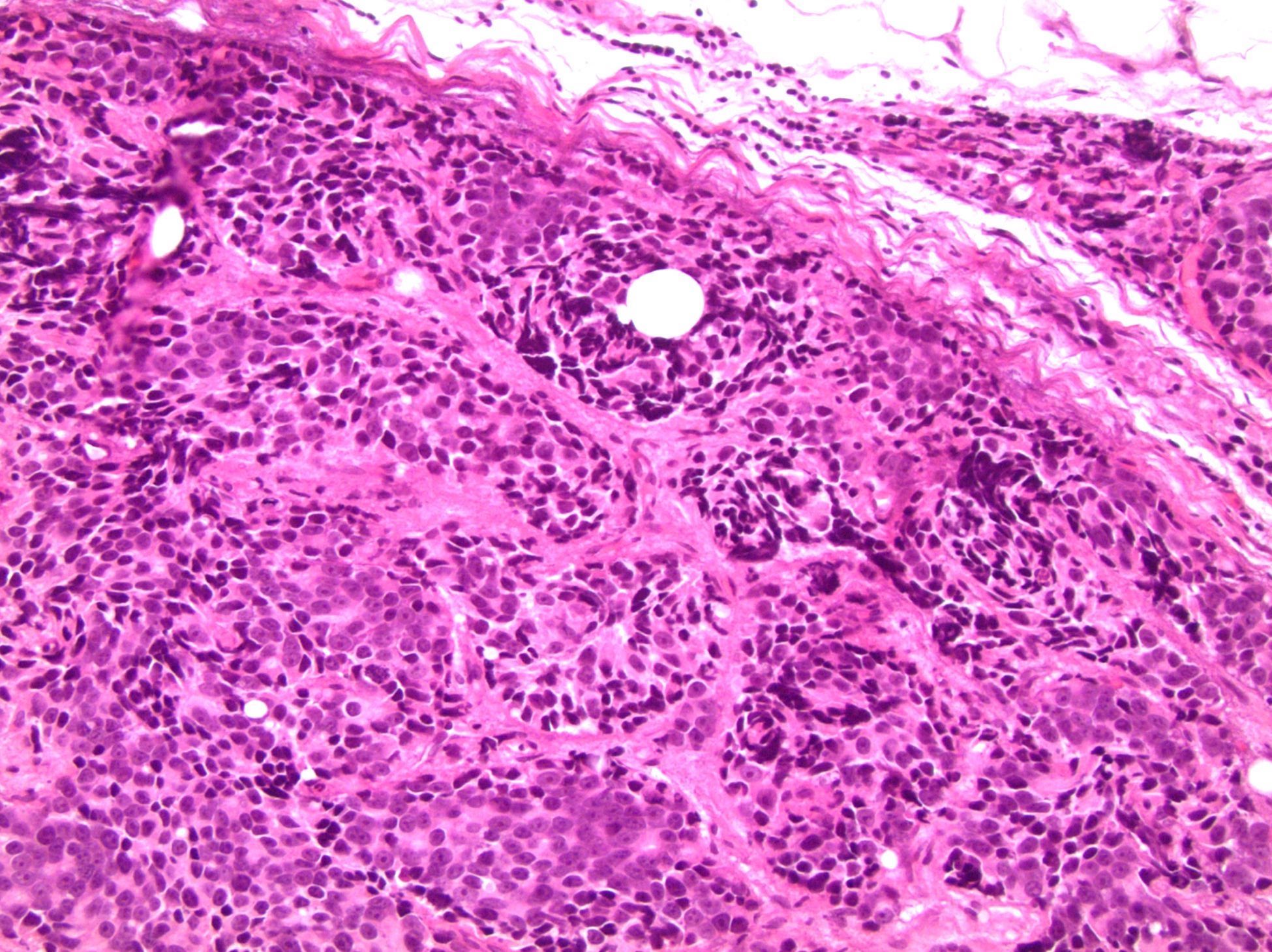
Rectal invasion (pT4)
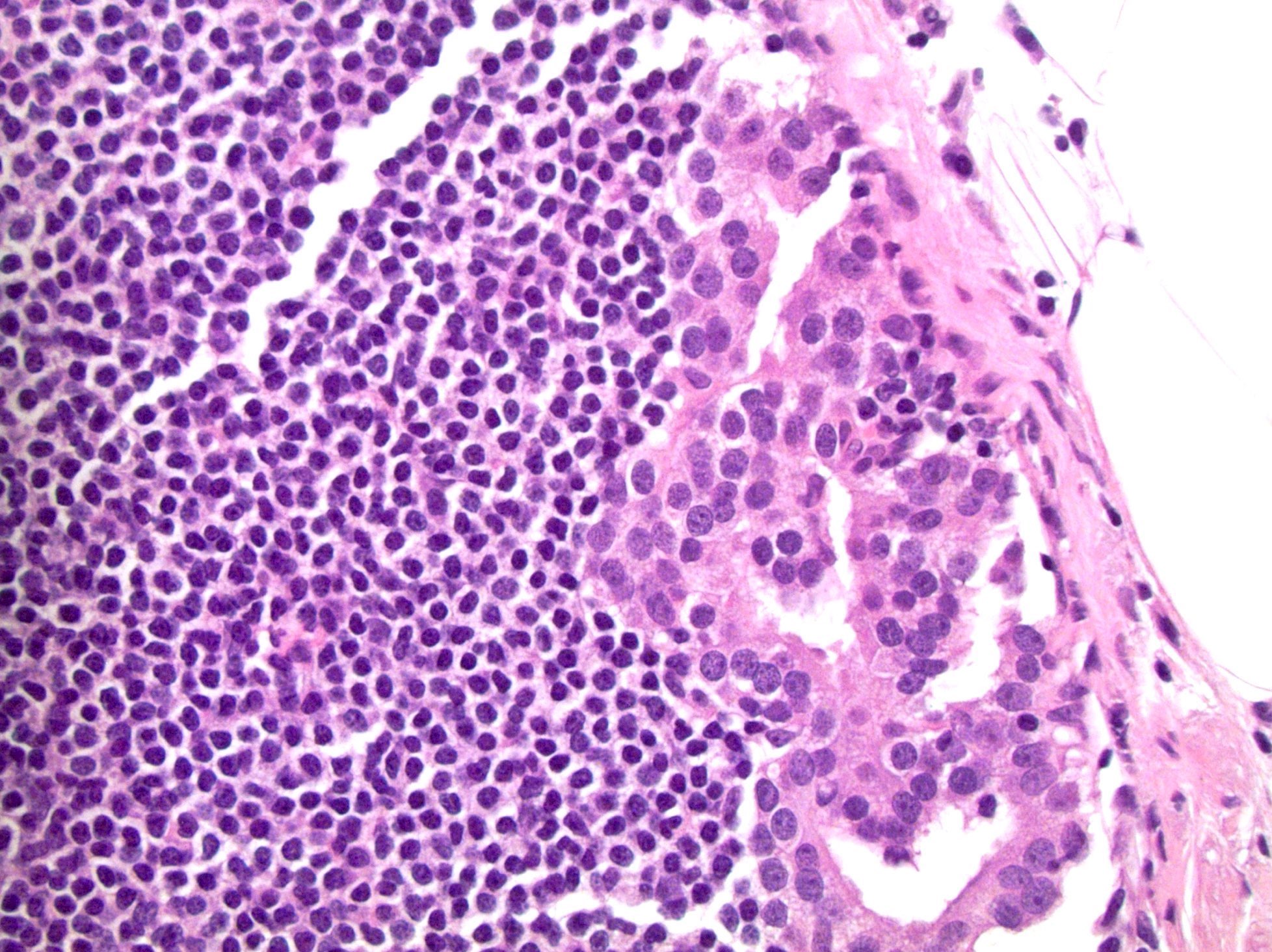
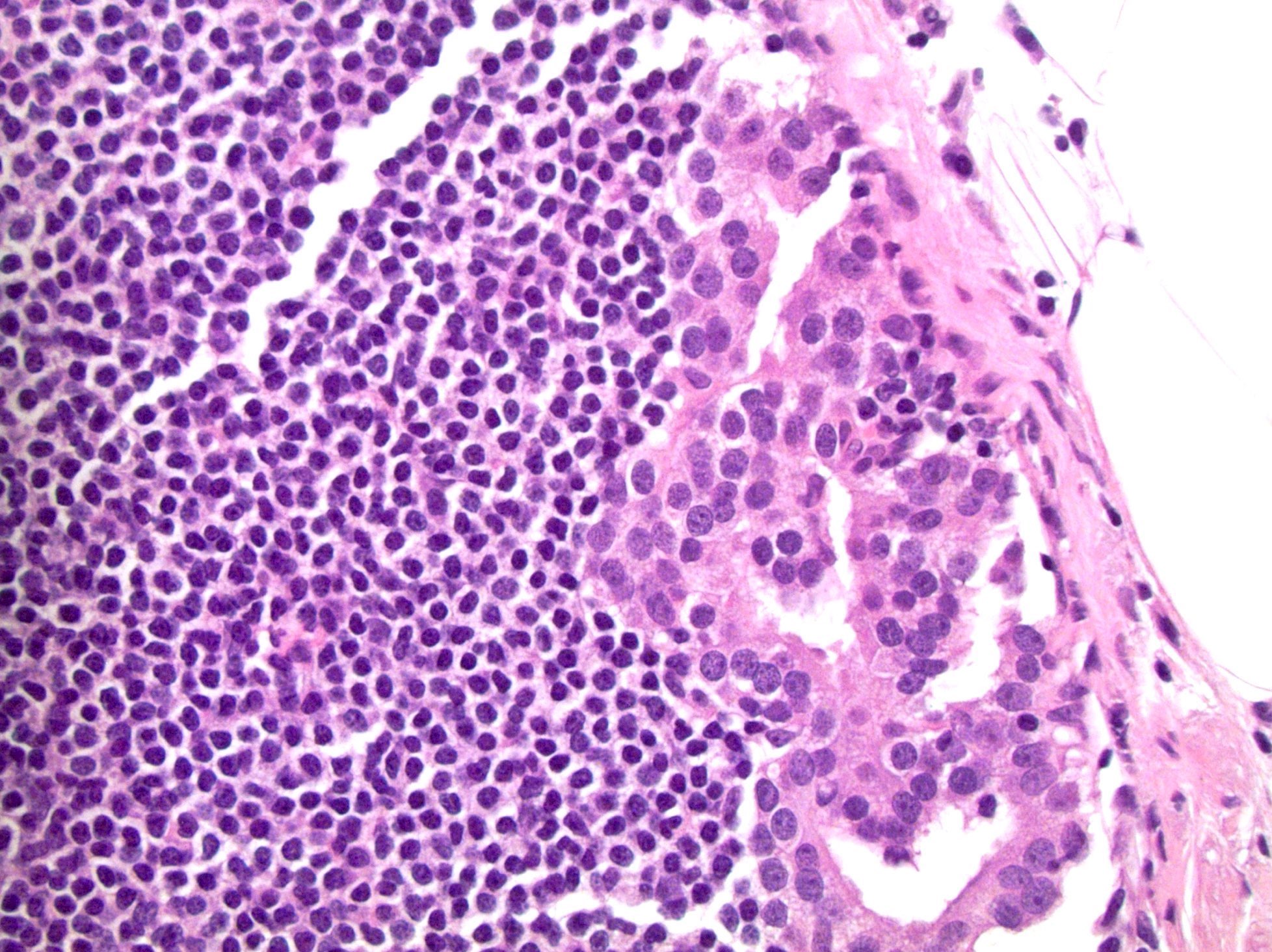
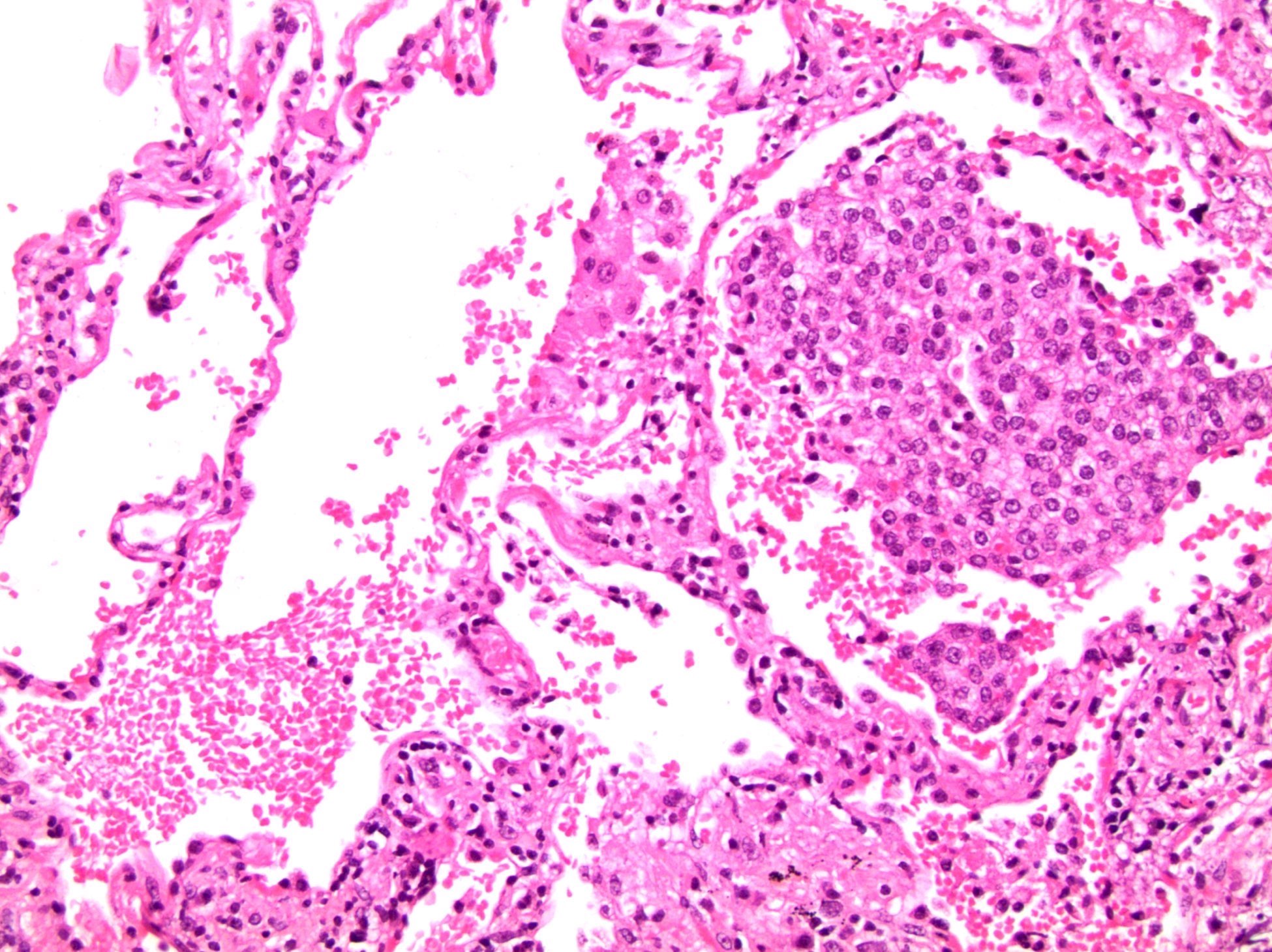
Periprostatic lymph node metastasis (pN1)
Pelvic lymph node metastasis (pN1)
Neck lymph node metastasis (pM1a)
Bone metastasis (pM1b)
Lung metastasis (pM1c)

Brain metastasis (pM1c)
Board review style question #1
A radical prostatectomy was performed and a cross section of the seminal vesicle wall is shown above. There is involvement by high grade prostatic adenocarcinoma. Which of the following is the correct pT?
- pT2
- pT3a
- pT3b
- pT4
Board review style answer #1
Back to top