Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Aivazian K, Gupta R. Carcinoma ex pleomorphic adenoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/salivaryglandsmalignantmixedtumor.html. Accessed April 18th, 2024.
Definition / general
- Epithelial or myoepithelial malignancy developing from primary or recurrent pleomorphic adenoma
Essential features
- Identification of both malignant and benign components is essential for diagnosis; in cases where the benign component has been obliterated by carcinoma, a history of pleomorphic adenoma at the site must be documented
- 5% of pleomorphic adenomas undergo malignant transformation, with the highest risk associated with recurrent or longstanding pleomorphic adenoma
- Typical clinical presentation is a longstanding palpable mass in the parotid region that has undergone recent rapid growth
- Salivary duct carcinoma and adenocarcinoma NOS are the most frequently encountered malignant components; other malignant components can be myoepithelial carcinoma or epithelial myoepithelial carcinoma
- Main predictors of outcome are patient age, tumor diameter, degree of capsule invasion, histological subtype of malignant component and lymph node or distant metastases
Terminology
- Malignant mixed tumor (not recommended due to possible confusion with carcinosarcoma)
- Carcinoma ex mixed tumor
ICD coding
- ICD-O: 8941/3 - carcinoma in pleomorphic adenoma
Epidemiology
- Uncommon malignancy; annual incidence of 0.17 tumors per 1 million people (Pathol Annu 1993;28 Pt 1:279)
- 11.6% of all malignant salivary gland neoplasms
- 5% of pleomorphic adenomas undergo malignant transformation
- Peak incidence in seventh decade of life (range: 17 - 97 years) (Am J Otolaryngol 2019;40:102279)
- Slight male predominance (Am J Otolaryngol 2019;40:102279)
Sites
- Parotid gland (77%), submandibular gland (18%); other major salivary glands less common (Am J Otolaryngol 2019;40:102279)
- Rare sites include oral cavity, pharynx, lacrimal gland, trachea, nasal cavity (Laryngoscope 2003;113:940, Histopathology 2007;51:868, Head Neck Pathol 2011;5:405)
Pathophysiology
- Incompletely understood
- Concept of stepwise acquisition of genetic aberrations with associated progression
- Earliest change is malignant transformation of ductal epithelial cells associated with dysfunctional p53 protein (Histopathology 2007;51:362)
- Subsequent progression to intracapsular carcinoma, minimally invasive carcinoma and widely invasive carcinoma (Histopathology 2011;59:741)
- Associated with:
- HER2 amplification (Histopathology 2012;60:E131)
- Loss of PLAG1 expression (Hum Pathol 2016;57:152)
- Associated with:
- Myoepithelial carcinomas may progress by different mechanisms (Histopathology 2011;59:741)
Etiology
- Unknown
Clinical features
- Most common presentation is palpable mass in parotid region (Ear Nose Throat J 2019;98:504)
- May present as a sudden increase in size of a preexisting lump, pain or facial paresis / paralysis
- Long history of a mass prior to sudden increase in size is common, suggesting that long delays in treatment of pleomorphic adenoma increase the likelihood of malignant transformation (Acta Oncol 2009;48:132)
- ≤ 25% of patients have a history of previously treated pleomorphic adenoma (Plast Reconstr Surg 2005;116:1206)
- Advanced cases may present with skin ulceration or dysphagia (Head Neck 2001;23:705)
Diagnosis
- Definitive diagnosis rests on microscopic analysis with documentation of both benign pleomorphic adenoma and malignant components
- Sudden increase in size of a longstanding pleomorphic adenoma can raise clinical suspicion of carcinoma ex pleomorphic adenoma
Radiology description
- MRI is superior to CT as it is most sensitive in detecting malignancy and allows better delineation of tissue planes and infiltrative edges (Head Neck Pathol 2012;6:1)
- Characteristic MRI finding is the presence of both encapsulated and invasive components
- Encapsulated (pleomorphic adenoma) component:
- Shows a variety of signal intensities on MRI, reflecting the variability in architectural and cytomorphologic features (AJNR Am J Neuroradiol 2008;29:865)
- Invasive component:
- Hemorrhage, necrosis, irregular margin or infiltration of surrounding tissues
- Low to intermediate signal intensities on T2 weighted images (Acta Radiol 2012;53:303)
- Diffusion weighted images may help differentiate between benign and malignant components (AJNR Am J Neuroradiol 2008;29:865)
- PET signal avidity is inconsistent in salivary gland tumors and therefore not recommended (Head Neck 2019;41:269)
Radiology images
Prognostic factors
- Noninvasive or minimally invasive carcinoma ex pleomorphic adenoma have exceptionally good prognosis (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1996;81:655)
- Older age, male gender, tumor diameter (> 40 mm), degree of capsule invasion, lymph node metastasis, histological subtype are independent predictors of disease specific survival (Am J Otolaryngol 2019;40:102279, Head Neck 2017;39:2416, Oral Surg Oral Med Oral Pathol Oral Radiol 2016;122:598)
- Some studies suggest worse outcomes when the malignant component is myoepithelial carcinoma (Hum Pathol 2010;41:927)
- Histological grade, invasiveness, lymph node involvement and perineural invasion are associated with distant metastases (World J Surg Oncol 2013;11:180)
- Prognosis for carcinoma ex recurrent pleomorphic adenoma is significantly worse than the prognosis for carcinoma ex primary pleomorphic adenoma (Histopathology 2011;59:741)
- Lymph node metastases may occur in 30% of cases (J Surg Oncol 2021;123:446)
- Distant metastases may occur in 4% of cases (J Surg Oncol 2021;123:446)
Case reports
- 28 year old woman presents with a painful growing swelling of the left face (Case Rep Otolaryngol 2020;2020:8325374)
- 40 year old man with an 8 year history of right parotid swelling presents with recent growth (J Cancer Res Ther 2018;14:706)
- 60 year old woman with a remote history of a left buccal lesion presents with a growing buccal mass (Clin Case Rep 2019;7:1994)
- 62 year old man presents with longstanding left temple swelling that has increased in size over several months (Case Rep Oncol Med 2020;2020:1790106)
- 64 year old man with a history of surgery for pleomorphic adenoma presents with a mass in the central face (Head Neck Pathol 2021 Jan 4 [Epub ahead of print])
Treatment
- Successful treatment requires input from a multidisciplinary team (Head Neck 2019;41:269)
- Surgical excision with negative surgical margins is the mainstay of treatment
- Extent of surgery depends on the size and location of the tumor, status of the adjacent cervical nodal basins and relationship to facial nerve, mandible, ear canal and lateral temporal bone
- Adjuvant radiotherapy should be considered in some cases, including (Int J Radiat Oncol Biol Phys 2005;61:103, Otolaryngol Head Neck Surg 2019;160:1048):
- Positive surgical margins
- Advanced stage
- Bone, perineural or lymphovascular invasion
- Involved cervical lymph nodes
- Adjuvant chemotherapy may be required in cases with distant metastases
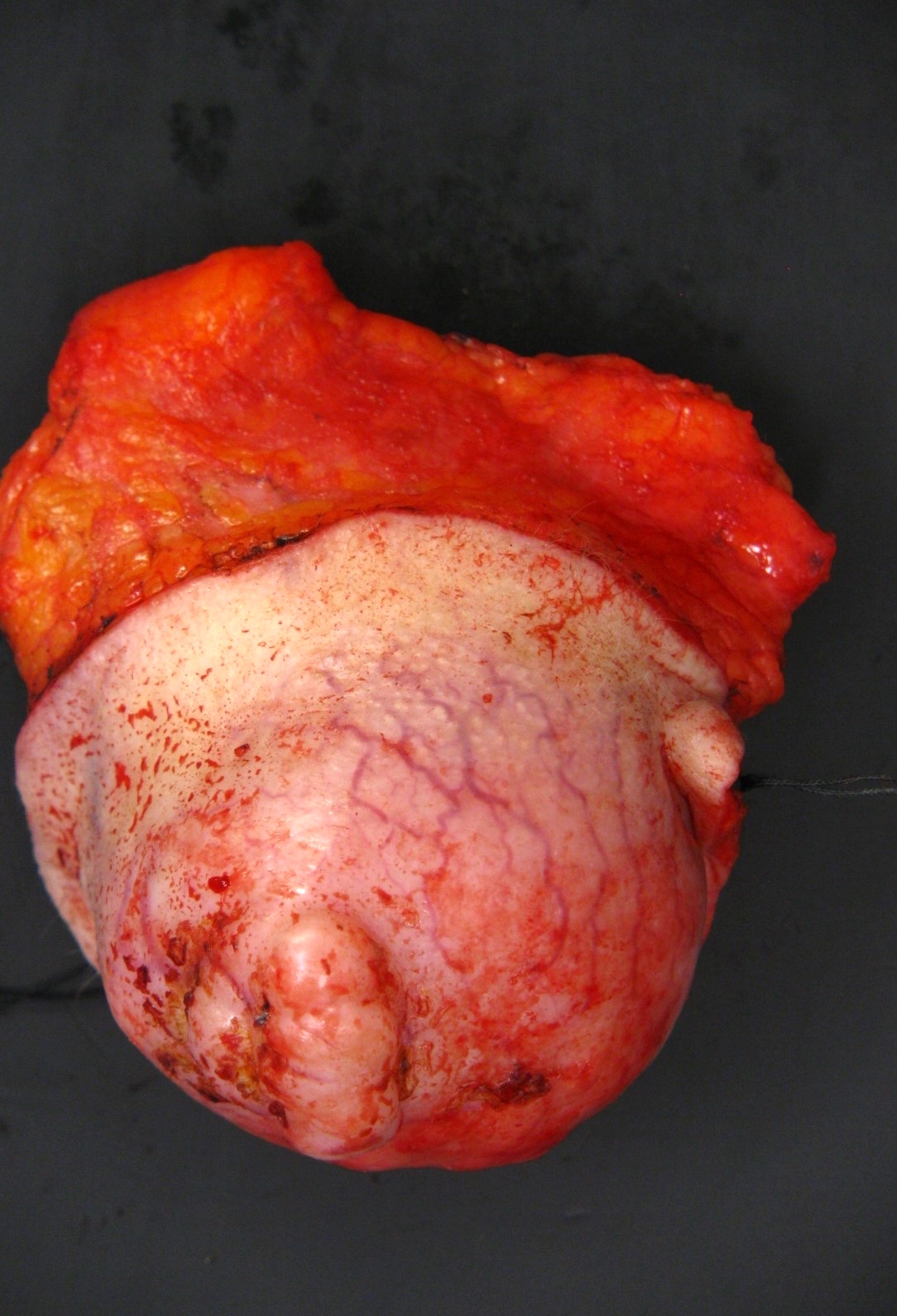
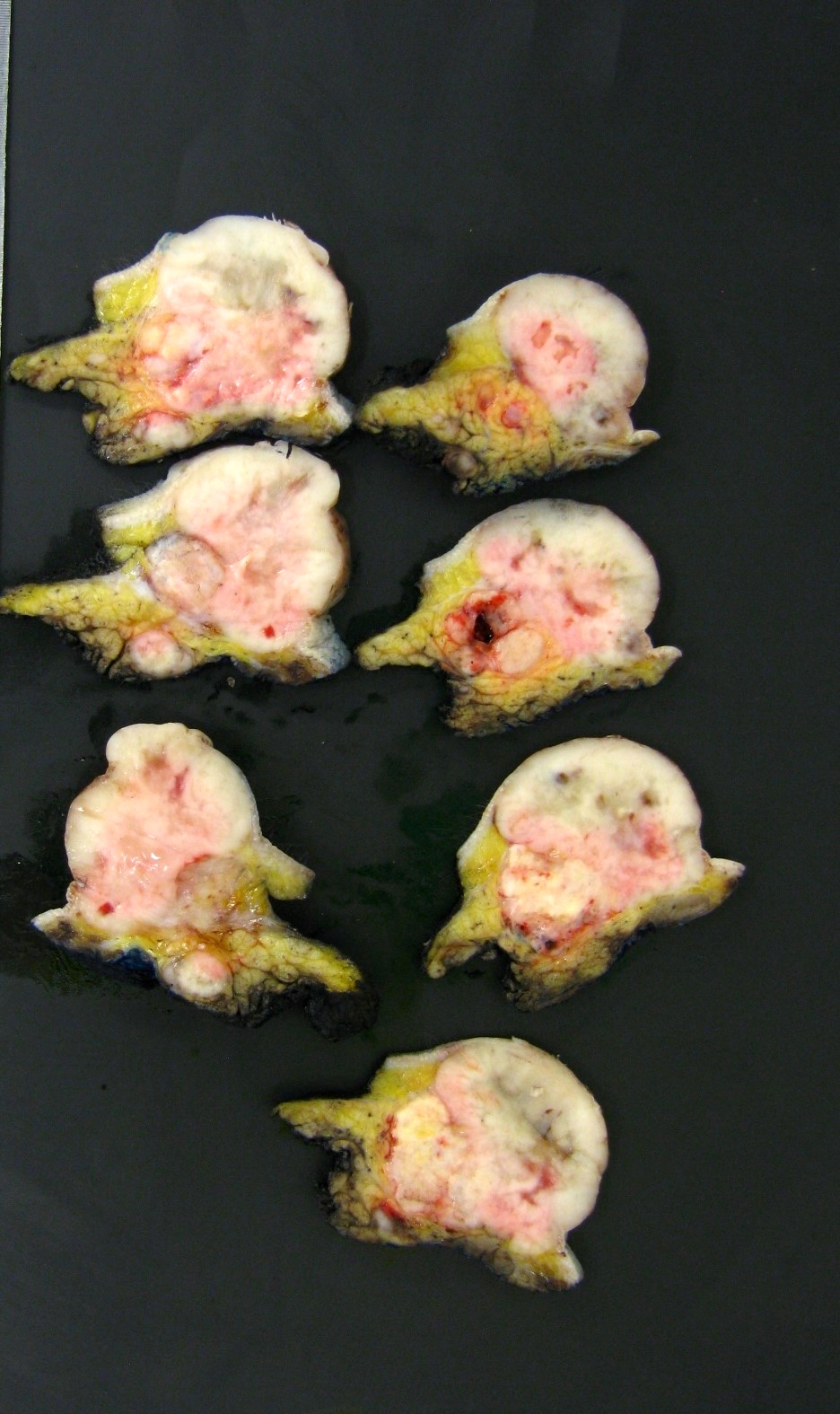
Gross description
- Gross appearance depends on the proportion of pleomorphic adenoma to carcinoma (Hum Pathol 2001;32:596, Head Neck 2001;23:705)
- If pleomorphic adenoma is the dominant component, it may appear circumscribed and gray, glistening or white
- If pleomorphic adenoma is not apparent, it may be a poorly circumscribed irregular infiltrative mass involving adjacent structures
- Malignant component can show necrosis or hemorrhage
Gross images
Frozen section description
- Routine use of frozen section for salivary gland tumors is not appropriate (Head Neck 2019;41:269)
- May be useful in some settings (e.g. in cases of facial nerve sacrifice to ensure negative nerve stump margin) (Head Neck 2019;41:269)
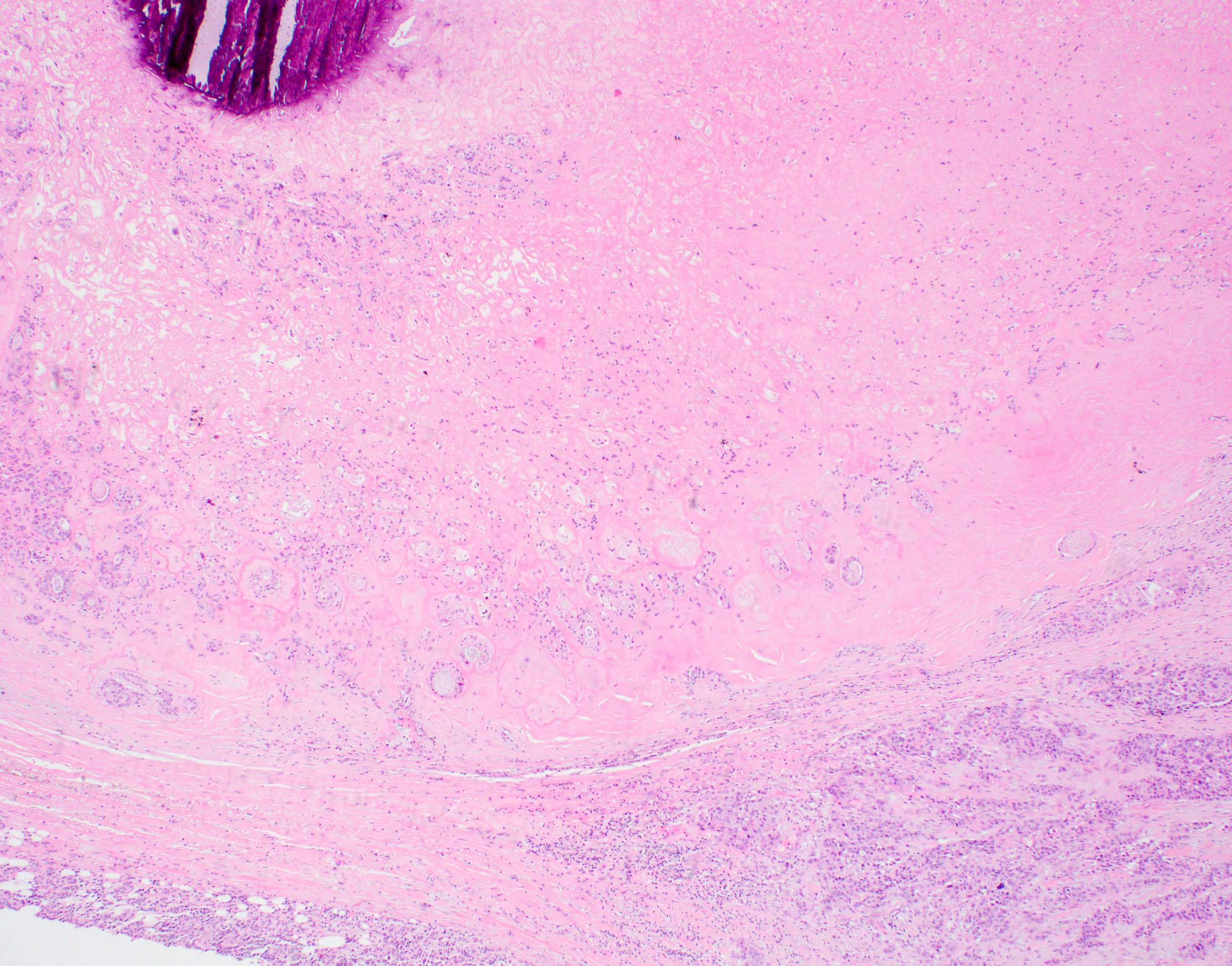
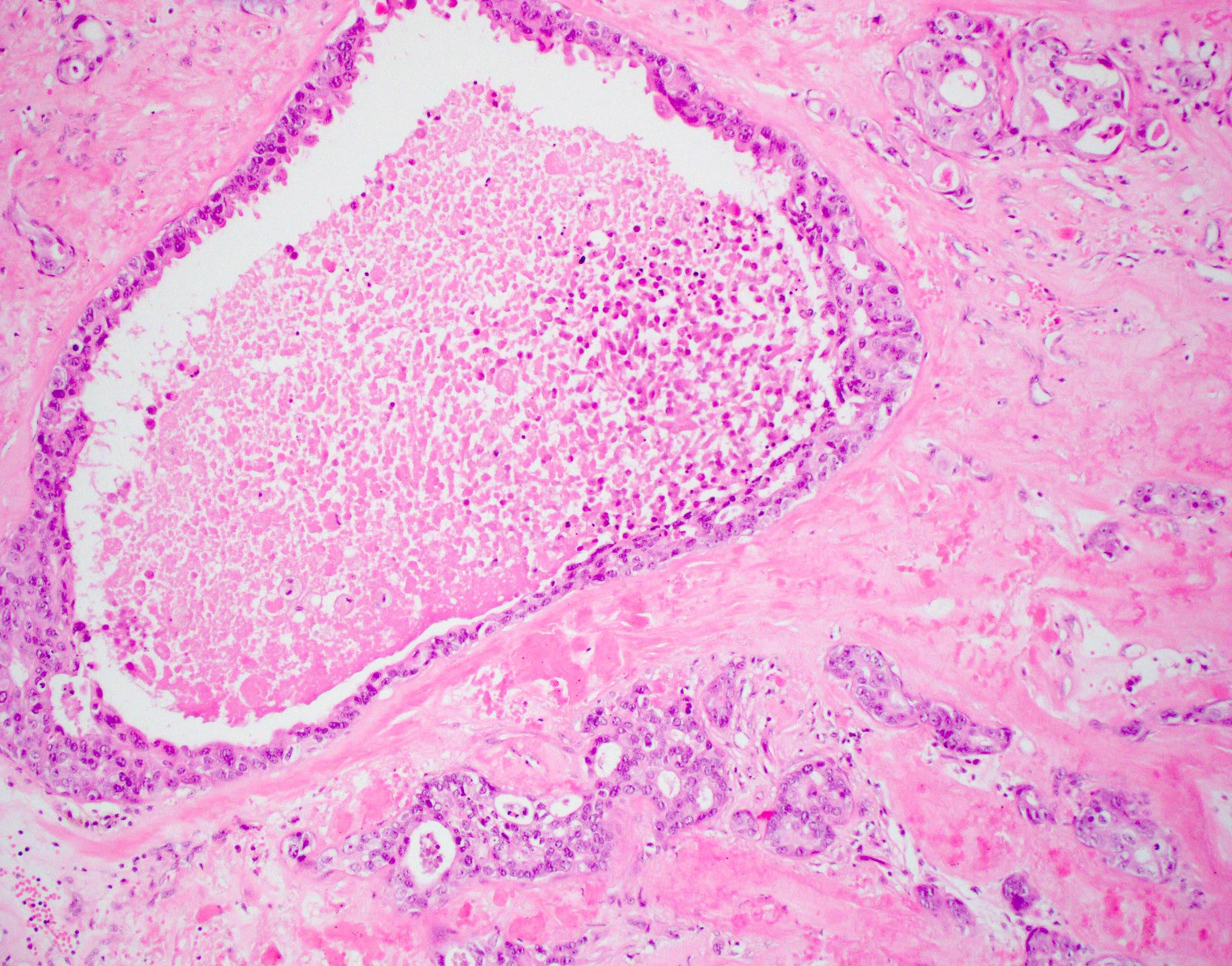
Microscopic (histologic) description
- Must have either:
- Microscopic confirmation of both benign and malignant components or
- Microscopic diagnosis of carcinoma (see below) and previously documented pleomorphic adenoma at the site
- Stratification based on extent of capsule invasion:
- Intracapsular: good prognosis
- Minimally invasive: generally considered as < 1.5 mm
- Poorly defined category
- Extent of invasion may be less relevant in intrinsically aggressive carcinomas, such as salivary duct carcinoma (Histopathology 2014;65:854)
- Requires histologic evaluation of the entire lesion and possible examination through multiple deeper levels / sections
- Widely invasive: ≥ 1.5 mm
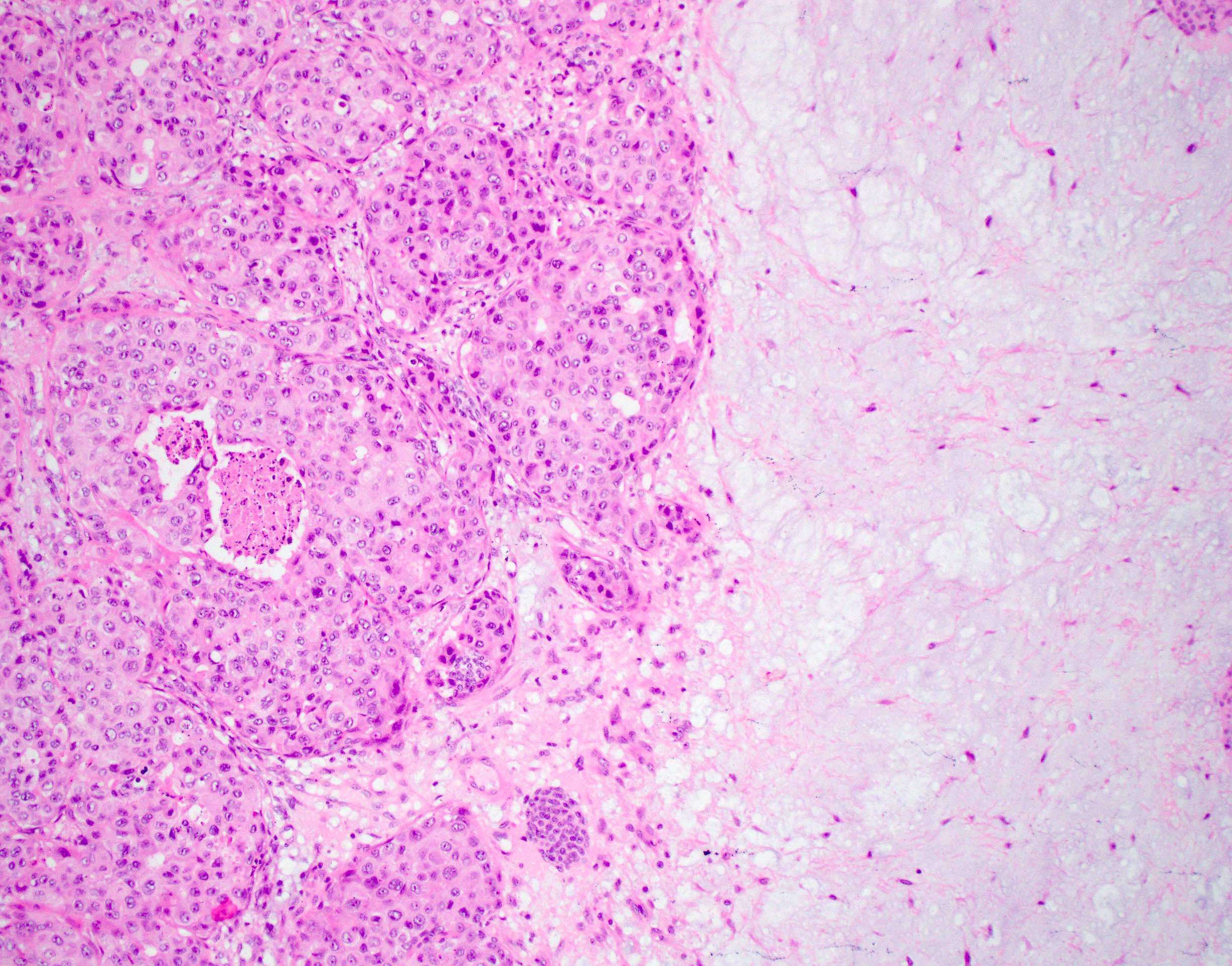
- Carcinomatous component may be salivary duct carcinoma, myoepithelial carcinoma or epithelial myoepithelial carcinoma
- If adenocarcinoma:
- Often high grade
- Salivary duct carcinoma and adenocarcinoma NOS are most common
- Other types of differentiation may be seen, including squamous, mucoepidermoid and polymorphous adenocarcinoma
- If myoepithelial carcinoma, it is often low grade
- Mixture of subtypes may also occur (Int J Oral Maxillofac Surg 2009;38:1116)
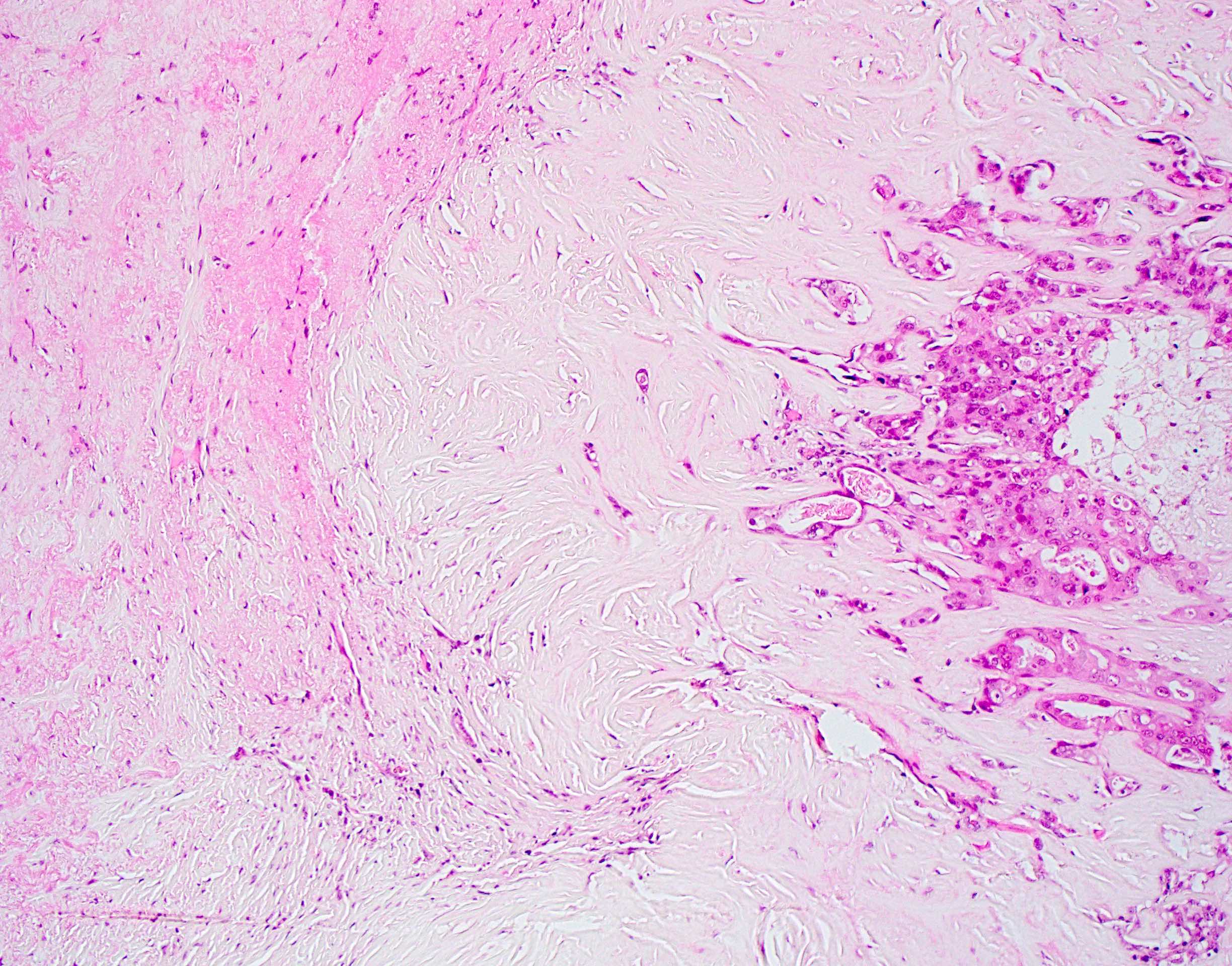
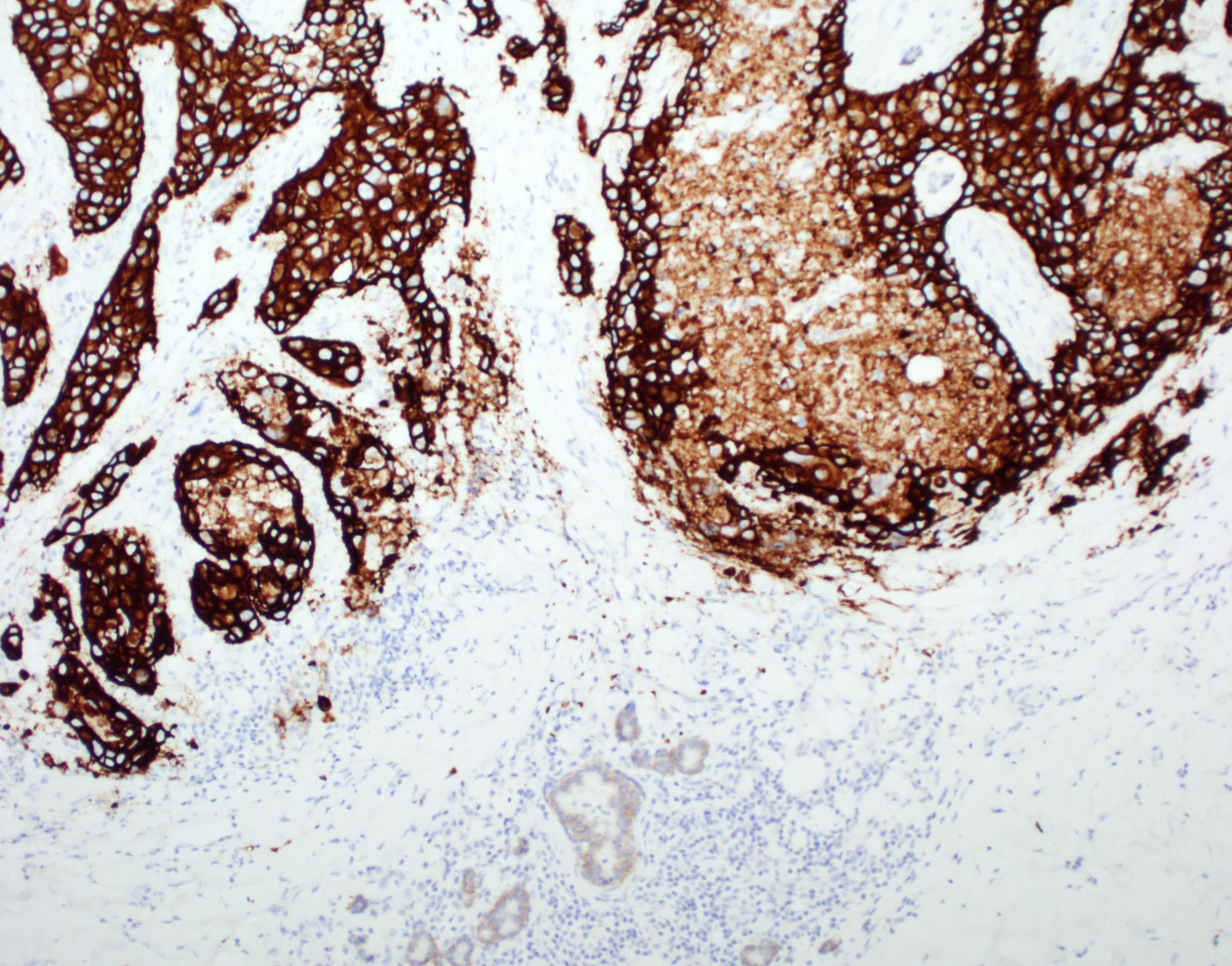
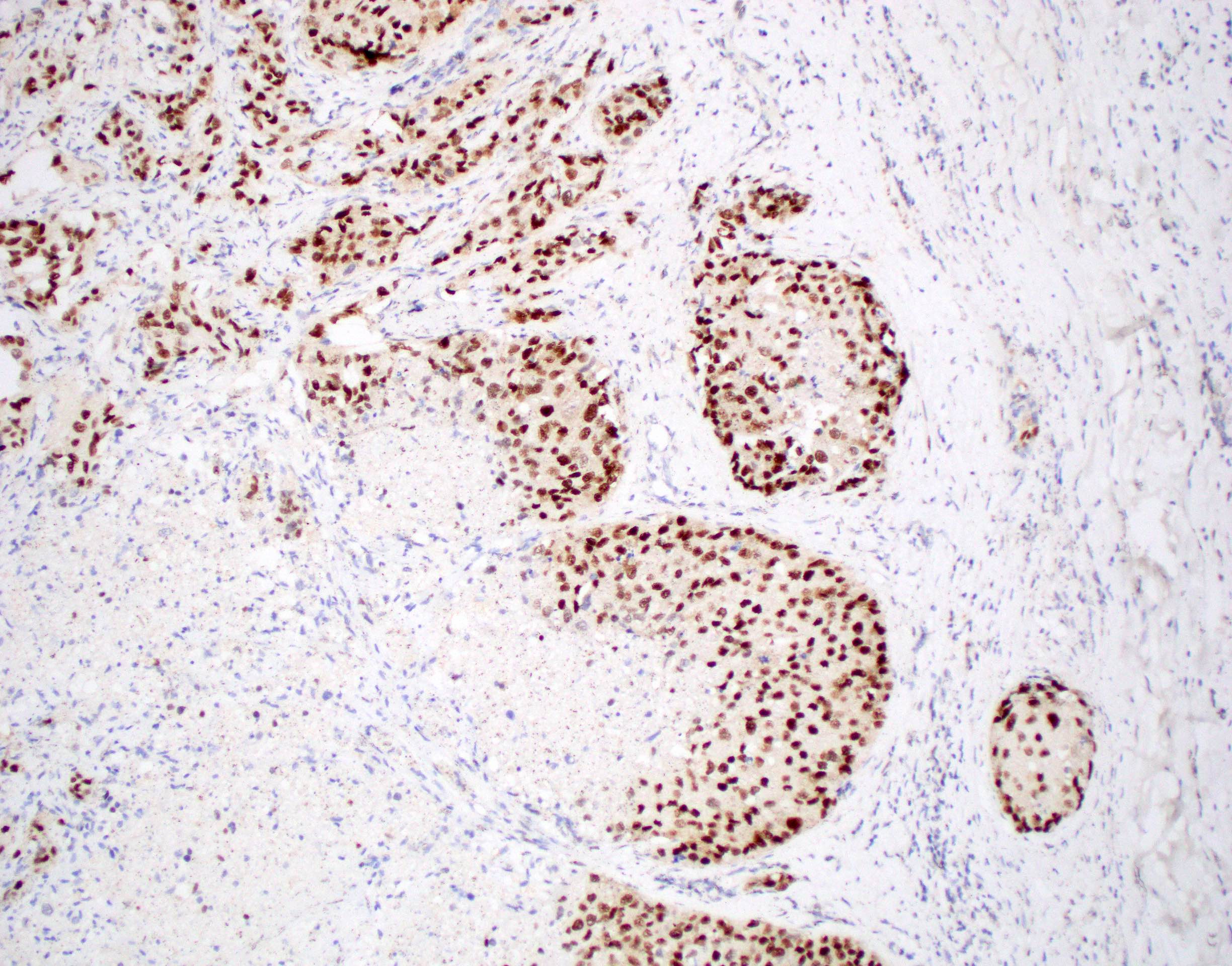
Microscopic (histologic) images
Cytology description
- Pleomorphic adenoma component:
- Sheets or cohesive groups of ductal cells
- Myoepithelial cells individually dispersed or in loose clusters
- Dense fibrillary metachromatic matrix is the most characteristic finding: appears magenta in Romanowsky type stains
- Carcinomatous component:
- Pleomorphic, hyperchromatic cells, clumped chromatin, high N/C ratio (Cytojournal 2015;12:7)
- Necrotic background
- Features specific to the type of carcinoma may be seen (e.g. mucous cells, squamoid cells)
- Fine needle aspiration has low sensitivity in the diagnosis of carcinoma ex pleomorphic adenoma, likely due to sampling error (Plast Reconstr Surg 2005;116:1206)
- Even when a diagnosis is possible, cannot differentiate between noninvasive and invasive tumors (Cytojournal 2015;12:7)
- Carcinomatous component is more likely to be identified on FNA if it is high grade and extensive (Diagn Cytopathol 2020;48:149)
Positive stains
- Pleomorphic adenoma:
- Carcinoma ex pleomorphic adenoma:
- Immunohistochemistry depends on the classification of the malignant component
- Salivary duct carcinoma: CK7, EMA, HER2, AR, p53 overexpressed in 60% of cases (Am J Surg Pathol 2015;39:744)
- Adenocarcinoma NOS: no useful stains
- Myoepithelial carcinoma: calponin, p63, p40, SMMHC (see above)
- Mucoepidermoid carcinoma: CK7, CK5/6 (squamoid cells), p63 (squamous cells), mucin stains (mucous cells)
- Ki67 is useful to highlight benign and malignant components:
- Labels < 5% of cells in pleomorphic adenoma, even in recurrences (Laryngoscope 2004;114:158)
- Can be very high in malignant component
- HMGA2 immunohistochemistry has high specificity but low sensitivity for carcinoma ex pleomorphic adenoma (Histopathology 2017;71:511)
Molecular / cytogenetics description
- Gene rearrangements or amplifications are seen in both pleomorphic adenoma and carcinoma ex pleomorphic adenoma involving:
- PLAG1 (Head Neck Pathol 2012;6:328)
- HMGA2 (Hum Pathol 2015;46:26)
- HMGIC and MDM2 (Am J Pathol 2002;160:433)
- HER2 amplification was found in 39% of carcinoma ex pleomorphic adenoma (Histopathology 2012;60:E131)
- TP53 mutations were detected in 37% of intracapsular carcinoma ex pleomorphic adenoma (Histopathology 2007;51:362)
- Copy number gains in 9p and 22q have been detected in carcinoma ex pleomorphic adenoma of lacrimal gland (Ophthalmology 2014;121:1125)
Sample pathology report
- Carcinoma ex pleomorphic adenoma (see comment)
- Comment: In large areas, the tumor shows a sclerotic nodule. Several infiltrative glands and ducts are seen extending from the periphery of this sclerotic nodule into the adjacent residual salivary gland and attached skeletal muscle. Occasional glands show internal cribriform architecture with Roman bridges and arches and resemble ductal carcinoma in situ of the breast. The glands are lined by cells with an apocrine appearance with apical snouts, moderate eosinophilic cytoplasm and enlarged nuclei with distinctive nucleoli. Mitoses are present. Multiple foci of lymphovascular involvement are present. Perineural involvement is seen. The tumor is present at the margin of resection. In addition, 5/25 lymph nodes in the accompanying neck dissection show metastatic carcinoma. History of a longstanding nodule in the region of the parotid gland with sudden increase in size and new onset facial palsy is noted. The clinical history and the morphologic features support a diagnosis of a carcinoma ex pleomorphic adenoma.
Differential diagnosis
- Recurrent pleomorphic adenoma:
- Commonly multinodular; may show numerous disconnected nodules with no obvious capsule, simulating invasion (Laryngoscope 2004;114:158)
- History of incompletely resected or previously recurrent pleomorphic adenoma is a clue to the diagnosis
- Pleomorphic adenoma with pseudopodia:
- Small protrusions of tumor beyond the tumor capsule, found in up to a quarter of cases and without clinical consequence unless incompletely excised (Laryngoscope 2001;111:2195, Cancer 1998;82:617)
- Must not be confused with malignant transformation
- De novo carcinoma:
- Identification of residual pleomorphic adenoma (or a history of recurrent / incompletely excised pleomorphic adenoma) is essential for diagnosis of carcinoma ex pleomorphic adenoma
- PLAG1 and HMGA2 genetic aberrations are seen in carcinoma ex pleomorphic adenoma but not its malignant de novo counterparts (Hum Pathol 2015;46:26)
- Metastatic carcinoma:
- History of other primary head and neck malignancy
- Absence of pleomorphic adenoma component
Board review style question #1
Regarding carcinoma ex pleomorphic adenoma, which of the following statements is true?
- Fine needle aspiration is a highly sensitive technique for the diagnosis of this entity
- Malignant transformation is equally likely to occur in a primary pleomorphic adenoma as it is in recurrent pleomorphic adenoma
- Not always possible to identify the preexisting pleomorphic adenoma macroscopically
- Submandibular gland is the most common site of origin
Board review style answer #1
C. It is sometimes not possible to identify the pleomorphic adenoma macroscopically or even microscopically; this is one of the reasons why thorough sampling is required. This is because the malignant component may overgrow and subsume the benign component. In such circumstances, a history of pleomorphic adenoma, particularly if longstanding or recurrent, is vital for correct diagnosis. Like pleomorphic adenoma, carcinoma ex pleomorphic adenoma arises most commonly in the parotid gland. Recurrent pleomorphic adenoma has a higher risk of malignant transformation than primary pleomorphic adenoma. Fine needle aspiration has low sensitivity in the diagnosis of carcinoma ex pleomorphic adenoma, largely due to sampling error.
Comment Here
Reference: Carcinoma ex pleomorphic adenoma
Comment Here
Reference: Carcinoma ex pleomorphic adenoma
Board review style question #2
A 57 year old man presents with right facial swelling and paralysis. Following appropriate workup, he undergoes surgical resection of the right facial mass. A representative histological image is provided above. Regarding his diagnosis, which statement is true?
- Component on the left is commonly encountered in this entity
- Molecular features of the cellular component are completely distinct from those of the paucicellular component
- Paucicellular component on the right is irrelevant to the final diagnosis
- Presence or absence of a complete capsule around the cellular component does not alter the patient’s prognosis
Board review style answer #2
A. The correct diagnosis is carcinoma ex pleomorphic adenoma. The component on the left is morphologically identical to salivary duct carcinoma, the most common malignant component of carcinoma ex pleomorphic adenoma other than adenocarcinoma NOS. The component on the right is the preexisting pleomorphic adenoma, which is a requirement for diagnosis. PLAG1 and HMGA2 molecular aberrations are encountered in both pleomorphic adenoma and carcinoma ex pleomorphic adenoma. The presence of a tumor capsule is of paramount prognostic significance, as noninvasive or minimally invasive carcinoma ex pleomorphic adenoma is associated with excellent outcomes.
Comment Here
Reference: Carcinoma ex pleomorphic adenoma
Comment Here
Reference: Carcinoma ex pleomorphic adenoma