Table of Contents
Definition / general | Essential features | CPT coding | Nondiagnostic (category I) | Nonneoplastic (category II) | Atypia of undetermined significance (AUS) (category III) | Neoplasm: benign (category IVA) | Neoplasm: salivary gland neoplasm of uncertain malignant potential (SUMP) (category IVB) | Suspicious for malignancy (SM) (category V) | Malignant (category VI) | Diagrams / tables | Cytology description | Cytology images | Videos | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Hang JF. Milan reporting system for salivary gland cytopathology. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/salivaryglandsmilandiagnostic.html. Accessed April 25th, 2024.
Definition / general
- The Milan System for Reporting Salivary Gland Cytopathology (MSRSGC) was developed by an international consortium of experts and endorsed by the American Society of Cytopathology (ASC) and the International Academy of Cytology (IAC)
- The effort started in September 2015 in Milan and the atlas was published in 2018
- Aims to standardize reporting terminology in order to replace the conventional, descriptive interpretation for salivary gland fine needle aspirations (FNA) for better communication between clinicians and between institutions
- Main outputs useful for clinical decisions and lab quality control are risk of malignancy (ROM) and frequency of each diagnostic category
Essential features
- Consists of 6 diagnostic categories:
- Nondiagnostic
- Nonneoplastic
- Atypia of undetermined significance (AUS)
- Neoplasm (benign and salivary gland neoplasm of uncertain malignant potential [SUMP])
- Suspicious for malignancy (SM)
- Malignant
Nondiagnostic (category I)
- 10 - 20% of salivary gland FNA (Cancer Cytopathol 2020;128:348)
- Diagnostic criteria:
- Insufficient cellular material: less than 60 lesional cells for a cytologic diagnosis
- Nonneoplastic acinar cells only in the setting of a clinically defined nodule
- Nonmucinous cyst fluid only
- Poorly prepared slides with artifacts (ex: air drying, obscuring blood, poor staining, etc.)
- Exceptions which should be diagnosed as atypia of undetermined significance (AUS):
- Presence of any amount of cells with significant cytologic atypia
- Mucinous cyst lesions with an absent or a very limited epithelial component
- Estimated risk of malignancy: 25%
- Real world risk of malignancy:
- With surgical follow up only: 16.3% (12.6 - 19.9%) (Diagn Cytopathol 2020;48:880)
- Overall: 4.4% (Am J Clin Pathol 2019;151:613)
- Management: clinical and radiologic correlation, repeat FNA
Nonneoplastic (category II)
- 15 - 25% of salivary gland FNA (Cancer Cytopathol 2020;128:348)
- Diagnostic criteria:
- Benign nonneoplastic conditions (ex: sialadenitis, sialolithiasis, granulomatous inflammation, infection, reactive lymph node, etc.)
- Common false negative conditions:
- Lymphoid rich tumors: low grade lymphoma, Hodgkin lymphoma, lymphoepithelial carcinoma
- Cystic tumors: mucoepidermoid carcinoma
- Exceptions which should be diagnosed as atypia of undetermined significance (AUS):
- Bland lymphocytic aspirates showing any evidence of monomorphic population; also consider flow cytometry
- Estimated risk of malignancy: 10%
- Real world risk of malignancy:
- With surgical follow up only: 9.6% (6.8 - 12.4%) (Diagn Cytopathol 2020;48:880)
- Overall: 2.1% (Am J Clin Pathol 2019;151:613)
- Management: clinical follow up and radiologic correlation
Atypia of undetermined significance (AUS) (category III)
- < 10% of salivary gland FNA (Cancer Cytopathol 2020;128:348)
- Diagnostic criteria:
- Limited cellular atypia
- Lacks qualitative or quantitative features for diagnosing a neoplasm
- Common AUS conditions:
- Reactive or reparative atypia
- Metaplastic changes indefinite for a neoplasm (ex: squamous, oncocytic, etc.)
- Mucinous cystic lesions with an absent or a very limited epithelial component
- Nonmucinous cystic lesions with atypical epithelial cells
- Low cellularity FNA suggestive but not diagnostic of a neoplasm
- Lymphoid lesions indefinite for lymphoproliferative disorder
- Estimated risk of malignancy: 20%
- Real world risk of malignancy:
- With surgical follow up only: 36.9% (25.6 - 48.2%) (Diagn Cytopathol 2020;48:880)
- Overall: 25.0% (Am J Clin Pathol 2019;151:613)
- Management: repeat FNA or surgery
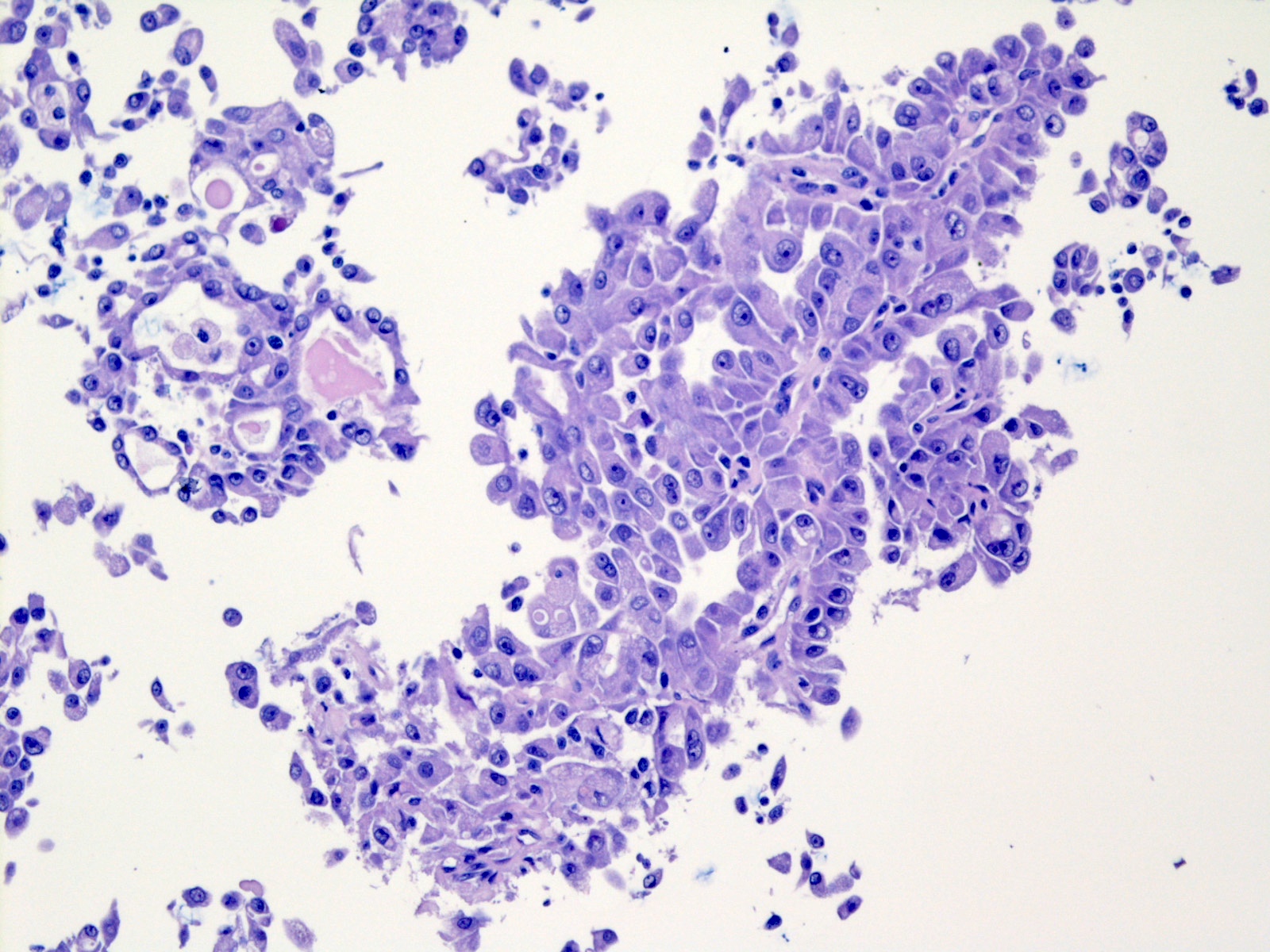
Neoplasm: benign (category IVA)
- 30 - 40% of salivary gland FNA (Cancer Cytopathol 2020;128:348)
- Diagnostic criteria:
- Characteristic cytomorphologic features of a specific benign neoplasm
- Common benign tumors diagnosed:
- Epithelial: pleomorphic adenoma (60 - 70%), Warthin tumor (20 - 30%), oncocytoma, etc.
- Mesenchymal: schwannoma, lipoma, hemangioma, etc.
- Conditions better classified as salivary gland neoplasm of uncertain malignant potential (SUMP):
- Matrix producing carcinomas with basaloid cells falsely interpreted as pleomorphic or basal cell adenoma (ex: adenoid cystic carcinoma, basal cell adenocarcinoma → SUMP with basaloid features)
- Carcinomas with oncocytic / oncocytoid cells or prominent lymphocytic infiltrates falsely interpreted as Warthin tumor or oncocytoma (ex: Warthin-like variant of mucoepidermoid carcinoma, mucoepidermoid carcinoma with lymphoid cuffing, acinic cell carcinoma with / without lymphoid infiltrates, secretory carcinoma → SUMP with oncocytic / oncocytoid features)
- Carcinomas with bland myoepithelial-like morphology falsely interpreted as pleomorphic adenoma or myoepithelioma (ex: myoepithelial carcinoma, epithelial myoepithelial carcinoma, secretory carcinoma → SUMP, not otherwise specified, with myoepithelial features)
- Basal cell adenoma, myoepithelioma and cystadenoma due to overlapping cytomorphology with other malignant tumors
- Estimated risk of malignancy: < 5%
- Real world risk of malignancy:
- With surgical follow up only: 2.4% (1.8 - 3.0%) (Diagn Cytopathol 2020;48:880)
- Overall: 1.5% (Am J Clin Pathol 2019;151:613)
- Management: surgery or clinical and radiological follow up
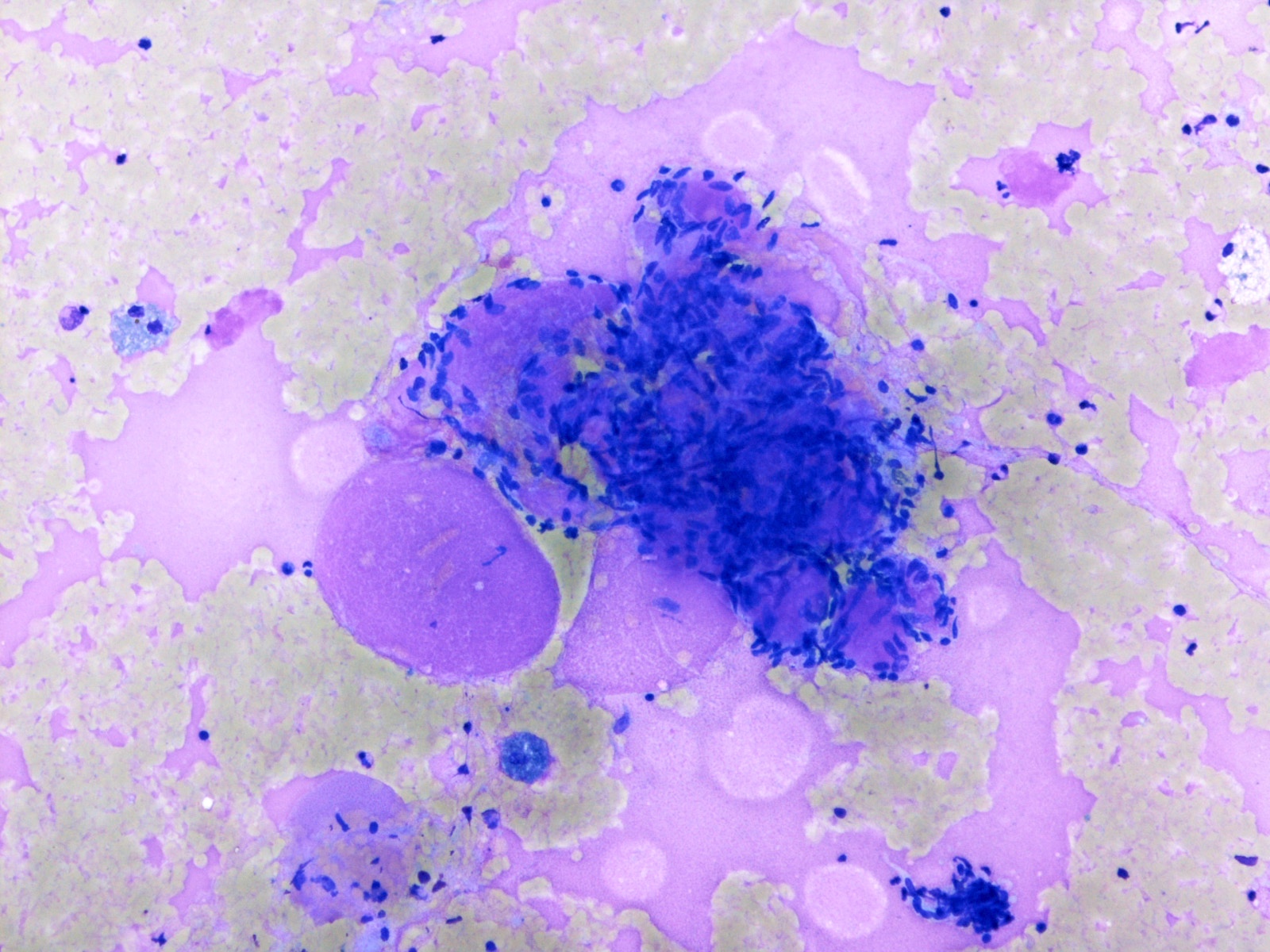
Neoplasm: salivary gland neoplasm of uncertain malignant potential (SUMP) (category IVB)
- < 10% of salivary gland FNA (Cancer Cytopathol 2020;128:348)
- Diagnostic criteria:
- Cytomorphologic features diagnostic of a neoplasm but indefinite for a specific tumor type to further distinguish between benign or malignant
- Common SUMP conditions:
- Cellular benign neoplasm (ex: cellular pleomorphic adenoma)
- Neoplasm with atypical features
- Cellular neoplasm with basaloid features (ex: pleomorphic adenoma, basal cell adenoma / adenocarcinoma, adenoid cystic carcinoma, epithelial myoepithelial carcinoma, polymorphous adenocarcinoma, etc.)
- Cellular neoplasm with oncocytic / oncocytoid features (ex: Warthin tumor, oncocytoma, mucoepidermoid carcinoma, acinic cell carcinoma, secretory carcinoma, etc.)
- Cellular neoplasm with clear cell features (ex: myoepithelioma, epithelial myoepithelial carcinoma, acinic cell carcinoma, secretory carcinoma, mucoepidermoid carcinoma, etc.)
- Low grade carcinoma (ex: low grade mucoepidermoid carcinoma)
- SUMP subclassifications proposed by different authors:
- Cellular basaloid neoplasm, cellular oncocytic / oncocytoid neoplasm, cellular neoplasm with clear cell features (Faquin: The Milan System for Reporting Salivary Gland Cytopathology, 1st Edition, 2018)
- Basaloid neoplasm (risk of malignancy: 27.6%), salivary gland neoplasm with predominant oncocytic cells (risk of malignancy: 20.0%) (Cancer Cytopathol 2018;126:490)
- Oncocytic / squamoid subtype (risk of malignancy: 61.1%), basaloid subtype (risk of malignancy: 40.0%) and myoepithelial subtype (risk of malignancy: 18.8%) (Cancer Cytopathol 2018;126:924)
- Basaloid features (risk of malignancy: 38.5%), oncocytic features (risk of malignancy: 7.7%), unspecified features (risk of malignancy: 41%) (Cancer Cytopathol 2019;127:377)
- Monomorphic basaloid SUMP (risk of malignancy: 23.5%), monomorphic oncocytic SUMP (risk of malignancy: 58.8%) (Cancer Cytopathol 2021 Mar 31 [Epub ahead of print])
- Estimated risk of malignancy: 35%
- Real world risk of malignancy:
- With surgical follow up only: 37.2% (30.5 - 44.0%) (Diagn Cytopathol 2020;48:880)
- Overall: 27.7% (Am J Clin Pathol 2019;151:613)
- Management: surgery
Suspicious for malignancy (SM) (category V)
- < 5% of salivary gland FNA (Cancer Cytopathol 2020;128:348)
- Diagnostic criteria:
- Features that are highly suggestive of but not unequivocal for malignancy
- Common SM conditions:
- Markedly atypical cells with poor preparation or obscuring factors
- Limited cytologic features of a specific malignancy (ex: adenoid cystic carcinoma with limited cellular atypia or hyaline globules, mucoepidermoid carcinoma with limited mucus cells or extracellular mucin, secretory carcinoma with limited cytoplasmic vacuolization or papillary formations)
- Suspicious cytologic features in a subset of cells but admixed with predominant features of a benign lesion (ex: carcinoma ex pleomorphic adenoma)
- Monomorphic population of small lymphocytes suspicious for a low grade lymphoma
- Scant large atypical lymphocytes suspicious for a high grade lymphoma or Hodgkin lymphoma
- Estimated risk of malignancy: 60%
- Real world risk of malignancy: 80.6% (70.6 - 85.7%) (Diagn Cytopathol 2020;48:880)
- Management: surgery
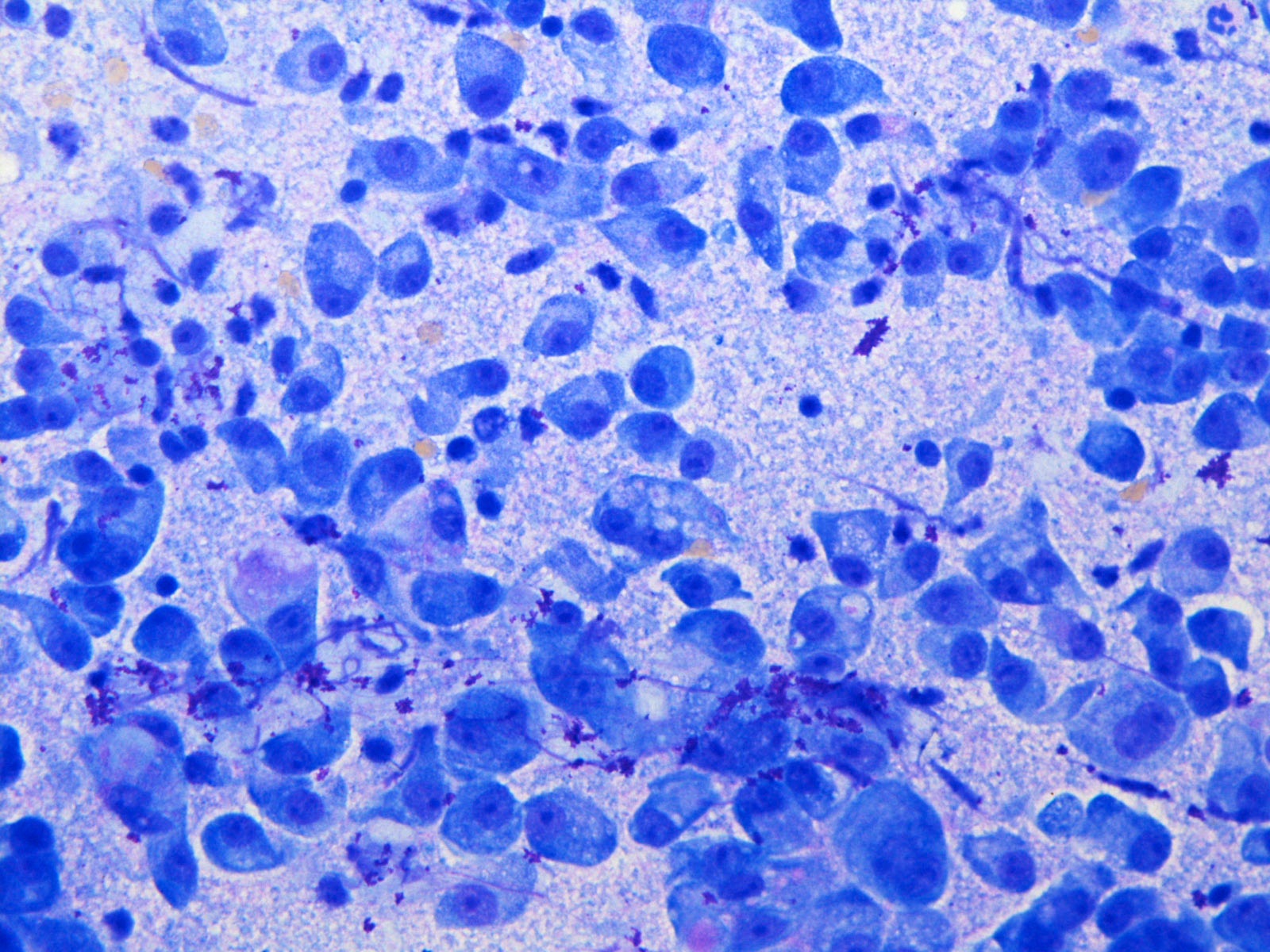
Malignant (category VI)
- 10 - 15% of salivary gland FNA (Cancer Cytopathol 2020;128:348)
- Diagnostic criteria:
- FNA showing diagnostic features of malignancy
- Common malignant conditions:
- Low grade carcinoma (ex: acinic carcinoma, secretory carcinoma, etc.)
- High grade carcinoma (ex: salivary duct carcinoma, lymphoepithelial carcinoma, tumor with high grade transformation, etc.)
- Carcinoma with intermediate or multiple grades (ex: mucoepidermoid carcinoma, adenoid cystic carcinoma, myoepithelial carcinoma, etc.)
- Other malignancy: lymphoma, sarcoma, metastasis, etc.
- Common false positive conditions:
- Pleomorphic or basal cell adenoma with prominent hyaline globules falsely interpreted as adenoid cystic carcinoma → better classified as SUMP with basaloid features
- Benign tumor or nonneoplastic lesion with squamous or mucinous metaplasia falsely interpreted as mucoepidermoid carcinoma (ex: pleomorphic adenoma, Warthin tumor, chronic sialadenitis → better classified as AUS or SUMP)
- Diagnostic tip:
- An attempt should be made to subclassify these aspirates into different grades and specific types of carcinoma if possible
- Estimated risk of malignancy: 90%
- Real world risk of malignancy: 97.4% (96.4 - 98.5%) (Diagn Cytopathol 2020;48:880)
- Management: surgery
Cytology description
- See above
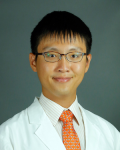
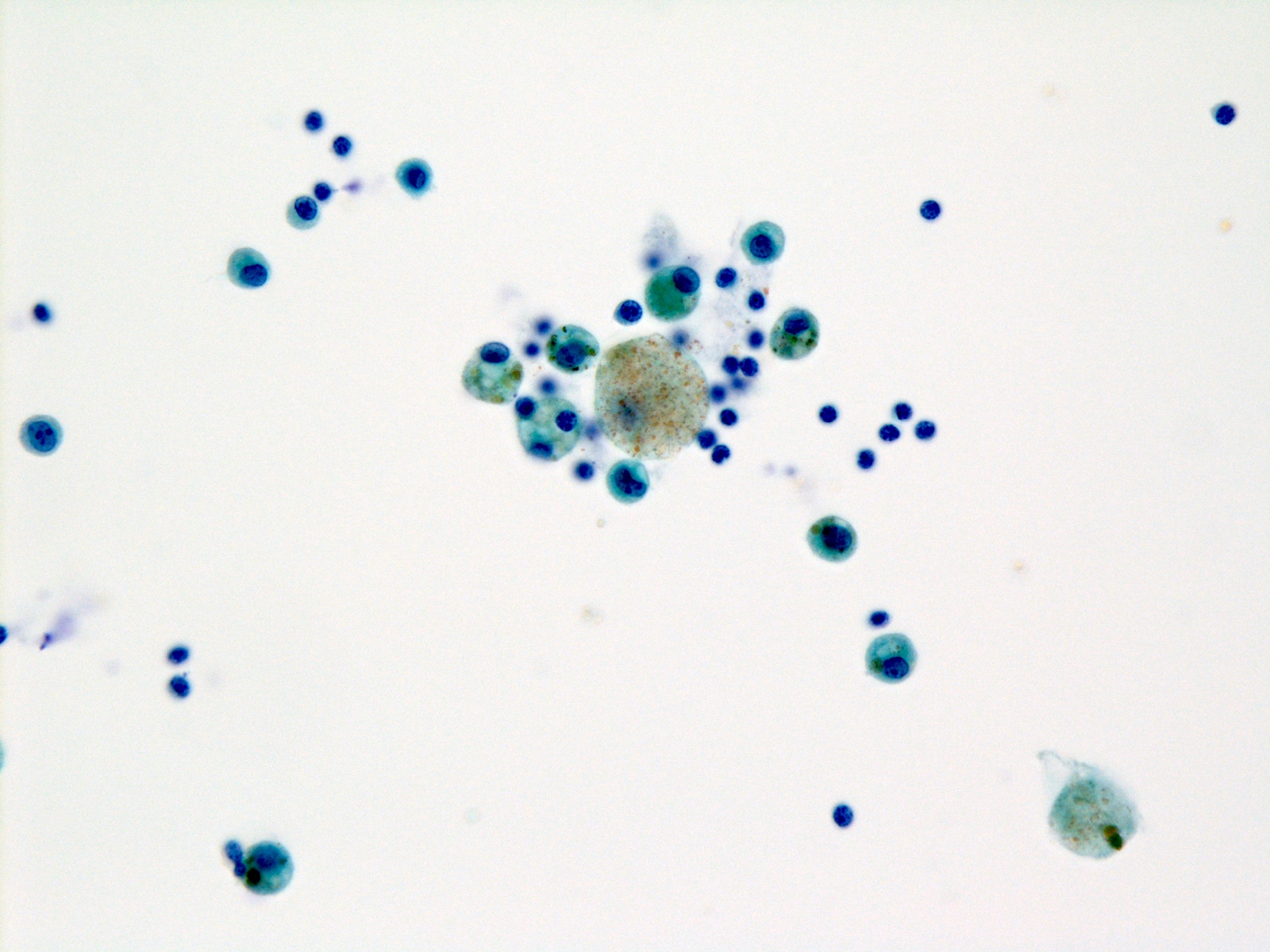
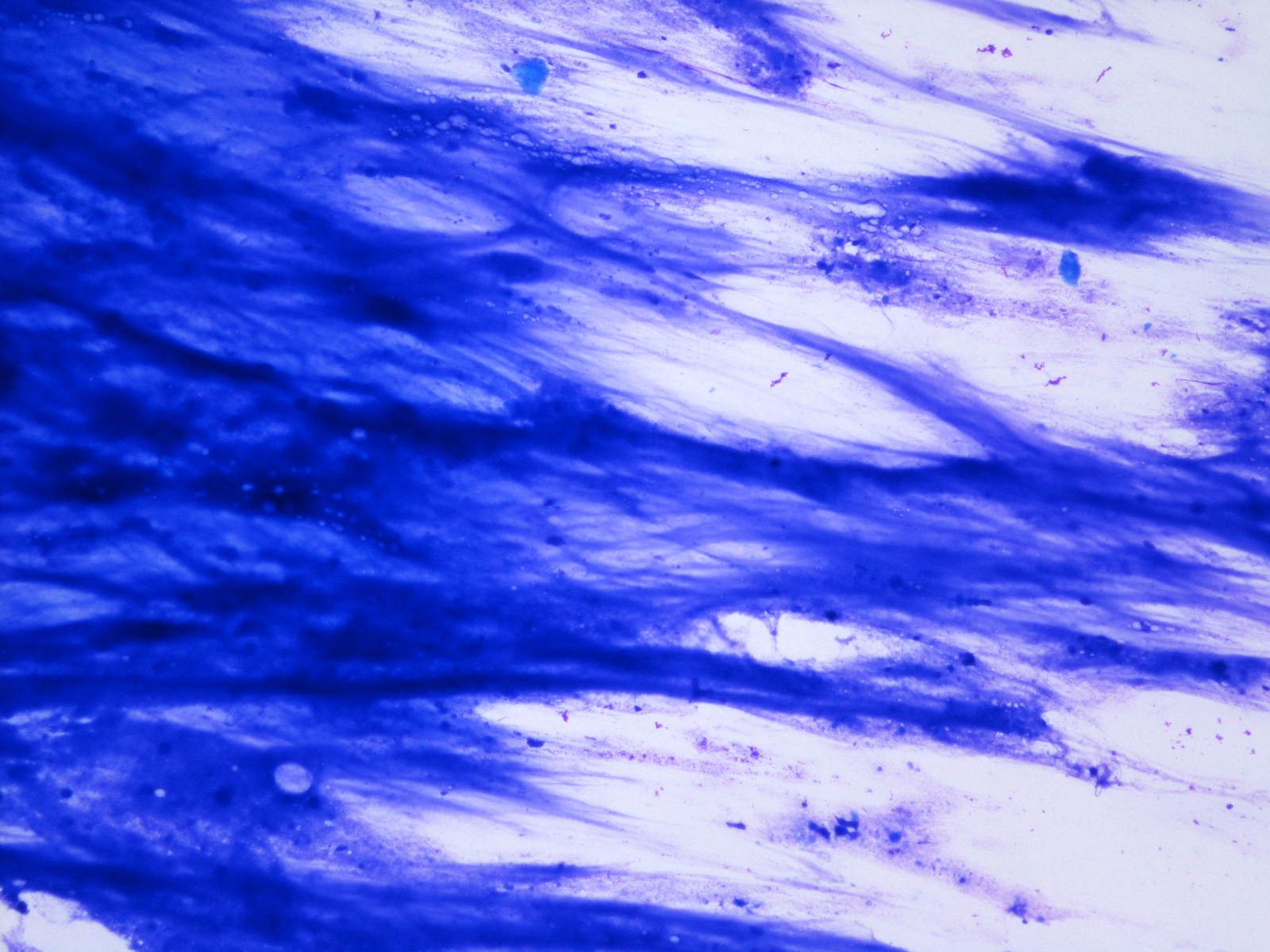
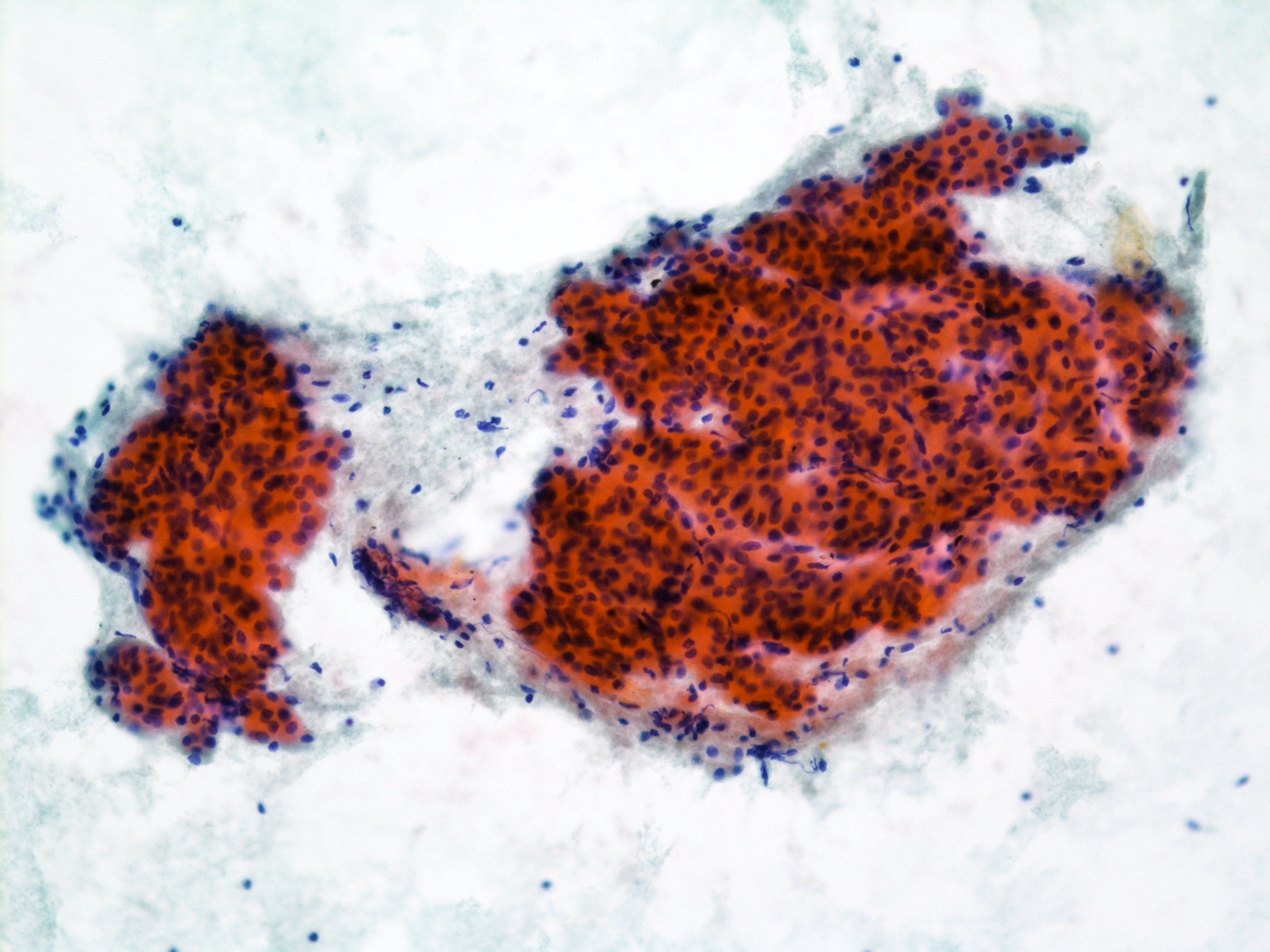
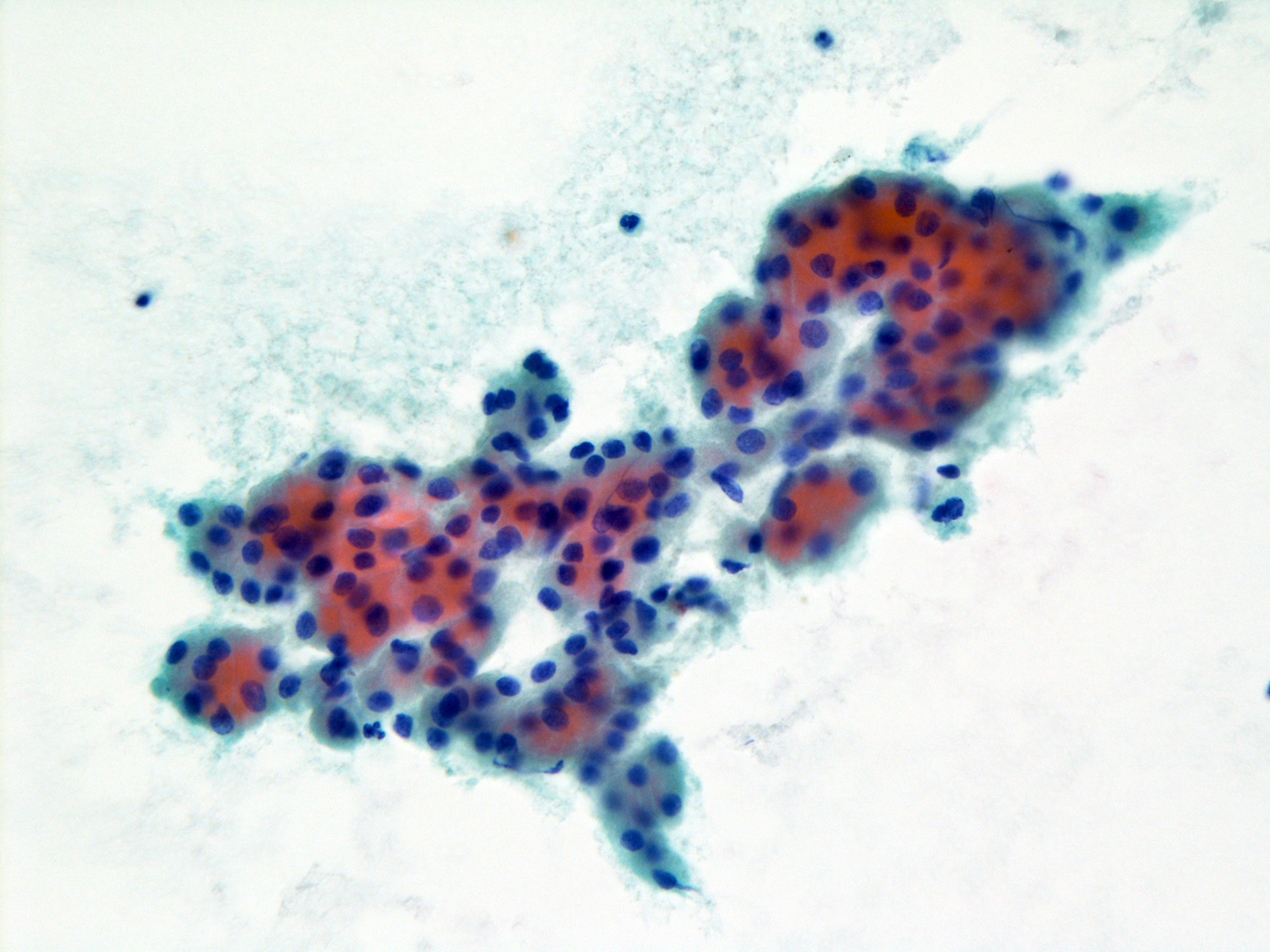
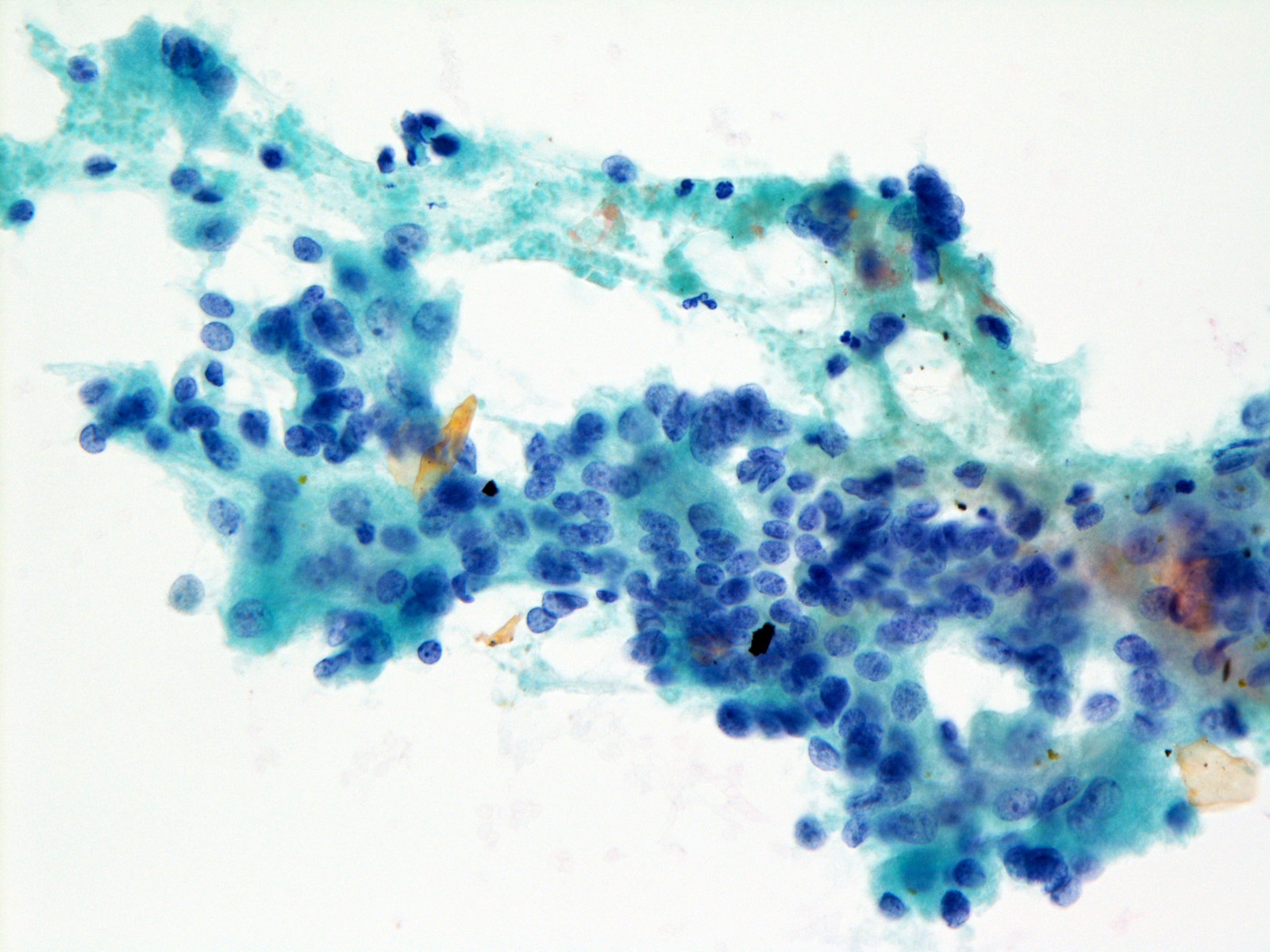
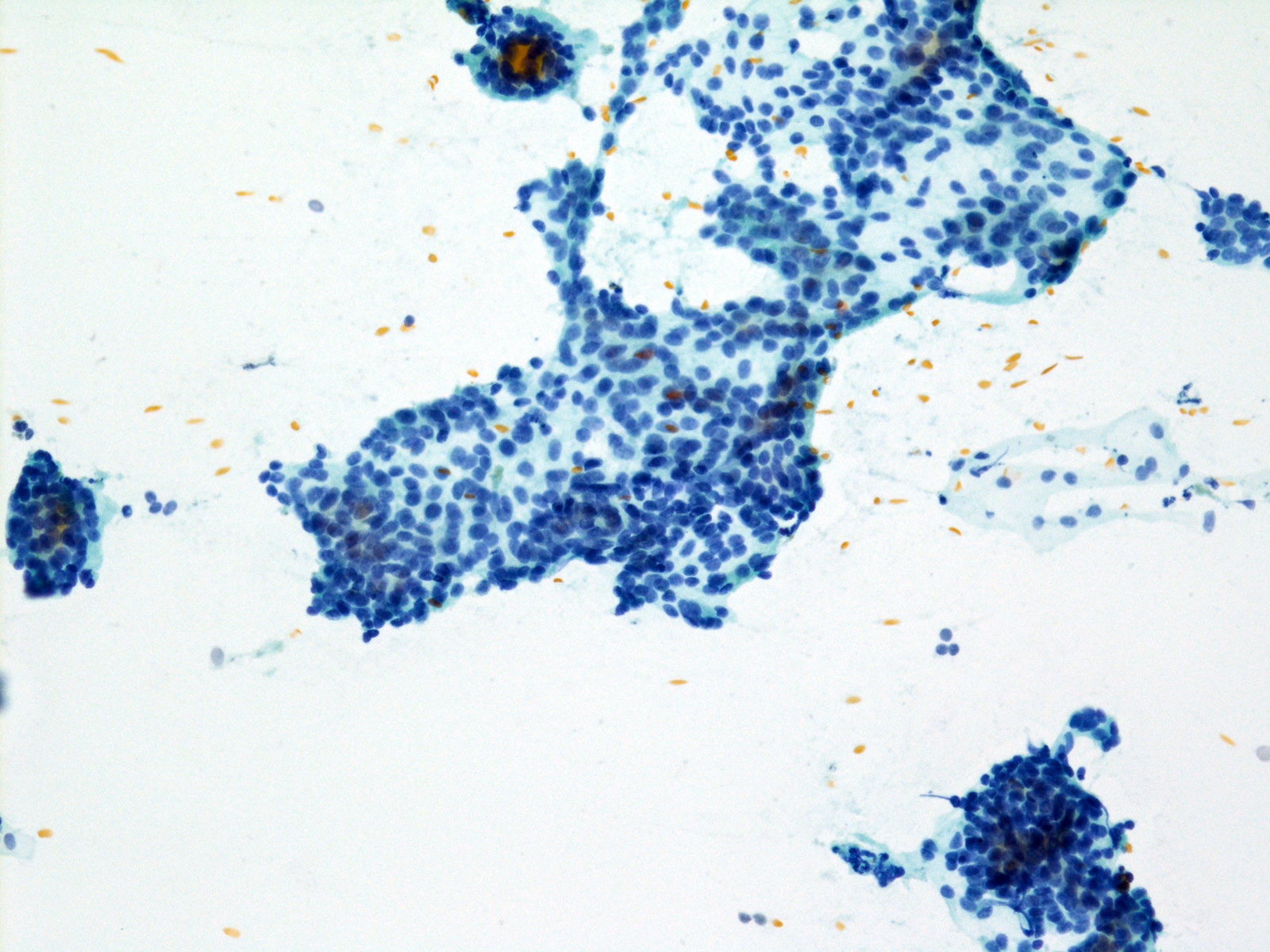
Cytology images
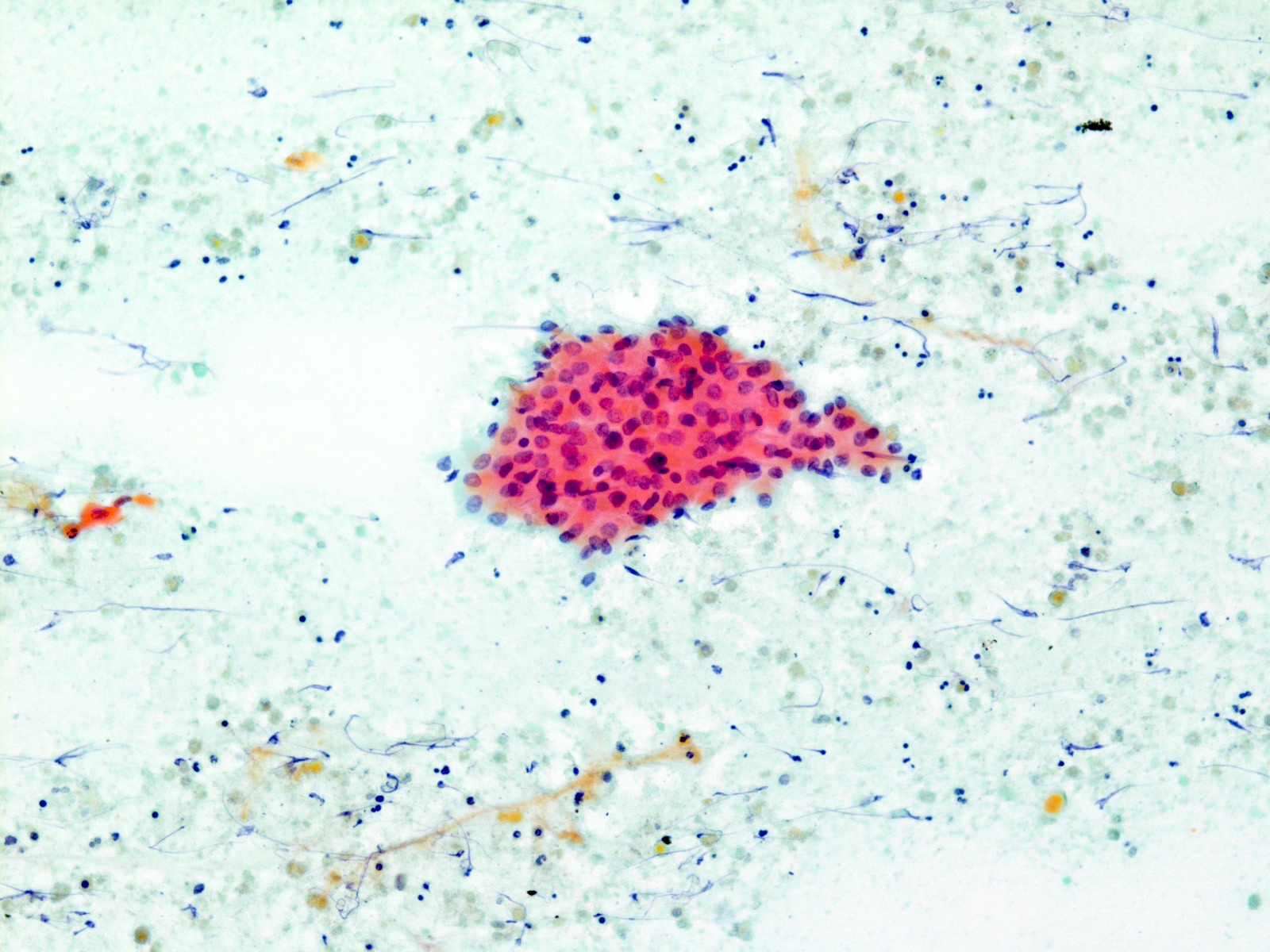
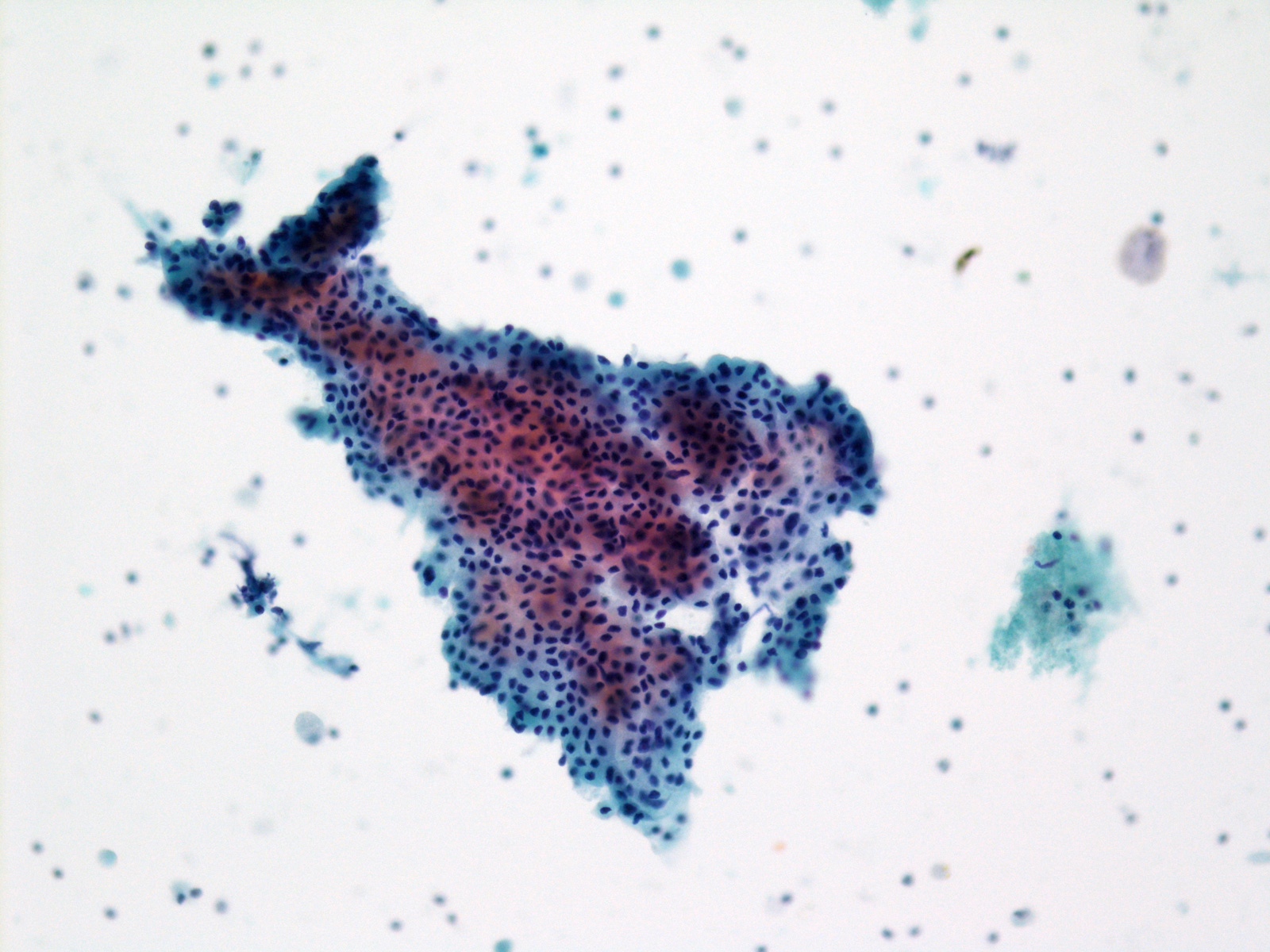
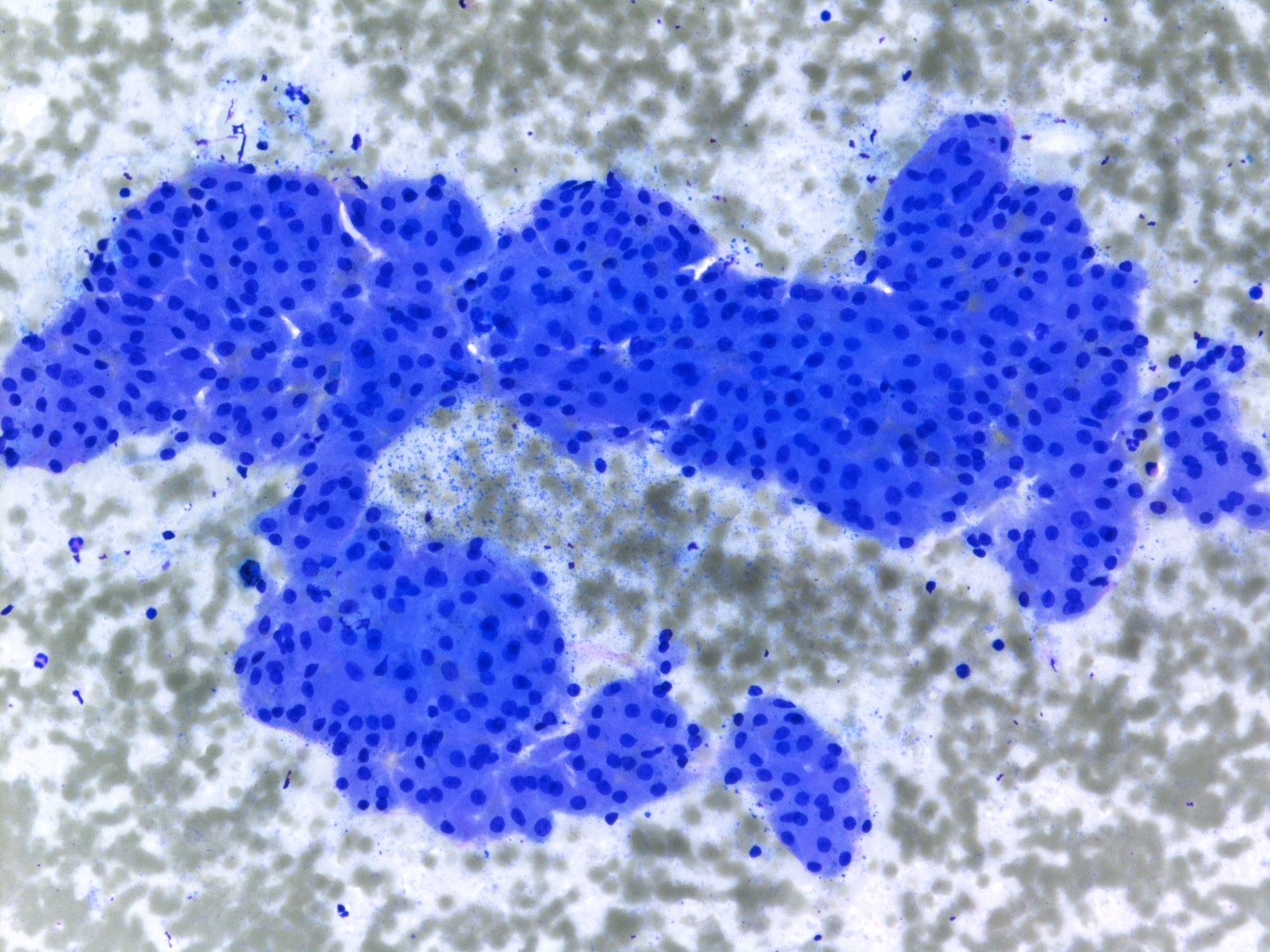
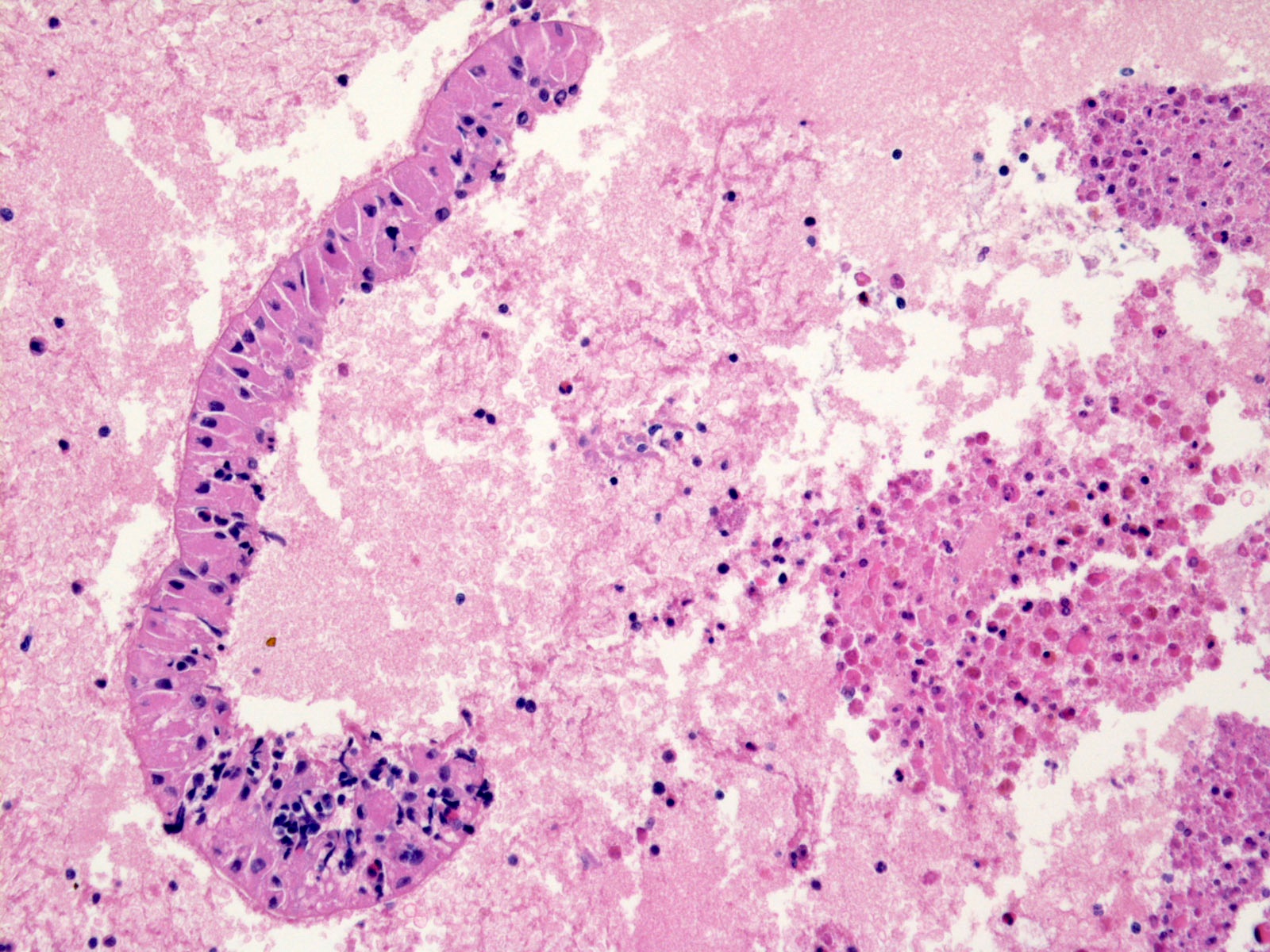
Contributed by Jen-Fan Hang, M.D.
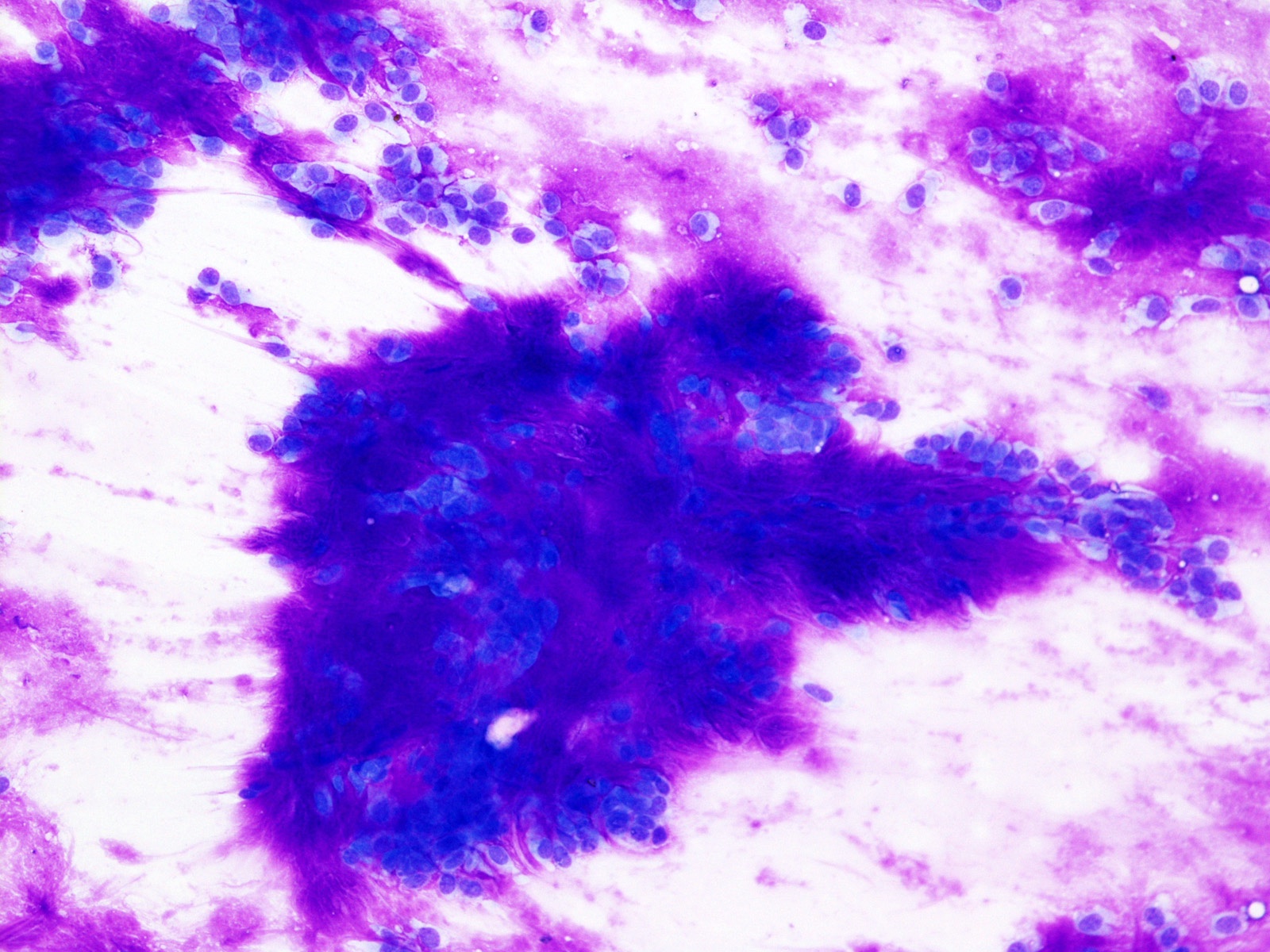
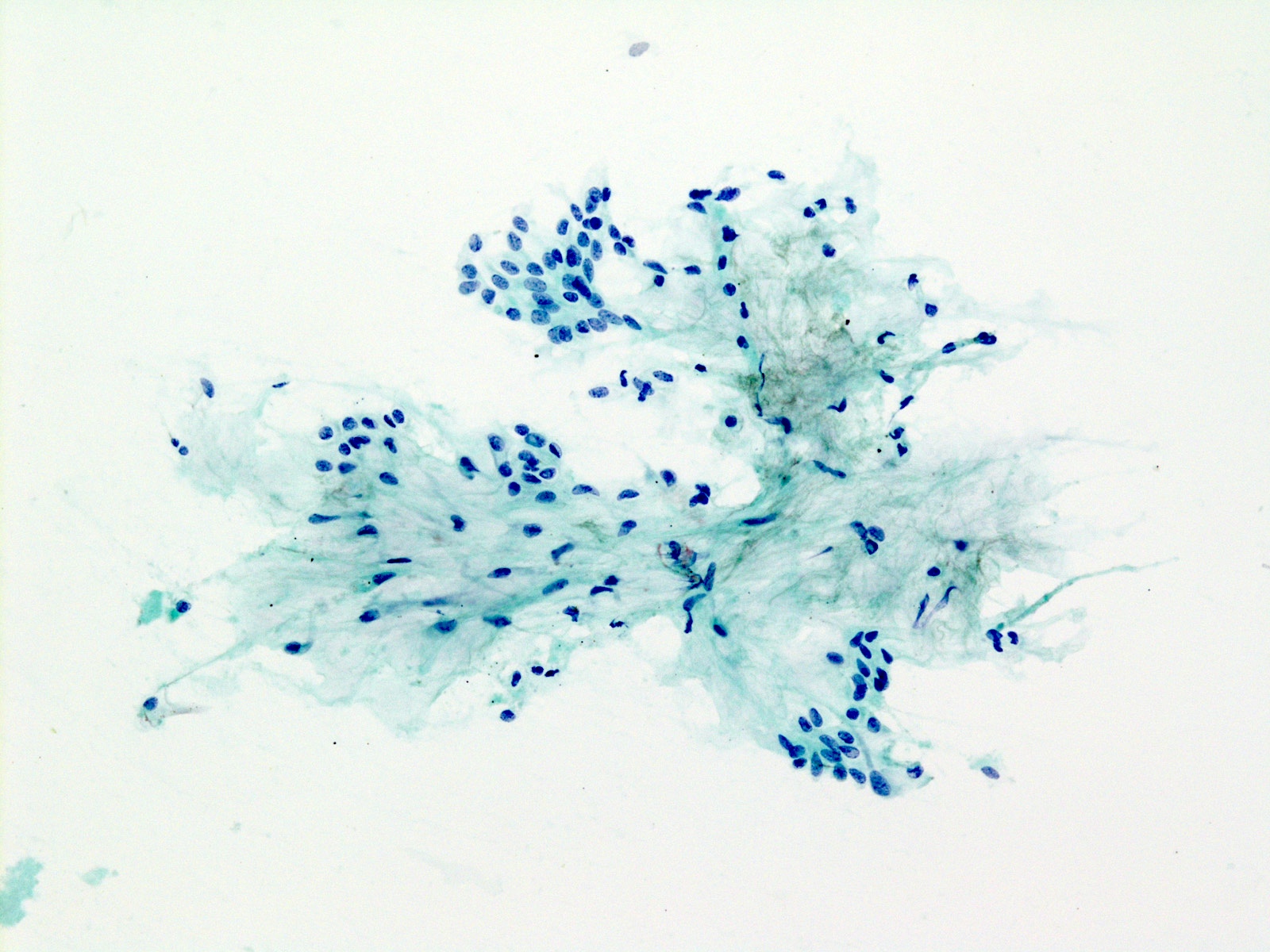
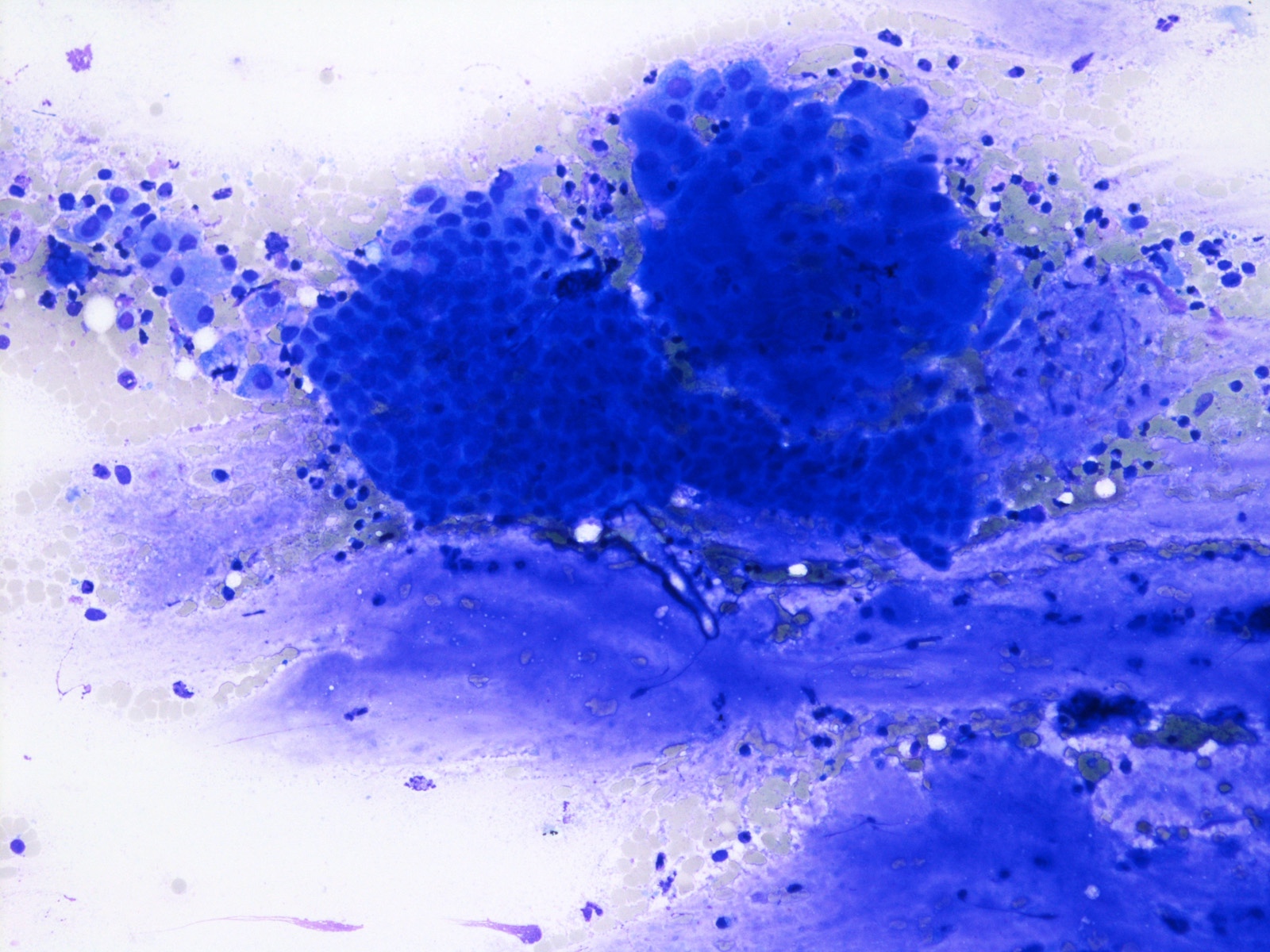
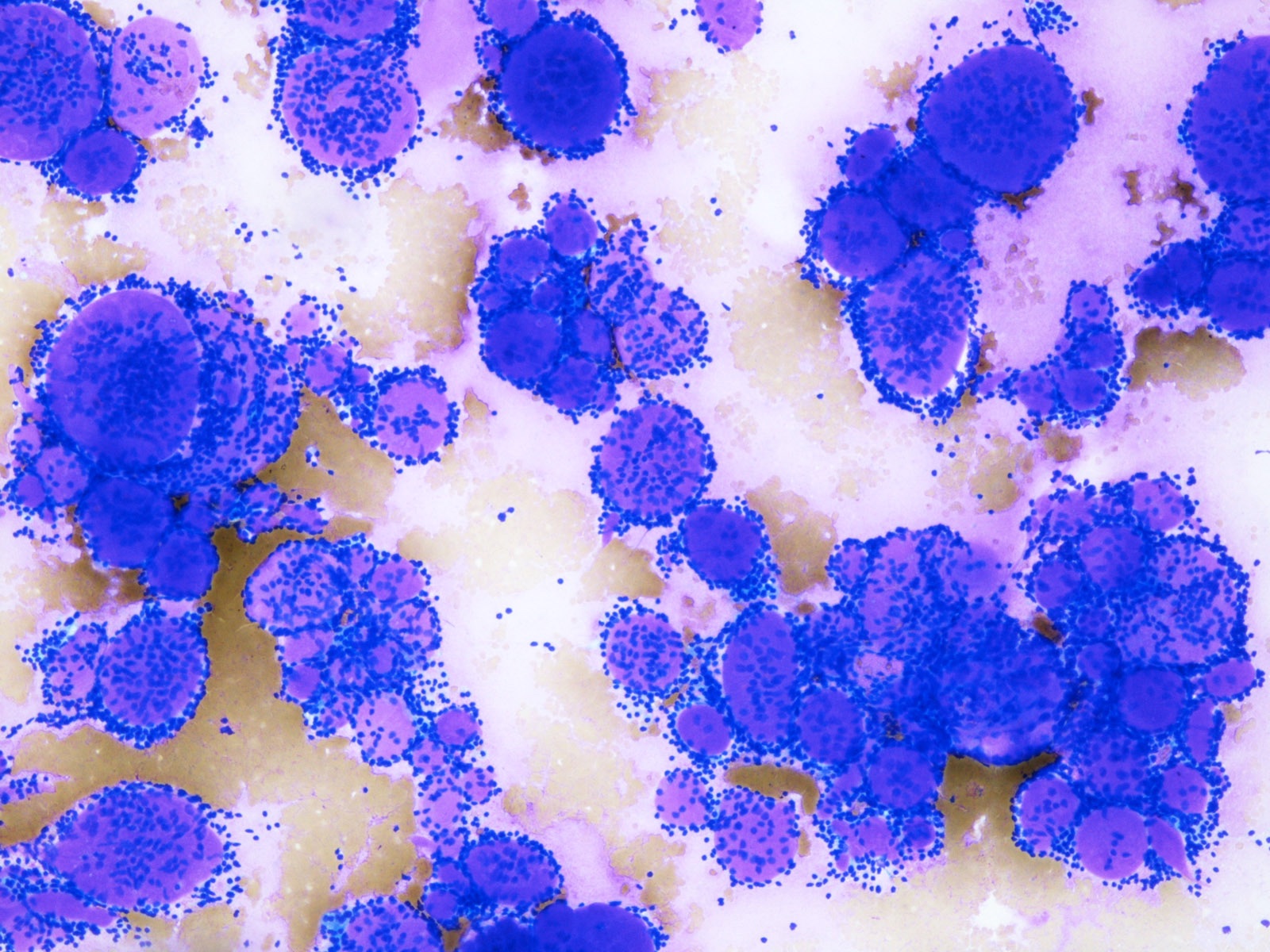
Neoplasm: benign
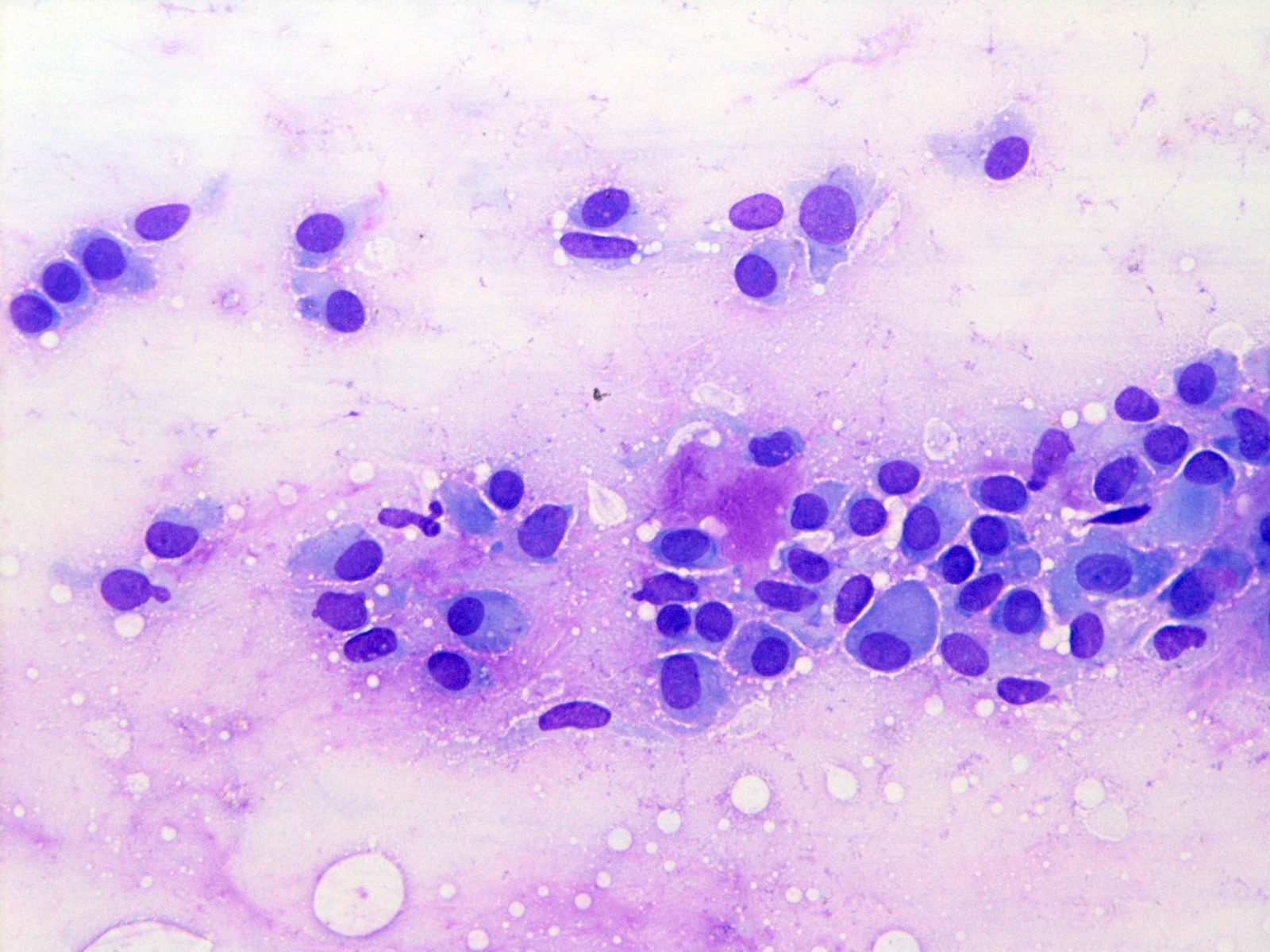
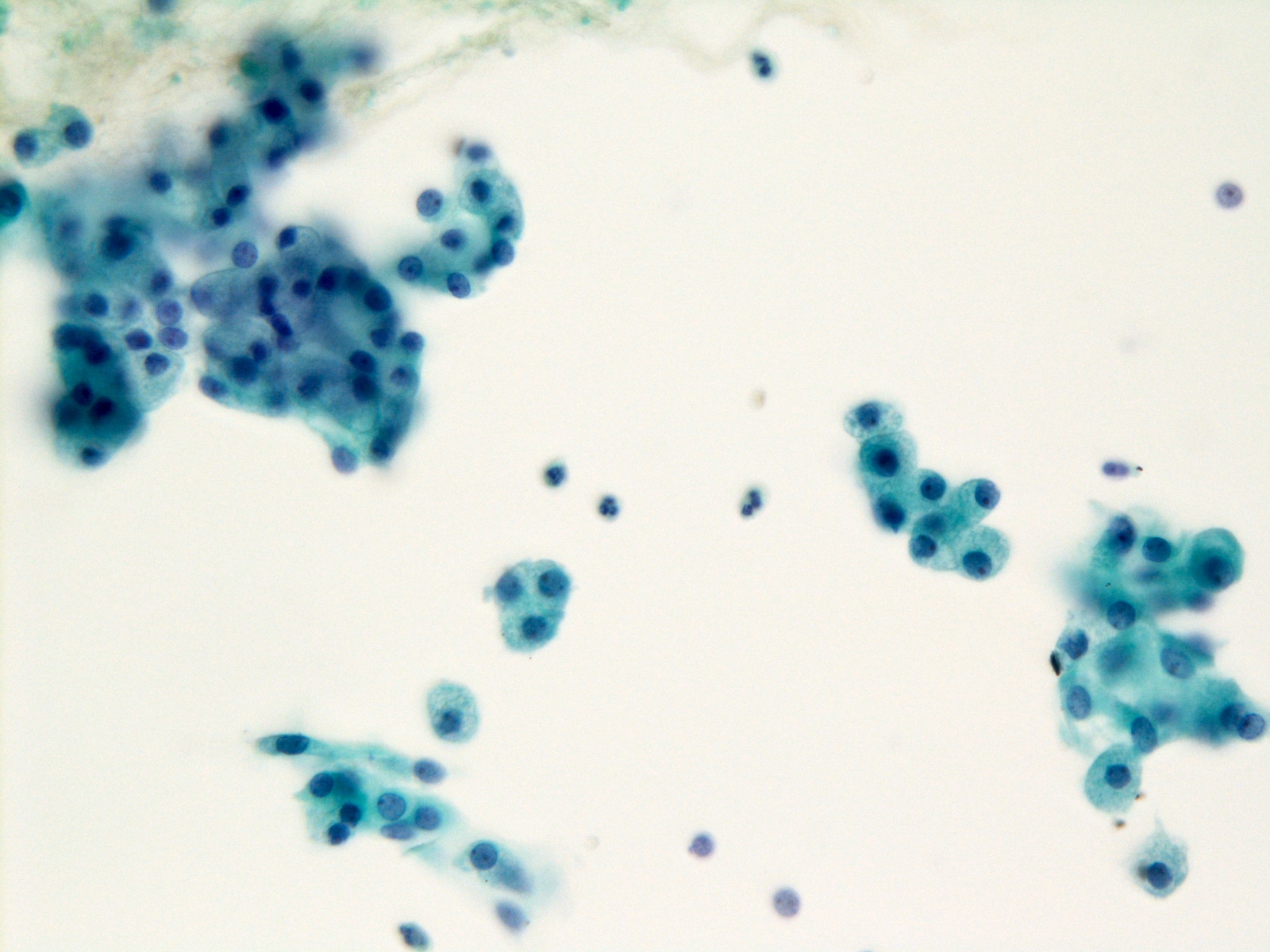
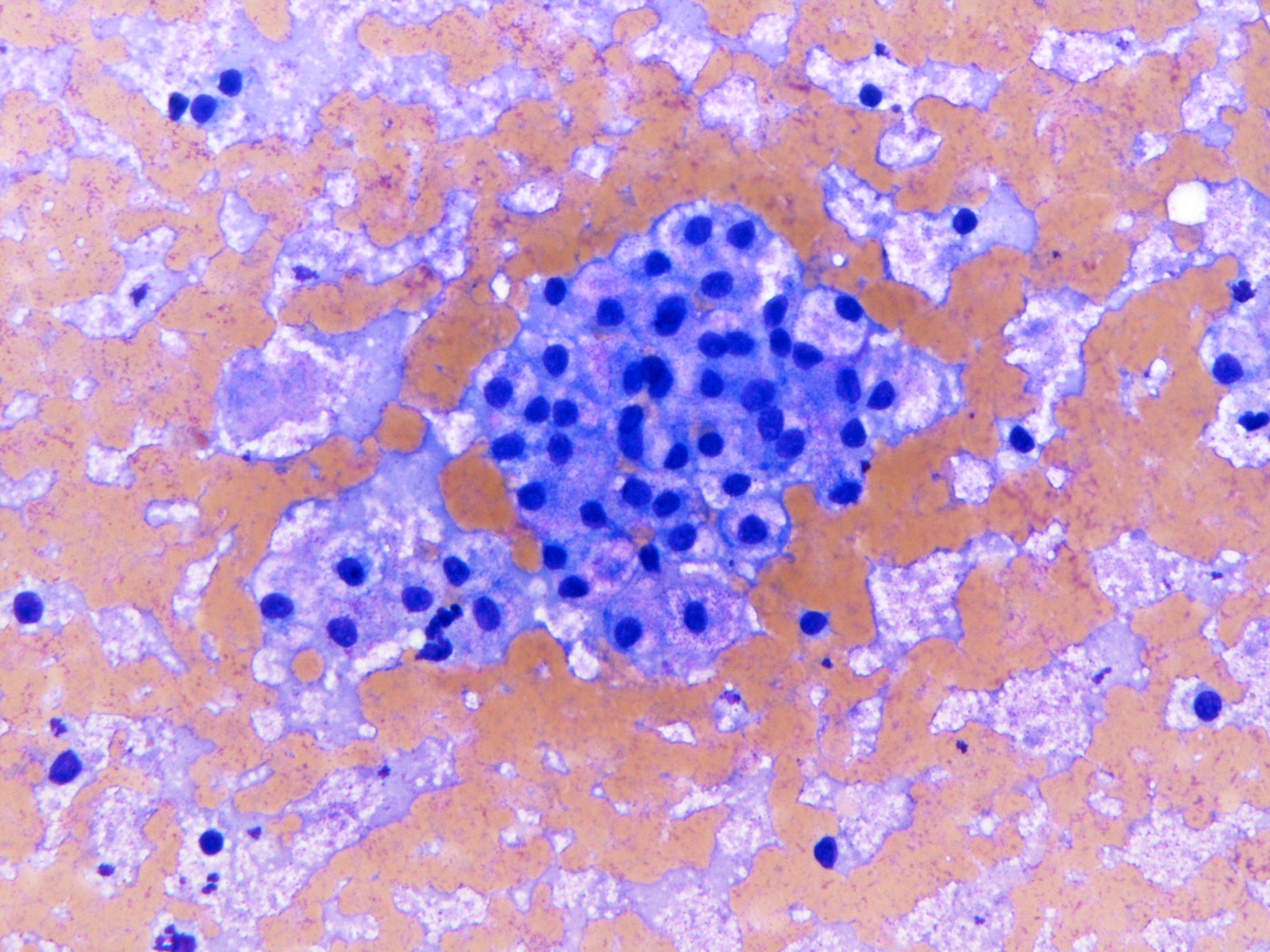
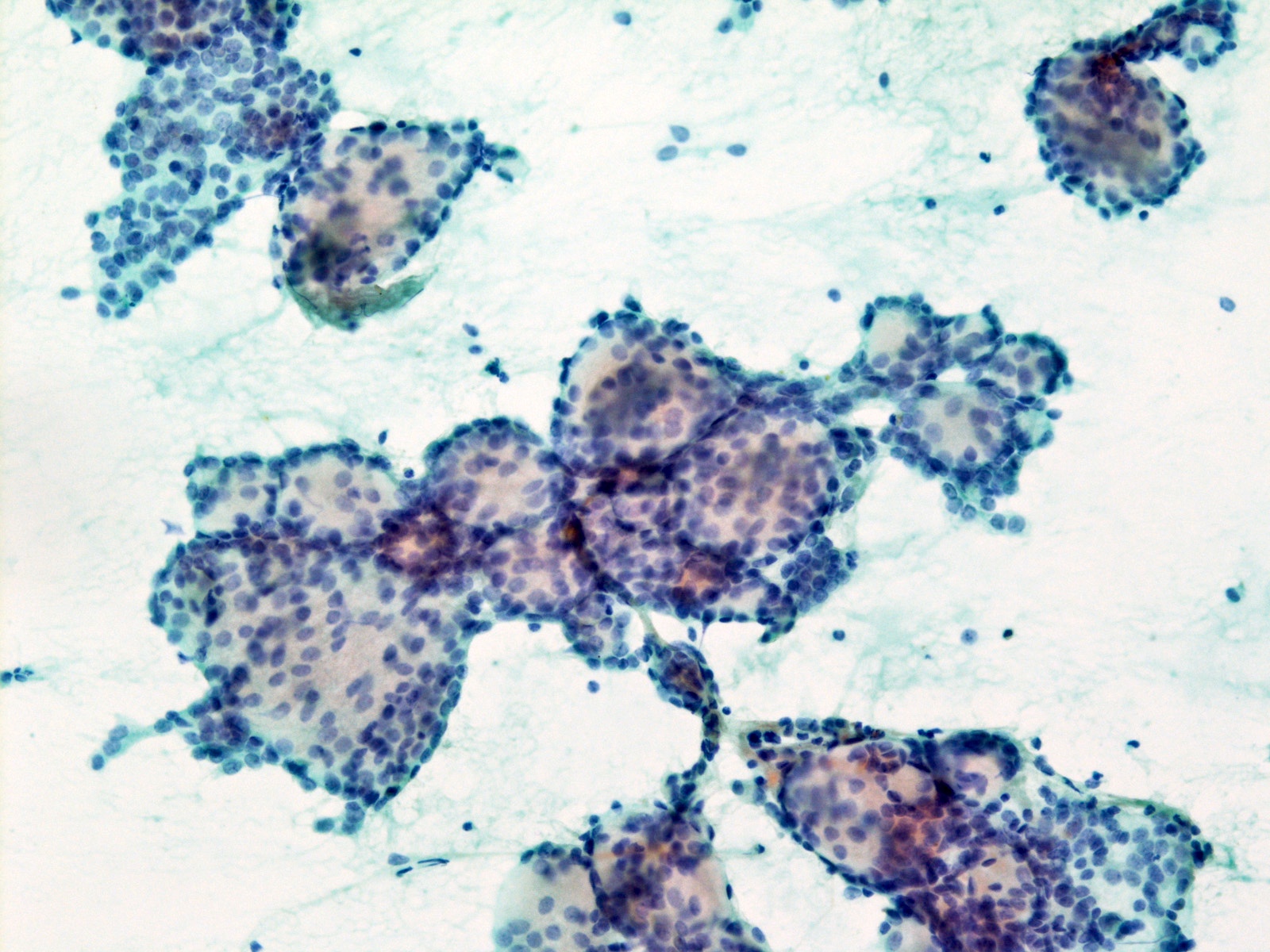
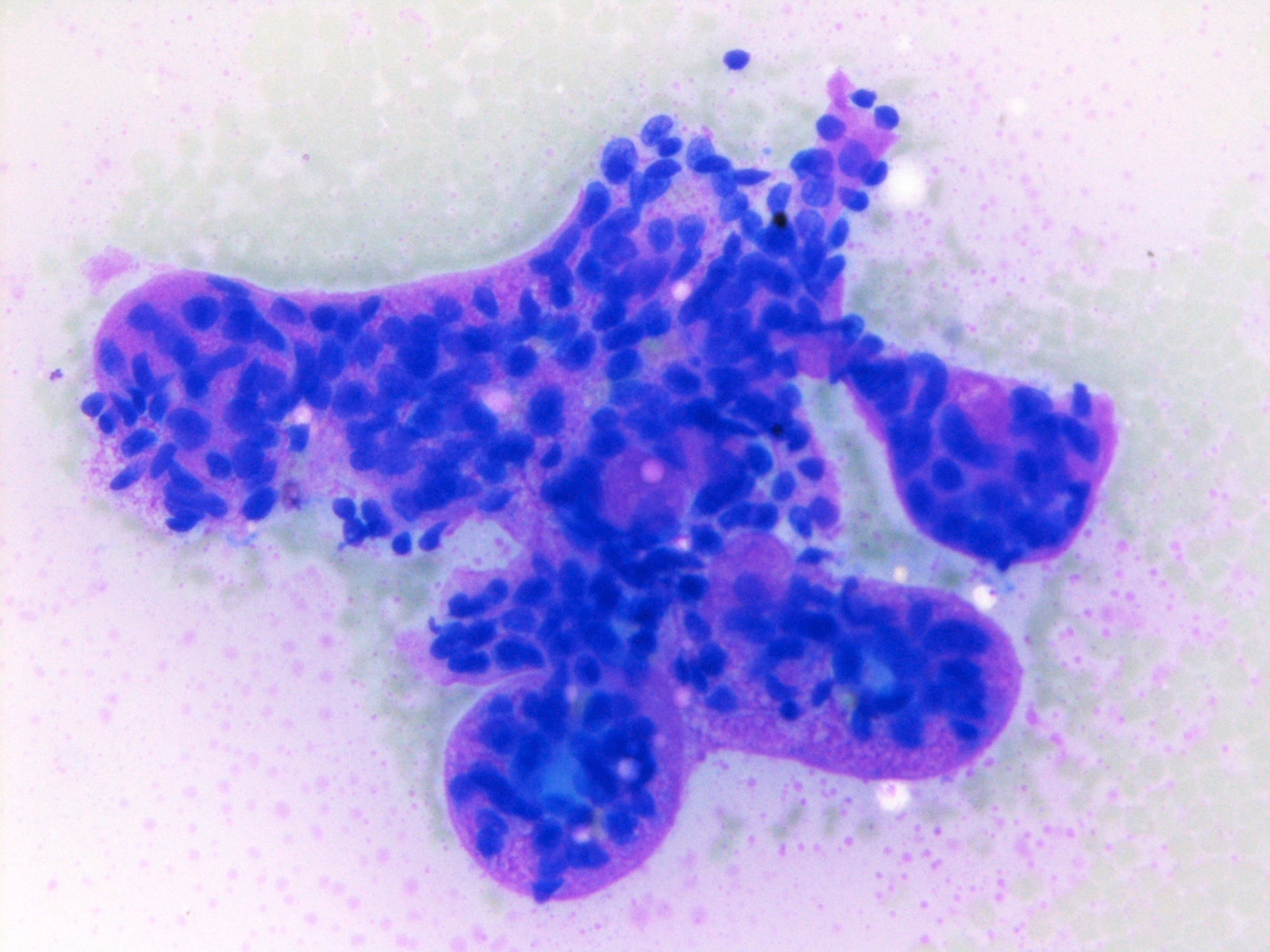
Neoplasm: salivary gland neoplasm of uncertain malignant potential (SUMP)
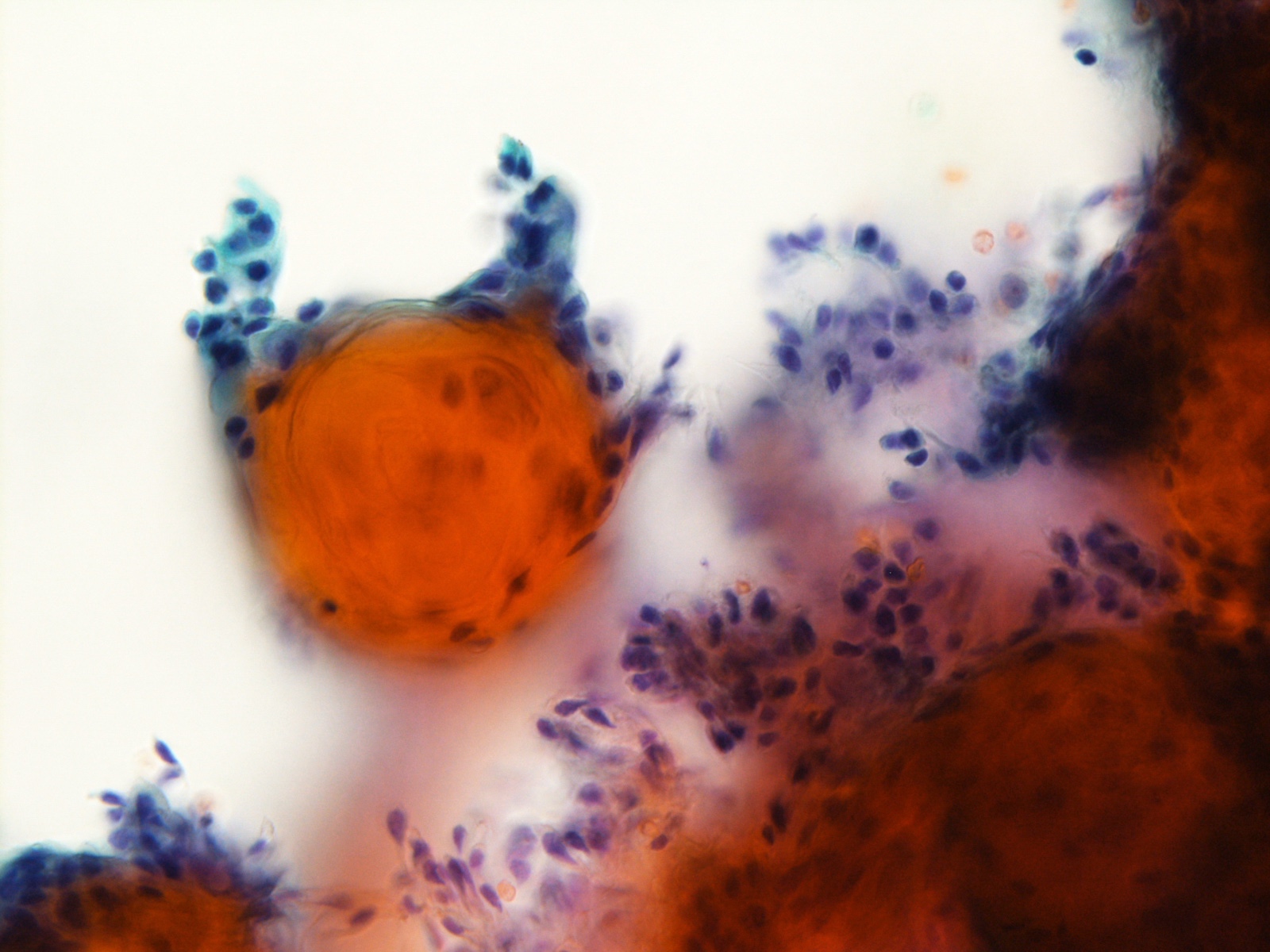
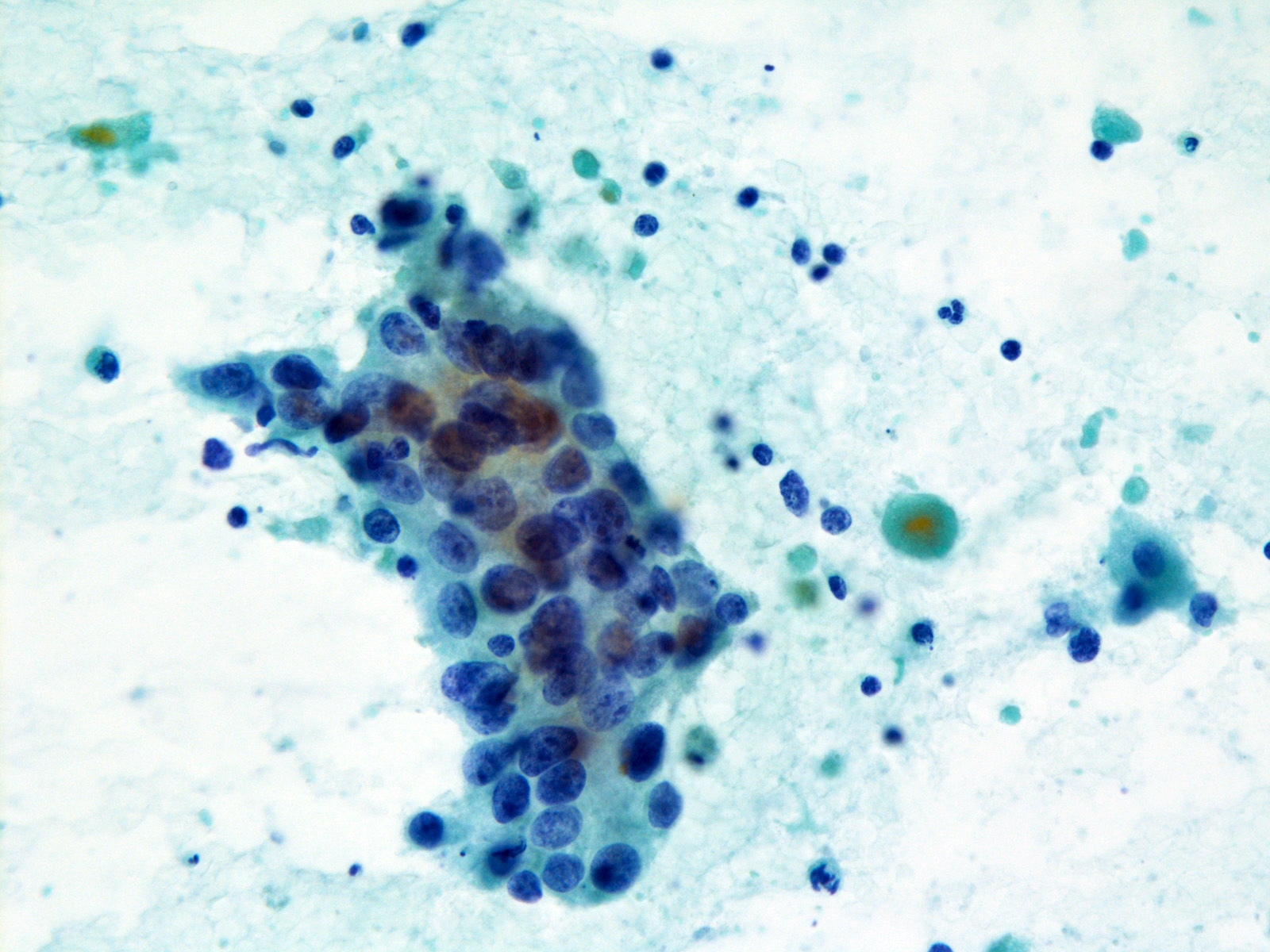
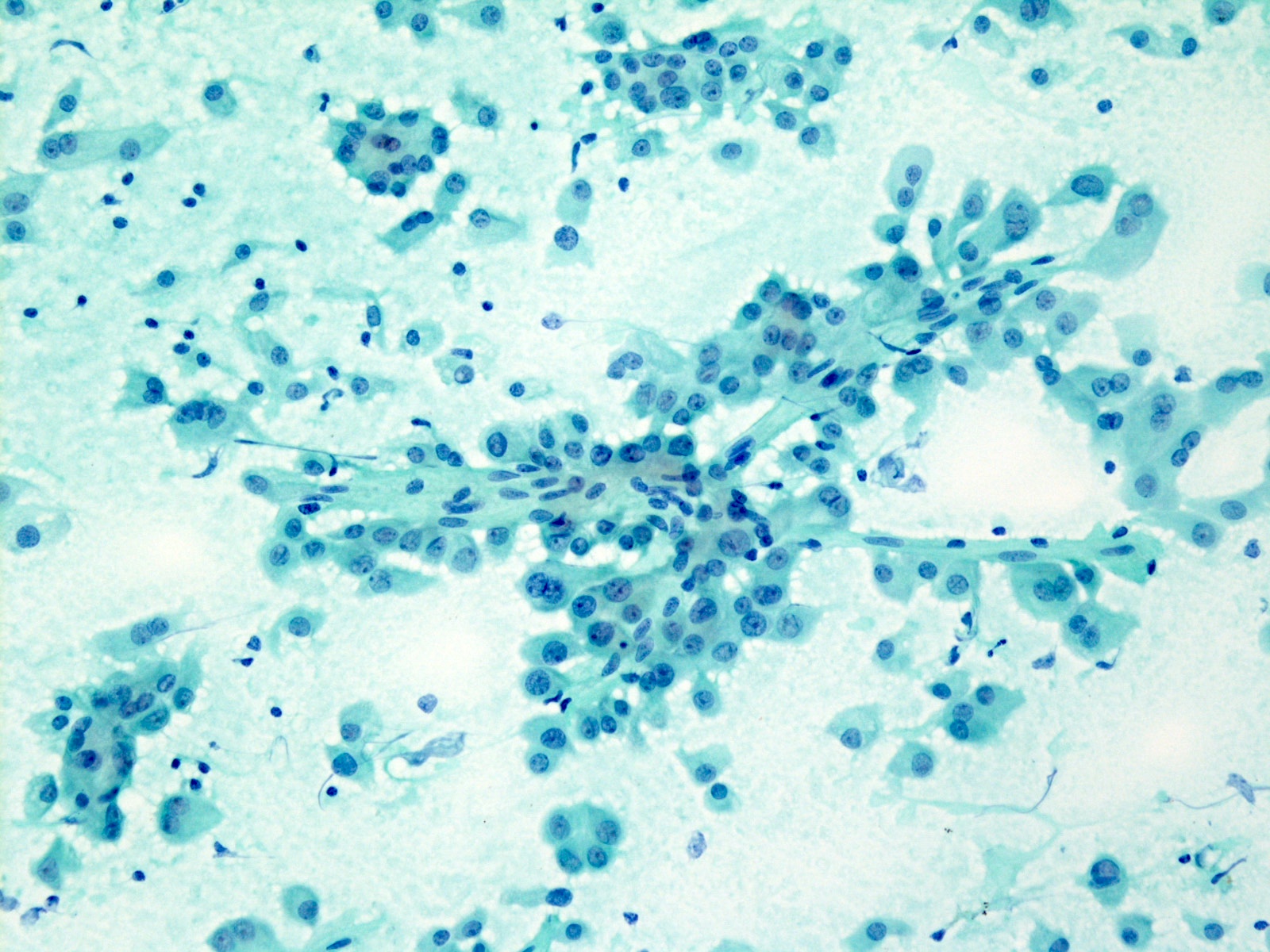
Malignant
Videos
Milan system
Algorithmic approach to everyday salivary gland cytology
Differential diagnosis
- See above
Additional references
Board review style question #1
A 62 year old man presents with a 3.6 cm left parotid nodule. The fine needle aspiration shows a cellular smear, which is composed of fragments of bland looking, basaloid cells intermingled with magenta colored hyaline globules. What is the best diagnosis according to the Milan System for Reporting Salivary Gland Cytopathology?
- Category III: atypia of undetermined significance
- Category IVA: benign neoplasm, pleomorphic adenoma
- Category IVB: salivary gland neoplasm of uncertain malignant potential, with basaloid features
- Category VI: malignant, adenoid cystic carcinoma
Board review style answer #1
C. Category IVB: salivary gland neoplasm of uncertain malignant potential, with basaloid features
Basaloid neoplasms showing overlapping morphology of bland basal cells and acellular metachromatic matrix are better classified as salivary gland neoplasm of uncertain malignant potential, with basaloid features. The final pathology of the same case showed a basal cell adenoma with prominent hyaline globules.
Comment Here
Reference: Milan system
Basaloid neoplasms showing overlapping morphology of bland basal cells and acellular metachromatic matrix are better classified as salivary gland neoplasm of uncertain malignant potential, with basaloid features. The final pathology of the same case showed a basal cell adenoma with prominent hyaline globules.
Comment Here
Reference: Milan system
Board review style question #2
A 39 year old woman presents with multiple submandibular nodules. A 2.3 cm intrasubmandibular gland nodule undergoes ultrasound guided fine needle aspiration. The cytology shows a proliferation of monotonous small lymphocytes and scattered tingible body macrophages. What is the best diagnosis according to the MSRSGC?
- Category I: nondiagnostic
- Category II: nonneoplastic
- Category III: atypia of undetermined significance
- Category VI: malignant, lymphoma
Board review style answer #2
C. Category III: atypia of undetermined significance
Bland lymphocytic aspirates showing any evidence of monomorphic population are better classified as atypia of undetermined significance. The subsequent excision of a lymph node adjacent to submandibular gland showed a follicular lymphoma.
Comment Here
Reference: Milan system
Bland lymphocytic aspirates showing any evidence of monomorphic population are better classified as atypia of undetermined significance. The subsequent excision of a lymph node adjacent to submandibular gland showed a follicular lymphoma.
Comment Here
Reference: Milan system