Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Benign metastasizing mixed tumors | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Cite this page: Xu B. Pleomorphic adenoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/salivaryglandspleomorphicadenoma.html. Accessed April 26th, 2024.
Definition / general
- Benign triphasic salivary gland neoplasm composed of epithelial (ductal) cells, myoepithelial cells and chondromyxoid stroma
Essential features
- Triphasic salivary gland tumors with ductal cells, myoepithelial cells and stromal component
- Most common salivary gland neoplasm
Terminology
- Benign mixed tumor
Epidemiology
- Most common salivary gland tumor in both children and adults (Hum Pathol 2018;73:194, El-Naggar: WHO Classification of Head and Neck Tumours, 4th Edition, 2017)
- Affects patients of all ages, most commonly in 30s - 60s
- F > M (2:1)
Sites
- Most commonly affected site is the parotid gland (84% of cases)
- May also occur in other major salivary glands (submandibular and sublingual glands), lacrimal gland and minor salivary glands of upper aerodigestive tract (El-Naggar: WHO Classification of Head and Neck Tumours, 4th Edition, 2017)
Etiology
- Prior radiation increases the risk of developing pleomorphic adenoma
Clinical features
- Slow growing, painless, well circumscribed mass involving salivary gland
Diagnosis
- Diagnosis can be rendered on preoperative cytology or biopsy, showing typical metachromatic fibrillary stroma (in cytology) or triphasic growth pattern (on biopsy)
Benign metastasizing mixed tumors
- Rare, controversial clinical entity with late metastasis (6 - 52 years) after tumor excision
- Metastatic sites include bone, CNS, kidney, liver, lung, lymph nodes, maxilla, pharynx, skin, sphenoid sinus
- Benign morphology in original and metastatic tumor
- Associated with incomplete pleomorphic adenoma surgery / local recurrence, post cardiac transplant patient / immunosuppression (Mod Pathol 1998;11:1142)
Radiology description
- Mass with well defined or bosselated border, hyperintense on T2 MRI
Prognostic factors
- Benign tumor: surgical resection with negative margin is considered curative
- Enucleation is associated with 15 - 25% risk of local recurrence
- Recurrences are usually within 18 months but can be up to 50 years later (Arch Pathol Lab Med 2008;132:1445)
- Risk of malignant transformation is ~5%
- Risk factors for malignant transformation: multiple recurrences, submandibular location, older age, larger size, prominent hyalinization, increased mitotic rate (if present, sample tumor more thoroughly), radiation exposure
Case reports
- 6 year old girl with pleomorphic adenoma of the parotid gland (Children (Basel) 2018;5:E127)
- 28 year old man with submandibular mass (Case #243)
- 54 year old man with painless swelling over left half of upper lip for past 10 years (Case #392)
- 84 year old man, a former smoker, with enlarging parotid gland lesion (Case #404)
- Metastasizing pleomorphic adenoma with recurrent PLAG1 or HMGA2 fusion (Am J Surg Pathol 2019;43:1145)
Treatment
- Complete surgical resection with negative margin is the mainstream treatment
- Enucleation is not advocated given the high risk of local recurrence
- Radiation therapy may be considered in symptomatic recurrent cases not amenable to surgical treatment (El-Naggar: WHO Classification of Head and Neck Tumours, 4th Edition, 2017)
Clinical images
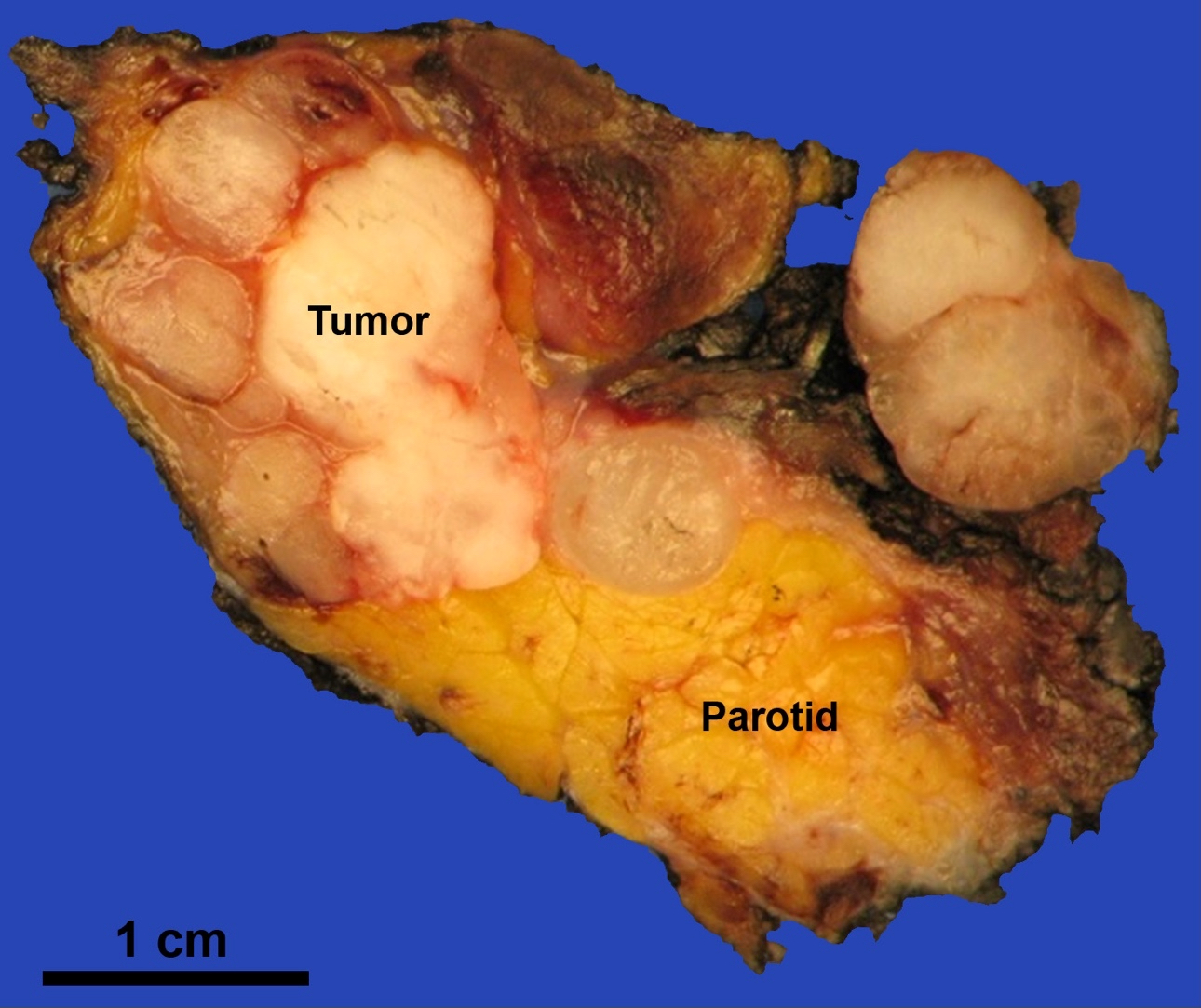
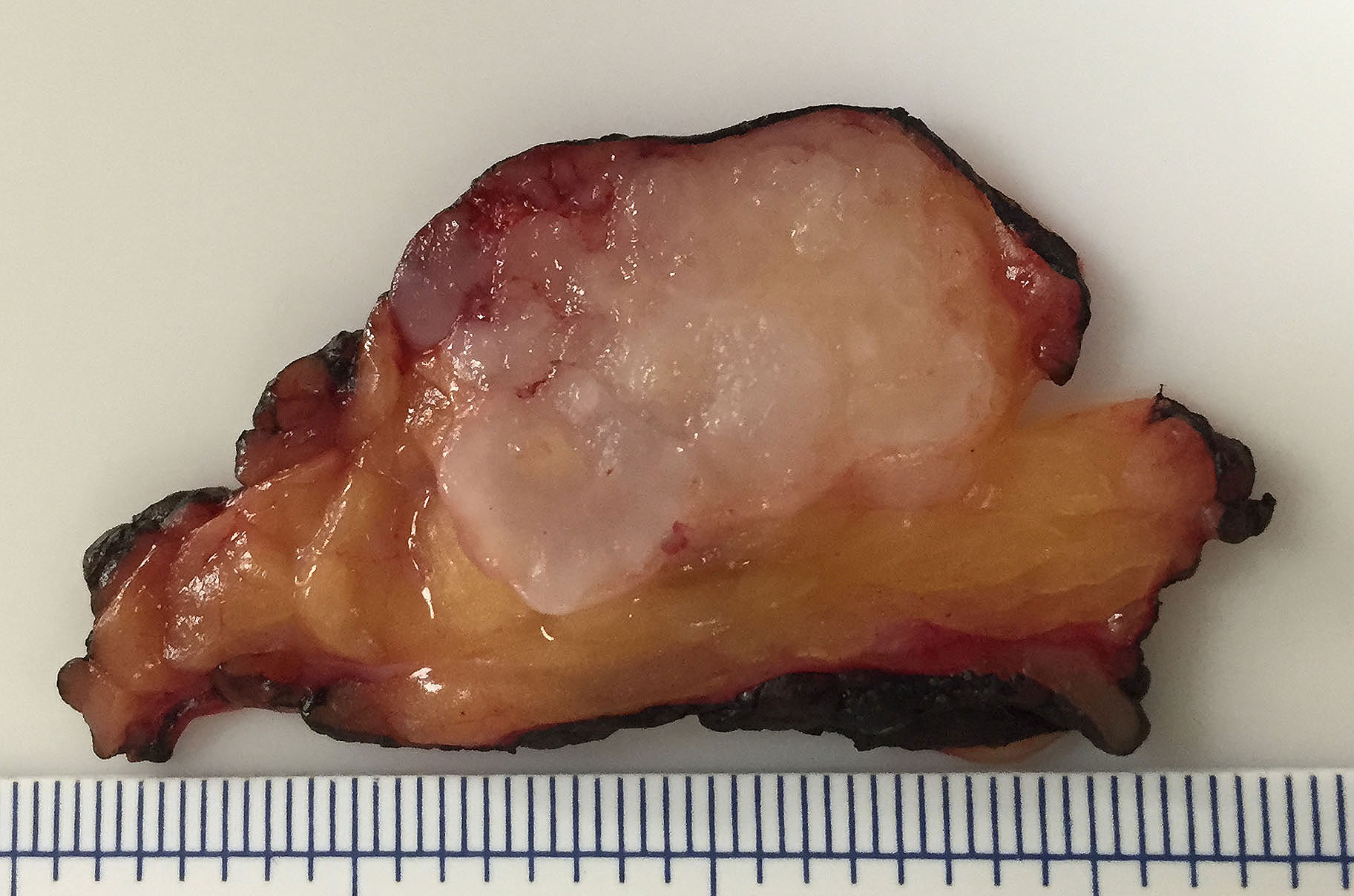
Gross description
- Primary tumor: well demarcated, bosselated gray-white myxoid mass
- Recurrent tumor: numerous myxoid to fibrotic nodules of various size, giving a shotgun bullet appearance
Gross images
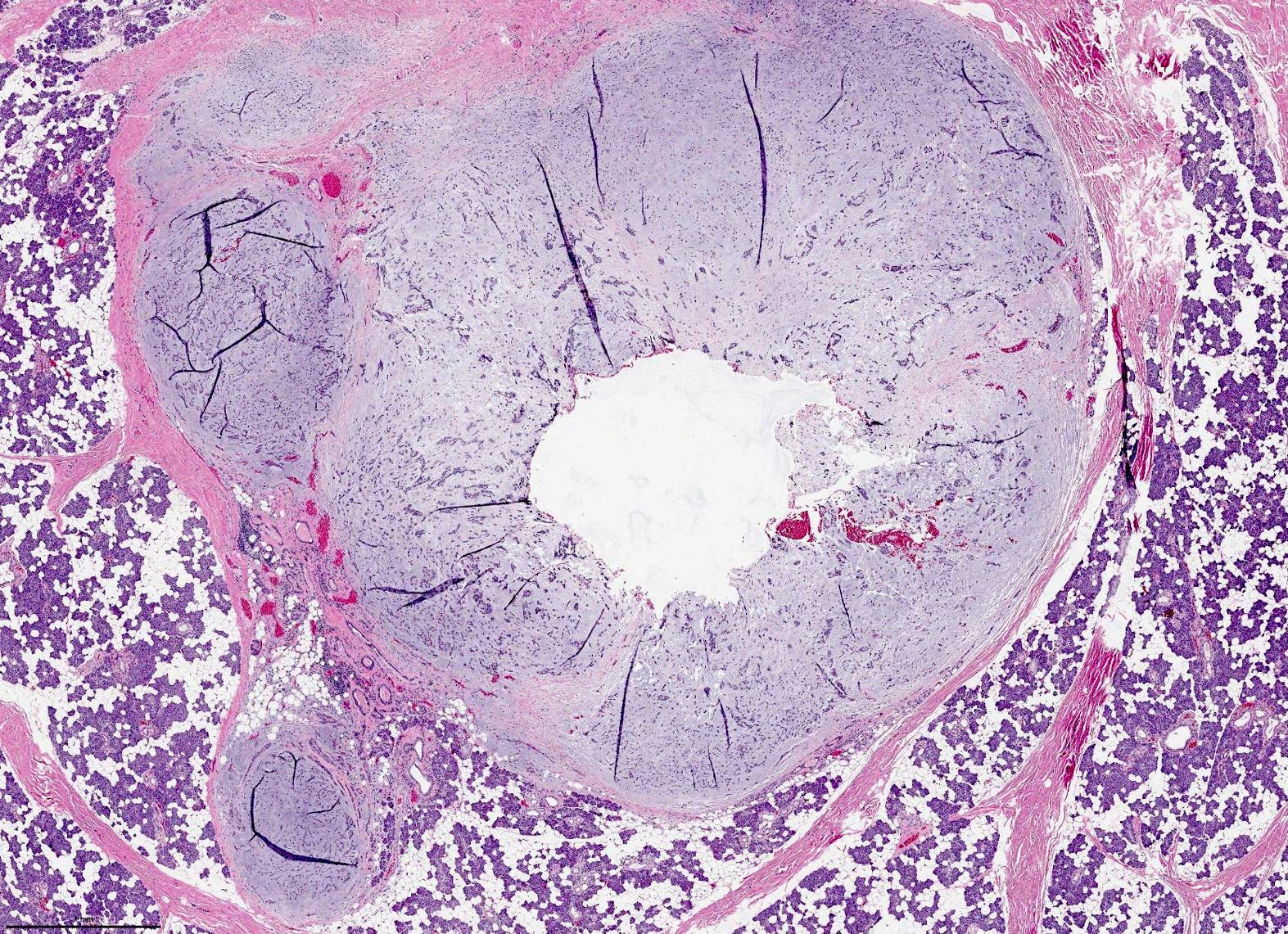
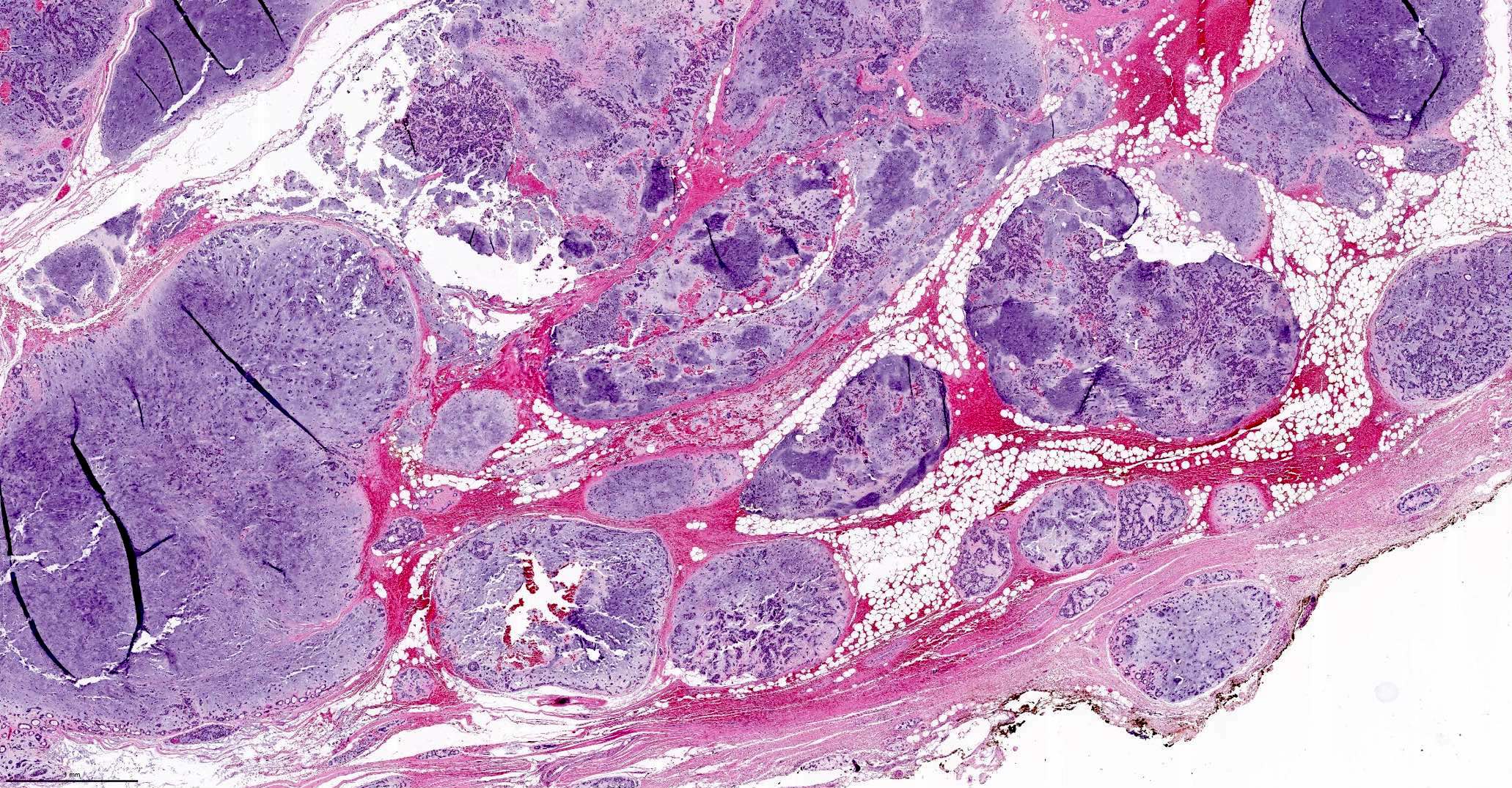
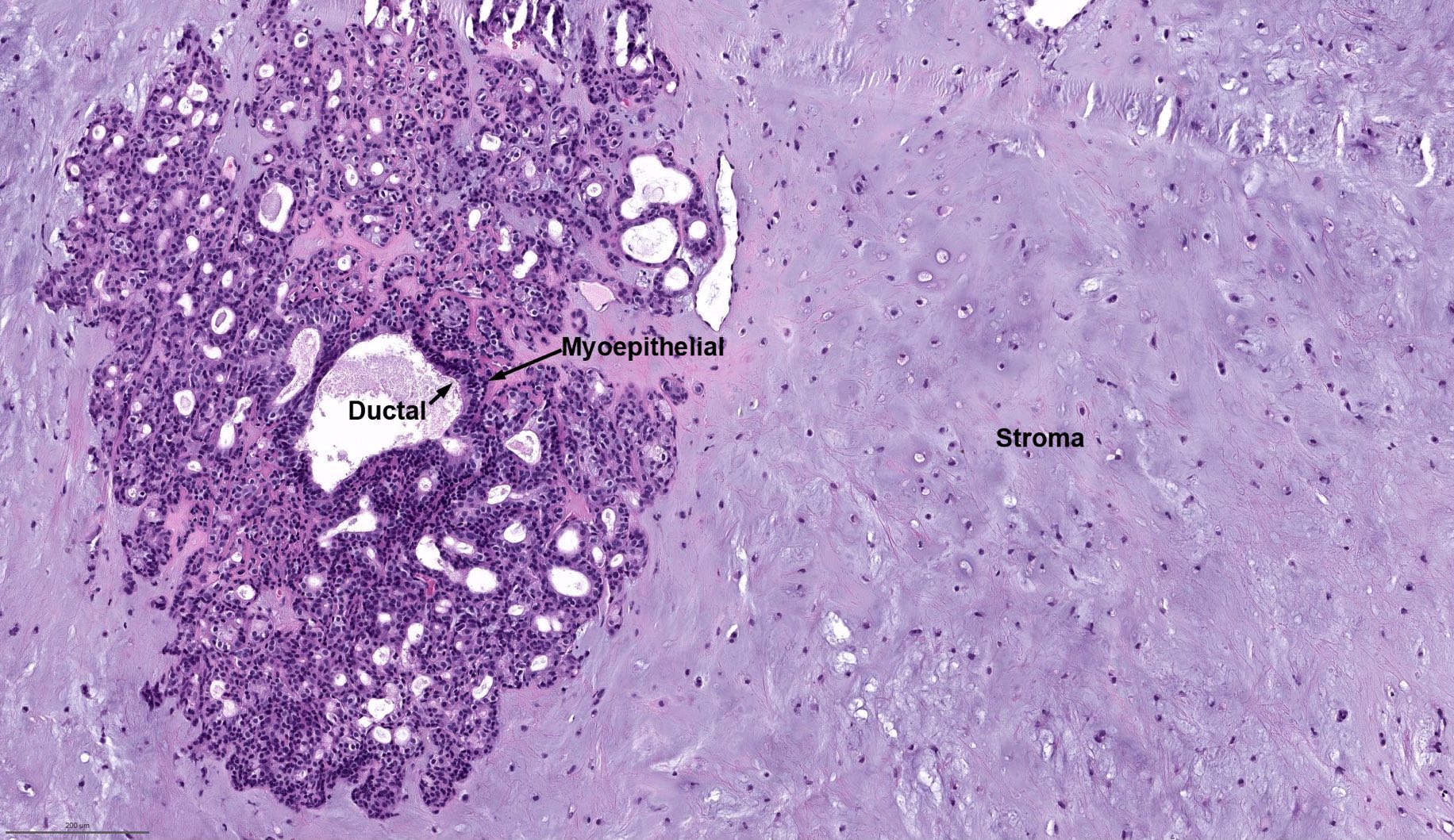
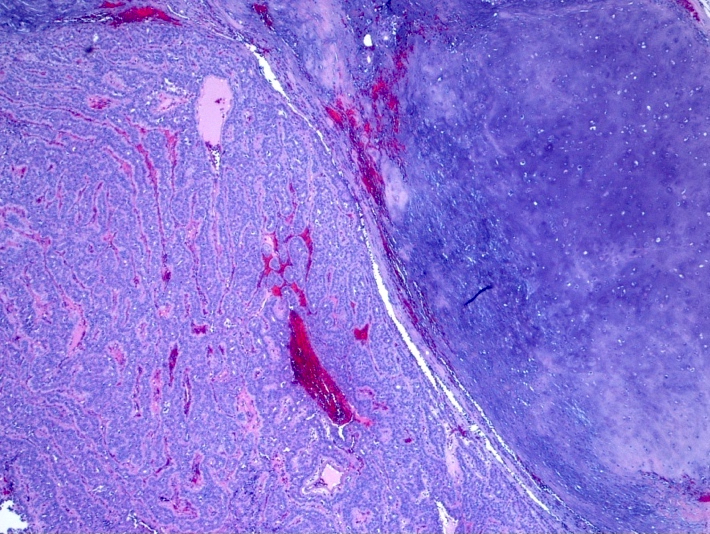
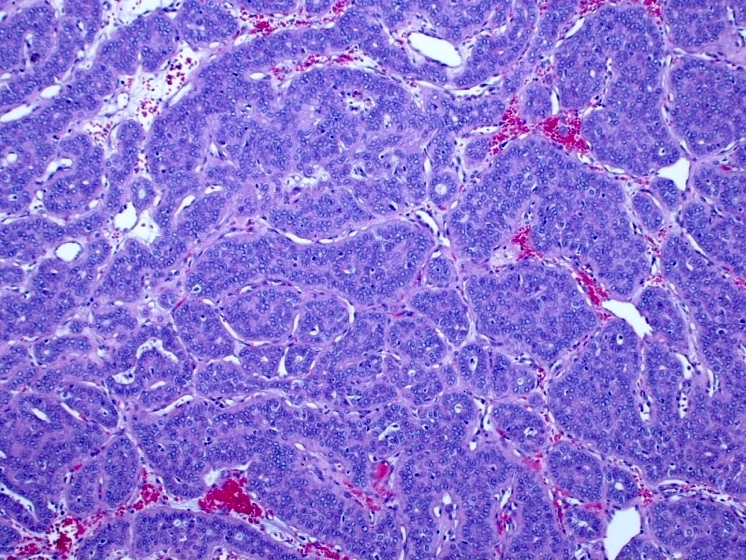
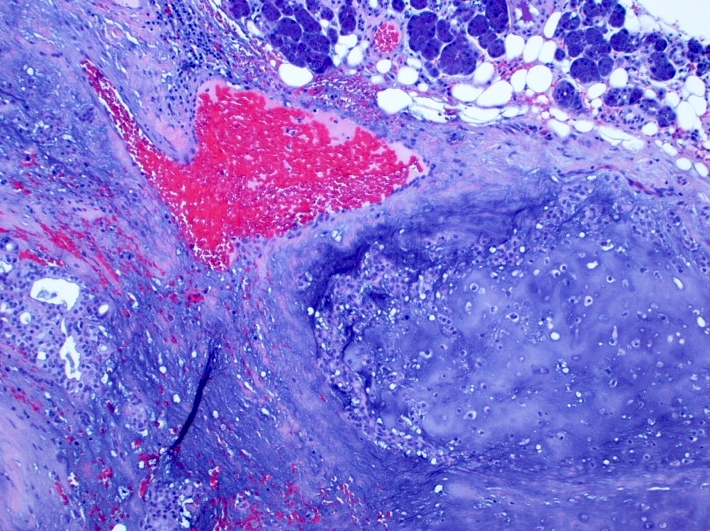
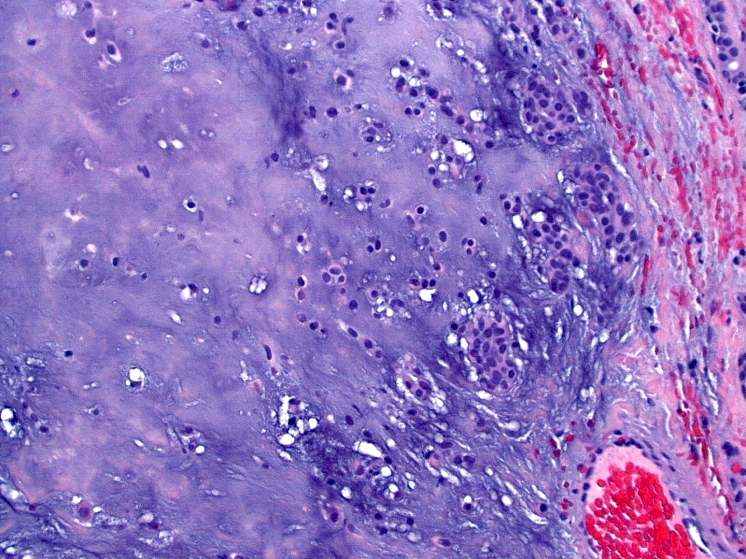
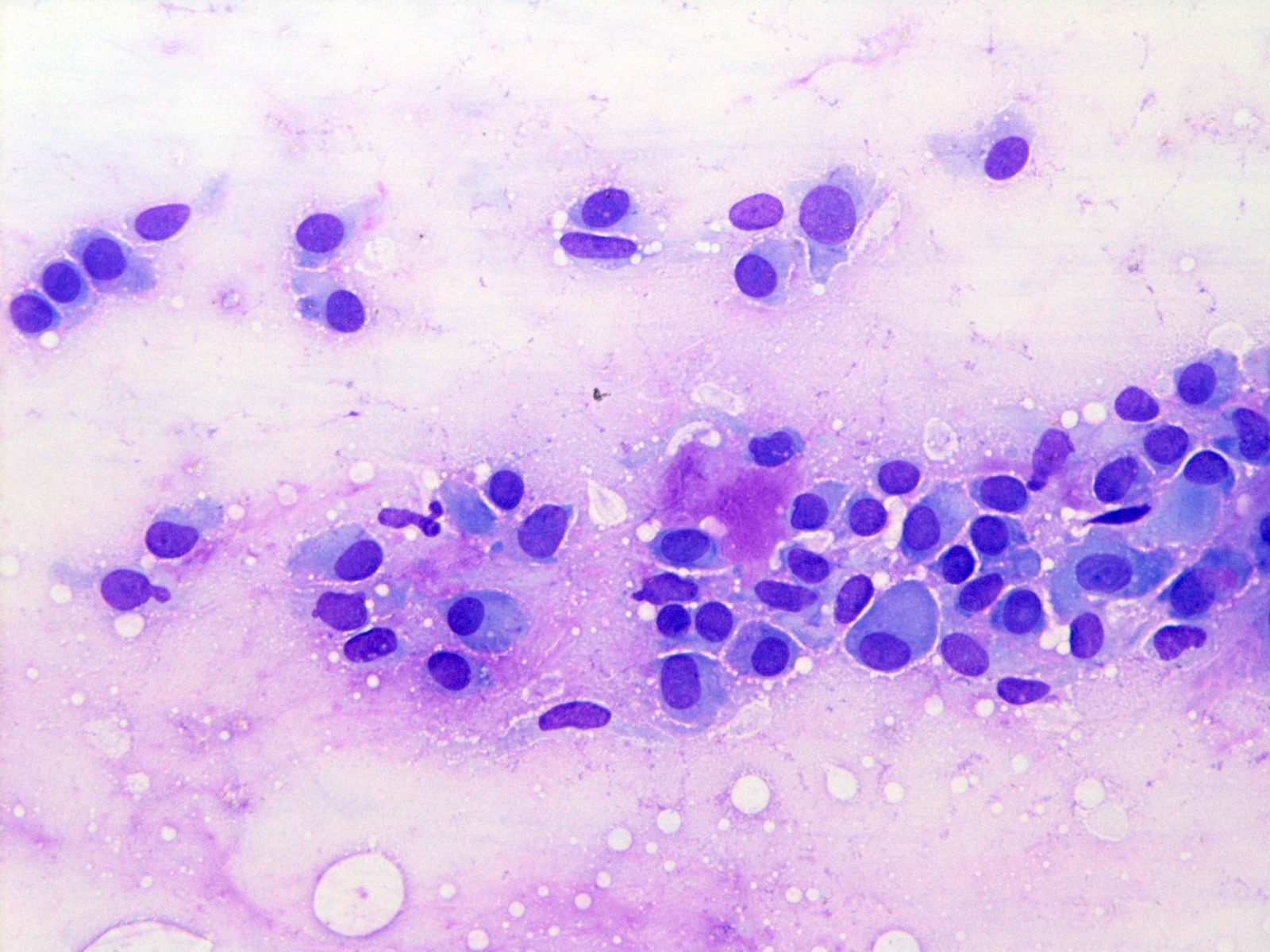
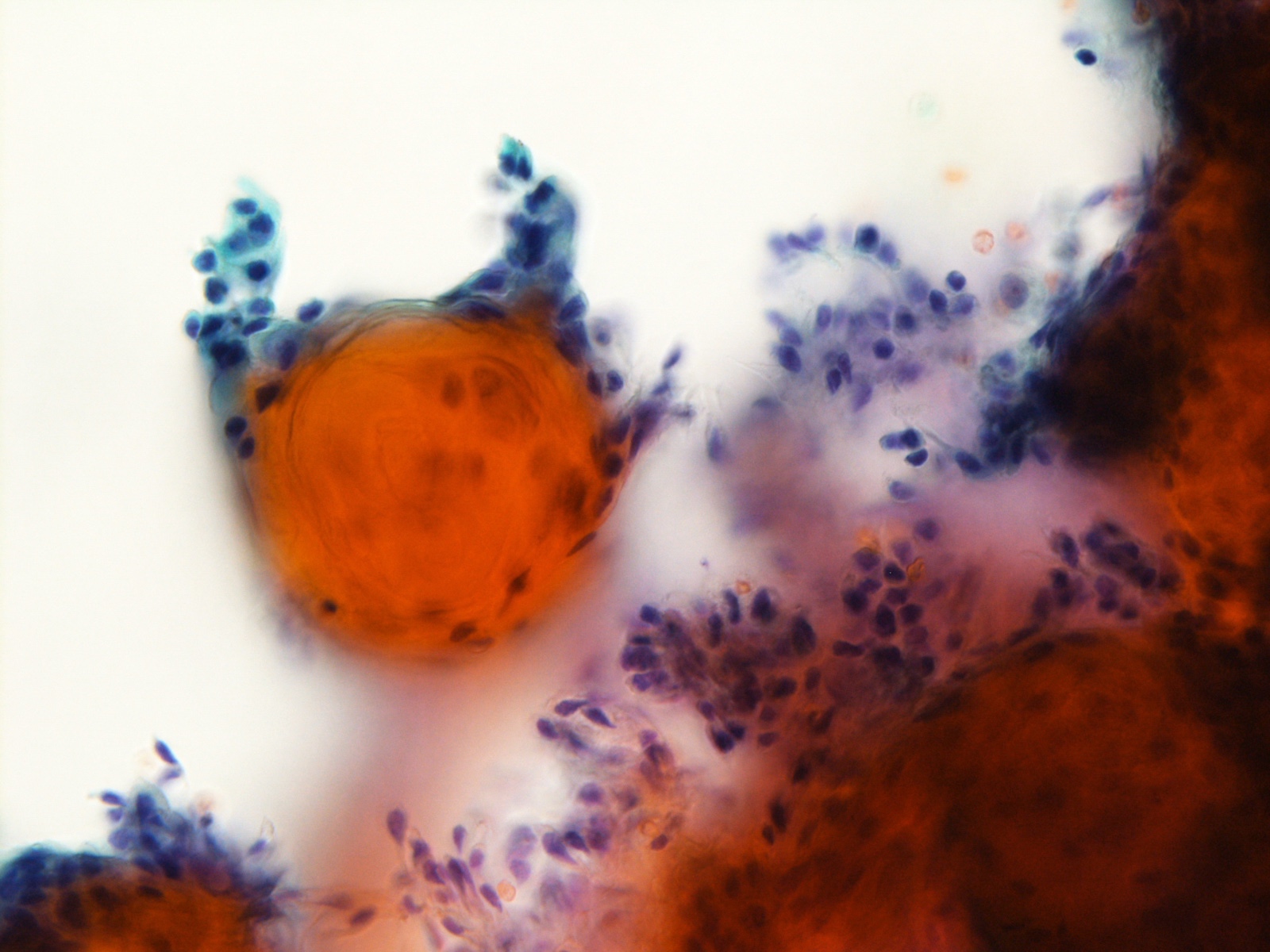
Microscopic (histologic) description
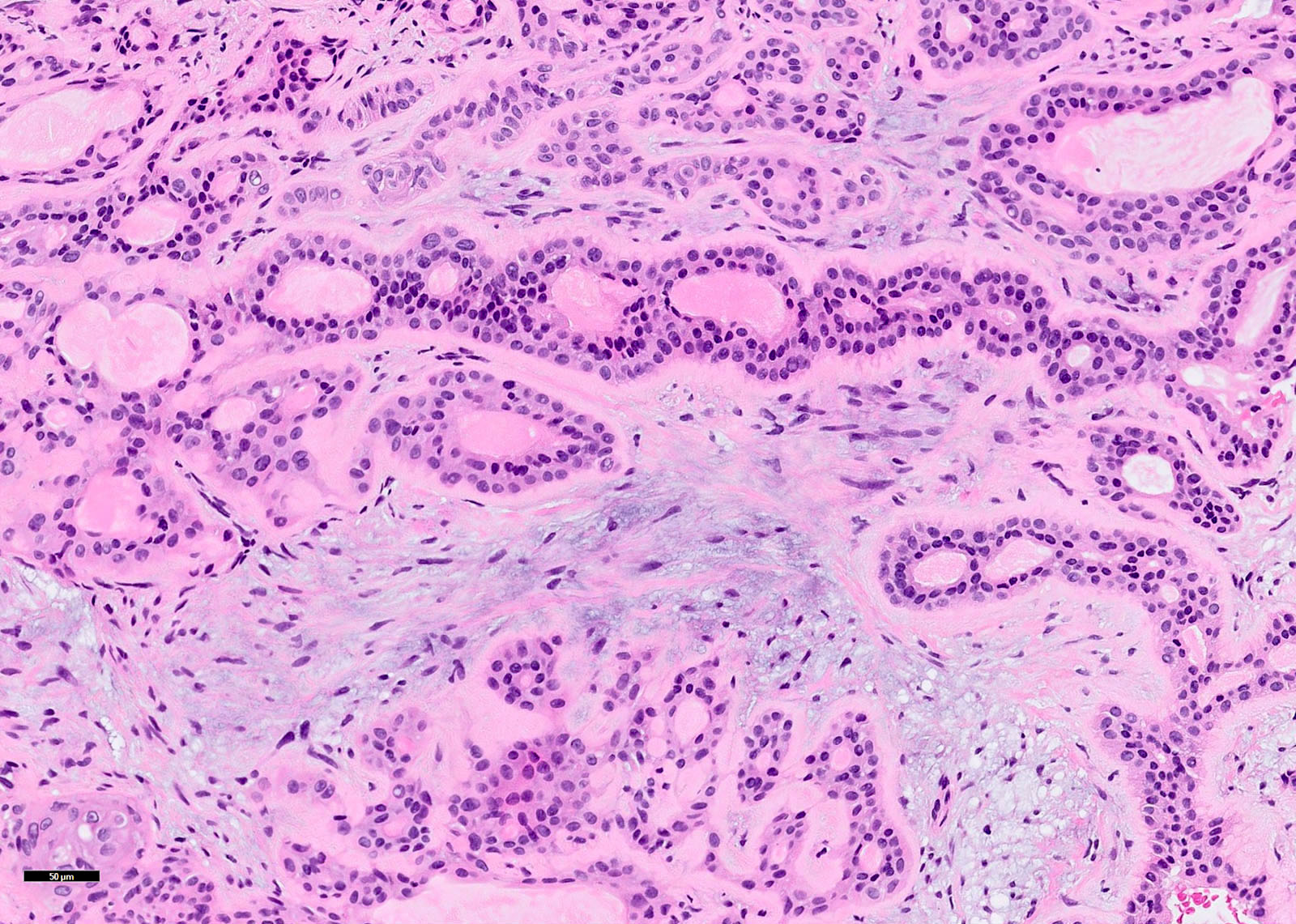
- Bosselated outer surface, often with tongue-like protrusions (pseudopods)
- Typically has 3 components:
- Epithelial (ductal) component forming the inner layer of cysts and tubules
- Myoepithelial cells as the outer layer of cysts and tubules and scattered within the myxoid stroma
- Cytology of myoepithelial cells can be plasmacytoid, spindled, epithelioid, clear or stellate shaped
- Stromal component is typically myxoid, chondroid or myxochondroid
- It can also be hyalinized or fibrotic
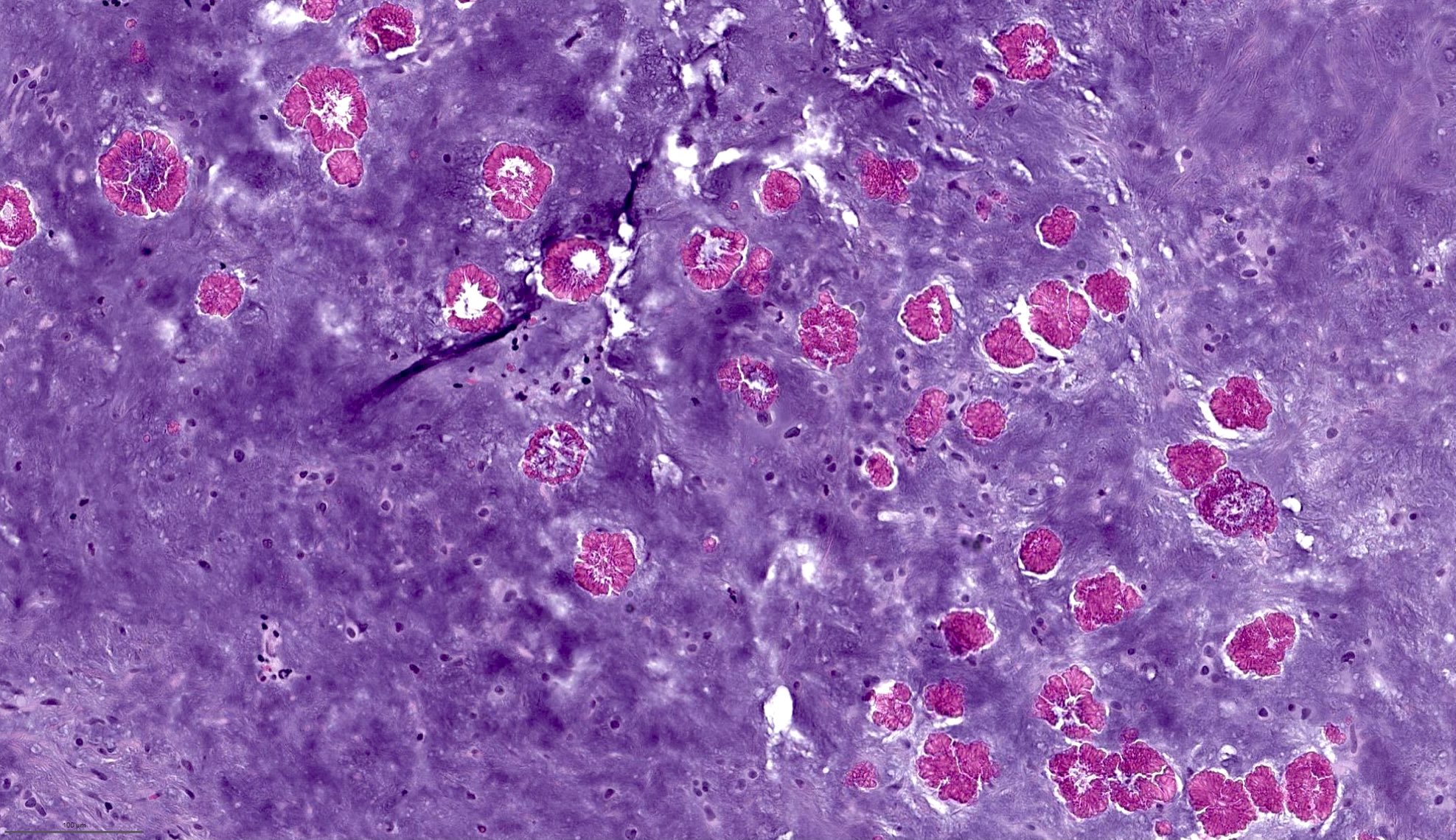
- Metaplastic changes may be seen, e.g. adipose metaplasia, osseous metaplasia, squamous metaplasia (sometimes with keratinization), sebaceous metaplasia and mucinous metaplasia
- Intravascular permeation has been reported in a small percentage of cases and does not increase the risk of recurrence or distant metastasis
- It is proposed to be a phenomenon associated with surgical manipulation (Am J Surg Pathol 2012;36:1674)
- Other features that may be seen in pleomorphic adenoma include
- Tyrosine crystal: dense amorphous eosinophilic floret shaped crystal
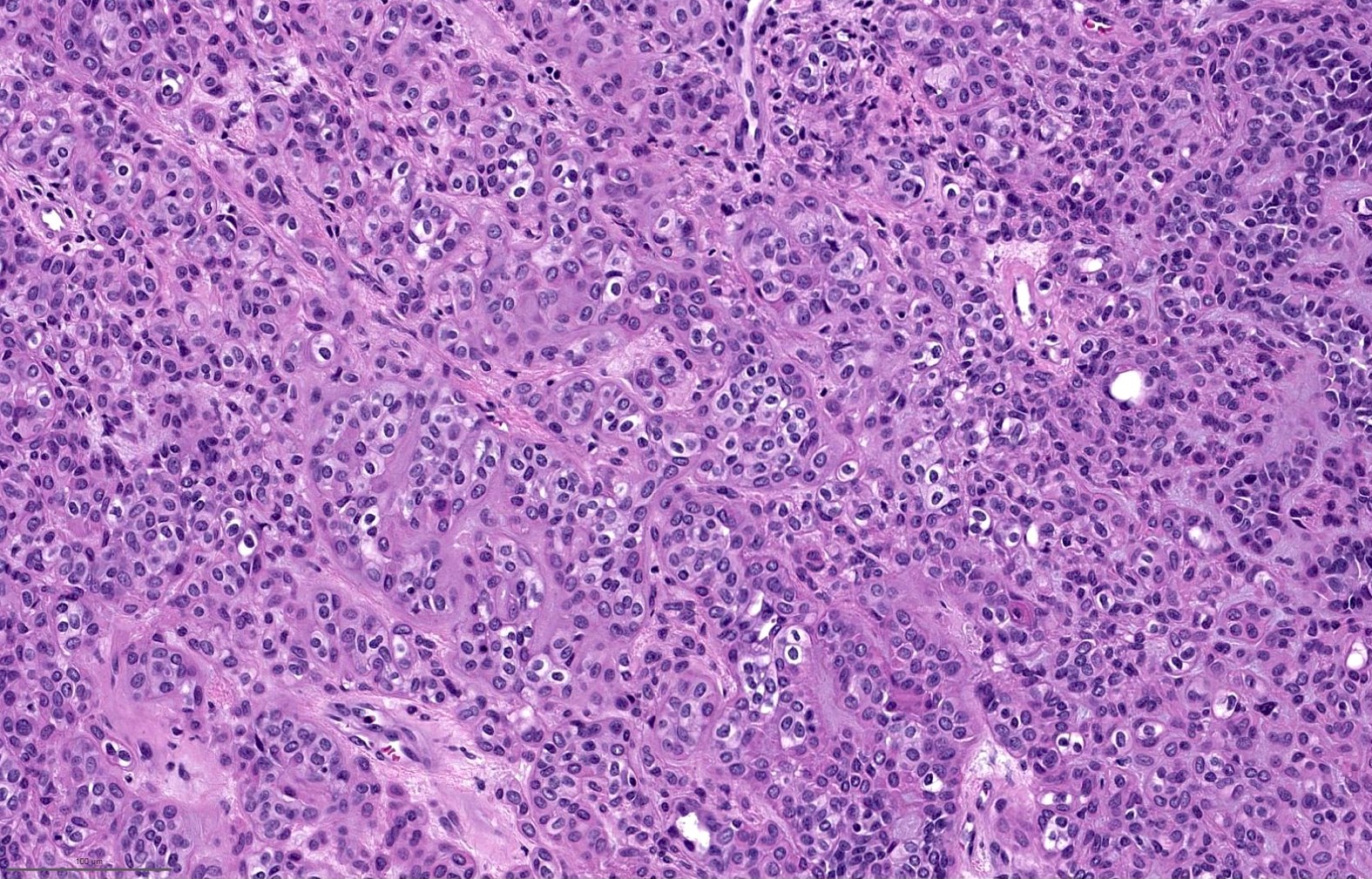
- Increased cellularity: so called cellular pleomorphic adenoma
- Increased mitotic activity
- Myoepithelial rich area or tumor
Microscopic (histologic) images
Contributed by Bin Xu, M.D., Ph.D. and Andrey Bychkov, M.D., Ph.D.
Case #404
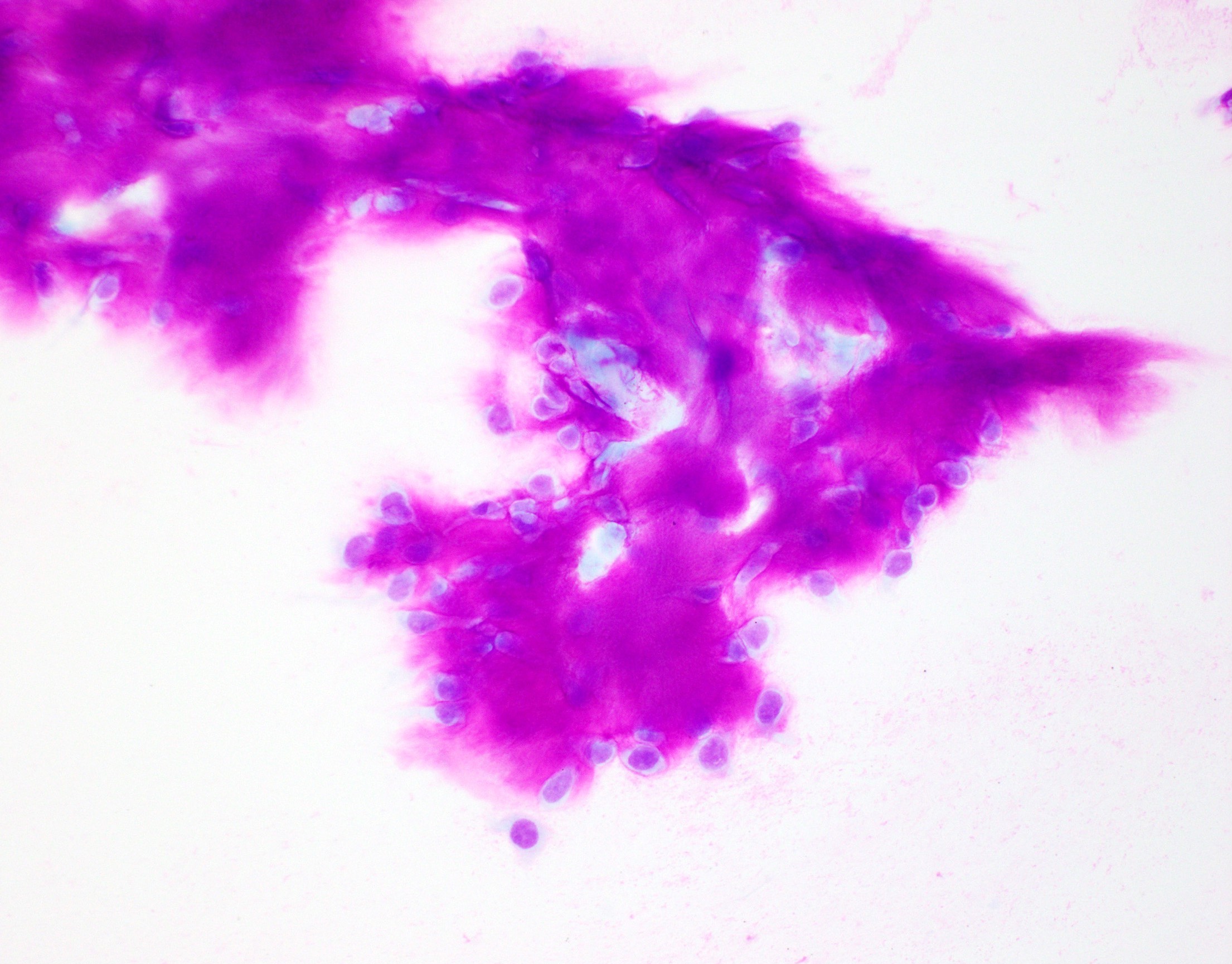
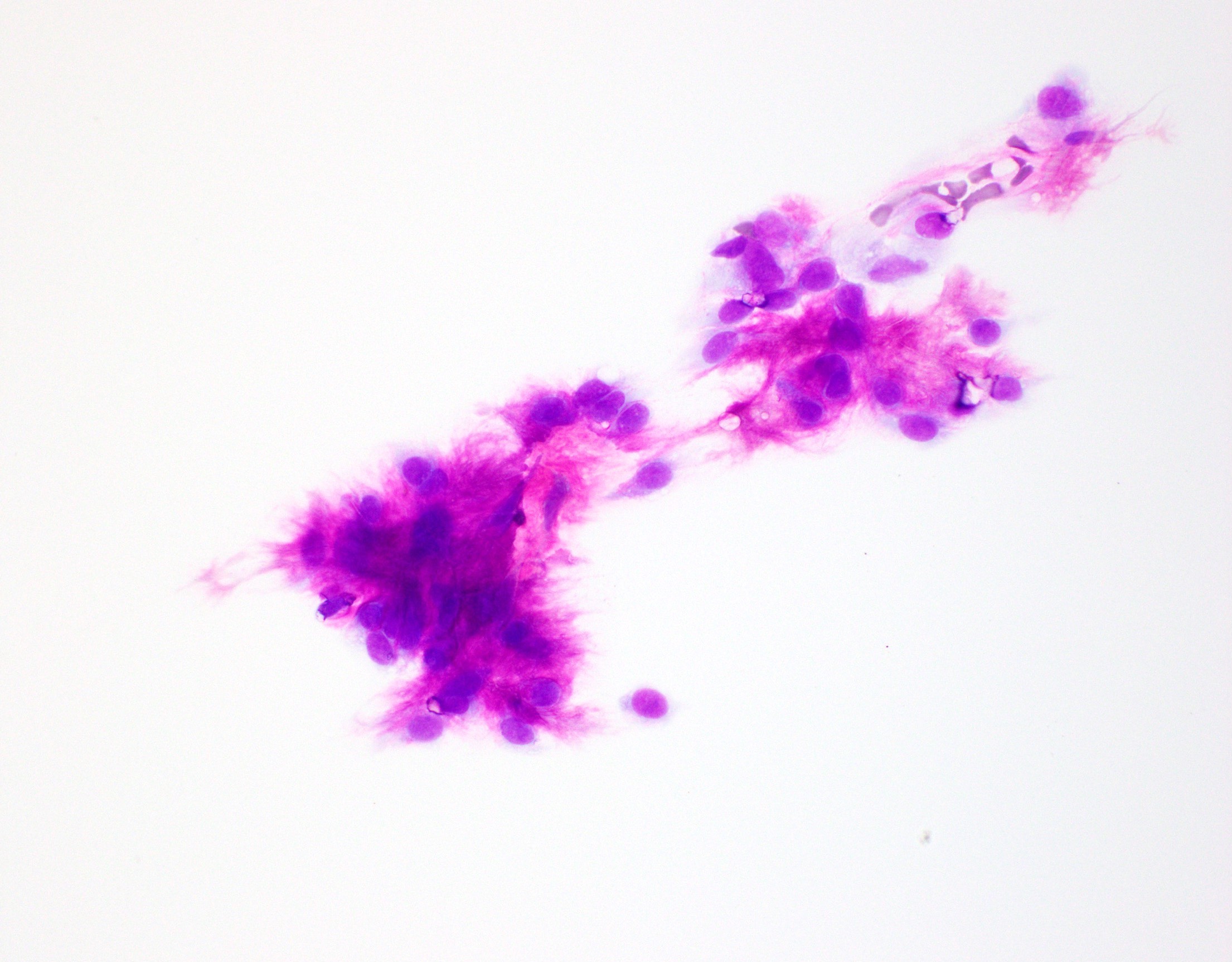
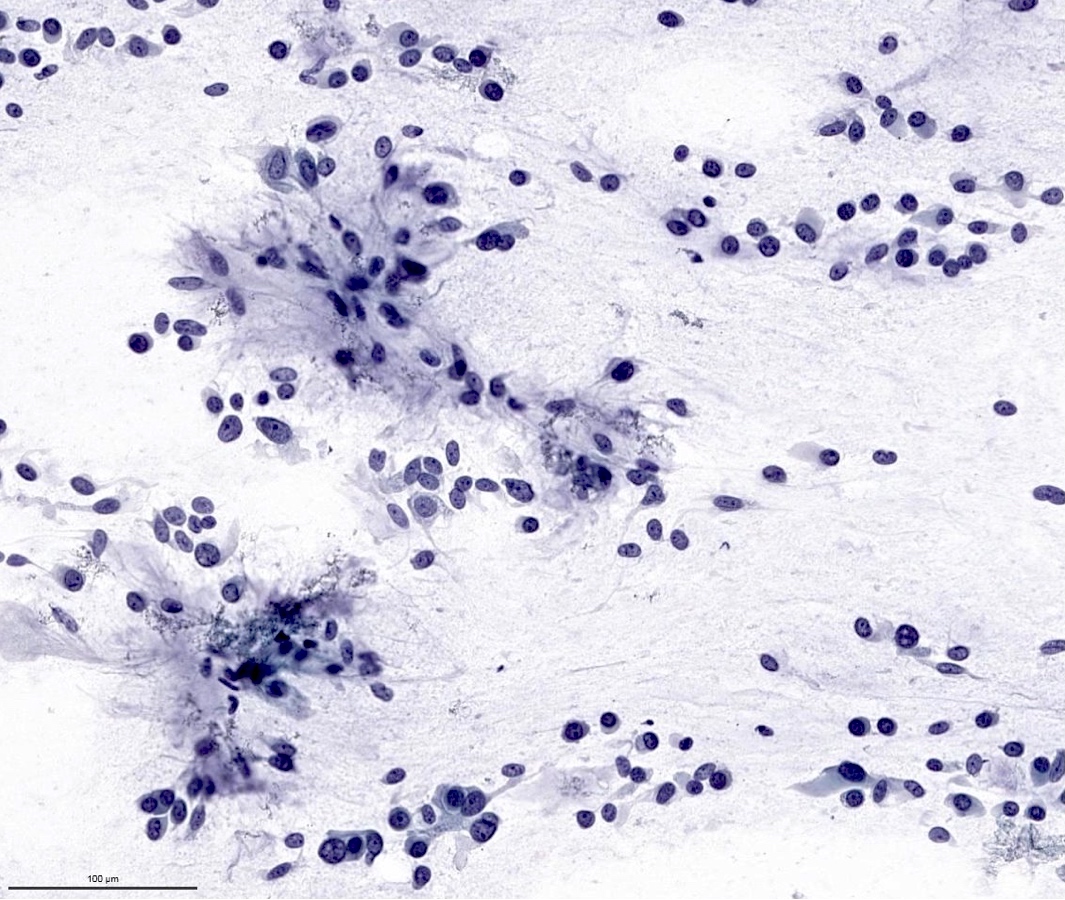
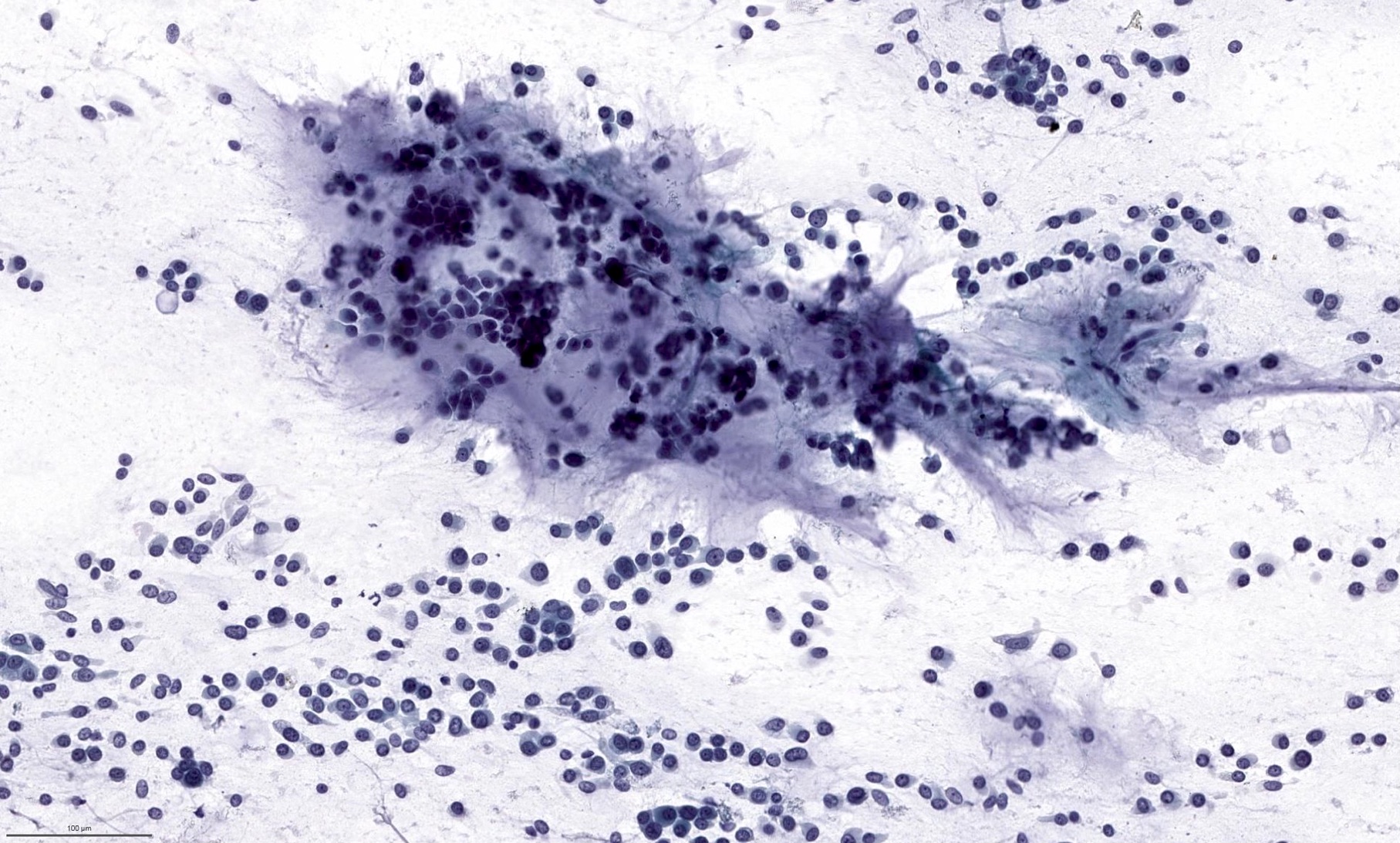
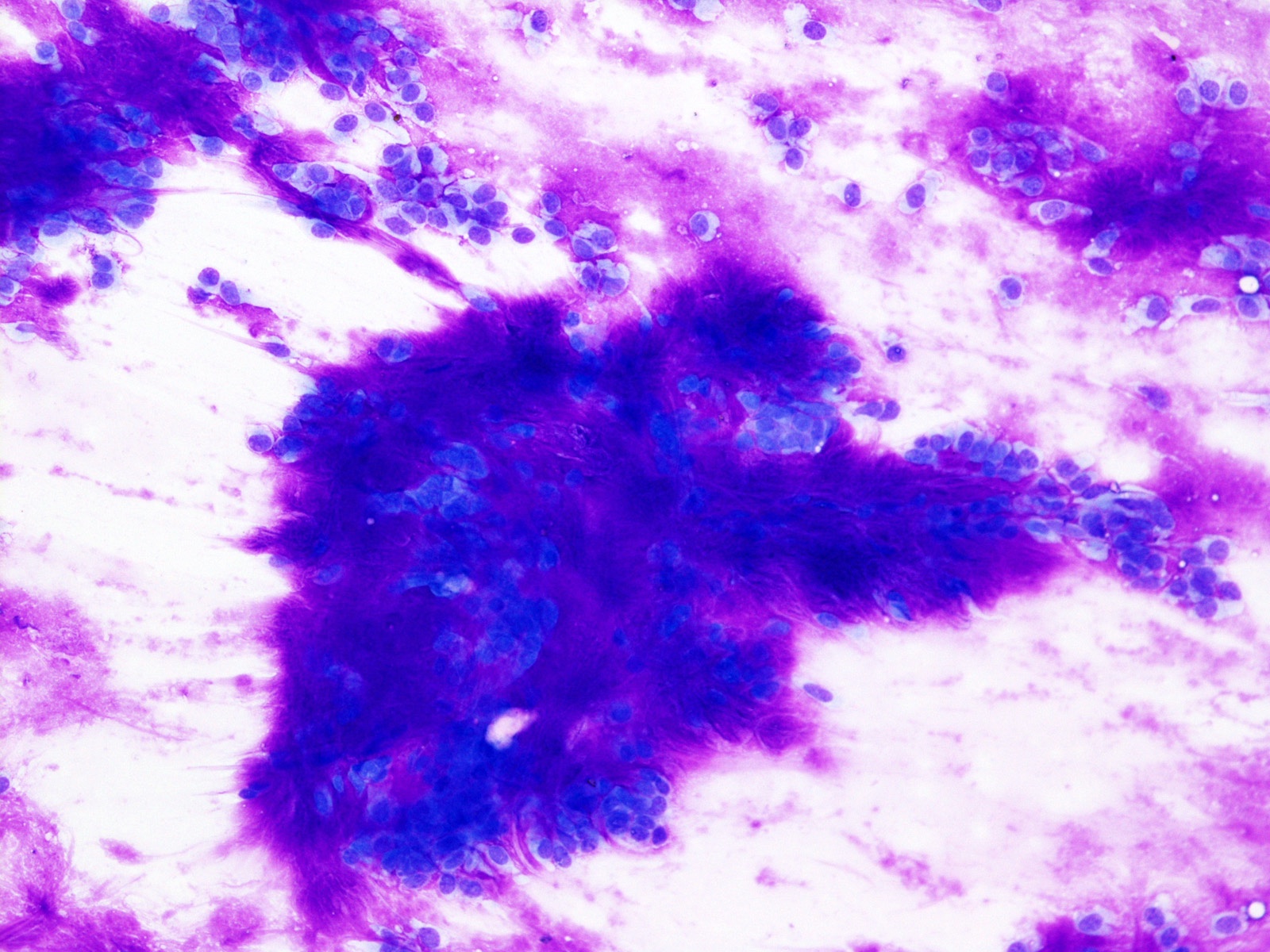
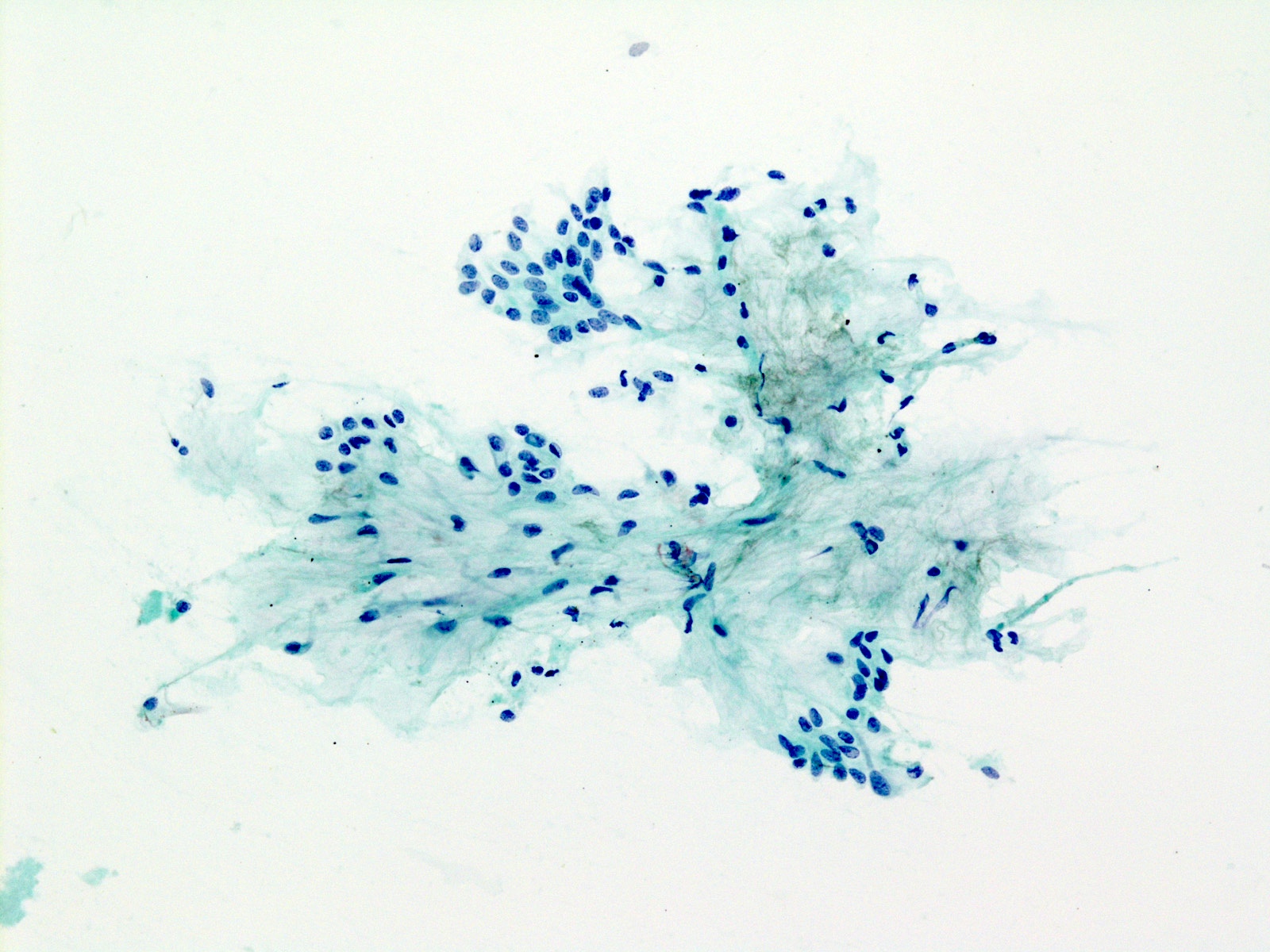
Cytology description
- Matrix containing tumor
- Typical feature is its unique fibrillary stroma
- Mixture of myoepithelial cells, ductal cells and extracellular stroma
- Myoepithelial cells are usually the predominant cell type with various cytomorphology, including round, polygonal, plasmacytoid, spindle, etc.
- Ductal cells show bland cytologic features with organized honeycombing or ductal arrangement
- Extracellular matrix shows characteristic feathery / fibrillary borders and bright magenta color on Romanowsky type stain and gray-green chondromyxoid features on Papanicolaou stain
Cytology images
Positive stains
- Ductal (epithelial) cells are typically positive for cytokeratins (e.g. AE1 / AE3, CAM5.2 and CK7)
- Myoepithelial cells are positive for GFAP, S100, SOX10, actin - alpha smooth muscle, calponin, p40 and p63
- PLAG1 and HMGA2 can be used as surrogate immunohistochemical markers for underlying PLAG1 or HMGA2 fusion (Histopathology 2018;72:285, Histopathology 2017;71:511)
Molecular / cytogenetics description
- PLAG1 fusion (chromosome 8q12) or HMGA2 fusion (chromosome 12q14-15) is present in ~70% of pleomorphic adenomas (Oncogene 1998;16:1409, Cancer Res 1997;57:13)
Sample pathology report
- Parotid, left, parotidectomy:
- Pleomorphic adenoma, 2.0 cm, margins negative for tumor
Differential diagnosis
- Carcinoma ex pleomorphic adenoma (malignant mixed tumor):
- Demonstrates frank evidence of malignancy, e.g. marked nuclear pleomorphism, frank necrosis, invasion beyond pre-existing capsule, perineural or lymphovascular invasion
- Both may contain PLAG1 or HMGA2 fusion (Hum Pathol 2015;46:26)
- Myoepithelioma and myoepithelial carcinoma:
- Contain (nearly) exclusively myoepithelial cells
- Ductal (epithelial) component is scant or absent
- Other salivary gland neoplasms (adenoid cystic carcinoma, polymorphous adenocarcinoma, epithelial myoepithelial carcinoma):
- Pleomorphic adenoma may show various architectural and cytologic features that resemble other salivary tumors
- Identifying areas typical of pleomorphic adenoma with triphasic ductal, myoepithelial and stromal components is helpful to establish the diagnosis
- Squamous cell carcinoma:
- Both may contain squamous epithelium with keratinization and may be difficult to differentiate in small biopsy or cytology material
- Is not triphasic; identification of ductal, epithelial and stromal components typical of pleomorphic adenoma rules out squamous cell carcinoma
Board review style question #1
Board review style answer #1
Board review style question #2
Which of the following statements regarding pleomorphic adenoma is true?
- Carries nearly zero risk of recurrence or malignant transformation
- Characterized by architectural diversity and is composed of one single type of cells
- Is the most common salivary gland neoplasm
- Typically treated with enucleation
Board review style answer #2
C. Pleomorphic adenoma is the most common salivary gland neoplasm
Comment Here
Reference: Pleomorphic adenoma
Comment Here
Reference: Pleomorphic adenoma
Board review style question #3
Board review style answer #3
C. Pleomorphic adenoma
Magenta colored extracellular matrix with feathery / fibrillary borders and intermingled bland myoepithelial cells are characteristic features for a pleomorphic adenoma.
Comment Here
Reference: Pleomorphic adenoma
Magenta colored extracellular matrix with feathery / fibrillary borders and intermingled bland myoepithelial cells are characteristic features for a pleomorphic adenoma.
Comment Here
Reference: Pleomorphic adenoma